Abstract
Background
In Tanzania, the information on Birth Preparedness and Complication Readiness is insufficiently provided to pregnant women and their families. The aim of this study was to evaluate the maternal and infant outcomes of a family-oriented antenatal group education program that promotes Birth Preparedness and Complication Readiness in rural Tanzania.
Methods
Pregnant women and families were enrolled in a program about nutrition and exercise, danger signs, and birth preparedness. The cross sectional survey was conducted one year later to evaluate if the participants of the program (intervention group) were different from those who did not participate (control group) with respect to birth-preparedness and maternal and infant outcomes.
Results
A total of 194 participants (intervention group, 50; control group, 144) were analyzed. For Birth Preparedness and Complication Readiness, the intervention group participants knew a health facility in case of emergency (OR: 3.11, 95% CI: 1.39–6.97); arranged accompaniment to go to a health facility for birth (OR: 2.56, 95% CI: 1.17–5.60); decided the birthplace with or by the pregnant women (OR: 3.11, 95% CI: 1.44–6.70); and attended antenatal clinic more than four times (OR: 2.39, 95% CI: 1.20–4.78). For birth outcomes, the intervention group had less bleeding or seizure during labour and birth (OR: 0.28, 95%CI: 0.13–0.58); fewer Caesarean sections (OR: 0.16, 95% CI: 0.07–0.36); and less neonatal complications (OR: 0.28, 95% CI: 0.13–0.60).
Conclusions
The four variables were significantly better in the intervention group, i.e., identifying a health facility for emergencies, family accompaniment for facility birth, antenatal visits, and involvement of women in decision-making, which may be key factors for improving birth outcome variables. Having identified these key factors, male involvement and healthy pregnant lives should be emphasized in antenatal education to reduce pregnancy and childbirth complications.
Trial registration
Registered 12 August 2013.
Keywords: Pregnancy, Childbirth, Birth preparedness, Antenatal education, Male involvement, Africa
Plain English summary
In Tanzania, the information on Birth Preparedness and Complication Readiness (BPCR) is insufficiently provided to pregnant women and their families. Tanzania has been struggling with reducing its maternal mortality ratio: 556/100,000 live births in 2015. As most deaths were from preventable causes, such as postpartum hemorrhage and high blood pressure-related complications, BPCR is essential to timely and safely arrive in health facility. The family-oriented antenatal group education was provided to pregnant women and their families in rural Tanzania. A Tanzanian midwife taught the program on nutrition and exercise, danger signs, and birth preparedness using a picture drama, and the control group received usual care. The same village was visited one year later to evaluate if the program participants were different from those who did not participate with respect to birth-preparedness and maternal and infant outcomes. A total of 194 participants (50 program participants and 144 who did not participate in the program) answered the survey. As a result, the education positively affected BPCR, such as identifying a health facility for emergencies, family accompaniment for facility birth, antenatal care visits, and involvement of women in decision-making. For birth outcomes, the intervention group had less bleeding or seizure during labour and birth, fewer Caesarean sections, and less neonatal complications. Having identified four key factors in BPCR, male involvement and healthy pregnant lives should be emphasized in antenatal education to reduce pregnancy and childbirth complications.
Introduction
In countries where the maternal mortality ratio remains high, antenatal education to increase Birth Preparedness and Complication Readiness (BPCR) is considered one of the top priorities [1]. BPCR includes birth plans during the antenatal period, such as the birthplace, birth attendant, transportation, health facility for complications, expenses, and birth materials, as well as family coordination to achieve such birth plans. In a meta-analysis of BPCR interventions and birth outcomes [2], exposure to BPCR interventions was associated with a non-significant reduction of 28% in maternal mortality risk (seven studies, RR = 0.72; 95% CI: 0.46, 1.13). Tanzania has been struggling with reducing its maternal mortality ratio despite the continuous efforts; the maternal mortality ratio increased to 556/100,000 live births in 2015 from 454 in 2011 [3, 4]. As most deaths were from postpartum hemorrhage and high blood pressure-related complications [5], identification of pregnancy complications and women’s awareness of the danger signs during the antenatal period are essential [6].
In Tanzania, although increasing, only about half of all pregnant women attend an antenatal clinic more than four times [4]. Moreover, the information provided during antenatal care (ANC) is insufficient. In a study in the Rufiji region, information, education, and communication about the danger signs of pregnancy are reportedly insufficiently provided; only 61% of the clinics provided information despite the national policy recommending the provision of this information in every visit [6].
In the resource-poor settings, antenatal group education is a potential approach because of the limited time for individual counseling at antenatal clinics [7, 8]. Patil et al. conducted an antenatal group counseling program called Centering Pregnancy in Malawi and Tanzania and found the program to be feasible and acceptable among pregnant women. Moreover, it increased respect between healthcare providers and pregnant women [9]. Additionally, Oka et al. suggested the importance of job-aid to provide necessary information to pregnant women during antenatal visits. Job aids were found to be helpful for understanding and recalling information for both health providers and pregnant women [10].
