Supplemental Digital Content is available in the text.
Abstract
Background:
Cosmetic surgery tourism is rapidly becoming more prevalent in the United Kingdom. We aim to identify the motivational factors underlying patients’ decisions to go abroad for their treatment and gather information about the ensuing complications.
Methods:
A retrospective review (January 2013–August 2017) was conducted of patients seen at a single major trauma center for complications from cosmetic surgery performed overseas. Cost analysis was performed based on national tariffs. Complications were grouped based on Clavien-Dindo classification and the Clinical Commissioning Group cost. A telephone survey was conducted to evaluate reasons for travel, details of complications, and impression of healthcare at home and abroad.
Results:
A total of 20 patients (one male, 19 females) with a mean age 36 years (23–59 years) were included. Lower cost was the most popular reason for travel, followed by lack of expertise and friend’s recommendation. Abdominoplasty (n = 9) had the highest number of complications followed by gluteal augmentation (n = 7). All major complications were due to gluteal augmentation (n = 4). The cost was for minor (n = 8, £3,448), intermediate (n = 8, £18,271), and major (n = 4, £42,083.59) complications.
Conclusions:
We raise serious concerns about the lack of regulation in cosmetic tourism and the absence of patient follow-up abroad. A particular concern was all gluteal augmentation cases had major complications. An international consensus to regulate surgical practice abroad is crucial to protect patients’ interests and promote safe cosmetic surgery.
INTRODUCTION
The cosmetic surgery industry is expanding at such a rate that it has outgrown the regulations that aim to monitor its practice. The International Society of Aesthetic Plastic Surgery (ISAPS) statistics in 2017 revealed an overall 9% rise in cosmetic procedures over 12 months.1 There is an increasing trend for patients to seek cosmetic surgery abroad for a multitude of factors, including ease of access to surgery, lower costs, affordable airfares, positive marketing, and use of social media for foreign surgeons or even friends’ recommendations. However, the exact reasons behind the choice of certain countries over others remain unknown.2–4 The overarching reason for travel is failure to qualify for free cosmetic surgery under the National Health Service (NHS). The stringent criteria include body mass index (BMI, <25 kg/m2), not smoking and the ability to demonstrate functional impairment or significant psychological distress.5,6
There are only a few reports about the outcome, cost, and patient perception of cosmetic surgery abroad.7–9 None of those articles covered all 3 aspects with patient perception in particular being ignored. The purpose of this study is to determine the complications of these operations, cost implications for the NHS, and patients’ views. The main motivation for seeking treatment abroad and the concerns about complications were investigated in the patient survey. Our study is novel as it aims to encompass all of these factors related to cosmetic surgery tourism.
METHODS
Study Population
A retrospective review was conducted in a tertiary hospital (The Royal London Hospital, Barts Health NHS Trust) for patients with complications following cosmetic surgery abroad. The project was approved by local institutions before data collection. The timeline for data spanned from January 2013 to August 2017. A minimum follow-up period of 6 months was mandatory.
Clinical Data Collection
The criteria for inclusion were being a patient with permanent residence in the United Kingdom, who had a cosmetic operation performed outside of the United Kingdom. The exclusion criteria was applied to the patients who were lost to follow-up due to relocation to a different country or county or whose care was transferred to another hospital.
Medical records based on cosmetic surgery codes were used to identify patients. Data were collected regarding basic demographics, medical comorbidities, smoking status, country and type of cosmetic surgery, complications, and timing of management [either early (<30 days) or delayed (>30 days)]. Data on number of admissions, length of inpatient hospital stay, outpatient (including dressing) clinics attended were also retrieved.
Cost Analysis
Patients were managed either as inpatients, outpatients, or a combination of both. Cost analysis was based on the NHS tariff and included inpatient hospital stay, investigations, and outpatient clinic appointments. The calculation used the following formula to work out an equitable reimbursement for similar treatments: Health Resource Groups × Market Forces Factor. The calculated cost is claimed from national health funding providers, Clinical Commissioning Groups (CCGs) across the United Kingdom. Complications were grouped into minor, intermediate, and major based on the cost and the CCG funding category. The Clavien-Dindo classification was used as a second system to group complications.10
Patient Telephone Survey
Patients were contacted via telephone to establish their views about their treatment abroad. The survey was conducted by one of the authors for consistency [SDC1; see figure, Supplemental Digital Content 1, which displays a breakdown of complications per year (2013–2017), http://links.lww.com/PRSGO/B114]. A total of 11 questions were asked including the reason for seeking treatment abroad, the cost of the procedure and how that compared to the UK quote, overall satisfaction with treatment for the ensuing complication, and whether, in hindsight, they would have had the surgery done in the United Kingdom.
