Abstract
Background
The US homeless population is aging. Older adults and those living in poverty are at a high risk of food insecurity.
Methods
We conducted a cross-sectional analysis of baseline data from a population-based study of 350 homeless adults aged ≥50. We assessed food security and receipt of food assistance. We used multivariable logistic regression to examine factors associated with very low food security.
Results
The majority of the cohort was male and African American. Over half (55.4%) met criteria for food insecurity, 24.3% reported very low food security. Half (51.7%) reported receiving monetary food assistance. In the multivariable model, those who were primarily sheltered in the prior 6 months, (multi-institution users [AOR = 0.44, 95% CI: 0.22–0.86]) had less than half the odds of very low food security compared with those who were unsheltered. Depressive symptoms (AOR = 3.01, 1.69–5.38), oral pain (AOR = 2.15, 1.24–3.74) and cognitive impairment (AOR = 2.21, 1.12–4.35) were associated with increased odds of very low food security.
Conclusions
Older homeless adults experience a high prevalence of food insecurity. To alleviate food insecurity in this population, targeted interventions must address specific risk groups.
Keywords: adults, ageing, housing
Introduction
Approximately half of single homeless adults in the USA are aged 50 and older, and the median age continues to rise.1 Older homeless adults have health problems resembling those of community-dwelling adults in their 70 and 80s, including a high prevalence of chronic disease and functional and cognitive impairments.1 Older adults’ functional and cognitive impairments may constrain ability to obtain adequate food, worsening food insecurity.2 Prior work on food insecurity among the general population has identified older adults as a sub-population vulnerable to food insecurity and health consequences of poor nutrition.2
Individuals living in poverty are at high risk of food insecurity yet there is little known about the experiences of food insecurity among older homeless adults living in extreme poverty.3,4 Food insecurity, defined as having limited access to adequate food due to lack of resources, affects ~49 million Americans.5 Individuals who are food insecure have poorer health and are more likely to consume foods deficient in nutrients.6 Insufficient nourishment complicates chronic disease management, presenting a major challenge for older adults, who have a higher prevalence of chronic disease.1,6
Food insecurity interventions in the USA include the Federal Supplemental Nutrition Assistance Program (SNAP) and local efforts to provide free and low-cost food assistance (i.e. food pantries and free and low-cost meal programs).3 SNAP eligibility is determined by gross and net limits on household income, assets and receipt of public assistance.7 Eligible homeless individuals have lower SNAP enrollment rates compared to other eligible populations, partly because of additional barriers to providing eligibility documentation and difficulty navigating processes for applying for benefits.3 They may face barriers receiving food assistance, including limited transportation and lack of kitchens in which to prepare and store food.6
Homelessness, as defined by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act, includes both those lacking a fixed residence or residing in places not typically used for sleeping and those at imminent risk of losing housing within 14 days.8 Approximately 40% of homeless adults in the USA experiencing homelessness are unsheltered.9 In a population-based sample of homeless adults aged 50 and older, we examine the prevalence of food insecurity (defined as low and very low food security). Using a multivariable model, we examine factors associated with very low food security (the most severe form of food insecurity that affects both dietary quality and quantity). We explore whether residential history, health status, depressive symptoms, cognitive and functional impairment, health-related behaviors and social support are associated with very low food security.
Methods
Setting and participants
The HOPE HOME (Health Outcomes of People Experiencing Homelessness in Older Middle Age) Study is a longitudinal study of 350 homeless adults aged 50 years and older. We analyzed baseline data collected from July 2013 to June 2014. We constructed our sampling frame to approximate the source population and randomly selected potential participants at each recruitment site: homeless encampments, recycling centers, overnight homeless shelters (n = 5), and free and low-cost meal programs (n = 5) serving at least three meals a week in Oakland, CA.1,10,11
Recruitment and data collection
Participants were eligible if they were English-speaking, aged 50 years and older, homeless as defined by the HEARTH Act,8 and able to provide informed consent, as determined by a teach-back method.12 We excluded individuals unable to provide consent or communicate due to hearing impairments. After determining eligibility, study staff conducted structured interviews and performed clinical assessments at a non-profit community-based center in Oakland that serves low-income older adults. Study participants did not have to receive services there to participate. Participants received $25 gift cards to a major retailer.
Measures
Dependent variable: food insecurity
We assessed food security using the Six-Item Short Form of the US Household Food Security Survey Module (FSSM), a validated measure of food security in the general population and among older adults.13 The US Department of Agriculture defines food security as high or marginal (raw score 0–1), low (2–4) and very low food security (5–6). Those with low food security or very low food security are considered to be food insecure. Individuals with low food security (former label: food insecurity without hunger) meet their food budget by choosing low quality foods but experience little or no reduced food intake. Individuals with very low food security (former label: food insecurity with hunger) have both reduced food quality and quantity.14 We analyzed very low food security (the most severe form of food insecurity) as a dichotomous dependent variable in our multivariable model.
