Abstract
Context
Prior literature has focused on the impact of informal caregiving (presence of a family member in the home or nearby) on caregiver employment, but little research has analyzed the impact of informal caregiving on health care utilization patterns.
Objective
To study the effect of informal caregivers on postacute care and recovery of Medicare patients.
Design
We used cross-sectional Health Plan administrative data to measure differences in health care utilization for Medicare patients who did and did not have coresident adult caregivers available. We identified coresident caregivers as those residing at the same postal address as discharged patients. Analysis was a combination of Poisson and logit models.
Main Outcome Measures
Length of hospitalization, type of hospitalization (ambulatory-care sensitive vs not), likelihood of discharge to postacute care (skilled nursing facility or home health), and likelihood of hospital readmission and postdischarge Emergency Department visits.
Results
Patients with caregivers were discharged after shorter hospital lengths of stay and were less likely to require postacute emergency care, home health services, or discharge to skilled nursing facilities. Savings were smaller when caregivers were younger, in poor health, or female. We extrapolated the reduced utilization associated with a coresidential caregiver to estimate Medicare savings of $514 million in 2015.
Conclusion
By calculating the impact of informal caregiving on patterns of health care utilization, we support the need to integrate the availability of caregivers into discharge planning. Future quantification of differences by caregiver characteristics is important.
Keywords: care transitions, health care utilization, informal caregiving, inpatient care, Medicare
INTRODUCTION
Care at home is increasing because of an aging population, technologic advances, and reimbursement pressure. Caregiving in the home, both formal and informal, is the backbone of health care for elderly individuals. Effective postacute care after an inpatient stay is an important aspect of high-quality care and has been shown to prevent hospital readmissions and complications.1–3 The growing emphasis on safe discharge under Medicare’s Hospital Readmission Reduction Program reinforces the need for outstanding postacute care in the home. The presence of a family member in the home or nearby has been argued to serve as a substitute for both formal care and institutional monitoring.2,4 The literature primarily focuses on the impact of informal caregiving on caregiver employment.5–7 Some survey-based research documented characteristics of nonresidential8 and coresidential informal caregivers.9 However, because of challenges associated with linking residential information to individual medical records, there is very little research quantifying the benefits from informal caregiving by analyzing its impact on patterns of health care utilization.
This article helps fill this gap by studying the effect of informal caregivers on postacute care and recovery, using administrative data collected by a large Health Plan, linking residential information with insurance claims data. Specifically, we studied how the presence of an informal caregiver in the home affects care transition from an inpatient setting, and the extent to which these effects might be mitigated by the caregiver’s characteristics.
The outcomes of interest include the length of hospitalization, type of hospitalization (ambulatory-care sensitive [ACS] vs not), likelihood of discharge to postacute care (skilled nursing facility [SNF] or home health), as well as the likelihood of hospital readmission and Emergency Department (ED) visits after discharge.
METHODS
Our data were drawn from the administrative files of an upper Midwest Health Plan. The Health Plan offers managed Medicare, managed Medicaid, and commercial products. Our index members were managed Medicare enrollees who experienced an inpatient admission in 2014 or 2015. We excluded residents of long-term care facilities. (Members with a recorded place of service code 33 [custodial care] accounted for less than 1% of our initial sample.) Staff at the Health Plan identified coresident adults (“caregivers”) using an address matching process. They converted the addresses of index members to the US Postal Service standardized format. They then compared these addresses with US Postal Service standardized addresses from the entire adult Health Plan membership in the year of inpatient admission, including Medicare, Medicaid, and commercial products. This address-matching process generated precise and unique matches, even in multiunit housing.
This matching process identified coresident adults for 49% of our index members. Because 2.7% of caregivers were 18 or more years younger than the index member, some of these adults may actually be adult children or other nonspousal family members. The caregivers’ age averaged 8 months older for female index members and 3 years younger for male index members.
The Health Plan extracted detailed enrollment and claims information for claims incurred and paid between January 2013 and July 2016. We used 2013 and 2014 data to identify members’ baseline health status before 2014 and 2015 admissions using resource utilization bands identified by the Johns Hopkins ACG System (www.hopkinsacg.org/). To minimize the likelihood of reverse causality, we measured health status for patients in the year before the admission, although we used current-year health status for their coresident caregivers. We captured data through July 2016 to ensure we observed completed claims-associated care after discharge. The Health Plan matched members’ neighborhood characteristics from the American Community Survey to the enrollment data at members’ census tract or block group level (depending on the statistic). All geographic identifiers were stripped before the dataset was delivered to the research team. The study was deemed exempt from review by the parent organization’s (Quorum Health Corp, Brentwood, TN) institutional review board.