RESULTS
A total of 20 patients (1 male and 19 females) were identified over a 4.5-year study period. Six cases were excluded due to loss of follow-up, transfer of care, or a lack of accurate cost data being available. One patient was excluded from the results analysis due to case complexity, follow-up in a different country, and significant cost implications. The excluded cases were abdominoplasties (n = 3), abdominoplasty and bilateral mastopexy (n = 1), abdominal liposuction (n = 1), liposuction, and fat transfer (n = 1). All excluded cases were managed in the outpatient setting for minor complications.
Mean age of included patients was 36 years (23–59 years). Mean BMI was 31 kg/m2 (20–39). Seven patients were smokers before their overseas operations. One patient with a history of schizophrenia, intravenous drug use and hypertension had multiple simultaneous cosmetic operations (bilateral thigh lift, breast implants, and liposuction) and was later treated for severely infected wounds. Four patients had other comorbidities (Type II diabetes mellitus, anemia, hypertension, and gastric bypass) that may have affected wound healing.
Surgical Procedures
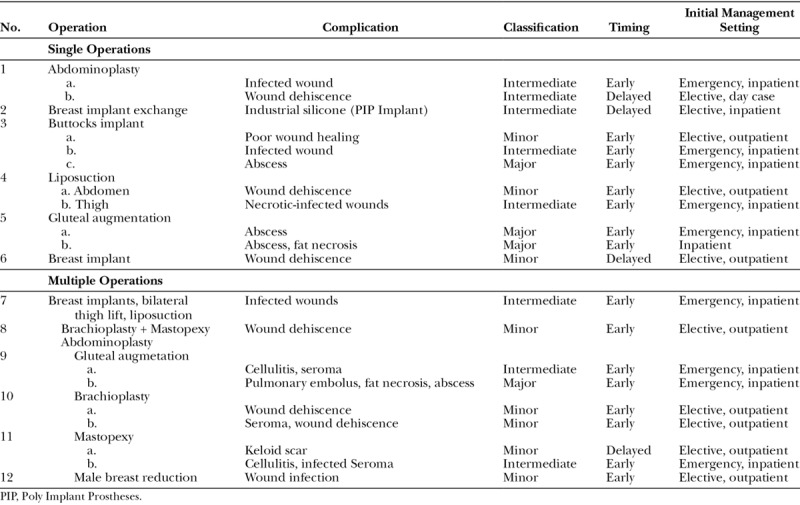
Abdominoplasty was the commonest operation causing complications (n = 9), either as a single operation (n = 2) or combined with other procedures (n = 7). The second commonest was buttock augmentation (n = 7) with either fat transfer (n = 4) or implants (n = 3). Third was breast augmentation (n = 3). The remaining operations causing complications were liposuction (n = 2), breast implant and mastopexy (n = 1), or breast implant exchange (n = 1; Table 1).
Table 1.
Type of Operations Performed Abroad
COMPLICATIONS AND MANAGEMENT SETTING
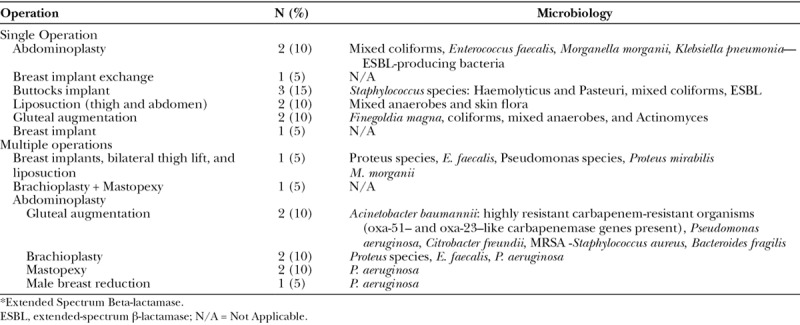
Infection, whether superficial or abscess-forming, was the commonest complication (n = 9) and microbiological findings from wound swabs were taken into account when prescribing antibiotics (Table 1). Complications were grouped based on degree of clinical severity into minor, intermediate, or major. Patients with intermediate and major complications (Clavien-Dindo Grade III and IV, respectively; n = 11) were admitted to hospital at the time of initial presentation. All of the major complications (n = 4) followed buttock augmentation operations performed abroad in 2017 and all required Intensive Treatment Unit (ITU) care. Intermediate complications required an inpatient stay and an emergency operation with 2 sole exceptions: a breast implant exchange (n = 1) and a wound dehiscence following abdominoplasty (n = 1), which were managed electively as an inpatient and as a day case, respectively. Patients with minor complications (Clavien-Dindo Grade II; n = 8) attended outpatient clinics and required pharmaceutical management (eg, antibiotics) only (Table 2). The period of hospitalization was highly variable (ie, 1–35 days; mean = 9 days), the longest being due to ITU admissions and multiple operations. Despite initial management abroad for severe complications in 2 out of 4 cases, patients still traveled back to the United Kingdom early for definitive treatment.
