Abstract
Background:
Partial anterior cruciate ligament (ACL) tears are observed in 10% to 27% of isolated ACL tears. There is currently no consensus on diagnosis and treatment protocols, and the outcomes of nonoperative treatment remain undefined.
Purpose:
To assess the incidence and risk factors for the progression of partial ACL tears to complete ruptures after nonoperative treatment in active patients younger than 30 years.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A total of 41 patients, all younger than 30 years and active in sports, were diagnosed with a partial ACL tear, with no associated meniscal or chondral lesions on magnetic resonance imaging (MRI). All were assigned to a nonoperative treatment program. The Lachman test, ≤4-mm side-to-side difference in laxity by Rolimeter, and MRI were utilized for the diagnosis. Tegner and International Knee Documentation Committee (IKDC) scores were assessed before and after the first lesion, and the Anterior Cruciate Ligament Return to Sport After Injury (ACL-RSI) score was assessed at last follow-up. Postinjury Tegner and IKDC scores were assessed before the second injury for patients progressing to a complete ACL tear and at last follow-up for patients without progression.
Results:
At a mean of 43 months (range, 24-96 months), the partial ACL injury progressed to a complete ACL tear in 16 (39%) patients. In the remaining 25 patients without progression, the mean Tegner and IKDC scores were 7.0 and 96.0 before the injury and 5.9 and 85.7, respectively, at last follow-up. The mean ACL-RSI score was 69.3. The Tegner and IKDC scores were significantly lower at final follow-up (P = .0002 and P < .0001, respectively). Only 18 (44%) patients returned to their preinjury level of sports activities. A significantly increased risk of progression to a complete ACL tear was seen in patients ≤20 years (odds ratio, 5.19; P = .037) or patients practicing pivoting contact sports (odds ratio, 6.29; P = .026). Meniscal lesions were found in 50% of patients with a partial tear that progressed to a complete ACL tear.
Conclusion:
A partial ACL injury progressed to a complete ACL tear in 39% of young active patients treated conservatively, with half of the complete tears presenting with a concomitant meniscal lesion at the time of reconstruction. Age ≤20 years and participation in pivoting contact sports were identified as significant risk factors for progression to a complete tear.
Keywords: anterior cruciate ligament, partial tear, pivoting sport, conservative treatment, meniscal injury
Partial anterior cruciate ligament (ACL) tears have been observed in 10% to 27% of isolated ACL injuries.11,47 There is no consensus on the definition of a partial ACL tear, and there is a lack of consistency in the literature with regard to its treatment. Patients present with moderate anterior knee laxity, a firm but delayed endpoint on the Lachman test, and a pivot glide or no pivot shift.3,47 The definitive diagnosis of a partial ACL tear is provided by arthroscopic surgery14,17,36,47; however, systematic arthroscopic surgery as a diagnostic tool is not feasible or recommended. Several authors have made the diagnosis of a partial ACL tear based on a clinical examination with a focus on establishing whether a firm endpoint exists during Lachman testing, whether an instrumented assessment establishes a side-to-side difference in laxity of less than 4 to 5 mm, and also based on the findings of magnetic resonance imaging (MRI).39,42–44
Conservative treatment is usually reserved for patients with a mean side-to-side difference in laxity of less than 4 or 5 mm as measured by the Rolimeter (Aircast) without a pivot shift.39,41–44 However, there is a high degree of variability with regard to the success rate of this approach in young and very active patients after a partial ACL injury.4,20,27 After 1.5 to 5.3 years of follow-up, partial tears have progressed to complete tears in 14% to 56% of cases with nonoperative management.4,5,11,15 The capacity for spontaneous healing and remodeling after a complete ACL injury is relatively poor.12,21,52 Barrack et al5 compared nonoperative treatment outcomes in partial versus complete ACL tears and found a significantly lower rate of associated meniscal tears and subsequent ACL reconstruction in partial tears, with better clinical scores.
There is no consensus with regard to the surgical treatment of partial ACL tears. Preserving native ACL remnant fibers may provide several theoretical advantages over reconstruction, including preservation of the natural anatomy, physiology, proprioception, vascularity, and mechanoreceptors.1,2,14,28,35,38,40 The purpose of this study was to assess the incidence and risk factors for the progression of partial ACL tears to complete ruptures after nonoperative treatment in young active patients.
Methods
A retrospective analysis of prospectively collected data was performed in patients who underwent nonoperative treatment for a partial ACL tear between October 1, 2008, and June 30, 2014. Approval from an institutional review board was granted before commencement of this study.
The inclusion criteria were age younger than 30 years, a high activity level, and a diagnosis of a partial ACL tear. A high activity level corresponded to regular sports activity (recreational or competitive) and not occasional activity. This could include patients who did not participate in sports/activities with cutting/pivoting. The diagnosis of a partial ACL tear was based on the following:
clinical examination demonstrating a delayed but firm endpoint on the Lachman test,
≤4-mm side-to-side difference in laxity with the Rolimeter without a positive pivot shift,39,42–44
MRI without evidence of a complete ACL tear and primary and/or secondary signs of a partial ACL tear.16 MRI was also performed to assess the articular cartilage and menisci. MRI scans were read by dedicated musculoskeletal radiologists and surgeons with significant experience in reviewing ACL injuries at the time of the first or second (if MRI had not been performed before the first presentation) visit to the clinic.
