Abstract
Objective Knowledge of internal anatomy of the teeth is of great importance in endodontics, leading to success in root canal therapy (RCT). The aim of this study was to assess the root anatomy and canal configuration of maxillary molars in a Brazilian subpopulation using tomographic images using a voxel size of 125 μm.
Materials and Methods This in vivo retrospective study assessed 651 cone-beam computed tomographic scans from 328 maxillary first molars and 323 maxillary second molars. The images were assessed by two endodontists and an oral radiologist. Only permanent molars with fully developed roots and with no signs of RCT were included.
Results Maxillary first and second molars presented three separated roots in 99.39 and 90.09% of the cases, respectively. The presence of mesiolingual canals in the mesiobuccal roots was 64.22% for maxillary first molars and 33.56% for maxillary second molars. Distobuccal canals in the maxillary first and second molars presented Vertucci's Type I configuration in 99.39 and 99.66%, respectively, and palatal canals in the maxillary first and second molars presented Vertucci's Type I configuration in 99.69 and 99.68%, respectively. Maxillary second molars were more subjected to anatomical variations than first molars. Female patients presented higher prevalence of mesiolingual canals in the maxillary second molars.
Conclusions The most prevalent morphology in the maxillary first and second molars was three root canals. The presence of only one or two roots is more likely to occur in the maxillary second molars than in the maxillary first molars. Mesiolingual canals in mesiobuccal roots are more frequent in the maxillary first molars than in the maxillary second molars, and the occurrence of two distobuccal or two palatal canals is rare.
Keywords: canal configuration, cone-beam computed tomography, maxillary molars, morphology, root anatomy, root canal therapy
Introduction
The domain of internal anatomy of the teeth is a key point for the achievement of disinfection in root canal therapy (RCT). Proper location, cleaning, and shaping of the canals are paramount for success in endodontics; on the other hand, missing canals are one of the main reasons for failures in RCT. 1 Maxillary molars are known for their complex anatomy mainly due to the variation in the mesiolingual canals in mesiobuccal roots (MB2), therefore presenting as a challenging tooth. 2
Different methodologies have been used for the assessment of internal anatomy of maxillary molars. 3 Vertucci used extracted teeth to propose an anatomical classification of internal morphology of roots. 4 Scanning electronic microscopic (SEM) and micro-computed tomographic (micro-CT) studies were also used to evaluate the variances in the anatomy of maxillary molars. 5 6 Nonetheless, results might be discrepant between clinical and laboratory studies. 7 8
Clinically, the domain of the anatomy will be fulfilled with the use of magnification, tools for root canal location, and previous image evaluation. 9 10 Despite its limitation, cone-beam CT (CBCT) has been largely used before RCT for a better assessment of internal anatomy. 9 11 The three-dimensional (3-D) characteristics of such images are claimed to render a better visualization of the root canal system. 12 The operators are able to read the volumes in axial, sagittal, and coronal views.
Several studies have evaluated the internal anatomy of permanent maxillary molars in different populations with CBCT scans obtained with different voxel sizes. 13 14 15 16 17 Recent studies have assessed the internal anatomy of maxillary molars in Brazilian subpopulations using CBCT, with a voxel size of 200 μm. 18 19 Recent advances in the CBCT devices along with the development of image software lead to smaller voxel sizes and diminished radiation exposure. Therefore, the objective of this study was to assess the internal anatomy of first and second maxillary molars in a Brazilian populace using CBCT images obtained with a voxel size of 125 μm.
Materials and Methods
This retrospective study was submitted to the Institutional Review Board of the Faculdade de Odontologia São Leopoldo Mandic, and an exempt status was obtained (#68465817.6.0000.5374). Images from 651 CBCT scans were assessed. The images were obtained from examinations in a private radiology clinic taken from July 2014 to December 2017 for routine examinations used for treatment planning not related to this study. The inclusion criteria were adult patients aged from 18 to 45 years, presenting with maxillary molars with mature apices and fully developed roots. Teeth presenting metallic crowns or any signs of previous RCT were removed from the study. The assessment of the images was performed retrospectively from April 2017 until December 2017, starting from the images obtained in July 2014 until the images obtained in December 2017.
