Abstract
Telemedicine is now in vogue, allowing computer and communication tools to be deployed in different fields of health, such as Cardiology, Dermatology, areas in which it has received interest, and in international studies. As the population ages, older people are increasingly concerned about this innovative practice. This is a narrative review of both the literature and Internet pertaining to telemedicine projects within the field of geriatric subjects in France. Since the beginning of the 2000’s, several telemedicine projects and trials focused on chronic heart failure have been developed in the elderly, and also in the field of dermatology. The potential contribution of second-generation telemedicine projects in terms of mortality, morbidity, and the number of hospitalizations avoided is currently under study. Their impact in terms of health economics is likewise being investigated, taking into account that the economic and social benefits brought up by telemedicine solutions were previously validated by the original telemedicine projects. We take a look at telemedicine projects in France concerning the elderly.
Keywords: Telemedicine, elderly, France, cardiology, dermatology, mortality
1. INTRODUCTION
The European Union, and notably France, is experiencing population ageing. This will jeopardize the future balance of public finance, including that of health care. Life expectancy at birth continues to rise worldwide, and in Europe, it is approaching or exceeding 85 years for women and 80 years for men. The quality of life in these extra years, experienced after ages 80 or 85, is of increasing concern to authorities seeking to delay the onset of chronic diseases, senescence, functional decline, frailty and loss of autonomy. The growing number of elderly people in France has caused increased usage of the healthcare system. In 1997, people aged 60 and over, represented nearly one-third of the total medical expenditure and almost half of the drug expenditure, while making up only 20% of the total population. These figures highlight the impact of the increasing number of elderly people in our country.
The development of Information and Communication Technologies (ICTs) for the elderly is a promising venture, which has created new opportunities to assist and care for the elderly people at home or in specialized institutions, including nursing homes and hospitals. Grouped under the term gerontotechnology, the first analyses of their contributions to this field appeared in the mid-1990s. Gerontotechnology studies technology and aging to improve living conditions, working environments, and medical care for dependent seniors.
2. BACKGROUND
Elderly and very elderly people living in nursing homes are frequently being hospitalized, more often than not in emergency situations, and the number is steadily increasing. To combat this problem, the French government has implemented a policy to increase accommodation by constructing new nursing homes across most regions of France. Thus, the number of patients admitted to the hospital emergency departments from nursing homes continues to grow year after year, particularly for people in nursing homes with little medical attention that have no overnight nurses, and often very limited medical time (coordinating doctors). Nursing home healthcare staff must be given tools to limit the flow of these polypathological older patients to Emergency Services - such as assistance in the prevention of decompensation of some geriatric syndromes, to create a preventive policy and improve the quality of life for residents. Literature data support this: trips to Emergency Units cause increased rates of morbidity and mortality.
2.1. Increasing number of Elderly Subjects, Increasing Occurrence of Comorbidities
Since 2012, Europe's working age population has been shrinking, while the number of people aged 60 and over continues to grow. By 2060, one-third of French people will be over 60 years of age and 5 million will be over 85, compared to 1.4 million today. This will jeopardize the future public financial equilibrium, including that of healthcare. Life expectancy from birth continues to increase around the world, approaching or exceeding 85 years for women and 80 years for men in Europe [1]. Today’s nursing home residents are polypathological (heart failure, diabetes, COPD, renal insufficiency, etc.) and polymedicated. At a medical level, this implies the need for regular monitoring and a high level of medical or multidisciplinary expertise for the healthcare teams.
A person over the age of 75 often has:
A functional reserve of vital organs reduced by advancing age.
Various chronic diseases.
Various drug treatments.
The number of preventable Emergency Unit hospitalizations is increasing every year in France, especially for elderly people residing in nursing homes. They make frequent use of the hospital, and most often in cases of emergency.
According to the EHPA survey conducted by the Directorate for Research in Evaluation and Statistical Studies (DRESS), there were 728,000 people residing in nursing homes in France at the end of 2015 [2]. The elderly are increasingly entering nursing homes and becoming more dependent after entering; as the 2011 Morley study shows, the proportion of residents in the GIR (Iso-resource Group) ranked from 4 to 1 accounted for 91% [3]. According to the results of a 2015 national analysis conducted in nursing homes by ANESM (Agence Nationale de l’Evaluation et de la qualité des établissements et Services sociaux et Médico-sociaux, National Agency for Assessment and Quality of Institutions and Social and Medical-Social Services), more than half of these residents are admitted to hospital each year for an average stay of about three weeks, after being passed through Emergency Services [4].
Visits to Emergency Units are frequent for nursing home residents, with one in four admitted at least once a year and one in ten at least twice a year [5]. According to the HCAAM (Haut Conseil pour l’Avenir de l’Assurance Maladie, High Council for the Future of Health Insurance), hospitalizations for this population cost 1.7 billion euros per year in health insurance [6]. Emergency hospitalizations for nursing home residents are considered preventable, according to the authors, in 7 to 67 percent of cases [7], and their frequency could be reduced by improving decision-making procedures. Causes of preventable hospitalizations include lack of medical availability and lack of communication between paramedics and healthcare physicians [8].
To explain the geriatric phenomena, it is necessary to understand the Bouchon 1-2-3 model [9]:
The effects of aging that gradually reduce functional reserves, without ever leading to decompensation.
The superimposed chronic conditions that alter functions.
Decompensation factors that often co-occur in the same patient: acute medical conditions, iatrogenic pathology and psychological stress.
For example, the effects of aging on the brain promote the confusional state, acute cerebral decompensation. Chronic neuropsychiatric conditions, including dementia, are the main areas. Its triggering factors are many: disorders that are cardiovascular, metabolic or infectious, and iatrogenic and environmental stressors.
Prolonged life expectancy is real and we are witnessing the growing importance of anticipatory medicine, i.e. preventive medicine.
2.2. Telemedicine: Towards a Preventive Medicine
According to the Public Health Code, telemedicine is defined as a form of remote medical practice that uses information and communication technologies. It connects one or more health professionals to themselves or to a patient; this includes a medical professional and, where appropriate, other professionals providing patient care. It allows healthcare professionals, with or without their patient’s presence, to connect with one another, or with other specialists involved in the patient’s care (Table 1).
Telemedicine is a recent development in healthcare, enabled by technological progress and promoted by public authorities due to its possibilities, including improved accessibility to care, optimized use of professionals' time, improved collaboration between professionals, optimized care pathways, and revived innovation in therapeutic treatment plans.
Telemedicine has shown efficacy in the treatment of chronic diseases such as heart failure and high blood pressure. The monitoring of patients with chronic pathologies through telemedicine systems is one way of optimizing their care [10] (Fig. 1). Telemonitoring would significantly reduce the number of re-hospitalizations that directly correlate to social costs, while also promoting a better quality of life in elderly patients. Further, these solutions promote the collection of precise medical data that permits adaptive monitoring of a patient's state of health. The objectives are thus ambitious, ranging from improvements in the morbidity-mortality rate to decreased re-hospitalizations, increased quality of life and reduced medico-economic costs.
Fig. (1).
Telemedicine and chronic illnesses.
Telemonitoring is a branch of telemedicine that aims to give home autonomy to people suffering from various pathologies and disabilities that would normally force them into hospitalization or placement in specialized institutions, such as patients suffering from certain chronic diseases, the disabled, and dependent older persons [11].
Telemonitoring is a medical procedure that involves the transmission and interpretation of a clinical, radiological or biological indicator, collected either by the patient or by a health professional [12]. Interpretation can lead to the decision to treat the patient. Today, this is done by a doctor who may delegate a future course of action to another health professional based on a written protocol for monitoring the said indicator, which has been validated by the attending physician or a called-upon physician. The medical time devoted to monitoring a chronic disease indicator is not the same as that which a doctor must devote to the diagnostic procedure or to therapeutic education. Telemonitoring a patient with a chronic disease is based on the regular monitoring of one or more indicators that lets the attending physician know whether or not the patient's disease is stabilized. Any possible destabilization of the indicator is immediately corrected to prevent complications that would justify hospitalization. Telemonitoring provides appropriate responses to the monitoring of most chronic diseases by avoiding the multiplication of traditional consultation procedures and by shortening the length and repetition of hospital stays. The advantages of medical telemonitoring - minimized risk of acute decompensation of the chronic pathology, decreased re-hospitalizations and their economic costs, more appropriate medical monitoring, and a greater commitment to the patient in the management of their pathology - result in better therapeutic compliance and quality of life [13]. The relevant indicators are digitally transferred (via internet, network) for interpretation by a doctor, who must be the custodian of the professional medical record. Indicator results are recorded therein, along with any possible prescription resulting from them. The transfer of these indicators must be secure. Integrating telemonitoring into the care system of a chronically ill patient can help prevent certain complications and unplanned hospitalizations. For example, the hospitalization rate for patients over the age of 70 with chronic heart failure has increased by 30% over the last ten years [13]. In Quebec, home telemonitoring of heart failure has reduced the rate of hospitalization by more than 60% [13]. Limoges University Hospital participates in the Icare project, a pilot research study that evaluates the effectiveness of home telemonitoring for elderly people with chronic diseases. Unique to Europe, its aim is to prevent the loss of home autonomy for elderly people by showing that remotely monitoring chronic diseases in elderly patients minimizes decompensation (disruption of balance) and unplanned hospitalizations. The study is being conducted over a 12-month period with 500 elderly volunteers, some of whom will receive remote monitoring through biometric sensors installed in their homes. These (non-worn) sensors monitor constants, such as blood pressure, blood glucose, weight, blood oxygenation rate and temperature, and transmit the data securely to the patient’s attending physician and nurse, as well as to the geriatric doctor at the hospital, each day [14]. Further work has focused on medical telemonitoring. Minutolo et al. offer a decision support system for telemonitoring people with heart failure [15]. The system is based on an ontology that aggregates patient-related data, such as posture, heart rate, physical activity, and alerts. Franco et al. worked on a telemonitoring study of elderly people with Alzheimer's disease [16, 17]. Their system detects drifts in nycthemeral rhythms from location data. A study by Edirippulige et al. suggests there is little evidence to support telemedicine, but this only represents one randomized study [18]. In addition, most studies are observational and qualitative, as well as use-oriented. They are mainly based on surveys and interviews of stakeholders (patients and health staff). Some studies have evaluated the costs associated with implementing telemedicine services. The Edirippulige et al. study looks at the feasibility of telemedicine in long-term care facilities in a number of clinical specialties, including geriatrics [18].