Patients required at least 12 months of clinical follow-up and at least 24 months of patient-reported outcome data to be included in the study. Exclusion criteria were associated meniscal or chondral lesions at the time of diagnosing the partial ACL tear, a ≥5-mm side-to-side difference in laxity as measured with the Rolimeter, a positive pivot shift, previous surgery to the knee, a contralateral partial or complete ACL tear, concomitant non-ACL ligamentous injuries of either knee, and patients not involved in sports activities.
The type of sport was classified into 3 categories: pivoting contact sport (soccer, rugby, handball, basketball, etc), pivoting sport (tennis, badminton, skiing, etc), and nonpivoting sport (running, swimming, cycling, etc).
All patients followed a standardized rehabilitation protocol. During the first 6 weeks, weightbearing was allowed with the aid of crutches with no brace, and rehabilitation focused on range of motion restoration and progressive quadriceps strengthening. Between 6 weeks and 3 months, there was a progressive increase in the intensity of quadriceps and hamstring strengthening, and a neuromuscular training program was introduced. After 3 months, patients engaged in nonpivoting sports and, after 4 months, pivoting sports.
Patients were assessed with a clinical examination at a minimum of 1 year after the injury. The Lachman test was utilized to assess anterior knee laxity, pivot-shift test was used to assess rotatory knee instability, and side-to-side difference in laxity was measured by the Rolimeter. Furthermore, all patients were contacted to check if they had any new ipsilateral knee symptoms or injuries.
Knee function was examined using the International Knee Documentation Committee (IKDC)24 subjective score, and the level of sport was evaluated with the Tegner score . The Anterior Cruciate Ligament Return to Sport After Injury (ACL-RSI)6 score was obtained to analyze the psychological response to returning to sports after a partial ACL tear.
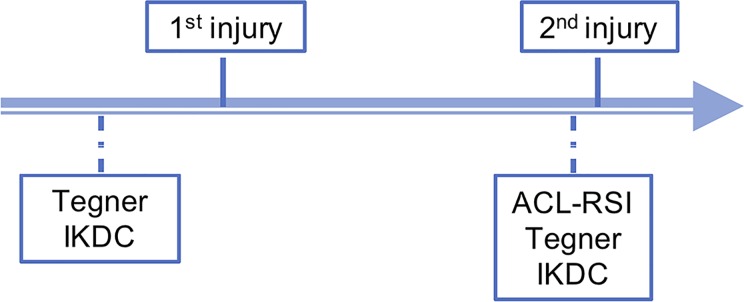
Preinjury Tegner and IKDC scores were obtained at the time of the initial consultation and denoted patients’ baseline activity level. The IKDC score was utilized at final follow-up to establish the resultant knee function. Finally, the ACL-RSI score was established at final follow-up or, if this occurred, at the time before the second injury with progression to a complete ACL tear (Figure 1).
Figure 1.
Timeline of evaluation. ACL-RSI, Anterior Cruciate Ligament Return to Sport After Injury scale; IKDC, International Knee Documentation Committee.
The time between the ACL injury and diagnosis, the type and level of sports activities before and after the injury, the incidence of progression to a complete ACL tear, and any development of cartilaginous and meniscal lesions were recorded. Failure of conservative treatment was defined as knee instability, manifest as a sensation of the knee “giving way,” increased ligamentous laxity on examination, and evidence of knee abnormalities and/or complete ACL tears on MRI.
Statistical Analysis
Descriptive statistics were expressed as means, medians, and standard deviations for continuous data or as frequency counts and percentages for categorical data. Because of the small sample size, nonparametric statistical inference was conducted in this study. Comparisons between patients with a partial ACL tear and those with a complete ACL tear were performed using the Mann-Whitney U test for continuous variables. The Wilcoxon signed-rank test was used for comparisons between “pre and post” partial ACL tears for continuous variables. A backward multivariate logistic regression model was used to identify the factors for the progression of partial ACL tears. The level of significance was set at 5% (α = 0.05), and all tests were 2-tailed. SAS version 9.4 (SAS Institute) was used for all statistical analyses.