The images were achieved using a 3D Accuitomo 80 CBCT (J. Morita, Kyoto, Japan) at 90 KVA, 8 mA, exposure time of 18 second small field of view (FOV) 40 mm × 40 mm, and voxel size of 125 μm. The slices ranged from 0.125 to 2 mm and radiation dose of 20 μSv. When an FOV of 60 mm × 60 mm was applied, the radiation dose was of 43 μSv.
The images were evaluated simultaneously by two experienced endodontists in duplicate, with at least 14 days of interval between the evaluations. In case of disagreement between the examiners, an oral radiologist discussed the cases until a consensus was reached. The examiners, in a dark room, used a high-definition screen Dell U2312HM DIGITAL (1920 × 1080, TrueColor 32 bits, 60 Hz), with dedicated memory video board 1024 MB (Dell Inc., Austin, Texas, United States). The software i-Dixel (J Morita, Tokyo, Japan) was used for image manipulation. Root anatomy was classified as proposed by Zhang et al 20 and root canal morphology followed the types proposed by Vertucci. 4
Descriptive analysis was used to summarize the overall results for root morphology and canal anatomy. For differences in root morphology between male and female patients, the Z-test was used; Fisher's exact test was used for differences between male and female patients with regard to the presence of MB2 canals at p = 0.05.
Results
Overall, 328 maxillary first molars and 323 maxillary second molars were assessed based on 510 patients (297 males) with a mean age of 31.41 years.
Morphological Distribution of Maxillary First Molars
Three hundred and twenty-eight maxillary first molars were assessed; 326 presenting three roots (99.39%) and two (0.61%) presenting two roots. The morphological aspect of these teeth based on Zhang et al is shown in Table 1 .
Table 1. Root configuration of maxillary first and second molars.
| Variant | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | VIII | N/A a | |
| N/A, not available. a Morphology not included in any variant of Zhang et al. 20 | |||||||||
| Maxillary first molars, n (%) | 121 (36.78) | 203 (61.70) | 1 (0.30) | 0 | 1 (0.30) | 0 | 0 | 0 | 2 (0.60) |
| Maxillary second molars, n (%) | 194 (60.06) | 96 (29.72) | 21 (6.50) | 3 (0.93) | 1 (0.31) | 7 (2.17) | 0 | 0 | 1 (0.31) |
Characteristics of Roots of Maxillary First Molars
Based on Vertucci's classification, 35.78% of mesiobuccal roots presented Vertucci's Type I classification, meaning that only one canal was present; 64.22% of the mesiobuccal roots presented two canals, encompassing Types II to VII; none of the roots presented three canals (Type VIII).
The distobuccal roots presented only one root canal in 99.38% and two root canals in 0.62%.
The palatal roots of maxillary first molars presented only one root canal in 99.69% of the cases and two root canals in 0.31% of the cases. The complete classification of root canals is shown in Table 2 .
Table 2. Configuration of root canal systems of maxillary first and second molars, number, and percentage.
| Type I | Type II | Type III | Type IV | Type V | Type VI | Type VII | Type VIII | ||
|---|---|---|---|---|---|---|---|---|---|
| Abbreviations: DB, distobuccal; MB, mesiobuccal. | |||||||||
| First molar | |||||||||
| MB | 117 (35.78) | 95 (29.05) | 4 (1.23) | 95 (29.05) | 8 (2.45) | 4 (1.22) | 4 (1.22) | – | |
| DB | 325 (99.39) | 1 (0.31) | – | 1 (0.31) | – | – | – | – | |
| Palatal | 326 (99.69) | 1 (0.31) | – | – | – | – | – | – | |
| Second molar | |||||||||
| MB | 194 (66.44) | 45 (15.41) | 7 (2.4) | 38 (13.01) | 3 (1.03) | 5 (1.71) | – | – | |
| DB | 291 (99.66) | 1 (0.34) | – | – | – | – | – | – | |
| Palatal | 312 (99.68) | – | – | 1 (0.32) | – | – | – | – | |
Morphological Distribution of Maxillary Second Molars
Three hundred and twenty-three maxillary second molars were assessed; 291 (90.09%) presenting three roots, 22 (6.81%) presenting two roots, and 10 (3.10%) presenting one root. The morphological aspect of these teeth based on Zhang et al is shown in Table 1 .
