Abstract
Background
Acute coronary syndrome (ACS) has become an important cause of death from cardiovascular disease. Cardiac rehabilitation (CR) plays an essential role in ACS patients after treatment. Therefore, in order to detect the impact of CR on mortality and major adverse cardiac events in patients with ACS, we conducted this meta-analysis.
Material/Methods
We searched PubMed, Web of science, and EMBASE databases to obtain published research results from 2010 to August 2018 to determine the relevant research. Random-effects model or fixed-effects model were used to calculate relative risk (RR) and 95% confidence interval (CI).
Results
Overall, a total of 25 studies with 55 035 participants were summarized in our meta-analysis. The results indicated that the hazard ratio (HR) of mortality significantly lower in the CR group than in the non-CR group (HR=−0.47; 95% CI=(−0.56 to −0.39; P<0.05). Fourteen studies on mortality rate showed exercise was associated with reduced cardiac death rates (RR=0.40; 95% CI=0.30 to 0.53; P<0.05). We found the risk of major adverse cardiac events (MACE) was lower in the rehabilitation group (RR=0.49; 95% CI=0.44 to 0.55; P<0.05). In 11 articles on CR including 8098 participants, the benefit in the CR group was greater than in the control group concerning revascularization (RR=0.69, 95% CI: 0.53 to 0.88; P=0.003). The recurrence rate of MI was reported in 13 studies, and the risk was lower in the CR group (RR=0.63, 95% CI: 0.57–0.70; P<0.05).
Conclusions
Our meta-analysis results suggest that CR is clearly associated with reductions in cardiac mortality, recurrence of MI, repeated PCI, CABG, and restenosis.
MeSH Keywords: Acute Coronary Syndrome, Meta-Analysis, Rehabilitation
Background
Cardiovascular disease (CVD) is one of the world’s most well-known health problems. Over the course of the decades, the overall incidence of CVD, particularly in acute coronary syndrome (ACS), has risen rapidly [1]. ACS has become an important cause of death from cardiovascular disease, especially in elderly ACS patients [2]. The mortality rate of patients with ACS has declined due to advances in medical technology [3]. However, improper treatment of ACS patients not only seriously endangers national health, but also imposes a heavy public health and economic burden.
ACS is a group of clinical syndromes based on the rupture or invasion of coronary atherosclerotic plaque, followed by complete or incomplete occlusive thrombosis, including acute ST-segment elevation myocardial infarction (STEMI), acute non-ST-segment elevation myocardial infarction (NSTEMI), and unstable angina (UA). For the treatment of ACS, cardiologists have a very important sentence: “time is the heart muscle and time is life” [4]. ACS, especially acute ST-segment elevation myocardial infarction, treatment emphasizes the opening of blocked blood vessels as soon as possible, restores blood perfusion of the heart, and protects the viable myocardium to maximize the protection of cardiac function and improve long-term prognosis. The treatment of ACS mainly includes: (1) conservative treatment of drugs, (2) interventional therapy, and (3) surgical treatment [5]. ACS treatment is not a single treatment, but rather requires a comprehensive treatment strategy, including short-term anticoagulant therapy, long-term antiplatelet therapy, combined use of lipids and other drugs, and appropriate application of interventional or surgical treatment. Overall, 30-day mortality rates for ACS patients have decreased significantly over the past 10 years due to improved antithrombotic therapy and early revascularization. Therefore, the epidemiology of ACS has also undergone profound changes: more patients with ACS survive from the initial ischemic event, and then recurrent ischemic events, heart failure, atrial fibrillation or non-cardiac disease (such as cancer), and longer survival time [1]. Therefore, long-term care for ACS patients will receive more and more attention, and cardiac rehabilitation will be an important component.
Cardiac rehabilitation (CR) is a comprehensive method that includes exercise training, risk factor education, psychological support, lifestyle and behavior changes, and reducing common risk factors [6–8]. Exercise is the best medicine [9]. In the past few decades, many epidemiological studies have shown that exercise is good for human health by reducing the risk of dementia, providing protection against metabolic disorders, and improving quality of life. CR after PCI has become very popular, especially during the rehabilitation of PCI, which helps to alleviate the symptoms of the patient; exercise often was used in combination with conventional treatment. The American Heart Association (AHA) guidelines [10] recommend training as a core element of exercise-based cardiac rehabilitation [11]. Cardiac rehabilitation aims to improve health and outcomes after ACS. There are several meta-analyses that have been published before, such as Anderson et al’s study [12] and Yang et al’s study[13]. Anderson et al’s study included 63 studies, and the results showed that CR reduced heart mortality in patients with coronary heart disease, but had no significant effect on myocardial infarction and revascularization. Yang et al’s study showed that exercise was not obviously associated with cardiac death reductions, MI recurrence, repetitive PCI, CABG, or restenosis. No meta-analysis focused on the relationship between ACS and CR based on exercise. Therefore, in order to detect the influence of CR on mortality and major adverse cardiac events (MACE, which were defined as a composite of all-cause death, non-fatal acute myocardial infarction, or target vessel revascularization [14]) in ACS patients, we conducted this meta-analysis.
Material and Methods
Information source and search strategy
We conducted a systematic search in PubMed, Cochrane Central Register of Controlled Trials, and EMBASE from 2010 to August 2018 to assess the relevant research. The following terms were used to search related research in the database without language restrictions: “Acute myocardial infarction” or “Unstable angina” and “Coronary heart disease” and “Cardiac rehabilitation”. The list of references for searched articles were filtered to determine other eligible references.
Inclusion and exclusion criteria
Two researchers independently reviewed the title and abstract of the results. Disagreements were resolved by discussion with another author and the included articles needed to meet the following inclusion criteria: (1) Research population includes ACS patients of all ages; (2) If the study is a randomized controlled with follow-up for more than 6 months or retrospective study, we considered it to be compliant; and (3) Patients needed to participate in any form of exercise program or included comprehensive cardiac rehabilitation combined with education of improved lifestyle; and comprised a control group that did not accept any form of structural exercise training but included medical treatment. The following studies were excluded: (1) The patients had severe cardiac complications such as heart failure, or mitral valve prolapse; (2) The patients who has a malignant tumor. (3) Cardiovascular mortality or hazard ratio (HR) or incidence of MACE (non-fatal myocardial infarction, revascularization) have not been reported or cannot be calculated based on available data; and (4) Full texts were not published in English.
