Abstract
Background
Japan has experienced a low prevalence of childhood obesity. The Japanese nationwide school lunch program is suggested to have helped this phenomenon, but it has not been proven.
Methods
From official statistics, we combined annual data for 2006–15 about the prefecture-level school lunch coverage rate for public junior high school students and the prefecture-level nutritional indicators calculated by randomly selected age–sex groups of 13–15-year olds: the percentage of overweight, obese or underweight children, who are 20% heavier, 30% heavier or 20% lighter than the standard weight by sex, age and height; and mean body weight (kg) or height (cm). We estimated the impact of the school lunch coverage rate on the nutritional indicators in subsequent years, adjusting for the lagged dependent variable and dummies for prefecture, age and year.
Results
A 10 percentage point increase in the prefecture-level school lunch coverage rate significantly decreased the percentage of overweight (0.37%, 95% CI: 0.18–0.56) and obesity (0.23%, 0.10–0.37) in subsequent years among boys, but not among girls. No significant effect on the percentage of underweight or mean body weight/height was observed for either sex.
Conclusions
Appropriate nutritional intake through school lunch may be effective to reduce childhood obesity.
Keywords: children, food and nutrition, obesity
Introduction
Obesity and overweight in children have steadily increased in recent decades in developed and developing countries.1,2 Overweight children are more likely to be overweight or obese as adults, compared with their normal-weight peers.3,4 Preventing overweight in children is expected to be a promising approach to reducing obesity and obesity-related diseases in the future. Because children spend a substantial part of their daily lives at school, developing appropriate and effective school-based policies and interventions to reduce overweight and obesity is essential.5,6
The prevalence of childhood overweight and obesity in Japan has been kept low historically,7 and rather decreases in recent years,8,9 in contrast to other developed and developing countries.1 The reason for this phenomenon has attracted attention and some articles suggest that it may be partly explained by the Japanese school lunch program (SLP).10–12 The SLP in Japan has long been part of dietary education, designed to achieve children’s sound development, convey an understanding of portion size and meal balance, and nationwide serve managed and uniform meals based on adequately regulated nutrition standards.13 Thus, we hypothesized that the SLP keeps children’s weight at an appropriate level; it may help thin children to increase their weight and obese children to decrease their weight. However, it has not been demonstrated whether the SLP actually can reduce childhood overweight/obesity because overall energy intake and nutritional quality can be easily compensated by other meals and snacks. Therefore, this study aimed to investigate the impact of the SLP on overweight and obesity among early adolescents.
The summary of SLP in Japan
In Japan, the School Lunch Program Act of 1954 encouraged municipalities to develop the SLP for 6-year elementary schools and three-year junior high schools.14 School lunch was, at first, used to prevent malnutrition in children, but later was regulated as a part of dietary and nutritional education by the government’s educational guideline. By 2006, the SLP in Japan covered 98.6% of elementary school students but only 69.5% of junior high school students.15 Recently, however, the SLP has been gradually expanding even in junior high schools, but this has differed markedly across prefectures (the first level of administrative divisions in Japan) reflecting differing historical contexts and financial restrictions.15
The SLP offers a uniform menu including staple food, main dish, side dish, drink and dessert (Fig. 1) to all children in each school with the SLP 5 days per week,13 unlike the cafeteria-style school lunch in the USA and the UK.16,17 The children basically have no choice regarding menu items or whether to eat the school lunch or to bring their lunch from home (except for those with food allergies or other health problems). The proportion of junior high school students who always left food on their plate was <10% in 2010.18 Another survey reported that the percentage of the leftover meals to the provided meals in school lunch was quite low (6.9% on average in 2013).19 In contrast, the children in schools without the SLP bring their lunch from home or buy meals not regulated by the School Lunch Program Act in school cafeterias.
Fig. 1.
Examples of the menus provided in the school lunch program in Japan. Reprinted with permission from the website of Shinagawa Municipal Ebara Dai-ichi Junior High School .