In addition, the influence and decision-making power of the family cannot be ignored in Tanzania. Shimpuku et al. identified perceptional gaps among family members who decide the birthplace and stated that many women considered their husbands as the decision-maker [11]. Tancred et al. reported that women could not arrange transport to go to health facilities owing to financial constraints [12]. Therefore, an antenatal group education that addresses both BPCR and family involvement might be effective for ensuring that women reach health facilities at birth, and consequently serious complications could be identified at the proper time. With little or no research linking group education with birth outcomes, the present research intended to fill that gap.
Purpose
This study aimed to evaluate an antenatal group education program among pregnant women and their families with respect to birth-preparedness and maternal and infant outcomes in rural villages of Tanzania.
Hypothesis
The study hypothesis was if Tanzanian pregnant women and their families received a family-oriented antenatal group education, they would (1) have a higher level of BPCR, (2) attend antenatal clinic four or more times, (3) give birth in a health facility, (4) have less complications of women at birth, and (5) have less complications and deaths of infants than those who did not receive the education.
Methods
Study design and participants
This research was a cross sectional evaluation study to identify the effects of an antenatal education program on birth preparedness and maternal-infant outcomes (the second phase). All the participants were convenient samples of pregnant women and their families in villages. For the first phase, villagers were recruited to receive an antenatal education program. The details of the process were published elsewhere [13]. For the second phase, the participants in the first phase (the intervention group) were followed after one year. The research team visited the same villages of the first phase and requested the village leaders to announce the present research to both participants of the first phase and those who did not participate in the first phase of the study. The researchers explained the purpose, the content of the second phase, and the ethical considerations. The inclusion criteria were as follows: 16 years old or older, had experienced pregnancy and childbirth in their family including themselves, had no severe physical or psychological illness, and can read Kiswahili.
Setting
The study was conducted in Korogwe district, which is one of the eight districts in the Tanga region, located in the North Eastern area of the country. Maternal healthcare in Korogwe is provided at one district hospital, three government health centers, one faith-based organization, six private dispensaries, and 41 government dispensaries. Three villages were purposefully selected as the research sites, which were located at least 5 km away from the closest health facility. The distance of villages from health facilities was important as this study focused on preparation of birth and those who live distant from health facilities needed to prepare for birth to be able to seek healthcare when necessary. Thus, if villages were sufficiently close to health facilities, they could access healthcare even if they were not well prepared.
Family-oriented antenatal group education program
The purpose of this family-oriented antenatal group education program was to promote BPCR and family involvement in pregnancy and childbirth. A picture drama was developed by the research team to convey the story of two pregnant women. The material was first developed in English and then translated by a master-prepared bilingual Tanzanian midwife. The program lasts for approximately 45 min, including explanation of the research, pre-test/post-test, picture drama, and discussion among the participants. The result of the pre-test/post-test was published elsewhere [13]. The Tanzanian midwife led the entire program, reading picture drama and encouraging the participants to talk about the contents in the end.
As the picture drama unfolds, the story shows one woman who had attended an antenatal clinic more than four times. During the antenatal clinic visit, a midwife provided information on appropriate nutrition and exercise, danger signs, and birth preparedness. This pregnant woman and her family had prepared transportation, money, and an accompanying person, and identified a health facility to give birth. When she started having contractions, her family was ready to support her timely trip to a health facility. With the support of a Skilled Birth Attendant (SBA), she gave birth a healthy baby. The other pregnant woman had a family who did not understand the importance of antenatal clinic visits and facility births. She did not visit an antenatal clinic and expected a home birth. When she started having contractions, a Traditional Birth Attendant (TBA) came to support her, but she was having an obstructed labour at that time. They waited for many hours before birth, and then observed that the baby was not breathing after birth. The mother started bleeding after giving birth, thus both the mother and the baby were brought to the hospital, but it was too late to save either one of them. The story illustrated the importance of BPCR and family support, as most household decisions including the birthplace in Tanzania are made by the family members, particularly the husband, and not by the woman [11, 14–16].
Study outcomes
The primary outcome was whether the BPCR variables of pregnant women and their families were higher in the intervention group than in the control group. As the pre-test/post-test results of the education program was published elsewhere [13], the present report clarifies whether pregnant women had actually prepared for birth according to the BPCR variables, including a visit to an antenatal clinic four times or more. The questions were asked retrospectively in the second phase. The secondary outcomes were as follows: (1) birth in a health facility, (2) women’s complications at birth, and (3) infants’ complications and deaths.
To evaluate the outcomes, the survey items were developed on the basis of the elements of BPCR [1] in English. The survey included demographic information, BPCR, and outcomes of the most recent childbirth in the family including their own childbirth. A Kiswahili-English bilingual translated the English items into Kiswahili. Another Tanzanian researcher who is a PhD holder and is also a Kiswahili-English bilingual conducted the back translation and confirmed the accuracy of the survey items.
BPCR variables
As for the primary outcome, the BPCR variables included the following elements: desired place of birth; preferred birth attendant; location of the closest facility for birth and in case of complications; funds for any expenses related to birth and in case of complications; supplies and materials necessary to bring to the facility; an identified labour and birth companion; an identified support to look after the home and other children while the woman was away; transport to a facility for birth or in the case of a complications; and identification of compatible blood donors in case of complications. The questions were answerable by yes/no (e.g., “Did you arrange for someone to accompany you or her to go to a health center or a hospital for birth or emergency?”).
