Abstract
Purpose
In this review, we overview the pathophysiology of primary open-angle glaucoma as it relates to the trabecular meshwork (TM), exploring modes of TM dysfunction and regeneration via stem cell therapies.
Recent Findings
Stem cells from a variety of sources, including trabecular meshwork, mesenchymal, adipose and induced pluripotent stem cells, have shown the potential to differentiate into TM cells in vitro or in vivo and to regenerate the TM in vivo, lowering intraocular pressure (IOP) and reducing glaucomatous retinal ganglion cell damage.
Summary
Stem cell therapies for TM regeneration provide a robust and promising suite of treatments for eventual lowering of IOP and prevention of glaucomatous vision loss in humans in the future. Further investigation into stem cell homing mechanisms and the safety of introducing these cells into human anterior chamber, for instance, are required before clinical applications in treating glaucoma patients.
Keywords: trabecular meshwork, glaucoma, regeneration, stem cells, intraocular pressure
Introduction
Primary open-angle glaucoma (POAG) is the second-leading cause of irreversible blindness in the United States, expected to affect upwards of 80 million individuals worldwide by 2020 [1–3]. Glaucoma is a disease damaging retinal ganglion cells and the optic nerve, with subsequent vision loss. Elevated intraocular pressure (IOP) is a major risk factor for glaucoma, which is associated with inefficient outflow of aqueous humor. The trabecular meshwork (TM) is responsible for maintaining a precise IOP by providing proper resistance to aqueous humor outflow. Increased resistance in the TM results in elevated IOP. TM cellularity reduces in aged and glaucoma patients [4–7]. Current treatments aim to reduce IOP via alternative outflow routes or decreasing aqueous humor production, but none targets the trabecular meshwork itself [8]. Using different types of stem cells, including trabecular meshwork stem cells (TMSCs) [9], to repopulate the TM tissue and restore the TM function to reduce IOP has been reported to be a promising method for treating glaucoma [10–17]. Recent studies have shown that regeneration of functional TM tissue via stem cell therapy has special promise as a method of restoring functional TM, reducing IOP, and preventing glaucomatous vision loss.
Anatomy and Function of the TM
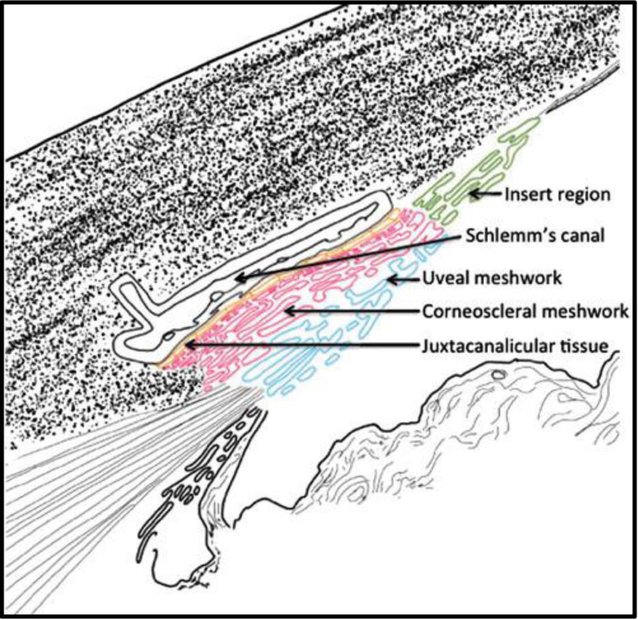
The TM, located at the corner in the anterior chamber and at the junction of the iris and cornea, is the primary area involved in aqueous humor outflow. The TM is comprised of three parts: the uveal meshwork, corneoscleral meshwork, and juxtacanalicular tissue (JCT). The uveal and corneoscleral meshworks filter aqueous humor, while the JCT, made up of loose extracellular matrix (ECM), together with the Schlemm’s canal inner-wall endothelium, is the primary site of outflow resistance and regulation [18]. Cells of the uveal and corneoscleral meshworks display endothelial and phagocytic activity, ridding the eye of oxidative stress and clearing debris before aqueous humor moves further [19]. These cells cover the collagen and elastin networks in order to make a smooth outflow pathway, functioning like both endothelial and phagocytic cells [20, 21]. TM cells of the JCT exhibit fibroblastic and smooth muscle-like qualities, turning over ECM proteins and maintaining the integrity required for adequate IOP [21].
The primary outflow of the aqueous humor is through the trabecular or conventional pathway. Aqueous humor flows through the uveal and corneoscleral meshworks of the TM, where debris is collected before passage through the JCT and Schlemm’s canal, exiting through the aqueous veins [20, 22]. TM cells in the JCT region and Schlemm’s canal endothelial cells serve to regulate outflow of this filtered aqueous humor [21]. This pathway is pressure-driven, with aqueous humor moving down a pressure gradient via bulk flow [23]. Given this, flow of aqueous humor is unequally distributed across the TM, also called segmental outflow, which has both high and low flow areas [24, 25].
Understanding the mechanisms of this segmental outflow and how the high flow and low flow areas change is an area of research for developing more targeted and effective treatments for glaucoma.
The uveoscleral or unconventional outflow pathway moves aqueous humor through the uvea, ciliary body and muscle into the sclera and choroid [26, 27]. The TM responds to changing pressure by initiating a homeostatic response, recycling the ECM and restoring adequate IOP. Dysfunction of this mechanism can result in elevated IOP as well [22].
Pathology and Pathophysiology of the TM in Glaucoma
The primary cause of elevated IOP and subsequent optic nerve damage is due to dysregulation of the trabecular pathway. This can occur in several ways. Increased age is one of the primary risk factors for glaucoma; increased apoptosis and senescence of TM cells have proven to correspond with increased IOP [28, 29]. TM cell loss with age corresponds with elevated IOP [4]. Loss of phagocytic function in TM cells also decreases outflow capacity and increases IOP [30]. In glaucoma patients, increased fusion of the trabecular beams, linkages found in the uveal meshwork, results from adhesion between degraded beams. This fusion and thickening due to loss of cellularity increases outflow resistance and IOP [7]. TM stiffness is positively related to increased outflow resistance and increased IOP [31].
