Abstract
Background
The Japanese National Clinical Database (NCD) is a large‐scale, nationwide, web‐based data entry system that is linked to the surgical board certification system and covers almost all surgical cases carried out in Japan.
Aim
To evaluate outcomes according to the gastroenterological section of the NCD.
Methods
The 115 surgical procedures stipulated by the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology” were registered from 2011 to 2017. The number of surgeries, preoperative comorbidities, and short‐term outcomes were compared between registration periods.
Results
In total, 3 818 414 cases have been registered. More than 70% of all surgeries were carried out at certified institutions. The annual number of cases has been increasing year after year, and the aged population has also been increasing. Although the rates of preoperative comorbidities and postoperative complications have been increasing, the postoperative mortality rate has remained relatively low; in 2017, the 30‐day mortality rate was 1.0% among those who underwent esophagectomy, 0.7% among those who underwent distal gastrectomy, 1.1% among those who underwent total gastrectomy, 1.3% among those who underwent right hemicolectomy, 0.5% among those who underwent low anterior resection, 1.3% among those who underwent hepatectomy, and 1.3% among those who underwent pancreaticoduodenectomy. The annual rate of endoscopic surgery dramatically increased over 7 years between 2011 and 2017, especially for low anterior resection (29.5%‐62.6%) and esophagectomy (31.0%‐56.1%).
Conclusion
This database is expected to ensure the quality of the board‐certification system and surgical outcomes in gastroenterological surgery.
Keywords: gastroenterological surgery, National Clinical Database, surgical outcome
1. INTRODUCTION
The Japanese National Clinical Database (NCD) is a large‐scale, nationwide, web‐based data entry system linked to the surgical board certification system, and covers almost all surgical cases (90%‐95%) carried out in Japan.1 The NCD was created in April 2010 with major support from the Japan Surgical Society and the Japanese Society of Gastroenterological Surgery (JSGS).2 Fifteen professional societies joined the NCD in 2018. The NCD has collected data on more than 9 690 000 surgical cases from almost 5000 facilities from January 2011 to December 2017.
In the gastroenterological section of the NCD, the JSGS selected 115 gastrointestinal operative procedures as important for the board certification system and eight main procedures (ie, esophagectomy, distal gastrectomy, total gastrectomy, right hemicolectomy, low anterior resection, hepatectomy, pancreaticoduodenectomy, and surgery for acute diffuse peritonitis) as especially important in terms of medical standards for improvement of surgical quality. All surgical cases are registered in the NCD with input of postoperative complications for the 115 procedures, and with detailed input such as comorbidities and morbidities for the eight main procedures.3 Risk models of mortality for the eight main procedures were established using approximately 120 000 surgical cases registered in 2011.4, 5, 6, 7, 8, 9, 10, 11 Risk models of morbidity for the eight main procedures were also established using approximately 250 000 surgical cases registered in 2011 and 2012.12, 13, 14, 15, 16, 17 Using the risk models of morbidity and mortality, the risk calculator was created. The risk calculator adjusts the risks of patients, provides the predicted morbidity and mortality of patients after inputting the preoperative data, and has been available on the websites of the participating hospitals since 2015.2 To evaluate the reliability of data collection, the JSGS started data verification activity in 2016 and found high accuracy of data entry.18
Following up on the 2011‐2016 Report,3 we herein summarize the 2011‐2017 data in the NCD based on gastroenterological surgery information on 3 818 414 cases of surgeries carried out and recorded from 2011 to 2017 along with the data on perioperative complications.
2. SUBJECTS AND METHODS
Methods were the same as previously reported.3 Subjects were patients whose surgical data were recorded in the NCD, and who underwent one or more of the 115 surgical procedures stipulated by the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology,” using the “New classification of surgical difficulty.” The board certification system of the JSGS consists of board‐certified training institutions and board‐certified surgeons in gastroenterological surgery.19 One requirement for board‐certified training institutions is having carried out 600 or more gastroenterological operations as determined by the certifying committee (of which more than 120 gastroenterological operations were essential major surgery) in the last 3 years. Board‐certified surgeons are required to have received gastroenterological surgical training for more than 5 years according to the training curriculum in a board‐certified training institution authorized by the JSGS and to have carried out 450 or more gastroenterological operations. We targeted data from 2011 to 2017, adding the data of complications to cases that have already been reported in the 2011‐2016 Report on the 115 gastroenterological surgical procedures. Complications included surgical site infection (SSI), wound dehiscence, anastomotic leakage, pancreatic fistula, bile leakage, pneumonia, unplanned intubation, pulmonary embolism, ventilator‐assisted respiration longer than 48 hours, progressive renal insufficiency, acute renal failure, urinary tract infection, cerebrovascular accident with neurological deficit, coma longer than 24 hours, peripheral nerve injury, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, bleeding complication defined as transfusion in excess of one unit of blood, deep venous thrombosis, and sepsis. Postoperative complications were categorized into six grades according to the Clavien‐Dindo (C‐D) classification.20 In this study, complications of grade III (complications requiring intervention) or higher were defined as severe complications. Furthermore, among the 115 surgical procedures, we separated and studied the eight main operative methods that we deemed important in terms of medical standards.
We clarified the number of surgical cases and the mortality rates related to the 115 selected gastroenterological operative procedures. We also clarified the changes over time in the annual number of surgical cases, preoperative morbidity rates, and mortality rates related to the eight main operative procedures from 2011 to 2017. We also comparatively studied patient gender, age groups, institution type, and percentage of surgeries carried out by certified surgeons related to the eight main operative procedures.
The following points need to be considered in the interpretation of the data reported here. (i) As a maximum of eight operative procedures can be recorded for each case in the NCD, the total number of surgeries in “Results of the 115 gastroenterological surgical procedures for board certification system” is not the actual total number of surgical cases; (ii) cases with abnormal data or missing information in patient age, gender, or 30‐day postoperative status were excluded; (iii) cases in which several operative methods were carried out simultaneously were tallied for all operative methods; (iv) postoperative 30‐day mortality included all cases of mortality within 30 days after surgery regardless of pre‐ or post‐discharge status. Calculation of operative mortality included all patients who died during the index hospitalization, including hospital stays of up to 90 days, and any patient who died after hospital discharge within 30 days of the operative date.
3. RESULTS
3.1. Analysis of cases who underwent one or more of the 115 selected gastrointestinal operative procedures in the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology”
The total number of cases that underwent one or more of the 115 selected gastroenterological surgical procedures reported in the NCD between January 1, 2011 and December 31, 2017 was 3 818 414. Based on organ involvement, 61 242 cases involved the esophagus (1.6%); 507 827 cases the stomach and duodenum (13.3%); 1 409 527 cases the small intestine and colon (36.9%); 360 101 cases the rectum and anus (9.4%); 182 462 cases the liver (4.8%); 894 793 cases the gallbladder (23.4%); 117 503 cases the pancreas (3.1%); 26 135 cases the spleen (0.7%), and 258 824 cases other organs (6.8%). The annual number of surgical cases for each organ generally showed an increasing trend over time except for surgeries on the stomach and duodenum, and surgeries on the spleen. The male : female ratio was approximately 8:2 for surgeries on the esophagus, 7:3 for surgeries on the stomach and duodenum, 7:3 for surgeries on the liver, and 6:4 for surgeries on other organs. Year by year, the percentages of older patients have been increasing for all organs (Table 1).
Table 1.
Annual changes in percentage of surgeries by gender and age group for 115 selected GI operative procedures in the training curriculum for board‐certified surgeons in gastroenterology classified according to target organ
| Organ | Year | No. of surgeries | Percentage by gender | Percentage according to age group (y) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | <60 | 60 to <65 | 65 to <70 | 70 to <75 | 75 to <80 | ≥80 | |||
| Esophagus | 2011 | 7246 | 81.8 | 18.2 | 22.5 | 19.6 | 21.1 | 18.7 | 12.0 | 6.0 |
| 2012 | 8819 | 82.2 | 17.8 | 22.1 | 19.7 | 20.0 | 19.5 | 12.9 | 6.0 | |
| 2013 | 8642 | 81.5 | 18.5 | 20.8 | 17.5 | 21.0 | 20.6 | 13.2 | 6.9 | |
| 2014 | 9021 | 81.5 | 18.4 | 20.8 | 16.5 | 21.4 | 20.9 | 13.8 | 6.6 | |
| 2015 | 8943 | 80.8 | 19.2 | 19.6 | 15.3 | 22.4 | 22.5 | 13.1 | 7.1 | |
| 2016 | 9212 | 79.6 | 20.4 | 20.1 | 14.4 | 22.9 | 20.5 | 14.5 | 7.5 | |
| 2017 | 9359 | 80.0 | 20.0 | 19.3 | 13.4 | 24.4 | 19.4 | 15.5 | 8.0 | |
| Stomach and duodenum | 2011 | 66 740 | 68.0 | 32.0 | 20.1 | 14.4 | 14.0 | 17.1 | 16.4 | 18.0 |
| 2012 | 76 186 | 68.3 | 31.7 | 18.9 | 14.4 | 14.5 | 17.1 | 16.4 | 18.6 | |
| 2013 | 75 583 | 67.9 | 32.1 | 18.6 | 13.1 | 15.5 | 17.2 | 16.9 | 18.7 | |
| 2014 | 74 920 | 67.6 | 32.4 | 17.9 | 12.1 | 16.0 | 17.8 | 16.7 | 19.5 | |
| 2015 | 73 877 | 67.8 | 32.2 | 17.4 | 11.1 | 17.1 | 17.8 | 16.6 | 19.9 | |
| 2016 | 72 234 | 67.8 | 32.2 | 17.0 | 10.2 | 18.1 | 17.1 | 16.6 | 21.0 | |
| 2017 | 68 287 | 67.2 | 32.8 | 16.3 | 9.9 | 17.5 | 17.3 | 17.2 | 21.8 | |
| Small intestine and colon | 2011 | 151 143 | 56.7 | 43.3 | 37.4 | 10.9 | 10.5 | 12.1 | 12.2 | 16.9 |
| 2012 | 184 810 | 56.7 | 43.3 | 36.4 | 10.7 | 10.7 | 12.2 | 12.5 | 17.4 | |
| 2013 | 198 677 | 56.9 | 43.1 | 35.6 | 10.1 | 11.3 | 12.7 | 12.4 | 17.8 | |
| 2014 | 206 857 | 56.9 | 43.1 | 34.7 | 9.4 | 12.0 | 13.1 | 12.4 | 18.4 | |
| 2015 | 214 453 | 57.1 | 42.9 | 34.0 | 8.9 | 12.9 | 13.1 | 12.3 | 18.7 | |
| 2016 | 218 228 | 57.3 | 42.7 | 33.7 | 8.4 | 13.6 | 12.5 | 12.4 | 19.3 | |
| 2017 | 235 359 | 56.7 | 43.3 | 32.7 | 8.0 | 13.2 | 12.7 | 12.9 | 20.5 | |
| Rectum and anus | 2011 | 41 061 | 59.1 | 40.9 | 22.0 | 16.1 | 14.6 | 15.4 | 14.2 | 17.7 |
| 2012 | 49 704 | 58.3 | 41.7 | 22.3 | 14.8 | 14.6 | 15.5 | 14.3 | 18.5 | |
| 2013 | 49 980 | 58.0 | 42.0 | 20.9 | 13.9 | 15.2 | 16.1 | 14.6 | 19.3 | |
| 2014 | 51 454 | 58.3 | 41.7 | 20.4 | 13.1 | 16.0 | 16.4 | 14.2 | 19.9 | |
| 2015 | 56 092 | 57.8 | 42.2 | 22.3 | 11.8 | 16.7 | 15.7 | 14.0 | 19.4 | |
| 2016 | 55 666 | 57.3 | 42.7 | 22.0 | 11.1 | 17.9 | 15.0 | 13.6 | 20.4 | |
| 2017 | 56 144 | 56.7 | 43.3 | 22.2 | 10.2 | 17.3 | 15.1 | 14.2 | 21.0 | |
| Liver | 2011 | 22 855 | 67.3 | 32.7 | 22.2 | 16.5 | 16.3 | 18.7 | 17.2 | 9.2 |
| 2012 | 26 288 | 66.3 | 33.7 | 22.1 | 15.7 | 16.7 | 18.0 | 17.4 | 10.2 | |
| 2013 | 25 814 | 66.1 | 33.9 | 21.3 | 14.6 | 17.6 | 18.7 | 17.3 | 10.5 | |
| 2014 | 26 518 | 66.3 | 33.7 | 21.5 | 13.7 | 18.1 | 19.8 | 16.6 | 10.3 | |
| 2015 | 26 378 | 65.7 | 34.3 | 20.8 | 12.8 | 18.9 | 19.4 | 16.5 | 11.5 | |
| 2016 | 27 212 | 66.4 | 33.6 | 20.3 | 11.5 | 20.5 | 18.6 | 17.0 | 12.1 | |
| 2017 | 27 397 | 65.8 | 34.2 | 20.1 | 11.0 | 20.2 | 18.8 | 17.2 | 12.7 | |
| Gallbladder | 2011 | 103 183 | 54.5 | 45.4 | 34.3 | 14.0 | 12.2 | 13.8 | 12.8 | 13.0 |
| 2012 | 122 513 | 55.2 | 44.8 | 32.9 | 13.8 | 12.4 | 13.9 | 13.2 | 13.8 | |
| 2013 | 129 162 | 55.3 | 44.7 | 32.6 | 12.9 | 13.0 | 14.2 | 13.2 | 14.0 | |
| 2014 | 131 182 | 55.6 | 44.4 | 32.1 | 11.8 | 13.9 | 14.5 | 13.2 | 14.5 | |
| 2015 | 133 126 | 55.6 | 44.4 | 32.0 | 11.2 | 15.0 | 14.1 | 13.0 | 14.8 | |
| 2016 | 137 360 | 55.4 | 44.6 | 32.6 | 10.6 | 15.5 | 13.1 | 12.9 | 15.3 | |
| 2017 | 138 267 | 55.6 | 44.4 | 32.2 | 10.2 | 15.1 | 13.5 | 13.2 | 15.8 | |
| Pancreas | 2011 | 13 477 | 59.9 | 40.1 | 20.0 | 15.6 | 16.9 | 19.7 | 17.7 | 10.2 |
| 2012 | 15 550 | 60.0 | 40.0 | 19.8 | 15.2 | 17.0 | 19.5 | 18.2 | 10.3 | |
| 2013 | 16 380 | 59.7 | 40.3 | 19.1 | 13.6 | 18.0 | 20.7 | 17.7 | 10.9 | |
| 2014 | 17 313 | 59.5 | 40.5 | 18.4 | 12.4 | 19.0 | 21.0 | 18.2 | 11.1 | |
| 2015 | 17 407 | 59.1 | 40.9 | 18.2 | 11.3 | 19.4 | 21.6 | 18.1 | 11.4 | |
| 2016 | 18 238 | 58.9 | 41.1 | 18.2 | 10.4 | 19.9 | 20.4 | 19.0 | 12.2 | |
| 2017 | 19 138 | 59.2 | 40.8 | 17.7 | 9.9 | 19.5 | 19.9 | 20.1 | 12.9 | |
| Spleen | 2011 | 3609 | 61.3 | 38.7 | 35.3 | 15.6 | 14.7 | 14.8 | 11.9 | 7.8 |
| 2012 | 4142 | 61.4 | 38.6 | 32.9 | 16.3 | 15.0 | 15.1 | 12.9 | 7.8 | |
| 2013 | 4509 | 61.8 | 38.2 | 30.8 | 14.9 | 15.9 | 16.5 | 13.1 | 8.7 | |
| 2014 | 4272 | 61.8 | 38.2 | 29.9 | 13.0 | 17.3 | 17.0 | 13.8 | 9.1 | |
| 2015 | 3568 | 60.4 | 39.6 | 29.7 | 11.4 | 17.3 | 16.6 | 14.1 | 10.8 | |
| 2016 | 3171 | 57.3 | 42.7 | 31.9 | 11.7 | 17.7 | 15.7 | 12.5 | 10.5 | |
| 2017 | 2864 | 58.7 | 41.3 | 31.6 | 11.0 | 18.1 | 16.0 | 13.3 | 10.0 | |
| Other | 2011 | 23 218 | 55.0 | 45.0 | 32.0 | 11.9 | 11.3 | 13.3 | 13.8 | 17.6 |
| 2012 | 28 779 | 55.4 | 44.6 | 31.1 | 11.7 | 11.7 | 13.8 | 13.7 | 18.0 | |
| 2013 | 36 363 | 53.1 | 46.9 | 28.3 | 10.9 | 12.7 | 14.1 | 14.8 | 19.1 | |
| 2014 | 39 854 | 53.7 | 46.3 | 28.1 | 10.1 | 13.1 | 14.5 | 14.4 | 19.8 | |
| 2015 | 41 465 | 53.2 | 46.8 | 27.4 | 9.4 | 14.0 | 14.5 | 14.2 | 20.6 | |
| 2016 | 43 523 | 54.0 | 46.0 | 27.5 | 9.2 | 14.6 | 13.5 | 14.0 | 21.2 | |
| 2017 | 45 622 | 54.1 | 45.9 | 27.0 | 8.2 | 14.7 | 13.5 | 14.6 | 21.9 | |
Abbreviation: GI, gastrointestinal.