Descriptive variables: food assistance
Participants reported if they had received any SNAP benefits in the prior 6 months and, if so, their monthly benefits amount and whether they had received any in the prior 30 days (any versus none).
We asked participants about their participation status in the federal social security programs Supplemental Security Income (SSI), an assistance program for those who are low-income and either aged ≥65, blind or disabled, and Social Security Disability Income (SSDI), an entitlement program for those with a disability and who have paid into the social security system for 10 years. Participants reported the total benefits they received in the prior month. In California, SSI beneficiaries also receive a State Supplementary Payment (SSP) that includes a benefit equivalent to the value of SNAP; they are ineligible for SNAP. We considered individuals who reported receiving SSI/SSDI benefits below the state maximum SSI/SSP benefit ($900 per month) as likely SSI/SSP recipients. We considered receipt of either SNAP or SSP as receipt of monetary food assistance. To assess potential SNAP eligibility, we classified individuals reporting over $15 000 in annual income from all sources as ineligible, based on eligibility criteria for single adults.
Participants reported if they had received any non-monetary food assistance (free or low-cost meal program, food pantry or other) in the last 6 months and, if so, where and whether they had received any in the last 30 days. We asked them to report the number of days they had used non-monetary food assistance (0–14, 15–21, over 21) in the past month. Participants reported where they obtained food most frequently (self-purchase, free or low-cost meal programs, a shelter, a food pantry, from family, friends or other individuals and other) and how safe they felt doing so (unsafe to completely safe). We asked participants to report how difficult it was to find food daily (not at all to extremely difficult).
Independent variables
Sociodemographic variables
We measured race/ethnicity (African American, White, Latino, multiracial/other), sex, age, highest level of education (less than high school, high school/General Educational Development (GED) test equivalency, or more than high school), and employment status (≥20 versus <20 h a week). Participants reported if they had any history of military service or of imprisonment in state or federal prison.
Residential history
Using a follow-back residential calendar method,15 we asked participants to report where they had stayed over the previous 6 months and the number of nights spent at each location (e.g. apartment, shelter, hospital, jail, unsheltered environment). Using these residential histories, we performed cluster analysis to develop a classification of residential categories based on participants’ primary living environments in the prior 6 months.11 Participants reported the duration of their current episode of homelessness (>1 versus ≤1 year), which was collinear with the residential categories. In our multivariable model, we included only residential categories, as this is more actionable. We present bivariate associations between very low food security and duration of homelessness for description only.
Health status
We assessed self-rated general health (fair or poor versus good, very good or excellent).16 Using questions from the National Health and Nutrition Examination Survey (NHANES), we asked participants if a health care provider had ever diagnosed them with hypertension, coronary artery disease or myocardial infarction, congestive heart failure, high cholesterol or diabetes.17 We assessed oral pain by asking participants if they had oral pain in the previous 6 months that kept them from eating or sleeping.
Mental health, cognitive and functional status
We assessed: (i) depressive symptoms using the Center for Epidemiologic Studies Depression Scale18 (score ≥16 = depressive symptomatology); (ii) cognitive impairment using the Modified Mini-Mental State Examination (score below the seventh percentile after adjustment for age and education);19,20 (iii) functional status using participant-reported difficulty performing five activities of daily living (ADLs) and six instrumental activities of daily living (IADLs);21,22 and (iv) IADLs with the Brief Instrumental Functioning Scale, a validated instrument developed for use in homeless persons.22 We defined ADL impairment as difficulty performing ≥1 ADLs; we defined IADL impairment similarly.
Health-related behaviors
We assessed: (i) history of cigarette smoking using questions from the California Tobacco Survey (never, former and current smoker),23 dichotomizing current smokers to every day smokers or some days smokers; (ii) alcohol use problems in the past 6 months using the Alcohol Use Disorders Identification Test adapted for a 6-month period, moderate to high symptoms of alcohol use problems (≥8);24 (iii) illicit substance use problems (opioids, methamphetamine and cocaine) in the past 6 months using the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test adapted for a 6-month period, moderate to high risk of substance use problems (≥4).25
Instrumental support
Participants reported if they were currently married or partnered. We administered Gielen’s questionnaire to assess instrumental support, and participants reported if they had someone to lend or give them money.26 Participants who reported not having anyone to lend money were categorized as having low instrumental support.
Analysis
We used descriptive statistics to describe participant characteristics, levels of food insecurity, and strategies for food acquisition. To categorize participants into distinct groups based on their primary living environments, we used the Ward’s linkage cluster method to minimize the sum-of-square differences within groups.11 We performed chi-square tests to examine differences between high-marginal, low and very low food security categories by demographic and independent variables.
