Abstract
Objective:
Depression is associated with poor outcomes following heart failure. Information regarding the use and effectiveness of antidepressants in heart failure patients is lacking. This study aims to evaluate the prescribing patterns of antidepressants in patients with heart failure residing in aged care facilities.
Methods:
This study was a cross-sectional analysis of de-identified Australian Residential Medication Management Reviews conducted between January 2016 and April 2017. SPSS version 24 software was used to analyze the data. Descriptive statistics were used to summarize age, gender, and antidepressants use. Wilcoxon signed-rank test was used to assess the differences in antidepressant prescribing between patients with and without heart failure.
Findings:
Of 4369 patients, 980 (22.4%) had heart failure. Of those with heart failure, 410 (41.8%) were using at least one antidepressant. Mirtazapine was the most commonly prescribed antidepressant in patients with heart failure (27.8%) and without heart failure (27.3%). When grouping antidepressants for class, selective serotonin reuptake inhibitors were the most commonly prescribed in both groups. There was no statistically significant difference in antidepressant prescribing patterns between patients with and without heart failure (P = 0.961).
Conclusion:
Mirtazapine was the most commonly used antidepressant in heart failure patients residing in aged care facilities. This study has highlighted a need for a randomized controlled trial to evaluate the efficacy and safety of mirtazapine in the management of depression in patients with heart failure.
KEYWORDS: Antidepressant, depression, heart failure, Mirtazapine, prescribing
INTRODUCTION
It is estimated that depression affects approximately 21.5% of heart failure patients.[1] In this patient group, depression is associated with increased hospitalization and mortality rates.[1,2] In addition, depression decreases patient adherence to treatment and self-care, and it can reduce patients' quality of life.[3] Appropriate management of depression in this patient group can improve their life expectancy and quality of life.[4] Selective serotonin reuptake inhibitors (SSRIs) are considered the first-line agents in managing major depression according to many published guidelines.[4,5,6,7]
Since no specific preferred treatment for depression in heart failure patients has been established, SSRIs are often used in this role.[2,4,8] However, there is conflicting information in the literature regarding the use of SSRIs in managing depression in heart failure patients. Currently, strong evidence to support their use in this population is lacking. Of the SSRIs drug class, paroxetine, sertraline, citalopram, and escitalopram have been investigated for their efficacy in the management of depression in patients with heart failure. These four drugs were studied in clinical trials that were double-blinded and placebo-controlled.[9,10,11,12] In a small pilot study (n = 28), paroxetine was shown to be effective in reducing depression and improving psychological aspects of patients' quality of life.[9] On the other hand, a small study (n = 72) which evaluated citalopram in elderly patients with heart failure found that citalopram efficacy in treating depression was not better than placebo.[12] In addition, two larger more recent trials involving sertraline and escitalopram (n = 469 and 372, respectively) failed to show statistically significant improvement in depression scores between control and treatment groups.[10,11] These three trials concluded that these agents are ineffective in treating depression in heart failure patients.[10,11,12]
Non-SSRI antidepressants have mainly been investigated for their safety in heart failure patients, rather than efficacy.[13,14] An exception was trimipramine which has been shown to be effective in treating depression in heart failure. However, the trial had a small sample size (n = 22) and an open-label design. Moreover, prolongation of QRS complex was observed with trimipramine during the trial.[15] These findings indicate that more investigation of the efficacy of non-SSRIs antidepressants in heart failure patients is needed.
To our knowledge, there have been no published studies conducted in Australia to investigate the prescribing patterns of antidepressants in patients with heart failure, in the aged care setting. This research provides an insight into the commonly used antidepressants in elderly patients with heart failure, in the Australian context. Findings from this study inform and guide future trials exploring the efficacy and safety of antidepressants in this population group, ultimately contributing to improved management of depression and patient care.