In terms of the type of institution in which the surgeries were carried out, more than 70% of all surgeries were carried out at certified institutions, and the percentage of surgeries carried out at certified institutions was particularly high in 2017 for surgeries on the esophagus (92.7%) and pancreas (90.4%). The percentage of surgeries with participation of an anesthesiologist was more than 90% for almost all organs, except 84.8% for the rectum and anus. More than 70% of surgeries on most organs were carried out with the participation of a board‐certified surgeon. In 2017, the percentage of surgeries in which a certified surgeon was the operator was high for surgeries on the esophagus (71.8%), liver (62.5%), and pancreas (63.9%; Table 2). Postoperative complications, operative mortality rates, and 30‐day postoperative mortality rates are shown in Table 3. Complication rates were comparatively higher in 2017 for surgeries on the esophagus (20.7%) and the pancreas (21.3%); however, the mortality rates for procedures on these organs were not so high. Figure 1 shows the number of surgeries, rates of complications and mortality rates among cases who underwent the 115 gastroenterological surgical procedures according to organ involvement. Tables 4, 5, 6, 7, 8, 9, 10, 11, 12 show the number of surgeries carried out using each of the 115 gastroenterological surgical procedures, according to recording year and organ.
Table 2.
Institution type, anesthesiologist and specialist participation rates in the 115 selected GI operative procedures that were classified according to target organ
| Organ | Year | No. of surgeries | Percentage by institution type | Anesthesiologist participation (%) | Board‐certified surgeon participation (%) | Medical practitioners (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| Certified institution | Related institution | Other | Board‐certified surgeons | Non‐board‐certified surgeons | |||||
| Esophagus | 2011 | 7246 | 93.5 | 5.9 | 0.6 | 97.0 | 87.0 | 62.8 | 37.2 |
| 2012 | 8819 | 78.1 | 5.9 | 16.0 | 97.4 | 87.0 | 62.7 | 37.3 | |
| 2013 | 8642 | 90.6 | 7.1 | 2.4 | 97.3 | 88.4 | 64.4 | 35.6 | |
| 2014 | 9021 | 91.1 | 6.1 | 2.8 | 97.9 | 90.1 | 67.6 | 32.4 | |
| 2015 | 8943 | 91.5 | 6.0 | 2.5 | 97.9 | 91.1 | 69.4 | 30.6 | |
| 2016 | 9212 | 92.4 | 5.0 | 2.6 | 98.2 | 91.2 | 70.0 | 30.0 | |
| 2017 | 9359 | 92.7 | 4.0 | 3.3 | 97.9 | 92.5 | 71.8 | 28.2 | |
| Stomach and duodenum | 2011 | 66 740 | 80.2 | 17.3 | 2.6 | 92.8 | 69.3 | 35.1 | 64.9 |
| 2012 | 76 186 | 63.5 | 15.6 | 20.9 | 93.5 | 70.3 | 35.6 | 64.4 | |
| 2013 | 75 583 | 76.3 | 19.3 | 4.4 | 93.3 | 73.5 | 37.7 | 62.3 | |
| 2014 | 74 920 | 77.0 | 18.2 | 4.8 | 93.6 | 75.9 | 39.2 | 60.8 | |
| 2015 | 73 877 | 77.1 | 18.3 | 4.6 | 93.9 | 76.1 | 39.2 | 60.8 | |
| 2016 | 72 234 | 79.6 | 16.1 | 4.3 | 94.6 | 78.7 | 41.0 | 59.0 | |
| 2017 | 68 287 | 79.6 | 15.3 | 5.1 | 94.8 | 79.7 | 41.8 | 58.2 | |
| Small intestine and colon | 2011 | 151 143 | 76.8 | 20.2 | 2.9 | 88.1 | 59.2 | 25.1 | 74.9 |
| 2012 | 184 810 | 60.6 | 18.2 | 21.2 | 88.9 | 59.9 | 25.4 | 74.6 | |
| 2013 | 198 677 | 72.6 | 22.2 | 5.2 | 89.6 | 62.7 | 26.6 | 73.4 | |
| 2014 | 206 857 | 73.0 | 21.4 | 5.6 | 90.8 | 65.4 | 28.1 | 71.9 | |
| 2015 | 214 453 | 73.8 | 20.7 | 5.5 | 91.6 | 66.3 | 28.5 | 71.5 | |
| 2016 | 218 228 | 75.6 | 19.0 | 5.5 | 92.4 | 68.1 | 29.5 | 70.5 | |
| 2017 | 235 359 | 76.0 | 18.0 | 6.0 | 92.9 | 70.1 | 31.1 | 68.9 | |
| Rectum and anus | 2011 | 41 061 | 76.9 | 19.0 | 4.1 | 86.3 | 68.3 | 36.9 | 63.1 |
| 2012 | 49 704 | 60.4 | 18.2 | 21.4 | 85.7 | 68.6 | 37.6 | 62.4 | |
| 2013 | 49 980 | 72.9 | 21.7 | 5.4 | 87.3 | 71.2 | 39.4 | 60.6 | |
| 2014 | 51 454 | 73.5 | 20.9 | 5.6 | 87.9 | 73.7 | 41.6 | 58.4 | |
| 2015 | 56 092 | 72.5 | 20.8 | 6.7 | 84.9 | 73.5 | 41.5 | 58.5 | |
| 2016 | 55 666 | 74.1 | 19.4 | 6.6 | 85.7 | 74.7 | 42.1 | 57.9 | |
| 2017 | 56 144 | 73.8 | 18.2 | 8.0 | 84.8 | 76.1 | 43.9 | 56.1 | |
| Liver | 2011 | 22 855 | 89.3 | 9.7 | 1.1 | 95.6 | 85.2 | 55.2 | 44.8 |
| 2012 | 26 288 | 74.2 | 9.2 | 16.7 | 95.4 | 85.7 | 57.4 | 42.6 | |
| 2013 | 25 814 | 86.3 | 10.7 | 2.9 | 96.3 | 87.5 | 57.1 | 42.9 | |
| 2014 | 26 518 | 86.3 | 10.0 | 3.7 | 96.4 | 89.0 | 59.6 | 40.4 | |
| 2015 | 26 378 | 87.3 | 9.5 | 3.2 | 96.6 | 89.1 | 59.1 | 40.9 | |
| 2016 | 27 212 | 88.4 | 8.8 | 2.9 | 96.8 | 90.0 | 59.6 | 40.4 | |
| 2017 | 27 397 | 89.0 | 7.8 | 3.1 | 97.1 | 91.8 | 62.5 | 37.5 | |
| Gallbladder | 2011 | 103 183 | 73.9 | 22.5 | 3.6 | 91.8 | 61.9 | 26.4 | 73.6 |
| 2012 | 122 513 | 57.5 | 19.6 | 22.9 | 92.1 | 62.8 | 26.3 | 73.7 | |
| 2013 | 129 162 | 69.9 | 24.1 | 5.9 | 92.2 | 65.4 | 27.3 | 72.7 | |
| 2014 | 131 182 | 70.3 | 23.3 | 6.4 | 92.3 | 67.4 | 28.1 | 71.9 | |
| 2015 | 133 126 | 70.8 | 22.8 | 6.4 | 92.9 | 68.4 | 28.1 | 71.9 | |
| 2016 | 137 360 | 72.4 | 21.3 | 6.3 | 93.5 | 69.4 | 28.9 | 71.1 | |
| 2017 | 138 267 | 72.6 | 20.1 | 7.3 | 93.7 | 71.4 | 29.9 | 70.1 | |
| Pancreas | 2011 | 13 477 | 88.1 | 10.8 | 1.2 | 95.8 | 85.2 | 57.7 | 42.3 |
| 2012 | 15 550 | 72.8 | 8.7 | 18.5 | 96.3 | 86.5 | 59.9 | 40.1 | |
| 2013 | 16 380 | 86.5 | 11.0 | 2.4 | 95.9 | 87.6 | 60.2 | 39.8 | |
| 2014 | 17 313 | 86.9 | 9.9 | 3.3 | 96.2 | 89.1 | 61.3 | 38.7 | |
| 2015 | 17 407 | 88.4 | 9.1 | 2.4 | 96.4 | 90.3 | 61.6 | 38.4 | |
| 2016 | 18 238 | 89.8 | 8.0 | 2.3 | 96.8 | 91.1 | 62.4 | 37.6 | |
| 2017 | 19 138 | 90.4 | 7.1 | 2.5 | 97.2 | 92.3 | 63.9 | 36.1 | |
| Spleen | 2011 | 3609 | 87.0 | 11.6 | 1.4 | 94.6 | 75.2 | 44.9 | 55.1 |
| 2012 | 4142 | 70.5 | 9.5 | 20.0 | 81.7 | 75.8 | 44.4 | 55.6 | |
| 2013 | 4509 | 83.2 | 13.8 | 3.0 | 95.2 | 75.4 | 43.3 | 56.7 | |
| 2014 | 4272 | 85.4 | 11.5 | 3.1 | 94.6 | 77.5 | 45.2 | 54.8 | |
| 2015 | 3568 | 85.6 | 12.3 | 2.1 | 94.8 | 78.9 | 45.5 | 54.5 | |
| 2016 | 3171 | 86.8 | 10.1 | 3.1 | 95.7 | 80.5 | 48.0 | 52.0 | |
| 2017 | 2864 | 87.4 | 9.3 | 3.3 | 95.3 | 82.3 | 49.1 | 50.9 | |
| Other | 2011 | 23 218 | 80.2 | 17.0 | 2.8 | 90.3 | 60.4 | 27.2 | 72.8 |
| 2012 | 28 779 | 65.7 | 15.2 | 19.1 | 91.0 | 61.1 | 27.6 | 72.4 | |
| 2013 | 36 363 | 76.1 | 19.3 | 4.6 | 91.5 | 63.4 | 28.5 | 71.5 | |
| 2014 | 39 854 | 76.6 | 18.2 | 5.1 | 91.9 | 64.9 | 29.7 | 70.3 | |
| 2015 | 41 465 | 78.0 | 17.2 | 4.8 | 92.4 | 65.6 | 29.4 | 70.6 | |
| 2016 | 43 523 | 79.4 | 15.8 | 4.8 | 92.7 | 67.3 | 30.3 | 69.7 | |
| 2017 | 45 622 | 80.1 | 14.8 | 5.1 | 93.1 | 69.7 | 32.3 | 67.7 | |
Abbreviation: GI, gastrointestinal.
Table 3.
