Abstract
Rationale:
Rigid bronchoscopy under general anesthesia enables performing diagnostic and/or therapeutic procedures in the tracheobronchial tree. As most patients undergoing rigid bronchoscopy have moderate to severe respiratory disease or central airway obstruction, the operators often face the risk of hypoxemia when inserting the rigid bronchoscope into the patients’ airway. Applying high flow nasal cannula (HFNC) oxygen therapy before the insertion of the bronchoscope allows to maintain high fractional inspired oxygen (FiO2) and thus leading to maximizing apnea time before desaturation.
Patient concerns and diagnosis:
Case 1: A 70-year-old female patient was diagnosed with lung cancer in the left lower lobe and a tracheal mass of about 2.6 cm ∗ 0.8 cm in size.
Case 2: A male patient, 77 years old, 55.7 kg and 157.3 cm in height, had been diagnosed with chronic obstructive pulmonary disease, and was scheduled for the bronchoscopic volume reduction surgery upon exacerbation of his symptoms of dyspnea and cough with sputum.
Interventions:
Preoxygenation was performed with HFNC (Fisher&Paykel Optiflow ThriveTM, New Zealand) for 3 minutes before the administration of anesthetic medications. The oxygen flow was set at 50 L/min and the FiO2 at 1.0. SpO2 increased to 100%.
Outcomes:
The HFNC oxygen has shown its effectiveness in safely maintaining the patients’ SpO2 during the prolonged apneic period of inserting bronchoscope.
Lessons:
HFNC oxygen is an effective tool in oxygenating the patients during the induction of rigid bronchoscopy, and that it may be a superior alternative to the conventional method of preoxygenation.
Keywords: high flow nasal cannula oxygen, rigid bronchoscopy
1. Introduction
Induction of general anesthesia for rigid bronchoscopy is associated with various risks including hypoxemia, collapse of upper airways, laryngospasm, leading to difficulties in inserting the rigid bronchoscope.[1] As it is for the procedure of endotracheal intubation in general anesthesia, preoxygenation is important for maintaining proper oxygen saturation during the apneic state in the rigid bronchoscopy. Although the technique may vary among institutions, it is a standard practice to oxygenate the patients with 100% oxygen before induction of anesthesia, whether it is for the endotracheal intubation, or for rigid bronchoscopy. Usually, patients can maintain an adequate level of oxygen saturation for approximately 5 minutes during intubation if preoxygenation is performed using a bag valve mask with 15 L/min and 100% oxygen is maintained with normal tidal volume for 3 minutes.[2] However, hypoxemia is associated in 10% to 30% of patients even if sufficient preoxygenation is performed.[3] This bears even greater significance for the patients going through the rigid bronchoscopy as these patients are likely to have moderate respiratory disease, which makes them more susceptible to hypoxemia even after a brief period of apnea.
High flow nasal cannula (HFNC) oxygen therapy which delivers high flow heated and humidified oxygen and air via nasal prongs at a prescribed fractional inspired oxygen (FiO2) and a maximum flow of 60 L/min, can be continued during the passage of the orotracheal tube through the mouth,[4] and hence enables the patients to maintain blood oxygenation for a significant period of time in breathless conditions. The following are 2 cases that show HFNC is an effective tool in oxygenating the patients during the induction of rigid bronchoscopy, and that it may be a superior alternative to the conventional method of preoxygenation.
2. Case description
2.1. Case 1
A 70-year-old female patient was diagnosed with lung cancer in the left lower lobe and a tracheal mass of about 2.6 cm ∗ 0.8 cm in size (Fig. 1). The patient's initial symptoms were hemoptysis, cough, and dyspnea. Her body weight was 49.7 kg and 155.8 cm in height. The operation was scheduled for the removal of the tracheal mass. Written informed consent was obtained from the patient for the publication of this case report and accompanying images. Preoperative pulmonary function test revealed minimal obstructive lung defect. She arrived at the operating theater with a nasal prong of oxygen flow at 5 L/min. The initial vital signs were blood pressure of 125/84 mm Hg, heart rate 83 bpm, and SpO2 of 93%. The initial arterial blood gas analysis showed pH 7.42, PCO2 41 mm Hg, PaO2 73 mm Hg, HCO3 27.9 mmol/L, BE 1.9 mmol/L, and SaO2 95%. A bag valve mask and alternative airway devices were prepared in case of unexpected failed intubation or unrecovered hypoxemia.
Figure 1.