Characteristics of Roots of Maxillary Second Molars
Based on Vertucci's classification, 66.44% of mesiobuccal roots presented Vertucci's Type I classification, meaning that only one canal was present; 33.56% of the mesiobuccal roots presented two canals encompassing Types II to VII; none of the roots presented three canals (Type VIII).
The distobuccal roots presented only one root canal in 99.66% and two root canals in 0.34%.
The palatal roots of maxillary first molars presented only one root canal in 99.68% of the cases and two root canals in 0.32% of the cases. The complete classification of root canals is shown in Table 2 . Figs. 1 2 show the examples of axial view of maxillary molars.
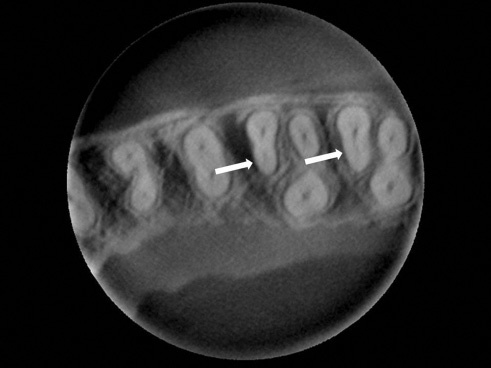
Fig. 1.

Axial view of first and second maxillary molars presenting with three separated roots and a single canal in each root.
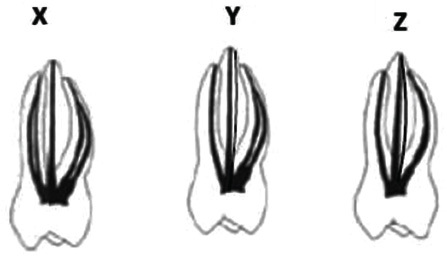
Fig. 2.
Axial view of first and second maxillary molars, arrows pointing mesiobuccal root configuration with two canals (first molar) and one canal (second molar).
Morphological Distribution of Maxillary Molars of Male Patients
Two hundred and ninety-seven maxillary molars of male patients were assessed; 289 (97.31%) presenting three roots, 3 (1.01%) presenting two roots, and 5 (1.68%) presenting one root.
Characteristics of Roots of Maxillary Molars of Male Patients
Male patients presented in maxillary first molars 38.96% of mesiobuccal roots presenting Vertucci's Type I classification, meaning that only one canal was present. About 61.04% of the mesiobuccal roots presented two canals encompassing Types II to VII; none of the roots presented three canals (Type VIII). In the maxillary second molars 68.53% of mesiobuccal roots presented Vertucci's Type I classification; 31.47% of the mesiobuccal roots presented two canals encompassing Types II to VII; none of the roots presented three canals (Type VIII).
Morphological Distribution of Maxillary Molars of Female Patients
Three hundred and fifty-four maxillary molars of male patients were assessed; 328 (92.66%) presenting three roots, 19 (5.93%) presenting two roots, and 5 (1.41%) presenting one root.
Characteristics of Roots of Maxillary Molars of Female Patients
Based on Vertucci's classification, female patients presented in maxillary first molars 32.76% of mesiobuccal roots presenting Vertucci's Type I classification, meaning that only one canal was present; 67.24% of the mesiobuccal roots presented two canals encompassing Types II to VII; none of the roots presented three canals (Type VIII). In maxillary second molars 53.33% of mesiobuccal roots presented Vertucci´s Type I classification; 46.67% of the mesiobuccal roots presented two canals encompassing Types II to VII; none of the roots presented three canals (Type VIII).
Female patients presented statistically significant more Variant I and III in the maxillary second molars when compared with male patients ( p < 0.05). No statistically significant differences were found in the other variants; no differences were found in the maxillary second molars ( p < 0.05). Table 3 displays the root morphology based on Zhang et al's 20 classification.
