Background:
The risk of subsequent joint replacement following an index joint replacement for osteoarthritis and the association of this risk with demographic and patient-specific factors are not well understood. The purpose of this study was to determine how demographic and other patient-specific factors are associated with the risk of subsequent joint replacement in the contralateral or a different joint following an index joint replacement for osteoarthritis.
Methods:
The Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) of New York was used to identify the first (primary) total hip arthroplasty (THA), total knee arthroplasty (TKA), or total shoulder arthroplasty (TSA) and the risk of subsequent joint replacement in the contralateral or a different joint over 5 to 8 years. The association of demographic and other patient-specific factors with subsequent joint replacement was assessed via multivariable Cox proportional hazards modeling. We also investigated the time between the index and subsequent joint replacement.
Results:
Of 85,616 patients, 20,223 (23.6%) underwent a subsequent replacement of the contralateral joint within 5 to 8 years (median, 343 days) after the index joint replacement. The strongest predictors were obesity (adjusted hazard ratio [HR] = 1.28; p < 0.001) and index TKA compared with THA (1.72; p < 0.001). A total of 3,197 patients (3.7%) underwent a subsequent replacement of a different joint within 5 to 8 years (median, 876 days) after the index joint replacement. The strongest predictors were obesity (adjusted HR = 1.41; p < 0.001) and index TSA compared with THA (adjusted HR = 2.52; p < 0.001).
Conclusions:
There is a relatively high risk of subsequent replacement of the contralateral joint and a relatively low risk of subsequent replacement of a different joint within 5 to 8 years after an index THA, TKA, or TSA. Obesity was associated with a higher risk of subsequent replacement of the contralateral joint or a different joint.
Level of Evidence:
Prognostic Level IV. See Instructions for Authors for a complete description of levels of evidence.
The prevalence of symptomatic osteoarthritis is substantial and rising1,2. Osteoarthritis is projected to affect 25% of the U.S. adult population by 2020, with working-age adults (ages 45 to 64 years) comprising one-third of cases2. Current data suggest a similar prevalence in Europe, and while the prevalence throughout the world is variable, osteoarthritis remains a major cause of disability globally3,4. Osteoarthritis is more common in older5 and obese5-7 patients. As the world population ages and becomes heavier, the prevalence of symptomatic osteoarthritis will continue to increase2,8,9. Similarly, the incidence of total knee arthroplasty (TKA), total hip arthroplasty (THA), and total shoulder arthroplasty (TSA) has substantially increased over the past 2 decades and is projected to continue to increase8-11.
While several studies have projected a significantly increased demand for joint replacement8,12, there have been few large database studies addressing the risk of subsequent joint replacement following an index joint replacement for osteoarthritis13 and, to our knowledge, no large database study has addressed the association of demographic and other patient-specific factors with subsequent joint replacement. The primary purpose of this study was to determine which demographic and other patient-specific factors are associated with the risk of subsequent replacement of the contralateral or a different joint following an index joint replacement for osteoarthritis. Specifically, we sought to determine (1) the proportional distribution of subsequent joint replacements among the hip, knee, and shoulder following index THA, TKA, and TSA and (2) whether age, sex, smoking status, obesity, and diabetes mellitus were associated with an increased risk of subsequent joint replacement following an index joint replacement.
Materials and Methods
The Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) maintained by the Agency for Healthcare Research and Quality (AHRQ) contains administrative data relevant to hospital reimbursement for inpatient encounters in all continental U.S. states. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to identify the first recorded primary THA (81.51), TKA (81.54), or TSA (81.80) in the period from 2006 to 2008 for patients in the New York SID. The indication for joint replacement was based on the ICD-9-CM code recorded as “Diagnosis #1” (primary admission diagnosis) for the inpatient encounter when the joint replacement was performed. In addition to primary osteoarthritis of the hip, knee, or shoulder, we compiled a list of alternate primary diagnoses consistent with primary osteoarthritis that were eligible for inclusion (see Appendix Table E-1). We had access to the database starting in 2005, when the patient-link variable was introduced, allowing multiple hospital encounters for a single patient to be linked together. We began to record index joint replacements starting in 2006 and therefore had at least 1 year of inpatient data on every patient prior to what was recorded as their index joint replacement.