The school lunch nutrition standards, regulated by the School Lunch Program Act, set appropriate levels of energy (850 kcal), protein (19–35 g), fat-to-energy ratio (25–30% of total energy), calcium (470 mg), magnesium (140 mg), zinc (3 mg), iron (4 mg), vitamin A expressed as retinol activity equivalents (210 μg RAE), vitamin B1 (0.6 mg), vitamin B2 (0.6 mg), vitamin C (33 mg), salt (3 g) and dietary fiber (7.5 g) (bracketed numbers are the reference amounts per lunch for junior high school students in the 2009 school lunch nutrition standards).20 Based on these criteria, school lunch is cooked in each school or in a central school lunch center under the supervision of nutritionists.
Methods
Data
Data from two nationwide survey reports, the ‘Annual Reports of School Lunch Implementation Survey’15 (SLIS) and the ‘Annual Reports of School Health Statistics Survey’21 (SHSS), conducted by the Ministry of Education, Culture, Sports, Science and Technology, were used. The annual school lunch coverage rate (the percentage of public school students receiving school lunches at prefecture level as of May 1) among junior high school students was extracted from the SLIS from 2006 to 2015 for all prefectures (except Fukushima, Miyagi and Iwate prefectures in 2011 because of the Great East Japan Earthquake).15 Yearly data on mean body height and weight and the percentages of overweight, obese, and underweight children in each prefecture by age and sex were extracted from the SHSS. These data were calculated using body height and weight measured yearly from April to June among stratified randomly selected samples of children who lived in a prefecture; the samples comprised around 5% of all children aged 5–17 in Japan.21 The SLIS and SHSS included prefecture-level aggregated data, but not individual-level or school-level data. Using the data on children aged 13–15 years (8th–10th grades) on 1 April of each year, panel data were constructed in which the unit of observation was a cohort determined by sex, prefecture and birth year (denoted as ‘cohort’ below). No ethical approval was required because published aggregated data were used.
Quality control
For the anthropometry in the SHSS, the School Health and Safety Act22 required health professionals to measure body weight without clothes or by subtracting the weight of the clothes. Children needed to keep still on the scale. Also, the Act required measuring body height without shoes and socks. Children needed to close both heels; bring the back, the buttocks, and the heel upright against the pillar of the height meter; hang both arms down at sides; and keep the head in a normal position.
Outcomes
Five prefecture-level indicators of nutritional conditions as outcomes were used: (i) ‘overweight percentage’ (the percentage of overweight children); (ii) ‘obesity percentage’ (the percentage of obese children); (iii) ‘underweight percentage’ (the percentage of underweight children); (iv) mean body weight (kg); and (v) mean body height (cm). These indicators were measured and calculated by age–sex group across prefectures annually. We included underweight percentage as an outcome because the SLP was originally introduced to control malnutrition. In Japan, overweight, obesity, and underweight in children aged 5–17 are evaluated using the ratio of measured weight to the expected ‘standard weight’ determined by sex, age, and height. The standard weight was calculated using ~70 000 children from the 2000 Annual Reports of School Health Statistics Survey.23 The present study regarded those who were 20% heavier, 30% heavier or 20% lighter than the standard weight as ‘overweight’, ‘obese’ or ‘underweight,’ respectively.23 A prior study showed that, among children with average body height, being overweight/underweight (20% heavier/lighter than the standard weight) corresponds to a body mass index (BMI: kg/m2)-for-age percentile of over 86–89%/under 2–6% and being 30–36% heavier than the standard weight corresponds to a 95% BMI-for-age percentile. This indicates that our definition of ‘overweight’ was a little stricter and our definition of ‘obesity’ was a little milder, compared with those used by the Centers for Disease Control and Prevention.23,24 It has also been reported that the ratio of measured weight to the standard weight is associated with risk factors for cardiovascular diseases such as uric acid, visceral fat and cytokines, including adiponectin and leptin.25–27 Our definition of ‘underweight’ is also slightly stricter compared with ‘moderate wasting’ used by the World Health Organization.28
Explanatory variables
The previous year’s school lunch coverage rate (%) among public junior high schools in a prefecture was used as the main explanatory variable. This value was supposed to reflect the percentage of children receiving school lunch in the prefecture because the proportion of non-public junior high schools students was quite low in Japan (only 7.9%).29 The 1-year lagged dependent variable and dummy variables for prefecture, year and age were included as covariates. The prefecture dummy could control for factors such as income, education, health and dietary indices of residents at prefecture level, which could be confounding factors in the association between school lunch coverage rate and overweight/obesity percentage.