Data extraction
The required data were extracted from all eligible studies, including the first author’s last name, publication time, number of patients in all studies, method of rehabilitation, and follow-up time. We obtained 4 tables of mortality and MACE incidence directly from the article to calculate RR and 95% CI. In addition, we directly obtained the HR and 95% CI of mortality.
Statistical analysis
Statistical analysis was conducted using STATA 14.0 software. χ2 and I-squared (I2) tests were used to evaluate the heterogeneity. If p≤0.10 and I2≥50%, which means there is heterogeneity between the studies, a random-effects model was used; otherwise, a fixed-effects model was used. Bilateral p<0.05 was regarded as statistically significant. We use forest plots to present the results of the meta-analysis.
Results
Selected studies and characteristics
We initially retrieved 2071 original studies, with and 1820 remaining after removing 251 duplicate articles. By screening the title and abstract in these 1820 articles, we found that 1784 did not match the topic. We reviewed 34 selected studies to determine their compliance with inclusion criteria. After screening full texts, 7 articles did not contain specific data for death or MACE, 1 was a review article, and 1 was not published in English, so these articles were excluded. Thus, a total of 25 studies with 55035 participants were summarized in our systematic review. The search and selection processes are shown in Figure 1. The characteristics and data of all 25 studies [15–39] are described in Table 1.
Figure 1.
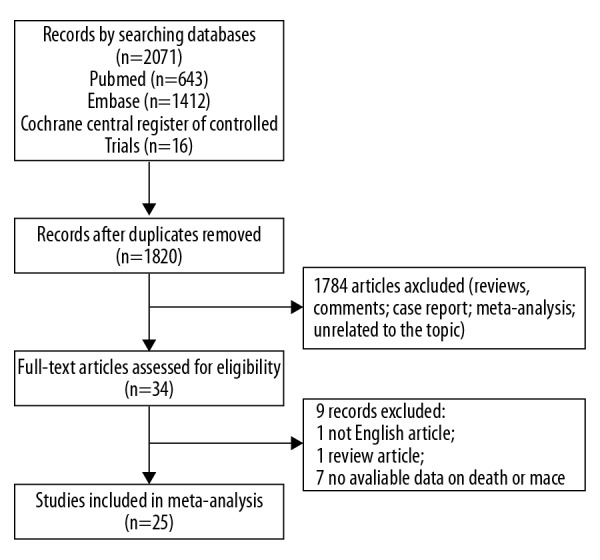
Results of the studies search.
Table 1.
Characteristics of the studies included in the meta-analysis.
| Year | Author | Country | Type of Study | Participants | Rehabilitation method and duration | Follow-up time (mouth) |
|---|---|---|---|---|---|---|
| 2018 | Sara Doimo | United States | Retrospective research | ACS patients (PCI or CABG) | Stationary bicycle training for 45 min, 2 time per week for 5 weeks, and gym training for 45 min, 3 times per week for 6 weeks; counseling about lifestyle; 5M | 60 |
| 2018 | Yong Zhang | China | Randomized controlled study | AMI patients (PCI) | Exercise for 3 phases; 6M | 6 |
| 2018 | Madoka Sunamura | Netherlands | Retrospective research | Patients with PCI | Exercise for 1.5h, twice per week; 12 W | 120 |
| 2017 | Manuel F. Jimenez-Navarro | United States | Retrospective research | Patients with PCI | Multidisciplinary rehabilitation for 3 h per week; 12W | 120 |
| 2017 | A. J. Hautala | Netherlands | Cohort design | ACS patients | Exercise for once per week; 6M | 12 |
| 2016 | Marion Pouche | French | Cohort design | AMI patients | N/A | 60 |
| 2016 | Jong-Young Lee | Korea | Retrospective research | Patients with PCI | Multidisciplinary rehabilitation for 3 times per week; 3M | 85 |
| 2015 | Han de Vries | Netherlands | Retrospective research | ACS patients (PCI or CABG) | Exercise for 30min, 2–3 times per week; relaxation therapy consists of 4–6 sessions lasting 60–90 min; 6–12W | 48 |
| 2015 | Hui-Ming Chen | Taiwan | Retrospective research | AMI patients (PCI) | Range of motion, muscle strengthening, breathing, and chest expansion exercises | 60 |
| 2014 | Roser Coll-Fernandez | Spanish | Cohort design | AMI <3 months | N/A | 18 |
| 2014 | Hee Eun Choi | Korea | Retrospective research | Patients with PCI | Main exercise for 30 min, 3 times per week; 8W | 9 |
| 2014 | Shannon M. Dunlay | United States | Retrospective research | AMI patients | N/A | 91 |
| 2014 | Bernhard Rauch | Germany | Randomized controlled study | AMI patients | Physiotherapy (3h per week), motivation, information, and education (7.2 and 7.0 h per week), social support service (0.9 and 1.1 hours per week), psychological support and supervision (2.3 and 3.4 h per week), and nursing (3.5 and 2.5 hours per week); −-4W | 12 |
