Abstract
Mucin-producing gallbladder carcinoma (MPGBC) is a rare and aggressive subtype of gallbladder carcinoma. We present a case of MPGBC with associated magnetic resonance imaging (MRI) / magnetic resonance cholangiopancreatography (MRCP) findings that may raise suspicion of this diagnosis preoperatively.
Keywords: mucin producing gallbladder carcinoma, mrcp
Introduction
In the United States, the incidence of gallbladder carcinoma is less than 5,000 cases per year [1]. Though this malignancy has several histological variants, mucin-producing gallbladder carcinoma (MPGBC) is a particularly rare and aggressive subtype. Recent studies suggest that it accounts for only 2.5%-5.5% of all gallbladder carcinomas [2-3].
MPGBC often presents with nonspecific, cholecystitis-like symptoms or is found incidentally during a cholecystectomy [4]. It can be difficult to differentiate from more benign entities using ultrasonography (US) or computed tomography (CT) alone [5-7]. As our case demonstrates, magnetic resonance imaging (MRI) / magnetic resonance cholangiopancreatography (MRCP) may be valuable in evaluating, and possibly diagnosing, MPGBC.
Case presentation
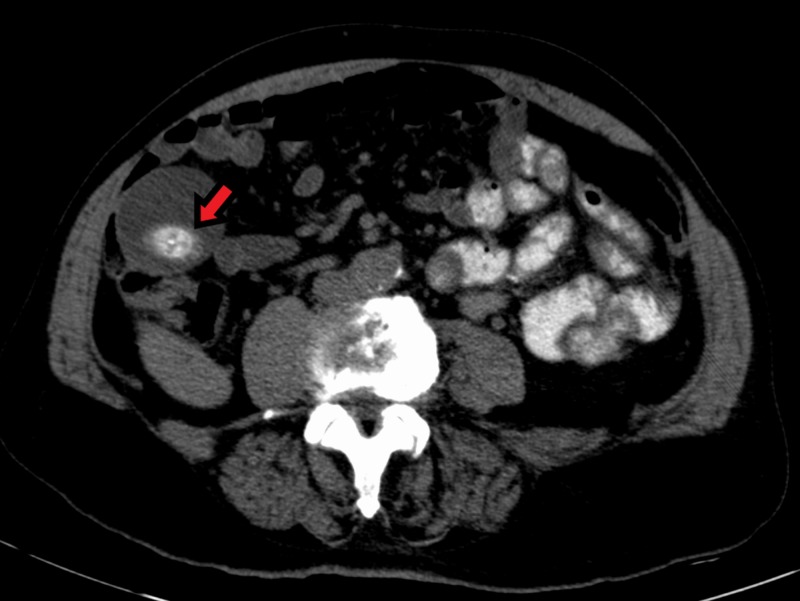
We present a 78-year-old male with a past medical history of dementia, coronary artery disease, hypertension, and chronic obstructive pulmonary disease (COPD) who presented to the emergency department for evaluation of severe jaundice and itching. He denied abdominal pain. His hypertransaminemia and hyperbilirubinemia suggested obstructive jaundice. Abdominal CT with oral contrast was nonspecific, showing gallbladder dilation and what appeared to be a simple calcified gallstone in the dependent portion of the fundus (Figures 1-2). Notably, what was likely the same stone was seen on a CT abdomen performed 10 years prior, but further imaging was not done at that time (Figure 3).
Figure 1. Coronal CT of the abdomen with oral contrast demonstrating a significantly dilated gallbladder. A 3 cm calcification is seen in the dependent portion of the fundus (arrow).
CT - Computed Tomography
Figure 2. Axial view CT abdomen with oral contrast demonstrating a significantly dilated gallbladder. A 3 cm calcification is seen in the dependent portion of the fundus (arrow).
CT - Computed tomography
Figure 3. Axial CT of the abdomen without contrast taken 10 years prior. Prominent irregular calcification visible in the gallbladder fundus (arrow).