Measures
For index members, we identified the first admission in 2014 to 2015 preceded by at least 180 days without inpatient services, defining the beginning of an episode of inpatient services. For each of these index admissions, we identified the length of hospitalization and designated whether or not the admissions were ACS. ACS admissions are those with diagnoses for which timely and effective outpatient care can help to reduce the risks of hospitalization (www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf). The ACS admissions were determined using the methods available at http://wagner.nyu.edu/faculty/billings/acs-algorithm.
We defined use of transition care after discharge by place of service codes identifying SNF or home health care (HHC) use. Use of a SNF was recorded if it began on the day of inpatient discharge or the subsequent day. The number of HHC visits after an inpatient admission was defined as the number of unique HHC service dates in the 100 days after discharge.
Emergent care after discharge was identified as ED use or an inpatient readmission within 30 and 90 days of the inpatient discharge. Readmissions excluded rehabilitation and chemotherapy admissions, which are often planned.
Empirical Strategy
Our data are cross-sectional, comprising one index admission per member. Inpatient length of stay (LOS) was modeled using a Poisson regression. All other variables were binary indicators, modeled using logit regression.
The variable of interest was the presence of a caregiver in the home; our baseline results predict care patterns as a function of this indicator and control variables. Control variables included annual trend; the index member’s age, sex, and health status (lagged a year to prevent confounding with current care patterns); type of Medicare coverage; and the patient’s neighborhood characteristics. These included distributions of race/ethnicity and education, and measures of poverty and language.
Our supplemental model interacts the presence of a caregiver with the caregiver’s age, sex, and health status to test the influence of these characteristics. For example, if the caregiver’s health status was poor, his/her caregiving effectiveness may be compromised.
RESULTS
Descriptive Results
Summary statistics are displayed in Table 1. Members without an identified caregiver were a year older on average, more likely to be female, and likelier to have dual Medicare/Medicaid coverage compared with members with an identified caregiver. The distributions of health risk and neighborhood characteristics were similar for both groups.
Table 1.
Summary of population characteristics by family status
| Characteristic | No informal caregiver in home | Informal caregivera in home | Total |
|---|---|---|---|
| Number of index members | 10,141 | 9674 | 19,815 |
| Number of informal caregivers | 0 | 9674 | 9674 |
| Percentage of patients with an informal caregiver | 0 | 100.0 | 48.8 |
| Member characteristics | |||
| Average age (SD) | 76.3 (7.9) | 75.1 (6.4) | 75.7 (7.2) |
| Percent female | 59.5 | 41.7 | 50.8 |
| Health status distribution | |||
| Healthy/low risk | 5.0 | 5.0 | 5.0 |
| Medium risk | 36.9 | 39.6 | 38.2 |
| High risk | 31.0 | 30.1 | 30.5 |
| Very high risk | 27.2 | 25.3 | 26.3 |
| Percentage with dual Medicare/Medicaid coverage | 7.1 | 1.7 | 4.5 |
| Neighborhood characteristics (%) | |||
| White, non-Hispanic | 87.4 | 89.9 | 88.6 |
| Less than high school diploma | 8.9 | 7.9 | 8.4 |
| High school diploma/GED | 62.8 | 63.1 | 62.9 |
| 4-y college degree | 28.3 | 29.0 | 28.6 |
| Under the federal poverty limit | 11.3 | 10.0 | 10.7 |
| Speaking English only | 91.9 | 93.2 | 92.5 |
| Informal caregiver characteristics | |||
| Average age (SD) | 73.6 (8.0) | 73.6 (8.0) | |
| Percentage female | 59.3 | 59.3 | |
| Health status distribution | |||
| Healthy/low risk | 9.3 | 9.3 | |
| Medium risk | 49.5 | 49.5 | |
| High risk | 25.6 | 25.6 | |
| Very high risk | 15.7 | 15.7 | |
| Admission and care transition outcomes | |||
| Average index admission length of stay (SD) | 3.21 (3.05) | 3.11 (2.99) | 3.16 (3.02) |
| Percentage of index admissions ACSb | 23.32 | 17.95 | 20.70 |
| Percentage of discharges to SNF | 1.21 | 0.50 | 0.86 |
| Percentage of discharges with HHC within 100 days | 2.64 | 0.61 | 1.65 |
| Percentage of discharges with readmissions | |||
| Within 30 days | 1.23 | 0.33 | 0.79 |
| Within 90 days | 5.86 | 3.93 | 4.91 |
| Percentage of discharges with ED use | |||
| Within 30 days | 12.93 | 11.31 | 12.14 |
| Within 90 days | 22.41 | 18.83 | 20.66 |
“Informal caregiver” is defined as an adult coresident with the index member, as identified in the enrollment data held by the health plan.