Statistical analyses
A lagged dependent variable model was applied for each outcome variable by sex, using the following equation:
| (1) |
Here, j = prefecture, t = year and a = cohort as determined by birth year, sex and prefecture. represents each of the four outcomes measured for the children’s cohort a in prefecture j at year t. is the school lunch coverage rate (%) among public junior high school students in prefecture j in year t−1. included the dummies for prefecture, age and year. is an idiosyncratic error term. We dispensed with the cohort-level time-invariant unobserved effect, because we directly controlled for the lagged dependent variable. An ordinary least squares (OLS) estimation was applied. The standard errors were clustered by cohort a. The coefficients of were estimated and reported. Our estimation strategy essentially compared observations with large school lunch coverage rates to observations with small school lunch coverage rates. Appendix 1 demonstrates that (or ) indicates individual-level effects of receiving school lunch on the probability of being overweight/obese/underweight (or body weight/height). It means that (or ) represents the prefecture-level impact of one percentage point change in the school lunch coverage rate on the percentage of overweight/obese/underweight children (or mean body weight/height). We dropped data where lagged variables were not defined. P values below 0.05 were interpreted as statistically significant. All analyses were carried out using Stata version 14.30
Sensitivity analyses
Two sensitivity analyses were conducted. First, a falsification test, where we evaluated the effect of school lunch coverage rate in junior high school on the outcomes among children aged 7–12 in the same way to the main analyses, was conducted. Since they had been in elementary school in the previous year and the school lunch coverage rate was constantly almost 100% in public elementary school since 2006,15 the results of this falsification test should be null, which means the confounding of omitted factors were not strong and therefore the equation (1) was acceptable. Second, although few children in Japan were in non-public junior high schools, some prefectures, especially in urban areas, had a relatively greater proportion of children attending these schools. Thus, we omitted information from prefectures where more than 10% of junior high school students attended non-public schools in 2015,29 and the analysis was repeated using the data from this restricted sample.
Results
Descriptive statistics
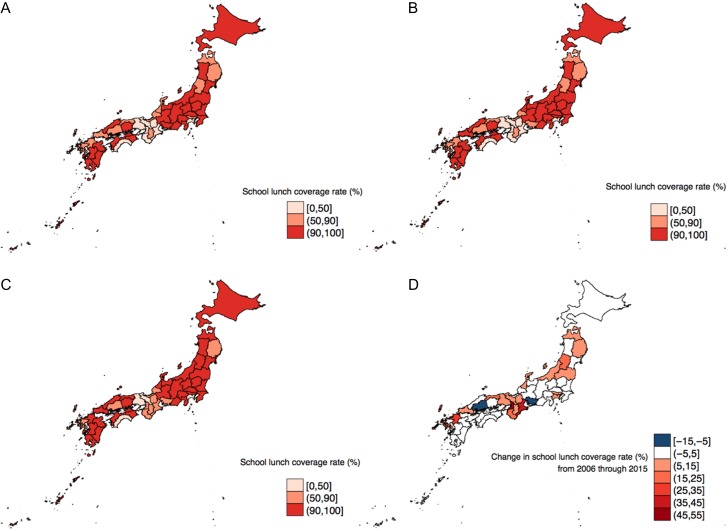
Figure 2 illustrates the trends in the school lunch coverage rate among public junior high school students. In 2006, about half of the 47 prefectures had school lunch coverage rates over 90% (panel A). Three-fifths and two-thirds of the prefectures had attained school lunch coverage rates over 90% by 2010 and 2015, respectively (panels B and C). Two-fifth of the prefectures experienced 5 or more percentage point increase in school lunch coverage rate from 2006 through 2015 (panel D). The annual school lunch coverage rates for each prefecture over the 10 years are shown in Fig. A1.