| 2013 | Quinn R. Pack | United States | Retrospective research | Patients with CABG | Exercise for 30–45 min, 3 times per week; | 120 |
| 2010 | Tomo Onishi | Japan | Cohort design | AMI patients (PCI) | Exercise for 1h, twice per week; dietary and education program; 6M | 30 |
| 2009 | Dominique Hansen | Belgium | Cohort design | AMI patients (PCI or CABG) | Exercise for 1 h, 3 times per week; psychological and dietary counseling; 3M | 24 |
| 2008 | Paul Dendale | Belgium | Cohort design | Patients with PCI | Exercise for 1 h, 3 times per week; psychological and dietary counseling consisted of 8 education sessions; 3M | 54 |
| 2008 | David A. Alter | Canada | Retrospective research | ACS patients | 36 supervised exercise sessions; 1Y | 62 |
| 2008 | Kirsten M. Nielsen | Denmark | Cohort design | ACS patients (PCI or CABG) | Exercise, twice per week; 4 individual consultations; 6W | 24 |
| 2005 | Paul Dendale | Belgium | Retrospective research | ACS patients (PCI) | Exercise for 1 h, 3 times per week; psychological and dietary counseling consisted of 8 education sessions; 3M | 15 |
| 2005 | Jan Lisspers | Sweden | Randomized controlled study | Patients with PCI | Multidisciplinary rehabilitation-based health education and training activities; 1M | 60 |
| 2002 | Maria Teresa La Rovere | Italy | Randomized controlled study | ACS patients | Exercise for 30min, 5 times per week; 4W | 120 |
| 2001 | Romualdo Belardinelli | Italy | Randomized controlled study | Patients with PCI or PTCA | Exercise for 1h, 3 times per week; 6M | 33 |
| 2001 | Johan Denollet | Belgium | Cohort design | Patients with CABG | Exercise for 36 sessions. The first 24 sessions (3 times per week) included ECG-monitored aerobic exercise. The last 12 sessions (2 times per week) were performed without ECG monitoring; psychosocial group intervention comprised 6 sessions (2 hours, 1 time per week); 3W | 108 |
| 2001 | Bo Hedback | Sweden | Cohort design | Patients with CABG | Exercise for 30–40 min, twice per week; psychosocial support; 3M | 120 |
Meta-analysis
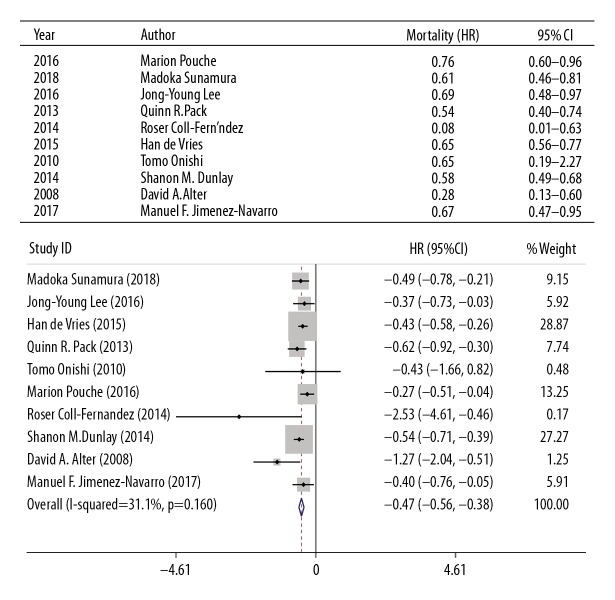
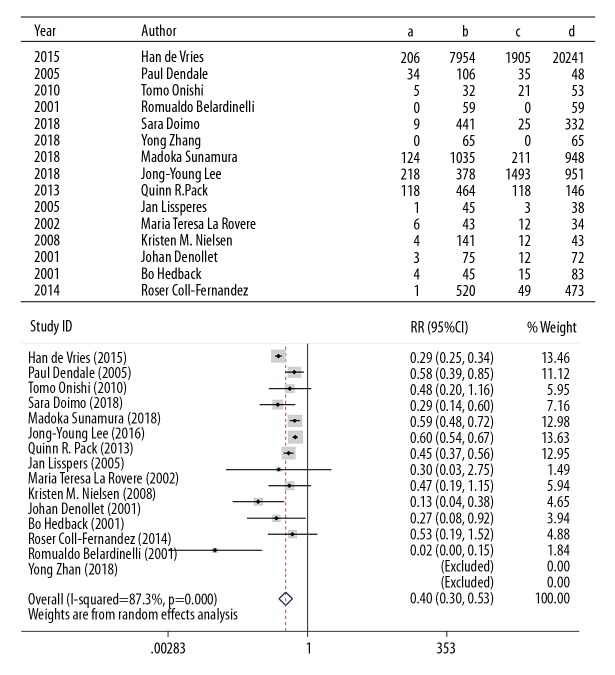
Cardiac rehabilitation and cardiovascular mortality
Ten articles were included that analyzed the relationship between cardiac rehabilitation and hazard ratio (HR) of cardiovascular mortality. We summarized the results of HR by fixed-effects models, and the analysis indicated cardiovascular mortality was significantly lower in the cardiac rehabilitation group than in the non-cardiac rehabilitation group (HR=−0.47; 95% CI=(−0.56, −0.39); P<0.05) (Figure 2). Fourteen studies reported the relationship between cardiovascular mortality rate and cardiac rehabilitation. Significant heterogeneity in the cardiovascular mortality rate of the pooled estimates was observed (I–squared=87.3%). Thus, we used a random-effects model. The results showed exercise was associated with significantly reduced cardiac death rates (RR=0.40; 95% CI=0.30–0.53; P<0.05) (Figure 3).
Figure 2.
Meta-analysis for the association between CR and HR of cardiovascular mortality.
Figure 3.
Meta-analysis for the association between CR and cardiac death rates.
Because of the greater heterogeneity of the included articles, we conducted a subgroup analysis. Meta-analysis with a follow-up of less than 2 years showed that cardiac rehabilitation exercise was not associated with cardiac death. However, meta-analysis with a follow-up of 2–4 years, 4.1–6 years, 6.1–10 years showed a positive correlation between exercise and decreased cardiac death (Figure 4).
Figure 4.
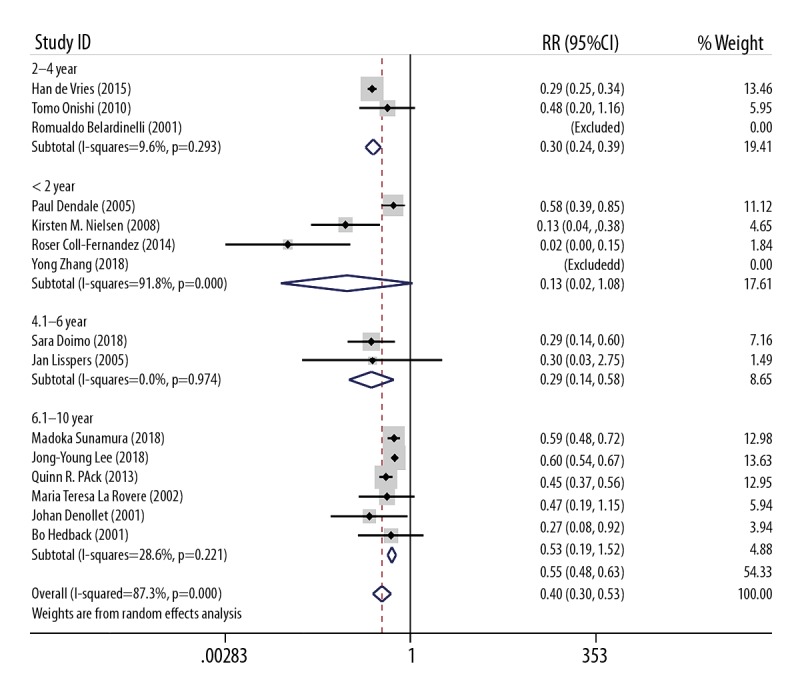
Subgroup meta-analysis based on follow-up time between CR and cardiac death rates.