Next, we used logistic regression to model bivariate associations between independent variables, selected a priori, and very low food security. These included age, race/ethnicity, employment, residential history, health status, depressive symptoms, cognitive and functional impairment, health-related behaviors and social support. We included independent variables with bivariate P-values of ≤0.20 in a multivariable model. We then reduced the model using backward elimination, retaining variables with P ≤ 0.05 in the final model. We performed data analysis using Stata version 11.0 (StataCorp LP, College Station, TX) and SAS version 9.4 (SAS Institute, Cary, NC).
Results
Participant characteristics
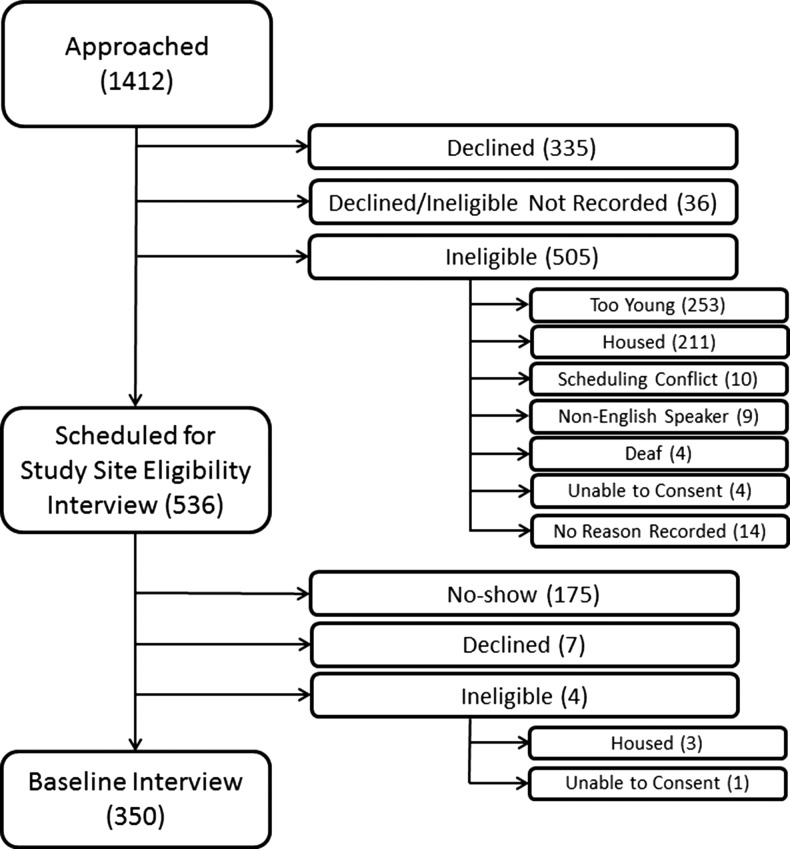
We recruited 350 participants (Fig. 1). Most were men and African American with a median age of 58 (interquartile range, 54–61). (Table 1).
Fig. 1.
Summary of sample.
Table 1.
Baseline characteristics of homeless adults aged 50 and older in Oakland, CA (N = 350), by level of food insecuritya
| Total (N = 350) | High-marginal food security (N = 156) | Low food security (N = 109) | Very low food security (N = 85) | P-value | |
|---|---|---|---|---|---|
| Race, no. (%) | |||||
| Black | 279 (79.7) | 127 (81.4) | 90 (82.6) | 62 (72.9) | 0.42 |
| White | 38 (10.9) | 16 (10.3) | 11 (10.1) | 11 (12.9) | |
| Hispanic/Latino | 16 (4.6) | 7 (4.5) | 5 (4.6) | 4 (4.7) | |
| Mixed/other | 17 (4.9) | 6 (3.8) | 3 (2.8) | 8 (9.4) | |
| Male, no. (%) | 270 (77.1) | 113 (72.4) | 88 (80.7) | 69 (81.2) | 0.17 |
| Age, median years (IQR)b | 58 (54.0, 61.0) | 58.0 (54.0, 61.0) | 59.0 (55.0, 63.0) | 56 (53.0, 59.0) | 0.01 |
| Annual income >$15 000 | 26 (7.4) | 11 (7.1) | 12 (11.0) | 3 (3.5) | 0.14 |
| Less than high school education, no. (%) | 90 (25.7) | 37 (23.7) | 32 (29.4) | 21 (24.7) | 0.57 |
| Employment | |||||
| Worked 0 h/week, no. (%) | 306 (87.7) | 137 (87.8) | 98 (90.7) | 71 (83.5) | 0.03 |
| Worked 1–19 h/week, no. (%) | 26 (7.4) | 13 (8.3) | 2 (1.9) | 11 (12.9) | |
| Worked 20+ h/week, no. (%) | 17 (4.9) | 6 (3.8) | 8 (7.4) | 3 (3.5) | |
| History of military service, no. (%) | 76 (21.7) | 28 (17.9) | 28 (25.7) | 20 (23.5) | 0.29 |
| Ever in prison, no. (%) | 119 (34.3) | 59 (38.6) | 33 (30.3) | 27 (31.8) | 0.32 |
| Housing status, no. (%) | |||||
| Staying temporarily with family or friends | 57 (16.3) | 31 (19.9) | 15 (13.8) | 11 (12.9) | 0.08 |
| Users of multiple institutionsc | 88 (25.1) | 44 (28.2) | 28 (25.7) | 16 (18.8) | |
| Renters/recently homeless | 43 (12.3) | 19 (12.2) | 17 (15.6) | 7 (8.2) | |
| Unsheltered | 162 (46.3) | 62 (39.7) | 49 (45.0) | 51 (60.0) | |
| Current episode of homelessness ≥1 year, no. (%)d | 172 (49.6) | 72 (46.8) | 48 (44.0) | 52 (61.9) | 0.03 |
| Health status, no. (%) | |||||
| Fair/poor self-reported health | 195 (55.7) | 80 (51.3) | 58 (53.2) | 57 (67.1) | 0.05 |
| Any chronic health condition, no. (%)e | 228 (65.1) | 107 (68.6) | 68 (62.4) | 53 (62.4) | 0.48 |
| Hypertension | 195 (55.7) | 91 (58.3) | 58 (53.2) | 46 (54.1) | 0.67 |
| Coronary artery disease/myocardial infarction | 32 (9.1) | 15 (9.6) | 24 (9.1) | 8 (9.4) | 0.93 |