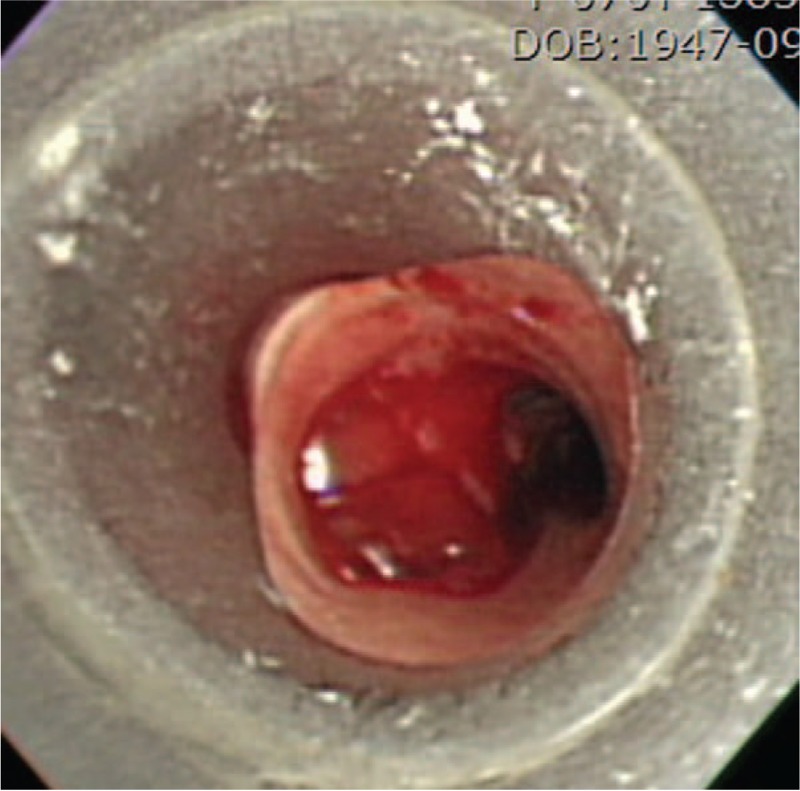
Rigid bronchoscopy shows the tracheal mass.
Preoxygenation was performed with HFNC (Fisher&Paykel Optiflow ThriveTM, New Zealand) for 3 minutes before the administration of anesthetic medications. The oxygen flow was set at 50 L/min and the FiO2 at 1.0. SpO2 increased to 100%. ABGA after 3 minutes of HFNC was pH 7.45, PCO2 38 mm Hg, PaO2 232 mm Hg, HCO3 26.4 mmol/L, BE 2.4 mmol/L, and SaO2 100%. The patient was then inserted with the rigid bronchoscope after propofol 2 to 5 μg/mL and remifentanil 1 to 5 ng/mL followed by rocuronium 50 mg for muscle relaxation. The HFNC device was maintained during the insertion of the rigid bronchoscope and the SpO2 remained at 100% for the entire insertion process. The ABGA performed after the insertion of the bronchoscope showed pH 7.34, PCO2 51 mm Hg, PaO2 294 mm Hg, HCO3 27.5 mmol/L, BE 1.7 mmol/L, and SaO2 100%. The total apneic time was 3 minutes 20 seconds. Mechanical ventilation was maintained after the insertion of the rigid bronchoscope. Pulmonologist successfully removed the tracheal mass and controlled bleeding with an electrocoagulator under the rigid bronchoscopy.
2.2. Case 2
A male patient, 77 years old, 55.7 kg and 157.3 cm in height, had been diagnosed with chronic obstructive pulmonary disease, and was scheduled for the bronchoscopic volume reduction surgery upon exacerbation of his symptoms of dyspnea and cough with sputum. The pulmonary function test showed severe obstructive lung defect (FVC 73, FEV1 38, FEV1/FVC ratio 34). Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
He arrived at the operation room wearing a nasal prong with the oxygen flow at 5 L/min. The vital signs were monitored: blood pressure of 140/80 mm Hg, heart rate of 90 and SpO2 of 92%. The initial ABGA showed pH 7.49, PCO2 38 mm Hg, PaO2 68 mm Hg, HCO3 29 mmol/L, BE 5.4 mmol/L, and SaO2 95%. Preoxygenation was performed with HFNC (Fisher&Paykel Optiflow ThriveTM) for 3 minutes before anesthetic medications; the oxygen flow was set at 50 L/min and the FiO2 at 1.0. After preoxygenation, SpO2 reached 100%, and the ABGA after HFNC showed pH 7.49, PCO2 39 mm Hg, PaO2 343 mm Hg, HCO3 29.7 mmol/L, BE 5.9 mmol/L, and SaO2 100%. While maintaining the HFNC, the rigid bronchoscope was then inserted after the administration of propofol 2 to 5 μg/mL, remifentanil 1 to 5 ng/mL and rocuronium 50 mg.