No. of surgeries, postoperative complication rates and mortality rates in the 115 selected GI operative procedures that were classified according to target organ
| Organ | Year | No. of surgeries | No. of postoperative complicationsa/rate (%) | No. of postoperative 30‐d mortalities/rate (%) | No. of postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|
| Esophagus | 2011 | 7246 | 1294/17.9 | 87/1.2 | 279/3.9 |
| 2012 | 8819 | 1653/18.7 | 117/1.3 | 315/3.6 | |
| 2013 | 8642 | 1593/18.4 | 121/1.4 | 327/3.8 | |
| 2014 | 9021 | 1679/18.6 | 115/1.3 | 289/3.2 | |
| 2015 | 8943 | 1709/19.1 | 103/1.2 | 304/3.4 | |
| 2016 | 9212 | 1805/19.6 | 100/1.1 | 238/2.6 | |
| 2017 | 9359 | 1938/20.7 | 108/1.2 | 208/2.2 | |
| Stomach and duodenum | 2011 | 66 740 | 5354/8.0 | 992/1.5 | 2183/3.3 |
| 2012 | 76 186 | 6447/8.5 | 1085/1.4 | 2381/3.1 | |
| 2013 | 75 583 | 6380/8.4 | 1059/1.4 | 2269/3.0 | |
| 2014 | 74 920 | 6328/8.4 | 1064/1.4 | 2174/2.9 | |
| 2015 | 73 877 | 6418/8.7 | 1007/1.4 | 2110/2.9 | |
| 2016 | 72 234 | 6413/8.9 | 1066/1.5 | 2016/2.8 | |
| 2017 | 68 287 | 6455/9.5 | 1046/1.5 | 1863/2.7 | |
| Small intestine and colon | 2011 | 151 143 | 12 184/8.1 | 2943/1.9 | 5390/3.6 |
| 2012 | 184 810 | 15 395/8.3 | 3564/1.9 | 6583/3.6 | |
| 2013 | 198 677 | 16 709/8.4 | 3723/1.9 | 6803/3.4 | |
| 2014 | 206 857 | 17 776/8.6 | 3822/1.9 | 6961/3.4 | |
| 2015 | 214 453 | 18 372/8.6 | 4019/1.9 | 7092/3.3 | |
| 2016 | 218 228 | 19 020/8.7 | 3933/1.8 | 6621/3.0 | |
| 2017 | 235 359 | 21 854/9.3 | 4588/1.9 | 7118/3.0 | |
| Rectum and anus | 2011 | 41 061 | 3584/8.7 | 395/1.0 | 676/1.6 |
| 2012 | 49 704 | 4488/9.0 | 462/0.9 | 802/1.6 | |
| 2013 | 49 980 | 4684/9.4 | 517/1.0 | 858/1.7 | |
| 2014 | 51 454 | 4711/9.2 | 449/0.9 | 792/1.5 | |
| 2015 | 56 092 | 4986/8.9 | 519/0.9 | 824/1.5 | |
| 2016 | 55 666 | 5194/9.3 | 503/0.9 | 766/1.4 | |
| 2017 | 56 144 | 5600/10.0 | 556/1.0 | 829/1.5 | |
| Liver | 2011 | 22 855 | 1933/8.5 | 309/1.4 | 590/2.6 |
| 2012 | 26 288 | 2454/9.3 | 310/1.2 | 605/2.3 | |
| 2013 | 25 814 | 2549/9.9 | 275/1.1 | 575/2.2 | |
| 2014 | 26 518 | 2466/9.3 | 246/0.9 | 481/1.8 | |
| 2015 | 26 378 | 2537/9.6 | 234/0.9 | 451/1.7 | |
| 2016 | 27 212 | 2543/9.3 | 222/0.8 | 382/1.4 | |
| 2017 | 27 397 | 2724/9.9 | 214/0.8 | 364/1.3 | |
| Gallbladder | 2011 | 103 183 | 3473/3.4 | 483/0.5 | 946/0.9 |
| 2012 | 122 513 | 4587/3.7 | 531/0.4 | 1082/0.9 | |
| 2013 | 129 162 | 4982/3.9 | 546/0.4 | 1130/0.9 | |
| 2014 | 131 182 | 5020/3.8 | 569/0.4 | 1097/0.8 | |
| 2015 | 133 126 | 5231/3.9 | 541/0.4 | 1036/0.8 | |
| 2016 | 137 360 | 5320/3.9 | 559/0.4 | 980/0.7 | |
| 2017 | 138 267 | 5761/4.2 | 576/0.4 | 968/0.7 | |
| Pancreas | 2011 | 13 477 | 1994/14.8 | 175/1.3 | 386/2.9 |
| 2012 | 15 550 | 2595/16.7 | 213/1.4 | 437/2.8 | |
| 2013 | 16 380 | 2917/17.8 | 211/1.3 | 482/2.9 | |
| 2014 | 17 313 | 2966/17.1 | 195/1.1 | 423/2.4 | |
| 2015 | 17 407 | 3229/18.6 | 185/1.1 | 379/2.2 | |
| 2016 | 18 238 | 3543/19.4 | 185/1.0 | 390/2.1 | |
| 2017 | 19 138 | 4076/21.3 | 219/1.1 | 365/1.9 | |
| Spleen | 2011 | 3609 | 400/11.1 | 83/2.3 | 137/3.8 |
| 2012 | 4142 | 528/12.7 | 84/2.0 | 138/3.3 | |
| 2013 | 4509 | 575/12.8 | 79/1.8 | 139/3.1 | |
| 2014 | 4272 | 549/12.9 | 88/2.1 | 137/3.2 | |
| 2015 | 3568 | 543/15.2 | 88/2.5 | 144/4.0 | |
| 2016 | 3171 | 449/14.2 | 76/2.4 | 117/3.7 | |
| 2017 | 2864 | 434/15.2 | 65/2.3 | 89/3.1 | |
| Others | 2011 | 23 218 | 3494/15.0 | 1163/5.0 | 1887/8.1 |
| 2012 | 28 779 | 4388/15.2 | 1399/4.9 | 2293/8.0 | |
| 2013 | 36 363 | 4712/13.0 | 1401/3.9 | 2346/6.5 | |
| 2014 | 39 854 | 5176/13.0 | 1521/3.8 | 2489/6.2 | |
| 2015 | 41 465 | 5380/13.0 | 1541/3.7 | 2545/6.1 | |
| 2016 | 43 523 | 5975/13.7 | 1760/4.0 | 2684/6.2 | |
| 2017 | 45 622 | 6539/14.3 | 1909/4.2 | 2699/5.9 |
Abbreviation: GI, gastrointestinal.
Complications with Clavien‐Dindo grades IIIa to V.
Figure 1.
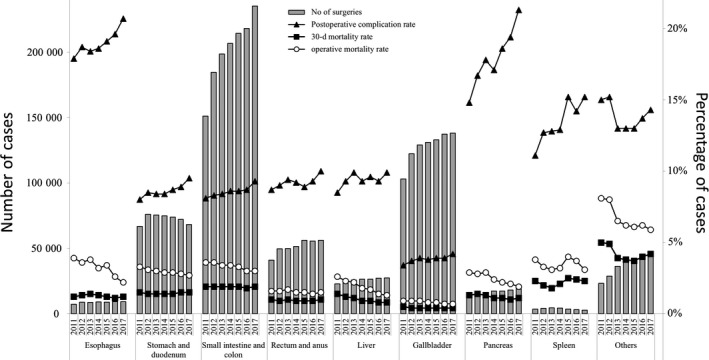
Annual changes in the number of surgeries, postoperative complication rate, operative mortality rate, and 30‐d postoperative mortality rate: analysis of the 115 selected surgical procedures that were classified according to the involved organ. Postoperative complication rate: the rate of complications with Clavien‐Dindo (C‐D) classification of grade III (complications requiring intervention) or higher
Table 4.
Changes in the annual number of surgeries among the GI operative procedures on the esophagus
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Esophagus | Low | Cervical periesophageal abscess drainage | 23 | 27 | 34 | 42 | 37 | 43 | 39 |
| Med | Esophageal suture (perforation, injury) | 156 | 204 | 198 | 185 | 199 | 215 | 202 | |
| Med | Thoracic periesophageal abscess drainage | 22 | 23 | 18 | 27 | 27 | 21 | 21 | |
| Med | Esophageal foreign body extraction | 19 | 21 | 26 | 25 | 30 | 32 | 35 | |
| Med | Esophageal diverticulum resection | 27 | 32 | 35 | 48 | 41 | 34 | 47 | |
| Med | Benign esophageal tumor removal | 61 | 69 | 66 | 68 | 52 | 64 | 73 | |
| Med | Esophageal resection (removal only) | 388 | 506 | 580 | 570 | 571 | 721 | 720 | |
| Med | Esophageal reconstruction: reconstruction only (gastric tube reconstruction) | 699 | 844 | 888 | 799 | 848 | 772 | 828 | |
| Med | Esophageal fistula construction | 97 | 106 | 128 | 126 | 125 | 162 | 176 | |
| Med | Esophagocardioplasty | 321 | 418 | 392 | 398 | 362 | 365 | 366 | |
| Med | Achalasia surgery | 77 | 109 | 84 | 118 | 101 | 210 | 208 | |
| High | Esophagectomy | 4916 | 5946 | 5694 | 6091 | 6060 | 6041 | 6100 | |
| High | Esophageal reconstruction: reconstruction only (colon reconstruction) | 65 | 56 | 63 | 77 | 51 | 40 | 41 | |
| High | Esophageal bypass | 93 | 110 | 137 | 143 | 152 | 130 | 154 | |
| High | Bronchoesophageal fistula surgery | 6 | 5 | 9 | 12 | 7 | 13 | 5 | |
| High | Secondary esophageal reconstruction | 276 | 343 | 290 | 292 | 280 | 349 | 344 | |
Abbreviation: GI, gastrointestinal; Med, medium.
Table 5.
Changes in the annual number of surgeries among the GI operative procedures on the stomach and duodenum
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Stomach and duodenum | Low | Gastrostomy and suture gastrorrhaphy | 52 | 69 | 74 | 66 | 65 | 77 | 64 |
| Low | Diverticulum, polypectomy (excluding endoscopic resection) | 156 | 186 | 231 | 247 | 226 | 202 | 230 | |
| Low | Truncal vagotomy | 3 | 6 | 6 | 2 | 6 | 3 | 4 | |
| Low | Gastroenterostomy (including duodenal jejunostomy) | 4651 | 5330 | 5571 | 5893 | 5636 | 5633 | 5867 | |
| Low | Gastric fistula construction (excluding PEG) | 1717 | 1698 | 1633 | 1722 | 1790 | 1748 | 1695 | |
| Low | Gastric pyloroplasty | 116 | 129 | 115 | 126 | 100 | 69 | 82 | |
| Low | Gastric volvulus (volvulus) surgery and rectopexy | 40 | 38 | 39 | 0 | 47 | 42 | 56 | |
| Low | Gastric suture (including gastric suture for gastric rupture, suture closure for gastroduodenal perforation, omental implantation and omental transposition) | 4707 | 5738 | 5669 | 5837 | 5858 | 6164 | 5847 | |
| Low | Local gastrectomy (including wedge resection) | 2466 | 3108 | 3233 | 3354 | 3625 | 3766 | 4076 | |
| Med | Gastrectomy (including distal gastrectomy, pylorus‐preserving gastrectomy and segmental [transverse] gastrectomy) | 34 160 | 38 750 | 39 957 | 38 584 | 37 819 | 36 852 | 35 517 | |
| Med | Selective vagotomy | 8 | 8 | 10 | 7 | 6 | 4 | 6 | |
| High | Total gastrectomy (including fundusectomy) | 18 652 | 21 122 | 19 035 | 19 071 | 18 695 | 17 670 | 14 840 | |
| High | Left upper abdominal exenteration | 12 | 4 | 10 | 11 | 4 | 4 | 3 | |
Abbreviations: GI, gastrointestinal; PEG, percutaneous endoscopic gastrostomy.
Table 6.
Changes in the annual number of surgeries among the GI operative procedures on the small intestine and colon
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Small intestine and colon | Low | Enterotomy and enterorrhaphy | 2982 | 3505 | 4025 | 4362 | 4412 | 4311 | 4378 |
| Low | Disinvagination (invasive) | 172 | 250 | 234 | 239 | 209 | 242 | 221 | |
| Low | Partial enterectomy (benign) | 5792 | 7602 | 8564 | 8938 | 9449 | 9591 | 9465 | |
| Low | Ileocecal resection (benign) | 3238 | 4104 | 4313 | 4472 | 4523 | 4675 | 4643 | |
| Low | Partial colectomy and sigmoid colectomy (benign) | 4946 | 6239 | 6626 | 7358 | 7583 | 7971 | 8115 | |
| Low | Appendectomy | 43 437 | 51 316 | 54 421 | 54 319 | 54 897 | 55 168 | 55 261 | |
| Low | Enterostomy and closure (without enterectomy) | 15 192 | 19 371 | 21 600 | 23 425 | 24 666 | 25 458 | 26 795 | |
| Med | Enterectomy (malignant) | 2448 | 2703 | 3016 | 3082 | 3320 | 3360 | 3671 | |
| Med | Ileocecal resection (malignant) | 5492 | 9274 | 10 327 | 11 368 | 12 224 | 12 872 | 13 133 | |
| Med | Partial colectomy and sigmoid colectomy (malignant) | 25 034 | 29 863 | 31 495 | 32 092 | 33 518 | 33 936 | 32 986 | |
| Med | Right hemicolectomy | 17 890 | 21 034 | 21 814 | 22 446 | 22 850 | 22 829 | 22 543 | |
| Med | Left hemicolectomy | 5241 | 5347 | 5644 | 5763 | 6119 | 6178 | 5991 | |
| Med | Total colectomy | 2846 | 3131 | 1892 | 1701 | 1752 | 1735 | 1789 | |
| Med | Intestinal obstruction surgery (with bowel resection) | 5117 | 6496 | 7412 | 7775 | 7912 | 7898 | 24 142a | |
| Med | Enterostomy and closure (with enterectomy) | 11 008 | 14 162 | 16 853 | 19 049 | 20 520 | 21 525 | 21 774 | |
| High | Proctocolectomy and ileoanal (canal) anastomosis | 308 | 413 | 441 | 468 | 499 | 479 | 452 | |
Abbreviation: GI, gastrointestinal.
2011‐2016: Intestinal obstruction surgery with bowel resection, 2017: Intestinal obstruction surgery with or without bowel resection.
Table 7.