The overall aim of the present study is to analyze the prescribing patterns of antidepressants in patients with heart failure residing in aged care facilities, with the specific objectives of estimating the frequency of antidepressant prescribing in patients with heart failure, identifying the commonly prescribed antidepressants, and their indication(s) in patients with heart failure, and comparing the antidepressant prescribing patterns between patients with and without heart failure.
METHODS
This study was a cross-sectional retrospective review of de-identified Australian Residential Medication Management Review (RMMR) records. The study was approved by Curtin University Human Research Ethics Committee (approval number: HRE2017-0152).
RMMR records were obtained from Ward Medication Management, based in Victoria, Australia, which specializes in medication management and reviews for aged care patients across Australia. RMMRs conducted between January 2016 and April 2017 were used for sample extraction. There were a total of 12,685 reviews conducted for 12,276 residents.
As part of the routine procedure, this organization codes all medical conditions based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes and all medications based on the World Health Organization's Anatomical Therapeutic Chemical (ATC) Classification System.
A patient's record was included in the study if they had heart failure (coded with the ICD-10 code “I50”) or were using at least one antidepressant (coded with ATC code “N06A”). An ideal de-identified record of RMMR included the following information: de-identified resident code, review number, age, gender, medical conditions, allergies, medications, and doses. However, some records had incomplete information. Accordingly, records with missing medications or medical conditions information were removed from the analysis. Finally, some residents had more than one review conducted during that period; only the latest review was included in the analysis.
After this initial phase, two datasets were formed. The first included all patients with heart failure while the second included all patients prescribed at least one antidepressant [Figure 1].
Figure 1.
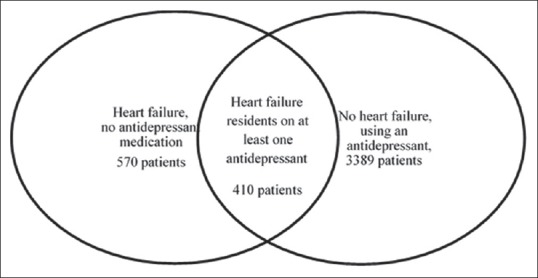
Venn diagram of the two datasets used for the study
A final file was created by combining both datasets with a sample size of 4369 patients. This file was used to extract demographic and clinical variables such as age, gender, total number of medications prescribed, and most common diagnosis. In addition, the names of the antidepressants used were extracted. Frequency of use was reported for single antidepressant agents. Consequently, single agents were grouped into their commonly identified class to report on class use.
Records of patients with heart failure using an antidepressant were reviewed manually to assess indications for antidepressant use. An indication was considered acceptable if it was Therapeutic Goods Administration approved, listed in the Australian Medicines Handbook, or included in the electronic Therapeutic Guidelines.
Data were analyzed using the IBM SPSS Statistics for Windows, version 24 software. Descriptive statistics were used to analyze demographics (mean, standard deviation, median, and percentages) and antidepressant use (frequency and percentages). Wilcoxon signed-rank test was used to compare antidepressant prescribing between patients with and without heart failure. A P < 0.05 was taken to indicate a statistically significant association in all tests.
RESULTS
The mean age of all patients was 85.2 ± 8.6 years. Approximately 70% of the patients were females. Patients were prescribed an average of 15 medications per day per patient. Depression affected 35.4% of all patients, while heart failure was reported in 22.4% of patients.
Of the 980 patients with heart failure, 410 patients (41.8% [410/980]) were using at least one antidepressant and comprised 9.4% of the total sample (n = 4369).
The prevalence of depression (based on ICD-10 coding) in patients with heart failure residing in aged care facilities was found to be 36.0% (353/980). In patients with a combined diagnosis of depression and heart failure, 70.0% (247/353) received at least one antidepressant, while the remaining 30.0% (106/353) were not prescribed any antidepressant. The main findings for this dataset are summarized in Table 1.
Table 1.