The TM is also responsible for degradation and synthesis of the ECM, recycling it in order to maintain the homeostasis and prevent stiffness and crosslinking [14]. Cytoskeleton rearrangements of the TM increase IOP via increased actin cross-links, stiffening the TM and reducing outflow. Additionally, increased ECM deposition and interactions between the ECM and cytoskeleton may also increase IOP [20]. Loss of cellularity in the TM and lack of outflow surface area are also contributing factors to reduced aqueous humor outflow [7].
Other reasons for TM degradation have been implicated. Oxidative stress has been studied as a factor reducing TM function and increasing damage on the retinal ganglion cells and optic nerve. The lack of an antioxidant mechanism of TM cells leads to an accumulation of oxidative damage, especially within the mitochondria of the TM cells. These damages to TM mitochondria alter mtDNA, which then results in a greater accumulation of reactive oxygen species. The damage leads to apoptosis and increased autophagy, resulting in TM cell loss, rearrangement, and elevated IOP [32–34].
Current Treatment Options
The pathophysiology of glaucoma renders it challenging to treat effectively. While the TM is the primary site of dysfunction in glaucoma, it is difficult to treat directly. For many years, medical treatment of glaucoma has been limited to increase aqueous humor outflow via the uveoscleral pathway, or decrease aqueous humor production. The prostaglandin agonists are the most widely prescribed drugs for glaucoma [8]. These drugs target the unconventional pathway via ECM remodeling to increase aqueous humor outflow [35]. Non-prostaglandin drug classes, such as beta antagonists, alpha agonists and carbonic anhydrase inhibitors, decrease aqueous humor production hence reducing IOP [8]. Drugs targeting the conventional outflow pathway, including the TM, Schlemm’s canal and distal vessels are needed. Two novel drug classes, nitric oxide agonists and Rho kinase inhibitors target directly to the conventional outflow pathway [36]. Latanoprostene bunod, a novel nitric oxide-donating prostaglandin F2α analogue, reduces IOP by increasing both non-conventional and conventional outflow [36–38]. It relaxes TM cells and decreases TM cellular volume to increase aqueous humor outflow[36].
Rho-associated kinase (ROCK) inhibitors are a relatively new class of therapy shown to lower IOP by directly targeting the conventional pathway, relaxing cells in the TM and altering ECM organization [39–42]. Some new eye drops, Netarsudil and Ripasudil, have been developed and show promising results in reducing IOP ex vivo, in vivo in animals, and in clinical trials [43–49]. Currently two new ocular hypotensive agents has been approved and commercially available for clinical use: Rhopressa (netarsudil ophthalmic solution) 0.02% is the first FDA-approved ROCK inhibitor for improving TM outflow and reducing IOP; GLANATEC (Ripasudil hydrochloride hydrate) ophthalmic solution 0.4% is also a ROCK inhibitor that has been launched in Japan for IOP reduction.
These treatments, alongside laser trabeculoplasty and surgical approaches to shunt aqueous humor away from the TM, comprise the current scope of first-line treatments for glaucoma [50–52].
Trabecular Meshwork Regeneration by TM Stem Cells
Because the TM is the primary site of outflow resistance and reduced cellularity is associated with elevated IOP, treatments that aim to restore TM cellularity and/or function would be optimal in reducing IOP and preventing glaucomatous vision loss. Given the immune privileged status of the eye, stem cell therapies for treatment of glaucoma and other ophthalmological diseases show particular promise [50, 53–56]. Are there stem cells in situ for TM regeneration? Can they be activated in vivo or isolated and expanded in vitro? In 1982, it was first shown that the Schwalbe’s line cells, also called insert cells, were morphologically different from the rest of the TM cells [57].
Repopulation and restoration of TM function after laser trabeculoplasty and observation of progenitor cell colonies in the TM led to the hypothesis that stem cells exist in the TM [58, 59]. BrdU label-retaining cells detected in the insert region in monkeys [60] and mice [14] confirmed the slow-cycling, label-retaining stem cells existing in the TM within a specific niche (Figure 1).
Figure 1.
Illustration of the TM structure. Insert region (green, nonfilter region) is between the TM and the corneal endothelium. The TM consists of uveal meshwork (blue), corneoscleral meshwork (red), and JCT (yellow). JCT, juxtacanalicular tissue; TM, trabecular meshwork. Reprinted with permission from J Ocul Pharmacol Ther. Volume 32, Yun et al.14 published by Mary Ann Liebert, Inc., New Rochelle, NY.
These trabecular meshwork stem cells (TMSCs) have been isolated and identified via various methods, from flow cytometry to immunostaining [9, 61–64]. They have been shown to be multipotent, capable of differentiation into neurons, adipocytes, and corneal keratocytes [9, 65, 66]. In the presence of fetal bovine serum, TMSCs differentiate into TM cells, suggesting that differentiation into TM cells is the default lineage, and the TMSCs are a unique subset of stem cells, distinct from ordinary mesenchymal stem cells. Positive staining for TM cell-specific markers have shown that TMSCs differentiate into phagocytic TM cells when cultured in either aqueous humor or serum [9].
TMSCs have the ability to actively home to the TM region after injection into normal mouse anterior chamber [10]. Interestingly, the TMSCs specifically homed and integrated to laser-damaged TM region, where they are needed for regeneration [17]. The cells integrated into the TM tissue, appearing in all the cell layers of the TM, and some of them differentiated into functional TM cells expressing TM cell markers AQP1 and CHI3L1. At the same time, some of those cells still maintained their stemness characteristics, expressing stem cell markers and remained slow-cycling. This ensures the stem cell pool with the ability for self-renewal and long-term regeneration.