CT - Computed tomography
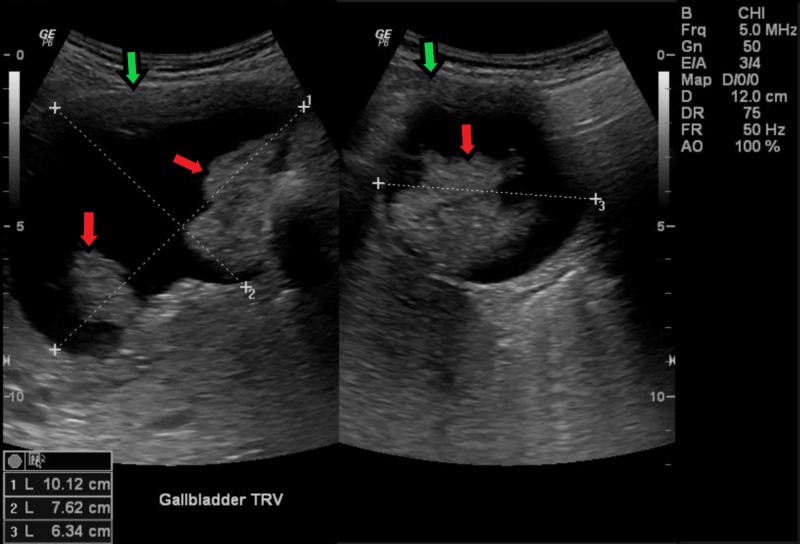
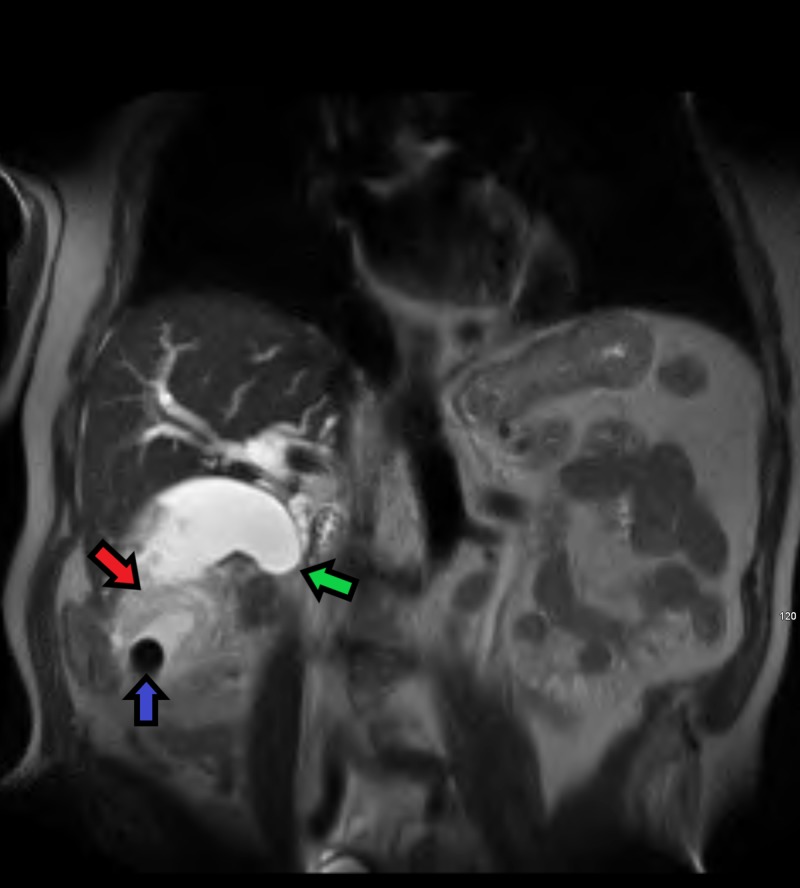
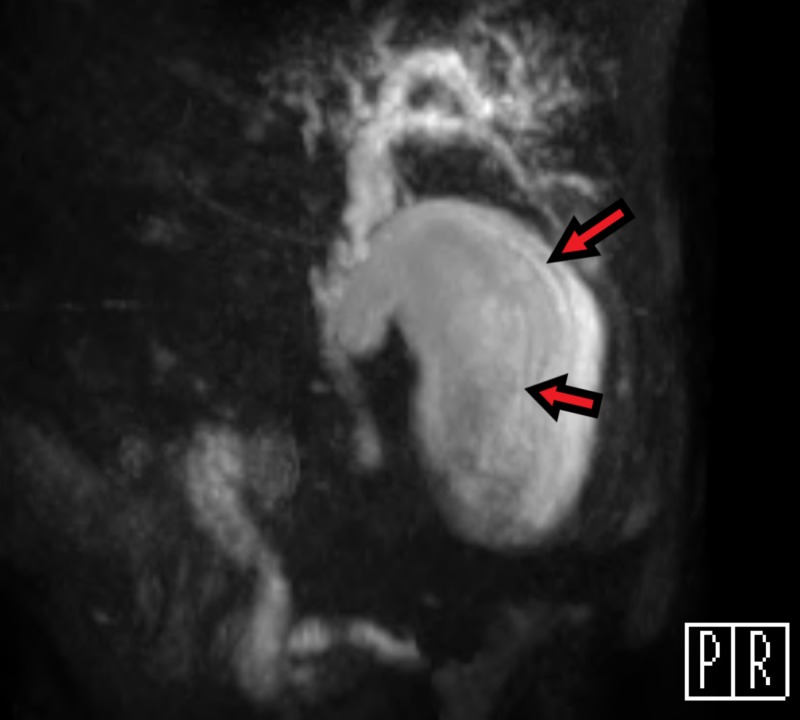
During this evaluation, follow-up US revealed irregular intraluminal masses that raised suspicions for malignancy (Figure 4). Subsequent MRI/MRCP clearly demonstrated a large, irregular mass surrounding the gallstone. Of note, hypointense curvilinear striations were visible along the long axis of the gallbladder (Figures 5-6). This characteristic finding has been seen before and was coined a “mucous thread” sign. It has been theorized to be the result of excessive viscous mucin produced by this carcinoma [8].