With respect to cost, this study makes the following observations:
In medical coordination, the management of telemedicine patients becomes economically affordable when usage exceeds about 850 per year;
In dermatology, tele-expertise proves to be most profitable;
In geriatrics, geriatric assessment and patient education seem to be the most cost-effective.
Telemedicine is likely to help, and even optimize, the care of elderly patients by minimizing certain emergencies and repeat hospitalizations [19].
3. TELEMEDICINE AND CARDIAC DEFICIENCY IN THE ELDERLY
The SEDIC study (Suivi Educatif à Domicile des patients avec Insuffisance Cardiaque, or Educational Home Monitoring of Patients with Heart Failure), from France’s Basse-Normandie region, studied the suitability of a telemedicine program in the context of clinical home monitoring (suivi clinique à domicile, or SCAD) beginning in 2007. Patient care was based on the collection of data entered by the patient and sent to the educational monitoring center. This data corresponded to a randomized, open, multi-center prospective trial evaluating the impact of educational follow-up via telemedicine for a period of three months in patients over age 65 who have been hospitalized for acute heart failure (LVEF<45%). The main evaluation criterion was the number of days of hospitalization for an acute cardiac event at the one-year mark. Preliminary results after three months included data from 73 patients: 35 were randomized into the conventional treatment arm, and 38 in the telemedicine arm. There was no significant difference in the main evaluation criterion. At the conclusion of the study, 1,040 days of hospitalization for acute heart failure were recorded. Educational telemedicine monitoring enabled a reduction in days (control group: 590 days vs. telemedicine group: 450 days). Quality-of-life factors similarly improved within the two groups. A significant decrease in cardiovascular mortality was noted [20].
Several points are worth highlighting and discussing in view of the data from the literature. The SEDIC study’s average patient age was 76.8 years, which was higher than other studies, such as the average age of 61 years in Tele-HF (“Telemonitoring to Improve Heart Failure Outcomes”) [21]. In terms of therapy, patients coming out of the SEDIC study received better treatment than those in Tele-HF. In the SEDIC study, 20% of patients had one or more cardiovascular events within three months (death or rehospitalization) - results similar to those of Rich et al. [22]. The results after the first three months of the SEDIC study, though not statistically significant, reinforce the notion that telemedicine is of practical interest in the follow-up care of elderly patients with heart failure.
Moreover, implementing telemedicine in this population may reduce mortality. In the TEN–HMS study (Trans-European Network-Home-Care Management System) [23], patients monitored via telemedicine lost fewer days of life when compared to patients in the conventional monitoring group. The meta-analyses are positive, with a reduction in morbidity and mortality in the telemonitored groups; these meta-analyses include those conducted by the Cochrane Group and by Inglis et al. [24].
With regard to the SEDIC study, 42 patients sent out 319 alerts over the course of three months of telemonitoring; only four patients sent out no alerts. The primary cause for these alerts was the aggravation of respiratory symptoms, followed by weight gain. Nurses responded to 204 alerts (131 phone calls, 73 messages on tablets). The most common paramedical response was a reinforcement of therapeutic education, along with advice to consult the patient’s doctor in the absence of clinical improvement. It is worth noting that the telemonitoring system did trigger some false alerts, particularly for weight gain [25]. As for the patients who did not respond to educational telemedicine in the SEDIC study, 16 of the 45 patients in the group died or were rehospitalized for acute heart failure within the year (36%). However, none of the strong prognostic markers of heart failure (such as BNP, left bundle branch block, LVEF, six-minute walk test, or hemoglobin levels) stood out in univariate analysis. Thus, patients who were non-responsive to educational telemedicine were often more symptomatic and had a higher geriatric depression score upon enrollment in the study than the responsive patients [26].
A study by Dary P aimed to use at-home telemonitoring to evaluate treatment optimization as a possible alternative to hospitalization [27]. 29 women and 54 men were included, with an average age of 78 years; 41% had preserved ejection fraction and 59% had an altered ejection fraction. To evaluate the benefits of short-term telemonitoring, weight, blood pressure, and electrocardiograms were collected using a take-home telemedicine kit. Telemonitoring occurred directly between the patient and their cardiologist, so treatment could be adapted in real time. The monitoring was not used as an alert system, but rather to continually modify the treatment plan according to measured parameters. The results showed an average weight loss of 2kg (p<0.0001), linked to a 50% increase in the dosage of diuretics.
Weight is an effective warning sign and powerful educational tool: it can foreshadow short-term developments and indicate whether a situation is getting worse. During edema flare-ups, the rate of weight loss is a prognostic tool; if slow, it can predict hospitalization. The decrease in blood pressure is limited to 6 mmHg for systolic pressure (p=0.002) and 7 mmHg for diastolic pressure (p<0.0001), allowing for an increase in enzyme-converting inhibitors and sartans. Heart rate drops from 87 to 73bpm (p<0.0001), which is more important in cases of atrial fibrillation. This is the second important criterion, after weight control, that can be used to predict the risk of hospitalization.
By employing this method, researchers were able to offer an alternative to hospitalization for 31 patients (37%) - specifically, management during edema flare-ups and emergencies to avoid hospitalization. During their first 30 days after leaving the hospital, 4.4% of patients died while 5% were readmitted for recurrence. This figure rose to 20% when all causes were included.
In 2003, Goldberg et al. [28] published the WHARF study, which included the largest randomized multi-center sample and compared the value of telemonitoring aftercare to that of in-person aftercare. After six months, there was no significant difference in the rate or time frame of hospital readmissions (p=0.28), but there was a reduction in mortality rates (p<0.003). The Tele-HF study (Telemonitoring to Improve Heart Failure Outcomes) [21] included patients who had presented with decompensated heart failure in the last 30 days. The average age was 61. There was no notable difference between the two groups based on the criteria of mortality rate and hospitalization for any cause, nor on the secondary criteria of death, hospital readmission and length of hospital stay.
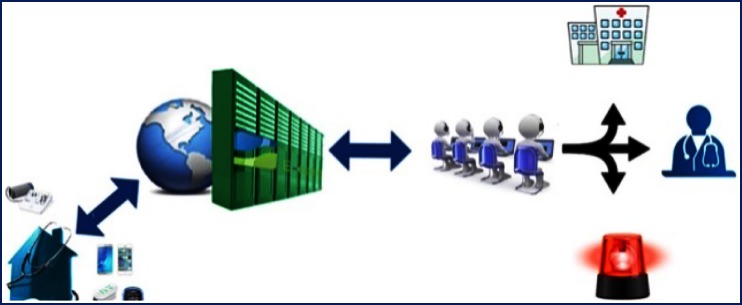
In this context, Andrès et al. developed a telemedicine project called E-Care, which was dedicated to “the early detection of risk situations in heart failure patients” (PIA, 2014) [29]. This detection is based on: an internet-connected touch-screen tablet; non-intrusive sensors (arterial pressure, heart rate, oxygen saturation, weight); questionnaires; and artificial intelligence (Figs. 2 and 3).
Fig. (2).
E-care’s connected non-intrusive medical sensors.
Fig. (3).
E-care platform.
The E-care telemonitoring platform was rolled out with patients in the context of an experiment directed by the University Hospitals of Strasbourg (Hôpitaux Universitaires de Strasbourg, HUS, Strasbourg). It was developed in collaboration with the University of Technology of Belfort-Montbéliard (Université de Technologie de Belfort-Montbéliard, UTBM) and PREDIMED Technology.
The platform consists of connected, non-intrusive medical sensors, a touchscreen tablet connected to Wi–Fi, and a router or 3G/4G, making it possible to interact with the patient and provide education on treatment, diet and lifestyle.
The system involves a server that hosts the patient’s data and a secure internet portal to which the patient and hospital as well as non-hospital based healthcare professionals can connect.