Table 3. Root configuration of maxillary first and second molars according to the patient's gender.
| Gender | Tooth type | Variant | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | VIII | N/A a | ||
| N/A, not available. a Indicates statistically significant difference at p < 0.05. | ||||||||||
| Male | First molars, n (%) | 61 (39.61) | 92 (59.72) | 0 | 0 | 0 | 0 | 0 | 0 | 1 (0.65) |
| Second molars, n (%) | 98 (68.53) a | 37 (25.87) | 3 (2.10) a | 2 (1.40) | 0 | 3 (2.10) | 0 | 0 | 0 | |
| Female | First molars, n (%) | 60 (34.48) | 110 (63.22) | 1 (0.57) | 0 | 1 (0.57) | 0 | 0 | 0 | 2 (1.15) |
| Second molars, n (%) | 96 (53.33) a | 60 (33.33) | 18 (10.00) a | 1 (0.56) | 1 (0.56) | 4 (2.22) | 0 | 0 | 0 | |
The incidence of MB2 canals was not statistically different between male (61.04%) and female (67.24%) patients in maxillary first molars ( p > 0.05). In the maxillary second molars, female (46.67%) patients presented significantly more MB2 canals present than male patients (31.47%) ( p < 0.05).
Discussion
The complete cleaning of the root canal is highly dependent on the proper domain of anatomy. However, two-dimensional radiographic examination is limited to reveal internal morphology of teeth. Diaphanization, sectioning, SEM, and micro-CT examinations are more prone to expose the real internal morphology of the root canals, but these methods are not clinically useful. 2 5 6 Therefore, a CBCT scan is the current gold standard for clinical assessment of internal morphology before RCT. 21 22 Interpretation of CBCT volumes might be difficult for inexperienced operators and endodontists 23 24 ; thus, the images of the present study were assessed by two experienced endodontists and an oral radiologist who discussed the discrepancies until a consensus was reached. To avoid artifacts related to filled root canals, only teeth presenting no root canal treatment were assessed in the present study. 23
Overall, our results differ slightly from the results of Zhang et al as discovered in a Chinese population. 20 In our study, Variant I was present in 36.78% of maxillary first molars and Variant II in 61.70%, while Zhang et al found similar results for both variations (48% and 52%, respectively). In maxillary second molars, however, our results are similar to that study, as Variant I was present in 60.06% in our subpopulation and 63.3% in the Chinese population; however, our findings showed remarkable predominance of Variant II (29.72%) in the remaining teeth, while the Chinese study showed 17.6% of Variant II. 20 In addition, two maxillary first molars (0.60%) and one maxillary second molar (0.31%) presented configuration not included in any of Zhang et al's variations ( Fig. 3 ). The high incidence of three rooted first molars (99.39%) and second molars (90.09%) is in agreement with the findings of different populations. 14 16 17
Fig. 3.
Variations in root morphology of maxillary molars found in Zhang et al. 20
Variations in mesiobuccal roots of maxillary molars present a great defiance for endodontic therapy. Specifically, the presence of MB2 canals is of utmost importance in treating maxillary molars. Our results showed a higher frequency of two canals in first molars (64.22%) than in second molars (33.56%), and high variation in anatomies encompassing seven out of eight possible types proposed by Vertucci. The greater incidence of two canals in mesiobuccal roots in maxillary first molars than in maxillary second molars concurs with studies in different populations such as Chinese (52 and 22%), 20 Egyptian (74.55 and 57.94%), 17 Thai (73.6 and 56.2%), 14 Spanish (87.2 and 47.3%), 13 Iranian (44.8 and 18.5%), 25 Italian (40.3 and 15.1%), 26 and Portuguese (71.05 and 43.56%). 27