Birth outcome variables
For the secondary outcome, the birth outcome variables included the following: did they give birth in a health facility, did an SBA assisted their birth, were there any complications, was the birth by Caesarean section, was it a live birth, did the baby have any complications, and did they want to give birth again at a health facility. The related questions were to be answered by yes or no (e.g., “Did you or she gave birth at a health center or a hospital?”, “Were there any problems like bleeding or seizure during the labour and birth?”).
Sample size
The sample size of this study was calculated on the basis of the basic formula with two groups, a two-sided alternative and normal distributions with the same variances. The sample size was calculated as 64 for each group to detect a difference (10 points) between groups at a 5% level of significance with 80% power.
Data collection
The first phase: intervention
During the first phase of the study, the family-oriented antenatal group education program was provided to pregnant women and their families in the intervention group to promote BPCR and family involvement in the villages, as we intended to reach people who were neither attending an antenatal clinic nor planned to give birth at a health facility.
The second phase: outcome survey
At the second phase of the study, that is, one year later after providing the education program, we returned to the same three villages and contacted those who attended the education program and those in the control group who did not. Those who agreed to participate answered a survey about their BPCR before childbirth and their behaviors and childbirth outcomes for the most recent childbirth they experienced. For the first phase, the education program was provided in August 2013. For the second phase, the outcome survey was conducted in August 2014.
Ethical clearance
Ethical clearance and permissions were obtained from the 1) Institutional Review Board at St. Luke’s International University, Tokyo, Japan (14–040); 2) Director of Korogwe District Council, 3) National Institute for Medical Research (NIMR), Tanzania (NIMR/HQ/R.8/Vol.IX/1604), and 4) Tanzania Commission for Science and Technology (COSTECH) (No.2013–273-NA-2013-101).
Statistical analysis
For background data, the t-test was used for numerical control of the intervention and control groups (i.e., age and number of children). Pearson’s chi-square test was used for other nominal background data. Those who missed values were excluded from the final analysis, so there was no missing data. For BPCR and outcome variables, the odds ratios (ORs) and 95% confidence intervals (CIs) were also calculated with logistic analysis, comparing the intervention group with the control group. As the number of antenatal visits might affect facility delivery [17, 18], the variable of antenatal visit was used as cofounder in the analysis of outcome variables. Data were analyzed using SPSS ver. 24 (SPSS Inc., Chicago, IL, USA).
Results
Sociodemographic characteristics of study population
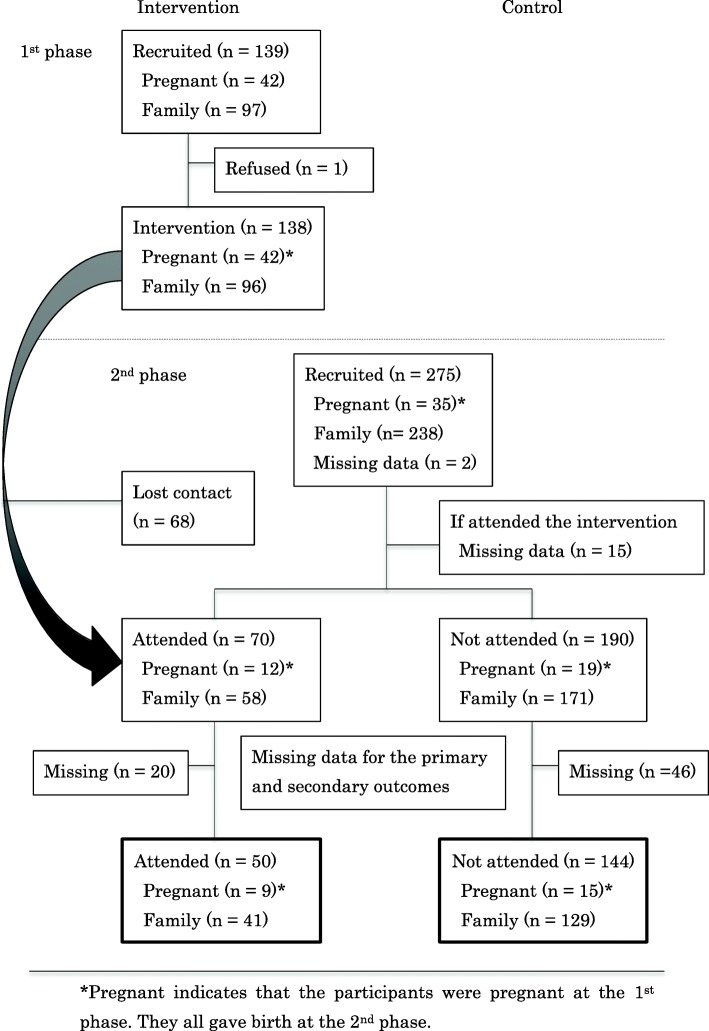
Figure 1 shows the flow of recruitment and the number of participants in both the intervention group and control group in each phase. A total of 275 people were recruited and agreed to participate in the second phase. A total of 260 people answered if they participated in the first phase (n = 70 in intervention group; n = 190 in control group). Furthermore, after eliminating the participants with missing data related to the main outcome variables (n = 20 in intervention group; n = 46 in control group), the valid responses were 194 (n = 50 in intervention group; n = 144 in control group). Table 1 shows the sociodemographic variables of both groups. There were no significant differences in the age, gender, marital status, number of children, educational level, occupation, daily expense, and household asset ownership between the two groups based on chi-square test.