| Congestive heart disease | 25 (7.1) | 8 (5.1) | 9 (8.3) | 8 (9.4) | 0.40 |
| High cholesterol | 101 (28.9) | 43 (27.6) | 32 (29.4) | 26 (30.6) | 0.88 |
| Diabetes | 49 (14.0) | 20 (12.8) | 16 (14.7) | 13 (15.3) | 0.84 |
| Oral painf | 112 (32.0) | 43 (27.6) | 29 (26.6) | 40 (47.1) | 0.03 |
| Mental health | |||||
| Any depressive symptoms, no. (%)g | 185 (53.3) | 55 (35.7) | 68 (62.4) | 62 (73.8) | <0.001 |
| Cognitive impairment, no. (%)h | 90 (25.8) | 47 (30.1) | 28 (25.9) | 15 (17.6) | 0.11 |
| ADL impairment, no. (%)i | 136 (38.9) | 57 (36.5) | 39 (35.8) | 40 (47.1) | 0.20 |
| IADL impairment, no. (%)j | 173 (49.4) | 72 (46.2) | 56 (51.4) | 45 (52.9) | 0.53 |
| Health behaviors | |||||
| Smoking status | |||||
| Non-smoker | 121 (34.6) | 56 (35.9) | 37 (33.9) | 28 (32.9) | 0.02 |
| Smoke every day | 157 (44.9) | 77 (49.4) | 51 (46.8) | 29 (34.1) | |
| Smoke some days | 72 (20.6) | 23 (14.7) | 21 (19.3) | 28 (32.9) | |
| Alcohol use problem, no. (%)k | 90 (25.8) | 38 (24.5) | 22 (20.2) | 30 (35.3) | 0.05 |
| Illicit drug use problem, no. (%)l | 177 (50.6) | 72 (46.2) | 59 (54.1) | 46 (54.1) | 0.33 |
| Social support, no. (%) | |||||
| Currently married/partnered, no. (%) | 30 (8.6) | 15 (9.6) | 9 (8.3) | 6 (7.1) | 0.79 |
| Did not have someone to lend money, no. (%) | 144 (42.0) | 55 (35.7) | 46 (42.6) | 43 (53.1) | 0.04 |
We used the chi-square test of proportions for all comparisons except as noted.
aFor analytic purposes, we aggregated low food security with high-marginal food security (0–4) and dichotomized between these individuals and those with very low food security (Table 3).
bWe utilized the Wilcoxon non-parametric test for age to estimate group differences in food security.
cMultiple institution users spent the majority of days in shelters, jail, transitional housing and other institutions.
dLength of current episode of homelessness calculated from date participant reported most recently becoming homeless.
eChronic conditions included hypertension, coronary artery disease or myocardial infarction, congestive heart failure, high cholesterol or diabetes.
fOral pain defined as oral pain that prevented eating or sleeping.
gDepressive symptomatology defined as Center for Epidemiological Studies Depression (CES-D) score ≥ 16.
hCognitive impairment defined as a Modified Mini-Mental State Examination score below the seventh percentile (i.e. 1.5 standard deviations below the demographically adjusted cohort mean).
iADL (Activity of Daily Living) impairment defined as self-reported difficulty performing one or more ADLs.
jIADL (Instrumental Activity of Daily Living) impairment defined as self-reported difficulty performing one or more IADLs.
kAlcohol use problem, past 6 months defined as an Alcohol Use Disorders Identification Test score ≥8 (range 0–20; higher scores indicate more problems).
lIllicit drug use problem (excluding marijuana), past 6 months defined as a World Health Organization Alcohol, Smoking and Substance Involvement Screening Test score for either cocaine, methamphetamines or opioids of ≥4 (range 0–39; higher scores indicate more problems).