Changes in the annual number of surgeries among the GI operative procedures on the rectum and anus
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Rectum and anus | Low | Transanal rectal tumor removal | 2483 | 3300 | 1657 | 1513 | 3690 | 3651 | 3761 |
| Low | Proctocele surgery (transanal) | 1802 | 2461 | 2488 | 2602 | 2773 | 2805 | 2810 | |
| Med | Rectectomy (benign) | 300 | 386 | 2196 | 2060 | 1914 | 1688 | 1491 | |
| Med | High anterior resection | 7053 | 8920 | 8985 | 9496 | 9934 | 10 477 | 10 546 | |
| Med | Hartmann's procedure | 3562 | 4614 | 4865 | 5194 | 5650 | 5755 | 6034 | |
| Med | Proctocele surgery (abdominoperineal) | 659 | 996 | 1119 | 1181 | 1411 | 1538 | 1771 | |
| Med | Malignant anorectal tumor excision (transanal) | 1517 | 1037 | 898 | 864 | 821 | 778 | 735 | |
| Med | Anal sphincteroplasty (by tissue replacement) | 969 | 1378 | 1721 | 1718 | 2132 | 2045 | 2520 | |
| High | Rectectomy (malignant) | 5308 | 5828 | 4474 | 4531 | 4825 | 5096 | 5082 | |
| High | Low anterior resection | 16 984 | 20 321 | 21 096 | 21 861 | 22 493 | 21 387 | 20 879 | |
| High | Pelvic evisceration | 359 | 389 | 412 | 374 | 385 | 402 | 456 | |
| High | Anorectal malignant tumor excision (posterior approach) | 65 | 74 | 69 | 60 | 64 | 44 | 59 | |
Abbreviation: GI, gastrointestinal.
Table 8.
Changes in the annual number of surgeries among the GI operative procedures on the liver
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Liver | Low | Hepatorrhaphy | 172 | 202 | 161 | 196 | 147 | 161 | 64 |
| Low | Liver abscess drainage (excluding percutaneous procedures) | 42 | 47 | 54 | 44 | 59 | 55 | 51 | |
| Low | Hepatic cyst resection. Suture. Drainage | 425 | 535 | 606 | 695 | 695 | 741 | 861 | |
| Low | Partial hepatectomy | 9431 | 10 919 | 10 708 | 11 598 | 12 063 | 12 604 | 12 847 | |
| Low | Liver biopsy (excluding percutaneous procedures) | 122 | 264 | 176 | 165 | 175 | 126 | 138 | |
| Low | Liver coagulonecrotic therapy (excluding percutaneous procedures) | 1958 | 2122 | 1083 | 1069 | 939 | 854 | 811 | |
| Med | Lateral segmentectomy of the liver | 1390 | 1632 | 1773 | 1807 | 1666 | 1704 | 1598 | |
| Med | Esophageal and gastric varix surgery | 94 | 109 | 67 | 61 | 46 | 67 | 52 | |
| High | Hepatectomy (segmented or more; excluding lateral segments) | 7434 | 8239 | 7937 | 7666 | 7439 | 7610 | 7698 | |
| High | Systematic subsegmentectomy | 996 | 1353 | 2374 | 2257 | 2221 | 2367 | 2391 | |
| High | Liver transplant | 692 | 775 | 757 | 848 | 790 | 800 | 748 | |
| High | Hepatopancreatoduodenectomy | 99 | 91 | 118 | 112 | 138 | 123 | 138 | |
Abbreviation: GI, gastrointestinal.
Table 9.
Changes in the annual number of surgeries among the GI operative procedures on the gallbladder
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Gallbladder | Low | Cholangiotomy | 142 | 163 | 174 | 139 | 141 | 132 | 106 |
| Low | Cysticolithectomy | 1094 | 1093 | 750 | 641 | 611 | 571 | 63 | |
| Low | Cholecystectomy | 93 665 | 112 048 | 119 455 | 122 026 | 124 267 | 128 809 | 130 570 | |
| Low | External cholecystostomy | 104 | 119 | 127 | 124 | 109 | 146 | 143 | |
| Low | Cystoenteric anastomosis | 70 | 73 | 61 | 61 | 67 | 59 | 54 | |
| Med | Cysticolithectomy | 3682 | 4117 | 3880 | 3574 | 3342 | 3057 | 2962 | |
| Med | Biliary tract reconstruction | 150 | 162 | 265 | 315 | 362 | 347 | 332 | |
| Med | Biliary bypass | 1594 | 1751 | 1765 | 1686 | 1613 | 1490 | 1300 | |
| Med | Cholangioplasty | 201 | 180 | 192 | 168 | 156 | 176 | 128 | |
| Med | Duodenal papilloplasty | 66 | 68 | 50 | 33 | 31 | 37 | 30 | |
| Med | Choledochal dilatation | 217 | 240 | 254 | 242 | 248 | 291 | 264 | |
| Med | Biliary fistula closure | 43 | 42 | 42 | 37 | 40 | 34 | 39 | |
| High | Malignant gallbladder tumor surgery (excluding simple cholecystectomy) | 869 | 1013 | 929 | 963 | 969 | 948 | 1027 | |
| High | Malignant bile duct tumor surgery | 1268 | 1426 | 1202 | 1153 | 1155 | 1245 | 1232 | |
| High | Biliary atresia surgery | 18 | 18 | 16 | 20 | 15 | 18 | 17 | |
Abbreviation: GI, gastrointestinal.
Table 10.
Changes in the annual number of surgeries among the GI operative procedures on the pancreas
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Pancreas | Low | External pancreatic cyst drainage | 29 | 27 | 13 | 21 | 8 | 13 | 15 |
| Low | External pancreatic duct drainage | 17 | 20 | 26 | 28 | 22 | 34 | 13 | |
| Med | Pancreatorrhaphy | 22 | 17 | 21 | 34 | 27 | 17 | 5 | |
| Med | Partial pancreatic resection | 126 | 148 | 202 | 182 | 165 | 177 | 187 | |
| Med | Distal pancreatectomy (benign) | 1018 | 1398 | 1372 | 1557 | 1477 | 1536 | 1568 | |
| Med | Pancreatoenteric anastomosis | 81 | 71 | 59 | 49 | 44 | 39 | 35 | |
| Med | Pancreatic (duct) anastomosis | 223 | 295 | 309 | 388 | 280 | 269 | 328 | |
| Med | Acute pancreatitis surgery | 94 | 117 | 104 | 103 | 90 | 132 | 76 | |
| Med | Pancreatolithiasis surgery | 17 | 17 | 14 | 35 | 31 | 29 | 22 | |
| Med | Plexus pancreaticus capitalis resection | 1 | 1 | 2 | 0 | 1 | 1 | 0 | |
| High | Pancreaticoduodenectomy | 8305 | 9329 | 10 068 | 10 400 | 10 576 | 11 028 | 11 580 | |
| High | Distal pancreatectomy (malignant) | 2861 | 3344 | 3483 | 3750 | 3930 | 4173 | 4508 | |
| High | Total pancreatectomy | 348 | 408 | 423 | 496 | 503 | 545 | 561 | |
| High | Duodenum‐preserving pancreas head resection | 201 | 193 | 111 | 85 | 63 | 49 | 50 | |
| High | Segmental pancreatic resection | 131 | 163 | 138 | 165 | 162 | 169 | 155 | |
| High | Distal pancreatectomy | 3 | 2 | 35 | 20 | 28 | 27 | 35 | |
Abbreviation: GI, gastrointestinal.
Table 11.
Changes in the annual number of surgeries among the GI operative procedures on the spleen
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Spleen | Low | Splenorrhaphy | 22 | 35 | 26 | 24 | 17 | 30 | 32 |
| Med | Splenectomy | 3564 | 4063 | 4457 | 4215 | 3525 | 3117 | 2811 | |
| Med | Partial splenic resection | 23 | 44 | 26 | 33 | 26 | 24 | 21 | |
Abbreviation: GI, gastrointestinal.
Table 12.
Changes in the annual number of surgeries among the GI operative procedures on other organs
| Organ | Degree of difficulty | Procedure | No. of surgeries | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Other | Low | Localized intra‐abdominal abscess surgery | 2526 | 2944 | 3231 | 3262 | 2942 | 2764 | 2630 |
| Low | Exploratory laparotomy | 5036 | 6852 | 7532 | 8271 | 8982 | 9629 | 10 416 | |
| Med | Acute diffuse peritonitis surgery | 7753 | 9177 | 10 447 | 12 085 | 13 030 | 13 981 | 14 423 | |
| Med | Ventral hernia surgery | 5053 | 6095 | 11 387 | 12 298 | 12 494 | 12 896 | 13 663 | |
| Med | Diaphragm suture | 183 | 218 | 246 | 213 | 257 | 253 | 313 | |
| Med | Esophageal hiatus hernia surgery | 511 | 602 | 725 | 757 | 800 | 842 | 981 | |
| Med | Retroperitoneal tumor surgery | 622 | 837 | 806 | 805 | 807 | 850 | 829 | |
| Med | Abdominal wall/mesenteric/omental tumor resection | 979 | 1398 | 1402 | 1509 | 1506 | 1707 | 1767 | |
| Med | Gastrointestinal perforation closure | 504 | 576 | 522 | 589 | 587 | 549 | 530 | |
| High | Diaphragmatic hiatus hernia surgery | 51 | 80 | 65 | 65 | 60 | 52 | 70 | |
Abbreviation: GI, gastrointestinal.
3.2. Eight main operative procedures
The number of surgeries carried out annually for the eight main operative procedures, the percentage by gender, and the percentage according to age group between 2011 and 2017 are shown in Table 13. The percentage of patients who were ≥80 years has been increasing for all eight main procedures. Regarding the institution type in which the surgeries were carried out, more than 75% of the surgeries were carried out at certified institutions and the percentage of surgeries done at certified institutions was particularly high in 2017 for esophagectomy (95.3%), hepatectomy (non‐lateral segments; 91.2%), and pancreaticoduodenectomy (90.5%). The percentage of surgeries with participation of an anesthesiologist was more than 90% for all eight procedures. Approximately 95% of esophagectomy, hepatectomy (non‐lateral segments), and pancreaticoduodenectomy procedures involved participation of a board‐certified surgeon, whereas the percentages of right hemicolectomy and acute diffuse peritonitis surgeries with participation of a board‐certified surgeon were 76.4% and 69.0% in 2017, respectively (Table 14).
Table 13.