Results
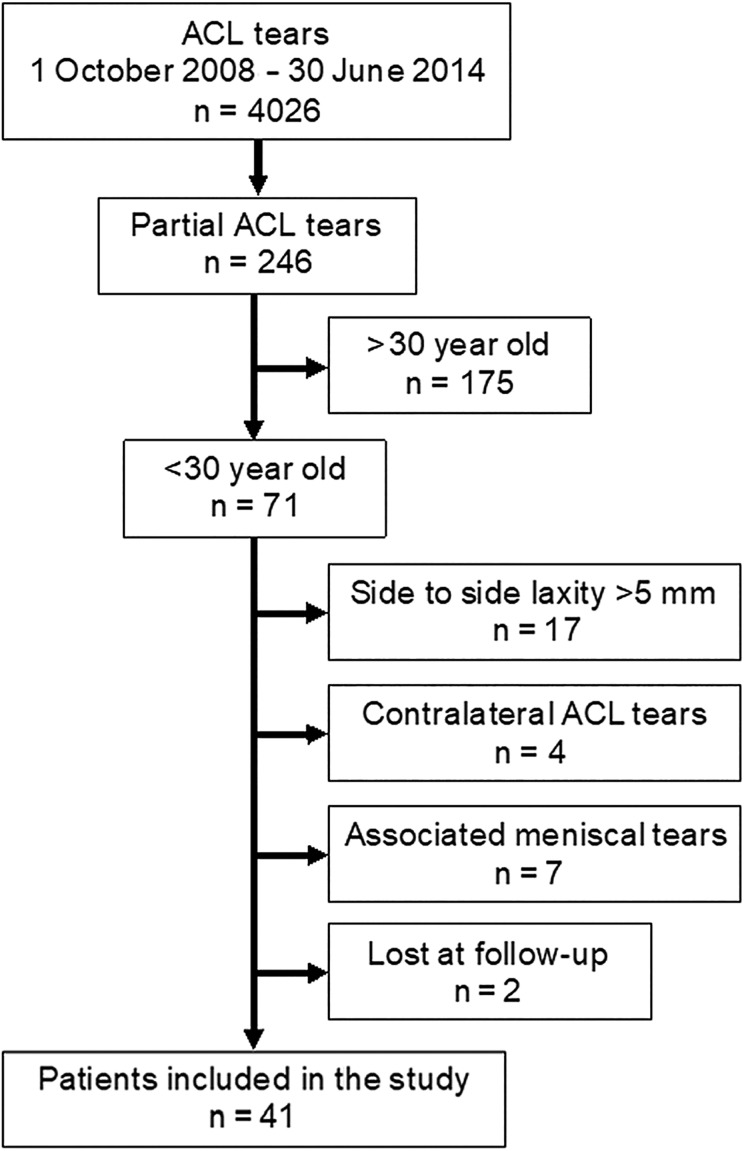
A total of 41 patients satisfied the study criteria and were evaluated for a mean of 43 months (range, 24-96 months) (Figure 2). There were 24 men (59%) and 17 women (41%). The mean age at the time of the ACL tear was 20.6 years (range, 14-28 years). The left knee was injured in 22 patients and the right knee in 19 patients (Table 1). The mean time between the injury and the first consultation was 60 days (range, 2-271 days). The mean side-to-side difference was 2.6 mm (range, 0-4 mm) (Table 2). The diagnosis of partial ACL tears for patients with a side-to-side difference of 0 and 1 mm was made with reference to type of trauma, swelling, and MRI findings.
Figure 2.
Flow chart. ACL, anterior cruciate ligament.
TABLE 1.
Demographic Dataa
| Partial Tear (n = 25) | Complete Tear (n = 16) | Total (N = 41) | |
|---|---|---|---|
| Sex | |||
| Male | 13 (52.0) | 11 (68.8) | 24 (58.5) |
| Female | 12 (48.0) | 5 (31.3) | 17 (41.5) |
| Age, mean (range), y | 21.6 (14-28) | 19.1 (14-27) | 20.6 (14-28) |
| Injured side | |||
| Left | 11 (44.0) | 11 (68.8) | 22 (53.7) |
| Right | 14 (56.0) | 5 (31.3) | 19 (46.3) |
| Type of sport | |||
| Pivoting contact | 10 (40.0) | 12 (75.0) | 22 (53.7) |
| Pivoting | 10 (40.0) | 2 (12.5) | 12 (29.3) |
| Nonpivoting | 5 (20.0) | 2 (12.5) | 7 (17.1) |
aData are presented as n (%) unless otherwise indicated.
TABLE 2.
Side-to-Side Differences by Rolimeter
| Side-to-Side Difference | No. of Patients |
|---|---|
| 0 mm | 2 |
| 1 mm | 1 |
| 2 mm | 19 |
| 3 mm | 8 |
| 4 mm | 11 |
The mean Tegner score was 7.3 (range, 5-10) before the injury and 6.3 (range, 3-10) at last follow-up. Only 18 (44%) patients returned to sports activities at the same level as before the injury (mean Tegner score, 7.4). The mean IKDC score was 96.8 (range, 84-100) before the partial ACL injury and 84.1 (range, 54-100) at last follow-up. Tegner and IKDC scores were significantly lower at final follow-up (P = .0002 and P < .0001, respectively). The mean ACL-RSI score was 69.3 (range, 25-98) (Table 3).
TABLE 3.