SpO2 remained at 100% until the rigid bronchoscope was completely inserted and the ABGA performed at the point showed pH 7.36, PCO2 59 mm Hg, PaO2 209 mm Hg, HCO3 33.3 mmol/L, BE 6.2 mmol/L, and SaO2 100%. The total apneic time measured was 3 minutes 10 seconds. Mechanical ventilation combined with assisted ventilation was maintained during the surgery. The rigid bronchoscope was removed after the volume reduction surgery (Fig. 2). The procedural time was 1 hour 20 minutes and the anesthetic time was 1 hour 35 minutes. HFNC was applied in the recovery room with the oxygen flow of 20 L/min. However, the patient complained of dyspnea in the recovery room, with decrease of SpO2 from 90% to 85%. Endotracheal intubation was performed with 8.0 ID and the patient was sent to the intensive care unit with an Ambu- bag streamed with the oxygen flow of 5 L/min.
Figure 2.
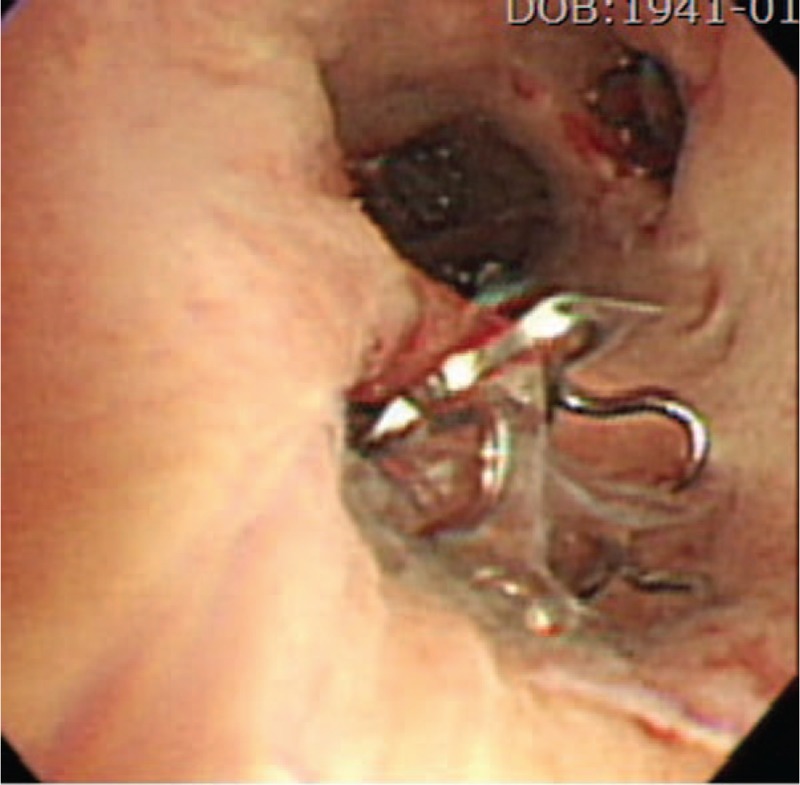
Endobronchial valve is inserted under rigid bronchoscopy for lung volume reduction.
3. Discussion
Rigid bronchoscopy under general anesthesia offers a wide range of diagnostic and therapeutic options for the upper airway diseases. The anesthetic management for the rigid bronchoscopy is challenging in a sense that it integrates various aspects of airway management and ventilation techniques. Patients undergoing the rigid bronchoscopy usually suffer from critical respiratory diseases and present variable degrees of dyspnea or respiratory distress.[1] The patients described in these cases had mild to severe obstructive pulmonary defect due to tracheal mass and COPD, and they needed oxygenation via a nasal prong to maintain SpO2 above 90%. Not only these issues make the insertion of the bronchoscope itself problematic, but it also increases the risk of hypoxemia as well.