Changes in the annual percentage of surgeries by gender and age group for the eight main operative procedures
| Procedure | Year | No. of surgeries | Percentage by gender | Percentage according to age group (y) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | <60 | 60 to <65 | 65 to <70 | 70 to <75 | 75 to <80 | ≥80 | |||
| Esophagectomy | 2011 | 4916 | 84.1 | 15.9 | 20.4 | 20.8 | 22.5 | 19.4 | 12.2 | 4.7 |
| 2012 | 5946 | 84.4 | 15.6 | 19.7 | 21.3 | 20.7 | 20.3 | 13.1 | 4.9 | |
| 2013 | 5694 | 83.6 | 16.4 | 18.3 | 18.3 | 22.6 | 21.3 | 13.8 | 5.8 | |
| 2014 | 6091 | 84.0 | 16.0 | 18.7 | 17.8 | 22.8 | 22.0 | 13.4 | 5.2 | |
| 2015 | 6060 | 82.9 | 17.1 | 17.9 | 16.3 | 23.6 | 23.5 | 13.1 | 5.7 | |
| 2016 | 6041 | 81.7 | 18.3 | 17.8 | 15.8 | 25.3 | 21.6 | 14.3 | 5.2 | |
| 2017 | 6100 | 82.3 | 17.7 | 17.0 | 14.6 | 25.6 | 20.6 | 15.8 | 6.3 | |
| Gastrectomy (distal) | 2011 | 34 160 | 66.6 | 33.4 | 18.1 | 15.0 | 14.2 | 17.4 | 16.8 | 18.5 |
| 2012 | 38 750 | 66.9 | 33.1 | 16.9 | 14.8 | 15.0 | 17.8 | 16.5 | 18.8 | |
| 2013 | 39 957 | 66.7 | 33.3 | 16.3 | 13.5 | 15.8 | 17.8 | 17.6 | 19.0 | |
| 2014 | 38 584 | 66.4 | 33.6 | 15.7 | 12.4 | 16.6 | 18.4 | 17.3 | 19.5 | |
| 2015 | 37 819 | 66.6 | 33.4 | 14.8 | 11.3 | 17.5 | 18.2 | 17.5 | 20.6 | |
| 2016 | 36 852 | 66.6 | 33.4 | 14.5 | 10.4 | 18.5 | 17.6 | 17.4 | 21.6 | |
| 2017 | 35 517 | 66.8 | 33.2 | 13.4 | 9.9 | 18.0 | 18.1 | 18.0 | 22.6 | |
| Total gastrectomy | 2011 | 18 652 | 73.7 | 26.3 | 16.6 | 14.7 | 16.0 | 19.7 | 18.0 | 15.0 |
| 2012 | 21 122 | 74.2 | 25.8 | 15.5 | 14.8 | 15.7 | 19.2 | 18.5 | 16.3 | |
| 2013 | 19 035 | 74.0 | 26.0 | 14.7 | 13.5 | 16.9 | 19.4 | 19.2 | 16.3 | |
| 2014 | 19 071 | 73.7 | 26.3 | 14.0 | 12.3 | 17.2 | 20.1 | 18.9 | 17.5 | |
| 2015 | 18 695 | 74.5 | 25.5 | 13.7 | 11.1 | 18.9 | 20.8 | 18.2 | 17.4 | |
| 2016 | 17 670 | 74.4 | 25.6 | 12.6 | 10.3 | 19.6 | 19.5 | 19.0 | 19.0 | |
| 2017 | 14 840 | 74.2 | 25.8 | 12.2 | 9.9 | 19.0 | 19.6 | 19.8 | 19.5 | |
| Right hemicolectomy | 2011 | 17 890 | 50.5 | 49.5 | 12.8 | 11.6 | 13.1 | 17.3 | 18.8 | 26.5 |
| 2012 | 21 034 | 50.3 | 49.7 | 13.1 | 10.9 | 13.1 | 17.0 | 19.0 | 26.9 | |
| 2013 | 21 814 | 50.6 | 49.4 | 13.0 | 10.0 | 13.4 | 17.6 | 18.9 | 27.1 | |
| 2014 | 22 446 | 50.6 | 49.4 | 12.0 | 9.2 | 13.8 | 18.2 | 18.6 | 28.2 | |
| 2015 | 22 850 | 50.5 | 49.5 | 11.5 | 8.6 | 14.6 | 18.1 | 18.1 | 29.1 | |
| 2016 | 22 829 | 51.3 | 48.7 | 11.4 | 7.7 | 15.9 | 16.7 | 18.5 | 29.8 | |
| 2017 | 22 543 | 50.9 | 49.1 | 11.3 | 7.4 | 14.9 | 16.3 | 19.3 | 30.8 | |
| Low anterior resection | 2011 | 16 984 | 64.8 | 35.2 | 24.1 | 18.5 | 16.5 | 16.2 | 12.9 | 11.7 |
| 2012 | 20 321 | 64.8 | 35.2 | 24.2 | 17.6 | 16.5 | 16.6 | 13.1 | 12.0 | |
| 2013 | 21 096 | 64.2 | 35.8 | 23.8 | 16.5 | 17.4 | 16.9 | 13.5 | 11.8 | |
| 2014 | 21 861 | 64.8 | 35.2 | 23.1 | 15.7 | 18.3 | 17.9 | 13.1 | 11.9 | |
| 2015 | 22 493 | 64.4 | 35.6 | 23.5 | 14.2 | 19.6 | 17.1 | 13.6 | 12.0 | |
| 2016 | 21 387 | 64.4 | 35.6 | 23.4 | 13.6 | 20.7 | 16.8 | 13.2 | 12.2 | |
| 2017 | 20 879 | 64.2 | 35.8 | 23.2 | 12.6 | 20.9 | 16.7 | 13.5 | 13.2 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7434 | 70.4 | 29.6 | 20.1 | 16.4 | 16.5 | 20.4 | 18.0 | 8.7 |
| 2012 | 8239 | 69.5 | 30.5 | 19.8 | 16.1 | 17.4 | 19.5 | 18.5 | 8.8 | |
| 2013 | 7937 | 69.4 | 30.6 | 19.4 | 14.2 | 18.0 | 20.3 | 18.2 | 9.9 | |
| 2014 | 7666 | 69.2 | 30.8 | 18.5 | 13.8 | 18.5 | 21.5 | 17.6 | 10.0 | |
| 2015 | 7439 | 68.9 | 31.1 | 18.7 | 12.5 | 19.3 | 20.9 | 17.6 | 11.1 | |
| 2016 | 7610 | 68.7 | 31.3 | 18.0 | 11.9 | 21.1 | 20.4 | 17.5 | 11.1 | |
| 2017 | 7698 | 69.5 | 30.5 | 17.2 | 11.3 | 20.5 | 20.4 | 18.7 | 11.9 | |
| Pancreaticoduodenectomy | 2011 | 8305 | 61.9 | 38.1 | 16.1 | 16.0 | 17.3 | 20.9 | 18.8 | 10.9 |
| 2012 | 9329 | 62.0 | 38.0 | 14.7 | 15.8 | 18.0 | 20.6 | 20.2 | 10.6 | |
| 2013 | 10 068 | 60.9 | 39.1 | 14.0 | 12.6 | 19.6 | 22.5 | 19.4 | 11.8 | |
| 2014 | 10 400 | 59.5 | 40.5 | 18.4 | 12.4 | 19.0 | 21.0 | 18.2 | 11.1 | |
| 2015 | 10 576 | 60.7 | 39.3 | 14.2 | 11.7 | 20.0 | 22.9 | 19.3 | 12.0 | |
| 2016 | 11 028 | 61.1 | 38.9 | 14.2 | 10.3 | 20.6 | 21.8 | 20.3 | 12.7 | |
| 2017 | 11 580 | 61.1 | 38.9 | 13.8 | 9.8 | 20.4 | 20.8 | 21.6 | 13.6 | |
| Acute diffuse peritonitis surgery | 2011 | 7753 | 60.0 | 40.0 | 31.4 | 11.2 | 9.7 | 11.7 | 13.2 | 22.9 |
| 2012 | 9177 | 61.0 | 39.0 | 30.3 | 11.2 | 10.1 | 11.6 | 13.4 | 23.4 | |
| 2013 | 10 447 | 60.1 | 39.9 | 29.1 | 10.3 | 11.5 | 11.8 | 13.1 | 24.1 | |
| 2014 | 12 085 | 61.2 | 38.8 | 28.4 | 9.5 | 12.2 | 12.3 | 12.9 | 24.7 | |
| 2015 | 13 030 | 59.4 | 40.6 | 28.2 | 8.9 | 12.5 | 13.1 | 12.3 | 25.0 | |
| 2016 | 13 981 | 60.2 | 39.8 | 27.4 | 8.6 | 13.4 | 12.4 | 12.3 | 26.0 | |
| 2017 | 14 423 | 59.4 | 40.6 | 26.5 | 7.8 | 13.0 | 12.0 | 13.6 | 27.1 | |
Table 14.
Institution type, anesthesiologist and specialist participation rates in the eight main operative procedures
| Procedure | Year | No. of surgeries | Percentage by institution type | Anesthesiologist participation (%) | Board‐certified surgeon participation (%) | Medical practitioners (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| Certified institution | Related institution | Other | Board‐certified surgeons | Non‐board‐certified surgeons | |||||
| Esophagectomy | 2011 | 4916 | 94.2 | 5.3 | 0.5 | 97.6 | 88.4 | 63.5 | 36.5 |
| 2012 | 5946 | 78.3 | 4.9 | 16.8 | 98.1 | 89.0 | 64.8 | 35.2 | |
| 2013 | 5694 | 92.9 | 5.9 | 1.2 | 98.0 | 90.8 | 66.6 | 33.4 | |
| 2014 | 6091 | 93.6 | 4.7 | 1.7 | 98.6 | 92.6 | 70.2 | 29.8 | |
| 2015 | 6060 | 93.6 | 4.6 | 1.8 | 98.5 | 93.5 | 72.1 | 27.9 | |
| 2016 | 6041 | 94.5 | 3.8 | 1.7 | 98.8 | 93.7 | 73.2 | 26.8 | |
| 2017 | 6100 | 95.3 | 3.1 | 1.7 | 98.8 | 94.8 | 74.7 | 25.3 | |
| Gastrectomy (distal) | 2011 | 34 160 | 81.1 | 16.6 | 2.3 | 93.2 | 71.3 | 37.0 | 63.0 |
| 2012 | 38 750 | 64.5 | 15.2 | 20.3 | 93.9 | 72.5 | 37.9 | 62.1 | |
| 2013 | 39 957 | 76.6 | 19.2 | 4.1 | 93.6 | 76.1 | 40.6 | 59.4 | |
| 2014 | 38 584 | 77.7 | 17.8 | 4.5 | 94.0 | 78.4 | 42.1 | 57.9 | |
| 2015 | 37 819 | 77.3 | 18.3 | 4.4 | 94.1 | 78.1 | 41.3 | 58.7 | |
| 2016 | 36 852 | 80.2 | 15.9 | 4.0 | 95.0 | 81.8 | 43.8 | 56.2 | |
| 2017 | 35 517 | 80.2 | 14.9 | 4.8 | 95.4 | 82.4 | 45.2 | 54.8 | |
| Total gastrectomy | 2011 | 18 652 | 80.9 | 16.8 | 2.3 | 93.9 | 71.6 | 37.4 | 62.6 |
| 2012 | 21 122 | 63.0 | 15.3 | 21.7 | 94.3 | 72.1 | 38.0 | 62.0 | |
| 2013 | 19 035 | 77.2 | 18.9 | 3.9 | 94.2 | 75.0 | 39.5 | 60.5 | |
| 2014 | 19 071 | 77.8 | 17.9 | 4.3 | 94.4 | 77.7 | 41.7 | 58.3 | |
| 2015 | 18 695 | 77.9 | 17.9 | 4.1 | 94.5 | 78.2 | 42.6 | 57.4 | |
| 2016 | 17 670 | 80.0 | 15.9 | 4.0 | 95.0 | 81.4 | 45.0 | 55.0 | |
| 2017 | 14 840 | 79.3 | 15.8 | 4.9 | 95.0 | 80.7 | 44.3 | 55.7 | |
| Right hemicolectomy | 2011 | 17 890 | 75.7 | 21.2 | 3.1 | 92.7 | 66.0 | 30.5 | 69.5 |
| 2012 | 21 034 | 60.0 | 18.3 | 21.7 | 93.0 | 67.1 | 30.8 | 69.2 | |
| 2013 | 21 814 | 72.1 | 22.3 | 5.6 | 92.9 | 69.7 | 32.6 | 67.4 | |
| 2014 | 22 446 | 71.2 | 23.1 | 5.7 | 93.4 | 71.9 | 33.6 | 66.4 | |
| 2015 | 22 850 | 72.1 | 22.0 | 5.9 | 94.1 | 72.4 | 33.5 | 66.5 | |
| 2016 | 22 829 | 73.8 | 20.1 | 6.1 | 94.5 | 74.2 | 34.3 | 65.7 | |
| 2017 | 22 543 | 75.0 | 18.4 | 6.6 | 94.7 | 76.4 | 37.1 | 62.9 | |
| Low anterior resection | 2011 | 16 984 | 79.4 | 17.7 | 2.9 | 93.4 | 72.7 | 41.6 | 58.4 |
| 2012 | 20 321 | 64.0 | 16.2 | 19.7 | 93.8 | 73.0 | 42.3 | 57.7 | |
| 2013 | 21 096 | 76.3 | 19.5 | 4.2 | 93.7 | 75.5 | 44.3 | 55.7 | |
| 2014 | 21 861 | 76.2 | 19.0 | 4.9 | 94.4 | 78.2 | 47.2 | 52.8 | |
| 2015 | 22 493 | 76.9 | 18.3 | 4.8 | 94.6 | 79.2 | 47.7 | 52.3 | |
| 2016 | 21 387 | 79.0 | 16.4 | 4.7 | 95.0 | 81.0 | 48.8 | 51.2 | |
| 2017 | 20 879 | 79.3 | 15.6 | 5.1 | 95.2 | 83.1 | 51.2 | 48.8 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7434 | 91.1 | 8.0 | 0.8 | 96.4 | 88.9 | 61.5 | 38.5 |
| 2012 | 8239 | 75.9 | 7.9 | 16.3 | 96.8 | 89.3 | 64.0 | 36.0 | |
| 2013 | 7937 | 88.1 | 9.7 | 2.2 | 96.9 | 91.0 | 65.2 | 34.8 | |
| 2014 | 7666 | 88.2 | 8.7 | 3.1 | 96.7 | 92.3 | 66.6 | 33.4 | |
| 2015 | 7439 | 89.2 | 8.6 | 2.2 | 97.2 | 92.3 | 66.6 | 33.4 | |
| 2016 | 7610 | 90.7 | 7.1 | 2.1 | 97.1 | 93.3 | 67.7 | 32.3 | |
| 2017 | 7698 | 91.2 | 6.6 | 2.2 | 97.7 | 95.1 | 72.3 | 27.7 | |
| Pancreaticoduodenectomy | 2011 | 8305 | 87.8 | 11.0 | 1.2 | 95.9 | 85.7 | 58.7 | 41.3 |
| 2012 | 9329 | 72.4 | 8.8 | 18.8 | 96.6 | 87.2 | 60.9 | 39.1 | |
| 2013 | 10 068 | 85.9 | 11.7 | 2.4 | 96.0 | 87.9 | 60.5 | 39.5 | |
| 2014 | 10 400 | 86.4 | 10.4 | 3.3 | 96.4 | 90.3 | 62.2 | 37.8 | |
| 2015 | 10 576 | 88.5 | 9.2 | 2.4 | 96.9 | 90.9 | 62.1 | 37.9 | |
| 2016 | 11 028 | 89.4 | 8.3 | 2.3 | 97.1 | 91.7 | 63.3 | 36.7 | |
| 2017 | 11 580 | 90.5 | 7.2 | 2.3 | 97.3 | 93.0 | 65.0 | 35.0 | |
| Acute diffuse peritonitis surgery | 2011 | 7753 | 80.6 | 16.9 | 2.4 | 90.0 | 58.5 | 23.5 | 76.5 |
| 2012 | 9177 | 65.2 | 16.4 | 18.4 | 90.4 | 59.4 | 22.7 | 77.3 | |
| 2013 | 10 447 | 77.7 | 18.1 | 4.2 | 91.2 | 62.4 | 23.9 | 76.1 | |
| 2014 | 12 085 | 77.7 | 17.2 | 5.1 | 91.9 | 63.3 | 25.1 | 74.9 | |
| 2015 | 13 030 | 79.8 | 15.9 | 4.3 | 92.2 | 64.5 | 24.9 | 75.1 | |
| 2016 | 13 981 | 82.2 | 13.8 | 4.0 | 93.0 | 66.8 | 26.1 | 73.9 | |
| 2017 | 14 423 | 83.1 | 13.0 | 3.8 | 93.3 | 69.0 | 27.2 | 72.8 | |
The rate of preoperative chemotherapy within 90 days increased over time and was 50.9% for esophagectomy in 2017. Although the rates of preoperative chemotherapy in patients who underwent total gastrectomy, low anterior resection, or pancreaticoduodenectomy were relatively low (<10%), the rates of preoperative chemotherapy in patients who underwent these procedures showed an increasing trend over time (Table 15).
Table 15.