Trabecular Meshwork Regeneration by Other Types of Stem Cells
Since stem cells are characterized by their multipotency and plasticity, both bone marrow-derived mesenchymal stem cells (MSCs) and adipose-derived stem cells (ADSCs) have also been shown to differentiate into TM-like cells and reduce IOP after in vivo transplantation [11, 13, 67]. Induced pluripotent stem cells (iPSCs) have been induced to differentiate into TM-like cells responsive to dexamethasone treatment and acquiring phagocytic function [68, 12]. These iPSC-TM-like cells have been shown to reduce IOP by repopulating the TM and increasing cell proliferation and migration of the eye’s internal pool of TMSCs [12, 15, 16]. The application of iPSC-TM-like cells is especially promising in the cases where th e immune privilege of the eye is imperfect. Using patients’ own autologous cells, such as skin fibroblasts, after reprogramming to generate iPSCs and differentiating into TM-like cells, provides a potential method in individualized, effective treatment for glaucoma. TM-like cells must be verified following the guidelines [69] to have the characteristics of primary TM cells, such as being responsive to dexamethasone treatment with increased expression of myocilin.
Glaucoma animal models for trabecular meshwork regeneration
The development of animal models that mimic human glaucoma pathophysiology has been an evolving and necessary area for the development of stem cell therapies for glaucoma. Ideally, these models should display all of the hallmarks of POAG: long-term increased IOP, reduced TM cellularity, an open iridocorneal angle and eventually retinal ganglion cell loss. Several models have been developed that adequately exhibit these traits.
Laser photocoagulation has been the standard in elevating IOP in rats and mice since 2002, and is a frequently used method [70–72]. However, the majority of these laser-based treatments alter outflow pathway morphology in exchange for long-term IOP elevation. A more recently developed technique has proven effective in providing a long-term increase in IOP without a loss of native morphology of the conventional outflow pathway, providing a more useful model of POAG and a more specific way of testing the effectiveness of regenerative stem cell therapies [23] [73].
The genetic basis of glaucoma has also been manipulated to provide useful animal models. Myocilin, a gene of unknown function, is often implicated in cases of glaucoma, with over 43 different mutations found in glaucoma patients [74]. The myocilin gene, MYOC, encodes a protein of undetermined function that is highly presented in the TM and secreted into the aqueous humor of the eye. Mutations in MYOC are the most common genetic cause of POAG, accounting for almost 4% of all cases. The Y437HMYOC mutation is responsible for elevated IOP primarily in the second decade of life, and was used to generate Tg-MYOCY437H transgenic mice. These mice proved a useful model for POAG, displaying elevated IOP, loss of retina ganglion cells and optic nerve function. The mouse model is suitable for studying TM repair and regeneration from glaucomatous damage [75].
Another genetic target for generating model organisms with elevated IOP involves connective tissue growth factor (CTGF). CTGF is a target gene of transforming growth factor TGF-β2, which is found circulating in the aqueous humor and affects over 50% those with POAG. High CTGF expression results in contractile activity within the actinmyosin cytoskeleton of the TM, rendering it overly stiff and less efficient in aqueous humor outflow. Generation of transgenic mice overexpressing CTGF [76] showed higher CTGF levels in the TM and elevated IOP in vivo, and strongly supported morphological changes in the ECM as the cause of the raised IOP. Most importantly, this model was found to be responsive to Rho kinase inhibitors, which provided a noticeable and reversible decrease in IOP. This finding is especially important, as it solidifies this model as the most accurate mimic of human POAG to date, as other models either deal with alternative forms of glaucoma (DBA/2J mice for secondary angle closure, for example) or are not as widely relevant to POAG (MYOC mutations only account for 4% of POAG cases, and mutant myocilin increases IOP via an unknown mechanism) [75]. This model shows special promise by reacting favorably with current first-line glaucoma therapies, and will serve as a useful model for more detailed studies of both the mechanisms of IOP increase in POAG and the potential effects of novel glaucoma therapies [76].
A recent developed dex-induced mouse model [77, 78] shows the mouse TM cells encounter ER stress and the mice had increased IOP. The model should be another suitable mouse model for studying TM regeneration using stem cells.
Several studies have shown that stem cell therapies prove effective in lowering IOP in various different models (Table 1). Mesenchymal stem cells (MSCs) have been shown to lower IOP in mice with laser-induced IOP elevation [11]. Injection of bone marrow cells, among which MSCs exist, has proved effective in homing to the site of injury, reducing IOP and increasing aqueous humor outflow. MSCs did not differentiate to TM cells in vitro and were cleared within 96 hours in vivo, after proposed apoptosis and phagocytosis by ocular microglia. However, in this short time, they proved to assist in long-term repair well beyond their time of clearance through secretion of paracrine factors, recruiting endogenous progenitor cells to the TM to restore cellularity and function. Further investigation regarding both the nature of the paracrine factors released from stem cell and the exact mechanisms of stem cell recruitment is necessary in order to advance the possibility of MSCs as a cell therapy source for TM regeneration and IOP reduction [56, 11].
Table 1.
Ex vivo and in vivo studies on trabecular meshwork regeneration
| Studies | Cell species | Inj Cell# | Volume | animal | model | Observing period | References |
|---|---|---|---|---|---|---|---|
| TMSCs | human | 5×104 | 2ul | mouse | WT | 3 months | Du 201310 |
| MSC | mouse | 1×106 | 10ul | rat | laser | 35 days | Manuguerra-gagne 201311 |
| iPSCs | Human | 3×105 | Human anterior segment | Saponin depletion | Several days | Abu-Hassan 201512 | |
| MSC | rat | 5×105 | 6ul | rat | Episcleral vein cauterization | 25 days | Roubeix 201513 |
| iPSC-TM | mouse | 5×104 | 3ul | mouse | Tg-MYOCY437H | 9 weeks | Zhu 201615 |
| iPSC-TM | mouse | 5×104 | 3ul | mouse | Tg-MYOCY437H | 12 weeks | Zhu 201716 |
| TMSCs | human | 5×104 | 2ul | mouse | laser | 4 weeks | Yun Comm Bio 201817 |
Ex vivo experiments were performed using perfused human outflow pathway organ culture have shown iPSC-TM-like cells are effective in restoring the TM homeostasis and lowering IOP. Human and porcine anterior segment cultures were treated with saponin, effectively reducing TM cellularity and eliminating the TM’s homeostatic response to pressure elevation. Cultured TM cells from human and porcine donors were added to these perfused cultures, and were shown to restore the homeostatic pressure response upon integration into the TM [12].
iPSC-derived TM-like cells were shown to decrease IOP upon injection into transgenic mice expressing a pathogenic mutation, Y437H, in the human myocilin gene (Tg-MYOCY437H) [15]. In this experiment, transgenic mice exhibited elevated IOP and reduced TM cellularity. Injection of iPSC-TM-like cells showed improved outflow facility and increased TM cellularity from endogenous cells when compared to a control [15,16]. IOP elevation and retinal ganglion cell reduction was prevented in these Tg-MYOCY437H mice after iPSC-TM-like cell injection at 9 weeks [15] and 12 weeks [16].