Patients with a primary diagnosis associated with a joint-compromising disease process other than osteoarthritis, diagnosed before or after the index or subsequent joint replacement, were excluded from the study (see Appendix Table E-2). Patients who underwent revision arthroplasty with documentation of primary joint replacement involving another joint prior to 2006, those who had a previous arthrotomy, and those who died had during the index joint replacement were also excluded (see Appendix Table E-3). Although laterality was not defined in the data set because of limitations of ICD-9-CM coding, revision joint replacements were differentiated from primary joint replacements by ICD-9-CM codes. Seventeen patients who had multiple joint replacements performed on different joints (that is, not bilateral TKA or THA) during the index admission were also excluded. Elective multiple-joint replacement involving different joints is extremely rare, and it was difficult to ascertain the primary joint involved or any extenuating factors contributing to the operative plans.
We then determined the incidence proportion of subsequent joint replacement following index joint replacement. The cohort was limited to individuals who underwent the index joint replacement from 2006 to 2008, with data available through 2013, thus providing a minimum 5-year follow-up on all included patients. We identified all individuals who underwent subsequent joint replacement, applying the same, aforementioned exclusion criteria as used to exclude index joint replacements. Patients with no additional hospital admissions following index joint replacement, or with readmissions with no indication of a subsequent joint replacement or any ICD-9-CM diagnosis meeting the exclusion criteria, were assumed to have not undergone subsequent joint replacement and to have not developed any exclusion criteria. These individuals were maintained in the analysis as part of the eligible at-risk population.
The primary outcome was subsequent joint replacement for end-stage osteoarthritis in ≥1 joints within 5 to 8 years after the index joint replacement. Secondary outcomes included the proportional distribution of subsequent joint replacement among the hip, knee, and shoulder. The relative risk of, age at, and most likely site of subsequent joint replacement were then calculated for, and compared among, the 3 index procedures. We also investigated the association between age, sex, obesity, diabetes mellitus, and smoking and the incidence proportion of, time interval to, and age at subsequent joint replacement. Individuals who underwent bilateral same-joint replacement as the index surgery were analyzed as having an index and second surgery performed on the same joint (i.e., the second surgery on the contralateral joint), an age at the second surgery equal to the age at the index surgery, and a time between the surgical procedures equal to 0 days.
Statistical Analysis
Continuous variables are presented as the mean and standard deviation (SD) or the median with first and third quartiles (Q1 and Q3, respectively) depending on the distribution of the data. Categorical variables are presented as numbers and percentages. Chi-square tests were used to compare the proportions of subsequent joint replacements on other joints with those on the contralateral joint. The association of the index surgery and demographic and other patient-specific factors with subsequent replacement of the contralateral joint, a different joint, or either outcome was assessed via multivariable Cox proportional hazards modeling with robust standard errors to account for clustering of patients within hospitals. Data analysis was conducted with SAS Enterprise Guide software (SAS Institute).
Results
Patient Population
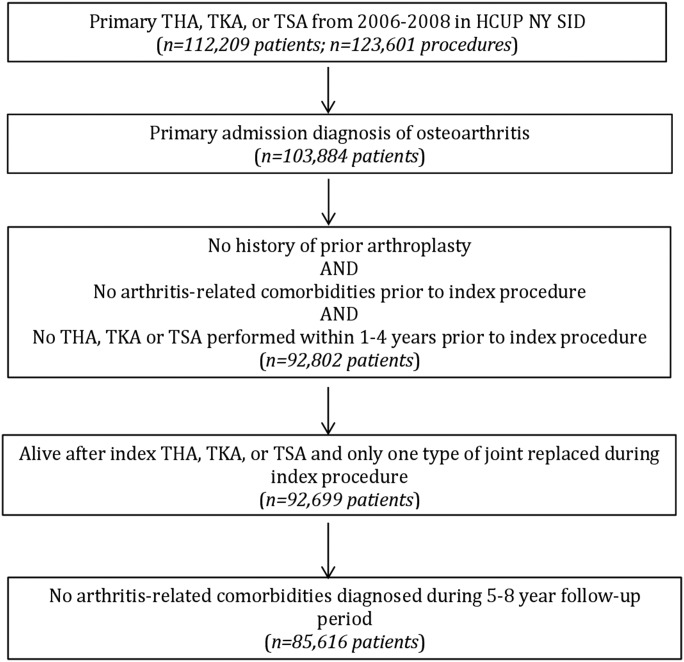
The patient-selection algorithm and resulting eligible patient population are summarized in Figure 1. The index procedures were primarily unilateral, with bilateral same-joint replacement comprising only 5.3% of all index procedures. Demographics are presented in Table I.