Ambulatory-care sensitive admissions were determined using the methods available at http://wagner.nyu.edu/faculty/billings/acs-algorithm.
ACS = ambulatory-care sensitive; ED = Emergency Department; GED = General Educational Development; HHC = home health care; SD = standard deviation; SNF = skilled nursing facility.
Those with a caregiver had a shorter average LOS in the hospital, had fewer ACS admissions, relied less on postacute care (SNF, HHC), and were less likely to require emergent care (readmissions, ED use) after discharge.
In addition, we have summarized the most frequent 10 diagnosis-related groups for index admissions and for 90-day readmissions in Table 2. The presence of joint replacement as a frequent diagnosis-related group in the 90-day readmission list emphasizes that not all readmissions are related to the index admission. We also included in Table 3 the 10 most frequent categories of ACS admissions, which were based on the Billings algorithm used. There was a strong concentration in ACS admissions; 75% were clustered in the top 4 conditions.
Table 2.
Most frequent diagnosis-related groups (DRGs) for index admissions and readmisssions
| DRG | DRG description | Frequency, % |
|---|---|---|
| Most frequent DRGs for index admissions | ||
| 470 | MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W/O MCC | 10.82 |
| 247 | PERC CARDIOVASC PROC W DRUG-ELUTING STENT W/O MCC | 2.68 |
| 871 | SEPTICEMIA OR SEVERE SEPSIS W/O MV 96+ HOURS W MCC | 2.50 |
| 392 | ESOPHAGITIS, GASTROENT & MISC DIGEST DISORDERS W/O MCC | 2.42 |
| 378 | GASTROINTESTINAL HEMORRHAGE WITH CC | 1.8 |
| 194 | SIMPLE PNEUMONIA & PLEURISY W CC | 1.85 |
| 872 | SEPTICEMIA OR SEVERE SEPSIS W/O MV 96+ HOURS W/O MCC | 1.64 |
| 310 | CARDIAC ARRHYTHMIA & CONDUCTION DISORDERS W/O CC/MCC | 1.36 |
| 460 | SPINAL FUSION EXCEPT CERVICAL W/O MCC | 1.34 |
| 292 | HEART FAILURE & SHOCK W CC | 1.31 |
| Most frequent DRGs for 90-day readmissions | ||
| 470 | MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W/O MCC | 5.39 |
| 871 | SEPTICEMIA OR SEVERE SEPSIS W/O MV 96+ HOURS W MCC | 4.78 |
| 291 | HEART FAILURE & SHOCK W MCC | 2.35 |
| 392 | ESOPHAGITIS, GASTROENT & MISC DIGEST DISORDERS W/O MCC | 2.26 |
| 194 | SIMPLE PNEUMONIA & PLEURISY W CC | 2.17 |
| 885 | PSYCHOSES | 2.17 |
| 872 | SEPTICEMIA OR SEVERE SEPSIS W/O MV 96+ HOURS W/O MCC | 2.00 |
| 378 | GASTROINTESTINAL HEMORRHAGE WITH CC | 1.74 |
| 190 | CHRONIC OBSTRUCTIVE PULMONARY DISEASE W MCC | 1.74 |
| 292 | HEART FAILURE & SHOCK W CC | 1.48 |
CARDIOVASC = cardiovascular; CC = complications and comorbidities; DIGEST = digestive; GASTROENT = gastroenteritis; MCC = major complications and comorbidities; MISC = miscellaneous; MV = mechanical ventilation; PERC = percutaneous; PROC = procedure; W = with; W/O = without.
Table 3.
Most frequent conditions indicating an ambulatory-care sensitive admission
| Billings code | Condition | Frequency, % |
|---|---|---|
| 23 | Secondary dehydration | 23.16 |
| 11 | Congestive heart failure | 20.17 |
| 9 | Bacterial pneumonia | 17.70 |
| 8 | Chronic obstructive pulmonary disease | 12.55 |
| 14 | Cellulitis | 6.28 |
| 21 | Kidney/urinary infection | 6.05 |
| 27 | Secondary nutritional deficiencies | 2.25 |
| 10 | Asthma | 2.20 |
| 22 | Primary dehydration | 1.93 |
| 12 | Hypertension | 1.59 |
Impact of a Caregiver on Inpatient Admission and Care Transitions
Results of our multivariate analysis agree with those of the descriptive analysis. Figures 1 and 2, and the baseline results in Table 4, display the impact of having a caregiver on the index admission. Table 4 shows a small but statistically significant decline in average LOS (−0.10 days; p < 0.001; Figure 2) and a 3.6 percentage-point decline in the probability of an ASC admission associated with the presence of a caregiver (p < 0.001; Figure 3). We also estimated the impact of having a caregiver by type of ASC condition (data available on request to the corresponding author [CSC]) and found consistently negative marginal effects across conditions, although our statistical power weakened.