During this experiment, the E-care telemonitoring platform was used daily by patients and healthcare professionals according to a set usage protocol tailored to each patient. The average age of these patients was 72 years, with a male/female ratio of 0.7. These patients presented with multiple conditions, with a Charlson Comorbidity Index of 4.1. Among the most frequent conditions were: heart failure in over 60% of the individuals; anemia in over 40%; atrial fibrillation in 30%; type 2 diabetes in 30%; and Chronic Obstructive Pulmonary Disease (COPD) in 30%.
More than 1,500 measurements were taken from these 175 patients, causing the E-care system to generate 700 alerts regarding 68 patients. During the monitoring period, 107 individuals (61.1%) produced no alerts. The follow-up study on those patients showed that they presented no clinical health events that could result in hospitalization. An analysis of the alerts showed that the E-care platform enables health professionals to automatically and non-intrusively detect declines in health status, particularly for cardiac decompensation. Indeed, it is in this last situation that the system offers the best sensitivity (Se) and specificity (Spe) values, as well as positive and negative predictive values (PPV and NPV): 100%, 72%, 90%, and 100% respectively.
The E-care project is, to our knowledge, the first such program rolled out for heart failure patients who are elderly (average age: 72), have multiple medical conditions, and belong to the geriatric population (Charlson Comorbidity Index: 4.1), using a telemedicine solution for early detection of situations that could lead to acute decompensation. In this sense, we are in the realm of predictive medicine, which, in the context of the E-care platform, aims to offer increasingly personalized care adapted to the phenotype of each patient. For practitioners, the E-care telemonitoring platform allows for the detection of all instances of cardiac decompensations, with three-quarters of alerts referring to such cases. Only 10% of the alerts lacked a direct relationship to heart failure.
To date, this is the first time that such a communicative, “smart” system has been built with new technological tools, anticipating Telemedicine 2.0 solutions. None of the patients or healthcare professionals involved in the experiment reported any difficulties using the E-care system. For the study of non-autonomous patients, the system was used by either a nurse - in addition to his/her other duties (washing, injection of various medications, etc.) - or the patient’s family, friends, or caregivers. It should be noted that the system and its tools were tested and developed in advance by patients and professionals at the National Information Technology Center for Autonomy (Centre d'Expertise National des Technologies de l'Information et de la Communication pour l'autonomie, “Centich,” Angers). As in this experiment, age did not appear to be a limiting factor the acquisition and use of these new technologies.
Other representative telemedicine projects currently in development in France in the area of heart failure include:
PIMPS (Plateforme Interactive Médecins Patients Santé, Doctor/Patient Health Interactive Platform), a platform built for everyone involved with heart failure, from the patient to the healthcare professional. The primary objective of this project, led by Professor Jourdain, is to demonstrate the impact of a telemonitoring program on heart failure patients, including training for professionals, reinforcement of patient education and therapeutic follow-up care. It is based on at-home measurements of a biomarker. The study involves 330 heart failure patients randomized into three groups: arm 1 includes 110 patients who visit a cardiologist every three months; arm 2 includes 110 patients who receive supervised telemonitoring and regularly scheduled care; and arm 3 includes 110 patients who are given interactive follow-ups through supervised telemonitoring, regularly scheduled care, and a BNP monitor [30]. The results of this study are due to be announced shortly.
OSICAT (Optimisation de la Surveillance ambulatoire des insuffisants cardiaques par télécardiologie, Optimization of Ambulatory Monitoring of Heart Failure Patients through Telecardiology), which is employed at 12 local university health centers and coordinated by CHU Toulouse. The OSICAT study is a telemedicine program launched by CHU Toulouse (Professors Pathak and Galinier), with the goal of using telecardiology to optimize the ambulatory monitoring of heart failure patients. It relies on a telemedicine association, therapeutic education, and a phone-based platform staffed with specialized nurses. Its primary objective is to evaluate the impact of a telecardiology program on morbidity and mortality in heart failure patients. The study model involves a randomized, open, controlled clinical trial with two parallel arms of 435 patients. For enrollment, the trial accepted heart failure patients, both men and women over 18 years of age, who had been hospitalized in the previous 12 months for cardiac decompensation. As such, this study is not limited to geriatric patients. The telecardiology program includes daily weight measurements, daily questions about symptoms associated with heart failure, and regular phone calls made by nurses. All-cause mortality and hospitalizations were evaluated after 6, 12, and 18 months in the two groups. The study will produce a medico-economic analysis [31]. Patients in the control group were treated conventionally and released to their homes, with follow-up consultations with their general practitioner or referring cardiologist. For patients in the telemonitoring group, the materials required for their monitoring were delivered to them at home within a week of their baseline visit. This included a connected electronic scale and an electronic unit allowing them to respond to the questionnaire evaluating the course of their symptoms. These patients were also able to speak with nurses over the phone to ensure their full understanding of their disease and treatment, as well as daily management of their symptoms. The results of this study will be made public soon.
MEDICA (Monitorage Electronique à domicile de l’insuffisance cardiaque chronique, Electronic Home Monitoring of Chronic Heart Failure), supported by Reunica Domicile and GMC-Solutions Santé.
Cardiauvergne, which is handling the follow-up and coordinated care of 2,000 heart failure patients over the age of 60 in the Auvergne region, by sharing information via computerized medical records. Each patient is equipped with just one sensor: a scale with a remote transmitter. Nurses are provided with a smartphone to access the patient’s medical records - as laboratories and pharmacists access it – and track their clinical progression (edemas, heart rate, arterial pressure). Biological monitoring is automatically included in the patient record by testing labs, and the dispensing pharmacist records every delivery of prescription medication. An evaluation was made at the end of the program’s first two-year period (with an average 355 days of monitoring) for the first 558 patients enrolled in the study. The death rate was 12% per year, and instances of rehospitalization (for acute heart failure) were reduced to 13.6% per year (compared with 26 to 40% in European data sets). Alarms and alerts were prioritized: a gain or loss of 2 kg set off an alert, while a gain or loss of 5 kg triggered an alarm. If a patient failed to weigh him or herself for three days in a row, this too triggered an alert. In the first two years of the Cardiauvergne program, 558 patients were included: 165 were female, with an average age of 69 years (range: 22-94), and 171 (30.6%) were over the age of 80. Over those two years, 67 patients died, at an average age of 78.6 years (range: 47-94), and 54 patients were rehospitalized one or more times for new cases of heart failure, with an average hospital stay of 9.2 days [32].
4. TELEMEDICINE AND ARRHYTHMIAS IN ELDERLY SUBJECTS
Dary et al. conducted a study on the telemonitoring of atrial fibrillation. The monitoring was ambulatory in nature, and conducted daily from 8 to 12 o’clock, alternating day/night periods. The monitor was used for an average of 11 hours per day for 11 days, for the detection of arrhythmias and automatic ECG transmissions. For better observation, it was programmed to conduct an electrocardiogram every hour. On average, 266 readings were taken per patient for a total of over 51,000 for all patients combined. In total, 200 patients were enrolled at the start of the study: 45% male and 55% female, with an average age of 67 years. 16% of the enrolled patients were over the age of 80; 35% had a history of treated arrhythmias.
One key distinction was made between the two groups. The first group was in sinus rhythm upon enrollment in the study, with the discovery of an atrial fibrillation in 31% of them and regular episodes of tachycardia in 24%. The second group was already in arrhythmia, with a choice between monitoring heart rate (62%) and rhythm (38%). For the 200 patients enrolled in the study, 63 had a known arrhythmia and 137 patients were in sinus rhythm at the outset. Of the latter group of 137 patients, 61 had a normal pattern, 43 (22%) had a detected atrial fibrillation, and 33 (16%) had episodes of tachycardia. For the 63 patients in arrhythmia, 24 had their rhythm monitored and 39 had their heart rate monitored. Thus, for 33% of this study’s patients, telemonitoring improved the diagnosis and treatment of atrial fibrillation, allowing their treatment to be adapted according to rhythm, rate, and conduction time [33].
As for telemedicine in cardiology, the telemonitoring of implanted cardiac rhythm devices (pacemakers and defibrillators) is a developing field in France. Thus, the ECOST study, coordinated by Salem Kacet [34], and Philippe Mabo’s EVATEL study [35] are the first two forays into this area. The EVATEL study has not led to any publications, but its results were disappointing overall. The ECOST study, however, showed that the telemonitoring of implantable defibrillators can have a positive medico-economic impact, with a reduction in inappropriate shocks due to early regulations and a reduction in hospitalizations related to these shocks. By lowering outpatient costs and follow-up costs (baseline consultations and transport), the average savings amount to 315 euros per patient per year - but the program had no effect on hospital costs.
As the TRUST study shows, the telemonitoring of cardiac defibrillators also allows for a reduction in the frequency of face-to-face monitoring, without any impact on major undesirable events such as death or stroke [36].
The ECOST and EVATEL studies, conducted in France on 433 and 1,501 patients respectively, confirmed the safety of telemonitoring defibrillators based on “hard” composite criteria, including mortality, cardiovascular hospitalizations, and system malfunction. In addition, telemonitoring enabled health professionals to reduce the incidence of inappropriate shocks by 52% in ECOST and 37% in EVATEL, with the potential for additional improvement by extending the life of the devices (according to the ECOST study).