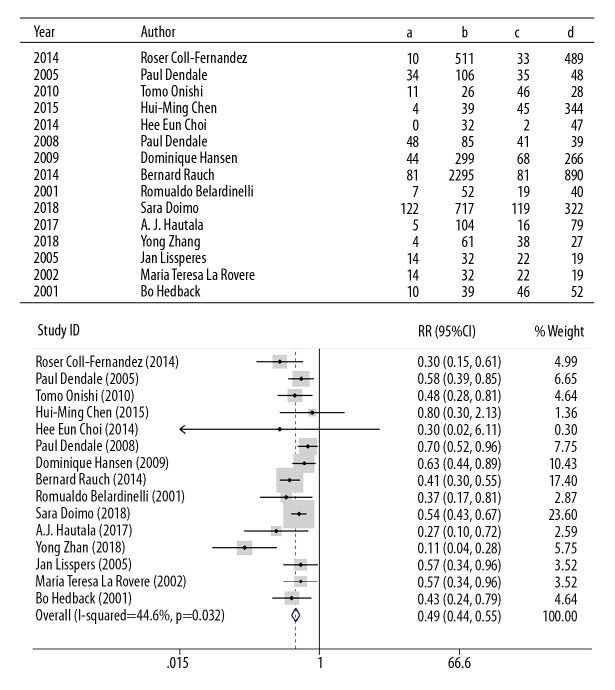
Cardiac rehabilitation and major adverse cardiovascular events
We included 15 articles about cardiac rehabilitation and MACE, and fixed-effects models showed that the risk of MACE was lower in the rehabilitation group (RR=0.49; 95% CI=0.44–0.55; P<0.05) (Figure 5).
Figure 5.
Meta-analysis for the association between CR and MACE.
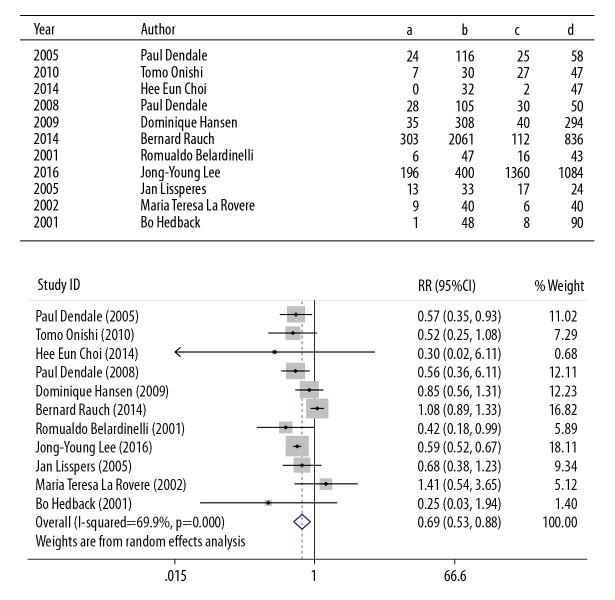
Cardiac rehabilitation and revascularization (re-PCI or CABG)
In the 11 articles on CR, which included 8098 participants, we found that the benefit in the CR group was greater than in the control group (RR=0.69, 95% CI: 0.53–0.88; P=0.003) by random-effects model (p=0.000, I-squared=69.9%) (Figure 6).
Figure 6.
Meta-analysis for the association between CR and revascularization.
We performed a subgroup analysis based on whether PCI/CABG was performed before the rehabilitation exercise, and the results showed that CR was not associated with revascularization in the AMI group. We could not confirm whether the intervention was PCI/CABG (RR=0.94, 95% CI: 0.70–1.26; P>0.05). Moreover, CR significantly reduced the incidence of vascular remodeling in the PCI/CABG group (RR=0.69, 95% CI: 0.53–0.88; P<0.05) (Figure 7).
Figure 7.
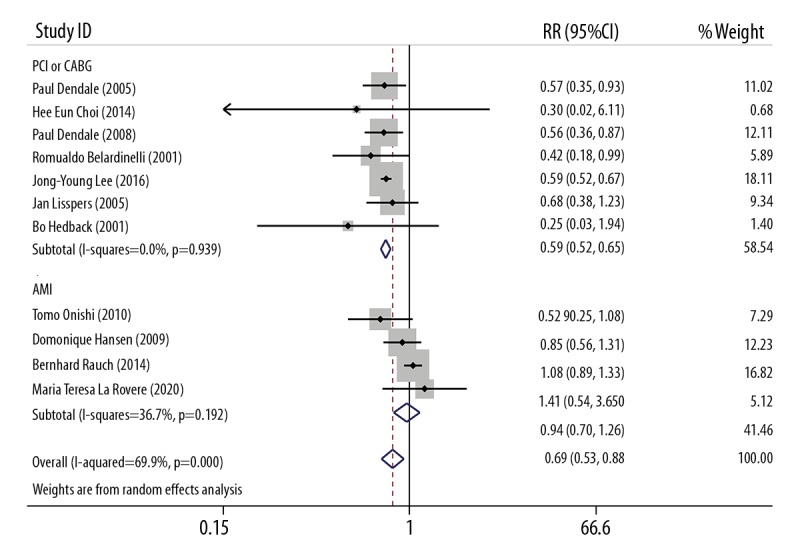
Subgroup meta-analysis based on treatment before CR between CR and revascularization.