Fig. 2.
Trends in school lunch program expansion in junior high schools by prefecture. Annual Reports of School Lunch Implementation Survey, 2006–15. The school lunch coverage rates (percentage of students for whom school lunch was provided at prefecture level as of May 1) among public junior high school students in 47 prefectures are displayed for 2006 (A), 2010 (B) and 2015 (C). (D) The change in the school lunch coverage rate from 2006 through 2015.
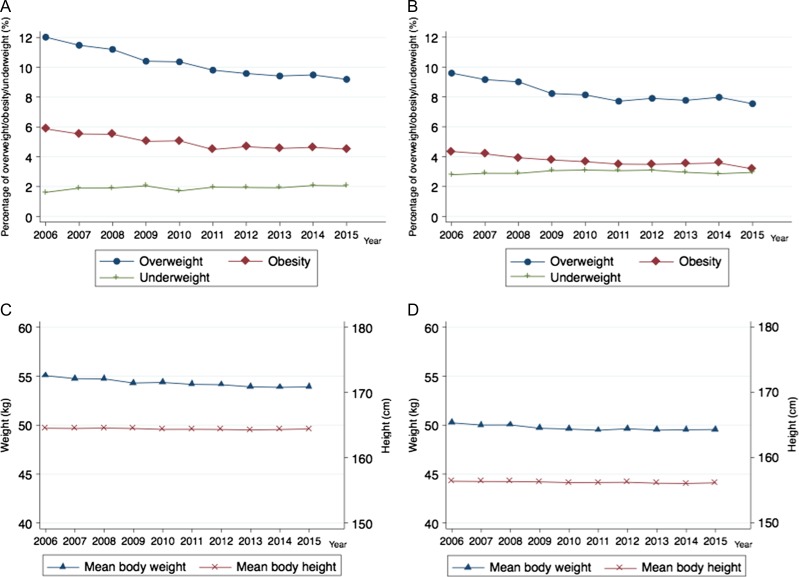
Figure 3 illustrates the 10-year trend for overweight/obesity/underweight percentage and mean body weight/height across Japan among the children aged 13–15 years, which were calculated as weighted means of the prefecture-level values with the Statistics Bureau’s yearly prefecture-level population (children aged 10–14) estimates as weight.31 The percentages of overweight, obesity or underweight children were 10–12%, around 5% or around 2% among boys, and 8–10%, around 4% or around 3% among girls, respectively. The percentage of overweight or obesity children and the mean body weight tended to decrease over time.
Fig. 3.
The 10-year trends for overweight/obesity/underweight percentage and mean body weight/height across Japan. Annual Reports of School Health Statistics Survey, 2006–15. Percentage of overweight/obesity/underweight is the percentage of children whose measured body weight is 20% heavier, 30% heavier, or 20% lighter than the standard weight. (A and C) are for boys and (B and D) are for girls. (A and B) are for the percentage of overweight/obesity/underweight, and (C and D) are for body weight/height.
Main results
Table I shows the main results of this study. The first and second columns show that a 10 percentage point increase in the school lunch coverage rate is associated with a 0.37 percentage point decrease in the overweight percentage (95% confidence interval [CI]: 0.18–0.56) and a 0.23 percentage point decrease in the obesity percentage (95% CI: 0.10–0.37), with statistical significance among boys. Among girls, the point estimates of the effect of the school lunch coverage rate on the overweight percentage and obesity percentage were negative, but these effects were not statistically significant. Underweight percentage and mean body weight and height were not significantly affected by changes in the school lunch coverage rate for either girls or boys.