We should mention that COMPAS (COMPArative Follow-up Schedule with Home Monitoring), with the Biotronik company, involved the monitoring of pacemakers with 538 patients randomized into two arms (remote transmission vs. traditional monitoring). It demonstrated the safety of monitoring patients via telecardiology over a period of 18 months. This study, conducted in France, reached the same conclusions for the monitoring of pacemakers, with a 56% reduction in follow-up consultations and a reduction in hospitalizations for atrial arrhythmia or stroke [37].
Finally, the SETAM study (Strategy of Early Detection and Active Management of Supraventricular Arrhythmia with Telecardiology) was a randomized study of telemedicine in rhythmology, looking at two groups of patients with pacemakers. It showed that telemedicine promoted the early detection of events, with a 66% reduction in hospitalizations related to atrial arrhythmias, and the prevention of strokes. The study showed that telecardiology allowed for earlier diagnosis and treatment of patients with atrial arrhythmias, and a reduction in the atrial fibrillation burden after nine months of monitoring in patients in sinus rhythm upon enrollment with a score of CHA2DS2-VASc>= 2. In total, 595 patients were enrolled in 57 general hospitals (CHGs) in France, for an average period of 12.8 +/- 3.3 months and an average age of 79 +/- 8 years [38].
5. TELEMEDICINE AND DERMATOLOGY IN THE ELDERLY
In Aquitaine, an experiment on teleconsultation was conducted from September 2012 to September 2013 involving six nursing homes. 19 patients were included, with an average age of 82.4 years. 51 teleconsultations were performed, looking at aftercare for bedsores (57.9%), trophic vascular ulcers (26.3%) and trauma wounds (15.8%). Telemedicine significantly improved the wound healing process and reduced expenditure on bandages by reducing the rate of dressing changes (p <0.005). The stakes of telemedicine are high in geriatrics, especially in regard to aftercare for elderly people with chronic conditions requiring repeated trips and admissions to the hospital. This work showed an excellent level of aftercare, with the rate of recommendations close to 100%. The information and assistance available during teleconsultations provided notable theoretical and practical training to nursing home care staff. On the economic side, this study showed that remote consultations were able to eliminate the need for in-person consultations or hospitalization for 79% of the patients included [39]. Telemedicine could also play an essential part in improving the isolation and education of nursing home care staff.
In 2009, at the CHU Besançon Dermatology Department’s outpatient treatment center for chronic wounds, 240 patients received 820 bandages from outpatient services. Most of these cases involved frail, elderly patients with limited mobility. The Dermatology Department decided to set up a telemedicine service to provide remote follow-up care and diagnostics for the wounds. The objectives were to improve patient aftercare by limiting the number of consultations at CHRU Besançon’s treatment center, reducing the cost of care, and offering local hospitals, private practices, and nursing homes a structured support network [40]. In 2003, a study by the American Telemedicine Association (ATA) had already reported 62 experiments in 37 different U.S. states using telemedicine for dermatology [41]. There are two methods of support defined by the ATA:
store-and-forward teledermatology involves an expert consultant communicating remotely with the patient's dermatologist and using digital images and clinical information to make a diagnosis.
live interactive teledermatology is a teleconsultation between the patient and health professionals using videoconference equipment [40, 41].
This method of care is currently widespread, as shown by the Télégéria network. Télégéria is one of only a few teleconsultation experiments in dermatology, and approximately 100 consultations have been completed since the project’s launch in 2004 [42].
An experiment in treating chronic wounds in elderly subjects residing in nursing home through tele-expertise was conducted in the Haute-Vienne region. The goal was to avoid moving elderly patients (often with reduced mobility) and reduce costs generated by ambulance transportation. Of the 40 nursing homes in Haute-Vienne invited to participate, 22 agreed but only the first 10 were accepted. Between April, 2010 and April, 2012, digital photographs of 34 patients selected by 10 nursing homes were sent to the messaging service set up specifically for Limoges University Hospital. The average number of teletransmissions by these nursing homes was 3.4 in 2 years. These 34 cases accounted for 26 chronic wounds in 24 patients. There were 10 pressure sores, 2 perforating foot ulcers, and 14 leg ulcers. 20 round-trip ambulatory commutes were avoided. Tele-expertise allowed for 20 patients to receive better care for chronic wounds without being moved to a hospital [43]. Further telemedicine experiments in the field of chronic wounds are being explored in France, such as CICAT in Languedoc Rousillon (now Occitanie) and TELAP in Normandy. According to a medico-economic analysis by the CICAT-Occitanie network [44], the Domoplaies telemedicine service has enabled a rate of healing for complex wounds and/or chronic conditions at half the cost of typical treatment.
6. TELEMEDICINE IN GERIATRIC HOME CARE AND NURSING HOMES
Telemedicine projects in geriatric home care are starting to multiply. The ESOPPE project, conducted in Corrèze, France, is unique in Europe. It is an economic, social and environmental assessment of home automation and advanced remote assistance (DTA) among elderly subjects living at home with limited autonomy. The program included 194 adults aged 65 years and over living at home and registered on a list of frail elderly people. Participants were uniformly asked about their history of falls during the year prior to their most recent health examination. The recall period was one year. 77 (40.5%) elderly subjects fell at home, 29 (30.9%) in the exposed group and 48 (50.0%) in the unexposed group. The use of light paths, coupled with tele-assistance, was significantly associated with the reduction in falls at home (p value=0.0012). There was also a greater reduction in post-fall hospitalizations among the exposed group (p value=0.009). In fact, a 30% decrease in falls was noted among people using the home automation and remote assistance package. In terms of falls, DTA considerably improved outcomes, both in number and severity. At the end of the experiment, elderly people with DTA were significantly less depressed than the control subjects. In terms of dependence, the trend seems positive, with a marked improvement according to the French index for measuring independence (GIR), but this has yet to be validated over a longer period. For the duration of the experiment, there were no known cancellations of the DTA package [45].
Since the autumn of 2015, 268 patients over the age of 65 from Limousin and Loir-et-Cher have been receiving aftercare from the Geriatric Department and Chronic Disease Department of the Limoges Hospital without actually going to the hospital. Their care depends on home nurses who examine them using internet-connected devices. Limoges University Hospital is a participant in the Icare project. Its only kind in Europe, this pilot research project evaluates the effectiveness of at-home, medical telemonitoring for elderly people with chronic diseases. Their objective is to demonstrate that telemonitoring chronic diseases in elderly patients prevents decompensation, loss of balance, and unexpected hospitalization.
The study was conducted over a period of 12 months with 500 senior citizen volunteers. Among them, some had the benefit of telemonitoring through biometric sensors installed in their homes. These sensors, which do not need to be worn on the body, monitor constants, such as blood pressure, blood glucose, weight, blood oxygenation level and temperature. Each day, a transmitter securely sent the data to the patient's attending physician, private nurse, and a CHU geriatric specialist [46]. Franco et al. worked on a study of elderly people with Alzheimer's disease who had telemonitoring in their homes [16]. The system allowed them to detect nycthemeral rhythm drifts from location data.
The DETECT study, which looks at telemedicine for the management of psychobehavioral disorders across 20 nursing homes, should also be mentioned. Sponsored by Toulouse University Hospital and coordinated by Professor Soto, it is a randomized, open-label, multi-center intervention study, with a control group receiving usual care and an intervention group receiving remote expert consultations. The main objective is to evaluate the acceptability of expert teleconsultation, with the secondary goal of tracing and comparing specific parameters in the two nursing home groups, such as the rate of hospitalizations and consultations for Behavioural and Psychological Symptoms of Dementia (BPSD), the rate of prescriptions for neuroleptic and psychotropic drugs, patient care costs, and patient quality of life [47].
The GERONTOACCESS study (2015-2017) looked at the use of telemedicine in rural gerontology in the Saint-Laurent-sur-Gorre commune. It included 9 nursing homes and 428 seniors in Limousin, with the main objective of reducing unscheduled hospital admissions. 1,000 incidents per year were counted, including those from DETECT [48]. The results are currently being analyzed.
SALVEO is a smart monitoring and tele-assistance system developed for elderly patients living alone at home. It analyzes collected data from environmental sensors deployed on site and can send alerts to family members or nursing assistants for certain triggers. Events detected by this system include: failures to wake up, falls, absence of movements, abnormal temperatures inside the house, sleep disturbances, time length of kitchen and bathroom use, and the individual's mobility [49].
The OURSES (Supplying Rural Use of Services by Satellite) project is in the competitive Aeronautics, Space and Embedded Systems cluster of the Midi-Pyrénées and Aquitaine regions. This project aims to highlight the benefits of communication technologies by satellite for direct surveillance of isolated individuals in rural areas who do not have the means to access high-speed networks. It is a telemedicine system designed to remotely monitor the electrocardiogram in real time. The system analyzes signals from the ECG sensor the patient wears, and can remotely analyze all stored data. It also seeks to track any behavioral deviations of the subject at night, thanks to motion detectors activated in the room. Alerts are sent to the remote doctor when an unusual situation has been detected. The OURSES system was the subject of a clinical assessment called the “Tibirian-Jaunac” in the middle of a rural region in the Hautes-Pyrenées [50].