Mechanisms of Trabecular Meshwork Regeneration
Stem cell therapies help alleviate elevated IOP by repopulating and restoring function to the TM. So far, all the in vivo results are in animals with intracameral injection. Upon injection into the anterior chamber, cells have the opportunity to connect and attach to the surface of the tissues including the corneal endothelium, the iris, the lens epithelium, the ciliary body processes and the TM. Our group shows that human TMSCs actively homed to the TM region after injection while fibroblasts attached to other tissues as well as to the TM by passively following the aqueous humor outflow [10, 17]. TMSCs also selectively homed to laser-damaged TM region for repairing [17].
While the entire mechanisms of this localization is unknown, there is evidence of TMSC homing to the TM after photocoagulation and the role of chemokines in this response [17]. Chemokine CXC-type receptor 4 (CXCR4) is a G-protein coupled receptor, proven (alongside stromal derived factor 1 or SDF1) to play roles in organogenesis, vascularization, and homing of hematopoietic stem cells [56, 79, 80]. In vivo experiments with a primate model proved that a CXCR4 agonist (ATI-2341) increased mobilization of hematopoietic stem cells, establishing CXCR4 as a therapeutic target [80]. Given its ubiquity as a proven mobilizer of stem cells, the mechanism by which CXCR4/SDF1 drives stem cell homing has been predicted to affect TMSCs as well.
The roles of the CXCR4/SDF1 chemokine axis in TMSC homing was recently explored in vitro and in vivo [17]. Examination of CXCR4 and SDF1 levels showed higher CXCR4 levels in passaged human TM cells and higher SDF1 levels in differentiated TM cells. SDF1 was shown to increase both affinity and chemotaxis between TMSCs and TMs in vitro; treatment with CXCR4 antagonists AMD3100 or IT1t almost completely eliminated this effect. Human TMSCs were injected into the anterior chamber of C57BL/6 mice after 180° laser photocoagulation on the TM. At two and four weeks after injection, TMSCs were found to reconstruct the TM, suppressing the inflammatory response and preventing fibrosis. The CXCR4/SDF1 axis was shown to be just one of potentially many moving parts involved in TMSC homing, and interactions from cadherins, integrins, and the ECM are likely contributors requiring further study. The success of a TMSC xenotransplantation into mice combined with new evidence towards the TMSC homing mechanism further supports the promise of TMSC incorporation as an effective regenerative therapy [17].
The homed cells integrated into TM tissue and increased TM cellularity [15–17]. What the exact effects of the replenished cells are and how TM homeostasis is recovered and remained exert need further studies.
Challenges in Trabecular Meshwork Regeneration
The stem cell homing process is multifactorial, involving elements from both the immune response in addition to cadherins and integrins. Understanding the details of this mechanism will lead to more accurate troubleshooting of the TMSC repair process and an array of possible sites for therapeutic intervention in order to more effectively reduce IOP in vivo [17].
Additionally, several of the issues plaguing all ocular regenerative therapies apply to TM regeneration. Though not a current issue, immune response to allotransplantation of TMSCs into human subjects appears to be one of the primary concerns for effective human treatment in the future. More accurate cell characterization, especially as human TMSC banks expand, will be crucial in ensuring consistency and efficacy in future human transplantation. Establishing preclinical studies will be the first step towards addressing these concerns and moving towards stem cell therapies that are safe and effective options for the treatment of glaucoma [81].
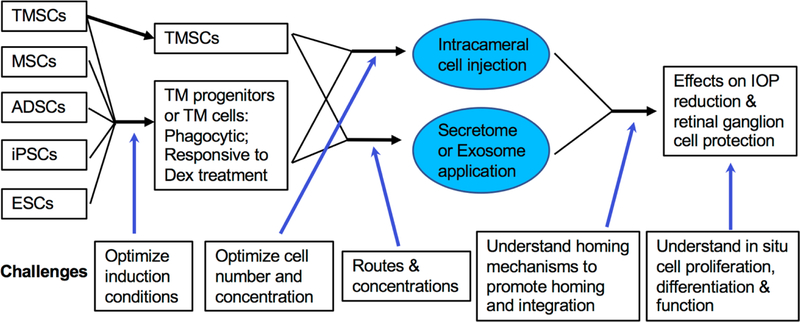
Furthermore, increased evidence has shown that the exosome or secretome from stem cells have regenerative effects [82–85]. Recently studies indicate that small extracellular vesicles/exosomes from mesenchymal stem cells protect retinal ganglion cells in optic nerve crush rat models [86] and in glaucoma animal models [87, 88]. Stem cell-free therapies for TM regeneration for glaucoma are in need for further exploration. The current processes of stem cells and animals with the challenges are listed in Figure 2.
Figure 2.
Schematics of the trabecular meshwork regeneration using stem cells and the challenges.
Conclusion
TM remains a very promising area of interest for further development for stem cell-based therapies. The advent of iPSCs, TMSCs, and other stem cell technologies have enabled a breadth of new possibilities for potential treatment for glaucoma. Recent efforts in establishing model organisms, differentiating progenitor cells into TM cells, and evidence of TM regeneration both ex vivo and in vivo have provided a robust platform for further work, making the ideal of TMSC regeneration as a safe and effective method of treatment for glaucoma ever closer to reality.
Acknowledgments
This work was supported by NIH grants EY025643 (Y.D.) and P30-EY008098; Eye and Ear Foundation (Pittsburgh, PA); Research to Prevent Blindness;
University of Pittsburgh Summer Premedical Academic Enrichment Program (SPAEP) (A.C.).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Author Disclosure Statement
Alexander Castro declares that he has no conflicts of interest.