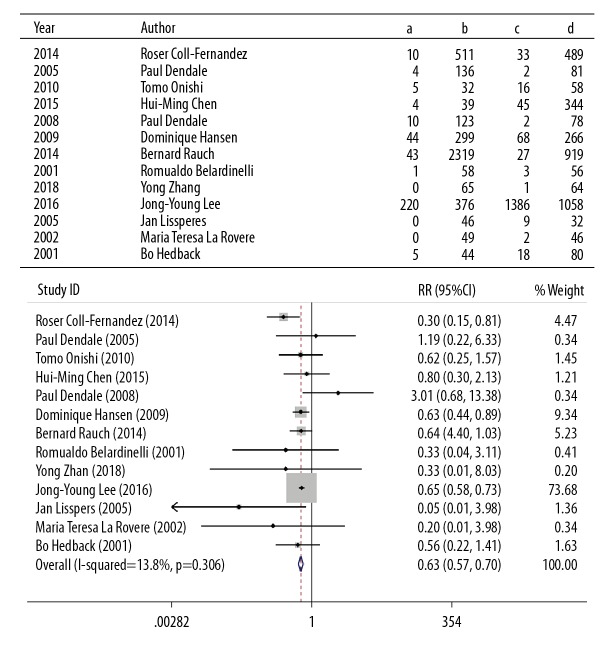
Cardiac rehabilitation and non-fatal myocardial infarction
Based on heterogeneity studies, we use fixed-effects models to analyze CR and non-fatal myocardial infarction. The recurrence rate of myocardial infarction was reported in 13 studies that included 9626 participants. In terms of the comparison between the CR groups and control groups, there was a significant difference in risk (RR=0.63, 95% CI: 0.57–0.70; P<0.05) (Figure 8).
Figure 8.
Meta-analysis for the association between CR and non-fatal myocardial infarction.
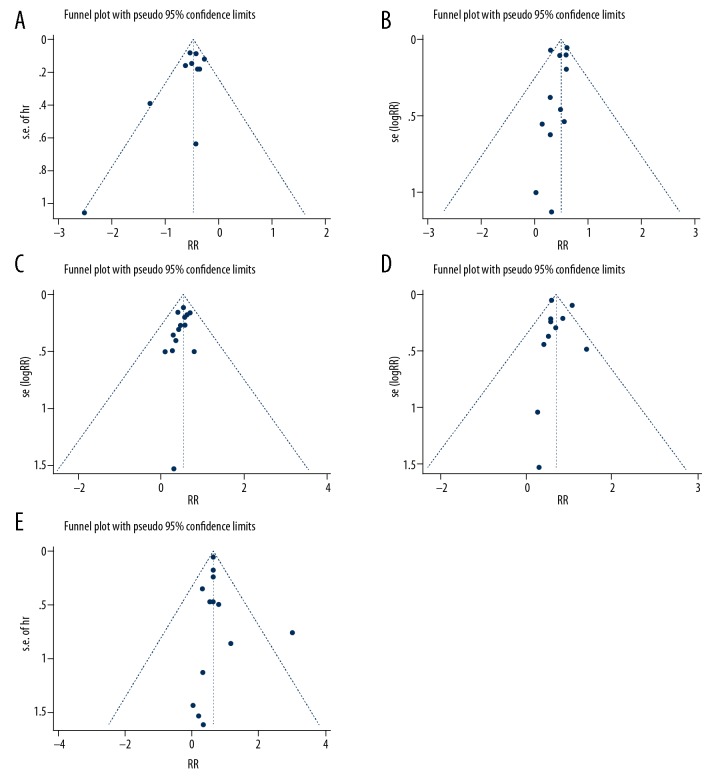
Publication bias
Funnel plots were used to assess possible publication bias. Priorities for positive findings were found in articles about CR and more patients or longer follow-up time needed to reduce publication bias (Figure 9).
Figure 9.
Funnel plot for the meta-analysis ((A) HR of cardiovascular mortality; (B) cardiac death rates; (C) MACE; (D) revascularization; (E) non-fatal myocardial infarction).
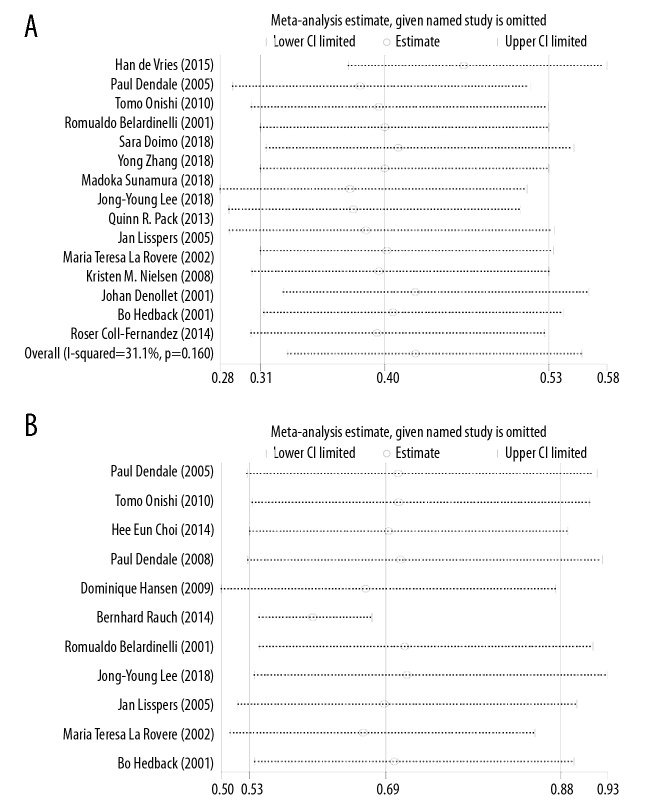
Sensitivity analysis
Because of the high degree of heterogeneity between the meta-analysis of CR and cardiac death and the meta-analysis of CR and revascularization, we performed a sensitivity analysis to assess the reliability of the results. The results indicate that the reliability of the results may have been affected by the short follow-up time [26,32,35] and large [22] or small [39] sample numbers (Figure 10).
Figure 10.
Sensitivity analysis results ((A) cardiac death rates; (B) revascularization).
Discussion
To the best of our knowledge, this is the first a meta-analysis on the effects of cardiac rehabilitation in ACS patients. Our review contained 25 studies and 55 035 participants who presented with ACS. The purpose of our meta-analysis was to determine if endpoint events could be reduced or survival could be improved by exercise in patients with ACS. In this analysis of studies, we found that CR was obviously related to decrease in cardiac death, recurrence of MI, repeated PCI, CABG, and restenosis.
In the past few years, CR has evolved from a simple plan to monitor patients’ safe physical activity into a comprehensive discipline program that includes post-operative patient care, drug therapy optimization, nutritional counseling, smoking cessation, risk stratification, stress management, and lifestyle improvement [40], and different projects have different rehabilitation plans.