The HOMECARE project aims at testing and qualifying, in operational terms, a complete system of telesurveillance for elderly individuals suffering from Alzheimer's disease. A surveillance platform was installed at the local hospital in Caussade. Doctors and nursing staff receive alarm notifications based on location data collected from a network of hybrid sensors. These consultations presuppose remote access and must be conducted via a computer interface [51].
These days, nursing home residents often suffer from a number of medical conditions (including heart failure, diabetes, COPD, and kidney failure) and take multiple medications. From a medical perspective, this implies the need for regular follow-ups and a high level of medical and even multidisciplinary expertise for the team providing care. According to a survey performed by EHPA and DRESS (the Department of Research, Evaluation and Statistical Studies) [52] there were 728,000 individuals living in nursing homes in France at the end of 2015. Elderly people are entering nursing homes at later ages than before, and are increasingly dependent on others when they do. This was shown in the study undertaken by Morley in 2011, where the proportion of residents in Healthcare Resource Groups (HRGs) 1-4 represented 91% of the population [53].
7. TELEGERIA: FRANCE’S MODEL TELEMEDICINE PROJECT
Among the first telemedicine experiments in France involving nursing homes is Télégéria [42]. Télégéria is a system offering teleconsultations and video consultations with experts, as well as teleassistance for elderly patients in geriatric hospitals and nursing homes. A telemedicine network founded in 2004, Télégéria provides patients (who are living in nursing homes or hospitalized at the Vaugirard Gabriel-Pallez geriatric hospital) with expert advice through teleconsultations with the Georges Pompidou European Hospital (HEGP, AP-HP). The network is based on the observation of polypathology among the elderly, which requires input from multidisciplinary specialists. The medical objective is to evaluate the interest and potential of using telemedicine for clinical sessions in more than 20 areas of expertise, including orthopedics, dermatology, care of pressure ulcers, vascular medicine, palliative care, pneumology, neurology, and urology, as well as sessions between hospital geriatricians and coordinating physicians from nursing homes.
Dr. Pierre Espinoza is a coordinator for the remote geriatrics Télégéria project aiming to connect retirement homes with hospital specialists through telemedicine. A 15-month activity report was able to identify 700 telemedicine sessions that involved the following areas in the following distributions: orthopedics (35%), cardiology and cardiac and vascular ultrasounds (32%), dermatology (17%), neurology (4%), and geriatrics (2%). Télégéria's regional deployment in Ile-de-France has plans to expand to 30 nursing homes connected to two major hospitals in the 75th and 95th districts [54].
Further programs have emerged, such as the TELEHPAD program aimed at facilitating access to care in rural areas. Patients, including both nursing home residents and the general local population, can access teleconsultations through rooms set up in the nursing homes that are directly connected to general and psychiatric hospitals. There, they can receive teleconsultations in geriatric medicine, psychiatry, dermatology, cardiology and neurology. Also of note is the TELEFIGAR program, which aims to provide nursing home residents with remote consultation services and telemedicine in the fields of geriatrics, neurology, dermatology and diabetology. This is a combined initiative by the Rennes University Hospital, the Centre Régional de Gériatrie de Chantepie, three nursing homes and the Réseau Diabète 35 Diabetes Network of Ile-et-Vilaine. The TELEHPAD and TELEFIGAR projects were both launched by Sterenn, a platform for telemedical services in Brittany that became operational in March of 2015. The platform enables consultations, expertise and assistance to be delivered remotely. Since March of 2016, Sterenn has progressively expanded to incorporate 10 expert centers, 24 client sites and 12 independent healthcare professionals acting as clients, in a total of six clinical fields. 407 sessions have been delivered since March of 2015, involving psychiatry, geriatrics, and a broad spectrum of medical issues including vascular surgery, diabetic feet, dermatology and wounds and bedsores [55].
Outside the TELEHPAD and TELEFIGAR programs, other projects include:
Agetelepsy: Remote consultation and delivery of expertise in the field of psychiatry, offered by the Guillaume Régnier Hospital in Rennes, to residents at four senior care centers.
TLM Chronic Wounds: Remote consultation and assistance for patients suffering from chronic wounds with a specialist nurse, occupational therapist, or doctor. Led by the Saint-Hélier (Rennes) Hub, this program involves six senior care centers and two organizations providing care to home-based patients.
Télémédecine T6 Saint Malo Cancale: Multi-specialty care for nursing home residents, led by the Communauté Hospitalière de Territoire (CHT) Rance Emeraude Local Hospital Community.
Télémédecine EPSM 56: Remote consultation and remote delivery of expertise and medical assistance in the field of psychiatry, provided by the Etablissement Public de Santé Mentale (EPSM) de Saint-Avé Pubilic Mental Health Institution, to nursing home residents in the No. 4 Healthcare Region, covering Vannes, Ploërmel, and Malestroit.
Téléplaies T7: Remote expertise in chronic wounds and scarring, led by the CHT d’Armor (Centre Hospitalier de Paimpol Hospital) in conjunction with the region’s independent healthcare professionals [55].
Further telemedicine projects include the e-Consult49 project in Anjou Mayenne, which was developed in conjunction with the Angers University Hospital. Looking at remote consultations in accommodation for dependent older people that have been arranged since 2014, this project involves a number of charitable and public nursing homes and represents five medical fields (psychiatry, cardiology, vascular medicine, wounds and internal medicine). There is also the remote healthcare project organized by the Mutualité Retraite Loire Retirement non-profit, which organizes remote consultation, expertise and monitoring in four areas (geriatric, chronic medicine and cardiology as the target) for patients in nursing homes, in conjunction with the Saint-Nazaire Hospital. The Mutualité Française Loire telemedicine project, which has been in nursing homes since 2014, offers remote consultation and delivery of expertise in four fields (psychiatry, pain, geriatrics and ophthalmology) for patients in nursing homes, in conjunction with the Saint-Etienne University Hospital. Finally, the Telem’ehpad project provided by the Mutualité Française Puy-de-Dôme has been in existence since 2013, covering both non-profit and public nursing homes. Remote consultations for patients in nursing homes, covering a single specialty only (namely geriatrics) are also organized in conjunction with the Gérontopole de Clermont-Ferrand Geriatrics Hub [56].
7.1. Telemedicine and Geriatrics
Standardized geriatric assessment can also be performed by telemedicine in nursing homes. This was shown by a retrospective study carried out in Bordeaux, with remote consultations provided to 39 nursing homes in Gironde and Dordogne [57]. 304 residents benefited from telemedicine services, dealing with complex solutions including psychiatric and behavioral issues associated with Alzheimer’s disease and related conditions, chronic wounds, psychiatric illness and palliative situations. Variables that were recorded included the average age of residents, ADL, MMSE, CIRS-G, and the number and types of medications taken per day during scheduled hospitalizations. In this context, 500 remote consultations were performed, primarily for psychiatric and behavioral issues (28.4%) and complex chronic wounds (27.8%) [58].
The remote consultation project for nursing homes in Lorraine was initiated by the ARS Lorraine Regional Health Agency in conjunction with the Nancy University Hospital and Télésanté Lorraine, a telemedicine company. This formed part of the “Elderly People at Risk of Loss of Independence” or PAERPA experiment. The first remote consultations in nursing homes in Lorraine took place on June 24th, 2014. Two nursing homes were included in the experiment (the Residence Le Parc and Residence Saint-Joseph), with three other institutions joining the experiment at a later stage for a total of five. Five categories of medical assistance were targeted, with cardiovascular and pulmonary conditions, geriatric psychiatry, dermatology, iatrogenic conditions and palliative care. A total of sixty remote consultations were performed for 41 residents with an average age of 87.2 years. Limitations encountered were related to time and technology (availability, technical problems due to network issues, poor speed, and lack of Wi-Fi coverage) [59].
Other telemedicine projects in the field of geriatrics are currently in development, such as the e-Vline and TMG 91 projects (for remote geriatric medicine in Essonne). For TMG 91, the Magnolias Private Geriatric Hospital implemented an innovative telemedicine project enabling senior citizens to be supported at home via a medical platform that operated 24 hours per day. The benefit of this platform is that the supervising physician has access to the senior citizen’s electronic medical and social care records remotely. The patient can call using a free, secure card (which is paid for by the hospital for a 45-day period). This enables the physician to take rapid, informed decisions. The tool was extended in 2013 to permanently cover treatments at five nursing homes that benefit from remote consultation sessions and expertise from two hospitals (including the Magnolias Private Geriatric Hospital) [60].
At the Parc de Diane Senior Care Home, which is located in Nantes and accommodates 70 permanent and 13 temporary residents with further space for 15 daytime visitors, a telemedicine project focusing on behavioral issues was implemented. This institution is dedicated to providing full support for patients suffering from neurodegenerative conditions who present with behavioral issues. The first telemedicine session with Nantes University Hospital was delivered in February, 2015. The project was extended to four more nursing homes: La Chézalière in Nantes, Creisker in Pornichet, Ile Verte in Saint Philbert and the Residence Saint Joseph.
Feedback was obtained from 27 treating physicians, who were approached between January 30th, 2017 and March 20th, 2017. 66.7% were satisfied or very satisfied with the remote consultation; 16.6% were somewhat or entirely dissatisfied; 75% were satisfied with the record of the consultation. For 50% of physicians, remote consultations prevented an admission to hospital; for 91.7% of treating clinicians, remote consultation had prevented a consultation at the hospital premises and 83.3% followed the psychotropic suggestions, but only 66.6% followed other suggested measures (without explanation) [61].