Table 2.
Severity of Complications of Cosmetic Surgery Abroad and Initial Management
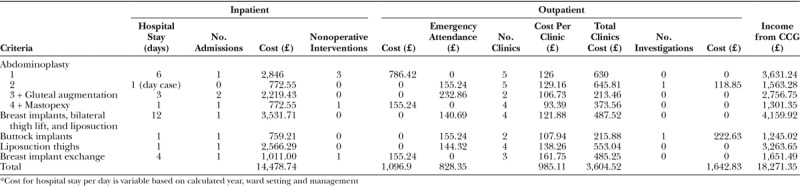
COST ANALYSIS
A detailed cost analysis taking into account complication severity and subsequent management was conducted. Minor and intermediate complications each formed 40% of the study population, whereas major cases provided the remaining 20%. Nevertheless, the total cost of minor cases (£3,448.60) was over 5 times that of intermediate cases (£18,271.35). Major complications (£42,083.59) cost more than double the intermediate group (Tables 3–5). The total cost of all complications was £63,803.54. This underestimates total cost as 6 cases were excluded from the study.
Table 3.
Minor Complications Calculated Cost Analysis for Outpatients Management
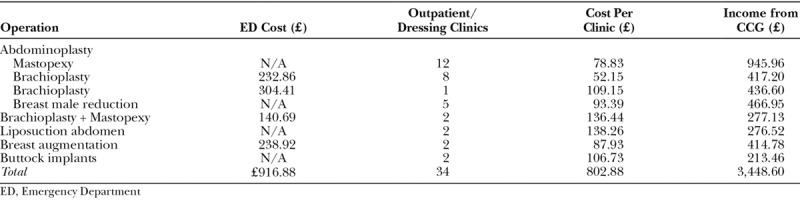
Table 5.
Major Complications Cost Analysis
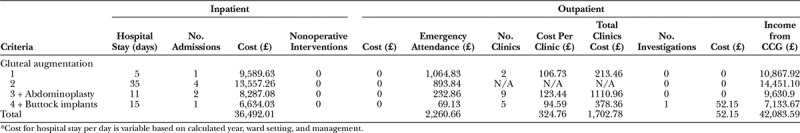
Table 4.
Intermediate Complications Cost Analysis
PATIENT SATISFACTION SURVEY
A total of 12 patients completed the telephone survey, which constituted a 60% response rate. The remaining patients were not contactable due to changes in telephone numbers. We captured views across all complication categories (minor, intermediate, and major) on reasons for travel and on postoperative care both abroad and in the United Kingdom (Figs. 1 and 2).
Fig. 1.
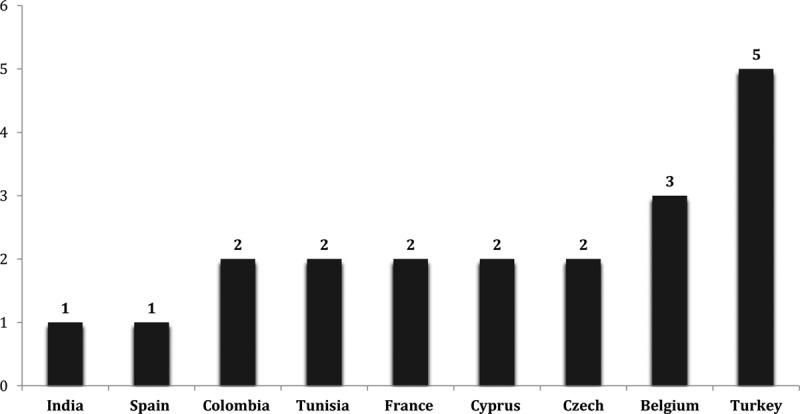
Countries of choice for cosmetic surgery tourism.
Fig. 2.
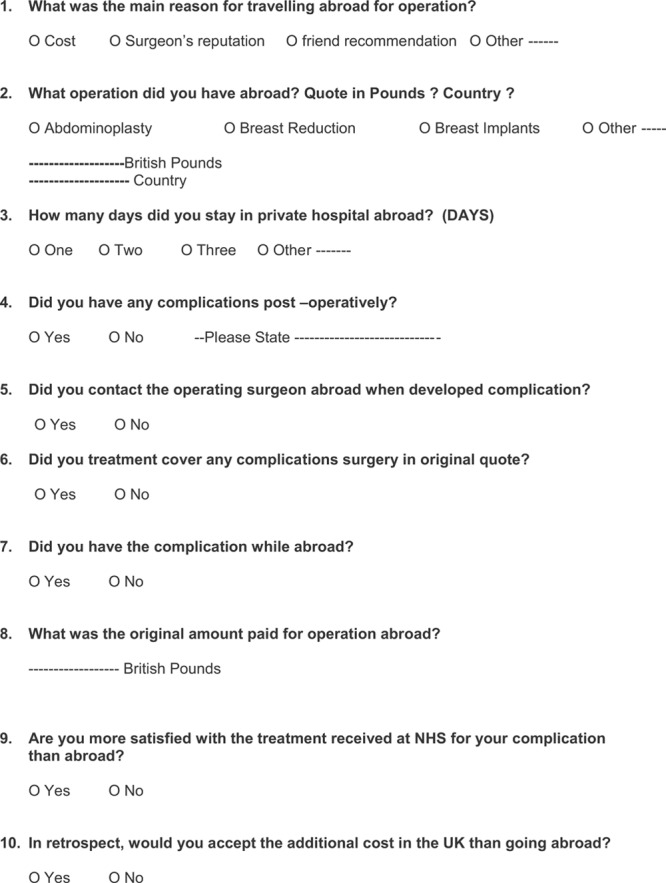
Patient Satisfaction Questionnaire with cosmetic surgery abroad and NHS management.