Table 1.
Impact of the school lunch coverage rate on overweight/obesity/underweight percentage and mean body weight/height among junior high school students
| Outcome | |||||
|---|---|---|---|---|---|
| Overweight percentage (%) | Obesity percentage (%) | Underweight percentage (%) | Mean body weight (kg) | Mean body height (cm) | |
| Girls | |||||
| Coefficient | −0.014 | −0.007 | 0.002 | −0.004 | 0.002 |
| 95% CI | −0.032, 0.005 | −0.018, 0.003 | −0.007, 0.004 | −0.009, 0.001 | −0.002, 0.005 |
| R-squared | 0.592 | 0.531 | 0.320 | 0.958 | 0.942 |
| Observations | 1251 | 1251 | 1251 | 1251 | 1251 |
| Boys | |||||
| Coefficient | −0.037*** | −0.023** | −0.003 | −0.005 | 0.004 |
| 95% CI | −0.056, −0.018 | −0.037, −0.010 | −0.010, 0.004 | −0.011, 0.001 | 0.000, 0.009 |
| R-squared | 0.701 | 0.600 | 0.444 | 0.985 | 0.991 |
| Observations | 1251 | 1251 | 1251 | 1251 | 1251 |
Notes: **P < 0.01, ***P < 0.001. 95% CI indicates 95% confidence intervals using clustered standard errors. Ordinary least square estimations were applied with adjustment for the lagged dependent variable and dummy variables for prefecture, age and year. For overweight/obesity/underweight percentage, the coefficient indicates the impact of a one percentage point change in the school lunch coverage rate on each outcome. For mean body weight/height, the coefficient × 100 indicates the impact of a one percentage point change in the school lunch coverage rate on each outcome. The unit of observation was determined by prefecture, sex, year and birth year.
Sensitivity analyses
Table A1 shows the results of the ‘falsification test’. No statistically significant effects of school lunch coverage rate in junior high school on outcomes among children aged 7–12 were observed. Table A2 shows the results of the analyses using the limited samples. The point estimates and statistical significance were largely unchanged.
Discussion
Main finding of this study
This nationwide study in Japan used the cross-sectional and longitudinal variations in the school lunch coverage rate in junior high schools at prefecture level to reveal significant preventive effects of the school lunch coverage rate on overweight and obesity percentages in prefectures among junior high school boys. The magnitude of the effects found was clinically significant. Among boys, a 10 percentage point increase in the school lunch coverage rate would result, ceteris paribus, in a 0.37 percentage point and a 0.23 percentage point reduction in overweight and obesity percentages the following year, respectively. These results correspond to reductions of 3.7 and 4.6% in the numbers of overweight and obese boys, respectively, if the baseline overweight and obesity percentages among boys are supposed to be 10 and 5% as shown in Fig. 3.
In contrast, among girls, an increased school lunch coverage rate did not lead to a statistically significant reduction in overweight or obesity percentages. This finding may be explained by the fact that thinness is an increasing problem, especially among young Japanese women.32 If girls without access to school lunches tended to consume less than the recommended daily energy levels because of misconceptions regarding self-image and body image, as reported in the literature,32 the effect of school lunch on overweight and obesity would be weakened. We did not find statistically significant effects of the school lunch coverage rate on mean body weight or height, though the point estimates were negative for body weight and positive for body height. A prior study finds that children in Japan are more likely to attain an appropriate level of nutritional intake (e.g. fat, protein, calcium and magnesium) on a day when school lunch is provided than on a day when it is not.13 Excess energy intake from fat could cause body weight increase,33 and protein, calcium and magnesium are important determinants of body height via the growth of long bones.34 Thus, each of higher body height or lower body weight might explain the reduction in the overweight or obesity percentage. Meanwhile, no significant effect on the underweight percentage was observed in this study even though school lunches had originally targeted undernutrition. Our findings suggest that the SLP especially prevented overweight/obesity in Japan, where severe undernutrition that can be treated by receiving the SLP is rarely observed.