Also in 2015, a telemedicine project was implemented in the field of geriatric psychiatry involving an LNA Santé nursing home, Les Jardins d’Olonne and CHS Mazurelle in Olonne. In 2017, this project was extended to four new nursing homes (two belonging to LNA Santé and two to AGAPE). It should be noted that between 2013 and 2017, a total of 22 telemedicine projects were implemented within nursing homes belonging to LNA Santé in France [62]. A telemedicine project at a nursing home in the northwestern region of the Vendée was completed with 174 patients benefiting from remote geriatric consultations between May 1st, 2012 and August 15th, 2017.
Finally, a telemedicine project in the field of palliative care, TELEPAL, covered 51 nursing homes within the territory of GCS Gériatrie (including 11 that are attached to hospital): Valenciennes, St-Amand, Denain, le Quesnoy, and two palliative care centers at Denain and Valenciennes, as well as mobile palliative care teams and the Avesnois and Cambrésis private and regionally-run nursing homes [63].
7.2. Telemedicine and Dermatology
Further experiments in telemedicine in the field of chronic wounds exist within the borders of mainland France, such as CICAT in Occitanie, and TELAP in Normandie. As such, the Domoplaies telemedicine service has resulted in a comparable rate of scar formation in complex and/or chronic wounds at half the cost of traditional treatments, according to a medical economic analysis undertaken by the CICAT-Occitanie Network. Consequently, since October 2013, experts in CICAT-Occitanie have delivered some 14,000 remote sessions for 4,500 patients [44] in the Occitanie region. The cumulative results over a decade show that 75% of wounds were improved or cured, while the number of hospitalizations fell by 72% and ambulance usage to transport patients for admission to a specialist chronic wound center was reduced by 56%. Of the 14,000 remote sessions delivered as part of the Domoplaies Project, most were performed at home (54%) and in a mobile context using secure consultations on tablets or smartphones. Nursing home sessions accounted for 32% of the sessions. These remote delivery sessions related to bedsores, leg ulcers, diabetic wounds of the feet, and cancerous wounds.
Since 2013, the Rouen University Hospital has been developing its telemedicine services through remote consultations and remote delivery of expertise in the field of dermatology for around twenty nursing homes and a number of other healthcare facilities in Seine-Maritime and Eure. The University Hospital’s dermatology department uses telemedicine to consult with patients remotely, view photos of lesions, and support healthcare professionals in the delivery of treatment, such as applying dressing. In 2016, 376 such sessions were completed: 303 remote consultations and 73 sessions involving remote delivery of expertise, with 86% of sessions relating to senior care facilities. Aside from improvements in the standard of treatment provided, particularly by reducing waiting times for consultations, these sessions also enabled cost savings in transportation, as well as reducing the number of visits to Emergency Services by elderly patients. The resulting sessions were eligible for the ETAPES (Experimental Telemedicine And Provision of Enhanced Services) program and its associated billing processes [64].
In 2017, the ARS Normandy Regional Health Agency launched a tender for projects to enhance and further develop its telemedicine services for residents at senior care facilities. In this context, the CHU de Rouen University Hospital and its GHT (regional grouping of hospitals) for the Rouen and Seine Heartland region submitted a proposal to enhance their dermatological activities and expand to cover other specialties, including geriatrics, ENT, anesthetics, and palliative care. The GHT also benefits from the involvement of the CHS Rouvray Specialist Hospital, which has provided around 350 remote psychiatric consultations per year for the last decade or so, once again for patients accommodated in senior care facilities [65].
7.3. Telemedicine and Psychiatry
In France, the team of psychiatrists at the Rouvray Specialist Hospital at Rouen University Hospital benefits from a telemedicine tool that enables psychiatric consultations to be delivered to nursing homes in the Seine-Maritime region. Since the program’s outset, it has grown from around 100 consultations per year to around 100 per month. Data in the literature shows that remote psychiatric medicine is a tool that justifiably has a place in the heart of our healthcare system; however, data in the field of geriatric psychiatry are somewhat sporadic. Remote psychiatric services seem to provide solutions to issues of treatment deserts and regionally aligned medical inequality. The institution has continued to develop its telemedicine tools, particularly by implementing medical and social organizational structures. In this context, a regional telemedicine project was launched by the ARS Haute-Normandie Regional Health Agency (TISSE: the Telemedicine In a Socially Structured Environment) in 2012. As such, 100 remote consultations were delivered in 2012, followed by 300 remote consultations in 2013, then 462 remote consultations in 2014. Over the course of 2014, 71 patients benefited from follow-up care in the form of remote consultations and remote delivery of expertise, with an average age of 78.4 years. The reasons for these remote consultations related to follow-ups for depression and delusions, while the majority of remote expert evaluations were delivered for psychiatric behavioral issues in the context of dementia. The institution has also implemented a new pilot organization, led by the EMPPA mobile geriatric psychiatry team, which has been tested in seven senior care homes covering the Pays de Bray geographic region since 2014 [66, 67].
7.4. Telemedicine and Odontology
Other studies have been conducted concerning telemedicine and oral health among patients in nursing homes. The oral health of residents in communal medical institutions is alarming. The few studies carried out show that nearly half of elderly people living in long-term care facilities had not had consultations with a dentist in over five years [68]. The rate of appointments with dentists among the residents of these facilities is less than 25% of that for senior citizens living at home [69]. The primary objective of the e-DENT project is to validate the use of telemedicine in dentistry, mainly for residents in nursing homes [70]. This is the first experiment of its kind in France. It will include 400 teleconsultations in 8 nursing homes managed by the Alzès Central Hospital, and 200 teleconsultations in 4 nursing homes managed by the Thau Basin Central Hospital. These 600 patients will receive 2 remote consultations each, at 6-month intervals. In nursing homes, remote oral consultations will finally enable general health checkups for each resident. Oral health is often neglected, despite recommendations from the French National Authority for Health (HAS) and health insurers that senior citizens in care have an oral checkup and at least one dentist appointment every year. Dental telemedicine lowers the cost of these checkups. A specially-trained nurse uses a Soprocare camera with fluorescent light to take videos and photos of the inside of the patient's mouth, allowing for easy detection of cavities and gum disease. A study in Limousin called TELEDENT examined the same issue. This study was conducted by the Limoges University Hospital and Guéret Hospital, with the goal of using telemedicine to prevent dental problems in the elderly. In total, 235 patients were examined. The average age was 84.4, ± 8.3 years, and 59.1% of the subjects were women. A total of 128 (55.4%) patients had a dental disease. The sensitivity of the remote sensing was 93.8% for the diagnosis of dental disease (95% confidence interval 90.7-96.9), and the specificity was 94.2% (95% CI 91.2-97.2). Of the 128 cases of dental disease identified by remote sensing, 6 (4.8%) were false positives. Remote sensing assessments were faster than face-to-face exams, taking 12 and 20 minutes, respectively [71].
8. GER-E-TECH: TELEMONITORING PROJECT FOR ELDERLY RESIDENTS IN NURSING HOMES
With this in mind, we set up the Ger-e-Tech project to study the telemonitoring of residents in Rouen University Hospital nursing homes. Through the organization and recording of medical care, we aim to avoid situations of acute decompensation and complications of geriatric risks.
Our objective is to develop a codified, preventive approach for the management of major geriatric risks in nursing homes using a personalized telemonitoring platform dedicated to residents, and developed to avoid the occurrence of an acute decompensation factor in the elderly. The collection of information by the platform will not only allow personalized monitoring, but will also increase patient knowledge and provide a particularly effective tool for transmission between nursing staff (doctors, nurses, etc.) in nursing homes, thus allowing continuity of care. The collected data will also extract markers to improve early detection of any decompensation, thereby improving patient monitoring and reducing hospitalizations. Further, this work will allow for the creation of resident liaison files, providing any paramedical and medical health professional with residents’ up-to-date geriatric data, including anthropometric, nutritional, cognitive and iatrogenic data. Thanks to a simple, streamlined approach, this constitutes a real illustration integrated into the electronic platform of the standardized gerontological evaluation. Geriatric risks will include the risk of falling, constipation, dehydration, confusion, iatrogenicity, undernutrition, heart failure, diabetes, infections and bedsores.