Changes in the annual number of surgeries in patients who received preoperative chemotherapy or radiation prior to the eight main operative procedures
| Year | No. of surgeries | No. with preoperative chemotherapy within 30 d/rate (%) | No. with preoperative chemotherapy within 90 d/rate (%) | No. with preoperative radiotherapy within 90 d/rate (%) | |
|---|---|---|---|---|---|
| Esophagectomy | 2011 | 4914 | 928/18.9 | –/– | 235/4.8 |
| 2012 | 5947 | 1131/19.0 | 2476/41.6 | 432/7.3 | |
| 2013 | 5694 | 982/17.2 | 2386/41.9 | 374/6.6 | |
| 2014 | 6092 | 1145/18.8 | 2733/44.9 | 435/7.1 | |
| 2015 | 6058 | 1153/19.0 | 2842/46.9 | 416/6.9 | |
| 2016 | 6041 | 1150/19.0 | 2955/48.9 | 398/6.6 | |
| 2017 | 6100 | 1103/18.1 | 3103/50.9 | 400/6.6 | |
| Gastrectomy (distal) | 2011 | 32 241 | 469/1.5 | –/– | 47/0.1 |
| 2012 | 36 715 | 502/1.4 | 902/2.5 | 45/0.1 | |
| 2013 | 39 094 | 516/1.3 | 1028/2.6 | 51/0.1 | |
| 2014 | 37 718 | 479/1.3 | 1002/2.7 | 36/0.1 | |
| 2015 | 37 082 | 492/1.3 | 990/2.7 | 50/0.1 | |
| 2016 | 36 197 | 481/1.3 | 1070/3.0 | 36/0.1 | |
| 2017 | 34 861 | 462/1.3 | 1073/3.1 | 46/0.1 | |
| Total gastrectomy | 2011 | 18 046 | 814/4.5 | –/– | 33/0.2 |
| 2012 | 20 467 | 835/4.1 | 1540/7.5 | 31/0.2 | |
| 2013 | 18 777 | 656/3.5 | 1364/7.3 | 48/0.3 | |
| 2014 | 17 962 | 713/4.0 | 1002/5.6 | 48/0.3 | |
| 2015 | 17 385 | 638/3.7 | 1452/8.4 | 38/0.2 | |
| 2016 | 16 188 | 583/3.6 | 1366/8.4 | 34/0.2 | |
| 2017 | 14 840 | 566/3.8 | 1385/9.3 | 28/0.2 | |
| Right hemicolectomy | 2011 | 17 884 | 157/0.9 | –/– | 24/0.1 |
| 2012 | 21 027 | 184/0.9 | 317/1.5 | 32/0.2 | |
| 2013 | 21 816 | 187/0.9 | 363/1.7 | 0.1 | |
| 2014 | 22 444 | 192/0.9 | 370/1.6 | 29/0.1 | |
| 2015 | 22 851 | 204/0.9 | 409/1.8 | 53/0.2 | |
| 2016 | 22 829 | 256/1.1 | 438/1.9 | 56/0.2 | |
| 2017 | 22 543 | 192/0.9 | 416/1.8 | 46/0.2 | |
| Low anterior resection | 2011 | 16 982 | 355/2.1 | –/– | 293/1.7 |
| 2012 | 20 319 | 481/2.4 | 1131/5.6 | 484/2.4 | |
| 2013 | 21 097 | 477/2.3 | 1273/6.0 | 523/2.5 | |
| 2014 | 21 854 | 531/2.4 | 1533/7.0 | 641/2.9 | |
| 2015 | 22 496 | 565/2.5 | 1721/7.7 | 599/2.7 | |
| 2016 | 21 387 | 507/2.4 | 1682/7.9 | 627/2.9 | |
| 2017 | 20 879 | 526/2.5 | 1759/8.4 | 665/3.2 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7439 | 420/5.6 | –/– | 31/0.4 |
| 2012 | 8242 | 508/6.2 | 1290/15.7 | 38/0.5 | |
| 2013 | 7937 | 454/5.7 | 1293/16.3 | 36/0.5 | |
| 2014 | 7663 | 419/5.5 | 1170/15.3 | 32/0.4 | |
| 2015 | 7439 | 358/4.8 | 1152/15.5 | 25/0.3 | |
| 2016 | 7610 | 350/4.6 | 1121/14.7 | 46/0.6 | |
| 2017 | 7698 | 326/4.2 | 1137/14.8 | 64/0.8 | |
| Pancreaticoduodenectomy | 2011 | 8306 | 227/2.7 | –/– | 88/1.1 |
| 2012 | 9336 | 229/2.5 | 440/4.7 | 155/1.7 | |
| 2013 | 10 069 | 291/2.9 | 584/5.8 | 213/2.1 | |
| 2014 | 10 395 | 304/2.9 | 631/6.1 | 214/2.1 | |
| 2015 | 10 577 | 339/3.2 | 766/7.2 | 272/2.6 | |
| 2016 | 11 028 | 374/3.4 | 850/7.7 | 268/2.4 | |
| 2017 | 11 580 | 410/3.5 | 907/7.8 | 240/2.1 | |
| Acute diffuse peritonitis surgery | 2011 | 7751 | 277/3.6 | –/– | 47/0.6 |
| 2012 | 9182 | 352/3.8 | 463/5.0 | 61/0.7 | |
| 2013 | 10 452 | 412/3.9 | 573/5.5 | 62/0.6 | |
| 2014 | 12 085 | 396/3.3 | 570/4.7 | 60/0.5 | |
| 2015 | 13 030 | 483/3.7 | 669/5.1 | 76/0.6 | |
| 2016 | 13 981 | 511/3.7 | 732/5.2 | 88/0.6 | |
| 2017 | 14 423 | 553/3.8 | 762/5.3 | 82/0.6 |
‐/‐ indicates lack of data
The number and rate of comorbidities and American Society of Anesthesiologists (ASA) score in patients who underwent the eight main procedures are shown in Table 16. The annual rates of diabetes mellitus and hypertension increased over time for all eight procedures.
Table 16.
Changes in the annual number of surgeries in patients with preoperative comorbidities among patients who underwent the eight main operative procedures
| Year | No. of surgeries | No. with diabetes mellitus/rate (%) | No. with dyspnea within 30 d/rate (%) | No. with COPD/rate (%) | No. with hypertension within 30 d/rate (%) | No. with myocardial infarction within 6 mo/rate (%) | No. receiving dialysis within 14 d/rate (%) | Percentage according to ASA score (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||||||||
| Esophagectomy | 2011 | 4914 | 628/12.8 | 102/2.1 | 302/6.1 | 1531/31.2 | 8/0.2 | 13/0.3 | 39.5 | 52.9 | 7.4 | 0.1 | 0.0 |
| 2012 | 5947 | 773/13.0 | 92/1.5 | 374/6.3 | 1881/31.6 | 22/0.4 | 12/0.2 | 31.8 | 61.0 | 6.8 | 0.2 | 0.2 | |
| 2013 | 5694 | 737/12.9 | 98/1.7 | 360/6.3 | 1944/34.1 | 17/0.3 | 16/0.3 | 29.5 | 62.5 | 7.7 | 0.2 | 0.1 | |
| 2014 | 6092 | 824/13.5 | 100/1.6 | 497/8.2 | 2144/35.2 | 17/0.3 | 8/0.1 | 27.6 | 64.7 | 7.5 | 0.2 | 0.1 | |
| 2015 | 6058 | 895/14.8 | 82/1.4 | 527/8.7 | 2200/36.3 | 13/0.2 | 22/0.4 | 24.3 | 67.6 | 7.8 | 0.2 | 0.1 | |
| 2016 | 6041 | 895/14.8 | 76/1.3 | 501/8.3 | 2233/37.0 | 12/0.2 | 23/0.4 | 19.7 | 71.7 | 8.4 | 0.1 | 0.1 | |
| 2017 | 6100 | 941/15.4 | 72/1.2 | 469/7.7 | 2357/38.6 | 11/0.2 | 20/0.3 | 16.5 | 72.4 | 10.9 | 0.1 | 0.1 | |
| Gastrectomy (distal) | 2011 | 32 250 | 5079/15.7 | 737/2.3 | 1182/3.7 | 11 192/34.7 | 185/0.6 | 271/0.8 | 40.5 | 49.7 | 9.2 | 0.4 | 0.2 |
| 2012 | 36 689 | 6143/16.7 | 772/2.1 | 1316/3.6 | 13 397/36.5 | 249/0.7 | 294/0.8 | 35.2 | 54.0 | 10.1 | 0.5 | 0.2 | |
| 2013 | 39 094 | 6742/17.2 | 740/1.9 | 1639/4.2 | 14 665/37.5 | 211/0.5 | 331/0.8 | 31.7 | 57.1 | 10.6 | 0.4 | 0.2 | |
| 2014 | 37 719 | 6652/17.6 | 702/1.9 | 1754/4.7 | 14 677/38.9 | 161/0.4 | 290/0.8 | 28.7 | 59.8 | 11.0 | 0.4 | 0.1 | |
| 2015 | 37 083 | 6830/18.4 | 649/1.8 | 1833/4.9 | 15 023/40.5 | 174/0.5 | 279/0.8 | 25.7 | 62.2 | 11.7 | 0.4 | 0.1 | |
| 2016 | 36 197 | 6791/18.8 | 627/1.7 | 1890/5.2 | 14 910/41.2 | 175/0.5 | 295/0.8 | 23.1 | 63.9 | 12.4 | 0.4 | 0.1 | |
| 2017 | 34 862 | 6580/18.9 | 563/1.6 | 1693/4.9 | 14 631/42.0 | 159/0.5 | 283/0.8 | 19.9 | 66.4 | 13.2 | 0.4 | 0.1 | |
| Total gastrectomy | 2011 | 18 048 | 2951/16.4 | 448/2.5 | 796/4.4 | 5983/33.2 | 125/0.7 | 95/0.5 | 38.0 | 52.2 | 9.2 | 0.4 | 0.2 |
| 2012 | 20 462 | 3424/16.7 | 482/2.4 | 868/4.2 | 7335/35.8 | 166/0.8 | 125/0.6 | 33.0 | 56.2 | 10.0 | 0.5 | 0.3 | |
| 2013 | 18 775 | 3304/17.6 | 368/2.0 | 880/4.7 | 6999/37.3 | 98/0.5 | 116/0.6 | 28.8 | 59.8 | 10.8 | 0.4 | 0.2 | |
| 2014 | 17 963 | 3332/18.5 | 346/1.9 | 922/5.1 | 6850/38.1 | 81/0.5 | 105/0.6 | 25.6 | 62.4 | 11.4 | 0.4 | 0.1 | |
| 2015 | 17 387 | 3178/18.3 | 341/2.0 | 915/5.3 | 6761/38.9 | 65/0.4 | 109/0.6 | 23.3 | 64.5 | 11.6 | 0.4 | 0.2 | |
| 2016 | 16 191 | 3117/19.3 | 322/2.0 | 917/5.7 | 6535/40.4 | 79/0.5 | 94/0.6 | 20.8 | 65.8 | 12.8 | 0.5 | 0.1 | |
| 2017 | 14 840 | 2875/19.4 | 271/1.8 | 784/5.3 | 6046/40.7 | 71/0.5 | 98/0.7 | 17.4 | 68.7 | 13.2 | 0.5 | 0.1 | |
| Right hemicolectomy | 2011 | 17 885 | 3073/17.2 | 518/2.9 | 526/2.9 | 6495/36.3 | 125/0.7 | 182/1.0 | 31.8 | 53.8 | 13.0 | 1.0 | 0.4 |
| 2012 | 21 022 | 3564/17.0 | 573/2.7 | 586/2.8 | 7830/37.2 | 155/0.7 | 210/1.0 | 29.2 | 56.0 | 13.3 | 1.1 | 0.4 | |
| 2013 | 21 816 | 3802/17.4 | 470/2.2 | 614/2.8 | 8431/38.6 | 112/0.5 | 223/1.0 | 26.4 | 58.3 | 13.8 | 1.0 | 0.4 | |
| 2014 | 22 444 | 4230/18.8 | 514/2.3 | 684/3.0 | 9048/40.3 | 118/0.5 | 226/1.0 | 23.1 | 61.3 | 14.4 | 0.9 | 0.3 | |
| 2015 | 22 851 | 4355/19.1 | 471/2.1 | 705/3.1 | 9419/41.2 | 121/0.5 | 216/0.9 | 21.0 | 62.3 | 15.5 | 0.9 | 0.4 | |
| 2016 | 22 829 | 4484/19.6 | 477/2.1 | 721/3.2 | 9575/41.9 | 88/0.4 | 247/1.1 | 19.0 | 63.3 | 16.4 | 1.0 | 0.3 | |
| 2017 | 22 543 | 4481/19.9 | 447/2.0 | 715/3.2 | 9535/42.3 | 105/0.5 | 274/1.2 | 16.4 | 64.7 | 17.4 | 1.1 | 0.4 | |
| Low anterior resection | 2011 | 16 981 | 2908/17.1 | 259/1.5 | 443/2.6 | 5321/31.3 | 72/0.4 | 80/0.5 | 42.1 | 50.3 | 7.5 | 0.1 | 0.0 |
| 2012 | 20 306 | 3421/16.8 | 300/1.5 | 524/2.6 | 6533/32.2 | 102/0.5 | 102/0.5 | 38.7 | 52.7 | 8.3 | 0.2 | 0.1 | |
| 2013 | 21 097 | 3505/16.6 | 241/1.1 | 597/2.8 | 6965/33.0 | 75/0.4 | 112/0.5 | 35.5 | 55.7 | 8.4 | 0.3 | 0.1 | |
| 2014 | 21 854 | 3836/17.6 | 277/1.3 | 851/3.9 | 7634/34.9 | 90/0.4 | 105/0.5 | 32.1 | 58.7 | 8.9 | 0.2 | 0.1 | |
| 2015 | 22 496 | 4013/17.8 | 263/1.2 | 755/3.4 | 7917/35.2 | 101/0.4 | 116/0.5 | 29.9 | 60.8 | 8.9 | 0.2 | 0.1 | |
| 2016 | 21 387 | 3855/18.0 | 221/1.0 | 797/3.7 | 7693/36.0 | 68/0.3 | 104/0.5 | 27.5 | 62.5 | 9.7 | 0.2 | 0.1 | |
| 2017 | 20 879 | 3885/18.6 | 236/1.1 | 720/3.4 | 7512/36.0 | 67/0.3 | 108/0.5 | 24.2 | 65.4 | 10.1 | 0.3 | 0.1 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7439 | 1852/24.9 | 125/1.7 | 202/2.7 | 2728/36.7 | 39/0.5 | 60/0.8 | 33.9 | 55.7 | 9.9 | 0.3 | 0.1 |
| 2012 | 8242 | 2061/25.0 | 100/1.2 | 235/2.9 | 3112/37.8 | 36/0.4 | 63/0.8 | 28.1 | 61.0 | 10.4 | 0.3 | 0.2 | |
| 2013 | 7937 | 1975/24.9 | 79/1.0 | 253/3.2 | 3155/39.8 | 28/0.4 | 71/0.9 | 23.4 | 65.0 | 11.2 | 0.2 | 0.1 | |
| 2014 | 7663 | 1968/25.7 | 100/1.3 | 290/3.8 | 3066/40.0 | 28/0.4 | 55/0.7 | 20.2 | 68.3 | 11.0 | 0.4 | 0.1 | |
| 2015 | 7439 | 1973/26.5 | 90/1.2 | 299/4.0 | 3059/41.1 | 27/0.4 | 71/1.0 | 17.9 | 69.3 | 12.3 | 0.4 | 0.1 | |
| 2016 | 7610 | 2026/26.6 | 78/1.0 | 293/3.9 | 3269/43.0 | 16/0.2 | 66/0.9 | 15.6 | 72.6 | 11.4 | 0.3 | 0.1 | |
| 2017 | 7698 | 2153/28.0 | 79/1.0 | 308/4.0 | 3418/44.4 | 20/0.3 | 67/0.9 | 13.7 | 73.2 | 12.9 | 0.1 | 0.1 | |
| Pancreaticoduodenectomy | 2011 | 8306 | 2280/27.5 | 95/1.1 | 227/2.7 | 2819/33.9 | 36/0.4 | 50/0.6 | 34.3 | 56.5 | 8.9 | 0.2 | 0.2 |
| 2012 | 9331 | 2660/28.5 | 113/1.2 | 247/2.6 | 3297/35.3 | 38/0.4 | 49/0.5 | 28.1 | 62.3 | 9.2 | 0.3 | 0.1 | |
| 2013 | 10 069 | 2830/28.1 | 84/0.8 | 269/2.7 | 3729/37.0 | 45/0.4 | 60/0.6 | 24.9 | 64.4 | 10.4 | 0.2 | 0.1 | |
| 2014 | 10 395 | 3011/29.0 | 88/0.8 | 362/3.5 | 3973/38.2 | 34/0.3 | 58/0.6 | 22.6 | 66.2 | 10.9 | 0.2 | 0.0 | |
| 2015 | 10 577 | 3057/28.9 | 92/0.9 | 385/3.6 | 4150/39.2 | 36/0.3 | 48/0.5 | 19.1 | 69.3 | 11.3 | 0.2 | 0.1 | |
| 2016 | 11 028 | 3321/30.1 | 112/1.0 | 443/4.0 | 4380/39.7 | 31/0.3 | 62/0.6 | 16.7 | 70.3 | 12.6 | 0.2 | 0.1 | |
| 2017 | 11 580 | 3517/30.4 | 97/0.8 | 416/3.6 | 4712/40.7 | 36/0.3 | 66/0.6 | 14.6 | 72.8 | 12.4 | 0.1 | 0.1 | |
| Acute diffuse peritonitis surgery | 2011 | 7751 | 1063/13.7 | 655/8.5 | 264/3.4 | 2252/29.1 | 49/0.6 | 306/3.9 | 20.7 | 35.3 | 29.0 | 9.9 | 5.1 |
| 2012 | 9179 | 1253/13.7 | 737/8.0 | 300/3.3 | 2799/30.5 | 70/0.8 | 341/3.7 | 19.3 | 36.6 | 30.2 | 9.6 | 4.3 | |
| 2013 | 10 452 | 1422/13.6 | 731/7.0 | 348/3.3 | 3306/31.6 | 63/0.6 | 411/3.9 | 17.3 | 36.5 | 33.7 | 8.8 | 3.7 | |
| 2014 | 12 085 | 1745/14.4 | 758/6.3 | 416/3.4 | 3913/32.4 | 65/0.5 | 444/3.7 | 16.0 | 37.6 | 34.4 | 9.2 | 2.8 | |
| 2015 | 13 030 | 1862/14.3 | 732/5.6 | 366/2.8 | 4338/33.3 | 62/0.5 | 466/3.6 | 13.9 | 40.4 | 33.9 | 9.0 | 2.8 | |
| 2016 | 13 981 | 2113/15.1 | 765/5.5 | 441/3.2 | 4811/34.4 | 79/0.6 | 517/3.7 | 13.2 | 40.0 | 34.5 | 9.7 | 2.7 | |
| 2017 | 14 423 | 2259/15.7 | 724/5.0 | 386/2.7 | 5118/35.5 | 63/0.4 | 496/3.4 | 11.4 | 40.6 | 36.3 | 9.2 | 2.5 | |
Abbreviations: ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease.