Fig. 1.
Patient selection flow diagram.
TABLE I.
Patient Demographics
| Demographics | No. (%) of Patients* (N = 85,616) |
| Female | 54,366 (63.5) |
| Obese | 12,917 (15.1) |
| Diabetic | 14,428 (16.9) |
| Smoker | 3,974 (4.6) |
| Index total joint replacement | |
| THA | 30,144 (35.2) |
| TKA | 53,931 (63.0) |
| TSA | 1,541 (1.8) |
| Age at index total joint replacement (yr) | 66.2 ± 10.9 |
With the exception of age, which is given as the mean and SD.
Incidence Proportion and Location of Subsequent Joint Replacement
Overall, 27.3% (95% confidence interval [CI] = 27.1% to 27.7%) of the patients underwent a subsequent joint replacement within 5 to 8 years after the index total joint replacement, at a median of 381 days (Q1, Q3 = 105, 982) following the index joint replacement. Regardless of whether the index joint replacement was a THA, TKA, or TSA, the subsequent replacement was most frequently performed in the joint contralateral to the index procedure (23.6% [95% CI = 23.3% to 23.9%]), at a median of 343 days (Q1, Q3 = 70, 871) following the index joint replacement. Similar to the distribution of the index joint replacements, the subsequent joint replacements were most commonly performed on the knee, comprising 70.1% (95% CI = 69.5% to 70.7%) of all subsequent joint replacements performed (Table II). Patients who underwent an index TKA were more likely to undergo subsequent replacement of the contralateral joint within 5 to 8 years than those who underwent an index THA or TSA (Table III). A total of 3,197 patients (3.7% [95% CI = 3.6% to 3.9%]) underwent a subsequent replacement of a different joint within 5 to 8 years after the index joint replacement, at a median of 876 days (Q1, Q3 = 413, 1,365) after the index joint replacement. Patients who underwent an index TSA were more likely to undergo subsequent replacement of a different joint than those treated with THA or TKA (Table IV).
TABLE II.
Prevalence of Subsequent Total Joint Replacement at 5 to 8 Years According to Index Joint Replaced
| Index/2nd Event | No. (%) | Relative Risk (95% CI)* | P Value |
| Index THA | |||
| 2nd total joint replacement | 6,750 (22.4) | ||
| THA | 5,198 (17.2) | Reference | Reference |
| TKA | 1,445 (4.8) | 0.28 (0.27, 0.29) | <0.001 |
| TSA | 107 (0.4) | 0.02 (0.02, 0.02) | <0.001 |
| No 2nd total joint replacement | 23,394 (77.6) | ||
| Index TKA | |||
| 2nd total joint replacement | 16,278 (30.2) | ||
| THA | 1,226 (2.3) | 0.08 (0.08, 0.09) | <0.001 |
| TKA | 14,835 (27.5) | Reference | Reference |
| TSA | 217 (0.4) | 0.02 (0.01, 0.02) | <0.001 |
| No 2nd total joint replacement | 37,653 (69.8) | ||
| Index TSA | |||
| 2nd total joint replacement | 392 (25.4) | ||
| THA | 61 (4.0) | 0.32 (0.25, 0.41) | <0.001 |
| TKA | 141 (9.1) | 0.74 (0.63, 0.88) | <0.001 |
| TSA | 190 (12.3) | Reference | Reference |
| No 2nd total joint replacement | 1,149 (74.6) |
Relative risk compared with contralateral joint.
TABLE III.
Subsequent Total Joint Replacement of Contralateral Joint
| No. (%)* |
||||
| Demographics | Subsequent Replacement of Contralateral Joint (N = 20,223) | No Subsequent Replacement of Contralateral Joint (N = 65,393) | Adjusted HR (95% CI) | P Value |
| Female | 13,340 (66.0) | 41,026 (62.7) | 1.08 (1.05, 1.12) | <0.001 |
| Obese | 3,843 (19.0) | 9,074 (13.9) | 1.28 (1.22, 1.34) | <0.001 |
| Diabetic | 3,250 (16.1) | 11,178 (17.1) | 0.87 (0.83, 0.91) | <0.001 |
| Smoker | 835 (4.1) | 3,139 (4.8) | 0.80 (0.75, 0.85) | <0.001 |
| Index total joint replacement | ||||
| THA | 5,198 (25.7) | 24,946 (38.1) | Reference | Reference |
| TKA | 14,835 (73.4) | 39,096 (59.8) | 1.72 (1.66, 1.79) | <0.001 |
| TSA | 190 (0.9) | 1,351 (2.1) | 0.76 (0.66, 0.87) | <0.001 |
| Age at index total joint replacement (yr) | 64.7 ± 9.9 | 66.7 ± 11.1 | 0.99 (0.98, 0.99) | <0.001 |
With the exception of age, which is given as the mean and SD.