Number of patients and their characteristics
| Characteristics | Number of patients (%) |
|---|---|
| Total sample (n=4369) | |
| HF | 980 (22.4) |
| HF and antidepressant use | 410 (9.4) |
| HF group (n=980) | |
| HF and using at least one antidepressant | 410 (41.8) |
| HF and have reported depression | 353 (36.0) |
| HF and depression (n=353) | |
| HF + depression and use at least one antidepressant | 247 (70.0) |
| HF + depression without any antidepressant | 106 (30.0) |
HF=Heart failure
There were 410 patients in the heart failure group who used at least one antidepressant. The total number of antidepressants used was 428 since some patients used more than one antidepressant. The most commonly prescribed antidepressants in the heart failure patient group were mirtazapine (27.8% [119/428]), sertraline (15.7% [67/428]), escitalopram (15.4% [66/428]), citalopram (8.6% [37/428], and amitriptyline (6.5% [28/428]).
The most commonly prescribed class of antidepressants was SSRI (46.7% [200/428]) followed by noradrenaline and specific serotonergic antidepressants (28.7% [123/428]), serotonin-norepinephrine reuptake inhibitors (14.0% [60/428]), tricyclic antidepressants (TCAs) (9.8% [42/428]), monoamine oxidase inhibitors (MAOIs) (0.5% [2/428]), and others (bupropion) (0.2% [1/428]), respectively. Table 2 includes a summary of all antidepressant classes and single agents used in heart failure patients.
Table 2.
Antidepressants classes and single agents used with and without heart failure in the sample
| Antidepressant classes and single agents | Total frequency (n=3799) | Percentage from all antidepressants used | With HF (n=410) | Percentage within HF | Without HF (n=3389) | Percentage within without HF | P* for Percentage HF and no HF |
|---|---|---|---|---|---|---|---|
| SSRI | 1846 | 45.67 | 200 | 46.73 | 1646 | 45.55 | 0.917 |
| Sertraline | 663 | 16.40 | 67 | 15.65 | 596 | 16.49 | |
| Escitalopram | 506 | 12.52 | 66 | 15.42 | 440 | 12.17 | |
| Citalopram | 439 | 10.86 | 37 | 8.64 | 402 | 11.12 | |
| Paroxetine | 122 | 3.02 | 11 | 2.57 | 111 | 3.07 | |
| Fluoxetine | 87 | 2.15 | 15 | 3.50 | 72 | 1.99 | |
| Fluvoxamine | 29 | 0.72 | 4 | 0.93 | 25 | 0.69 | |
| NaSSA | 1121 | 27.73 | 123 | 28.74 | 998 | 27.61 | 0.180 |
| Mirtazapine | 1107 | 27.39 | 119 | 27.80 | 988 | 27.34 | |
| Mianserin | 14 | 0.35 | 4 | 0.93 | 10 | 0.28 | |
| SNRI | 641 | 15.86 | 60 | 14.02 | 581 | 16.08 | 0.285 |
| Venlafaxine | 287 | 7.10 | 27 | 6.31 | 260 | 7.19 | |
| Duloxetine | 204 | 5.05 | 23 | 5.37 | 181 | 5.01 | |
| Desvenlafaxine | 150 | 3.71 | 10 | 2.34 | 140 | 3.87 | |
| TCA | 405 | 10.02 | 42 | 9.81 | 363 | 10.04 | 0.753 |
| Amitriptyline | 323 | 7.99 | 28 | 6.54 | 295 | 8.16 | |
| Dothiepin | 30 | 0.74 | 3 | 0.70 | 27 | 0.75 | |
| Doxepin | 26 | 0.64 | 3 | 0.70 | 23 | 0.64 | |
| Nortriptyline | 23 | 0.57 | 7 | 1.64 | 16 | 0.44 | |
| Imipramine | 2 | 0.05 | 1 | 0.23 | 1 | 0.03 | |
| Clomipramine | 1 | 0.02 | 0 | 0 | 1 | 0.03 | |
| MAOI† | 12 | 0.30 | 2 | 0.47 | 10 | 0.28 | 0.655 |
| Others‡ | 17 | 0.42 | 1 | 0.23 | 16 | 0.44 | 0.593 |
| Total | 4042 | 100 | 428 | 100 | 3614 | 100 | 0.961 |
*Difference comparison P value based on Wilcoxon–Signed rank test, †The most commonly prescribed MAOI was moclobemide. Tranylcypromine was used once. ‡Other prescribed antidepressants were agomelatine, reboxetine, and bupropion. The frequency was in respective order. HF=Heart failure, MAOI=Monoamine oxidase inhibitor, NaSSA=Noradrenaline and specific serotonergic antidepressant, SNRI=Serotonin norepinephrine reuptake inhibitor, SSRI=Selective serotonin reuptake inhibitor, TCA=Tricyclic antidepressant