Figure 1.
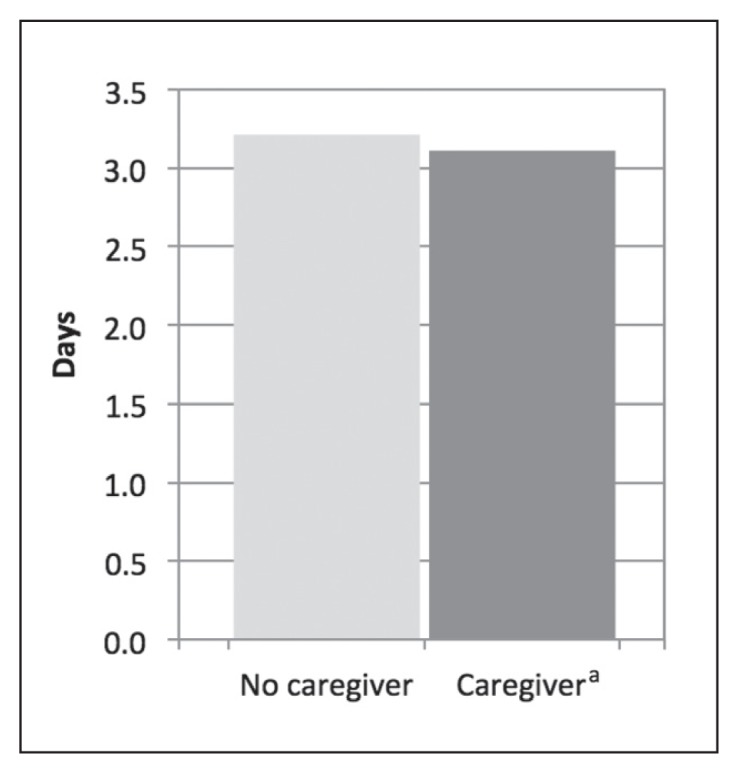
Projected average length of stay by caregiver status.
a Statistical significance of difference is p < 0.001.
Figure 2.
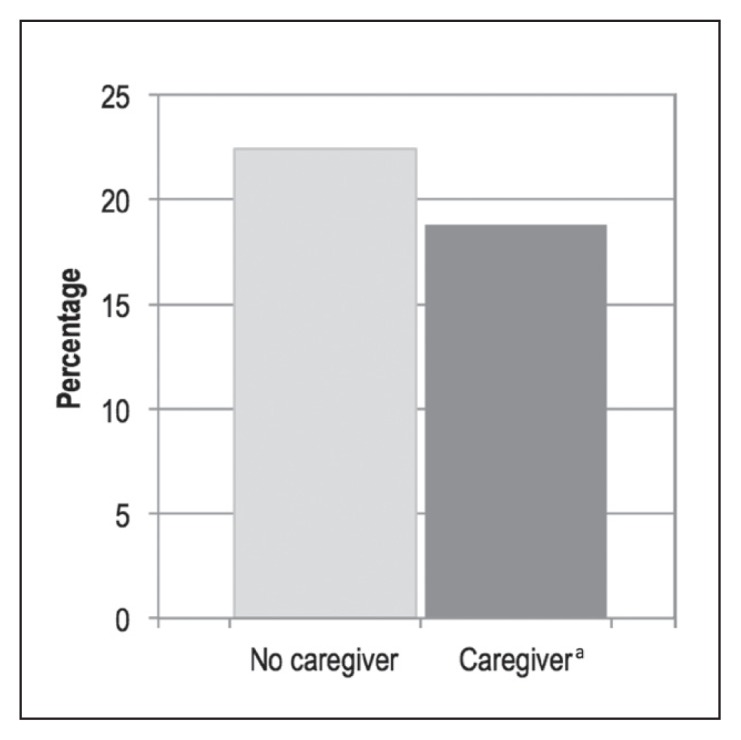
Projected probability index admission was ambulatory care sensitive by caregiver status.
a Statistical significance of difference is p < 0.001.