University of Pittsburgh owns a patent “trabecular meshwork stem cells” with Yiqin Du as one of the inventors.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwon YH, Fingert JH, Kuehn MH, Alward WL. Primary open-angle glaucoma. N Engl J Med. 2009;360(11):1113–24. doi: 10.1056/NEJMra0804630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook C, Foster P. Epidemiology of glaucoma: what’s new? Can J Ophthalmol. 2012;47(3):223–6. doi: 10.1016/j.jcjo.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Alvarado J, Murphy C, Juster R. Trabecular meshwork cellularity in primary open-angle glaucoma and nonglaucomatous normals. Ophthalmology. 1984;91(6):564–79. [DOI] [PubMed] [Google Scholar]
- 5.Grierson I, Howes RC. Age-related depletion of the cell population in the human trabecular meshwork. Eye (Lond). 1987;1 (Pt 2):204–10. doi: 10.1038/eye.1987.38. [DOI] [PubMed] [Google Scholar]
- 6.Gabelt BT, Kaufman PL. Changes in aqueous humor dynamics with age and glaucoma. Prog Retin Eye Res. 2005;24(5):612–37. doi: 10.1016/j.preteyeres.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Gong HSD. The histopathological changes in the trabecular outflow pathway and their possible effects on aqueous outflow in eyes with primary open-angle glaucoma In: Samples PAKJR, editor. Glaucoma Research and Clinical Advances 2016–2018 Kugler; Amsterdam: 2016. p. 17–40. [Google Scholar]
- 8.Kopczynski CC, Epstein DL. Emerging trabecular outflow drugs. J Ocul Pharmacol Ther. 2014;30(2–3):85–7. doi: 10.1089/jop.2013.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Du Y, Roh DS, Mann MM, Funderburgh ML, Funderburgh JL, Schuman JS. Multipotent stem cells from trabecular meshwork become phagocytic TM cells. Invest Ophthalmol Vis Sci. 2012;53(3):1566–75. doi: 10.1167/iovs.11-9134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du Y, Yun H, Yang E, Schuman JS. Stem cells from trabecular meshwork home to TM tissue in vivo. Invest Ophthalmol Vis Sci. 2013;54(2):1450–9. doi: 10.1167/iovs.12-11056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manuguerra-Gagne R, Boulos PR, Ammar A, Leblond FA, Krosl G, Pichette V et al. Transplantation of mesenchymal stem cells promotes tissue regeneration in a glaucoma model through laser-induced paracrine factor secretion and progenitor cell recruitment. Stem Cells. 2013;31(6):1136–48. doi: 10.1002/stem.1364. [DOI] [PubMed] [Google Scholar]
- 12.**.Abu-Hassan DW, Li X, Ryan EI, Acott TS, Kelley MJ. Induced pluripotent stem cells restore function in a human cell loss model of open-angle glaucoma. Stem Cells. 2015;33(3):751–61. doi: 10.1002/stem.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows that exogenous TM-like cells derived from iPSC restored the TM function in an ex vivo tissue perfusion model.
- 13.Roubeix C, Godefroy D, Mias C, Sapienza A, Riancho L, Degardin J et al. Intraocular pressure reduction and neuroprotection conferred by bone marrow-derived mesenchymal stem cells in an animal model of glaucoma. Stem Cell Res Ther. 2015;6:177. doi: 10.1186/s13287-015-0168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.**.Yun H, Zhou Y, Wills A, Du Y. Stem Cells in the Trabecular Meshwork for Regulating Intraocular Pressure. J Ocul Pharmacol Ther. 2016;32(5):253–60. doi: 10.1089/jop.2016.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study illustrated the characteristics of trabecular meshwork stem cells and their niche as well as other stem cells types for TM regeneration and suitable animal models for studying stem cell-based therapies.
- 15.***.Zhu W, Gramlich OW, Laboissonniere L, Jain A, Sheffield VC, Trimarchi JM et al. Transplantation of iPSC-derived TM cells rescues glaucoma phenotypes in vivo. Proc Natl Acad Sci U S A. 2016;113(25):E3492–500. doi: 10.1073/pnas.1604153113. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows that iPSC-derived TM cells prevented IOP elevation in a mouse glaucoma model and prevented retinal ganalion cell loss. It indicates that stem cel-based therapy is feasible for TM regeneration and preventing vision loss in glaucoma.
- 16.Zhu W, Jain A, Gramlich OW, Tucker BA, Sheffield VC, Kuehn MH. Restoration of Aqueous Humor Outflow Following Transplantation of iPSC-Derived Trabecular Meshwork Cells in a Transgenic Mouse Model of Glaucoma. Invest Ophthalmol Vis Sci. 2017;58(4):2054–62. doi: 10.1167/iovs.16-20672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.***.Yun H, Wang Y, Zhou Y, Wang K, Sun M, Stolz DB et al. Human stem cells home to and repair laser-damaged trabecular meshwork in a mouse model. Commun Biol. 2018;1:216. doi: 10.1038/s42003-018-0227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows that human trabecular meshwork stem cells can successfully home to laser-damaged TM region and repair the damage tissue. It also explored the stem cell homing and regeneration mechanisms.
- 18.Keller KE, Acott TS. The Juxtacanalicular Region of Ocular Trabecular Meshwork: A Tissue with a Unique Extracellular Matrix and Specialized Function. J Ocul Biol. 2013;1(1):3. [PMC free article] [PubMed] [Google Scholar]
- 19.Chhunchha B, Singh P, Stamer WD, Singh DP. Prdx6 retards senescence and restores trabecular meshwork cell health by regulating reactive oxygen species. Cell Death Discov. 2017;3:17060. doi: 10.1038/cddiscovery.2017.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bermudez JY, Montecchi-Palmer M, Mao W, Clark AF. Cross-linked actin networks (CLANs) in glaucoma. Exp Eye Res. 2017;159:16–22. doi: 10.1016/j.exer.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.***.Stamer WD, Clark AF. The many faces of the trabecular meshwork cell. Exp Eye Res. 2017;158:112–23. doi: 10.1016/j.exer.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study points the different types of trabecular meshwork cells and their characteristics.