Fig. 1.
Flow of participants for data collection
Table 1.
Sociodemographic characteristics
| Intervention group (n = 50) | Control group (n = 144) | p-value | |||
|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | ||
| Age | 39.42 (15.83) | 38.42 (15.53) | 0.696 | ||
| Gender | 0.672 | ||||
| Women | 25 (50) | 67 (46.5) | |||
| Men | 25 (50) | 77 (53.5) | |||
| Marital status | 0.487 | ||||
| Married | 41 (82) | 109 (77.3) | |||
| Not married | 9 (18) | 32 (22.7) | |||
| Number of children | 2.23 (1.65) | 2.65 (2.05) | 0.241 | ||
| Educational level | 0.109 | ||||
| Below secondary | 48 (96) | 126 (87.5) | |||
| Secondary and above | 2 (4) | 18 (12.5) | |||
| Occupation | 0.603 | ||||
| Farmer/Engineer | 45 (91.8) | 125 (87.4) | |||
| Housewife/student | 4 (8.2) | 18 (12.6) | |||
| Daily expense | 0.328 | ||||
| < 5000 Tanzanian Shillings | 37 (74) | 116 (80.6) | |||
| ≥ 5000 Tanzanian Shillings | 13 (26) | 28 (19.4) | |||
| Household assets ownership | 0.860 | ||||
| Low (0–1) | 33 (68.8) | 95 (67.4) | |||
| High (2+) | 15 (31.3) | 46 (32.6) | |||
| Birth in family within 12 months | |||||
| Women | 25 | 67 | 0.186 | ||
| Herself | 9 (36) | 15 (22.4) | |||
| Others | 16 (64) | 52 (77.6) | |||
| Men | 25 | 77 | 0.140 | ||
| Wife | 10 (40) | 19 (24.7) | |||
| Others | 15 (60) | 58 (75.3) | |||
Primary outcome: BPCR variables
Table 2 shows the ORs of the BPCR variables in the comparison between the intervention group and the control group. The intervention group participants were more likely to know a health center or a hospital in case of emergency (OR: 3.11, 95% CI: 1.39–6.97, p = 0.006), were more likely to arrange someone to accompany them to go to a health center or a hospital for birth or emergency (OR: 2.56, 95% CI: 1.17–5.60, p = 0.019), were more likely to decide their birth place (OR: 3.11, 95% CI: 1.44–6.70, p = 0.004), and attended an antenatal clinic more than four times (OR: 2.39, 95% CI: 1.20–4.78, p = 0.014).
Table 2.
Odds ratios of BPCR variables in the comparison between the intervention group and the control group (n = 194)
| Item | OR | 95% CI | p-value |
|---|---|---|---|
| Knew about the danger signs? | 0.64 | 0.33–1.23 | 0.182 |
| Planned where she would give birth | 0.81 | 0.37–1.76 | 0.593 |
| Planned who would attend birth? | 0.38 | 0.11–1.34 | 0.133 |
| Made arrangement with a nurse, a midwife or a doctor for birth? | 0.81 | 0.39–1.68 | 0.572 |
| Prepared money for childbirth? | 1.60 | 0.66–3.87 | 0.295 |
| Prepared transportation to go to a health center or a hospital before labour and birth | 0.74 | 0.37–1.51 | 0.412 |
| Knew a health center or a hospital in case of emergency | 3.11 | 1.39–6.97 | 0.006** |
| Identified a blood donor for childbirth? | 0.83 | 0.43–1.60 | 0.580 |
| Arranged someone to accompany her to go to a health center or a hospital for birth or emergency | 2.56 | 1.17–5.60 | 0.019* |
| Obtained permission from the head of the household to seek skilled care in the event that a birth emergency occurs in his absence | 1.60 | 0.79–3.23 | 0.190 |
| Arranged a source of household support to provide temporary family care during her absence | 1.13 | 0.50–2.56 | 0.777 |
| Decided the birthplace with someone or by the pregnant women themselves | 3.11 | 1.44–6.70 | 0.004** |
| Attended antenatal clinic more than four times | 2.39 | 1.20–4.78 | 0.014* |
Crude model
* p < 0.05, ** p < 0.01
Secondary outcomes: birth outcome variables
Table 3 shows the ORs of the birth outcome variables in the comparison between the intervention group and the control group when adjusted for sociodemographic variables. The intervention group participants were less likely to have problems such as bleeding or seizures during labour and birth (OR: 0.28, 95% CI: 0.13–0.58, p = 0.001) and less likely to have a Caesarean section (OR: 0.16, 95% CI: 0.07–0.36, p = 0.000). The babies in the intervention group were less likely to have complications (OR: 0.28, 95% CI: 0.13–0.60, p = 0.001). Although it was an important birth outcome variable, there was no significant difference in health facility birth (OR: 1.98, 95% CI: 0.95–4.15, p = 0.064).
Table 3.
