Abstract
Rationale:
Propylthiouracil (PTU) is a common antithyroid drug which can treat hyperthyroidism effectively. PTU is, however, associated to multiple adverse effects. In rare case, PTU can cause interstitial pneumonia.
Patient concerns:
A 40-year-old woman presented with dyspnea and was diagnosed with pulmonary infection at the first time. After the treatment with moxifloxacin, her symptoms still got worse.
Diagnosis:
The lung tissues biopsy confirmed the diagnosis of organizing pneumonia (OP) and the administration of PTU suggested the diagnosis of PTU-induced OP.
Intervention:
Withdrawal of PTU and the administration of methylprednisolone.
Outcomes:
The patient's symptoms relieved significantly 1 month later and lung computed tomography (CT) scan also demonstrated significant reduction of lung lesions.
Lessons:
Here we report the first case of histologically confirmed OP induced by PTU and conduct a literature review of the cases of PTU-induced interstitial pneumonia. The awareness of PTU-induced OP can help physicians reduce the possibility of misdiagnosis.
Keywords: organizing pneumonia, propylthiouracil
1. Introduction
Propylthiouracil (PTU) is an antithyroid drug, which can inhibits iodine binding to tyrosine. Currently, it is commonly used in the patients with hyperthyroidism. However, PTU has been reported to cause a variety of adverse effects, such as skin rashes, pancytopenia, hepatic impairment, antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, and interstitial pneumonia.[1,2]
Until now, only 6 reported cases of PTU-induced interstitial pneumonia have been reported.[3–7] Here we report another case of PTU-induced organizing pneumonia (OP) and conduct a literature review of the cases of PTU-induced interstitial pneumonia. To our knowledge, this is the first reported case of histologically confirmed OP induced by PTU.
2. Case report
In April 2017, a 40-year-old woman was admitted to our hospital due to dyspnea for more than 1 month. She complained of dyspnea after exercise, such as a mile walking, and exercise tolerance was gradually reduced since the onset of the disease. She also complained of cough with a small amount of white phlegm. She reported no fever, headache, hemoptysis, night sweats, rashes, oral ulcers, arthralgia, and paroxysmal nocturnal dyspnea. Her medical history only included hyperthyroidism which she was diagnosed with in 1996. She used to take methimazole (20 mg/daily) to treat hyperthyroidism. In February 2016, she started to take PTU (100 mg/daily) and vitamin B4 (20 mg/daily) after the recurrence of hyperthyroidism. She was a nonsmoker and did not drink alcohol. She did not have any other medical conditions and take any other drugs. Meanwhile, she did not have access to toxic substances.
On physical examination, her heart rate was 84 beats/ min, blood pressure 110/80 mm Hg, respiratory rate 20 breaths/min, temperature 36.2°C, and oxygen saturation 96% while she was breathing ambient air. She was a little anxious and not in acute distress. There were no lesions in the oropharynx, and her thyroid was enlarged in second-degree bilaterally. The lungs were clear without any wheezes, rales, or rhonchi, and her heart rate was regular without murmurs. Her abdomen was soft and there was no organomegaly. The neurologic examination was negative.
Laboratory tests showed the white-cell count was 6300 per cubic millimeter, with 75.6% neutrophils, 16.7% lymphocytes, and 6.6% monocytes, and the platelet count was 246,000 mm3. The erythrocyte sedimentation was 48 mm/h, procalcitonin was under 0.05 ng/mL and C-reactive protein was 3.13 mg/L. The cytokeratin 19 fragment was 8.35 ng/mL. The T-SPOT.TB was positive (A spot was 7, whereas B spot was 0). The thyroid-stimulating hormone concentration was 0.836 mIU/mL, the free T3 concentration was 5.54 pmol/L, and the free T4 concentration was 15.56 pmol/L, which were within normal ranges. Liver function, renal function, and coagulation function were normal. Other serum chemistry was unremarkable, with no detectable antinuclear bodies, ANCA, or antinuclear antibodies. Tests for parasites and viruses were negative.
A chest CT scan in local hospital showed bilateral interstitial enlargement along the bronchovascular bundle (Fig. 1A). The chest CT scan in our hospital revealed the lung lesions were progressing with many new ground-glass lesions (Fig. 1B). Pulmonary function tests revealed a severe restrictive ventilatory pattern and a severe obstructive ventilatory pattern with decreased diffusing capacity: forced vital capacity (FVC) of 3.29 L (37% of predicted value), forced expiratory volume in 1 second (FEV 1) of 2.84 L (40.1% predicted), FEV 1/FVC of 111.2%. Fiberoptic bronchoscopy showed bronchial inflammation and there were no findings in bronchial secretion cultures.