Using cluster analysis, we classified almost half of the cohort as spending the majority of the prior 6 months unsheltered, over a quarter as spending most of their time in various institutional settings (shelters, hospitals), less than one-fifth as staying temporarily with family or friends, and ~10% as recently homeless or having spent most of the prior 6 months living in housing that they rented.11
Half of the sample reported a current episode of homelessness lasting for over one year. Two-thirds reported any chronic condition, and a third reported oral pain that prevented them from eating or sleeping. Half the sample reported depressive symptoms. Over one-third reported any ADL impairment, and almost half reported any IADL impairment. Two-thirds smoked tobacco and a quarter had high risk of an alcohol use problem. Just over half reported having someone to lend money.
Food insecurity and food assistance
The majority of participants met criteria for food insecurity, with a third reporting low food security and an additional quarter reporting very low food security (Table 1). Half received monetary food assistance; almost a third and an additional fifth reported current receipt of SNAP and SSP, respectively (Table 2). Less than a 10th were ineligible for SNAP based on income. Of those who reported receiving SNAP, nearly all reported using SNAP benefits at least once in the last 30 days. Participants reported free or low-cost meal programs as the most common type of food assistance, followed by food pantries (Table 2). Participants reported that the most common sources of food were free and low-cost food programs, self-purchased food, and shelters that provided food. Over half of those with food insecurity (n = 103; 53.7%) received monetary food assistance. Most of those with food insecurity (n = 167; 86.1%) received non-monetary food assistance in the past 30 days. Less than 5% of food insecure individuals did not receive assistance (n = 9; 4.7%). The prevalence of receiving assistance did not differ significantly between those with low and very low food security.
Table 2.
Food assistance, acquisition and strategies among the HOPE HOME sample
| Total (N = 350) n (%) | |
|---|---|
| Annual income > $15 000 | 26 (7.4) |
| Receive monetary food assistancea | 178 (51.7) |
| Receive SSP benefits in last 30 days | 76 (21.7) |
| Receive SNAP benefits in last 30 days | 102 (29.1) |
| Amount received in SNAP, median (quartiles) | 189.0 (185.0, 200.0) |
| Received non-monetary food assistance in last 6 monthsc | 309 (88.3) |
| Received non-monetary food assistance in last 30 days | 286 (81.7) |
| Days used non-monetary food assistance in last 30 days | |
| <2 weeks | 100 (28.6) |
| 2–3 weeks | 78 (22.3) |
| >3 weeks | 108 (30.9) |
| Non-monetary food assistancec | |
| Free and low-cost meal program | 272 (77.7) |
| Food pantry | 76 (21.7) |
| Otherd | 2 (0.6) |
| Most common sources of food | |
| Self-purchased | 168 (54.5) |
| Free or low-cost food program | 95 (30.8) |
| Food pantry | 74 (21.1) |
| Shelter | 42 (13.6) |
| Family or friend’s house | 19 (6.2) |
| Receive food from other individualse | 18 (5.8) |
| Forage from bins | 2 (0.6) |
| Other | 17 (4.9) |
| Felt completely safe where eat most often | 240 (78.4) |
| Moderate to severe difficulty finding food | 69 (22.6) |
aWe defined monetary food assistance as receipt of SNAP or receipt of SSI/SSDI benefits <$900 monthly.
bMonetary and non-monetary food assistance and food sources were similar for both individuals with low to high food security and those with very low food security.
cOther sources of non-monetary food assistance include food from restaurants.
dFood from other individuals includes leftovers from markets or restaurants and food from strangers.
Multivariable findings: factors associated with very low food security
In our multivariable model, being unsheltered was associated with very low food security. Compared to the unsheltered group, individuals who stayed temporarily with family and friends, used multiple institutions, or were recently homeless had less than half the odds of very low food security oral pain, cognitive impairment and depressive symptoms were associated with very low food security (Table 3). Being a sometime smoker compared to being a non-smoker was marginally associated (Table 3).
Table 3.