A total of 346 indications were recorded in the 410 patients with heart failure who were using at least one antidepressant. Some patients had more than one indication, while 129 (31.5% [129/410]) patients were prescribed an antidepressant without clear indication. The total number of antidepressants uses with and without indication was 475. Depression was the most common indication for using antidepressants in heart failure patients (52% of all users [247/475]), followed by other mental and behavioral disorders (13.3% [63/475]) with anxiety being the most frequent disorder. Chronic pain (5.5% [26/475]), urinary incontinence (1.3% [6/475]), and diabetic neuropathy (0.8% [4/475]) were also reported. Mirtazapine was the most frequently prescribed antidepressant without a clear indication, and approximately 40% (46/119) of patients who were prescribed mirtazapine had no clear indication.
Of the 3799 patients who were using at least one antidepressant, 3389 (89.2% [3389/3799]) patients had no heart failure. The total number of antidepressants used among this group was 3614 drugs as some patients were taking more than one antidepressant. In this group, mirtazapine was the most commonly prescribed antidepressant (27.3% [988/3614]), followed by sertraline (16.5% [596/3614]), escitalopram (12.2% [440/3614]), citalopram (11.1% [402/3614]), and amitriptyline (8.2% [295/3614]). The ranking of these antidepressants is the same as in patients with heart failure. Table 2 shows the commonly prescribed antidepressant classes and agents in all patients and in patients with and without heart failure.
There was no significant difference between antidepressant prescribing in patients with and without heart failure (related samples Wilcoxon signed-rank test, P = 0.961 for all antidepressants). Table 2 includes information about significant differences in class of antidepressants prescribed between patients with and without heart failure.
DISCUSSION
This study found that the prevalence of depression in heart failure patients residing in aged care facility was 36%. Approximately 42% of the patients with heart failure were using at least one antidepressant, and mirtazapine was the most commonly prescribed antidepressant, regardless of whether they had heart failure or not.
The prevalence of depression among heart failure patients identified in this study was higher than the prevalence found by a meta-analysis which was reported to be 21.5%.[1] However, this may be attributed to the setting. An Australian study published in 2007 demonstrated that the prevalence of depression in the residential aged care setting was 32% which was higher compared to the elderly residing in the community.[16] Similarly, Snowdon and Fleming reported a depression prevalence of around 35% in residents of aged care facilities in Australia.[17]
Mirtazapine was found to be the most commonly prescribed antidepressant in heart failure patients. This is in line with another study that reported mirtazapine being the most commonly used antidepressant in nursing homes.[18] Despite its wide use, adverse events have been reported with the use of mirtazapine. Mirtazapine has the potential to cause QT prolongation and weight gain.[2] Furthermore, it is commonly known to cause localized and generalized edema as a side effect;[19] however, it is not known whether this edema can adversely affect the health of heart failure patients. Nonetheless, mirtazapine was reported to have a low rate of cardiovascular side effects when compared to other antidepressants.[20,21] In addition, in relation to cardiovascular diseases, mirtazapine was found to be safe and effective in managing postmyocardial infarction depression.[22] This in itself is of interest and further investigation is needed to evaluate mirtazapine's efficacy and safety among heart failure patients, which should guide the development of a treatment guideline for the management of depression among this patient group.