What is already known on this topic
In the school setting, existing work has consistently found the combination of nutrition and physical activity interventions,35 with the restriction of access to junk food effective at reducing children’s overweight and obesity.36 Policymakers are also paying attention to school lunches to address children’s overweight and obesity.37,38 Prior studies have revealed that school lunch implemented following nutritional regulations improves nutritional intakes,39,40 though the protective effect of school lunch on overweight and obesity has yet to be established. Some studies focused the National School Lunch Program (NSLP) implemented in the USA,41 but found no protective effects on childhood obesity, even after addressing the selection bias caused by differences in unobserved characteristics between NSLP participants and non-participants.42–44 This might be because NSLP meals often exceeded the statutory limits for total energy intake, grams of fat, and saturated fat, and NSLP participants consumed more total fat and saturated fat than did non-participants, at the point of time their studies were conducted.45,46 In fact, one study revealed that stringent school lunch standards improved weight status among children subsidized by the NSLP.47
What this study adds
The present study revealed the protective effect of the SLP on overweight and obesity among junior high school boys for the first time using 10-year nationally representative data in Japan.
Limitations of this study
Some limitations should be noted. First, we used the prefecture-level school lunch coverage rate as an exposure. Nevertheless, it would reflect the actual intake of school lunch in individuals because the leftover rate of the school lunch was reported to be quite low.19 Second, because this study used aggregated data, we estimated the average association between the school lunch coverage rate and prefecture-level outcomes, even if the estimators indicate the individual-level effects of school lunches under some plausible conditions (as explained in the Appendix). Further research including the analysis of individual data is warranted. Third, the present study was unique in assessing the effects of SLP on overweight/obesity but could not evaluate the effects on nutritional intakes. The mechanism of school lunch on overweight/obesity was not sufficiently clarified from this study. Fourth, our study used 5% sample of all the children aged 13–15. The generalizability to the total child population was limited. Fifth, different countries are implementing SLPs in diverse social and historical contexts. In Japan, the SLP is offered as part of education, including learning healthy dietary habits and gaining nutritional knowledge.10 Hence, this study could not separately evaluate the educational and nutritional effects. Our results suggest at least that the combination of access to nutritious food and dietary education through the SLP is effective in protecting children from overweight and obesity.
Conclusion
This nationwide study in Japan revealed the essential effect of the SLP on the reduction of overweight and obesity percentages among junior high school boys. This finding might partly explain the low prevalence of childhood obesity in Japan. School lunch based on adequately regulated nutrition standards may be a convincing way to decrease childhood overweight and obesity.
Supplementary Material
Acknowledgements
We thank Takuma Komiyama, the principal of Shinagawa Municipal Ebara Dai-ichi Junior High School, for offering the pictures of the school lunch, and Jennifer Barrett, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this article.
References
- 1. The GBD 2015 Obesity Collaborators Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lobstein T, Jackson-Leach R, Moodie ML et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385:2510–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Serdula MK, Ivery D, Coates RJ et al. Do obese children become obese adults? A review of the literature. Prev Med 1993;22:167–77. [DOI] [PubMed] [Google Scholar]
- 4. Whitaker RC, Wright JA, Pepe MS et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337:869–73. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization School Policy Framework: Implementation of the WHO Global Strategy on Diet, Physical Activity and Health Geneva, 2008. http://www.who.int/dietphysicalactivity/SPF-en-2008.pdf (22 May 2018, date last accessed).