Figure 1.
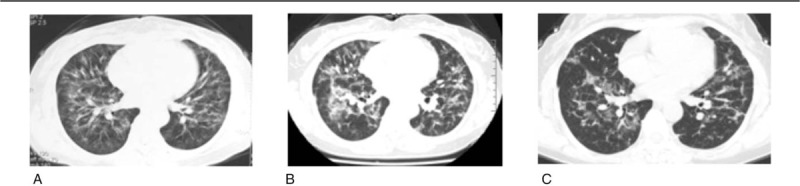
A, A chest computed tomography (CT) scan in local hospital showed bilateral interstitial enlargement along the bronchovascular bundle. B, A chest CT scan in our hospital revealed the lung lesions were progressing with many new ground-glass lesions. C, The CT scan performed 1 month later showed the improvement of the lung lesions (C).
Initially, we diagnosed her illness as pulmonary infection and moxifloxacin (40 mg/daily) was administrated to treat her. However, the symptoms got worse. To elucidate the diagnosis, a CT-guided percutaneous transthoracic biopsy was performed. The pathological results of the lung tissues showed that there was obvious hyperplasia of the fibrous tissues alveolar septum and hemorrhage in the pulmonary alveoli, which suggested the diagnosis of OP (Fig. 2A, B). Based on this results and exclusion of other lung diseases, a diagnosis of PTU-induced CIP was considered. PTU was stopped and replaced by methimazole (5 mg/daily). We also gave her methylprednisolone (32 mg/daily) to reduce the inflammatory reactions. Her respiratory symptoms began to resolve 1 month after the PTU was stopped. The CT scan performed 1 month later also showed the improvement of the lung lesions (Fig. 1C).
Figure 2.
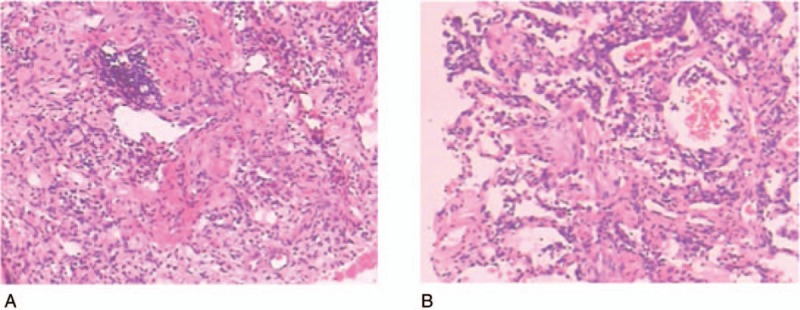
The pathological findings of lung tissues showed that there was obvious hyperplasia of the fibrous tissues alveolar septum (A) and hemorrhage in the pulmonary alveoli (B).
3. Discussion
Currently, it is estimated that >450 drugs can induce interstitial lung disease, including chemotherapeutic agents, antibiotics, antiarrhythmic drugs, and immunosuppressive agents, etc. Globally, approximately 2.5% to 3% interstitial lung disease is induced by drugs.[8] PTU had been reported to cause multiple pulmonary diseases, such as PTU-induced vasculitis and PTU-induced interstitial pneumonia.
To our knowledge, this is the first reported case of histologically confirmed OP induced by PTU. The diagnosis of PTU-induced OP was supported by following findings: the respiratory symptoms occurred after the administration of PTU for more than 1 year; other possible lung diseases were excluded; the pathological results suggested the diagnosis of OP; the respiratory symptoms improved significantly 1 month after the cessation of PTU; and the chest CT scan showed a remarkable improvement of the lung lesions.
To date, only 6 cases of PTU-induced interstitial pneumonia have been reported.[3–7] Time to onset is from 3 to 120 months. Two of them were interstitial pneumonitis,[3] 1 had no histological findings,[4] another one was nonspecific interstitial pneumonia[5] and other 2 were bronchiolitis obliterans OP.[6,7] Consequently, the patient we presented is the first reported case of histologically confirmed OP induced by PTU.
Among the above reported patients, 4 patients firstly took the methimazole and then gave it up due to its adverse effects including liver dysfunction, leukopenia, drug eruption, and itching.[3,4,6] Other 2 patients only took PTU.[5,7] By contrast, in our presented patient, methimazole was changed to PTU due to the recurrence of hyperthyroidism. Based on these findings, the development of interstitial pneumonia may be not related to the administration of methimazole. In some cases, the autoantibodies were positive, which indicate that the autoimmune disease might lead to interstitial pneumonia.[3,4,6] However, our patients and 2 patients previously reported showed that autoantibodies were negative.[5,7] Consequently, these cases cannot explain the role of autoimmune disease in the PTU-induced interstitial pneumonia. The previous patients were all older than 50 years,[3–7] whereas our patient is 40 years old, which indicate the PTU-induced interstitial pneumonia might likely to occur in relatively low-aged individuals.