Many reports have pointed out the setbacks regarding the use of facial mask for ventilation. The complications associated with active ventilation with a face mask include gastric mucosal laceration, gastric rupture, and aspiration with gastric regurgitation. It is also difficult to fix the face mask in cases of acute respiratory failure or acute mental deterioration, resulting in prolonged elapse time to secure advanced airway management, potentially leading to hypoxemia.[5]
On the other hand, HFNC oxygen can result in increased comfort and satisfaction while maintaining optimal oxygenation. Preoxygenation with high FiO2 is recommended to delay arterial desaturation during intubation.[6] HFNC oxygen can be used to improve preoxygenation before intubation, which in turn maximizes the time a patient can endure in an apneic state before desaturation. The beneficial effects of the HFNC system have been assessed: washout of pharyngeal dead space, reduction of airway resistance, increase in end-expiratory lung volume, generation of positive airway pressure, and positive pressure in the orolaryngeal cavity.[7] On top of these benefits, a major advantage of HFNC oxygen is that it can be continued during airway instrumentation takes place, as opposed to the face mask which must be removed following the induction of general anesthesia.[8] In a study, a median positive airway pressure of 7.4 cm H2O was observed with the month closed, while it was 2.7 cm H2O with the mouth open.[9] Patients with severe acute respiratory distress may have more inconsistent airway pressure due to their breathing through an open mouth. These patients kept closing the mouth during preoxygenation with HFNC. Therefore, HFNC oxygen might be maintained more effective oxygenation with the mouth closed. Ashraf-Kashani et al[10] described that HFNC oxygen is being increasingly used in the realm of airway management. HFNC oxygen is used successfully for awake fiberoptic intubation, acute hypoxic respiratory failure, during bronchoscopy, and for the postextubation period.[10] Its use allows delivery of oxygen at flow rates up to 70 L/min, extending apneic time, facilitating carbon dioxide elimination, reducing the work of breathing, and providing PEEP. Patel and Nouraei[11] reported that transnasal humidified rapid-insufflation increased apnea time (5–20 minutes) in difficult intubation. Apnea time measured in our cases was 3 minutes 20 seconds and 3 minutes 10 seconds, respectively. In both cases, HFNC oxygen could maintain 100% SaO2 after the insertion of rigid bronchoscope. However, PCO2 shown in the ABGA performed after the insertion of bronchoscope were 58 and 59 mm Hg, which brings about a doubt on whether HFNC oxygen could effectively eliminate carbon dioxide.
In conclusion, the anesthesiologists and the bronchoscopists have faced various problems regarding airway management and keeping patients’ oxygenation level was one of the major concerns. The field of interventional pulmonology is rapidly expanding, and it is important for the anesthesiologists to be accordingly updated on the related techniques. HFNC oxygen, to our satisfaction, has shown its effectiveness in maintaining patients’ oxygen saturation during induction of general anesthesia for rigid bronchoscopy, and it may be a superior alternative to the conventional method of preoxygenation. But, it calls for further studies to identify the specifics, such as its optimal flow rates.
Author contributions
Conceptualization: Mee Young Chung.
Data curation: Haedeun Jo, Mee Young Chung.
Investigation: Kyungmoon Roh.
Software: Kyungmoon Roh.
Writing – original draft: Ji Young Min, Mee Young Chung.
Writing – review and editing: Ji Young Min, Haedeun Jo, Kyungmoon Roh.
Mee Young Chung orcid: 0000-0002-1450-8724.
Footnotes
Abbreviations: FiO2 = fractional inspired oxygen, HFNC = high flow nasal cannula.
The authors have no conflicts of interest to disclose.
References
- [1].Dincq AS, Gourdin M, Collard E, et al. Anesthesia for adult rigid bronchoscopy. Acta Anaesth Belg 2014;65:95–103. [PubMed] [Google Scholar]
- [2].Bodily JB, Webb HR, Weiss SJ, et al. Incidence and duration of continuously measured oxygen desaturation during emergency department intubation. Ann Emerg Med 2016;67:389–95. [DOI] [PubMed] [Google Scholar]
- [3].Kang H, Park HJ, Baek SK, et al. Effects of preoxygenation with the three minutes tidal volume breathing technique in the elderly. Korean J Aneathesiol 2010;58:369–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Miguel-Montanes R, Hajage D, Messika J, et al. High flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild to moderate hypoxemia. Crit Care Med 2015;43:574–83. [DOI] [PubMed] [Google Scholar]
- [5].Kim TH, Hwang SO, Cha YS, et al. The utility of noninvasive nasal positive pressure ventilators for optimizing oxygenation during rapid sequence intubation. Am J of Emerg Med 2016;34:1627–30. [DOI] [PubMed] [Google Scholar]
- [6].Voure’h M, Asfar P, Volteau C, et al. High flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med 2015;41:1538–48. [DOI] [PubMed] [Google Scholar]
- [7].Simon M, Braune S, Frings D, et al. High flow nasal cannula oxygen versus non-invasive ventilation in patients with acute hypoxaemic respiratory failure undergoing flexible bronchoscopy-a prospective randomized trial. Crit Care 2014;18:712–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Millette BH, Athanassoglou V, Patel A. High flow nasal oxygen therapy in adult anaesthesia. Trends Anaesth Crit Care 2018;18:29–33. [Google Scholar]
- [9].Groves N, Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care 2007;20:126–31. [DOI] [PubMed] [Google Scholar]
- [10].Ashraf-Kashani N, Kumar R. High flow nasal oxygen therapy. BJA Educ 2017;17:57–62. [Google Scholar]
- [11].Patel A, Nouraei SAR. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in difficult airways. Anaesthesia 2015;70:323–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