The findings of the present in vivo study, using voxel size of 125 μm, showed 64.22% of MB2 canals in maxillary first molars and 33.56% of MB2 canals in maxillary second molars. Two recent studies assessed root canal configuration of maxillary molars in a population similar to the present study, nonetheless using CBCT images with voxel size of 200 μm. 18 19 The results of Silva et al presented two canals in mesiobuccal roots in 42.63 and 34.42% in first and second maxillary molars, respectively. A previous in vitro study has demonstrated that sharper images are provided by smaller voxel sizes 28 ; therefore, one might assume that the smaller voxel size used in the present study has led to better visualization of the MB2 canals. However, Reis et al, 19 also using a voxel size of 200 μm in a Brazilian subpopulation, showed an incidence of MB2 canals of 87.97 and 78.92% for maxillary first and second molars, respectively. Thereby, it is our understanding that the difference in voxel size was unable to influence the results, which concurs with a previous ex vivo study that showed no statistical differences in visualization of MB2 canals when voxel sizes of 125 or 200 μm voxel were used. 29 Some reasons might explain the discrepancies in the aforementioned clinical studies: small variations in the population observed—same country but different states—or the subjective evaluation applied by observers. Furthermore, in the present study, the mean age of the patients was 31.14 years, which is not mentioned by Silva et al; meanwhile, Reis et al showed that the visualization of MB2 canals decreases with aging. 18 19
In addition to race and age, gender has also been suggested to impact the internal root morphology of teeth. A recent study assessed differences in root morphology between male and female patients in the Portuguese population. 27 Indeed, in agreement with Martins et al, our results showed differences in root morphology in maxillary second molars but no difference between the groups in maxillary first molars ( Table 3 ). However, our results showed that a higher incidence of MB2 canals visualized in maxillary second molars of female patients (46.67%) than in male patients (31.47%), which is in disagreement with Martins et al. 27
The incidence of visualized MB2 canals in the present study is considerably lower than the 93.0 and 60.4% of MB2 canals located in vivo by an endodontic specialist. 7 Other clinical studies also showed a higher incidence of MB2 canals located by graduate 30 and undergraduate students 31 than the findings of the present study. These results corroborate Parker et al, 11 which presented the limitations of CBCT in showing MB2 canals, thus emphasizing the need for troughing under magnification for MB2 location in vivo, regardless of visualization in the tridimensional images.
Even though racial characteristics might influence the morphology of the teeth, our results are in consonance with previous studies showing high incidence of Vertucci's Type I configuration for distobuccal and palatal canals in both maxillary first and second molars. Overall, these studies presented this configuration in over 97% of these roots. 14 17 However, the clinician should be aware of the importance of proper magnification and troughing when searching for extra canals in these roots because previous case series presented two canals in palatal and distobuccal roots. 32 33
The presence of C-shaped canals in maxillary molars can be considered rare. 34 In fact, in the present study, there was no occurrence of such variation in both first and second molars. A recent study in a Korean population presented results that are divergent from ours as 1.8% of the sample displayed the occurrence of C-shaped canals. 35 Our findings showed fused roots in 0.61% (first molars) and 9.91% (second molars) of the cases. These results are lower than the results presented by Jo et al in the Korean population 3.2 and 19.5% for the maxillary first and second molars, respectively. 35 Martins et al, 36 in a Portuguese population, also showed a higher incidence of root fusion 7.1% in maxillary first molars and 25.2% in maxillary first molars. It seems that racial characteristics play an important role in the incidence of fused roots in maxillary molars.
According to the results of the present study, it is concluded that the most common morphology in maxillary first and second molars was three root canals. The presence of only one or two roots is more likely to occur in maxillary second molars than in maxillary first molars. MB2 canals are more frequent in maxillary first molars than in maxillary second molars, and the occurrence of two distobuccal or two palatal canals is rare.
Financial Support and Sponsorship
The authors would like to thank CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) for supporting this project.
Footnotes
Conflicts of Interest None declared.