Factors associated with very low food security among the HOPE HOME sample
| Unadjusted odds ratio (OR) for very low food securitya (95% CI) | Adjusted odds ratio (AOR) for very low food security (95% CI) | |
|---|---|---|
| Age | 0.93 (0.88–0.98) | – |
| Black (ref: Non-Black) | 0.60 (0.34–1.06) | |
| Employment (ref: 0 h/week) | ||
| Worked <20 h/week | 2.43 (1.06–5.57) | – |
| Worked 20+ h/week | 0.71 (0.20–2.57) | – |
| Current episode of homelessness ≥1 year | 1.77 (1.00–3.12) | – |
| Housing status (ref: unsheltered)b | ||
| Staying temporarily with family or friends | 0.52 (0.25–1.09)c | 0.41 (0.19–0.90) |
| Users of multiple institutionsd | 0.48 (0.26–0.91) | 0.44 (0.22–0.86) |
| Renters/recently homeless | 0.42 (0.18–1.02) | 0.31 (0.12–0.80) |
| Health status | ||
| Fair/poor self-reported health | 1.87 (1.12–3.14) | – |
| Any chronic health conditione | 0.85 (0.51–1.42) | – |
| Oral painf | 2.38 (1.43–3.97) | 2.15 (1.24–3.74) |
| Mental health | ||
| Any depressive symptoms (ref: none)g | 3.21 (1.85–5.56) | 3.01 (1.69–5.38) |
| Cognitive impairmenth | 1.85 (0.99–3.46) | 2.21 (1.12–4.35) |
| Functional status (ref: none) | ||
| ADL impairmenti | 1.56 (0.95–2.58) | – |
| IADL impairmentj | 1.20 (0.73–1.97) | – |
| Health behaviors | ||
| Smoking status (ref: non-smoker) | ||
| Smoke every day | 0.75 (0.42–1.36) | 0.67 (0.36–1.25) |
| Smoke some days | 2.11 (1.11–4.01) | 2.01 (1.00–4.04)k |
| Alcohol use probleml | 1.85 (1.09–3.17) | – |
| Social support | ||
| Did not have someone to lend money | 1.80 (1.09–3.00) | – |
aFor analytic purposes, we defined food insecurity as a dichotomous variable, either very low (5–6) versus high to low food security (0–4).
bType 3 P-value for housing group = 0.010.
cWe included independent variables with bivariate P-values of ≤0.20 in a multivariable model and used backwards elimination to reduce the model, retaining variables with P ≤ 0.05 (bolded) in the final model.
dMultiple institution users spent the majority of days in shelters, jail, transitional housing and other institutions.
eChronic conditions included hypertension, coronary artery disease or myocardial infarction, congestive heart failure, high cholesterol or diabetes.
fOral pain defined as oral pain that prevented eating or sleeping.
gDepressive symptomatology defined as Center for Epidemiological Studies Depression (CES-D) score ≥16.
hCognitive impairment defined as a Modified Mini-Mental State Examination score below the seventh percentile (i.e. 1.5 standard deviations below the demographically adjusted cohort mean).
iADL (activity of daily living) impairment defined as self-reported difficulty performing one or more ADLs.
jIADL (instrumental activity of daily living) impairment defined as self-reported difficulty performing one or more IADLs.
kType 3 P-value for smoking = 0.007.
lAlcohol use problem, past 6 months defined as an Alcohol Use Disorders Identification Test score ≥8 (range 0–20; higher scores indicate more problems).
Discussion
Main finding of this study
In a population-based sample of older homeless adults, over half reported food insecurity: one-third reported low food security and one quarter reported very low food security. This is similar to food insecurity estimates among other homeless populations27–30 and two times higher than national estimates in the US poverty population (below 185% of the poverty threshold).31 In the general population, older adults are less likely to experience food insecurity than younger adults.31 Among adults 50 and over in the general population, fewer than 10% experience food insecurity; in California, fewer than 20% of those over 50 do so.32
These data suggest an emerging crisis in a growing population of older homeless adults. Despite the vast majority meeting income requirements, only half of participants reported receipt of monetary food assistance, the primary strategy to address food insecurity in the USA, presenting a potential target for intervention. While low SNAP participation could reflect individuals not meeting non-income related SNAP eligibility criteria (e.g. having prior drug-related felony charges), homeless individuals face additional barriers to SNAP enrollment: difficulty receiving eligibility and renewal paperwork via mail, or low health literacy and cognitive impairment that may complicate ability to understand eligibility criteria and complete necessary documentation. Homelessness itself is not a disqualification for SNAP, those experiencing homelessness may deduct costs for shelter from their income to further eligibility.33
Older homeless individuals with SNAP may face additional barriers to food security. SNAP does not allow recipients to purchase prepared food. Due to limited access to cooking and storage facilities for non-prepared foods, homeless individuals face barriers to making optimal use of SNAP or non-monetary food aide, such as food pantries, that distribute foods requiring preparation.34,35 Home-delivered meals, a common source of food assistance for older adults, require a physical address and food storage.36
We found that certain characteristics increased odds of very low food security: being unsheltered placed individuals at twice the odds. Approximately half of our study participants, and over 40% of single homeless adults in the USA are unsheltered, a population with less access to services. Unsheltered individuals may experience heightened social isolation, and difficulty accessing food, housing and social services.35,37
Other factors associated with increased odds included having oral pain, depressive symptoms or cognitive impairment, suggesting the need to target interventions. Oral pain, common due to poor access to dental care, may restrict food choices and impair the ability to take advantage of non-monetary food aide.38 The association with depressive symptoms may be bidirectional. Depression may increase food insecurity via lower self-efficacy to seek out services or community programs, and food insecurity may cause depression via nutritional deficiencies and chronic stress related to searching for food.3,28,39 Individuals with cognitive impairment may be unable to navigate processes to apply for SNAP and access available food assistance sources.6
We found an association between non-daily smoking and very low food security. Individuals who experience hunger may smoke to decrease sensations of hunger.40 Smokers with very low food security may be unable to afford cigarettes and therefore engage in non-daily, instead of daily, smoking.