Odds ratios of the birth outcome variables in the comparison between the intervention group and the control group (n = 194)
| Item | OR | 95% CI | p-value |
|---|---|---|---|
| Gave birth at a health center or a hospital | 1.96 | 0.96–3.98 | 0.064 |
| Gave birth with an SBA | 1.68 | 0.87–3.25 | 0.123 |
| Had problems such as bleeding or seizure during labour and birth | 0.28 | 0.13–0.58 | 0.001** |
| Had Caesarean section | 0.16 | 0.07–0.36 | 0.000** |
| Baby was alive when born | 2.32 | 0.99–5.44 | 0.052 |
| Baby had complication | 0.28 | 0.13–0.60 | 0.001** |
Crude model
* p < 0.05, ** p < 0.01
As the ‘ANC visit more than 4 times’ is an important factor that affects other outcomes [15, 16], the birth outcome variables were adjusted for ANC visits. Table 4 shows the ORs of the birth outcome variables in the comparison between the intervention group and the control group. The items with statistical significance in Table 3 remained statistically significant after adjustment.
Table 4.
Odds ratios of the birth outcome variables in the comparison between the intervention group and the control group adjusted for ANC visit (n = 194)
| Item | OR | 95% CI | p-value |
|---|---|---|---|
| Gave birth at a health center or a hospital | 1.65 | 0.79–3.48 | 0.185 |
| Gave birth with an SBA | 1.69 | 0.86–3.32 | 0.129 |
| Had problems such as bleeding or seizure during labour and birth | 0.27 | 0.13–0.57 | 0.001** |
| Had Caesarean section | 0.14 | 0.06–0.31 | 0.000** |
| Baby was alive when born | 2.21 | 0.91–5.34 | 0.079 |
| Baby had complication | 0.24 | 0.11–0.55 | 0.001** |
Adjusted for visit to antenatal clinic more than 4 times
* p < 0.05, ** p < 0.01
Discussion
The current study showed that the family-oriented antenatal group education program had a potential significant effect on BPCR, namely, identifying a health facility for emergency, family accompaniment for facility birth, ANC visits, and involvement of women in decision-making as well as maternal/neonatal complications. Firstly, the change in women’s involvement in decision-making for their birthplace had a unique cultural aspect that warrants discussion. In Tanzanian culture, many women lack the decision-making power within the family which hinders their birth preparedness particularly on transportation and birthplace as those require financial preparation [11, 12, 19, 20]. Moshi and Nyamhanga reported that men perceived their role in providing financial support; however, they tended to be less concerned about birthplace because they considered birth as women’s role [21]. Although the Tanzanian Ministry of Health supported the involvement of men in childbirth [22], it has been difficult to involve them in reality owing to traditional roles and lack of knowledge [23–25]. Similarly, though the education of the present study involved husbands and taught them the need of preparation for transportation, there were no statistically significant differences in the actual preparation for transportation despite the fact that women’s involvement in decision-making improved. It suggests emphasizing resource mobilization to men in the education as Moshi and Nyamhanga argued that as long as male partners did not perceive that childbirth contained risks, they did not mobilize financial resources [21]. August et al. suggested potential contributions of community health workers to male involvement from their study in Rufiji and Mkuranga [26]. Additionally, the importance of financial resource mobilization could be supported as Shimamoto and Gipson showed that increase in women’s higher household decision-making power and employment were related to SBA use in Tanzania [27].
Another important aspect of the study was that the intervention group was more likely to attend ANC clinic more than four times. In Tanzania, the rate of ANC attendance for more than four times was still 51% [4]. The number of ANC clinic is important as other study revealed the relationship with neonatal birth outcomes, such as the number of low-birth-weight (LBW) babies, and LBW was associated with stillbirths, low Apgar score, and early neonatal deaths [28]. McMahon et al. reported that birth before arrival of health facility was associated with the low number of ANC visits in rural districts of Morogoro Region [20]. Challaghan-Koru et al. described from their qualitative study in Morogoro that one of the barriers against attending ANC clinic was miscommunication between providers and pregnant women about when and how often they should visit ANC clinic [29]. The success in increasing the number of ANC visits in this study might have been because the education was clear about the number of ANC visits and explained why it was important to visit, i.e., receiving examinations and education from health providers. Oka et al. used the same content and showed the positive effect in communication between healthcare providers and pregnant women [10]. Although facility delivery was not significantly different between two groups in this study, Choe et al. had a congruent result and stated that cultural and family barrier is one of the reason of disconnection between the number of ANC visits and facility delivery in rural Tanzania [30]. As WHO recently changed the number of ANC contacts in the guideline to eight, and they emphasize the importance of women’s positive pregnancy experience, promotion of clear communication between healthcare providers and pregnant women on the number and timing of ANC contacts needs to be continued [31].
Regarding improvement of family members’ accompaniment to health facility, the education had been provided for pregnant women to timely and safely reach a health facility, but it might have influenced quality of care they received at the health facility. Although there was no statistical difference in facility delivery, significant differences were found in self-reported birth complications and Caesarean section between two groups. A Cochrane review showed the continuous support during labor reduced Caesarean section [32]. The intervention group might have had family companion as they are more prepared for family members to accompany pregnant women to health facility. On contrary, Dynes et al.’s study in Kigoma Region reported that clients had significantly greater odds of having a birth companion if they self-reported labor complications (aOR 2.82, 95% CI 1.02–7.81) [33]. However, they discussed that it might be because women having perceptions of risks might request family attendance.