The project’s objective is to experiment with recorded personalized medical monitoring of Rouen University Hospital nursing home residents using the E-care intelligent telemedicine platform, winner of the Investissements d’Avenir (Future Investments) in 2012, and the Fondation d’Avenir (Future Foundation) in 2015 and 2017. The platform assists caregivers by automating the processing of information from sensors and questionnaires to detect anomalies and make early diagnoses of medically risky situations. E-care will provide personalized care for major geriatric risks to avoid the occurrence of an acute decompensation factor in elderly patients. The information collected will be supplemented by codified therapeutic management that follows international recommendations, for direct use in nursing homes. The project will rely on a multidisciplinary team built on the necessary medical, scientific and structural skills. The E-care platform uses an intelligent algorithm to process data and generate alerts based on medical knowledge of the pathologies treated and modeled by ontologies. The general principle adopted by this platform is the anticipation of decompensation through the detection of warning signs that ultimately lead to hospitalization. Tested at the Strasbourg University Hospital from 2013 to 2014 and in homes in 2015, the platform is currently deployed in the PRADO-INCADO project in Strasbourg (a collaborative project between the Strasbourg University Hospital, the Bas-Rhin Medical Insurance and the Grand-Est Regional Health Agency) to monitor heart failure patients where they live. This platform is in the process of being certified as an EU Medical Device and the DIABETe platform has recently been accredited by the Alsace BioValley Competitiveness and Innovation Centre. We will develop a series of measures and questions to be integrated into the E-Care platform for the personalized and adaptive monitoring of patient health in nursing homes. This study, starting in September 2018, is supported by the CENTICH (Centre d'Expertise National des Technologies de l'Information et de la Communication pour l'autonomie, National Expertise Centre for Information Technologies and Communication for Autonomy).
CONCLUSION
As examined above, telemedicine applications are progressively expanding to incorporate geriatrics, and more projects should be delivered in the coming years. The various projects have a variety of different aims, but preserving quality of life for elderly subjects in nursing homes is a particularly widespread priority. Our team is currently striving to develop, via an upgraded version of the E-Care Platform, a remote monitoring system for geriatric risks applied to residents of nursing homes at the Rouen University Hospital, with the aim of reducing preventable hospitalizations through emergency medicine, as well as the occurrence of geriatric risks in advance. Once again, as in the case of cardiac failure, this project will make use of artificial intelligence and alerts that are specific and adapted to each individual nursing home resident.
Table 1. Terms and definitions used in the field of telemedicine.
| Terms | Definitions |
|---|---|
| Telemonitoring | A telemedicine practice allowing a healthcare professional to remotely interpret the data necessary for the patient’s medical follow-up in order to make decisions regarding his or her care remote data collection from a patient via a connected device or questionnaire to monitor his or her vital signs and symptoms at home on a daily basis. |
| Teleexpertise | The practice of telemedicine consisting, for a medical professional, of seeking the opinion of one or more medical professionals regarding elements of the patient’s medical file - the remote seeking, by a health professional, of a second medical opinion via the sending of images (scans, X-rays, eye fundus exams, etc.) and sometimes exchanges via Internet-based videoconferences. |
| Teleconsultation | A telemedicine practice allowing a medical professional to have a remote consultation with a patient in the context of a teleconsultation, a health professional assisting the remote professional, as well as a psychologist at the patient’s side a second opinion consultation by a specialist. |
ACKNOWLEDGEMENTS
Declared none.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.OCDE. Panorama de la santé 2015: les indicateurs de l’OCDE. Paris: Editions OCDE; 2015. [DOI] [Google Scholar]
- 2.DRESS. « 728000 résidents en établissements d’hébergements pour personnes âgées en 2015. Premiers résultats de l’enquête EHPA 2015 »; Etudes et résultats, n° 1015, juillet. 2017. [Google Scholar]
- 3.Morley J.E., Rolland Y., Tolson D., et al. The time has come to enhance nursing home care. Arch. Gerontol. Geriatr. 2011;53(1):1–2. doi: 10.1016/j.archger.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 4.HAS-ANESM. Methodological note and documentary synthesis. Key points course organization; 2015. Jul, How to reduce the unplanned hospitalization of EHPAD residents? p. 97. [Google Scholar]
- 5.Salles N. The keys to launch. Experience sharing; 2017. Oct, Télémédecine en EHPAD. p. 168. [Google Scholar]
- 6.High Committee for the Future of Medicare (HCAAM) Medicare and loss of autonomy. 2011. June>. [Google Scholar]
- 7.Fur-Musquer É., Delamarre-Damier F., Sonnic A., et al. Are there any predictive factors for unphased hospitalization of EHPAD residents? Geriatr Psychol Neuropsy-chiatr Old. 2012;10(2):137–142. doi: 10.1684/pnv.2012.0344. [DOI] [PubMed] [Google Scholar]
- 8.Young Y., Barhydt N.R., Broderick S., et al. Factors associated with potentially preventable hospitalization in nursing home residents in New York state: A survey of directors of nursing. J. Am. Geriatr. Soc. 2010;58:901–907. doi: 10.1111/j.1532-5415.2010.02804.x. [DOI] [PubMed] [Google Scholar]
- 9.Bouchon J.P. 1+2+3 Or how to try to be effective in geriatrics. Rev. Prat. 1984;34:888. [Google Scholar]
- 10.Martínez-González N.A., Berchtold P., Ullman K., et al. Integrated care programmes for adults with chronic conditions: A meta-review. Int. J. Qual. Health Care. 2014;26(5):561–570. doi: 10.1093/intqhc/mzu071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barralon P. Classification and merging of actimetric data for medical telemonitoring. Joseph Fourier University,; Grenoble: 2005. [Google Scholar]
- 12.Telehealth: A new asset at the service of our well-being. A five- year eco-responsible plan for the deployment of telehealth in France. 2009 (Report submitted to Mrs. Rose-lyne Bachelot- Narquin, Minister of Health and Sports by Mr. Pierre Lasbordes, Member of Parliament for Essonne [Google Scholar]
- 13.Ahmed BA, Hajjam A, Talha S, et al. E-care: Ontological evolution and improvement of knowledge for the follow-up of heart failure. MT. 2014;20(2):79–86. [Google Scholar]
- 14. Available at: http://www.revue-hospitaliere.fr/Actualites/Telesur-veillance-a-domicile-des.
- 15.Minutolo A., Sannino G., Esposito M., et al. A rule-based mHealth system for cardiac monitoring.; 2010 IEEE EMBS Conference on Biomedical Engineering; Sciences, Kuala Lumpur. 2010. [Google Scholar]
- 16.Franco C., Demongeot J., Villemazet C., et al. Behavioral telemonitoring of the elderly at home: Detection of nycthemeral rhythms drifts from location data.; 24th International Conference on Advanced Information Networking and Applications Workshops; 2010. pp. 759–766. [Google Scholar]
- 17.Franco C., Demongeot J., Fouquet Y., et al. Perspectives in home TeleHealthCare system: Daily routine nycthemeral rhythm monitoring from location data.; International Conference on Complex, Intelligent and Software Intensive Systems; 2010. pp. 611–7. [Google Scholar]
- 18.Edirippulige S., Martin-Khan M., Beattie E., et al. A systematic review of telemedicine services for residents in long term care facilities. J. Telemed. Telecare. 2013;19(3):127–132. doi: 10.1177/1357633X13483256. [DOI] [PubMed] [Google Scholar]
- 19. Available at: http://www.has-sante.fr/portail/upload/docs/applica-tion/pdf/2012 04/guide_parcours_de_soins_ic_web.pdf 2014.