Preinjury and Postinjury Scoresa
| Partial Tear (n = 25) | Complete Tear (n = 16) | Total (N = 41) | |
|---|---|---|---|
| Before injury | |||
| Tegner | |||
| n | 24 | 12 | 36 |
| Mean ± SD (range) | 7.0 ± 1.4 (5-10) | 7.9 ± 1.3 (6-10) | 7.3 ± 1.4 (5-10) |
| IKDC | |||
| n | 23 | 12 | 35 |
| Mean ± SD (range) | 96.0 ± 4.0 (84-100) | 98.5 ± 2.9 (90-100) | 96.8 ± 3.8 (84-100) |
| After injury | |||
| Tegner | |||
| n | 23 | 12 | 35 |
| Mean ± SD (range) | 5.9 ± 1.6 (3-8) | 7.0 ± 1.8 (4-10) | 6.3 ± 1.7 (3-10) |
| IKDC | |||
| n | 23 | 12 | 35 |
| Mean ± SD (range) | 85.7 ± 10.0 (69-99) | 80.9 ± 12.4 (54-100) | 84.1 ± 10.9 (54-100) |
| ACL-RSI | |||
| n | 21 | 12 | 33 |
| Mean ± SD (range) | 69.3 ± 19.2 (25-98) | 66.7 ± 15.7 (38-100) | 68.3 ± 17.8 (25-100) |
aACL-RSI, Anterior Cruciate Ligament Return to Sport After Injury; IKDC, International Knee Documentation Committee.
Sixteen (39%) patients progressed to a complete ACL tear at a mean of 20 months (range, 6-43 months), as confirmed with MRI and/or intraoperatively. Thirteen patients underwent ACL reconstruction, and 3 were scheduled for surgery. A complete ACL tear was associated with sports-related trauma in 12 patients (75%; 10 in pivoting contact sports, 1 in skiing, and 1 in cycling) and was atraumatic in 3 patients (19%); in 1 patient (6%), the injury mechanism was unclear. The mean Tegner score in those 16 patients was 7.9 (range, 6-10) before the injury and 7.0 (range, 4-10) before the second injury. The mean ACL-RSI score in this population was 66.7 (range, 38-100) before the second injury (Table 3).
In the group of patients aged ≤20 years (20/41), there was a statistically significantly greater number (odds ratio, 5.19; P = .037) of complete ACL tears than in the older group (21-28 years). The mean Tegner score in this population was 7 (range, 5-10) before the injury and 6 (range, 3-9) at last follow-up. The mean IKDC score was 96 (range, 84-100) before the partial ACL injury and 82 (range, 69-98) at last follow-up. The mean ACL-RSI score in this population was 72 (range, 54-100) at last follow-up. Nine (45%) patients underwent surgery because of failure of nonoperative management. Eight (40%) patients were playing pivoting contact sports, and 6 of them (75%) progressed to a complete ACL rupture (Tables 3 and 4).
TABLE 4.
Predictive Factors for Complete Tear After Nonoperative Treatment
| 95% CI | P | |
|---|---|---|
| Age (at the time of partial tear) | ||
| >20 vs ≤20 y | 0.04-0.84 | .037a |
| Level of sports activity (before partial tear) | ||
| Competition vs training | 0.61-22.47 | .213 |
| Competition vs recreation | 0.53-9.51 | .283 |
| Type of sport | ||
| Pivoting contact vs others | 1.36-38.03 | .026a |
aStatistically significant.
Patients who returned to pivoting contact sports after a partial ACL tear experienced a statistically significant progression to a complete ACL tear (odds ratio, 6.29; P = .026) (Table 4). Patients without progression to a complete ACL tear had significantly lower Tegner scores (mean, 5.9 [range, 3-8]; P = .0002) compared with patients who progressed to a complete ACL tear (mean, 7.0 [range, 4-10]), but they also had a higher Tegner score before the injury (Table 3).
There were no statistically significant differences in sex, anterior laxity (as assessed with the Rolimeter at the time of the first injury), pivot-shift test results, or ACL-RSI scores between those who progressed to a complete tear and those who did not.
Meniscal lesions were found in 50% of patients with a partial tear that progressed to a complete ACL tear. These involved the lateral meniscus in 4 patients, the medial meniscus in 3 patients, and both the lateral and medial menisci in 1 patient (Table 5). Concerning lateral meniscal abnormalities, 4 cases presented with posterior instability, 3 were treated by all-inside suturing (Fast-Fix; Smith & Nephew), and the remaining cases resolved via spontaneous healing; 1 was a complex lesion treated by partial meniscectomy. Concerning the medial meniscus, 4 were ramp lesions, all treated by posteromedial hook sutures. No cartilage lesions were observed in tears that progressed.
TABLE 5.
MRI Findings of Complete Tearsa
| n (%) | |
|---|---|
| MRI performed | |
| Yes | 14/16 (87.5) |
| No | 2/16 (12.5) |
| Cartilage lesion | |
| Yes | 0/14 (0.0) |
| No | 14/14 (100.0) |
| Meniscal tear | 8/16 (50.0) |
| Lateral meniscus | 4/8 (50.0) |
| Medial meniscus | 3/8 (37.5) |
| Both menisci | 1/8 (12.5) |
aMRI, magnetic resonance imaging.