It was also considered that the education could have promoted healthier pregnant lives among the women in the intervention group as the education included nutrition and the appropriate amount of exercise. In fact, the pre-/post-evaluation immediately after the education in the first phase showed significant improvement in understanding nutrition during pregnancy [13]. Promoting healthier pregnancies that reduce the risk of complications is important where human and medical resources are limited, and where transportation is difficult to obtain. For example, maternal deaths in Bangladesh were reduced significantly from 574/100,000 live births in 1990 to 170 in 2013; however, their increase in facility birth rate was limited to 42.1% [34]. According to Alfreen et al., it was estimated that 52% of maternal deaths would have occurred in 2010 in view of the 2001 rates, but these were averted because of decreases in both fertility and risk factors for maternal death [35]. To decrease the high-prevalence risks in Tanzania, such as postpartum hemorrhage and complications related to high blood pressure [5], improving nutrition could be a feasible option. For example, WHO recommends calcium supplementation to avoid hypertensive disorders during pregnancy [36, 37]. A recent study in Tanzania showed that moderate-to-severe anemia (Hb < 90 g/L) was strongly associated with blood loss at birth and the immediate postpartum period, after adjusting for maternal covariates and variables of biological relevance to blood loss [38].
There were several limitations in this study that must be addressed. The convenient sampling might have caused selection bias such that the intervention group participants were more aware of danger signs or healthy pregnant life. As the study was cross sectional, we cannot eliminate potential baseline differences between the groups. The data were all retrieved retrospectively from women and their families, which might have caused recall bias. In addition, as the participants in both the intervention and control groups were from the same villages, cross-contamination of information such as the importance of facility use was possible. In terms of threats to external validity, we collected data in three villages of Korogwe district; therefore, generalizability might be limited when applying the findings to other places.
However, it is equally important to emphasize the key finding and the benefits of the study, that is, the family-oriented antenatal group education program is cost-effective compared with individual counseling or home visits. In the era of SDGs, global health projects are exposed to the question of sustainability [39]. As the present intervention has a potential aspect of sustainability and impact on birth outcomes, the next step is to train local healthcare providers or community health workers to continuously provide this family-oriented antenatal group education for women and their families during pregnancy in villages. This will pave the way for larger studies on BPCR and maternal-infant birth outcomes to be conducted.
Conclusions
This study revealed the potential positive effects of our family-oriented antenatal group education on four BPCR variables: identifying a health facility for emergencies, family accompaniment for facility birth, ANC visits, and involvement of women in decision-making. The outcomes related to maternal and neonatal complications and Caesarean section were fewer in the intervention group. With the identification of the above key factors, male involvement and promotion of healthier pregnant lives should be emphasized in antenatal education in rural Tanzania to reduce birth complications during pregnancy and childbirth.
Acknowledgements
The authors appreciate the contribution of all study participants. Our sincere gratitude goes to Dr. Maimbo Mndolwa, the Bishop of Korogwe who supported us in arranging data collection in the villages. Dr. Sarah E. Porter provided editing on behalf of St. Luke’s International University. We thank Dr. Edward Barroga (http://orcid.org/0000-0002-8920-2607) for the editorial review of the manuscript. The study was funded by the Japan Society for the Promotion of Science, Grant-in-Aid for Young Scientists (B) No. 26861940.
Abbreviations
- ANC
Antenatal Care
- BPCR
Birth Preparedness and Complication Readiness
- LBW
Low-Birth-Weight
- SBAs
Skilled Birth Attendants
- SDGs
Sustainable Development Goals
- TBAs
Traditional Birth Attendants
Authors’ contributions
YS conceptualized and designed of the study. YS, FM, and SL contributed to the provision of the intervention and the acquisition of data. YS and KK participated in data analysis and/or interpretation. YS drafted the first manuscript. SH reviewed and suggested revisions. All authors reviewed and approved the final manuscript.
Authors’ information
YS is a Japanese midwifery researcher who obtained her PhD from the University of Illinois at Chicago, USA. She has been conducting research on maternal child health and midwifery in Tanzania since 2008. She speaks fluent English and Swahili which were necessary for conducting this study. FM and SL are Tanzanian midwifery researchers who provided cultural understanding and language translation for the data collection. KK is a nurse and statistician who provided analytical expertise into the study. SH is a Japanese midwifery professor who has conducted, supervised, and published numerous midwifery research studies across the world, and who currently spearheads many on-going studies in this field.
Funding
The study was funded by the Japan Society for the Promotion of Science, Grant-in-Aid for Young Scientists (B) No. 26861940.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Verbal consent was obtained as the information gathered was unidentifiable and the study risk was minimal. Ethical clearance and permissions were obtained from the 1) responsible person from the first author’s institution; 2) Director of the Korogwe District Council, 3) National Institute for Medical Research, Tanzania, and 4) Tanzania Commission for Science and Technology.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yoko Shimpuku, Email: shimpuku.yoko.5n@kyoto-u.ac.jp.
Frida E. Madeni, Email: fridamadeni@yahoo.co.uk
Shigeko Horiuchi, Email: shigeko-horiuchi@slcn.ac.jp.