Figure 4. Transverse ultrasound of the gallbladder revealing multiple intraluminal masses (red arrows) and irregular wall thickening (green arrows). Gallbladder dimensions are given in the bottom left corner.
Figure 5. Coronal MRI T2 HASTE weighted image demonstrating a large mass (red arrow) surrounding a gallstone (blue arrow) in the distal portion of the gallbladder fundus. There is sharp tapering in the mid-to-distal common bile duct (green arrow) indicating obstruction secondary to infiltration by the mass.
MRI - Magnetic resonance image, HASTE - Half-Fourier Acquisition Single-shot Turbo Spin-Echo
Figure 6. Oblique MRCP view of the gallbladder. Shows peripheral hypointense curvilinear striations parallel to the long axis (arrows) consistent with a mucous thread sign.
MRCP - Magnetic resonance cholangiopancreatography
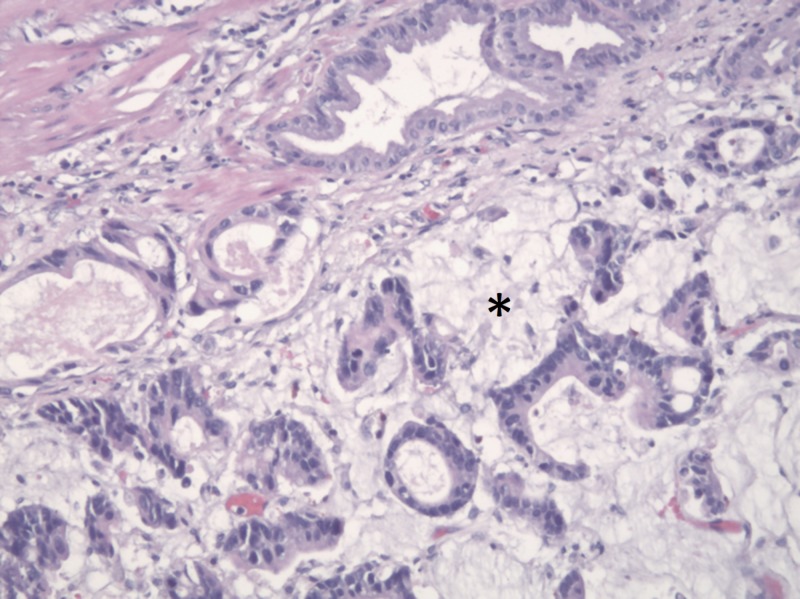
Though a laparoscopic cholecystectomy was performed, the area of invasion was too extensive for full resection. Histological samples confirmed MPGBC (Figure 7). The patient and his family declined further treatment of his malignancy, and he expired six months later.
Figure 7. H&E stain showing malignant epithelial cells and glands surrounded by pools of extracellular mucin (asterisk), consistent with MPGBC.
H&E - Hematoxylin and Eosin, MPGBC - Mucin-producing gallbladder carcinoma
Discussion
MPGBC is extremely rare and can be overlooked or confused with less dangerous entities. It typically mimics acute cholecystitis and, therefore, most cases are diagnosed in the operating room during what is assumed to be a routine cholecystectomy. A careful imaging workup prior to surgery could inform clinicians and patients that they are dealing with a more malignant process. It is important for radiologists and other clinicians to be aware that the unique properties of this cancer may render some imaging modalities inferior to others.
Our case demonstrates the difficulty that CT can have in identifying MPGBC. Simply, a CT image is constructed based on the densities of different structures within the patient. Within the lumen of our patient's gallbladder, a hyperdense calcified gallstone is clearly visible. However, in these images, there is little evidence of a large mass surrounding the stone. Other researchers have described similar CT findings in cases of MPGBC. They have speculated that the excessive amount of mucin produced within the tumor may give it a density near to that of water; obscuring the mass by making it impossible to differentiate from fluid already within the gallbladder [7].