Table 4.
Differences in impact of informal caregiver’s presence caused by characteristics of the informal caregiver
| Outcome | Baseline modela | With informal caregiver characteristicsb |
|---|---|---|
| Change in average length of stay, d | ||
| Informal caregiver present | −0.10c | −0.12d |
| Increment if informal caregiver is at high/very high health risk | −0.12e | |
| Increment if informal caregiver is female | 0.12d | |
| Increment if informal caregiver is in age range, y | ||
| Less than 55 | 0.18 | |
| 55–64 | −0.32c | |
| 65–74 | Reference | |
| 75–84 | 0.05 | |
| 85 or older | −0.04 | |
| Change in probability of ambulatory-care sensitive admission, ppf | ||
| Informal caregiver present | −0.0361c | −0.0606c |
| Increment if informal caregiver is at high/very high health risk | 0.0049 | |
| Increment if informal caregiver is female | 0.0235d | |
| Increment if informal caregiver is in age range, y | ||
| Less than 55 | 0.0664d | |
| 55–64 | 0.0174 | |
| 65–74 | Reference | |
| 75–84 | 0.0181 | |
| 85 or older | 0.0108 | |
| Change in probability of skilled nursing facility use, ppf | ||
| Informal caregiver present | −0.0033d | −0.0073d |
| Increment if informal caregiver is at high/very high health risk | 0.0019 | |
| Increment if informal caregiver is female | 0.0032 | |
| Increment if informal caregiver is in age range, y | ||
| Less than 55 | −0.0036 | |
| 55–64 | 0.0002 | |
| 65–74 | Reference | |
| 75–84 | 0.0018 | |
| 85 or older | 0.0105 | |
| Change in probability of home health care use, ppf | ||
| Informal caregiver present | −0.0146c | −0.0346c |
| Increment if informal caregiver is at high/very high health risk | 0.0154d | |
| Increment if informal caregiver is female | 0.0082 | |
| Increment if informal caregiver is in age range, y | ||
| Less than 55 | 0.1177e | |
| 55–64 | 0.0474d | |
| 65–74 | Reference | |
| 75–84 | 0.0058 | |
| 85 or older | 0.0175 | |
| Change in probability of 90-day readmission, ppf | ||
| Informal caregiver present | −0.0082d | −0.0082d |
| Increment if informal caregiver is at high/very high health risk | −0.0025 | |
| Increment if informal caregiver is female | 0.0144d | |
| Increment if informal caregiver is in age range, y | ||
| Less than 55 | −0.0180 | |
| 55–64 | −0.0001 | |
| 65–74 | Reference | |
| 75–84 | 0.0071 | |
| 85 or older | 0.0062 | |
| Change in probability of Emergency Department use within 90 days, ppf | ||
| Informal caregiver present | −0.0226c | −0.0226c |
| Increment if informal caregiver is at high/very high health risk | 0.0156 | |
| Increment if informal caregiver is female | 0.0086 | |
| Increment if informal caregiver is in age range, y | ||
| Less than 55 | 0.0407 | |
| 55–64 | −0.0253 | |
| 65–74 | Reference | |
| 75–84 | −0.0021 | |
| 85 or older | −0.0008 | |
The “Informal caregiver present” impact in the baseline model is the average across all informal caregivers.
The “Informal caregiver present” impact in this model is for a reference informal caregiver who is healthy or at low health risk, male, and aged 65 to 74 years. Increments listed are added to this reference change in length of stay or probability to get the impact for informal caregivers of other characteristics.
p < 0.001.
p < 0.05.
p < 0 .01.
−0.01 = 1 percentage-point decrease in probability.
pp = percentage point.
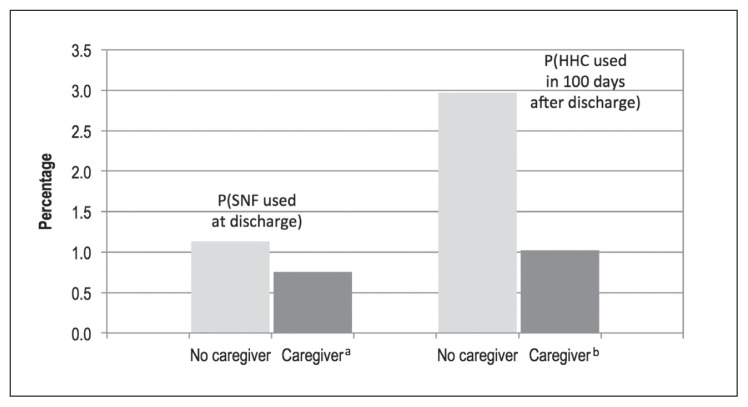
Figure 3.