- 22.Acott TS, Kelley MJ, Keller KE, Vranka JA, Abu-Hassan DW, Li X et al. Intraocular pressure homeostasis: maintaining balance in a high-pressure environment. J Ocul Pharmacol Ther. 2014;30(2–3):94–101. doi: 10.1089/jop.2013.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yun H, Lathrop KL, Yang E, Sun M, Kagemann L, Fu V et al. A laser-induced mouse model with long-term intraocular pressure elevation. PLoS One. 2014;9(9):e107446. doi: 10.1371/journal.pone.0107446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vranka JA, Bradley JM, Yang YF, Keller KE, Acott TS. Mapping molecular differences and extracellular matrix gene expression in segmental outflow pathways of the human ocular trabecular meshwork. PLoS One. 2015;10(3):e0122483. doi: 10.1371/journal.pone.0122483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang JY, Folz SJ, Laryea SN, Overby DR. Multi-scale analysis of segmental outflow patterns in human trabecular meshwork with changing intraocular pressure. J Ocul Pharmacol Ther. 2014;30(2–3):213–23. doi: 10.1089/jop.2013.0182. [DOI] [PubMed] [Google Scholar]
- 26.Pederson JE, Toris CB. Uveoscleral outflow: diffusion or flow? Invest Ophthalmol Vis Sci. 1987;28(6):1022–4. [PubMed] [Google Scholar]
- 27.Johnson M, McLaren JW, Overby DR. Unconventional aqueous humor outflow: A review. Exp Eye Res. 2017;158:94–111. doi: 10.1016/j.exer.2016.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baleriola J, Garcia-Feijoo J, Martinez-de-la-Casa JM, Fernandez-Cruz A, de la Rosa EJ, Fernandez-Durango R. Apoptosis in the trabecular meshwork of glaucomatous patients. Mol Vis. 2008;14:1513–6. [PMC free article] [PubMed] [Google Scholar]
- 29.Liton PB, Challa P, Stinnett S, Luna C, Epstein DL, Gonzalez P. Cellular senescence in the glaucomatous outflow pathway. Exp Gerontol. 2005;40(8–9):745–8. doi: 10.1016/j.exger.2005.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang X, Ognibene CM, Clark AF, Yorio T. Dexamethasone inhibition of trabecular meshwork cell phagocytosis and its modulation by glucocorticoid receptor beta. Exp Eye Res. 2007;84(2):275–84. doi: 10.1016/j.exer.2006.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang K, Li G, Read AT, Navarro I, Mitra AK, Stamer WD et al. The relationship between outflow resistance and trabecular meshwork stiffness in mice. Sci Rep. 2018;8(1):5848. doi: 10.1038/s41598-018-24165-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Izzotti A, Sacca SC, Longobardi M, Cartiglia C. Mitochondrial damage in the trabecular meshwork of patients with glaucoma. Arch Ophthalmol. 2010;128(6):724–30. doi: 10.1001/archophthalmol.2010.87. [DOI] [PubMed] [Google Scholar]
- 33.Pulliero A, Seydel A, Camoirano A, Sacca SC, Sandri M, Izzotti A. Oxidative damage and autophagy in the human trabecular meshwork as related with ageing. PLoS One. 2014;9(6):e98106. doi: 10.1371/journal.pone.0098106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sacca SC, Pascotto A, Camicione P, Capris P, Izzotti A. Oxidative DNA damage in the human trabecular meshwork: clinical correlation in patients with primary open-angle glaucoma. Arch Ophthalmol. 2005;123(4):458–63. doi: 10.1001/archopht.123.4.458. [DOI] [PubMed] [Google Scholar]
- 35.Goel M, Picciani RG, Lee RK, Bhattacharya SK. Aqueous humor dynamics: a review. Open Ophthalmol J. 2010;4:52–9. doi: 10.2174/1874364101004010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aliancy J, Stamer WD, Wirostko B. A Review of Nitric Oxide for the Treatment of Glaucomatous Disease. Ophthalmol Ther. 2017;6(2):221–32. doi: 10.1007/s40123-017-0094-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weinreb RN, Scassellati Sforzolini B, Vittitow J, Liebmann J. Latanoprostene Bunod 0.024% versus Timolol Maleate 0.5% in Subjects with Open-Angle Glaucoma or Ocular Hypertension: The APOLLO Study. Ophthalmology. 2016;123(5):965–73. doi: 10.1016/j.ophtha.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 38.Liu JHK, Slight JR, Vittitow JL, Scassellati Sforzolini B, Weinreb RN. Efficacy of Latanoprostene Bunod 0.024% Compared With Timolol 0.5% in Lowering Intraocular Pressure Over 24 Hours. Am J Ophthalmol. 2016;169:249–57. doi: 10.1016/j.ajo.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 39.Inoue T, Tanihara H. Rho-associated kinase inhibitors: a novel glaucoma therapy. Prog Retin Eye Res. 2013;37:1–12. doi: 10.1016/j.preteyeres.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 40.Tanna AP, Johnson M. Rho Kinase Inhibitors as a Novel Treatment for Glaucoma and Ocular Hypertension. Ophthalmology. 2018;125(11):1741–56. doi: 10.1016/j.ophtha.2018.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rao VP, Epstein DL. Rho GTPase/Rho kinase inhibition as a novel target for the treatment of glaucoma. BioDrugs. 2007;21(3):167–77. doi: 10.2165/00063030-200721030-00004. [DOI] [PubMed] [Google Scholar]
- 42.Zhang M, Maddala R, Rao PV. Novel molecular insights into RhoA GTPase-induced resistance to aqueous humor outflow through the trabecular meshwork. Am J Physiol Cell Physiol. 2008;295(5):C1057–70. doi: 10.1152/ajpcell.00481.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang RF, Williamson JE, Kopczynski C, Serle JB. Effect of 0.04% AR-13324, a ROCK, and norepinephrine transporter inhibitor, on aqueous humor dynamics in normotensive monkey eyes. J Glaucoma. 2015;24(1):51–4. doi: 10.1097/IJG.0b013e3182952213. [DOI] [PubMed] [Google Scholar]