Minor
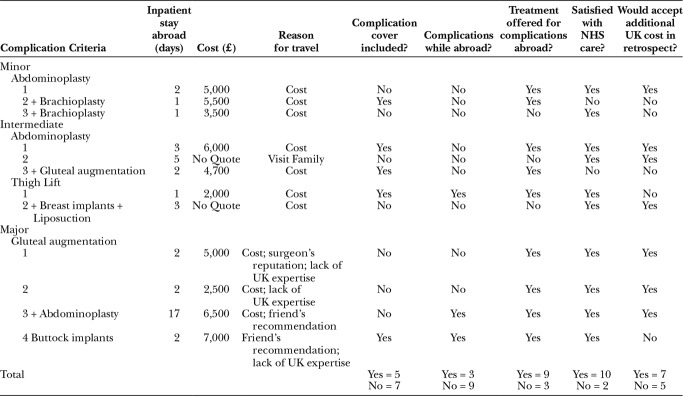
One patient who had a minor complication (seroma and wound dehiscence) following abdominoplasty and brachioplasty was willing to accept this outcome and felt that they still could not justify paying the far higher UK cost for the procedures. Another patient who underwent the same operation and developed minor wound infection shared a similar view. The latter paid less as the operation was in a different country but had no complications cover from the overseas surgeon. This brings to light the ethical issues surrounding whether the operating surgeon offers management of postoperative complications and whether this means anything in practice. Most complications (of all severities) occurred when the patient was back in the United Kingdom and so returning to the operating surgeon became impractical or impossible11 (Table 6).
Table 6.
Patient Survey for Travel Reasons, Complications Management, and Satisfaction
Intermediate
One of the patients who had a thigh lift developed a wound infection while abroad and was offered management of the complication there. However, the patient preferred to have treatment under the NHS and traveled back to the United Kingdom. The same patient also said that they would not accept the higher UK cost despite needing further surgery to manage her complication. In the same category, cellulitis and seroma postabdominoplasty and buttocks fat transfer was viewed to be a minor complication by patient. The operating surgeon abroad asked her to get an ultrasound scan but the eventual management of her infected wounds included hospital admission and intravenous antibiotics. These examples highlight the fact that the NHS often has to cover the complications of poor surgical follow-up abroad. On top of this, some patients express little regret in having their surgery abroad because they know that they are able to receive postoperative care in the United Kingdom if required. A 25-year-old woman presented with bilateral buttocks abscesses following fat transfer required incision and drainage with intravenous antibiotics during hospital admission (Fig. 3).
Fig. 3.
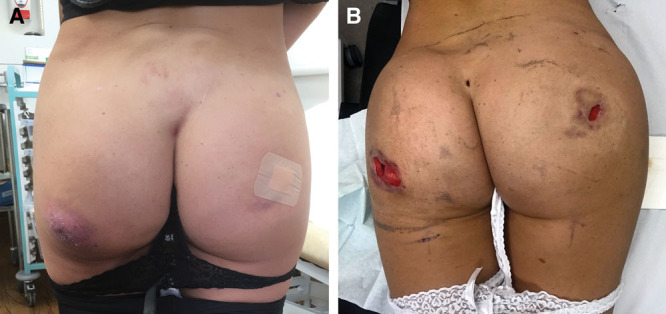
A, Preoperative bilateral buttocks abscesses following gluteal fat augmentation. B, Postoperative bilateral buttocks abscesses incision and drainage.
Major
This group had several very interesting findings. The sole operation was gluteal augmentation (fat transfer = 3, implant = 1). The main reason for travel was lack of UK expertise followed by friend’s recommendation and cost. Half of this group (50%, n = 2) developed complications while abroad. One case had both implants removed and washed out abroad. She continued to have unresolved infection upon her return requiring a further washout in the United Kingdom. The second patient had abdominoplasty and buttock fat transfer, remained in ITU abroad for 12 days, and was admitted to ITU in the United Kingdom when she returned. She suffered pulmonary embolism and her buttock wound required washout due to an abscess. All patients with major complications were satisfied with the care provided by the NHS (Table 6).