Discussion
The most important finding of the current study was that, in young active patients with partial ACL tears treated nonoperatively, 39% progressed to a complete tear at a mean of 43 months after the first injury. Age ≤20 years and participation in pivoting contact sports were significant predictive factors for failure of conservative treatment, that is, progression to a complete ACL tear. Meniscal lesions were found in 50% of cases that progressed to a complete ACL tear.
The diagnosis of a partial ACL tear remains controversial because there is no single “gold-standard” method, but rather, the diagnosis tends to rely on a combination of findings.11,17,43,47,49 Laxity measurements are very subtle in partial tears. Isberg et al25 found that 50% of KT-1000 arthrometer results led to a false negative finding. That rate improved when the patient was assessed under anesthesia, which is the best situation for evaluating the functional state of the remaining fibers.3,11,31,37 Imaging may reinforce the diagnosis. The Telos device measurement on lateral radiographs have shown a strong correlation with arthroscopic findings.37 MRI may suggest a partial ACL tear, although it has low sensitivity and specificity.1,7,16,23,48,49,54 Van Dyck et al50 suggested that certain axial and perpendicular views are more accurate in making diagnoses based on MRI and can be improved by a 3-T MRI protocol .13,16,46 We agree that a combination of these findings can confirm the diagnosis of a partial ACL tear.16,49 We note that some of our partial tears may have been complete tears, but caution during the pivot-shift examination and Rolimeter testing and possible difficulties interpreting MRI scans may have underdiagnosed these injuries.
Conversely, certain series have suggested that partial tears of the ACL are functionally equivalent to complete tears and that nonoperative management generates poor results.5,11,22,30 Many authors have reported ACL deficiency rates of 14% to 56% after the nonoperative management of partial tears.5,11,17,22,34,49 DeFranco and Bach16 suggested that this discrepancy is caused by variations in the definition of a partial injury of the ACL. These studies evaluated a heterogeneous population of patients in terms of age and meniscal injury status. The current study focused on a relatively homogeneous cohort presenting with a partial ACL tear. All the patients were active in sports and younger than 30 years. Initially, none had associated cartilaginous or meniscal lesions. Despite this homogeneous population, our rate of tear progression was similar to that in previous studies.5,11,17,22,34,49
Noyes et al34 described, in 1989, a high rate of progression from a partial tear to a complete ACL rupture (38%). In 1997, Fritschy et al20 published a study of 43 patients with partial tears in which 41.8% progressed to a complete tear, usually as the result of minor trauma. Bak et al4 reported a lower rate of progression to complete tears (11%) while stating that the best prognosis for ongoing knee function involved the cessation of knee-stressing activities. Barrack et al5 compared partial and complete tears treated nonoperatively and found that overall, the patients with partial tears had better outcomes than those with complete tears, despite a 31% rate of poor results in the partial tear population.
Nonoperative treatment has its particular indications and reasonable results, but the typical patient profile has changed. Patient expectations of long-term sports participation have grown exponentially in tandem with increased longevity. In addition, patients are increasingly aware of how much time they will be out of work or away from their sport and how these time periods may differ between nonoperative and operative approaches.
The current study demonstrated that age ≤20 years and participation in pivoting contact sports are significant predictive factors for failure of the nonoperative treatment of partial ACL tears. Nine patients ≤20 years of age (45%) developed a complete ACL tear and underwent surgery. The Danish registry for knee ligament reconstruction, with 12,193 cases of primary ACL reconstruction, revealed a high rerupture rate in patients under 20 years of age (8.7%) compared with patients older than 20 years (2.8%) after primary ACL reconstruction.30 A study from Ontario, Canada, with 12,967 primary ACL reconstructions in patients aged from 15 to 60 years, showed that patients under 20 years of age had a 5.6% increased risk of ACL reruptures after primary ACL reconstruction.51 Meanwhile, those aged over 20 years had a 2.5% increased risk of reruptures. The same study showed that patients younger than 20 years had a 7.9% increased risk and that patients older than 20 years had a 3.9% increased risk for contralateral ACL ruptures.51 These results trigger the question as to whether it is wise to rush to arthroscopic reconstruction of ACL ruptures and/or partial ACL ruptures in patients under 20 years of age.
The aim of most patients presenting with an ACL lesion is return to sports and ideally at the same level of performance as before the injury. Noyes et al34 did not find any correlation between the Tegner score before and after a partial ACL injury or with progression to complete ligament deficiency. At a mean 7.3-year follow-up, rate of return to sports at the same level was only 12.5% in their cohort.34 Barrack et al5 found that 40% of 35 patients with partial ACL tears were able to return to their preinjury level at a mean follow-up of 41 months. The age at the time of the injury ranged from 15 to 45 years, and the level of sport was not specified.5 Bak et al4 evaluated 56 patients presenting with a partial ACL tear, without associated meniscal or chondral lesions, at a mean follow-up of 5.3 years. Only 30% of patients resumed their preinjury level of activities.4 In the current study, the activities most frequently associated with an ACL injury were pivoting sports, especially skiing, rugby, and soccer. We found a significant decrease in the Tegner score at 24 months after nonoperative treatment for a partial ACL injury. Functional management allowed a return to preinjury level sports in only 44% (n = 18) of the patients. Among those patients ≤20 years of age, only 5 of 20 (25%) were able to return to their preinjury level. The ACL-RSI score analyzes the psychological impact of an ACL tear on return to sports. In the current study, a mean ACL-RSI score of 68 of 100 after a partial ACL tear at 12-month follow-up was observed. These scores may be explained by patient apprehension upon returning to sports. We did not find a significant relationship between the ACL-RSI score and progression to a complete rupture.