References
- 1.Song M, Kim H C, Lee W, Kim E. Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery. J Endod. 2011;37(11):1516–1519. doi: 10.1016/j.joen.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 2.Kulild J C, Peters D D. Incidence and configuration of canal systems in the mesiobuccal root of maxillary first and second molars. J Endod. 1990;16(07):311–317. doi: 10.1016/s0099-2399(06)81940-0. [DOI] [PubMed] [Google Scholar]
- 3.Cleghorn B M, Christie W H, Dong C C. Root and root canal morphology of the human permanent maxillary first molar: a literature review. J Endod. 2006;32(09):813–821. doi: 10.1016/j.joen.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 4.Vertucci F J. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58(05):589–599. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 5.Wolf T G, Paqué F, Woop A C, Willershausen B, Briseño-Marroquín B. Root canal morphology and configuration of 123 maxillary second molars by means of micro-CT. Int J Oral Sci. 2017;9(01):33–37. doi: 10.1038/ijos.2016.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilles J, Reader A. An SEM investigation of the mesiolingual canal in human maxillary first and second molars. Oral Surg Oral Med Oral Pathol. 1990;70(05):638–643. doi: 10.1016/0030-4220(90)90415-o. [DOI] [PubMed] [Google Scholar]
- 7.Stropko J J. Canal morphology of maxillary molars: clinical observations of canal configurations. J Endod. 1999;25(06):446–450. doi: 10.1016/S0099-2399(99)80276-3. [DOI] [PubMed] [Google Scholar]
- 8.Sempira H N, Hartwell G R. Frequency of second mesiobuccal canals in maxillary molars as determined by use of an operating microscope: a clinical study. J Endod. 2000;26(11):673–674. doi: 10.1097/00004770-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Patel S, Durack C, Abella F, Shemesh H, Roig M, Lemberg K. Cone beam computed tomography in Endodontics – a review. Int Endod J. 2015;48(01):3–15. doi: 10.1111/iej.12270. [DOI] [PubMed] [Google Scholar]
- 10.Brüllmann D D, Weichert C I, Daubländer M. Intraoral cameras as a computer-aided diagnosis tool for root canal orifices. J Dent Educ. 2011;75(11):1452–1457. [PubMed] [Google Scholar]
- 11.Parker J, Mol A, Rivera E M, Tawil P. CBCT uses in clinical endodontics: the effect of CBCT on the ability to locate MB2 canals in maxillary molars. Int Endod J. 2017;50(12):1109–1115. doi: 10.1111/iej.12736. [DOI] [PubMed] [Google Scholar]
- 12.Vizzotto M B, Silveira P F, Arús N A, Montagner F, Gomes B P, da Silveira H E. CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molar teeth: effect of voxel size and presence of root filling. Int Endod J. 2013;46(09):870–876. doi: 10.1111/iej.12075. [DOI] [PubMed] [Google Scholar]
- 13.Pérez-Heredia M, Ferrer-Luque C M, Bravo M, Castelo-Baz P, Ruíz-Piñón M, Baca P. Cone-beam computed tomographic study of root anatomy and canal configuration of molars in a Spanish population. J Endod. 2017;43(09):1511–1516. doi: 10.1016/j.joen.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 14.Ratanajirasut R, Panichuttra A, Panmekiate S. A cone-beam computed tomographic study of root and canal morphology of maxillary first and second permanent molars in a Thai population. J Endod. 2018;44(01):56–61. doi: 10.1016/j.joen.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 15.Zheng Q H, Wang Y, Zhou X D, Wang Q, Zheng G N, Huang D M. A cone-beam computed tomography study of maxillary first permanent molar root and canal morphology in a Chinese population. J Endod. 2010;36(09):1480–1484. doi: 10.1016/j.joen.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 16.Guo J, Vahidnia A, Sedghizadeh P, Enciso R. Evaluation of root and canal morphology of maxillary permanent first molars in a North American population by cone-beam computed tomography. J Endod. 2014;40(05):635–639. doi: 10.1016/j.joen.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Ghobashy A M, Nagy M M, Bayoumi A A. Evaluation of root and canal morphology of maxillary permanent molars in an Egyptian population by cone-beam computed tomography. J Endod. 2017;43(07):1089–1092. doi: 10.1016/j.joen.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Silva E J, Nejaim Y, Silva A I, Haiter-Neto F, Zaia A A, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod. 2014;40(02):173–176. doi: 10.1016/j.joen.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Reis A G, Grazziotin-Soares R, Barletta F B, Fontanella V R, Mahl C R. Second canal in mesiobuccal root of maxillary molars is correlated with root third and patient age: a cone-beam computed tomographic study. J Endod. 2013;39(05):588–592. doi: 10.1016/j.joen.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Zhang R, Yang H, Yu X, Wang H, Hu T, Dummer P M. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J. 2011;44(02):162–169. doi: 10.1111/j.1365-2591.2010.01826.x. [DOI] [PubMed] [Google Scholar]