- 6. Procter KL, Rudolf MC, Feltbower RG et al. Measuring the school impact on child obesity. Soc Sci Med 2008;67:341–49. [DOI] [PubMed] [Google Scholar]
- 7. Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 2006;1:11–25. [DOI] [PubMed] [Google Scholar]
- 8. Inokuchi M, Matsuo N, Takayama JI et al. Trends in thin body stature among Japanese male adolescents, 2003–2012. Ann Hum Biol 2014;41:277–81. [DOI] [PubMed] [Google Scholar]
- 9. Inokuchi M, Matsuo N, Takayama JI et al. Trends in thin body stature among Japanese female adolescents, 2003–2012. Ann Hum Biol 2014;42:533–37. [DOI] [PubMed] [Google Scholar]
- 10. Borovoy A, Roberto CA. Japanese and American public health approaches to preventing population weight gain: a role for paternalism? Soc Sci Med 2015;143:62–70. [DOI] [PubMed] [Google Scholar]
- 11. Fisher M. How Japan’s revolutionary school lunches helped slow the rise of child obesity. Washington Post 2013. https://www.washingtonpost.com/news/worldviews/wp/2013/01/28/how-japans-revolutionary-school-lunches-helped-slow-the-rise-of-child-obesity/?utm_term=.549523ad99be (22 May 2018, date last accessed).
- 12. Harlan C. On Japan’s school lunch menu: a healthy meal, made from scratch. Washington Post 2013. https://www.washingtonpost.com/world/on-japans-school-lunch-menu-a-healthy-meal-made-from-scratch/2013/01/26/5f31d208-63a2-11e2-85f5-a8a9228e55e7_story.html?utm_term=.3f89d6041354 (22 May 2018, date last accessed).
- 13. Asakura K, Sasaki S. School lunches in Japan: their contribution to healthier nutrient intake among elementary-school and junior high-school children. Public Health Nutr 2017;20:1523–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ministry of Education Culture Sports Science and Technology School Lunch Program Act http://law.e-gov.go.jp/htmldata/S29/S29HO160.html (22 May 2018, date last accessed).
- 15. Ministry of Education Culture Sports Science and Technology Annual Reports of School Lunch Implementation Survey.http://www.mext.go.jp/b_menu/toukei/chousa05/kyuushoku/1267027.htm (22 May 2018, date last accessed).
- 16. Hendy HM, Williams KE, Camise TS. ‘Kids Choice’ School lunch program increases children’s fruit and vegetable acceptance. Appetite 2005;45:250–63. [DOI] [PubMed] [Google Scholar]
- 17. Gould R, Russell J, Barker ME. School lunch menus and 11 to 12 year old children’s food choice in three secondary schools in England—are the nutritional standards being met? Appetite 2006;46:86–92. [DOI] [PubMed] [Google Scholar]
- 18. Japan Sport Council 2010. https://www.jpnsport.go.jp/anzen/Portals/0/anzen/kenko/siryou/chosa/syoku_life_h22/H22syokuseikatsu_4.pdf (22 May 2018, date last accessed).
- 19. Ministry of the Environment Ministry of the Environment 2015. http://www.env.go.jp/press/100941.html (22 May 2018, date last accessed).
- 20. Ministry of Education Culture Sports Science and Technology The Nutrition Standards for School Lunch http://www.mext.go.jp/b_menu/hakusho/nc/1332086.htm (22 May 2018, date last accessed).
- 21. Ministry of Education Culture Sports Science and Technology Annual Report of School Health Statistics Survey http://www.mext.go.jp/b_menu/toukei/chousa05/hoken/1268826.htm (22 May 2018, date last accessed).
- 22.School Health and Safety Act. 2016. http://elaws.e-gov.go.jp/search/elawsSearch/elaws_search/lsg0500/detail?lawId=333AC0000000056&openerCode=1 (22 May 2018, date last accessed).
- 23. Dobashi K. Evaluation of obesity in school-age children. J Atheroscler Thromb 2000;23:32–8. [DOI] [PubMed] [Google Scholar]
- 24. Centers for Disease Control and Prevention Defining Childhood Obesity https://www.cdc.gov/obesity/childhood/defining.html (22 May 2018, date last accessed).