SSRIs, in particular, sertraline and escitalopram, were the second and third most commonly used antidepressants, respectively. This finding is not surprising considering these agents are the first-line treatments for depression according to different guidelines.[4,5,6,7] However, recent evidence from two large clinical trials does not support their use in the heart failure population.[10,11]
SSRIs were the most commonly prescribed antidepressant class in this study. This is in line with other antidepressant prescribing patterns reported in the elderly.[23,24] Interestingly, one study in the elderly from Korea reported TCAs to be the most commonly used antidepressant class.[25] Despite being considered more effective than SSRIs in treating depression,[6] the safety profile of TCAs precludes them from being used in patients with concurrent cardiovascular disease.[2] In addition, TCAs should be avoided in the elderly due to their adverse effect profile.[26]
A significant proportion of the patients with heart failure in this study were using antidepressants with no clear recorded indication (31.5%). A study from Sweden conducted in nursing homes reported that 33% of the patients used antidepressants without a definitive diagnosis of depression.[27] Similarly, a study involving aged veterans found that 30% of the patients were using a psychotropic medication without a psychiatric diagnosis.[28] When accounting for psychiatric and nonpsychiatric indications of antidepressants, a large cohort from the United States of America found that 27% of antidepressant users had no clear indication for their use.[29] One of the factors leading to this rate can be underdiagnosis of depression as depression in heart failure may be poorly detected.[3,8] Another factor could be incomplete documentation.[28] Of concern with the use of antidepressants are their cardiovascular side effects; however, these adverse events vary among the different antidepressant groups.[21] The safety profile of TCAs and MAOIs renders them the least suitable in patients with concurrent cardiovascular disease.[2] Mirtazapine and SSRIs were found to have the best cardiovascular side effect profiles.[21] Nonetheless, the use of antidepressants without a clear indication should be evaluated.
Although patients with heart failure have a different response to first-class antidepressants,[10,11,12] this study found that there was no significant difference in antidepressant prescribing between patients with and without heart failure. The absence of clear guidelines for the management of depression in heart failure patients[2,8] can be a contributing factor to the lack of difference.
This study has identified that elderly patients are often prescribed a large number of medications. Although it is beyond the scope of the present study, as polypharmacy and other medications taken by the elderly population may have an effect on the cardiovascular system, this study highlights a need for future studies to be conducted to ascertain the effects of polypharmacy on depression and/or the cardiovascular system.
Every study has its limitations. Records with incomplete data were excluded from the analysis. The results are dependent on the accuracy of data entry by the data source. As this study only analyzed records of RMMRs, the findings are limited to residents of residential aged care facilities and may not be representative of the entire heart failure population.
This is the first study in Australia to examine the antidepressant prescribing patterns in patients with heart failure residing in aged care facilities. The study has identified that almost half of the patients with heart failure were prescribed at least one antidepressant, for a range of indications, and some with no clear indication. Mirtazapine was the most commonly prescribed antidepressant in this patient group, followed by the SSRIs sertraline and escitalopram. There was no significant difference in antidepressant prescribing between patients with and without heart failure.
This study has highlighted a need for future studies, such as a randomized controlled trial, to evaluate the efficacy and safety of antidepressants, particularly mirtazapine, in the management of depression, specifically in patients with heart failure. A need for the development of treatment guidelines for depression specifically in patients with heart failure was also identified.
AUTHORS' CONTRIBUTION
Ruba Marashdeh and Tin Fei Sim proposed the concept and conducted literature search. All authors contributed to the design, data acquisition, and analysis. Ruba Marashdeh and Richard Parsons conducted the statistical analysis. Ruba Marashdeh and Tin Fei Sim prepared the manuscript. All authors participated in the editing, reviewing and approval of the final version of the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to acknowledge Dr. Natalie Soulsby at Ward Medication Management for providing the data for this study.