Table 17 and Figure 2 show the morbidity and mortality rates of the eight main operative procedures. Other than for acute diffuse peritonitis surgery, the operative mortality rates for the procedures were 0.6%‐4.1%, and the postoperative 30‐day mortality rates were 0.3%‐2.1%. The operative mortality rate and the 30‐day postoperative mortality rate for acute diffuse peritonitis surgery were 10.9% and 8.0% in 2017, respectively. The annual numbers of cases of gastrectomy and total gastrectomy have been decreasing, and those of pancreaticoduodenectomy and acute diffuse peritonitis surgery have been increasing over time. Although there were differences in the incidences of complications and mortality according to the procedure, the annual postoperative complication rate of the eight main procedures generally increased and operative mortality rate generally decreased over time.
Table 17.
Annual number of surgeries and mortality rates among patients who underwent the eight main operative procedures
| Procedure | Year | No. of surgeries | No. of postoperative complicationsa/rate (%) | No. of reoperations/rate (%) | No. of postoperative | No. of postoperative |
|---|---|---|---|---|---|---|
| 30‐d mortalities/rate (%) | 90‐d mortalities/rate (%) | |||||
| Esophagectomy | 2011 | 4916 | 879/17.9 | 310/6.3 | 55/1.1 | 158/3.2 |
| 2012 | 5946 | 1135/19.1 | 345/5.8 | 63/1.1 | 183/3.1 | |
| 2013 | 5694 | 1067/18.7 | 375/6.6 | 67/1.2 | 161/2.8 | |
| 2014 | 6091 | 1178/19.3 | 367/6.0 | 49/0.8 | 140/2.3 | |
| 2015 | 6060 | 1171/19.3 | 392/6.5 | 57/0.9 | 166/2.7 | |
| 2016 | 6041 | 1240/20.5 | 357/5.9 | 49/0.8 | 109/1.8 | |
| 2017 | 6100 | 1374/22.5 | 355/5.8 | 61/1.0 | 108/1.8 | |
| Gastrectomy (distal) | 2011 | 34 160 | 1774/5.2 | 709/2.1 | 208/0.6 | 451/1.3 |
| 2012 | 38 750 | 2205/5.7 | 849/2.2 | 232/0.6 | 516/1.3 | |
| 2013 | 39 957 | 2450/6.1 | 892/2.2 | 239/0.6 | 542/1.4 | |
| 2014 | 38 584 | 2356/6.1 | 941/2.4 | 264/0.7 | 523/1.4 | |
| 2015 | 37 819 | 2325/6.1 | 851/2.3 | 222/0.6 | 452/1.2 | |
| 2016 | 36 852 | 2314/6.3 | 825/2.2 | 249/0.7 | 473/1.3 | |
| 2017 | 35 517 | 2445/6.9 | 859/2.4 | 253/0.7 | 437/1.2 | |
| Total gastrectomy | 2011 | 18 652 | 1716/9.2 | 634/3.4 | 177/0.9 | 427/2.3 |
| 2012 | 21 122 | 2135/10.1 | 758/3.6 | 224/1.1 | 503/2.4 | |
| 2013 | 19 035 | 1831/9.6 | 642/3.4 | 169/0.9 | 428/2.2 | |
| 2014 | 19 071 | 1840/9.6 | 698/3.7 | 185/1.0 | 379/2.0 | |
| 2015 | 18 695 | 1907/10.2 | 654/3.5 | 178/1.0 | 387/2.1 | |
| 2016 | 17 670 | 1835/10.4 | 638/3.6 | 174/1.0 | 336/1.9 | |
| 2017 | 14 840 | 1702/11.5 | 514/3.5 | 161/1.1 | 293/2.0 | |
| Right hemicolectomy | 2011 | 17 890 | 1150/6.4 | 588/3.3 | 213/1.2 | 410/2.3 |
| 2012 | 21 034 | 1470/7.0 | 677/3.2 | 263/1.3 | 471/2.2 | |
| 2013 | 21 814 | 1527/7.0 | 721/3.3 | 280/1.3 | 538/2.5 | |
| 2014 | 22 446 | 1544/6.9 | 771/3.4 | 287/1.3 | 530/2.4 | |
| 2015 | 22 850 | 1607/7.0 | 769/3.4 | 301/1.3 | 534/2.3 | |
| 2016 | 22 829 | 1510/6.6 | 791/3.5 | 253/1.1 | 449/2.0 | |
| 2017 | 22 543 | 1648/7.3 | 785/3.5 | 296/1.3 | 450/2.0 | |
| Low anterior resection | 2011 | 16 984 | 1616/9.5 | 1213/7.1 | 75/0.4 | 136/0.8 |
| 2012 | 20 321 | 2092/10.3 | 1413/6.9 | 88/0.4 | 149/0.7 | |
| 2013 | 21 096 | 2059/9.8 | 1473/7.0 | 80/0.4 | 175/0.8 | |
| 2014 | 21 861 | 2098/9.6 | 1546/7.1 | 70/0.3 | 152/0.7 | |
| 2015 | 22 493 | 2210/9.8 | 1550/6.9 | 95/0.4 | 156/0.7 | |
| 2016 | 21 387 | 2306/10.8 | 1492/7.0 | 68/0.3 | 126/0.6 | |
| 2017 | 20 879 | 2376/11.4 | 1330/6.4 | 96/0.5 | 148/0.7 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7434 | 886/11.9 | 203/2.7 | 155/2.1 | 303/4.1 |
| 2012 | 8239 | 1146/13.9 | 248/3.0 | 142/1.7 | 293/3.6 | |
| 2013 | 7937 | 1135/14.3 | 226/2.8 | 130/1.6 | 290/3.7 | |
| 2014 | 7666 | 1052/13.7 | 242/3.2 | 94/1.2 | 208/2.7 | |
| 2015 | 7439 | 1049/14.1 | 213/2.9 | 87/1.2 | 182/2.4 | |
| 2016 | 7610 | 1046/13.7 | 220/2.9 | 96/1.3 | 178/2.3 | |
| 2017 | 7698 | 1160/15.1 | 221/2.9 | 97/1.3 | 169/2.2 | |
| Pancreaticoduodenectomy | 2011 | 8305 | 1285/15.5 | 299/3.6 | 97/1.2 | 238/2.9 |
| 2012 | 9329 | 1654/17.7 | 365/3.9 | 137/1.5 | 281/3.0 | |
| 2013 | 10 068 | 1853/18.4 | 407/4.0 | 142/1.4 | 307/3.0 | |
| 2014 | 10 400 | 1847/17.8 | 374/3.6 | 111/1.1 | 267/2.6 | |
| 2015 | 10 576 | 2025/19.1 | 378/3.6 | 120/1.1 | 247/2.3 | |
| 2016 | 11 028 | 2242/20.3 | 393/3.6 | 98/0.9 | 232/2.1 | |
| 2017 | 11 580 | 2539/21.9 | 413/3.6 | 145/1.3 | 232/2.0 | |
| Acute diffuse peritonitis surgery | 2011 | 7753 | 2022/26.1 | 634/8.2 | 697/9.0 | 1096/14.1 |
| 2012 | 9177 | 2456/26.8 | 685/7.5 | 785/8.6 | 1289/14.0 | |
| 2013 | 10 447 | 2652/25.4 | 786/7.5 | 861/8.2 | 1408/13.5 | |
| 2014 | 12 085 | 2966/24.5 | 937/7.8 | 927/7.7 | 1472/12.2 | |
| 2015 | 13 030 | 3126/24.0 | 1051/8.1 | 943/7.2 | 1551/11.9 | |
| 2016 | 13 981 | 3445/24.6 | 1068/7.6 | 1052/7.5 | 1572/11.2 | |
| 2017 | 14 423 | 3756/26.0 | 1125/7.8 | 1152/8.0 | 1575/10.9 |
Complications with Clavien‐Dindo grades IIIa to V are shown.
Figure 2.
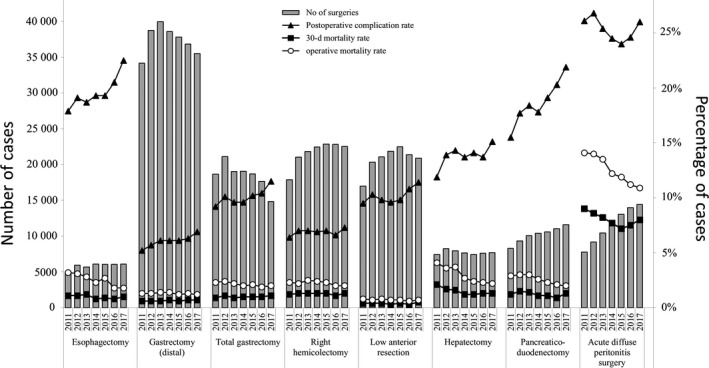
Annual changes in the number of surgeries, postoperative complication rate, operative mortality rate, and 30‐d postoperative mortality rate: analysis of the eight major surgical procedures. Postoperative complication rate: the rate of complications with Clavien‐Dindo (C‐D) classification of grade III or higher
The increase in the incidence of endoscopic surgery over time is shown in Figure 3 and Table 18. The annual percentage of surgeries carried out by endoscopic surgery is greatly increasing in low anterior resection and esophagectomy over time. In contrast, laparoscopic hepatectomy and pancreaticoduodenectomy have been carried out in a limited number of institutions.
Figure 3.
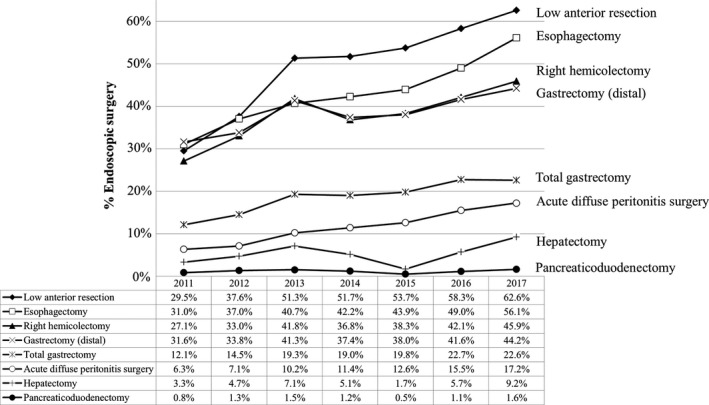
Annual changes in the percentage of surgeries carried out by endoscopic surgery: analysis of the eight major surgical procedures
Table 18.