Projected probability of transitional care used by caregiver status.
a Statistical significance of difference is p < 0.05.
b Statistical significance of difference is p < 0.001.
HHC = home health care; SNF = skilled nursing facility.
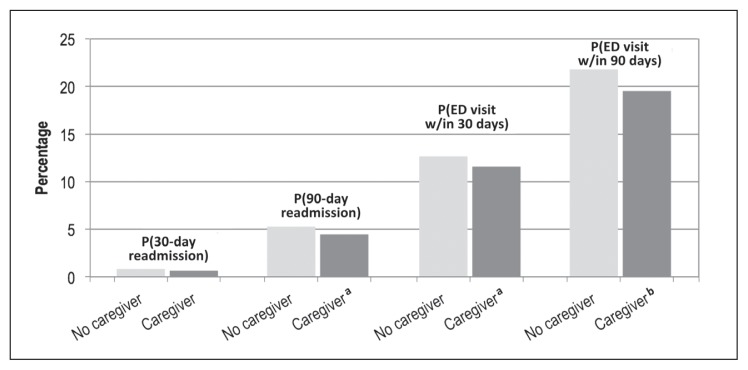
Likewise, these baseline results in Table 4 show a 0.33 percentage-point decrease in the likelihood of a hospital discharge to SNF (p < 0.05; Figure 3) and a 1.46 percentage-point reduction in the likelihood of receiving HHC visits when a caregiver was present (p < 0.001; Figure 3). Finally, baseline results in Table 4 show a projected reduction in emergent care when a caregiver was present. Ninety-day readmissions were reduced by 0.82 percentage points (p < 0.05; Figure 4) and ED use within 90 days was reduced by 2.26 percentage points (p < 0.001; Figure 4). Smaller, 30-day measures are shown in Figure 4, which were statistically significant only for ED use.
Figure 4.
Projected probability of emergent care accessed by caregiver status.
a Statistical significance of difference is p < 0.05.
b Statistical significance of difference is p < 0.001.
ED = Emergency Department.
Economic Value of Informal Caregiving
We calculated the dollar-denominated savings from informal caregiving as the product of average payments with the marginal effects of caregivers. We averaged the total paid by the plan and the member across our sample years for SNF admissions, HHC visits, ED visits, and readmissions. The payments for postinpatient SNF were $5240 per admission, $3593 per postinpatient HHC episode, $410 per ED visit within 90 days of discharge, and $5524 per readmission within 90 days of discharge. Multiplying these payments by the marginal effect of informal caregiving, we compute a savings of $124.31 per index inpatient discharge. Although this is a small dollar amount per individual, the national impact is substantial. There were 9,743,275 Medicare inpatient discharges in 2015.10 We use a 15% readmission rate to estimate 8,472,000 index admissions. Assuming our computed savings per discharge and 48.8% caregiver prevalence are representative of national averages, Medicare benefited from $514 million in savings from informal caregiving in 2015.
Differences in Impact by Spousal Characteristics
To test how these impacts vary by caregiver characteristics, we reestimated our model, including interactions with the caregiver’s age, sex, and health status. The final column of Table 4 shows these differences by caregiver type, displayed next to the average impact from our baseline model. The reference caregiver in this model has low health risk, is male, and is in the age group 65 to 74 years. The impact of this reference caregiver is shown on the “Informal caregiver present” line for each outcome. To obtain the net impact for other types of caregivers, the increments listed should be added to this reference amount. For example, the reference 70-year-old, male, healthy caregiver is expected to reduce the probability of HHC use by 3.46 percentage points. In contrast, a 70-year-old, male, high-health risk caregiver would reduce the probability of HHC use by only 1.92 percentage points (−0.0346 + 0.0154).
The heterogeneity of the caregiver’s impact on LOS is mixed. Sicker caregivers are associated with a shorter LOS; female caregivers, with a longer LOS; and the variance by age is nonlinear.
Among the other outcomes, the presence of a caregiver who is of high health risk increases the probability of HHC use, relative to the presence of a healthy caregiver. Female caregivers are associated with a greater probability of an ACS admission and a higher probability of a 90-day readmission, relative to the presence of a male caregiver. Caregivers under age 65 years are associated with a higher probability of an ACS admission and a greater need for HHC use.
Robustness Testing
To test the robustness of our results, we reestimated our baseline model using populations in which the spouse was less likely to still be on an employment-based Health Plan from another carrier, and thus missingness of data should be reduced (females only, members aged 70 years and older). In these subgroups, we found that the impact of caregivers on patterns of care were nearly identical to those presented here.