What is already known on this topic
Prior studies in homeless non-elderly populations found similar prevalence of food insecurity, with estimates between 40 and 64%.27–30 None, however, focused on older adults, who due a higher prevalence of chronic diseases, may face additional risks from food insecurity. There has been increased attention on food insecurity in the general poverty and older populations, but neither face risks as high as the older homeless population.
What this study adds
This study’s focus on older homeless adults is unique. Despite a growing population of older homeless adults, little is known about food insecurity in this population. This study increases understanding of who is at highest risk among older homeless adults, and such, will allow for targeted interventions.
Limitations of this study
Our study has several limitations. Our sampling frame included free and low-cost meal programs, which may have led to an overestimate of the proportion of older homeless adults who received non-monetary food aid. We did not have records to confirm SNAP receipt or distinguish between SSI and SSDI benefits in our questionnaire; using self-reported income to classify individuals receiving SSI/SSP may have led to slight misclassification of those with monetary food benefits. We did not have data on drug felony convictions to determine ineligibility for SNAP, thus, limiting our ability to understand one potential reason for low enrollment.41 Because the study was conducted in one city, our findings may not be generalizable to other areas.
Conclusion
Over half of older homeless adults are facing food insecurity at approximately five times the prevalence of older adults in the general population. One-third of older homeless adults experience the most severe form of food insecurity. Due to their poor health and multiple chronic conditions, food insecurity presents a direct threat to their health and safety. There is need to address the high prevalence of food insecurity in older homeless adults; efforts should focus on those at highest risk, including the growing population of unsheltered older adults, those with cognitive impairment and poor oral health.
Acknowledgements
Contributors: We gratefully acknowledge our colleagues Pamela Olsen, Nina Fiellin, Tauni Marin and Kenneth Perez for their invaluable contributions to the HOPE HOME study. We would like to acknowledge our colleague Angela Allen, who passed away in May of 2015, for her incredible contributions to the study. The authors also thank the staff at St. Mary’s Center and the HOPE HOME Community Advisory Board for their guidance and partnership. We acknowledge Lauren M. Kaplan, PhD for her editorial contributions to this article.
Conflicts of Interest
None.
Funding
This study was supported by grants from the National Institute on Aging [K24AG046372, R01AG041860]. These funding sources had no role in the preparation, review or approval of this article.
References
- 1. Brown RT, Hemati K, Riley ED et al. Geriatric conditions in a population-based sample of older homeless adults. Gerontologist 2017;57:757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lee J, Frongillo E Jr.. Factors associated with food insecurity among U.S. elderly persons: importance of functional impairments. J Gerontol B Psychol Sci Soc Sci 2001;56B(2):S94–9. [DOI] [PubMed] [Google Scholar]
- 3. Lee BA, Greif MJ. Homelessness and hunger. J Health Soc Behav 2008;49(1):3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Power M, Uphoff EP, Stewart-Knox B et al. Food insecurity and socio-demographic characteristics in two UK ethnic groups: an analysis of women in the Born in Bradford cohort. J Public Health 2018;40(1):32–40. [DOI] [PubMed] [Google Scholar]
- 5. Whittle HJ, Palar K, Hufstedler LL et al. Food insecurity, chronic illness, and gentrification in the San Francisco Bay Area: an example of structural violence in United States public policy. Soc Sci Med 2015;143:154–61. [DOI] [PubMed] [Google Scholar]
- 6. Robaina KA, Martin KS. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J Nutr Educ Behav 2013;45(2):159–64. [DOI] [PubMed] [Google Scholar]
- 7. Supplemental Nutrition Assistance Program (SNAP) Eligibility. United States Department of Agriculture Food and Nutrition Service; 2016.
- 8. Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009. Definition of Homelessness., P.L. 111–22, Sec. 1003 (2009).
- 9. Using homelessness and housing needs data to tailor and drive local solutions United States Interagency Council on Homelessness; 2017.