Ultrasonography is the initial imaging test of choice for any patient with possible gallbladder disease. Benefits include low cost and ease of use. In most cases, it adequately identifies masses in the gallbladder. However, it is less reliable in determining whether the mass is benign or malignant. It is inferior to other imaging modalities (CT and MRI) for identifying and staging gallbladder cancer. Due to this, current guidelines recommend following up any suspicious US findings with either a CT or an MRI [5-7].
As previously discussed, the MRI for our patient was much more informative than the other imaging techniques. While the CT could only visualize a gallstone, the MRI clearly depicted the large mass totally enveloping the stone and filling the gallbladder. At this point in the evaluation, a malignant process was obviously strongly suspected. Likely due to the rarity of MPGBC, it still came as a surprise when the intraoperative pathology report returned with this diagnosis.
Our retrospective investigation revealed that the MRCP may have suggested the lesion was this specific subtype of gallbladder cancer. It is possible that the hypointense striations along the long axis of the patient's gallbladder are unique radiographic signs of MPGBC. To our knowledge, there is no other case study discussing MRCP evaluation of MPGBC in United States literature. Japanese researchers, however, identified multiple patients with MPGBC who had similar linear hypointense areas visible on MRCP. They considered that the highly viscous properties of the mucin were responsible for the appearance of these characteristic striations and named this a “mucous thread” sign [8].
Conclusions
Our case highlights the limitations of CT and US, as well as the value of MRI/MRCP, in the diagnostic evaluation of MPGBC. In addition, we draw attention to a unique radiographic finding of MPGBC (mucous thread sign) that may lead to the early detection of this highly fatal disease.
Acknowledgments
Dr. Maryam Sharifian, David Costello
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Liver, gallbladder, extrahepatic bile ducts, and pancreas. Carriaga MT, Henson DE. https://www.ncbi.nlm.nih.gov/pubmed/8000995. Cancer. 1995;75:171–190. doi: 10.1002/1097-0142(19950101)75:1+<171::aid-cncr2820751306>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 2.Mucinous carcinoma of the gallbladder: clinicopathologic analysis of 15 cases identified in 606 carcinomas. Dursun N, Escalona OT, Roa JC, et al. https://www.archivesofpathology.org/doi/full/10.5858/arpa.2011-0447-OA. Arch Pathol Lab Med. 2012;136:1347–1358. doi: 10.5858/arpa.2011-0447-OA. [DOI] [PubMed] [Google Scholar]
- 3.Gallbladder carcinoma: an attempt of WHO histological classification on fine needle aspiration material. Yadav R, Jain D, Mathur SR, Sharma A, Iyer VK. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709381/ Cytojournal. 2013;10:12. doi: 10.4103/1742-6413.113627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallbladder carcinoma: radiologic-pathologic correlation. Levy AD, Murakata LA, Rohrmann CA Jr. https://pubs.rsna.org/doi/full/10.1148/radiographics.21.2.g01mr16295. RadioGraphics. 2001;21:295–314. doi: 10.1148/radiographics.21.2.g01mr16295. [DOI] [PubMed] [Google Scholar]
- 5.Biliary cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Valle JW, Borbath I, Khan SA, Huguet F, Gruenberger T, Arnold D. https://www.ncbi.nlm.nih.gov/pubmed/27664259. Ann Oncol. 2016;27:28–37. doi: 10.1093/annonc/mdw324. [DOI] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network. Gallbladder cancer. [May;2019 ];https://www.nccn.org/patients/guidelines/hepatobiliary/files/assets/common/downloads/SurveyQuickGuide_waldenstroms.pdf?uni=3efe6a42fd33d2c85a0f366f237da97d 2018
- 7.Imaging findings in mucin-producing carcinoma of the gallbladder. Huang CP, Chiou YY, Chou YH, Chiang JH, Chang CY. https://www.sciencedirect.com/science/article/pii/S0929664609601418. J Formos Med Assoc. 2006;105:427–430. doi: 10.1016/S0929-6646(09)60141-8. [DOI] [PubMed] [Google Scholar]
- 8.Mucin-producing carcinoma of the gallbladder: evaluation by magnetic resonance cholangiopancreatography in three cases. Ishiguro S, Onaya H, Esaki M, et al. https://synapse.koreamed.org/search.php?where=aview&id=10.3348/kjr.2012.13.5.637&code=0068KJR&vmode=FULL. Korean J Radiol. 2012;13:637–642. doi: 10.3348/kjr.2012.13.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]