DISCUSSION
The reductions in utilization when a coresident caregiver is present, although small at the member level, are meaningful when aggregated to the national level. Moreover, the heterogeneity in the effect of informal caregiving on care utilization by caregiver characteristics deserves further discussion.
In general, we would expect to see the greatest reductions in utilization when the caregiver is young and in good health and, because of caregiving acculturation, when the caregiver is female. However, our results show that this is not always the case. Specifically, we found that the index admission had a shorter LOS when the caregiver was in poor health, a longer LOS when the caregiver was female, and the impact of caregiver age on LOS was nonlinear. We found increased probability that the index admission was an ambulatory-care-sensitive admission when the caregiver was female and/or under age 65 years. Unexpected outcomes in postdischarge care occurred with higher readmission rates for female caregivers and higher home health use for caregivers under age 65 years.
We can develop possible conceptual models that explain these initially counterintuitive results. For example, caregiving acculturation may make female caregivers more sensitive to changes in patient health and more likely to advocate for aggressive care, leading to more ambulatory-care sensitive admissions, higher frequency of readmissions, and longer lengths of stay. Longer lengths of stay and more HHC use when the caregiver was younger than age 65 years may indicate conflict between caregiving and continued employment. Finally, shorter lengths of stay when the caregiver was in poor health may indicate reciprocal caregiving, with the admitted patient anxious to be discharged and get home to care for an ailing spouse. It is clear that additional quantitative and qualitative research is needed to help us understand these complex patterns.
Limitations
Our data came from a single Midwest carrier; hence, our results may not be generalizable to other regions across the nation. In addition, we have chosen to focus on Medicare patients because of the higher relevance of inpatient use for those older than age 65 years. The impact of family support is likely different when the index population is younger.
It is important to note that this carrier’s Medicare coverage was a Medicare cost product, not a Medicare Advantage product. Although this distinction primarily affects the way the carrier is reimbursed by Medicare and does not directly affect the way the carrier reimburses providers, there may be situations where there is a trickle-down impact. This risk to generalizability may be greater when the carrier and the providers are vertically integrated.
In our data, we identified an adult in the home through address matching by the Health Plan. Because most caregivers in our data are spouses, it is reasonable to expect they received their Medicare coverage from the same carrier. Nevertheless, it is possible that a caregiver was not identified in our sample because s/he was uninsured or was insured by carriers other than the Health Plan contributing data to our study. This is particularly likely when one member reached age 65 years and qualified for Medicare while his/her younger spouse still received employment-based coverage through a different carrier. We were also unable to identify sources of support who were not coresident with the index member. However, unidentified caregivers will bias our parameter estimates toward zero; therefore, our results can be viewed as a lower bound on the impact of caregivers.
In addition, the address of record may not reflect the residence of the patient. Although the carrier nominally records both address of residence (used for address matching) and mailing address, it is possible that these are confounded. The risk is greatest in situations such as the patient residing in custodial care with paperwork sent elsewhere, or an adult child receiving mail to provide financial and logistical support to his/her parents. In the latter case, we would have a similar bias toward zero as discussed in the preceding paragraph. To address the former scenario, we minimized the risk of treating a patient in custodial care as a patient without a caregiver by removing all observations in which the patient received any care with placement of service code 33, indicating custodial care. We believe it is unlikely that a patient would have both incorrectly recorded addresses and an index inpatient admission without any in-home care before or after the admission reflecting the placement of service code 33, but recognize that there is a risk of this misidentification.
Finally, it should be noted that the observed readmission rates we identified are dramatically lower than published statistics for Medicare populations. There are a number of explanatory factors, including the very low readmission rates in our geographic region and the index admission selection process we use, but none completely explain this difference. Because this is a Medicare cost product, there is a real risk that our use of claims data means that we are unable to observe all readmissions. This, again, biases our estimate of the impact of caregivers toward a lower bound.
Policy Implications
The need for and provision of care at home has been on the rise because of the aging of the US population, prevalence of chronic conditions, and shorter hospital stays.11 About 66 million Americans in 2011 benefited from 1 or more unpaid caregivers, typically family caregivers.11 By 2030, 1 in 5 adults will be aged 65 years or older, increasing the demand for caregiving—formal and informal.11
The important role that families play in discharge planning has been discussed12 but not quantified. By calculating the impact of informal caregiving on patterns of health care utilization, we support the need to integrate the availability of caregivers as an input into discharge planning. Our documentation of differential impact by caregiver characteristics suggests this is an important area for future investigation. Although continued systematic integration of informal caregivers into discharge planning decisions is suggested to yield important benefits for complex and frail patients in the US and abroad,13–16 our findings that patients are more likely to be discharged sooner and to home settings when a caregiver is present suggest that the discharge process is already, at least to some degree, attentive of informal caregiving.