One patient was excluded from the results analysis due to case complexity, follow-up in a different country, and significant cost implications: a 26-year-old woman who had abdominoplasty, bilateral thigh liposuction, and fat transfer for gluteal augmentation in Turkey. Day three postoperatively, the patient became septic and was admitted to ITU in Turkey. She returned to the United Kingdom on day 10 postoperatively and her sepsis treatment continued. The patient was diagnosed with necrotizing fasciitis and required multiple debridements of abdominal, buttock and thigh wounds. Intraoperative findings revealed frank pus inside gluteal muscles and fat necrosis. She remained in ITU for 18 days before being stepped down to the ward for a further 31 days in hospital. The patient went on to have abdominal, perineal, buttocks and thigh wound (total body surface area 20%) reconstruction with allograft temporarily then underwent split-thickness skin grafting for soft tissue reconstruction. The total cost for this case was £46,745. The patient was devastated by the final outcome and was physically deformed due to extensive soft tissue involvement.
DISCUSSION
There were a number of motivational factors behind traveling abroad to seek cosmetic surgery. Our results concurred with previous studies that cost is the main reason. Other factors included visiting a family member, a surgeon’s reputation, and what patients labeled “lack of UK expertise” for gluteal augmentation. Patients also may not qualify for these operations on the NHS in their countries of origin due to high BMI, smoking, or certain comorbidities. A high BMI (>25 kg/m2) has been deemed an independent risk factor for postoperative infection and thromboembolism in the literature,12–14 which was reflected in our study. It was also discovered that a psychiatric patient was allowed to undergo multiple cosmetic operations abroad simultaneously, which highlighted the potential lack of safe preoperative screening and the overlooking of ethical considerations by overseas surgeons for surgical tourists.11,15
It is difficult to comment on whether surgical technique or expertise played any role in the rate of complications. What is more clear is that the absence of a “cool off” recovery period after surgery led to the majority of postoperative complications occurring when the patient had already returned to the United Kingdom. Unfortunately, this illustrates the trend toward treating healthcare as a commodity to fulfill economic interests, which ultimately leads to poor and unsafe patient outcomes.16
Patients’ tendency to travel to accessible destinations is influenced by personal, economic, and social reasons.8 Most of our patients traveled from the United Kingdom on short flights to Europe (75%), South America (10%), Africa (10%), and Asia (5%).4 The rise of cosmetic surgery globalization has directly influenced the reduction in the number of operations performed in the developed world. One of the concerns is the tendency of patients to underestimate the risks of operations, viewing “major” operations to be “safe elective” ones. The authors of this article suggest 3 ways to help prevent UK residents from traveling abroad for their operation. Firstly, a more internationally competitive price quote; secondly, the UK promotion of a particular subset of operations (eg, gluteal augmentation). Finally, the need for increasing patient awareness regarding the safety, risks, and recovery for cosmetic operations performed overseas.17
CCG funding for cosmetic surgery varies throughout the United Kingdom. Many patients’ postmassive weight loss surgery do not meet the “functional reasons” requirement to qualify for body contouring surgery, causing an increase in the demand for cosmetic surgery abroad. On the other hand, offering such operations under the NHS may reduce the influx of complications from overseas. The cost of complications does not take into account the psychological, physical, and social impact of overall morbidity.18
Overall, in both single (55%) and multiple (45%) operations, the vast majority of complications presented early (<30 days) postoperatively. We suspect that this trend is explained primarily by the nature of postoperative care offered. This includes early discharge, failure of patients to comply with advice, additional cost of care, and no “cool off” period. Complication rates postabdominoplasty are higher (4%–10%) with combined body contouring operations. This is further increased with a high BMI, which fits with our findings. Abdominoplasty complications formed 45% of cases across all subgroups of minor, intermediate, and major.19 We believe that operations should be offered across the UK postmassive weight loss both for functional reasons and for debilitating appearance. Loss of productivity, lack of self-esteem, and social isolation are evident in this group of patients. The economic gain of performing operations labeled as “cosmetic” under the NHS could prove to be far more beneficial than withholding them.
The continued advancement in medical technology and treatment centers in low- and middle-income countries will lead to further growth of the overseas cosmetic surgery market.9 The British Association of Plastic, Reconstructive, and Aesthetic Surgeons (BAPRAS) has raised concerns about the scale of marketing and advertising approaches (eg, Billboards) abroad.20 The success of these marketing strategies is demonstrated in the yearly increase in the number of cosmetic operations performed overseas.