TABLE IV.
Subsequent Total Joint Replacement of Different Joint
| No. (%)* |
||||
| Demographics | Subsequent Replacement of Different Joint (N = 3,197) | No Subsequent Replacement of Different Joint (N = 82,419) | Adjusted HR (95% CI) | P Value |
| Female | 2,187 (68.4) | 52,179 (63.3) | 1.31 (1.21, 1.43) | <0.001 |
| Obese | 542 (17.0) | 12,375 (15.0) | 1.41 (1.30, 1.54) | <0.001 |
| Diabetic | 461 (14.4) | 13,967 (16.9) | 0.85 (0.77, 0.94) | 0.001 |
| Smoker | 124 (3.9) | 3,850 (4.7) | 0.83 (0.71, 0.99) | 0.034 |
| Index total joint replacement | ||||
| THA | 1,552 (48.5) | 28,592 (34.7) | Reference | Reference |
| TKA | 1,443 (45.1) | 52,488 (63.7) | 0.55 (0.49, 0.61) | <0.001 |
| TSA | 202 (6.3) | 1,339 (1.6) | 2.52 (2.14, 2.98) | <0.001 |
| Age at index total joint replacement (yr) | 67.7 ± 9.3 | 66.1 ± 10.9 | 1.01 (1.01, 1.01) | <0.001 |
With the exception of age, which is given as the mean and SD.
Factors Associated with Subsequent Joint Replacement
Age
Patients who underwent subsequent replacement of the contralateral joint were younger at the time of the index total joint replacement than those who did not (64.7 ± 9.9 compared with 66.7 ± 11.1 years, p < 0.001; adjusted hazard ratio [HR] = 0.99 [95% CI = 0.98, 0.99]; Table III). Interestingly, patients who underwent subsequent replacement of a different joint were actually older at the time of the index total joint replacement than those who did not (67.7 ± 9.3 compared with 66.1 ± 10.9 years, p < 0.001; adjusted HR = 1.01 [95% CI = 1.01, 1.01]; Table IV). Overall, patients who underwent any subsequent joint replacement (of either the contralateral or a different joint) were younger at the time of the index total joint replacement than those who did not (65.1 ± 9.8 compared with 66.6 ± 11.2 years, p < 0.001; adjusted HR = 0.99 [95% CI = 0.99, 0.99]; Table V).
TABLE V.
Subsequent Total Joint Replacement of Contralateral or Different Joint
| No (%)* |
||||
| Demographics | Subsequent Replacement (N = 23,420) | No Subsequent Replacement (N = 62,196) | Adjusted HR (95% CI) | P Value |
| Female | 15,527 (66.3) | 38,839 (62.4) | 1.11 (1.08, 1.15) | <0.001 |
| Obese | 4,385 (18.7) | 8,532 (13.7) | 1.30 (1.24, 1.35) | <0.001 |
| Diabetic | 3,711 (15.8) | 10,717 (17.2) | 0.86 (0.83, 0.90) | <0.001 |
| Smoker | 959 (4.1) | 3,015 (4.8) | 0.80 (0.76, 0.85) | <0.001 |
| Index total joint replacement | ||||
| THA | 6,750 (28.8) | 23,394 (37.6) | Reference | Reference |
| TKA | 16,278 (69.5) | 37,653 (60.5) | 1.45 (1.38, 1.51) | <0.001 |
| TSA | 392 (1.7) | 1,149 (1.8) | 1.18 (1.08, 1.32) | <0.001 |
| Age at index total joint replacement (yr) | 65.1 ± 9.8 | 66.6 ± 11.2 | 0.99 (0.99, 0.99) | <0.001 |
With the exception of age, which is given as the mean and SD.