REFERENCES
- 1.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–37. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 2.Teply RM, Packard KA, White ND, Hilleman DE, DiNicolantonio JJ. Treatment of depression in patients with concomitant cardiac disease. Prog Cardiovasc Dis. 2016;58:514–28. doi: 10.1016/j.pcad.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Chong VH, Singh J, Parry H, Saunders J, Chowdhury F, Mancini DM, et al. Management of noncardiac comorbidities in chronic heart failure. Cardiovasc Ther. 2015;33:300–15. doi: 10.1111/1755-5922.12141. [DOI] [PubMed] [Google Scholar]
- 4.Depression in Adults with a Chronic Physical Health Problem: Recognition and Management (CG91) London: National Institute for Health and Clinical Excellence; 2009. [Last accessed on 2016 May 28]. National Institute for Health and Clinical Excellence. Available from: https://www.nice.org.uk/guidance/cg91/resources/depression-in-adults-with-chronic-physical-health-problem-recognition-and-management-975744316357 . [Google Scholar]
- 5.Depression in adults [online database] Therapeutic Guidelines Ltd. 2015. [Last accessed on 2017 May 28]. Available from: https://tgldcdp.tg.org.au/etgcomplete .
- 6.Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand college of psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. 2015;49:1087–206. doi: 10.1177/0004867415617657. [DOI] [PubMed] [Google Scholar]
- 7.Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, et al. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. USA: American Psychiatric Association; 2010. [Google Scholar]
- 8.DeJongh B, Birkeland K, Brenner M. Managing comorbidities in patients with chronic heart failure:First, do no harm. Am J Cardiovasc Drugs. 2015;15:171–84. doi: 10.1007/s40256-015-0115-6. [DOI] [PubMed] [Google Scholar]
- 9.Gottlieb SS, Kop WJ, Thomas SA, Katzen S, Vesely MR, Greenberg N, et al. Adouble-blind placebo-controlled pilot study of controlled-release paroxetine on depression and quality of life in chronic heart failure. Am Heart J. 2007;153:868–73. doi: 10.1016/j.ahj.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 10.O'Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, et al. Safety and efficacy of sertraline for depression in patients with heart failure: Results of the SADHART-CHF (Sertraline against depression and heart disease in chronic heart failure) trial. J Am Coll Cardiol. 2010;56:692–9. doi: 10.1016/j.jacc.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angermann CE, Gelbrich G, Störk S, Gunold H, Edelmann F, Wachter R, et al. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: The MOOD-HF randomized clinical trial. JAMA. 2016;315:2683–93. doi: 10.1001/jama.2016.7635. [DOI] [PubMed] [Google Scholar]
- 12.Fraguas R, da Silva Telles RM, Alves TC, Andrei AM, Rays J, Iosifescu DV, et al. Adouble-blind, placebo-controlled treatment trial of citalopram for major depressive disorder in older patients with heart failure: The relevance of the placebo effect and psychological symptoms. Contemp Clin Trials. 2009;30:205–11. doi: 10.1016/j.cct.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Roose SP, Glassman AH, Giardina EG, Johnson LL, Walsh BT, Woodring S, et al. Nortriptyline in depressed patients with left ventricular impairment. JAMA. 1986;256:3253–7. [PubMed] [Google Scholar]
- 14.Roose SP, Glassman AH, Giardina EG, Johnson LL, Walsh BT, Bigger JT, Jr, et al. Cardiovascular effects of imipramine and bupropion in depressed patients with congestive heart failure. J Clin Psychopharmacol. 1987;7:247–51. [PubMed] [Google Scholar]
- 15.Cohn JB, Wilcox CS, Goodman LI. Antidepressant efficacy and cardiac safety of trimipramine in patients with mild heart disease. Clin Ther. 1993;15:114–26. [PubMed] [Google Scholar]
- 16.Anstey KJ, von Sanden C, Sargent-Cox K, Luszcz MA. Prevalence and risk factors for depression in a longitudinal, population-based study including individuals in the community and residential care. Am J Geriatr Psychiatry. 2007;15:497–505. doi: 10.1097/JGP.0b013e31802e21d8. [DOI] [PubMed] [Google Scholar]
- 17.Snowdon J, Fleming R. Recognising depression in residential facilities: An Australian challenge. Int J Geriatr Psychiatry. 2008;23:295–300. doi: 10.1002/gps.1877. [DOI] [PubMed] [Google Scholar]
- 18.Shah S, Schoenbachler B, Streim J, Meeks S. Antidepressant prescribing patterns in the nursing home: Second-generation issues revisited. J Am Med Dir Assoc. 2012;13:406.e13–8. doi: 10.1016/j.jamda.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Product Information Axit Mirtazapine. Therapeutic Goods Administration. 2017. [Last accessed on 2018 Apr 10]. Available from: https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP.2010.PI.05345.3&d=2018040916114622483&d=2018041016114622483 .