- 25. Asayama K, Hayashibe H, Dobashi K et al. Decrease in serum adiponectin level due to obesity and visceral fat accumulation in children. Obes Res 2003;11:1072–79. [DOI] [PubMed] [Google Scholar]
- 26. Oyama C, Takahashi T, Oyamada M et al. Serum uric acid as an obesity-related indicator in early adolescence. Tohoku J Exp Med 2006;209:257–62. [DOI] [PubMed] [Google Scholar]
- 27. Nishimura R, Sano H, Matsudaira T et al. Childhood obesity and its relation to serum adiponectin and leptin: a report from a population-based study. Diabetes Res Clin Pract 2007;76:245–50. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization Moderate Malnutrition http://www.who.int/nutrition/topics/moderate_malnutrition/en/ (22 May 2018, date last accessed).
- 29. Ministry of Education Culture Sports Science and Technology School Basic Survey http://www.mext.go.jp/b_menu/toukei/chousa01/kihon/1267995.htm (22 May 2018, date last accessed).
- 30. StataCorp Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015. [Google Scholar]
- 31. Statistics Bureau Ministry of Internal Affairs and Communications Population Estimates http://www.stat.go.jp/data/jinsui/2.htm (22 May 2018, date last accessed).
- 32. Takimoto H, Yoshiike N, Kaneda F et al. Thinness among young Japanese women. Am J Public Health 2004;94:1592–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Astrup A, Grunwald GK, Melanson EL et al. The role of low-fat diets in body weight control: a meta-analysis of ad libitum dietary intervention studies. Br J Nutr 2000;83:S25–32. [DOI] [PubMed] [Google Scholar]
- 34. Silventoinen K. Determinants of variation in adlult body weight. J Biosoc Sci 2003;35:263–85. [DOI] [PubMed] [Google Scholar]
- 35. Lavelle HV, MacKay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf) 2012;34:360–69. [DOI] [PubMed] [Google Scholar]
- 36. Anderson PM, Butcher KF. Reading, writing, and refreshments: are school finances contributing to children’s obesity? J Hum Resour 2006;41:467–94. [Google Scholar]
- 37. Adamson A, Spence S, Reed L et al. School food standards in the UK: implementation and evaluation. Public Health Nutr 2013;16:968–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Baidal JAW, Taveras EM. Protecting progress against childhood obesity—The National School Lunch Program. N Engl J Med 2014;371:1862–65. [DOI] [PubMed] [Google Scholar]
- 39. Gleason PM, Suitor CW. Eating at school: how the National School Lunch Program affects children’s diets. Am J Agric Econ 2003;85:1047–61. [Google Scholar]
- 40. Jaime PC, Lock K. Do school based food and nutrition policies improve diet and reduce obesity? Prev Med 2009;48:45–53. [DOI] [PubMed] [Google Scholar]
- 41. United States Department of Agriculture National School Lunch Program (NSLP) 2017. https://www.fns.usda.gov/nslp/national-school-lunch-program-nslp (22 May 2018, date last accessed).
- 42. Gundersen C, Kreider B, Pepper J. The impact of the National School Lunch Program on child health: a nonparametric bounds analysis. J Econom 2012;166:79–91. [Google Scholar]
- 43. Millimet DL, Tchernis R, Husain M. School nutrition programs and the incidence of childhood obesity. J Hum Resour 2010;45:640–54. [Google Scholar]
- 44. Schanzenbach DW. Do school lunches contribute to childhood obesity? J Hum Resour 2009;44:684–709. [Google Scholar]
- 45. Crepinsek MK, Gordon AR, McKinney PM et al. Meals offered and served in US public schools: do they meet nutrient standards? J Am Diet Assoc 2009;109:S31–43. [DOI] [PubMed] [Google Scholar]
- 46. Finkelstein DM, Hill EL, Whitaker RC. School food environments and policies in US public schools. Pediatrics 2008;122:e251–59. [DOI] [PubMed] [Google Scholar]
- 47. Taber DR, Chriqui JF, Powell L et al. Association between state laws governing school meal nutrition content and student weight status. JAMA Pediatr 2013;167:513. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.