Changes in the annual percentage of surgeries carried out by endoscopic surgery for the eight main operative procedures
| Procedure | Year | No. of surgeries | Endoscopic surgery | % Endoscopic surgery |
|---|---|---|---|---|
| Esophagectomy | 2011 | 4917 | 1525 | 31.0 |
| 2012 | 5948 | 2200 | 37.0 | |
| 2013 | 5694 | 2315 | 40.7 | |
| 2014 | 6091 | 2569 | 42.2 | |
| 2015 | 6060 | 2659 | 43.9 | |
| 2016 | 6041 | 2961 | 49.0 | |
| 2017 | 6100 | 3424 | 56.1 | |
| Gastrectomy (distal) | 2011 | 34 198 | 10 801 | 31.6 |
| 2012 | 38 774 | 13 098 | 33.8 | |
| 2013 | 39 959 | 16 507 | 41.3 | |
| 2014 | 38 584 | 14 432 | 37.4 | |
| 2015 | 37 819 | 14 357 | 38.0 | |
| 2016 | 36 852 | 15 333 | 41.6 | |
| 2017 | 35 517 | 15 696 | 44.2 | |
| Total gastrectomy | 2011 | 18 674 | 2258 | 12.1 |
| 2012 | 21 139 | 3060 | 14.5 | |
| 2013 | 19 038 | 3669 | 19.3 | |
| 2014 | 19 071 | 3620 | 19.0 | |
| 2015 | 18 695 | 3707 | 19.8 | |
| 2016 | 17 670 | 4007 | 22.7 | |
| 2017 | 14 840 | 3347 | 22.6 | |
| Right hemicolectomy | 2011 | 17 899 | 4842 | 27.1 |
| 2012 | 21 047 | 6954 | 33.0 | |
| 2013 | 21 816 | 9124 | 41.8 | |
| 2014 | 22 446 | 8269 | 36.8 | |
| 2015 | 22 850 | 8755 | 38.3 | |
| 2016 | 22 829 | 9622 | 42.1 | |
| 2017 | 22 543 | 10 341 | 45.9 | |
| Low anterior resection | 2011 | 16 996 | 5018 | 29.5 |
| 2012 | 20 333 | 7649 | 37.6 | |
| 2013 | 21 098 | 10 814 | 51.3 | |
| 2014 | 21 861 | 11 298 | 51.7 | |
| 2015 | 22 493 | 12 080 | 53.7 | |
| 2016 | 21 387 | 12 478 | 58.3 | |
| 2017 | 20 879 | 13 064 | 62.6 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7440 | 242 | 3.3 |
| 2012 | 8246 | 389 | 4.7 | |
| 2013 | 7938 | 567 | 7.1 | |
| 2014 | 7666 | 392 | 5.1 | |
| 2015 | 7439 | 127 | 1.7 | |
| 2016 | 7610 | 433 | 5.7 | |
| 2017 | 7698 | 712 | 9.2 | |
| Pancreaticoduodenectomy | 2011 | 8310 | 67 | 0.8 |
| 2012 | 9340 | 121 | 1.3 | |
| 2013 | 10 069 | 156 | 1.5 | |
| 2014 | 10 400 | 124 | 1.2 | |
| 2015 | 10 576 | 53 | 0.5 | |
| 2016 | 11 028 | 118 | 1.1 | |
| 2017 | 11 580 | 188 | 1.6 | |
| Acute diffuse peritonitis surgery | 2011 | 7767 | 488 | 6.3 |
| 2012 | 9189 | 652 | 7.1 | |
| 2013 | 10 452 | 1070 | 10.2 | |
| 2014 | 12 085 | 1381 | 11.4 | |
| 2015 | 13 030 | 1638 | 12.6 | |
| 2016 | 13 981 | 2164 | 15.5 | |
| 2017 | 14 423 | 2478 | 17.2 |
4. DISCUSSION
Since the start of NCD registration in 2011, a robust nationwide database has been constructed as a result of the work of data managers and surgeons at the participating hospitals. We can see the real clinical status of surgical outcomes in Japan. The gastroenterological section of the NCD database shows three features: aging of the population, low mortality rate, and increase in endoscopic surgery.
The Japanese Ministry of Internal Affairs and Communications reported that the percentage of senior citizens aged 65 years or over among the Japanese population was 27.7% and the percentage of those aged 75 years or over was 13.8% in 2017, and these are the highest percentages in the world.21 It has been estimated that aging of the population will progress and the percentage aged ≥65 years will increase to a little less than 40% in 2050. Our data showed that 50% of right hemicolectomies and 40% of gastrectomies were carried out in patients aged 75 years or over in 2017. With the increase in the aging population, the annual rates of preoperative comorbidities such as diabetes mellitus and hypertension also increased. Age category was reported as a risk factor for operative mortality in all eight main procedures.2
In spite of the high population of aged patients, the mortality rates for all of the procedures seemed to be acceptable as a nationwide outcome, as they are satisfactorily lower than those reported from other countries.22, 23 These results may be explained by the high participation rate of board‐certified surgeons in gastroenterological surgeries (BCS‐Gs). The association between the participation of BCS‐Gs and mortality was evaluated using 250 012 surgical cases registered in 2011 and 2012. The participation of BCS‐Gs contributed to favorable outcomes especially for distal gastrectomy and pancreaticoduodenectomy.19 From 2011 to 2017, the annual percentage of surgeries with participation of a board‐certified surgeon in the eight procedures gradually increased and the operative mortality was kept at a low level. Centralization of the surgical center may also be important for improving surgical outcomes. The operative mortality rate after distal gastrectomy definitively decreased as both surgeon volume and hospital volume increased.24 After risk adjustment for surgeon and hospital volume and patient characteristics, hospital volume (≥52 cases per year) was significantly associated with low operative mortality.24 As for esophagectomy, high‐volume hospitals (≥30 cases per year) had a lower risk‐adjusted mortality rate compared with low‐volume hospitals (≤10 cases).25
Although the postoperative mortality was kept at a low level, the annual rate of postoperative complications with C‐D classification of grade III or higher gradually increased over time. The reason for this increase in complications may be related to the aging population with increased comorbidities. The factors causing these phenomena should be investigated for each procedure. To improve short‐term surgical outcomes in aged patients, minimally invasive surgery might play a pivotal role. The annual rate of endoscopic surgery dramatically increased from 2011 to 2017. Studies using the NCD data showed that the length of hospital stay was significantly shorter in patients who underwent endoscopic surgery.26, 27
The NCD is currently estimated to contain data on approximately 95% of all surgical cases in Japan.28 The NCD provides transparency of surgical outcomes.2 Using the NCD, many studies have been conducted and other studies are in progress to improve surgical outcomes.
DISCLOSURE
Conflicts of Interest: Authors declare no conflicts of interest for this article.
ACKNOWLEDGEMENTS
We thank all the data managers and hospitals participating in this NCD project for their efforts in entering the data.
Hasegawa H, Takahashi A, Kakeji Y, et al. Surgical outcomes of gastroenterological surgery in Japan: Report of the National Clinical Database 2011‐2017. Ann Gastroenterol Surg. 2019;3:426–450. 10.1002/ags3.12258
REFERENCES
- 1. Tomotaki A, Kumamaru H, Hashimoto H, Takahashi A, Ono M, Iwanaka T, et al. Evaluating the quality of data from the Japanese National Clinical Database 2011 via a comparison with regional government report data and medical charts. Surg Today. 2019;49: 65–71. [DOI] [PubMed] [Google Scholar]
- 2. Gotoh M, Miyata H, Hashimoto H, Wakabayashi G, Konno H, Miyakawa S, et al. National Clinical Database feedback implementation for quality improvement of cancer treatment in Japan: from good to great through transparency. Surg Today. 2016;46: 38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kakeji Y, Takahashi A, Udagawa H, Unno M, Endo I, Kunisaki C, et al. Surgical outcomes in gastroenterological surgery in Japan: report of National Clinical database 2011‐2016. Ann Gastroenterol Surg. 2018;2:37–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web‐based database. Ann Surg. 2014;260:259–66. [DOI] [PubMed] [Google Scholar]
- 5. Kurita N, Miyata H, Gotoh M, Shimada M, Imura S, Kimura W, et al. Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a nationwide web‐based data entry system. Ann Surg. 2015;262: 295–303. [DOI] [PubMed] [Google Scholar]
- 6. Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, et al. Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internetbased database. Ann Surg. 2014; 260: 1034–39. [DOI] [PubMed] [Google Scholar]
- 7. Kobayashi H, Miyata H, Gotoh M, Baba H, Kimura W, Kitagawa Y, et al. Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol. 2014; 49:1047–55. [DOI] [PubMed] [Google Scholar]
- 8. Matsubara N, Miyata H, Gotoh M, Tomita N, Baba H, Kimura W, et al. Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large‐scale clinical database. Dis Colon Rectum. 2014;57:1075–81. [DOI] [PubMed] [Google Scholar]
- 9. Kenjo A, Miyata H, Gotoh M, Kitagawa Y, Shimada M, Baba H, et al. Risk stratification of 7,732 hepatectomy cases in 2011 from the National Clinical Database for Japan. J Am Coll Surg. 2014;218:412–22. [DOI] [PubMed] [Google Scholar]
- 10. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single‐race population (Japanese) using a web‐based data entry system: the 30‐day and in‐hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014;259:773–80. [DOI] [PubMed] [Google Scholar]
- 11. Nakagoe T, Miyata H, Gotoh M, Anazawa T, Baba H, Kimura W, et al. Surgical risk model for acute diffuse peritonitis based on a Japanese nationwide database: an initial report on the surgical and 30‐day mortality. Surg Today. 2015; 45: 1233–43. [DOI] [PubMed] [Google Scholar]
- 12. Kunisaki C, Miyata H, Konno H, Saze Z, Hirahara N, Kikuchi H, et al. Modeling preoperative risk factors for potentially lethal morbidities using a nationwide Japanese web‐based database of patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer. 2017;20:496–507. [DOI] [PubMed] [Google Scholar]
- 13. Kikuchi H, Miyata H, Konno H, Kamiya K, Tomotaki A, Gotoh M, et al. Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web‐based nationwide registry. Gastric Cancer. 2017;20: 987–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yoshida T, Miyata H, Konno H, Kumamaru H, Tangoku A, Furukita Y, et al. Risk assessment of morbidities after right hemicolectomy based on the National Clinical Database in Japan. Ann Gastroenterol Surg. 2018;2:220–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Watanabe T, Miyata H, Konno H, Kawai K, Ishihara S, Sunami E, et al. Prediction model for complications after low anterior resection based on data from 33,411 Japanese patients included in the National Clinical Database. Surgery. 2017;161:1597–1608. [DOI] [PubMed] [Google Scholar]
- 16. Aoki S, Miyata H, Konno H, Gotoh M, Motoi F, Kumamaru H, et al. Risk factors of serious postoperative complications after pancreaticoduodenectomy and risk calculators for predicting postoperative complications: a nationwide study of 17,564 patients in Japan. J Hepatobiliary Pancreat Sci. 2017; 24:243–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yokoo H, Miyata H, Konno H, Taketomi A, Kakisaka T, Hirahara N, et al. Models predicting the risks of six life‐threatening morbidities and bile leakage in 14,970 hepatectomy patients registered in the National Clinical Database of Japan. Medicine (Baltimore). 2016; 95:e5466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kanaji S, Takahashi A, Miyata H, Marubashi S, Kakeji Y, Konno H, et al. Initial verification of data from a clinical database of gastroenterological surgery in Japan. Surg Today. 2019;49:328–33. [DOI] [PubMed] [Google Scholar]
- 19. Konno H, Kamiya K, Kikuchi H, Miyata H, Hirahara N, Gotoh M, et al. Association between the participation of board‐certified surgeons in gastroenterological surgery and operative mortality after eight gastroenterological procedures. Surg Today. 2017;47:611–18. [DOI] [PubMed] [Google Scholar]
- 20. Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien‐Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Estimates of the population in Japan. [updated 2017]. https://www.stat.go.jp/data/jinsui/2017np/index.html
- 22. Anazawa T, Paruch JL, Miyata H, Gotoh M, Ko CY, Cohen ME, et al. Comparison of national operative mortality in gastroenterological surgery using web‐based prospective data entry systems. Medicine (Baltimore). 2015;94:e2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012;380:1059–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Iwatsuki M, Yamamoto H, Miyata H, Kakeji Y, Yoshida K, Konno H, et al. Effect of hospital and surgeon volume on postoperative outcomes after distal gastrectomy for gastric cancer based on data from 145,523 Japanese patients collected from a nationwide web‐based data entry system. Gastric Cancer. 2019;22:190–201. [DOI] [PubMed] [Google Scholar]
- 25. Nishigori T, Miyata H, Okabe H, Toh Y, Matsubara H, Konno H, et al. Impact of hospital volume on risk‐adjusted mortality following oesophagectomy in Japan. Br J Surg. 2016;103:1880–86. [DOI] [PubMed] [Google Scholar]
- 26. Yoshida K, Honda M, Kumamaru H, Kodera Y, Kakeji Y, Hiki N, et al. Surgical outcomes of laparoscopic distal gastrectomy compared to open distal gastrectomy: a retrospective cohort study based on a nationwide registry database in Japan. Ann Gastroenterol Surg. 2017;2:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hiki N, Honda M, Etoh T, Yoshida K, Kodera Y, Kakeji Y, et al. Higher incidence of pancreatic fistula in laparoscopic gastrectomy. Real‐world evidence from a nationwide prospective cohort study. Gastric Cancer. 2018;21:162–170. [DOI] [PubMed] [Google Scholar]
- 28. Seto Y, Kakeji Y, Miyata H, Iwanaka T. National Clinical Database (NCD) in Japan for gastroenterological surgery: brief introduction. Ann Gastroenterol Surg. 2017;1:80–81. [DOI] [PMC free article] [PubMed] [Google Scholar]