Sex
Females were more likely than males to undergo subsequent replacement of the contralateral joint (24.5% compared with 22.0%, adjusted HR = 1.08 [95% CI = 1.05, 1.12]; Table III), subsequent replacement of a different joint (4.0% versus 3.2%, adjusted HR = 1.31 [95% CI = 1.21, 1.43]; Table IV), and subsequent replacement overall (28.6% compared 25.2%, adjusted HR = 1.11 [95% CI = 1.08, 1.15]; Table V).
Obesity
Obese patients (body mass index [BMI] of ≥30 kg/m2) were more likely than nonobese patients to undergo subsequent replacement of the contralateral joint (29.8% compared 22.5%, adjusted HR = 1.28 [95% CI = 1.22, 1.34]; Table III), subsequent replacement of a different joint (4.2% compared 3.7%, adjusted HR = 1.41 [95% CI = 1.30, 1.54]; Table IV), and subsequent replacement overall (33.9% versus 26.2%, adjusted HR = 1.30 [95% CI = 1.24, 1.35]; Table V).
Diabetes Mellitus
Patients with diabetes mellitus were less likely than nondiabetic patients to undergo subsequent replacement of the contralateral joint (22.5% compared with 23.8%, adjusted HR = 0.87 [95% CI = 0.83, 0.91]; Table III), subsequent replacement of a different joint (3.2% compared with 3.8%, adjusted HR = 0.85 [95% CI = 0.77, 0.94]; Table IV), and subsequent replacement overall (25.7% compared with 27.7%, adjusted HR = 0.86 [95% CI = 0.83, 0.90]; Table V).
Smoking
Smokers were less likely than nonsmokers to undergo subsequent replacement of the contralateral joint (21.0% compared with 23.7%, adjusted HR = 0.80 [95% CI = 0.75, 0.85]; Table III), subsequent replacement of a different joint (3.1% compared with 3.8%, adjusted HR = 0.83 [95% CI = 0.71, 0.99]; Table IV), and subsequent replacement overall (24.1% compared with 27.5%, adjusted HR = 0.80 [95% CI = 0.76, 0.85]; Table V).
Discussion
This database study identified demographic and other patient-specific factors associated with subsequent joint replacement after primary THA, TKA, and TSA for osteoarthritis. More than one-quarter had a subsequent joint replacement within 5 to 8 years after the index joint replacement, and it was most frequently of the contralateral joint. Interestingly, even though the overall incidence proportion of subsequent TKA was higher than that of subsequent THA or TSA, patients who underwent either an index THA or an index TSA as well as a subsequent joint replacement were still more likely to have the contralateral joint replaced. The finding that the contralateral joint was the most common second joint to be replaced is consistent with previously published studies of THA and TKA13,14 but, to our knowledge, has not been previously described for TSA. Among patients who underwent subsequent joint replacement, those who underwent an index TSA were more likely to have a different joint replaced than those who underwent an index THA or TKA. Obesity and female sex also increased the likelihood of subsequent joint replacement whereas smoking and diabetes decreased the likelihood of subsequent joint replacement. Given recent heightened awareness of the increased risk to the patient and cost to the health-care system associated with total joint replacement, the decreased likelihood of subsequent joint replacement in smokers and diabetic patients may be secondary to patient selection by surgeons15. While we are not aware of any previous report of an association between subsequent joint replacement and obesity, previous studies have shown that obese patients were more likely to develop osteoarthritis and undergo joint replacement at a younger age than those with a normal BMI16-23. Similarly, we demonstrated a higher prevalence of subsequent joint replacement among obese patients independent of age.
While both hip and knee osteoarthritis are frequently bilateral14,24-28, shoulder osteoarthritis is less commonly so29. Furthermore, one study showed that shoulder osteoarthritis is a significant risk factor for knee osteoarthritis30. Therefore, it would be expected that patients who underwent an index TSA would be the least likely to undergo subsequent contralateral total joint replacement and most likely to undergo subsequent different-joint replacement, and that is what our study demonstrated. TKA was the most common index and subsequent joint replacement performed in our study. Since there were 16,421 subsequent TKAs performed compared with only 6,485 subsequent THAs and 514 subsequent TSAs, it is logical that patients with both knees at risk (that is, who have not undergone a prior TKA) might be at higher risk for a subsequent joint replacement. However, consistent with multiple previously published studies13,14,31, the most common subsequently replaced joint was the contralateral joint, accounting for 86.3% of all subsequent joint replacements.