These results lead to a discussion about the rehabilitation program for these patients. There is a lack of literature about rehabilitation for partial ACL tears. Among these patients progressing to complete tears, specific rehabilitation and a delayed return to sports should be discussed.
Over the years, many ACL reconstruction techniques have been described, including single-bundle repair, ACL augmentation, ACL reconstruction, and biological approaches. Single-bundle repair is rarely performed for the treatment of partial tears of the ACL because historically this mode of repair has resulted in poor clinical outcomes.29,41 Recently, arthroscopic techniques have improved ACL repair, augmentation, and reconstruction outcomes.18,36 Adachi et al1 performed hamstring and allogenic fascia lata augmentation and stated that ACL augmentation is superior to ACL reconstruction from the viewpoint of proprioception and joint stability because of mechanoreceptor preservation in ACL remnants. In the past decade, an interest in biological approaches has grown progressively, with studies on the healing response,45 cell therapy,8–10 augmentation with growth factors,15,26,32,53 platelet-rich plasma,40 and scaffolds + suture + platelet-rich plasma.19 Biological enhancement of the ACL33 has generated promising preclinical and short-term clinical outcomes, but further studies are necessary to define the role of these approaches in the treatment of partial ACL tears.14
This study has several limitations, including a limited sample size, lack of a control group, and retrospective design with prospectively collected data. There was a lack of a standard definition of a partial tear and no follow-up MRI to assess healing in those without further injuries. Despite these factors, this study cohort was relatively large when considering the incidence of partial ACL injuries. The last follow-up evaluation was conducted by telephone; only 35 of 41 patients provided both IKDC and Tegner scores, and only 33 of 41 patients provided the ACL-RSI score. The strengths of this study include a prospectively populated database and standardized diagnosis, treatment, and rehabilitation protocols.
Conclusion
A partial ACL injury progressed to a complete ACL tear in 39% of young active patients treated nonoperatively. Patient age ≤20 years and participation in pivoting contact sports were identified as significant risk factors for the progression to a complete tear.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.-M.F. is a paid consultant for Arthrex and Newclip Technics. B.S.-C. is a paid consultant for and receives royalties and research support from Arthrex. G.D.d.M.M. has received fellowship support from Arthrex. M.T. is a paid consultant for Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Ramsay-Générale de Santé Comité d’Ethique (#COS-RGDS-2018-11-001-Avis IRB-FAYARD-JM).
References
- 1. Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330–334. [DOI] [PubMed] [Google Scholar]
- 2. Adachi N, Ochi M, Uchio Y, Sumen Y. Anterior cruciate ligament augmentation under arthroscopy: a minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120(3-4):128–133. [DOI] [PubMed] [Google Scholar]
- 3. Araki D, Kuroda R, Matsushita T, et al. Biomechanical analysis of the knee with partial anterior cruciate ligament disruption: quantitative evaluation using an electromagnetic measurement system. Arthroscopy. 2013;29(6):1053–1062. [DOI] [PubMed] [Google Scholar]
- 4. Bak K, Scavenius M, Hansen S, Nørring K, Jensen K, Jørgensen U. Isolated partial rupture of the anterior cruciate ligament long-term follow-up of 56 cases. Knee Surg Sports Traumatol Arthrosc. 1997;5(2):66–71. [DOI] [PubMed] [Google Scholar]
- 5. Barrack RL, Buckley SL, Bruckner JD, Kneisl J, Alexander A. Partial versus complete acute anterior cruciate ligament tears: the results of nonoperative treatment. J Bone Joint Surg Br. 1990;72(4):622–624. [DOI] [PubMed] [Google Scholar]
- 6. Bohu Y, Klouche S, Lefevre N, Webster K, Herman S. Translation, cross-cultural adaptation and validation of the French version of the Anterior Cruciate Ligament-Return to Sport after Injury (ACL-RSI) scale. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1192–1196. [DOI] [PubMed] [Google Scholar]
- 7. Buda R, Di Caprio F, Giuriati L, Luciani D, Busacca M, Giannini S. Partial ACL tears augmented with distally inserted hamstring tendons and over-the-top fixation: an MRI evaluation. Knee. 2008;15(2):111–116. [DOI] [PubMed] [Google Scholar]
- 8. Caplan AI. All MSCs are pericytes? Cell Stem Cell. 2008;3(3):229–230. [DOI] [PubMed] [Google Scholar]