CR has several beneficial effects, including improvement of exercise capacity, muscle strength, cardiac risk factors, and health-related quality of life, as well as reducing mortality in ACS patients. Our analysis and others have shown that these benefits of CR even affect elderly patients with ACS [41–45].
The exact mechanism by which CR improves the prognosis of patients with ACS has not been fully elucidated [46]. In past clinical practice and experiments, CR has been shown to have many direct benefits for the cardiovascular system, such as enhancing myocardial oxygen supply, endothelial function, autonomic nervous tone, coagulation factors, inflammatory markers, and development of coronary collateral vessels [47,48]. However, this may also be regulated by the indirect effects of exercise by improving the risk factors for atherosclerotic disease [49]. In Onishi’s study, the BMI of the CR group was significantly lower, and the levels of TG and fasting blood glucose levels in the CR group were significantly lower than those in the control group [29]. Indeed, a randomized study showed that CR reduced fat weight without a reduction in lean body weight, and also reduced the levels of TC in older patients with CAD [41]. These direct and indirect effects may have led to the reduction in cardiovascular events, and these effects can predict MACE in ACS patients, such as neurogenic mechanism and CRP [50,51].
We found that randomized controlled trials and observational studies [28,49,52–55] showed that, after participating in CR, the mortality rate after MI was reduced in the patients. The difference observed in the randomized controlled trial was less than the crude difference in mortality in the observational study [52,56]. To some extent, this can be ascribed to the non-random nature of the intervention, i.e., older patients with more severe conditions are less likely to participate in CR, but are more likely to have poor outcomes. Older patients with comorbidities that are common in clinical practice will generally be excluded from trial registration and their response to interventions such as CR may vary. In addition, the mortality rates of various trends involved in CR continue to decrease, indicating that even the highest-risk events involved in CR have a lower mortality rate for MI survivors than those who do not participate in CR.
We conducted an updated meta-analysis of exercise-based CR in people with existing ACS. Due to inconsistent follow-up time, the meta-analysis was heterogeneous; therefore, we conducted a subgroup analysis and we still came to the conclusion that CR can reduce the cardiac death rate. In addition, Dendale et al’s studies found that non-fatal myocardial infarction in the rehabilitation group increased [33], which may be because exercise increased the instability of pre-existing coronary plaque. However, our meta-analysis combined all the literature to conclude that exercise reduces non-fatal myocardial infarction. Our meta-analysis was based on a large sample size with long follow-up times, and we performed sensitivity analysis and subgroup analysis, so our results showing that CR can reduce cardiac death and MACE reliability in patients with ACS are reliable.
Although it has long been recognized that CR can improve prognosis, the participation rate of CR has not been high. In Pouche’s study [20], the 22.1% participation rate for CR is comparatively low, and the 1998 PREVENIR study had similar conclusions (23.3%) [57]. Another study reported similar results, with 13.9% of patients who had ACS and 31% who had a coronary artery bypass grafting [58]. In Europe, less than half the patients eligible for CR actually attend the programs [59].
The factors that determine the restrictions on participation or compliance with CR [60] may include: personal barriers (thinking that CR is not useful, patients have low control of cardiovascular risk factors, negative perceptions of those involved in rehabilitation, language barriers); barriers related to medical staff (they may provide information that is contradictory or provided at inappropriate times, inadequate understanding of CR objectives, and exclusion criteria); environmental and socio-professional barriers (inconvenient planning, incompatible timing); economic barriers; family barriers (lack of family involvement in rehabilitation); and physical barriers, including lack of transport or transport difficulties. Gaining a better understand of these barriers will be very important in improving CR compliance [61].
Conclusions
This meta-analysis showed that CR was clearly associated with reductions in cardiac death, recurrence of MI, repeated PCI, CABG, and restenosis. Expanding the sample size and improving the quality of studies will be very important in future research.
Footnotes
Source of support: This study was supported by Traditional Chinese Medicine Science and Technology Project of Jiangsu Province, grant number ZD201709
Conflict of interest
None.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics – 2017 update: A report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mansencal N, Pillieere R, N’Guetta R, et al. Characteristics and prognosis of coronary revascularization procedure in patients age 80 and older presenting with acute myocardial infarction. Med Sci Monit. 2010;16(1):CR15–20. [PubMed] [Google Scholar]
- 3.Widimsky P, Crea F, Binder RK, Luscher TF. The year in cardiology 2018: Acute coronary syndromes. Eur Heart J. 2019;40(3):271–82. doi: 10.1093/eurheartj/ehy904. [DOI] [PubMed] [Google Scholar]
- 4.Antman EM. Time is muscle: Translation into practice. J Am Coll Cardiol. 2008;52(15):1216–21. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–77. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 6.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the American Heart Association. Circulation. 2011;124(25):2951–60. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 7.Smith SC, Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58(23):2432–46. doi: 10.1016/j.jacc.2011.10.824. [DOI] [PubMed] [Google Scholar]
- 8.Piepoli MF, Hoes AW, Agewall A, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur J Prev Cardiol. 2016;23(11):Np1–96. doi: 10.1177/2047487316653709. [DOI] [PubMed] [Google Scholar]