- 21.Studebaker B, Hollender L, Mancl L, Johnson J D, Paranjpe A. The incidence of second mesiobuccal canals located in maxillary molars with the aid of cone-beam computed tomography. J Endod. 2018;44(04):565–570. doi: 10.1016/j.joen.2017.08.026. [DOI] [PubMed] [Google Scholar]
- 22.Gambarini G, Piasecki L, Ropini P, Miccoli G, Di Nardo D, Testarelli L. Cone-beam computed tomographic analysis on root and canal morphology of mandibular first permanent molar among multiracial population in Western European population. Eur J Dent. 2018;12(03):434–438. doi: 10.4103/ejd.ejd_116_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beacham J T, Geist J R, Yu Q, Himel V T, Sabey K A. Accuracy of cone-beam computed tomographic image interpretation by endodontists and endodontic residents. J Endod. 2018;44(04):571–575. doi: 10.1016/j.joen.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 24.Parker J M, Mol A, Rivera E M, Tawil P Z. Cone-beam computed tomography uses in clinical endodontics: observer variability in detecting periapical lesions. J Endod. 2017;43(02):184–187. doi: 10.1016/j.joen.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Khosravifard N, Kajan Z D, Hasanpoor H. Cone beam computed tomographic survey of the mesiobuccal root canal anatomy in the maxillary first and second molar teeth of an Iranian population. Eur J Dent. 2018;12(03):422–427. doi: 10.4103/ejd.ejd_60_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plotino G, Tocci L, Grande N M. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: a cone-beam computed tomography study in vivo. J Endod. 2013;39(12):1545–1548. doi: 10.1016/j.joen.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 27.Martins J NR, Marques D, Mata A, Caramês J. Root and root canal morphology of the permanent dentition in a Caucasian population: a cone-beam computed tomography study. Int Endod J. 2017;50(11):1013–1026. doi: 10.1111/iej.12724. [DOI] [PubMed] [Google Scholar]
- 28.Maret D, Telmon N, Peters O A. Effect of voxel size on the accuracy of 3D reconstructions with cone beam CT. Dentomaxillofac Radiol. 2012;41(08):649–655. doi: 10.1259/dmf/81804525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bauman R, Scarfe W, Clark S, Morelli J, Scheetz J, Farman A. Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. Int Endod J. 2011;44(08):752–758. doi: 10.1111/j.1365-2591.2011.01882.x. [DOI] [PubMed] [Google Scholar]
- 30.Hartwell G, Appelstein C M, Lyons W W, Guzek M E. The incidence of four canals in maxillary first molars: a clinical determination. J Am Dent Assoc. 2007;138(10):1344–1346. doi: 10.14219/jada.archive.2007.0050. [DOI] [PubMed] [Google Scholar]
- 31.Coelho M S, Parker J M, Tawil P Z. Second mesiobuccal canal treatment in a predoctoral dental clinic: a retrospective clinical study. J Dent Educ. 2016;80(06):726–730. [PubMed] [Google Scholar]
- 32.Fogel H M, Cunha R S. Maxillary first molars with 2 distobuccal canals: a case series. J Endod. 2017;43(11):1925–1928. doi: 10.1016/j.joen.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 33.Fogel H M, Peikoff M D, Christie W H. Canal configuration in the mesiobuccal root of the maxillary first molar: a clinical study. J Endod. 1994;20(03):135–137. doi: 10.1016/S0099-2399(06)80059-2. [DOI] [PubMed] [Google Scholar]
- 34.De Moor R J. C-shaped root canal configuration in maxillary first molars. Int Endod J. 2002;35(02):200–208. doi: 10.1046/j.1365-2591.2002.00461.x. [DOI] [PubMed] [Google Scholar]
- 35.Jo H, Min J B, Hwang H K. Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography. Restor Dent Endod. 2016;41(01):55–62. doi: 10.5395/rde.2016.41.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martins J N, Mata A, Marques D, Caramês J. Prevalence of root fusions and main root canal merging in human upper and lower molars: a cone-beam computed tomography in vivo study . J Endod. 2016;42(06):900–908. doi: 10.1016/j.joen.2016.03.005. [DOI] [PubMed] [Google Scholar]