Guidance on cosmetic surgery practice is closely monitored in the United Kingdom. This is demonstrated by the Royal College of Surgeons (RCS) England, The General Medical Council, and BAPRAS guidelines21,22 to standardize practitioners’ qualifications and practice. These guidelines were issued in an attempt to standardize cosmetic surgery practice following the Poly Implant Prostheses breast implant complications and the 2013 Keogh report recommendations.23 The latter report recognized that the growing demand for cosmetic procedures is led by socioeconomic factors and has led to the trivializing of serious complication from such interventions.24 The guidance for cosmetic surgery abroad is comparatively basic and, in essence, often insufficient to make informed choices. Recently, the European Committee for Standardization (CEN) issued standards for cosmetic surgery within the member countries in an effort to improve the quality of services.25 Compliance with the guidance is voluntary. We would recommend a more global unified response.
Our series showed that major complications were predominantly related to gluteal augmentation alone or combined with other operations. This highlighted the concern regarding practicing new techniques with fat transfer and reconstruction. Implants for gluteal augmentation were originally described in 1969 with fat transfer arriving later, in 1989. The latter method has gained popularity in recent years.26 The ideal waist circumference to hip ratio is 0.7 regardless of ethnicity.27 It is unclear whether our cohort aimed for a trend beyond this ratio. The reported incidence in the literature of similar acute complications (implant removal, infection, and septic shock) is 0.4%–1.9%. The overall complication rate with gluteal fat transfer is lower than for implants in the literature (9.9% versus 21.6%).28 However, our series showed that 3 major complications were due to fat transfer compared to 1 implant case. It may suggest a poor technique abroad or a random pattern from a small sample size of patients that presented to our unit. The high infection rate can be explained by different surgical/medical care and bacterial pathogens abroad.29 Gluteal augmentation is a topic of great interest in cosmetic surgery as it is still evolving. Rohrich et al. set the principles of safe practice in terms of patient positioning, proper technique, anatomy, and trained surgeons.30 Complications with a high mortality risk like pulmonary embolism were evident in our series. This stems from either injury to the deep venous system or fat embolism. There remains serious concern surrounding the lack of patient awareness of significant risks and even mortality associated with these operations.
The success in negligence claims for cosmetic surgery (45%) compared to general operations (30%) in the United Kingdom has been reported by The Medical Defence Union.31
We suspect that the decline in offering particular cosmetic operations in the United Kingdom has contributed to this and to the resulting increase in insurance premiums. The reasons for such a trend were the ease of proving harm from “nonessential” cosmetic surgery, inadequate consent, and the inexperience of surgeons.31 None of the patients claimed for clinical negligence abroad regardless of the complication severity. Hence, the management of complications inevitably occurred at home and patients lost their rights to claim for negligence.32 This is one of the key factors behind the drive toward international consensus for cosmetic surgery practice. Patients are usually not aware of the rules and regulations for medical practice in the country where they choose to have their cosmetic surgery. Our results showed that 58% of patients surveyed were not covered for the cost of complications. Further surgical management was required for 25% of patients who had complications even after initial management abroad. This suggests that patients often assume that the surgery is “low risk” that is unlikely to require complication cover. There is an additional risk of traveling back so quickly after surgery, increasing the burden of complication management in the United Kingdom.33,34 We cannot begin to estimate the total number of complications following an unknown number of operations abroad in a rapidly growing worldwide industry. On a global scale, ISAPS and American Society for Aesthetic Plastic Surgery have issued guidance about the risks for patients seeking operations abroad. This entails operation details, quality of healthcare setting, qualifications tracking of surgeons, and patient suitability for procedures.1 Turkey is the commonest destination for our patients’ cohort. According to ISAPS, it ranked eighth country for top country performing cosmetic procedures worldwide (3.3%).1
It is clear that complication rates will rise with more patients traveling abroad. There is no clear national policy on how to deal with these cases other than offering emergency management for the complications. A striking finding was that 7 out of 12 patients surveyed would still travel abroad to have the same operation despite the complications. This is driven by the knowledge that any issues would be managed at home free of charge. The need for educating patients about the complications and recovery is critical to avert their intention to travel abroad for cosmetic surgery. BAPRAS states that the NHS is not there to underwrite cut-price surgery abroad.35,36 To reduce the risk of deep vein thrombosis (DVT), it advocates that patients must wait at least 5–7 days after breast augmentation or liposuction and 7–10 days after abdominoplasty before traveling home.37 This could lead to the alignment of operation quotes abroad with those in the United Kingdom. The risks of these operations being performed abroad can have grave consequences. In 2015, American Society for Aesthetic Plastic Surgery reported 4 deaths. A financial, legal, and ethical challenge remains in providing and sustaining follow-up care for complications.25,38 There are no accurate figures on a national or international level for the scale of cosmetic surgery complications. There is increasing concern whether the centers or even surgeons are certified to perform cosmetic plastic surgery operations. Hence, patients are strongly advised to check on this fact before committing to travel or intend to have cosmetic operations.