- 20.Mago R, Tripathi N, Andrade C. Cardiovascular adverse effects of newer antidepressants. Expert Rev Neurother. 2014;14:539–51. doi: 10.1586/14737175.2014.908709. [DOI] [PubMed] [Google Scholar]
- 21.Spindelegger CJ, Papageorgiou K, Grohmann R, Engel R, Greil W, Konstantinidis A, et al. Cardiovascular adverse reactions during antidepressant treatment: A drug surveillance report of German-speaking countries between 1993 and 2010. Int J Neuropsychopharmacol. 2014;18:pii: pyu080. doi: 10.1093/ijnp/pyu080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Honig A, Kuyper AM, Schene AH, van Melle JP, de Jonge P, Tulner DM, et al. Treatment of post-myocardial infarction depressive disorder: A randomized, placebo-controlled trial with mirtazapine. Psychosom Med. 2007;69:606–13. doi: 10.1097/PSY.0b013e31814b260d. [DOI] [PubMed] [Google Scholar]
- 23.Sultana J, Italiano D, Spina E, Cricelli C, Lapi F, Pecchioli S, et al. Changes in the prescribing pattern of antidepressant drugs in elderly patients: An Italian, Nationwide, population-based study. Eur J Clin Pharmacol. 2014;70:469–78. doi: 10.1007/s00228-013-1636-z. [DOI] [PubMed] [Google Scholar]
- 24.Huang YC, Wang LJ, Chong MY. Differences in prescribing psychotropic drugs for elderly with depression. Acta Neuropsychiatr. 2016;28:296–303. doi: 10.1017/neu.2016.4. [DOI] [PubMed] [Google Scholar]
- 25.Kwon K, Shin J, Kim Y, Choi N, Lee J, Park B. Prescribing Patterns of Antidepressants for the Elderly Depressive Patients in Korea. Pharmacoepidemiol Drug Saf. 2015;24:386. [Google Scholar]
- 26.American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616–31. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Midlöv P, Andersson M, Ostgren CJ, Mölstad S. Depression and use of antidepressants in Swedish nursing homes: A 12-month follow-up study. Int Psychogeriatr. 2014;26:669–75. doi: 10.1017/S1041610213002354. [DOI] [PubMed] [Google Scholar]
- 28.Wiechers IR, Kirwin PD, Rosenheck RA. Increased risk among older veterans of prescribing psychotropic medication in the absence of psychiatric diagnoses. Am J Geriatr Psychiatry. 2014;22:531–9. doi: 10.1016/j.jagp.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 29.Simon GE, Stewart C, Beck A, Ahmedani BK, Coleman KJ, Whitebird RR, et al. National prevalence of receipt of antidepressant prescriptions by persons without a psychiatric diagnosis. Psychiatr Serv. 2014;65:944–6. doi: 10.1176/appi.ps.201300371. [DOI] [PMC free article] [PubMed] [Google Scholar]