- 9. Caplan AI. Mesenchymal stem cells. J Orthop Res. 1991;9(5):641–650. [DOI] [PubMed] [Google Scholar]
- 10. Caplan AI. Mesenchymal stem cells: the past, the present, the future. Cartilage. 2010;1(1):6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Colombet P, Dejour D, Panisset J-C, Siebold R. Current concept of partial anterior cruciate ligament ruptures. Orthop Traumatol Surg Res. 2010;96(8):S109–S118. [DOI] [PubMed] [Google Scholar]
- 12. Costa-Paz M, Ayerza MA, Tanoira I, Astoul J, Muscolo DL. Spontaneous healing in complete ACL ruptures: a clinical and MRI study. Clin Orthop Relat Res. 2012;470(4):979–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Craig JG, Go L, Blechinger J, et al. Three-Tesla imaging of the knee: initial experience. Skeletal Radiol. 2005;34(8):453–461. [DOI] [PubMed] [Google Scholar]
- 14. Dallo I, Chahla J, Mitchell JJ, Pascual-Garrido C, Feagin JA, LaPrade RF. Biologic approaches for the treatment of partial tears of the anterior cruciate ligament: a current concepts review. Orthop J Sports Med. 2017;5(1):2325967116681724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Date H, Furumatsu T, Sakoma Y, et al. GDF-5/7 and bFGF activate integrin α2-mediated cellular migration in rabbit ligament fibroblasts. J Orthop Res. 2010;28(2):225–231. [DOI] [PubMed] [Google Scholar]
- 16. DeFranco MJ, Bach BR., Jr A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am. 2009;91(1):198–208. [DOI] [PubMed] [Google Scholar]
- 17. Dejour D, Ntagiopoulos PG, Saggin PR, Panisset J-C. The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy. 2013;29(3):491–499. [DOI] [PubMed] [Google Scholar]
- 18. DiFelice GS, van der List JP. Clinical outcomes of arthroscopic primary repair of proximal anterior cruciate ligament tears are maintained at mid-term follow-up. Arthroscopy. 2018;34(4):1085–1093. [DOI] [PubMed] [Google Scholar]
- 19. Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg. 2004;114(6):1502–1508. [DOI] [PubMed] [Google Scholar]
- 20. Fritschy D, Panoussopoulos A, Wallensten R, Peter R. Can we predict the outcome of a partial rupture of the anterior cruciate ligament? A prospective study of 43 cases. Knee Surg Sports Traumatol Arthrosc. 1997;5(1):2–5. [DOI] [PubMed] [Google Scholar]
- 21. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. [DOI] [PubMed] [Google Scholar]
- 22. Fruensgaard S, Johannsen H. Incomplete ruptures of the anterior cruciate ligament. J Bone Joint Surg Br. 1989;71(3):526–530. [DOI] [PubMed] [Google Scholar]
- 23. Hong SH, Choi J-Y, Lee GK, Choi J-A, Chung HW, Kang HS. Grading of anterior cruciate ligament injury: diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. J Comput Assist Tomogr. 2003;27(5):814–819. [DOI] [PubMed] [Google Scholar]
- 24. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 25. Isberg J, Faxèn E, Brandsson S, Eriksson BI, Kärrholm J, Karlsson J. KT-1000 records smaller side-to-side differences than radiostereometric analysis before and after an ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(6):529–535. [DOI] [PubMed] [Google Scholar]
- 26. Kobayashi D, Kurosaka M, Yoshiya S, Mizuno K. Effect of basic fibroblast growth factor on the healing of defects in the canine anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 1997;5(3):189–194. [DOI] [PubMed] [Google Scholar]
- 27. Kocher MS, Micheli LJ, Zurakowski D, Luke A. Partial tears of the anterior cruciate ligament in children and adolescents. Am J Sports Med. 2002;30(5):697–703. [DOI] [PubMed] [Google Scholar]
- 28. Lee BI, Min KD, Choi HS, et al. Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1095–1101. [DOI] [PubMed] [Google Scholar]
- 29. Liljedahl S-O, Lindvall N, Wetterfors J. Early diagnosis and treatment of acute ruptures of the anterior cruciate ligament: a clinical and arthrographic study of forty-eight cases. J Bone Joint Surg Am. 1965;47(8):1503–1513. [PubMed] [Google Scholar]
- 30. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 31. Lorenz S, Imhoff A. Reconstruction of partial anterior cruciate ligament tears. Oper Orthop Traumatol. 2014;26(1):56–62. [DOI] [PubMed] [Google Scholar]
- 32. Madry H, Kohn D, Cucchiarini M. Direct FGF-2 gene transfer via recombinant adeno-associated virus vectors stimulates cell proliferation, collagen production, and the repair of experimental lesions in the human ACL. Am J Sports Med. 2013;41(1):194–202. [DOI] [PubMed] [Google Scholar]