CONCLUSION
We estimated the impact of informal caregivers after an inpatient discharge to be substantial when aggregated to the national level. Continued integration of caregivers into discharge planning, taking into account the differences in caregiver characteristics, is an important factor in the efficient delivery of health care.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications performed a primary copy edit.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Boling PA. Care transitions and home health care. Clin Geriatr Med. 2009;25(1):135–48. viii. doi: 10.1016/j.cger.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Van Houtven CH, Norton EC. Informal care and Medicare expenditures: Testing for heterogeneous treatment effects. J Health Econ. 2008 Jan;27(1):134–56. doi: 10.1016/j.jheale.co.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Weaver FM, Weaver BA. Does availability of informal care within the household impact hospitalisation? Health Econ Policy Law. 2014 Jan;9(1):71–93. doi: 10.1017/S1744133113000169. [DOI] [PubMed] [Google Scholar]
- 4.Buckner L, Yeandle S. Valuing careers: Calculating the value of unpaid care. London, UK: Carers UK: 2011. [Google Scholar]
- 5.Haines KJ, Denehy L, Skinner EH, Warrillow S, Berney S. Psychosocial outcomes in informal caregivers of the critically ill: A systematic review. Crit Care Med. 2015 May;43(5):1112–20. doi: 10.1097/CCM.0000000000000865. [DOI] [PubMed] [Google Scholar]
- 6.Lilly MB, Laporte A, Coyte PC. Labor market work and home care’s unpaid caregivers: A systematic review of labor force participation rates, predictors of labor market withdrawal, and hours of work. Milbank Q. 2007 Dec;85(4):641–90. doi: 10.1111/j.1468-0009.2007.00504.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmitz H, Westphal M. Informal care and long-term labor market outcomes. J Health Eco. 2017 Dec;56:1–18. doi: 10.1016/j.jhealeco.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Kalwij A, Pasini G, Wu M. Home care for the elderly: The role of relatives, friends and neighbors. Review of Economics of the Household. 2014 Jun;12(2):379–404. doi: 10.1007/s11150-012-9159-4. [DOI] [Google Scholar]
- 9.Mentzakis E, McNamee P, Ryan M. Who cares and how much: Exploring the determinants of co-residential informal care. Review of Economics of the Household. 2009;7(3):283–303. doi: 10.1007/s11150-008-9047-0. [DOI] [Google Scholar]
- 10.Inpatient charge data FY 2015 [Internet] Baltimore, MD: Centers for Medicare & Medicaid Services; updated 2018 Mar 1 [cited 2018 Jan 25]. Available from: www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Inpatient2015.html. [Google Scholar]
- 11.Collins LG, Swartz K. Caregiver care. American Family Physician. 2011 Jun 1;83(11):1309–17. [PubMed] [Google Scholar]
- 12.Popejoy LL. Complexity of family caregiving and discharge planning. J Fam Nurs. 2011 Feb;17(1):61–81. doi: 10.1177/1074840710394855. [DOI] [PubMed] [Google Scholar]
- 13.Hahn-Goldberg S, Jeffs L, Troup A, Kubba R, Okrainec K. “We are doing it together”; The integral role of caregivers in a patients’ transition home from the medicine unit. PLoS One. 2018 May 24;13(5):e0197831. doi: 10.1371/journal.pone.0197831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shyu YI. The needs of family caregivers of frail elders during the transition from hospital to home: A Taiwanese sample. J Adv Nurs. 2000 Sep;32(3):619–25. doi: 10.1046/j.1365-2648.2000.01519.x. [DOI] [PubMed] [Google Scholar]
- 15.Jeffs L, Saragosa M, Law MP, Kuluski K, Espin S, Merkley J. The role of caregivers in interfacility care transitions: A qualitative study. Patient Prefer Adherence. 2017 Aug 21;11:1443–50. doi: 10.2147/PPA.S136058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bowman KF, Rose JH, Kresevic D. Family caregiving of hospitalized patients. Caregiver and nurse perceptions at admission and discharge. J Gerontol Nurs. 1998 Aug;24(8):8–16. doi: 10.3928/0098-9134-19980801-05. [DOI] [PubMed] [Google Scholar]