This study has several clinical implications. First, obesity was associated with a 28% increase in the risk of subsequent contralateral joint total joint replacement, a 41% increase in the risk of subsequent different-joint replacement, and a 30% increase in the risk of any subsequent joint replacement. The effect of obesity on the risk of subsequent joint replacement may be dampened by the fact that an extremely elevated BMI is considered a relative or absolute contraindication for joint replacement. As obesity is a modifiable risk factor18, patients should be counseled regarding the importance of weight loss strategies as a potential method to reduce the risk of future joint replacement14,18,32. Coggon et al.18 reported that 23.6% of TKAs could be avoided if all overweight and obese patients reduced their weight by 5 kg or until their BMI was within the normal range, which is consistent with the 28% to 41% increased risk of subsequent joint replacement that we report in the present study. Female patients had a 31% increase in the risk of a subsequent different-joint replacement. Finally, patients undergoing index TKA, THA, or TSA should be counseled that the contralateral joint is the most likely joint to be subsequently replaced.
There are several limitations to this study. As the data are drawn from a single U.S. state, the findings may not be generalizable to other states or countries, which may differ with respect to patient demographics and the prevalence of patient-specific factors such as obesity, cultural factors, diabetes mellitus, and smoking. Since we did not have access to this database until 2005, we were unable to determine whether a patient’s first joint replacement recorded in the period from 2005 to 2008 was truly the patient’s index joint replacement. While >75% of subsequent THAs and 86% of subsequent TKAs have been shown to occur within 10 years after the index THA or TKA, respectively31, a 5 to 8-year window likely did not encompass all subsequent joint replacements that occurred in this study. Furthermore, we relied on the accuracy of HCUP SID coding, including ICD-9-CM, which includes unicompartmental knee arthroplasty as part of ICD 81.54 (total knee replacement). Therefore, we were unable to determine how many knee replacements were unicompartmental, although previously published data suggest that they are a small percentage of the total33. There have been reports of inaccurate recording of comorbidities, including obesity, which tend to be underreported34,35. Smoking status, diabetes mellitus, and obesity are not quantified or categorized by severity within this database, but instead are simply dichotomized. As such, we were unable to assess the association of Class-2 obesity (BMI of 35 to 40 kg/m2) and Class-3 obesity (BMI of ≥40 kg/m2) with subsequent joint replacement. Future studies should aim to better elucidate these relationships. Given the large number of patients, it is also likely that the etiology of arthritis may have been inaccurately coded in some cases. Details regarding symptom severity and the degree of osteoarthritis seen radiographically were not available because of the nature of the study. Thus, we were unable to determine which patients presented with bilateral same-joint end-stage osteoarthritis and underwent sequential joint replacement in a staged fashion for surgical and/or medical reasons. We also did not assess the laterality of subsequent joint replacement, which reflects a limitation of the ICD-9-CM despite being evaluated in 2 prior studies13,14. Finally, replacements of other joints such as the elbow, ankle, and wrist were excluded from this study, so the incidence proportions may be an underestimate of the overall proportion of subsequent joint replacements following an index joint replacement.
In conclusion, patients treated with primary TSA, THA, or TKA had a significant likelihood of undergoing a subsequent joint replacement—most often on the contralateral joint—within 5 to 8 years. Obese patients had a higher likelihood of undergoing an additional joint replacement. These findings may facilitate counseling of patients considering or undergoing joint replacement regarding the likelihood, timing, and location of subsequent joint replacement. Medical providers and health-care organizations can also use this information to project the incidence and associated costs of subsequent joint replacements across care populations. Finally, identifying patients who are likely to undergo subsequent joint replacement on the basis of demographic and other patient-specific risk factors may facilitate the development and assessment of interventions to delay or prevent subsequent joint replacements.
Appendix
Tables showing included alternative primary diagnoses, excluded diagnoses, and excluded procedures are available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/E900).
Investigation performed at the Washington University School of Medicine, St. Louis, Missouri
Disclosure: Funding was provided through a Washington University Institute of Clinical and Translational Sciences grant (UL1 TR000448) from the National Center for Advancing Translational Sciences of the National Institutes of Health, Grant R24 HS19455 through the Agency for Healthcare Research and Quality, and Grant KM1CA156708 from the National Cancer Institute of the National Institutes of Health. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/E901).
Joseph D. Lamplot, MD, and Anchal Bansal, MD, contributed equally to this study.