On a different note, there is already a nationally growing concern regarding increased antibiotic resistance and spread of hospital infections. This is not helped by the ferrying back of resistant forms of bacteria from overseas, which increases the financial burden in terms of delayed discharge and potential spread to other patients.
CONCLUSIONS
Cosmetic surgery abroad is rapidly expanding and under-regulated worldwide. There is a need for international regulations to monitor cosmetic surgery and a register for all accredited surgeons to improve patient care. Further patient education about the expected treatment journey and ensuring informed choices is vital to reduce complication rates. When making the decision to have these operations abroad, patients should understand that there is so much more to take into account than just differences in cost. The active involvement of national plastic surgery organizations (eg British Association of Aesthetic Surgery in the United Kingdom) is crucial to minimize the negative impact of this trend. We would recommend further research into the patient perception that UK surgeons lack expertise in certain aesthetic operations (eg, gluteal augmentation) and into ways of creating affordable and safe cosmetic surgery on an international level. We propose a national and an international audit to collect data on cosmetic surgery complications performed locally or abroad.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Emer Kilbride, Specialist Registrar in Infectious Disease and Microbiology (The Royal London Hospital), for her assistance with microbiology data for this article.
Supplementary Material
Footnotes
Published online 12 June 2019.
Presented at the British Association of Aesthetic Surgery (BAAPS) International Conference 2018. Winner of Best Abstract Poster Prize.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.International Society of Aesthetic Plastic Surgeons (ISAPS) 2017 Global Statistics Survey. https://www.isaps.org/wp-content/uploads/2017/10/GlobalStatistics.PressRelease2016-1.pdf. Accessed July 28, 2018.
- 2.Lunt N, Hardey M, Mannion R. Nip, tuck and click: medical tourism and the emergence of web-based health information. Open Med Inform J. 2010;4:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vick L. The perils of cosmetic surgery/medical tourism. Clinical Risk 2012;18:106–109. [Google Scholar]
- 4.Fetscherin M, Stephano R-M. The medical tourism index: scale development and validation. Tour Manag. 2016;52:539556. [Google Scholar]
- 5.Reissis D, Shiatis A, Nikkhah D. Advertising on social media: the plastic surgeon’s prerogative. Aesthet Surg J. 2017;37:NP1NP2. [DOI] [PubMed] [Google Scholar]
- 6.National Health Service. Information for Commissioner of Plastic Surgery Services. http://www.bapras.org.uk/docs/default-source/commissioning-and-policy/information-for-commissioners-of-plastic-surgery-services.pdf?sfvrsn=2. Accessed July 28, 2018.
- 7.Miyagi K, Auberson D, Patel AJ, et al. The unwritten price of cosmetic tourism: an observational study and cost analysis. J Plast Reconstr Aesthet Surg. 2012;65:22–28. [DOI] [PubMed] [Google Scholar]
- 8.Franzblau LE, Chung KC. Impact of medical tourism on cosmetic surgery in the United States. Plast Reconstr Surg Glob Open. 2013;1:e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pashley HS. Medical tourism presents opportunities and risks for patients. AORN J. 2012;96:C6–C7. [DOI] [PubMed] [Google Scholar]
- 10.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crooks V, Turner L, Cohen I, Bristeir J, Snyder J, Casey V, Whitmore R. Ethical and legal implications of the risks of medical tourism for patients: a qualitative study of Canadian health and safety representatives’ perspectives. BMJ Open 2013; 3:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soldin M, Mughal M, Al-Hadithy N; Department of Health; British association of Plastic, Reconstructive and Aesthetic Surgeons; Royal College of Surgeons England. National commissioning guidelines: body contouring surgery after massive weight loss. J Plast Reconstr Aesthet Surg. 2014;67:1076–1081. [DOI] [PubMed] [Google Scholar]
- 13.BAPRAS and RCS England. UK commissioning guidelines: massive weight loss body contouring surgery. http://www.bapras.org.uk/docs/default-source/commissioning-and-policy/2017--draft-for-consultation--body-contouring-surgery-commissioning.pdf?sfvrsn=0. Accessed July 28, 2018.