- 44.Wang SK, Chang RT. An emerging treatment option for glaucoma: Rho kinase inhibitors. Clin Ophthalmol. 2014;8:883–90. doi: 10.2147/OPTH.S41000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin CW, Sherman B, Moore LA, Laethem CL, Lu DW, Pattabiraman PP et al. Discovery and Preclinical Development of Netarsudil, a Novel Ocular Hypotensive Agent for the Treatment of Glaucoma. J Ocul Pharmacol Ther. 2018;34(1–2):40–51. doi: 10.1089/jop.2017.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kiel JW, Kopczynski CC. Effect of AR-13324 on episcleral venous pressure in Dutch belted rabbits. J Ocul Pharmacol Ther. 2015;31(3):146–51. doi: 10.1089/jop.2014.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Inazaki H, Kobayashi S, Anzai Y, Satoh H, Sato S, Inoue M et al. One-year efficacy of adjunctive use of Ripasudil, a rho-kinase inhibitor, in patients with glaucoma inadequately controlled with maximum medical therapy. Graefes Arch Clin Exp Ophthalmol. 2017;255(10):2009–15. doi: 10.1007/s00417-017-3727-5. [DOI] [PubMed] [Google Scholar]
- 48.Ren R, Li G, Le TD, Kopczynski C, Stamer WD, Gong H. Netarsudil Increases Outflow Facility in Human Eyes Through Multiple Mechanisms. Invest Ophthalmol Vis Sci. 2016;57(14):6197–209. doi: 10.1167/iovs.16-20189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li G, Mukherjee D, Navarro I, Ashpole NE, Sherwood JM, Chang J et al. Visualization of conventional outflow tissue responses to netarsudil in living mouse eyes. Eur J Pharmacol. 2016;787:20–31. doi: 10.1016/j.ejphar.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dhamodaran K, Subramani M, Ponnalagu M, Shetty R, Das D. Ocular stem cells: a status update! Stem Cell Res Ther. 2014;5(2):56. doi: 10.1186/scrt445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fan BJ, Wiggs JL. Glaucoma: genes, phenotypes, and new directions for therapy. J Clin Invest. 2010;120(9):3064–72. doi: 10.1172/JCI43085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96–104. doi: 10.1097/ICU.0b013e32834ff1e7. [DOI] [PubMed] [Google Scholar]
- 53.Zhou R, Caspi RR. Ocular immune privilege. F1000 Biol Rep. 2010;2. doi: 10.3410/B2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pearson C, Martin K. Stem cell approaches to glaucoma: from aqueous outflow modulation to retinal neuroprotection. Prog Brain Res. 2015;220:241–56. doi: 10.1016/bs.pbr.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 55.Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901–11. doi: 10.1001/jama.2014.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chamling X, Sluch VM, Zack DJ. The Potential of Human Stem Cells for the Study and Treatment of Glaucoma. Invest Ophthalmol Vis Sci. 2016;57(5):ORSFi1–6. doi: 10.1167/iovs.15-18590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Raviola G Schwalbe line’s cells: a new cell type in the trabecular meshwork of Macaca mulatta. Invest Ophthalmol Vis Sci. 1982;22(1):45–56. [PubMed] [Google Scholar]
- 58.Acott TS, Samples JR, Bradley JM, Bacon DR, Bylsma SS, Van Buskirk EM. Trabecular repopulation by anterior trabecular meshwork cells after laser trabeculoplasty. Am J Ophthalmol. 1989;107(1):1–6. [DOI] [PubMed] [Google Scholar]
- 59.Gonzalez P, Epstein DL, Luna C, Liton PB. Characterization of free-floating spheres from human trabecular meshwork (HTM) cell culture in vitro. Exp Eye Res. 2006;82(6):959–67. doi: 10.1016/j.exer.2005.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Braunger BM, Ademoglu B, Koschade SE, Fuchshofer R, Gabelt BT, Kiland JA et al. Identification of adult stem cells in Schwalbe’s line region of the primate eye. Invest Ophthalmol Vis Sci. 2014;55(11):7499–507. doi: 10.1167/iovs.14-14872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tay CY, Sathiyanathan P, Chu SW, Stanton LW, Wong TT. Identification and characterization of mesenchymal stem cells derived from the trabecular meshwork of the human eye. Stem Cells Dev. 2012;21(9):1381–90. doi: 10.1089/scd.2011.0655. [DOI] [PubMed] [Google Scholar]
- 62.Whikehart DR, Parikh CH, Vaughn AV, Mishler K, Edelhauser HF. Evidence suggesting the existence of stem cells for the human corneal endothelium. Mol Vis. 2005;11:816–24. [PubMed] [Google Scholar]
- 63.McGowan SL, Edelhauser HF, Pfister RR, Whikehart DR. Stem cell markers in the human posterior limbus and corneal endothelium of unwounded and wounded corneas. Mol Vis. 2007;13:1984–2000. [PubMed] [Google Scholar]
- 64.Kelley MJ, Rose AY, Keller KE, Hessle H, Samples JR, Acott TS. Stem cells in the trabecular meshwork: present and future promises. Exp Eye Res. 2009;88(4):747–51. doi: 10.1016/j.exer.2008.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nadri S, Yazdani S, Arefian E, Gohari Z, Eslaminejad MB, Kazemi B et al. Mesenchymal stem cells from trabecular meshwork become photoreceptor-like cells on amniotic membrane. Neurosci Lett. 2013;541:43–8. doi: 10.1016/j.neulet.2012.12.055. [DOI] [PubMed] [Google Scholar]
- 66.Zhang Y, Cai S, Tseng SCG, Zhu YT. Isolation and Expansion of Multipotent Progenitors from Human Trabecular Meshwork. Sci Rep. 2018;8(1):2814. doi: 10.1038/s41598-018-21098-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Snider EJ, Vannatta RT, Schildmeyer L, Stamer WD, Ethier CR. Characterizing differences between MSCs and TM cells: Toward autologous stem cell therapies for the glaucomatous trabecular meshwork. J Tissue Eng Regen Med. 2018;12(3):695–704. doi: 10.1002/term.2488. [DOI] [PubMed] [Google Scholar]
- 68.Ding QJ, Zhu W, Cook AC, Anfinson KR, Tucker BA, Kuehn MH. Induction of trabecular meshwork cells from induced pluripotent stem cells. Invest Ophthalmol Vis Sci. 2014;55(11):7065–72. doi: 10.1167/iovs.14-14800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.***.Keller KE, Bhattacharya SK, Borras T, Brunner TM, Chansangpetch S, Clark AF et al. Consensus recommendations for trabecular meshwork cell isolation, characterization and culture. Exp Eye Res. 2018;171:164–73. doi: 10.1016/j.exer.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a direction for trabecular meshwork studies which shows how to isolate and culture TM cells and how to characterize and identify TM cells.