- 20.Biannic C., Coutance G., Calus J., et al. Educational home follow-up by telemedicine in cases of cardiac insufficiency. Randomised, multicentric study from the Basse-Normandie region. Preliminary results. Eur Telemed Res. 2012;1:40–48. [Google Scholar]
- 21.Chaudhry S.I., Barton B., Mattera J., et al. Randomized trial of telemonitoring to improve heart failure outcomes (Tele-HF): Study design. J. Card. Fail. 2007;13:709–714. doi: 10.1016/j.cardfail.2007.06.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rich M.W., Freedland K.E. Effect of DRGs on three-month readmission rate of geriatric patients with congestive heart failure. Am. J. Public Health. 1988;78:680–682. doi: 10.2105/ajph.78.6.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cleland J.G., Louis A.A., Rigby A.S., et al. Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: The Trans-European Network-Home-Care Management System (TEN-HMS) study. J. Am. Coll. Cardiol. 2005;45:1654–1664. doi: 10.1016/j.jacc.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 24.Inglis S.C., Clark R.A., Dierckx R., et al. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst. Rev. 2015;31:CD007228. doi: 10.1002/14651858.CD007228.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gudanis F., Nogues S., Houguet U., et al. A randomized study of educational telemedicine in the inadequate cardiac elderly patient. 6 th European Congress of ANTEL; Paris: 2013. Nov, Distribution and alert management in the SEDIC study. [Google Scholar]
- 26.Coutance G., Belin A., Targat-Biannic C., et al. a randomized trial of educational telemedicine in elderly heart failure patients. 6 th European Congress of ANTEL; Paris: 2013. Nov, Characteristics of non-responder patients in educational telemedicine in the SEDIC study: [Google Scholar]
- 27.Dary P. Remote monitoring in heart failure: Feasibility and results of a limited 14-day follow-up of 83 patients. Eur Telemed Res. 2014;3:125–132. [Google Scholar]
- 28.Goldberg L.R., Piette J.D., Walsh M.N., et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: The Weight Monitoring in Heart Failure (WHARF) trial. Am. Heart J. 2003;146:705–712. doi: 10.1016/S0002-8703(03)00393-4. [DOI] [PubMed] [Google Scholar]
- 29.Andrès E., Talha S., Benyahia A., et al. Experimentation of an e-platform to detect situations at risk of cardiac impairment (platform E-care) in an internal medicine unit. Rev. Med. Interne. 2016;37:587–593. doi: 10.1016/j.revmed.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Jourdain P., Desnos M., Jullière Y. 6 th European Congress of ANTEL; Paris: 2013. Nov, Establishment of an Interactive Patient Health Platform (PIMPS) based on home-based self- measurement of a bi-omarter in chronic ambulatory heart failure. [Google Scholar]
- 31.Bendelac H., Pathak A., Molinier L., et al. Optimization of ambulatory monitoring of patients with heart failure using telecardiology (OSICAT). Eur Res Telemed. 2014;3:161–167. [Google Scholar]
- 32.Eschalier R., D’Agrosa-Boiteux M.C., Mannenq P.H., et al. Cardiauvergne: Heart failure home management and remote monitoring system. Eur Res Telemed. 2014;3(4):169–176. [Google Scholar]
- 33.Dary P. Telemonitoring of atrial fibrillation: Feasibility study and results on 200 patients. Eur Res Telemed. 2013;2:113–120. [Google Scholar]
- 34.Kacet S. ECOST: Safety of implantable cardioverter defibrillator follow-up using remote monitoring: A randomized controlled trial.; ESC Congress; 2011. [Google Scholar]
- 35.Mabo P. The prospective randomized EVATEL study. ESC Congres; 2011. Remote follow-up of patients implanted with an ICD. Hot Line II. [Google Scholar]
- 36.Varma N., Epstein A.E., Irimpen A., et al. Efficacy and safety of automatic remote monitoring for implantable cardioverter-defibrillator follow-up: The Lumos-T safety reduces routine office device follow-up (TRUST) trial. Circulation. 2010;122:325–332. doi: 10.1161/CIRCULATIONAHA.110.937409. [DOI] [PubMed] [Google Scholar]
- 37.Mabo P., Victor F., Bazin P., et al. A randomized trial of long-term remote monitoring of pacemaker recipients (the COMPAS trial). Eur. Heart J. 2012;33(9):1105–1111. doi: 10.1093/eurheartj/ehr419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amara W., Montagnier C., Cheggour S., et al. Early detection and treatment of atrial arrhythmias alleviates the arrhythmic burden in paced patients: The SETAM study. Pacing Clin. Electrophysiol. 2017;40(5):527–536. doi: 10.1111/pace.13062. [DOI] [PubMed] [Google Scholar]
- 39.Salles N., Baudon M.P., Caubet C., et al. Telemedecine consultations for the elderly with chronic wounds, especially pressure sores. Eur Telemed Res. 2013;2:93–100. [Google Scholar]
- 40.Bonnans V., Droz-Bartholet L., Garcia E., et al. Implementation of a teledermatology department in the Franche-Comté region, France. Eur Telemed Res. 2012;1:96–103. [Google Scholar]
- 41. http://www.atmeda.org [site consulté en novembre 2017].
- 42.Simon P., Acker D. The place of telemedicine in the organization of care. CGES-Report Thematic Mission. 2008;7:1–145. [Google Scholar]
- 43.Sparsa A., Doffoel-Hantz V., Bonnetblanc J.M. Assessment of tele-expertise among elderly subjects in retirement homes. Ann. Dermatol. Venereol. 2013;140:165–169. doi: 10.1016/j.annder.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 44.Sood A., Granick M.S., Trial C., et al. The role of telemedicine in wound care: A review and analysis of a database of 5,795 patients from a mobile wound-healing center in languedoc-roussillon, France. Plast. Reconstr. Surg. 2016;138(3) Suppl.:248S–256S. doi: 10.1097/PRS.0000000000002702. [DOI] [PubMed] [Google Scholar]
- 45.Tchalla A.E., Lachal F., Cardinaud N., et al. Efficacy of simple home-based technologies combined with a monitoring assistive center in decreasing falls in a frail elderly population (results of the Esoppe study). Arch. Gerontol. Geriatr. 2012;55:683–689. doi: 10.1016/j.archger.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 46. http://www.revue-hospitaliere.fr/Actualites/Telesurveillance-a-domicile-despersonnes-agees-Projet-Icare [site consulté en no- vembre 2017].
- 47.Piau A., Nourhashemi F., De Mauléon A., et al. Telemedicine for the management of neuropsychiatric symptoms in long-term care facilities: the DETECT study, methods of a cluster randomised controlled trial to assess feasibility. BMJ Open. 2018;8(6):e020982. doi: 10.1136/bmjopen-2017-020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. https://www.nouvelle-aquitaine.ars.sante.fr/system/files/2018-01/Telemedecine_08_Presentation.pdf [site consulté en novembre 2017].
- 49. Pervaya, « SALVEO: Un systeme intelligent de suivi et de téléas- sistance de personnes agées vivant seules a domicile », SALVEO. [En ligne]. Disponible sur: http://www.pervaya.com/index.html.
- 50.Mailhes C., Comet B., de Bernard H., et al. IWSSC 2008. IEEE International Workshop; 2008. Telemedicine applica- tions in OURSES project, in Satellite and Space Communications, 2008. pp. 124–128. [Google Scholar]
- 51.Bourennane W. University Toulouse 2 Le Mirail; 2013. Sep, Study and design of a remote monitoring and critical situation detection system "by actimetric tracking" of people at risk in indoor and outdoor environments. p. 162. [Google Scholar]
- 52.DRESS. (2017). « 728000 residents in residential facilities for the elderly in 2015. First results of the 2015 EHPA survey "; Studies and results, n ° 1015 [Google Scholar]
- 53.Morley J.E., Rolland Y., Tolson D., et al. The time has come to enhance nursing home care. Arch. Gerontol. Geriatr. 2011;53(1):1–2. doi: 10.1016/j.archger.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 54.Espinoza P., Gouaze A., Bonnet B., et al. Deployment of telemedicine in health territory. Tele-geria, a precursor experimental model. Telemed Health. 2011;725:9–17. [Google Scholar]
- 55. http://esante.gouv.fr/sites/default/files/dp_sterenn_tlm.pdf
- 56. https://www.fondationdelavenir.org/wp-content/uploads/2016/04/T%C3%A9l%C3%A9m%C3%A9decine-en-EHPAD-rapport-complet-29-03-2016.pdf
- 57.Salles N., Lafargue A., Cressot V., et al. Global geriatric evaluation is feasible during interactive telemedecine in nursing homes. Eur Telemed Res. 2017;6:59–65. [Google Scholar]
- 58.Thiébaut S., Lupi-Pégurier L., Paraponaris A., et al. Comparison of the use of a dental surgeon between institutionalized persons and those living at home, France, 2008-2009. BEH. 2013;7:60–64. [Google Scholar]
- 59.Telemedicine and geriatric teleconsultations in EHPAD: state of the art after two years of experimentation in the residence EHPAD Le Parc in Nancy. Dr. Arnaud MORETTINI. 2016. p. 46.
- 60. http://novap.fehap.fr/living-labs/telemedecine-geriatrique-tmg91/
- 61.Georgeton E., Aubert L., Pierrard N., et al. General practitioners adherence to recommendations from geriatric assessments made during teleconsultations for the elderly living in nursing homes. Maturitas. 2015;82(2):184–189. doi: 10.1016/j.maturitas.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 62. Accessed on: https://www.lna-sante.com/actualite/la-telemedecine-une-solution-davenir.
- 63. Accessed on: https://www.hauts-de-france.ars.sante.fr/system/files/ 2017-06/Le%20projet%20TELEPALLIA.pdf.
- 64. Accessed on: http://solidarites-sante.gouv.fr/IMG/pdf/dgos_tele-medecine_etapes_rapport_parlement.pdf.
- 65. Accessed on: http://solidaritessante.gouv.fr/IMG/pdf/dgos_tele-medecine_etapes_rapport_parlement.pdf.
- 66.Desbordes M, Nebout S, Grès H, et al. Telemedicine in psychiatry of the elderly: Issues and perspectives. 2015 Oct;15(N° 89):270–273. [Google Scholar]
- 67.Elie-lefebvre C., Schuster J.P., Limosin F. Telepsychiatry: What role in the care of the elderly? Geriatr. Psychol. Neuropsychiatr. Vieil. 2016;14(3):325–331. doi: 10.1684/pnv.2016.0625. [DOI] [PubMed] [Google Scholar]
- 68. Accessed on: https://www.has-sante.fr/portail/upload/docs/ application/pdf/2010-10/corriges_synthese_carie_dentaire_version_postcollege-10sept2010.pdf.
- 69.Thiébaut S., Lupi-Pégurier L., Paraponaris A., et al. Comparison of the use of a dental surgeon between institutionalized persons and those living at home, France, 2008-2009. BEH. 2013;7:60–64. [Google Scholar]
- 70.Giraudeau N., Valcarcel J., Tassery H., et al. E-DENT Project: Oral teleconsultation in long-term care homes. Eur Telemed Res. 2014;3:51–56. [Google Scholar]
- 71.Queyroux A., Saricassapian B., Herzog D., et al. Accuracy of teledentistry for diagnosing dental pathology using direct examination as a gold standard: Results of the tel-e-dent study of older adults living in nursing homes. J. Am. Med. Dir. Assoc. 2017;18:528–532. doi: 10.1016/j.jamda.2016.12.082. [DOI] [PubMed] [Google Scholar]