- 14.Gupta V, Winocour J, Rodriguez-Feo C, et al. Safety of aesthetic surgery in the overweight patient: analysis of 127,961 patients. Aesthet Surg J. 2016;36:718–729. [DOI] [PubMed] [Google Scholar]
- 15.Badulescu D, Badulescu A. Medical tourism: between entrepreneurship opportunities and bioethics boundaries: narrative review article. Iran J Public Health. 2014;43:406–415. [PMC free article] [PubMed] [Google Scholar]
- 16.Pellegrino ED. The commodification of medical and health care: the moral consequences of a paradigm shift from a professional to a market ethic. J Med Philos. 1999; 24(3):243–266. [DOI] [PubMed] [Google Scholar]
- 17.Hanefeld J, Horsfall D, Lunt N, et al. Medical tourism: a cost or benefit to the NHS? PLoS One. 2013;8:e70406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bookman MZ, Bookman KR. Medical Tourism in Developing Countries. 2007New York and Hampshire: Palgrave Macmillan. [Google Scholar]
- 19.Winocour J, Gupta V, Ramirez JR, et al. Abdominoplasty: risk factors, complication rates, and safety of combined procedures. Plast Reconstr Surg. 2015;136:597e–606e. [DOI] [PubMed] [Google Scholar]
- 20.Livingston R, Berlund P, Eccles-Smith J, et al. The real cost of “cosmetic tourism” cost analysis study of “cosmetic tourism” complications presenting to a public hospital. Eplasty. 2015;15:e34. [PMC free article] [PubMed] [Google Scholar]
- 21.The General Medical Council (United Kingdom) guidance for doctors offering cosmetic interventions (2016). https://www.gmc-uk.org/-/media/documents/Guidance_for_doctors_who_offer_cosmetic_interventions_210316.pdf_65254111.pdf. Accessed July 28, 2018.
- 22.The Royal College of Surgeons (England) professional standards for cosmetic surgery (2016). https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/service-standards/cosmetic-surgery/professional-standards-for-cosmetic-surgery/. Accessed July 28, 2018.
- 23.Poly Implant Prostheses (PIP) Breast Implants. Interim Report of the Expert Group (Sir Bruce Keogh, NHS Medical Director). Available at https://www.nhs.uk/news/2012/01January/Documents/pip-report.pdf. Accessed July 28, 2018.
- 24.Nassab R, Hamnett N, Nelson K, et al. Cosmetic tourism: public opinion and analysis of information and content available on the Internet. Aesthet Surg J. 2010;30:465–469. [DOI] [PubMed] [Google Scholar]
- 25.Ross KM, Moscoso AV, Bayer LR, et al. Plastic surgery complications from medical tourism treated in a U.S. Academic Medical Center. Plast Reconstr Surg. 2018;141:517e–523e. [DOI] [PubMed] [Google Scholar]
- 26.Oranges CM, Tremp M, di Summa PG, et al. Gluteal augmentation techniques: a comprehensive literature review. Aesthet Surg J. 2017;c37:560–569. [DOI] [PubMed] [Google Scholar]
- 27.Oranges CM, Gohritz A, Kalbermatten DF, et al. Ethnic gluteoplasty. Plast Reconstr Surg. 2016;138:783e–784e. [DOI] [PubMed] [Google Scholar]
- 28.Sinno S, Chang JB, Brownstone ND, et al. Determining the safety and efficacy of gluteal augmentation: a systematic review of outcomes and complications. Plast Reconstr Surg. 2016;137:1151–1156. [DOI] [PubMed] [Google Scholar]
- 29.Adabi K, Stern CS, Weichman KE, et al. Population health implications of medical tourism. Plast Reconstr Surg. 2017;140:66–74. [DOI] [PubMed] [Google Scholar]
- 30.Villanueva NL, Del Vecchio DA, Afrooz PN, et al. Staying safe during gluteal fat transplantation. Plast Reconstr Surg. 2018;141:79–86. [DOI] [PubMed] [Google Scholar]
- 31.Griffiths D, Mullock A. Cosmetic surgery: regulatory challenges in a global beauty market. Health Care Anal. 2017;26:220–234. 10.1007/s10728-017-0339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burkett L. Medical tourism. Concerns, benefits, and the American legal perspective. J Leg Med. 2007;28:223–245. [DOI] [PubMed] [Google Scholar]
- 33.Schweikart S. Plastic surgery overseas: how much should a physician risk in the pursuit of higher-quality continuity of care? AMA J Ethics. 2018;20:357–365. [DOI] [PubMed] [Google Scholar]
- 34.Bhatt N. Medical Tourism and Plastic Surgery. 2014Bronx, NY: Montefiore Health System. [Google Scholar]
- 35.Iorio ML, Verma K, Ashktorab S, et al. Medical tourism in plastic surgery: ethical guidelines and practice standards for perioperative care. Aesthetic Plast Surg. 2014;38:602–607. [DOI] [PubMed] [Google Scholar]
- 36.Zavlin D, Chegireddy V, Echo A, et al. Population health implications of medical tourism. Plast Reconstr Surg. 2018;141:464e–465e. [DOI] [PubMed] [Google Scholar]
- 37.Gimlin D. National healthcare rhetoric beyond the nation: the materiality of narrative in cosmetic surgery tourism. 2014;14:302–318. [Google Scholar]
- 38.Kassim PN. Medicine beyond borders: the legal and ethical challenges. Med Law. 2009;28:439–450. [PubMed] [Google Scholar]