Kazumi Kubota, Email: kubotaa@yokohama-cu.ac.jp.
Sebalda C. Leshabari, Email: seolesh@yahoo.com
References
- 1.World Health Organization. WHO recommendations on health promotion interventions for maternal and newborn health. 2015 [cited 2017 Jan 14]. Available from: http://apps.who.int/iris/bitstream/10665/172427/1/9789241508742_report_eng.pdf. [PubMed]
- 2.Soubeiga D, Gauvin L, Hatem MA, Johri M. Birth preparedness and complication readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2014;14:129. doi: 10.1186/1471-2393-14-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Bureau of Statistics (NBS) [Tanzania] and ICF Macro. Tanzania Demographic and Health Survey . Dar es Salaam. Tanzania: NBS and ICF Macro; 2010. p. 2010. [Google Scholar]
- 4.Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF . Tanzania demographic and health survey and malaria Indicator survey (TDHS-MIS) Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF; 2016. pp. 2015–2016. [Google Scholar]
- 5.Butta A, Slevin KW, Barker C, Keahy-Madsen E. Maternal, newborn, and child health in Tanzania: cost and impacts of the One Plan II. The Health Policy Project. 2015 [cited 2017 March 13]. Available from: https://www.healthpolicyproject.com/pubs/666_HPPBriefTanzaniaOnePlanR.pdf.
- 6.Sarker M, Schmid G, Larsson E, Kirenga S, De Allegri M, Neuhann F, et al. Quality of antenatal care in rural southern Tanzania: a reality check. BMC Res Notes. 2010;3(1):209. doi: 10.1186/1756-0500-3-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Magoma M, Requejo J, Campbell OM, Cousens S, Filippi V. High ANC coverage and low skilled attendance in a rural Tanzanian district: a case for implementing a birth plan intervention. BMC Pregnancy Childbirth. 2010. [DOI] [PMC free article] [PubMed]
- 8.Magoma M, Requejo J, Merialdi M, Campbell OM, Cousens S, Filippi V. How much time is available for antenatal care consultations? Assessment of the quality of care in rural Tanzania. BMC Pregnancy Childbirth. 2011. [DOI] [PMC free article] [PubMed]
- 9.Patil CL, Abrams ET, Klima C, Kaponda CPN, Leshabari SC, Vonderheid SC, et al. Centering pregnancy-Africa: a pilot of group antenatal care to address millennium development goals. Midwifery. 2013;29(10):1190–1198. doi: 10.1016/j.midw.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oka M, Horiuchi S, Shimpuku Y, Madeni F, Leshabari S. Effects of a job aid-supported intervention during antenatal care visit in rural Tanzania. International Journal of Africa Nursing Sciences. 2019;10:31–37. doi: 10.1016/j.ijans.2018.11.005. [DOI] [Google Scholar]
- 11.Shimpuku Y, Madeni FE, Horiuchi S, Leshabari SC. Perceptional gaps among women, husbands and family members about intentions for birthplace: a cross-sectional study. Rev Lat Am Enfermagem. 2017;25:e2840. doi: 10.1590/1518-8345.1658.2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tancred T, Marchant T, Hanson C, Schellenberg J, Manzi F. Birth preparedness and place of birth in Tandahimba district, Tanzania: what women prepare for birth, where they go to deliver, and why. BMC Pregnancy Childbirth. 2016;16:165. doi: 10.1186/s12884-016-0945-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shimpuku Y, Madeni F, Horiuchi S, Kubota K, Leshabari S. Evaluation of a family-oriented antenatal group educational program in rural Tanzania: a pre-test/post-test study. Reprod Health. 2018;15(1):117. doi: 10.1186/s12978-018-0562-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mrisho M, Schellenberg JA, Mushi AK, Obrist B, Mshinda H, Tanner M, et al. Factors affecting home delivery in rural Tanzania. Tropical Med Int Health. 2007;12:862–872. doi: 10.1111/j.1365-3156.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- 15.Pembe AB, Urassa DP, Darj E, Carlsted A, Olsson P. Qualitative study on maternal referrals in rural Tanzania: decision making and acceptance of referral advice. Afr J Reprod Health. 2008;12:120–131. [PubMed] [Google Scholar]
- 16.Shimpuku Y, Madeni EF, Horiuchi S, Leshabari SC. Understanding discrepancies of birth preparedness among pregnant women, husbands, and their families in rural Tanzania. International Council of Nurses. Korea: conference Programme. 2015. [Google Scholar]
- 17.Rockers PC, Wilson ML, Mbaraku G, Kruk ME. Source of antenatal care influences facility delivery in rural Tanzania: a population-based study. Matern Child Health J. 2009;13(6):879–885. doi: 10.1007/s10995-008-0412-7. [DOI] [PubMed] [Google Scholar]
- 18.MohanD LFAE, George A, Mpembeni R, Bazant E, Rusibamayila N, Kilewo J, Winch PJ, Baqui AH. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plan. 2017;32(6):791–799. doi: 10.1093/heapol/czx005. [DOI] [PubMed] [Google Scholar]
- 19.August F, Pembe AB, Kayombo E, Mbekenga C, Axemo P, Darj E. Birth preparedness and complication readiness - a qualitative study among community members in rural Tanzania. Glob Health Action. 2015;8:26922. doi: 10.3402/gha.v8.26922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMahon SA, Chase RP, Winch PJ, Chebet JJ, Besana GVR, Mosha I, et al. Poverty, partner discord, and divergent accounts; a mixed methods account of births before arrival to health facilities in Morogoro Region, Tanzania. BMC Pregnancy Childbirth. 2016;16(1):284,016–1058-x. [DOI] [PMC free article] [PubMed]
- 21.Moshi F, Nyamhanga T. Understanding the preference for homebirth; an exploration of key barriers to facility delivery in rural Tanzania. Reprod Health. 2017;14(1):132,017–10397-z. doi: 10.1186/s12978-017-0397-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health. United Republic of Tanzania Ministry of Health and social welfare. The National Road map Strategic Plan to accelerate reduction of maternal. Newborn and child deaths in Tanzania. 2008-2015:1–84.