References
- 1.Nguyen US, Zhang Y, Zhu Y, Niu J, Zhang B, Felson DT. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011. December 6;155(11):725-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iorio R, Robb WJ, Healy WL, Berry DJ, Hozack WJ, Kyle RF, Lewallen DG, Trousdale RT, Jiranek WA, Stamos VP, Parsley BS. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg Am. 2008. July;90(7):1598-605. [DOI] [PubMed] [Google Scholar]
- 3.Cushnaghan J, Coggon D, Reading I, Croft P, Byng P, Cox K, Dieppe P, Cooper C. Long-term outcome following total hip arthroplasty: a controlled longitudinal study. Arthritis Rheum. 2007. December 15;57(8):1375-80. [DOI] [PubMed] [Google Scholar]
- 4.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014. July;73(7):1323-30. Epub 2014 Feb 19. [DOI] [PubMed] [Google Scholar]
- 5.Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil. 2006. November;85(11)(Suppl):S2-11, quiz :S12–4. [DOI] [PubMed] [Google Scholar]
- 6.Sharma L, Lou C, Cahue S, Dunlop DD. The mechanism of the effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis Rheum. 2000. March;43(3):568-75. [DOI] [PubMed] [Google Scholar]
- 7.Lane NE, Brandt K, Hawker G, Peeva E, Schreyer E, Tsuji W, Hochberg MC. OARSI-FDA initiative: defining the disease state of osteoarthritis. Osteoarthritis Cartilage. 2011. May;19(5):478-82. Epub 2011 Mar 23. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007. April;89(4):780-5. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014. April 16;96(8):624-30. [DOI] [PubMed] [Google Scholar]
- 10.Trofa D, Rajaee SS, Smith EL. Nationwide trends in total shoulder arthroplasty and hemiarthroplasty for osteoarthritis. Am J Orthop (Belle Mead NJ). 2014. April;43(4):166-72. [PubMed] [Google Scholar]
- 11.Jain NB, Higgins LD, Guller U, Pietrobon R, Katz JN. Trends in the epidemiology of total shoulder arthroplasty in the United States from 1990-2000. Arthritis Rheum. 2006. August 15;55(4):591-7. [DOI] [PubMed] [Google Scholar]
- 12.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005. July;87(7):1487-97. [DOI] [PubMed] [Google Scholar]
- 13.Gillam MH, Lie SA, Salter A, Furnes O, Graves SE, Havelin LI, Ryan P. The progression of end-stage osteoarthritis: analysis of data from the Australian and Norwegian joint replacement registries using a multi-state model. Osteoarthritis Cartilage. 2013. March;21(3):405-12. Epub 2012 Dec 26. [DOI] [PubMed] [Google Scholar]
- 14.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002. December;46(12):3185-9. [DOI] [PubMed] [Google Scholar]
- 15.Hustedt JW, Goltzer O, Bohl DD, Fraser JF, Lara NJ, Spangehl MJ. Calculating the cost and risk of comorbidities in total joint arthroplasty in the United States. J Arthroplasty. 2017. February;32(2):355-361.e1. Epub 2016 Aug 9. [DOI] [PubMed] [Google Scholar]
- 16.Liu B, Balkwill A, Banks E, Cooper C, Green J, Beral V. Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle-aged women. Rheumatology (Oxford). 2007. May;46(5):861-7. Epub 2007 Feb 4. [DOI] [PubMed] [Google Scholar]
- 17.Changulani M, Kalairajah Y, Peel T, Field RE. The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Joint Surg Br. 2008. March;90(3):360-3. [DOI] [PubMed] [Google Scholar]
- 18.Coggon D, Reading I, Croft P, McLaren M, Barrett D, Cooper C. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord. 2001. May;25(5):622-7. [DOI] [PubMed] [Google Scholar]
- 19.Apold H, Meyer HE, Nordsletten L, Furnes O, Baste V, Flugsrud GB. Weight gain and the risk of knee replacement due to primary osteoarthritis: a population based, prospective cohort study of 225,908 individuals. Osteoarthritis Cartilage. 2014. May;22(5):652-8. Epub 2014 Mar 12. [DOI] [PubMed] [Google Scholar]
- 20.Bourne R, Mukhi S, Zhu N, Keresteci M, Marin M. Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res. 2007. December;465(465):185-8. [DOI] [PubMed] [Google Scholar]