- 9.Deweerdt S. Prevention: Activity is the best medicine. Nature. 2011;475(7355):S16–17. doi: 10.1038/475S16a. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training: A scientific statement from the American Heart Association. Circulation. 2013;128(8):873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto S, Hotta K, Ota E, et al. Effects of resistance training on muscle strength, exercise capacity, and mobility in middle-aged and elderly patients with coronary artery disease: A meta-analysis. J Cardiol. 2016;68(2):125–34. doi: 10.1016/j.jjcc.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 13.Yang X, Li Y, Ren X, et al. Effects of exercise-based cardiac rehabilitation in patients after percutaneous coronary intervention: A meta-analysis of randomized controlled trials. Sci Rep. 2017;7:44789. doi: 10.1038/srep44789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kip KE, Hollabaugh K, Marroquin OC, Williams DO. The problem with composite end points in cardiovascular studies: the story of major adverse cardiac events and percutaneous coronary intervention. J Am Coll Cardiol. 2008;51(7):701–7. doi: 10.1016/j.jacc.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 15.Doimo S, Fabris E, Piepoli M, et al. Impact of ambulatory cardiac rehabilitation on cardiovascular outcomes: A long-term follow-up study. Eur Heart J. 2019;40(8):678–85. doi: 10.1093/eurheartj/ehy417. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Cao H, Jiang P, Tang H. Cardiac rehabilitation in acute myocardial infarction patients after percutaneous coronary intervention: A community-based study. Medicine (Baltimore) 2018;97(8):e9785. doi: 10.1097/MD.0000000000009785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sunamura M, Ter Hoeve N, van den Berg-Emons RJG, et al. Cardiac rehabilitation in patients with acute coronary syndrome with primary percutaneous coronary intervention is associated with improved 10-year survival. Eur Heart J Qual Care Clin Outcomes. 2018;4(3):168–72. doi: 10.1093/ehjqcco/qcy001. [DOI] [PubMed] [Google Scholar]
- 18.Jimenez-Navarro MF, Lopez-Jimenez F, Perez-Belmonte LM, et al. Benefits of cardiac rehabilitation on cardiovascular outcomes in patients with diabetes mellitus after percutaneous coronary intervention. J Am Heart Assoc. 2017;6(10) doi: 10.1161/JAHA.117.006404. pii: e006404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hautala AJ, Kiviniemi AM, Makikallio T, et al. Economic evaluation of exercise-based cardiac rehabilitation in patients with a recent acute coronary syndrome. Scand J Med Sci Sports. 2017;27(11):1395–403. doi: 10.1111/sms.12738. [DOI] [PubMed] [Google Scholar]
- 20.Pouche M, Ruidavets JB, Ferrieres J, et al. Cardiac rehabilitation and 5-year mortality after acute coronary syndromes: The 2005 French FAST-MI study. Arch Cardiovasc Dis. 2016;109(3):178–87. doi: 10.1016/j.acvd.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Lee JY, Ahn JM, Park DW, et al. Impact of exercise-based cardiac rehabilitation on long-term clinical outcomes in patients with left main coronary artery stenosis. Eur J Prev Cardiol. 2016;23(17):1804–13. doi: 10.1177/2047487316658570. [DOI] [PubMed] [Google Scholar]
- 22.de Vries H, Kemps HM, van Engen-Verheul MM, et al. Cardiac rehabilitation and survival in a large representative community cohort of Dutch patients. Eur Heart J. 2015;36(24):1519–28. doi: 10.1093/eurheartj/ehv111. [DOI] [PubMed] [Google Scholar]
- 23.Chen HM, Liu CK, Chen HW, et al. Efficiency of rehabilitation after acute myocardial infarction. Kaohsiung J Med Sci. 2015;31(7):351–57. doi: 10.1016/j.kjms.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 24.Rauch B, Riemer T, Schwaab B, et al. Short-term comprehensive cardiac rehabilitation after AMI is associated with reduced 1-year mortality: results from the OMEGA study. Eur J Prev Cardiol. 2014;21(9):1060–69. doi: 10.1177/2047487313486040. [DOI] [PubMed] [Google Scholar]
- 25.Dunlay SM, Pack QR, Thomas RJ, et al. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. 2014;127(6):538–46. doi: 10.1016/j.amjmed.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coll-Fernandez R, Coll R, Pascual T, et al. Cardiac rehabilitation and outcome in stable outpatients with recent myocardial infarction. Arch Phys Med Rehabil. 2014;95(2):322–29. doi: 10.1016/j.apmr.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 27.Choi HE, Lee BJ, Kim C. Impact of exercise-based cardiac rehabilitation on de novo coronary lesion in patients with drug eluting stent. Ann Rehabil Med. 2014;38(2):256–62. doi: 10.5535/arm.2014.38.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pack QR, Goel K, Lahr BD, et al. Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: A community-based study. Circulation. 2013;128(6):590–97. doi: 10.1161/CIRCULATIONAHA.112.001365. [DOI] [PubMed] [Google Scholar]
- 29.Onishi T, Shimada K, Sato H, et al. Effects of phase III cardiac rehabilitation on mortality and cardiovascular events in elderly patients with stable coronary artery disease. Circ J. 2010;74(4):709–14. doi: 10.1253/circj.cj-09-0638. [DOI] [PubMed] [Google Scholar]
- 30.Hansen D, Dendale P, Leenders M, et al. Reduction of cardiovascular event rate: Different effects of cardiac rehabilitation in CABG and PCI patients. Acta Cardiol. 2009;64(5):639–44. doi: 10.2143/AC.64.5.2042694. [DOI] [PubMed] [Google Scholar]
- 31.Alter DA, Oh PI, Chong A. Relationship between cardiac rehabilitation and survival after acute cardiac hospitalization within a universal health care system. Eur J Cardiovasc Prev Rehabil. 2009;16(1):102–13. doi: 10.1097/HJR.0b013e328325d662. [DOI] [PubMed] [Google Scholar]
- 32.Nielsen KM, Faergeman O, Foldspang A, Larsen ML. Cardiac rehabilitation: health characteristics and socio-economic status among those who do not attend. Eur J Public Health. 2008;18(5):479–83. doi: 10.1093/eurpub/ckn060. [DOI] [PubMed] [Google Scholar]
- 33.Dendale P, Hansen D, Berger J, Lamotte M. Long-term cost-benefit ratio of cardiac rehabilitation after percutaneous coronary intervention. Acta Cardiol. 2008;63(4):451–56. doi: 10.2143/AC.63.4.2033043. [DOI] [PubMed] [Google Scholar]
- 34.Lisspers J, Sundin O, Ohman A, et al. Long-term effects of lifestyle behavior change in coronary artery disease: Effects on recurrent coronary events after percutaneous coronary intervention. Health Psychol. 2005;24(1):41–48. doi: 10.1037/0278-6133.24.1.41. [DOI] [PubMed] [Google Scholar]