- 70.Fu CT, Sretavan D. Laser-induced ocular hypertension in albino CD-1 mice. Invest Ophthalmol Vis Sci. 2010;51(2):980–90. doi: 10.1167/iovs.09-4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kwong JM, Vo N, Quan A, Nam M, Kyung H, Yu F et al. The dark phase intraocular pressure elevation and retinal ganglion cell degeneration in a rat model of experimental glaucoma. Exp Eye Res. 2013;112:21–8. doi: 10.1016/j.exer.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Levkovitch-Verbin H, Quigley HA, Martin KR, Valenta D, Baumrind LA, Pease ME. Translimbal laser photocoagulation to the trabecular meshwork as a model of glaucoma in rats. Invest Ophthalmol Vis Sci. 2002;43(2):402–10. [PubMed] [Google Scholar]
- 73.Yu WY, Sheridan C, Grierson I, Mason S, Kearns V, Lo AC et al. Progenitors for the corneal endothelium and trabecular meshwork: a potential source for personalized stem cell therapy in corneal endothelial diseases and glaucoma. J Biomed Biotechnol. 2011;2011:412743. doi: 10.1155/2011/412743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fingert JH, Stone EM, Sheffield VC, Alward WL. Myocilin glaucoma. Surv Ophthalmol. 2002;47(6):547–61. [DOI] [PubMed] [Google Scholar]
- 75.Zode GS, Kuehn MH, Nishimura DY, Searby CC, Mohan K, Grozdanic SD et al. Reduction of ER stress via a chemical chaperone prevents disease phenotypes in a mouse model of primary open angle glaucoma. J Clin Invest. 2011;121(9):3542–53. doi: 10.1172/JCI58183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Junglas B, Kuespert S, Seleem AA, Struller T, Ullmann S, Bosl M et al. Connective tissue growth factor causes glaucoma by modifying the actin cytoskeleton of the trabecular meshwork. Am J Pathol. 2012;180(6):2386–403. doi: 10.1016/j.ajpath.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 77.Zode GS, Sharma AB, Lin X, Searby CC, Bugge K, Kim GH et al. Ocular-specific ER stress reduction rescues glaucoma in murine glucocorticoid-induced glaucoma. J Clin Invest. 2014;124(5):1956–65. doi: 10.1172/JCI69774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.***.Patel GC, Phan TN, Maddineni P, Kasetti RB, Millar JC, Clark AF et al. Dexamethasone-Induced Ocular Hypertension in Mice: Effects of Myocilin and Route of Administration. Am J Pathol. 2017;187(4):713–23. doi: 10.1016/j.ajpath.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows a steroid mouse glaucoma model which could be widely used in glaucoma research.
- 79.Irhimeh MR, Fitton JH, Lowenthal RM. Fucoidan ingestion increases the expression of CXCR4 on human CD34+ cells. Exp Hematol. 2007;35(6):989–94. doi: 10.1016/j.exphem.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 80.Tchernychev B, Ren Y, Sachdev P, Janz JM, Haggis L, O’Shea A et al. Discovery of a CXCR4 agonist pepducin that mobilizes bone marrow hematopoietic cells. Proc Natl Acad Sci U S A. 2010;107(51):22255–9. doi: 10.1073/pnas.1009633108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stern JH, Tian Y, Funderburgh J, Pellegrini G, Zhang K, Goldberg JL et al. Regenerating Eye Tissues to Preserve and Restore Vision. Cell Stem Cell. 2018;23(3):453. doi: 10.1016/j.stem.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 82.Vizoso FJ, Eiro N, Cid S, Schneider J, Perez-Fernandez R. Mesenchymal Stem Cell Secretome: Toward Cell-Free Therapeutic Strategies in Regenerative Medicine. Int J Mol Sci. 2017;18(9). doi: 10.3390/ijms18091852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Drago D, Cossetti C, Iraci N, Gaude E, Musco G, Bachi A et al. The stem cell secretome and its role in brain repair. Biochimie. 2013;95(12):2271–85. doi: 10.1016/j.biochi.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.**.Klingeborn M, Dismuke WM, Bowes Rickman C, Stamer WD. Roles of exosomes in the normal and diseased eye. Prog Retin Eye Res. 2017;59:158–77. doi: 10.1016/j.preteyeres.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reviews the basics and applications of exosomes and discusses future research studies for exosomes in the eye.
- 85.Zheng G, Huang R, Qiu G, Ge M, Wang J, Shu Q et al. Mesenchymal stromal cell-derived extracellular vesicles: regenerative and immunomodulatory effects and potential applications in sepsis. Cell Tissue Res. 2018;374(1):1–15. doi: 10.1007/s00441-018-2871-5. [DOI] [PubMed] [Google Scholar]
- 86.Mead B, Tomarev S. Bone Marrow-Derived Mesenchymal Stem Cells-Derived Exosomes Promote Survival of Retinal Ganglion Cells Through miRNA-Dependent Mechanisms. Stem Cells Transl Med. 2017;6(4):1273–85. doi: 10.1002/sctm.16-0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mead B, Amaral J, Tomarev S. Mesenchymal Stem Cell-Derived Small Extracellular Vesicles Promote Neuroprotection in Rodent Models of Glaucoma. Invest Ophthalmol Vis Sci. 2018;59(2):702–14. doi: 10.1167/iovs.17-22855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mead B, Ahmed Z, Tomarev S. Mesenchymal Stem Cell-Derived Small Extracellular Vesicles Promote Neuroprotection in a Genetic DBA/2J Mouse Model of Glaucoma. Invest Ophthalmol Vis Sci. 2018;59(13):5473–80. doi: 10.1167/iovs.18-25310. [DOI] [PMC free article] [PubMed] [Google Scholar]