- 23.August F, Pembe AB, Mpembeni R, Axemo P, Darj E. Men’s knowledge of obstetric danger signs, birth preparedness and complication readiness in rural Tanzania. PLoS One. 2015;10(5):e0125978. doi: 10.1371/journal.pone.0125978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kohi TW, Mselle LT, Dol J, Aston M. When, where and who? Accessing health facility delivery care from the perspective of women and men in Tanzania: a qualitative study. BMC Health Serv Res. 2018;18(1):564,018-3357-6. doi: 10.1186/s12913-018-3357-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.August F, Pembe AB, Mpembeni R, Axemo P, Darj E. Community health workers can improve male involvement in maternal health: evidence from rural Tanzania. Glob Health Action. 2016;9:30064. doi: 10.3402/gha.v9.30064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vermeulen E, Solnes Miltenburg A, Barras J, Maselle N, van Elteren M, van Roosmalen J. Opportunities for male involvement during pregnancy in Magu district, rural Tanzania. BMC Pregnancy and Childbirth. 2016;16:66. doi: 10.1186/s12884-016-0853-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shimamoto K, Gipson JD. The relationship of women’s status and empowerment with skilled birth attendant use in Senegal and Tanzania. BMC Pregnancy Childbirth. 2015;15:154. doi: 10.1186/s12884-015-0591-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kamala BA, Mgaya AH, Ngarina MM, Kidanto HL. Predictors of low birth weight and 24-hour perinatal outcomes at Muhimbili National Hospital in Dar Es Salaam, Tanzania: a five-year retrospective analysis of obstetric records. Pan Afr Med J. 2018;29:220. doi: 10.11604/pamj.2018.29.220.15247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Callaghan-Koru JA, McMahon SA, Chebet JJ, Kilewo C, Frumence G, Gupta S, et al. A qualitative exploration of health workers' and clients' perceptions of barriers to completing four antenatal care visits in Morogoro region, Tanzania. Health Policy Plan. 2016;31(8):1039–1049. doi: 10.1093/heapol/czw034. [DOI] [PubMed] [Google Scholar]
- 30.Choe SA, Kim J, Kim S, Park Y, Kullaya SM, Kim CY. Do antenatal care visits always contribute to facility-based delivery in Tanzania? A study of repeated cross-sectional data. Health Policy Plan. 2016;31(3):277–284. doi: 10.1093/heapol/czv054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. WHO recommendations on antenatal care for positive pregnancy experience. 2016 [cited 2017 Jan 14]. Available from: http://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1. [PubMed]
- 32.Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. John Wiley & Sons, Ltd. 2017. [DOI] [PMC free article] [PubMed]
- 33.Dynes MM, Binzen S, Twentyman E, Nguyen H, Lobis S, Mwakatundu N, et al. Client and provider factors associated with companionship during labor and birth in Kigoma region, Tanzania. Midwifery. 2019;69:92–101. doi: 10.1016/j.midw.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Planning Commission. Bangladesh Progress Report . [cited 2017 Oct 15]. General economics division. 2015. [Google Scholar]
- 35.El Arifeen S, Hill K, Ahsan KZ, Jamil K, Nahar Q, Streatfield PK. Maternal mortality in Bangladesh: a countdown to 2015 country case study. Lancet. 2014;384:1366–1374. doi: 10.1016/S0140-6736(14)60955-7. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. Calcium supplementation during pregnancy to reduce the risk of pre-eclampsia. 2017 [cited 2017 Oct 15]. Available from: http://www.who.int/elena/titles/calcium_pregnancy/en/.
- 37.Omotayo MO, Dickin KL, O’Brien KO, Neufeld LM, De Regil LM, Stoltzfus RJ. Calcium supplementation to prevent preeclampsia: translating guidelines into practice in low-income countries. Adv Nutr. 2016;7:275–278. doi: 10.3945/an.115.010736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kavle JA, Stoltzfus RJ, Witter F, Tielsch JM, Khalfan SS, Caulfield LE. Association between anaemia during pregnancy and blood loss at and after delivery among women with vaginal births in Pemba Island, Zanzibar. Tanzania J Health Popul Nutr. 2008;26:232–240. [PMC free article] [PubMed] [Google Scholar]
- 39.Yang A, Farmer PE, McGahan AM. ‘Sustainability’ in global health. Glob Public Health. 2010;5:129–135. doi: 10.1080/17441690903418977. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.