- 21.Lohmander LS, Gerhardsson de Verdier M, Rollof J, Nilsson PM, Engström G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population-based prospective cohort study. Ann Rheum Dis. 2009. April;68(4):490-6. Epub 2008 May 8. [DOI] [PubMed] [Google Scholar]
- 22.Leyland KM, Judge A, Javaid MK, Diez-Perez A, Carr A, Cooper C, Arden NK, Prieto-Alhambra D. Obesity and the relative risk of knee replacement surgery in patients with knee osteoarthritis: a prospective cohort study. Arthritis Rheumatol. 2016. April;68(4):817-25. [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Wluka AE, Simpson JA, Giles GG, Graves SE, de Steiger RN, Cicuttini FM. Body weight at early and middle adulthood, weight gain and persistent overweight from early adulthood are predictors of the risk of total knee and hip replacement for osteoarthritis. Rheumatology (Oxford). 2013. June;52(6):1033-41. Epub 2013 Jan 28. [DOI] [PubMed] [Google Scholar]
- 24.Chitnavis J, Sinsheimer JS, Suchard MA, Clipsham K, Carr AJ. End-stage coxarthrosis and gonarthrosis. Aetiology, clinical patterns and radiological features of idiopathic osteoarthritis. Rheumatology (Oxford). 2000. June;39(6):612-9. [DOI] [PubMed] [Google Scholar]
- 25.Cooper C, Egger P, Coggon D, Hart DJ, Masud T, Cicuttini F, Doyle DV, Spector TD. Generalized osteoarthritis in women: pattern of joint involvement and approaches to definition for epidemiological studies. J Rheumatol. 1996. November;23(11):1938-42. [PubMed] [Google Scholar]
- 26.Günther KP, Stürmer T, Sauerland S, Zeissig I, Sun Y, Kessler S, Scharf HP, Brenner H, Puhl W. Prevalence of generalised osteoarthritis in patients with advanced hip and knee osteoarthritis: the Ulm Osteoarthritis Study. Ann Rheum Dis. 1998. December;57(12):717-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Husted H, Overgaard S, Laursen JO, Hindsø K, Hansen LN, Knudsen HM, Mossing NB. Need for bilateral arthroplasty for coxarthrosis. 1,477 replacements in 1,199 patients followed for 0-14 years. Acta Orthop Scand. 1996. October;67(5):421-3. [DOI] [PubMed] [Google Scholar]
- 28.Spector TD, Hart DJ, Doyle DV. Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Ann Rheum Dis. 1994. September;53(9):565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kobayashi T, Takagishi K, Shitara H, Ichinose T, Shimoyama D, Yamamoto A, Osawa T, Tajika T. Prevalence of and risk factors for shoulder osteoarthritis in Japanese middle-aged and elderly populations. J Shoulder Elbow Surg. 2014. May;23(5):613-9. Epub 2014 Feb 20. [DOI] [PubMed] [Google Scholar]
- 30.Oh JH, Chung SW, Oh CH, Kim SH, Park SJ, Kim KW, Park JH, Lee SB, Lee JJ. The prevalence of shoulder osteoarthritis in the elderly Korean population: association with risk factors and function. J Shoulder Elbow Surg. 2011. July;20(5):756-63. Epub 2011 May 6. [DOI] [PubMed] [Google Scholar]
- 31.Sanders TL, Maradit Kremers H, Schleck CD, Larson DR, Berry DJ. Subsequent total joint arthroplasty after primary total knee or hip arthroplasty: a 40-year population-based study. J Bone Joint Surg Am. 2017. March 1;99(5):396-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller GD, Nicklas BJ, Davis C, Loeser RF, Lenchik L, Messier SP. Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity (Silver Spring). 2006. July;14(7):1219-30. [DOI] [PubMed] [Google Scholar]
- 33.Liddle AD, Pandit H, Judge A, Murray DW. Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Joint Surg Am. 2016. January 6;98(1):1-8. [DOI] [PubMed] [Google Scholar]
- 34.Al Kazzi ES, Lau B, Li T, Schneider EB, Makary MA, Hutfless S. Differences in the Prevalence of Obesity, Smoking and Alcohol in the United States Nationwide Inpatient Sample and the Behavioral Risk Factor Surveillance System. PLoS One. 2015. November 4;10(11):e0140165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Browne JA, Novicoff WM, D’Apuzzo MR. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014. November 5;96(21):e180. [DOI] [PubMed] [Google Scholar]