- 33. Murray MM, Fleming BC. Use of a bioactive scaffold to stimulate anterior cruciate ligament healing also minimizes posttraumatic osteoarthritis after surgery. Am J Sports Med. 2013;41(8):1762–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Noyes FR, Mooar LA, Moorman CT, 3rd, McGinniss GH. Partial tears of the anterior cruciate ligament: progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71(5):825–833. [DOI] [PubMed] [Google Scholar]
- 35. Ochi M, Adachi N, Uchio Y, et al. A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(2):117–122. [DOI] [PubMed] [Google Scholar]
- 36. Ouanezar H, Blakeney WG, Fernandes LR, et al. Clinical outcomes of single anteromedial bundle biologic augmentation technique for anterior cruciate ligament reconstruction with consideration of tibial remnant size. Arthroscopy. 2018;34(3):714–722. [DOI] [PubMed] [Google Scholar]
- 37. Panisset J, Duraffour H, Vasconcelos W, et al. Clinical, radiological and arthroscopic analysis of the ACL tear: a prospective study of 418 cases. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8 suppl):362–368. [DOI] [PubMed] [Google Scholar]
- 38. Proffen BL, Sieker JT, Murray MM. Bio-enhanced repair of the anterior cruciate ligament. Arthroscopy. 2015;31(5):990–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pujol N, Colombet P, Potel JF, et al. Anterior cruciate ligament reconstruction in partial tear: selective anteromedial bundle reconstruction conserving the posterolateral remnant versus single-bundle anatomic ACL reconstruction. Preliminary 1-year results of a prospective randomized study. Orthop Traumatol Surg Res. 2012;98(8):S171–S177. [DOI] [PubMed] [Google Scholar]
- 40. Seijas R, Ares O, Cuscó X, Álvarez P, Steinbacher G, Cugat R. Partial anterior cruciate ligament tears treated with intraligamentary plasma rich in growth factors. World J Orthop. 2014;5(3):373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sommerlath K, Odensten M, Lysholm J. The late course of acute partial anterior cruciate ligament tears: a nine to 15-year follow-up evaluation. Clin Orthop Relat Res. 1992;281:152–158. [PubMed] [Google Scholar]
- 42. Sonnery-Cottet B, Barth J, Graveleau N, Fournier Y, Hager J-P, Chambat P. Arthroscopic identification of isolated tear of the posterolateral bundle of the anterior cruciate ligament. Arthroscopy. 2009;25(7):728–732. [DOI] [PubMed] [Google Scholar]
- 43. Sonnery-Cottet B, Colombet P. Partial tears of the anterior cruciate ligament. Orthop Traumatol Surg Res. 2016;102(1):S59–S67. [DOI] [PubMed] [Google Scholar]
- 44. Sonnery-Cottet B, Lavoie F, Ogassawara R, Scussiato RG, Kidder JF, Chambat P. Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):47–51. [DOI] [PubMed] [Google Scholar]
- 45. Steadman JR, Cameron-Donaldson ML, Briggs KK, Rodkey WG. A minimally invasive technique (“healing response”) to treat proximal ACL injuries in skeletally immature athletes. J Knee Surg. 2006;19(1):8–13. [DOI] [PubMed] [Google Scholar]
- 46. Steckel H, Vadala G, Davis D, Musahl V, Fu FH. 3-T MR imaging of partial ACL tears: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1066–1071. [DOI] [PubMed] [Google Scholar]
- 47. Temponi EF, de Carvalho Júnior LH, Sonnery-Cottet B, Chambat P. Partial tearing of the anterior cruciate ligament: diagnosis and treatment. Rev Bras Ortop. 2015;50(1):9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Umans H, Wimpfheimer O, Haramati N, Applbaum YH, Adler M, Bosco J. Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. AJR Am J Roentgenol. 1995;165(4):893–897. [DOI] [PubMed] [Google Scholar]
- 49. Van Dyck P, De Smet E, Veryser J, et al. Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):256–261. [DOI] [PubMed] [Google Scholar]
- 50. Van Dyck P, Vanhoenacker FM, Gielen JL, et al. Three Tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skeletal Radiol. 2011;40(6):701–707. [DOI] [PubMed] [Google Scholar]
- 51. Wasserstein D, Khoshbin A, Dwyer T, et al. Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med. 2013;41(9):2099–2107. [DOI] [PubMed] [Google Scholar]
- 52. Woo SL-Y, Vogrin TM, Abramowitch SD. Healing and repair of ligament injuries in the knee. J Am Acad Orthop Surg. 2000;8(6):364–372. [DOI] [PubMed] [Google Scholar]
- 53. Xie J, Wang C, Huang D-Y, et al. TGF-beta1 induces the different expressions of lysyl oxidases and matrix metalloproteinases in anterior cruciate ligament and medial collateral ligament fibroblasts after mechanical injury. J Biomech. 2013;46(5):890–898. [DOI] [PubMed] [Google Scholar]
- 54. Yao L, Gentili A, Petrus L, Lee JK. Partial ACL rupture: an MR diagnosis? Skeletal Radiol. 1995;24(4):247–251. [DOI] [PubMed] [Google Scholar]