- 10. Burnam MA, Koegel P. Methodology for obtaining a representative sample of homeless persons: the Los Angeles Skid Row Study. Eval Rev 1988;12:117–52. [Google Scholar]
- 11. Lee CT, Guzman D, Ponath C et al. Residential patterns in older homeless adults: results of a cluster analysis. Soc Sci Med 2016;153:131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kripalani S, Bengtzen R, Henderson LE et al. Clinical research in low-literacy populations: using teach-back to assess comprehension of informed consent and privacy information. IRB 2008;30(2):13–9. [PubMed] [Google Scholar]
- 13. Lee JS, Johnson MA, Brown A et al. Food security of older adults requesting Older Americans Act Nutrition Program in Georgia can be validly measured using a short form of the U.S. Household Food Security Survey Module. J Nutr 2011;141(7):1362–8. [DOI] [PubMed] [Google Scholar]
- 14. Definitions of Food Security USDA Economic Research Service; 2017.
- 15. Tsemberis S, McHugo G, Williams V et al. Measuring homelessness and residential stability: The Residential Time-Line Follow-Back Inventory. J Community Psychol 2007;35(1):29–42. [Google Scholar]
- 16. Ware J Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- 17. National Health and Nutrition Examination Survey Questionnaire (NHANES) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2009.
- 18. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385–401. [Google Scholar]
- 19. Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3 MS) as a screen for dementia. Can J Psychiatry 2001;46(6):506–10. [DOI] [PubMed] [Google Scholar]
- 20. Bravo G, Hebert R. Age- and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry 1997;12(10):1008–18. [DOI] [PubMed] [Google Scholar]
- 21. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 1983;31(12):721–7. [DOI] [PubMed] [Google Scholar]
- 22. Sullivan G, Dumenci L, Burnam A et al. Validation of the brief instrumental functioning scale in a homeless population. Psychiatr Serv 2001;52(8):1097–9. [DOI] [PubMed] [Google Scholar]
- 23. Al-Delaimy WK, Edland S, Pierce JP et al. California Tobacco Survey (CTS): 2008. California Department of Health Services. 2011.
- 24. Babor TF, Higgins-Biddle JC, Saunders JB et al. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva: World Health Organization, 2001. [Google Scholar]
- 25. Humeniuk R, Henry-Edwards S, Ali R et al. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for Use in Primary Care. Geneva: World Health Organization, 2010. [Google Scholar]
- 26. Gielen AC, McDonnell KA, Wu AW et al. Quality of life among women living with HIV: the importance violence, social support, and self care behaviors. Soc Sci Med 2001;52(2):315–22. [DOI] [PubMed] [Google Scholar]
- 27. Bowen EA, Bowen SK, Barman-Adhikari A. Prevalence and covariates of food insecurity among residents of single-room occupancy housing in Chicago, IL, USA. Public Health Nutr 2015;19(6):1122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parpouchi M, Moniruzzaman A, Russolillo A et al. Food insecurity among homeless adults with mental illness. PLoS One 2016;11(7):e0159334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Holland AC, Kennedy MC, Hwang SW. The assessment of food security in homeless individuals: a comparison of the Food Security Survey Module and the Household Food Insecurity Access Scale. Public Health Nutr 2011;14(12):2254–9. [DOI] [PubMed] [Google Scholar]
- 30. Baggett TP, Singer DE, Rao SR et al. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med 2011;26(6):627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coleman-Jensen A, Rabbitt MP, Gregory CA et al. Household food security in the United States in 2016, ERR-237. Vol ERR-237: United States Department of Agriculture, Economic Research Service; 2017.
- 32. Food Insecurity Among Older Adults 2015 Update. American Association of Retired Persons (AARP) Foundation; 2015.
- 33. Supplemental Nutrition Assistance Program (SNAP) : Deductions. United States Department of Agriculture FaNS; 2016.
- 34. Martins DC, Gorman KS, Miller RJ et al. Assessment of food intake, obesity, and health risk among the homeless in Rhode Island. Public Health Nurs 2015;32(5):453–61. [DOI] [PubMed] [Google Scholar]
- 35. Cimino T, Steinman MA, Mitchell SL et al. Disabled on the street: the course of functional impairment in older homeless adults. JAMA Intern Med 2015;175(7):1237–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bazerghi C, McKay FH, Dunn M. The role of food banks in addressing food insecurity: a systematic review. J Community Health 2016;41(4):732–40. [DOI] [PubMed] [Google Scholar]
- 37. Huang DL, Rosenberg DE, Simonovich SD et al. Food access patterns and barriers among midlife and older adults with mobility disabilities. J Aging Res 2012;2012:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ford PJ, Cramb S, Farah CS. Oral health impacts and quality of life in an urban homeless population. Aust Dent J 2014;59:234–9. 0527 DCOM- 20140911 (18347819 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 39. Tsai AC, Bangsberg DR, Frongillo EA et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med 2012;74(12):2012–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jo YH, Talmage DA, Role LW. Nicotinic receptor-mediated effects on appetite and food intake. J Neurobiol 2002;53(4):618–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Denial of Assistance and Benefits for Certain Drug-related Convictions Section 115 2014.