From 6 patients previously described and our patient, we found an interesting phenomenon that most patients are East Asians with 3 Japanese, 2 south Koreans, and 1 Chinese.[3–5,7] We speculate that the racial differences between East Asians and other races may contribute to such a result. The mechanisms for such differences may involve multiple factors, such as the genetics or dietary.[9–11] Further investigations are warranted to fully define these mechanisms.
The primary treatment of PTU-induced interstitial pneumonia is withdrawal of PTU. Glucocorticoids can be administrated based on the disease's severity. Six patients including our patient stopped take PTU and took glucocorticoids, whereas 1 patient only quitted PTU. Their symptoms and chest imaging all improved markedly in the follow-up visits.[3–7]
In summary, to our knowledge, this is the first reported case of histologically confirmed OP induced by PTU. Until now, the mechanisms underlying the PTU-induced interstitial pneumonia remain unclear. Since most PTU-induced interstitial pneumonia patients are East Asians, we speculate that the racial difference may involve in the mechanisms. Further investigations are warranted to figure out the underlying mechanisms. The current treatments involve withdrawal of PTU and/or the administration of glucocorticoids. The follow-up visits are of high significance to evaluate efficacy after these treatments.
Acknowledgments
The authors are grateful to the patient for participation in our study. The authors declare that there is no conflict of interests regarding the publication of this article.
Author contributions
Conceptualization: Jian An.
Investigation: Xue-Wen Xiao, Jian An, Cheng-Ping Hu, Bai-Ling Luo.
Project administration: Jian An.
Supervision: Cheng-Ping Hu, Bai-Ling Luo.
Validation: Jian An.
Writing – original draft: Xue-Wen Xiao
Writing – review and editing: Jian An
Footnotes
Abbreviations: ANCA = antineutrophil cytoplasmic antibody, CT = computed tomography, FEV 1 = forced expiratory volume in 1 second, FVC = forced vital capacity, OP = organizing pneumonia, PTU = propylthiouracil.
Informed consent statement: Informed written consent was obtained from the patient for publication of this report.
The authors report no conflicts of interest.
References
- [1].Heidari R, Niknahad H, Jamshidzadeh A, et al. An overview on the proposed mechanisms of antithyroid drugs-induced liver injury. Adv Pharm Bull 2015;5:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Nebesio TD, Eugster EA. Antithyroid drugs. N Engl J Med 2005;352:2246–7. [PubMed] [Google Scholar]
- [3].Miyazono K, Okazaki T, Uchida S, et al. Propylthiouracil-induced diffuse interstitial pneumonitis. Arch Intern Med 1984;144:1764–5. [PubMed] [Google Scholar]
- [4].Ohwada R, Kato K, Ohmori K, et al. A man with interstitial pneumonia due to propylthiouracil. Intern Med 2003;42:1026–30. [DOI] [PubMed] [Google Scholar]
- [5].Ji YL, Chung JH, Lee YJ, et al. Propylthiouracil-induced nonspecific interstitial pneumonia. Chest 2011;139:687–90. [DOI] [PubMed] [Google Scholar]
- [6].Diazzi C, Brigante G, Rossi G, et al. Propylthiouracil-induced interstitial pneumonia in a Caucasian woman with amiodarone-induced thyrotoxicosis. Thyroid 2012;22:325–9. [DOI] [PubMed] [Google Scholar]
- [7].Lee J, Choi SH, Choi KJ, et al. Propylthiouracil-induced bronchiolitis obliterans organizing pneumonia. Intern Med 2013;52:2657–9. [DOI] [PubMed] [Google Scholar]
- [8].Schwaiblmair M, Behr W, Haeckel T, et al. Drug induced interstitial lung disease. Open Respir Med J 2012;6:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Empey P. Genetic predisposition to adverse drug reactions in the intensive care unit. Crit Care Med 2010;38:S106–16. [DOI] [PubMed] [Google Scholar]
- [10].Zhou HH, Koshakji RP, Silberstein DJ, et al. Racial differences in drug response. N Engl J Med 1989;321:257–9. [DOI] [PubMed] [Google Scholar]
- [11].Qiu J, Moore JH, Darabos C. Studying the genetics of complex disease with ancestry-specific human phenotype networks: the case of type 2 diabetes in East Asian populations. Genet Epidemiol 2016;40:293–303. [DOI] [PMC free article] [PubMed] [Google Scholar]