- 35.Dendale P, Berger J, Hansen D, et al. Cardiac rehabilitation reduces the rate of major adverse cardiac events after percutaneous coronary intervention. Eur J Cardiovasc Nurs. 2005;4(2):113–16. doi: 10.1016/j.ejcnurse.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 36.La Rovere MT, Bersano C, Gnemmi M, et al. Exercise-induced increase in baroreflex sensitivity predicts improved prognosis after myocardial infarction. Circulation. 2002;106(8):945–49. doi: 10.1161/01.cir.0000027565.12764.e1. [DOI] [PubMed] [Google Scholar]
- 37.Hedback B, Perk J, Hornblad M, Ohlsson U. Cardiac rehabilitation after coronary artery bypass surgery: 10-year results on mortality, morbidity and readmissions to hospital. J Cardiovasc Risk. 2001;8(3):153–58. doi: 10.1177/174182670100800306. [DOI] [PubMed] [Google Scholar]
- 38.Denollet J, Brutsaert DL. Reducing emotional distress improves prognosis in coronary heart disease: 9-year mortality in a clinical trial of rehabilitation. Circulation. 2001;104(17):2018–23. doi: 10.1161/hc4201.097940. [DOI] [PubMed] [Google Scholar]
- 39.Belardinelli R, Paolini I, Cianci G, et al. Exercise training intervention after coronary angioplasty: the ETICA trial. J Am Coll Cardiol. 2001;37(7):1891–900. doi: 10.1016/s0735-1097(01)01236-0. [DOI] [PubMed] [Google Scholar]
- 40.Piepoli MF, Corra U, Benzer W, et al. Secondary prevention through cardiac rehabilitation: From knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17(1):1–17. doi: 10.1097/HJR.0b013e3283313592. [DOI] [PubMed] [Google Scholar]
- 41.Seki E, Watanabe Y, Shimada K, et al. Effects of a phase III cardiac rehabilitation program on physical status and lipid profiles in elderly patients with coronary artery disease: Juntendo Cardiac Rehabilitation Program (J-CARP) Circ J. 2008;72(8):1230–34. doi: 10.1253/circj.72.1230. [DOI] [PubMed] [Google Scholar]
- 42.Lavie CJ, Milani R. Benefits of cardiac rehabilitation in the elderly. Chest. 2004;126(4):1010–12. doi: 10.1378/chest.126.4.1010. [DOI] [PubMed] [Google Scholar]
- 43.Seki E, Watanabe Y, Sunayama S, et al. Effects of phase III cardiac rehabilitation programs on health-related quality of life in elderly patients with coronary artery disease: Juntendo Cardiac Rehabilitation Program (J-CARP) Circ J. 2003;67(1):73–77. doi: 10.1253/circj.67.73. [DOI] [PubMed] [Google Scholar]
- 44.Pasquali SK, Alexander KP, Peterson ED. Cardiac rehabilitation in the elderly. Am Heart J. 2001;142(5):748–55. doi: 10.1067/mhj.2001.119134. [DOI] [PubMed] [Google Scholar]
- 45.Stahle A, Mattsson E, Ryden L, et al. Improved physical fitness and quality of life following training of elderly patients after acute coronary events. A 1 year follow-up randomized controlled study. Eur Heart J. 1999;20(20):1475–84. doi: 10.1053/euhj.1999.1581. [DOI] [PubMed] [Google Scholar]
- 46.Thompson PD, Buchner D, Pina IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: A statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity) Circulation. 2003;107(24):3109–16. doi: 10.1161/01.CIR.0000075572.40158.77. [DOI] [PubMed] [Google Scholar]
- 47.Clausen JP, Trap-Jensen J. Heart rate and arterial blood pressure during exercise in patients with angina pectoris. Effects of training and of nitroglycerin. Circulation. 1976;53(3):436–42. doi: 10.1161/01.cir.53.3.436. [DOI] [PubMed] [Google Scholar]
- 48.Hambrecht R, Wolf A, Gielen S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med. 2000;342(7):454–60. doi: 10.1056/NEJM200002173420702. [DOI] [PubMed] [Google Scholar]
- 49.Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 50.Lukin A, Novak K, Polic S, Puljak L. Prognostic value of low and moderately elevated C-reactive protein in acute coronary syndrome: A 2-year follow-up study. Med Sci Monit. 2013;19:777–86. doi: 10.12659/MSM.884014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Iwaszczuk P, Kolodziejczyk B, Kruczek T, et al. Ischemic versus non-ischemic (neurogenic) myocardial contractility impairment in acute coronary syndromes: Prevalence and impact on left ventricular systolic function recovery. Med Sci Monit. 2018;24:3693–701. doi: 10.12659/MSM.907466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Witt BJ, Jacobsen SJ, Weston SA, et al. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004;44(5):988–96. doi: 10.1016/j.jacc.2004.05.062. [DOI] [PubMed] [Google Scholar]
- 53.Jolliffe JA, Rees K, Taylor RS, et al. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001;(1):Cd001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 54.Oldridge NB, Guyatt GH, Fischer ME, Rimm AA. Cardiac rehabilitation after myocardial infarction. Combined experience of randomized clinical trials. JAMA. 1988;260(7):945–50. [PubMed] [Google Scholar]
- 55.Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54(1):25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 56.Beauchamp A, Worcester M, Ng A, et al. Attendance at cardiac rehabilitation is associated with lower all-cause mortality after 14 years of follow-up. Heart. 2013;99(9):620–25. doi: 10.1136/heartjnl-2012-303022. [DOI] [PubMed] [Google Scholar]
- 57.Cottin Y, Cambou JP, Casillas JM, et al. Specific profile and referral bias of rehabilitated patients after an acute coronary syndrome. J Cardiopulm Rehabil. 2004;24(1):38–44. doi: 10.1097/00008483-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 58.Suaya JA, Shepard DS, Normand SL, et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–62. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 59.Bjarnason-Wehrens B, McGee H, Zwisler AD, et al. Cardiac rehabilitation in Europe: Results from the European Cardiac Rehabilitation Inventory Survey. Eur J Cardiovasc Prev Rehabil. 2010;17(4):410–18. doi: 10.1097/HJR.0b013e328334f42d. [DOI] [PubMed] [Google Scholar]
- 60.Neubeck L, Freedman SB, Clark AM, et al. Participating in cardiac rehabilitation: A systematic review and meta-synthesis of qualitative data. Eur J Prev Cardiol. 2012;19(3):494–503. doi: 10.1177/1741826711409326. [DOI] [PubMed] [Google Scholar]
- 61.Pavy B, Darchis J, Merle E, Caillon M. [Cardiac rehabilitation after myocardial infarction in France: still not prescribed enough]. Ann Cardiol Angeiol (Paris) 2014;63(5):369–75. doi: 10.1016/j.ancard.2014.09.002. [in French] [DOI] [PubMed] [Google Scholar]