Abstract
Background:
A complete understanding of the variables that influence patient satisfaction has yet to be reached. The purpose of this study was to determine whether patient-reported physical function, pain, and/or anxiety are associated with patient satisfaction in a hand and upper-extremity outpatient setting.
Methods:
This is a cohort study of 1,160 adult patients presenting to an upper-extremity (non-shoulder) clinic from January 1, 2014, to December 31, 2016, who completed functional patient-reported outcome measures (PROMIS [Patient-Reported Outcomes Measurement Information System] Physical Function, PROMIS Upper Extremity, and abbreviated Disabilities of the Arm, Shoulder and Hand scale [QuickDASH]) and psychological patient-reported outcome measures (PROMIS Anxiety and PROMIS Pain Interference) immediately prior to their physician encounter. After the clinic visit, included patients filled out the Press Ganey Medical Practice satisfaction survey online. Logistic regression models were used to predict overall patient satisfaction and satisfaction with the care provider among all, new, and return clinic visit types from the patient-reported functional and psychological measures, controlling for age and provider.
Results:
Among all visit types, there was a significant negative association of both pain and anxiety with patient satisfaction, whereby a 10-point increase in PROMIS Pain Interference (higher self-reported pain symptomatology) was associated with a 17% decrease in the odds of overall satisfaction (odds ratio [OR], 0.83 [95% confidence interval (CI), 0.71 to 0.98]; p = 0.03), and a 10-point increase in PROMIS Anxiety (higher self-reported anxiety) was associated with a 16% decrease in the odds of satisfaction with the care provider (OR, 0.84 [95% CI, 0.72 to 0.97]; p = 0.02). A significant positive association was found between higher levels of self-reported physical function and new-patient satisfaction with their care provider (OR, 1.22 [95% CI, 1.02 to 1.47]; p = 0.03). Among return patient visits, there was a negative association with overall patient satisfaction between both pain interference (OR, 0.76 [95% CI, 0.58 to 0.98]; p = 0.04) and anxiety (OR, 0.69 [95% CI, 0.53 to 0.89]; p < 0.01).
Conclusions:
In hand and upper-extremity (non-shoulder) clinic visits, pre-encounter levels of patient-reported physical function, anxiety, and pain were significantly associated with patient satisfaction with the care provided. As the U.S. health-care system increasingly utilizes satisfaction scores in payment models and in quality assessment, these associations may influence how such metrics are interpreted and are utilized.
In the past several decades, the medical community has placed greater emphasis on patient-reported outcome assessments as valuable tools to measure health and function. For example, in an effort to improve, standardize, and utilize patient-reported outcome data, the National Institutes of Health (NIH) funded the development of the Patient-Reported Outcomes Measurement Information System (PROMIS)1.
At the same time, patient satisfaction scores have been popularized as a way to measure the patient experience of health-care delivery2. For example, the Consumer Assessment of Healthcare Providers and Systems (CAHPS) is a group of publicly available surveys that have been utilized since 1995, and the results of the CAHPS surveys are used by the Centers for Medicare & Medicaid Services (CMS) and other payers to adjust reimbursement for care as part of the ongoing pay-for-performance initiative.
Press Ganey is currently the nation’s largest provider of tools for measuring and analyzing the outpatient experience, and the results of the Press Ganey surveys impact health-care delivery, reimbursement, and care provider selection in a variety of ways3. As CMS increases its pay-for-performance initiatives, many hospitals and clinics are changing health-care delivery mechanisms on the basis of the results of proprietary surveys, such as those created by Press Ganey.
Although patient satisfaction scores are increasingly used to make policy decisions, the factors that influence satisfaction are incompletely understood. Within the orthopaedic literature, relationships have been shown between satisfaction and age4, depression5, pain6, psychological distress7, and travel distance to the clinic4. Furthermore, outside orthopaedics, satisfaction has been linked to age8-11, sex8, race10,11, education level12, insurance status13, employment status14, and other factors not directly related to the care provided.
The purpose of this study was to test the null hypotheses that antecedent levels of patient-reported physical function, pain, and anxiety are not associated with patient satisfaction, as measured by the Press Ganey Medical Practice (PGMP) survey.
Materials and Methods
This was a cohort study including all patients ≥18 years of age who presented to the hand and upper-extremity (non-shoulder) clinic at a single academic orthopaedic center between January 1, 2014, and December 31, 2016. This study received approval from the institutional review board at our institution.
As a part of the standard care in our hand clinics, on the same day and immediately prior to the clinic encounter with the provider, patients used tablet computers to complete the abbreviated version of the Disabilities of the Arm, Shoulder and Hand scale (QuickDASH) and the computer adaptive test (CAT) versions of the PROMIS Physical Function, PROMIS Upper Extremity, PROMIS Anxiety, and PROMIS Pain Interference metrics. Subsequent to their clinic visit, all patients with a valid e-mail address were sent a link to the PGMP survey.
All patients who completed at least 1 patient-reported outcome measure and the PGMP survey were included in this study. If a study participant had multiple clinic visits, only the first visit was used for analysis. Both the patient-reported outcome data and the Press Ganey data were linked to the patient medical record. Patient demographic characteristics (age, sex, race, insurance, and visit type) were recorded.
The PGMP survey for outpatients consisted of 27 questions divided into 7 subdomains: Access, Moving Through Your Visit, Nurse/Assistant, Care Provider, Laboratory Tests, Personal Issues, and Overall Assessment. The 2 questions relating to laboratory tests were omitted from this study. Each question measures responses on a scale from 0 (very poor) to 100 (very good). Scores for each of the 6 subdomains are calculated by averaging the items within each subdomain, and the overall score is calculated by averaging the 6 subdomain scores. Thus, individual items, subdomains, and the overall score range from 0 to 100 points, in which 100 indicates perfect satisfaction. The PGMP survey scoring instructions document is available by contacting Press Ganey3.
Patients were categorized as less satisfied if their overall score was in the bottom 33rd percentile of included patients, and those with overall scores above this were categorized as more satisfied. This threshold was chosen a priori, using methodology similar to that used in a prior study, and corresponds to an overall score of 87.9 points4. Satisfaction with the care provider was defined as a score of 100 points using the Care Provider (CP) subscale of the PGMP survey.
Each of the 4 PROMIS CATs used in this study measures a specific dimension of a patient’s physical health (Physical Function, Upper Extremity) or psychological health (Anxiety, Pain Interference). Like the QuickDASH, answers range from 1 to 5 and are converted to a 100-point scale. However, rather than being a fixed length, each CAT is completed when the expected change in the score with additional answered questions drops below a predetermined threshold for accuracy. For the Physical Function and Upper Extremity CATs, higher scores indicate better function. Higher scores indicate greater anxiety for the Anxiety CAT and greater pain for the Pain Interference CAT.
The QuickDASH is a well-described, 11-question survey that asks about a patient’s symptoms and his or her ability to perform certain tasks, in which a score of 0 represents no disability and a score of 100 represents the maximum disability measurable by this metric15.
Logistic regression was used to compare each of the 5 measures of patient-reported function and psychological distress with overall satisfaction (defined a priori as a Press Ganey score above the 33rd percentile) and satisfaction with the care provider (defined a priori as a score of 100 using the CP subscale of the PGMP survey).
Odds ratios (ORs), 95% confidence intervals (CIs), and p values were reported for 10-point increases in the PROMIS and QuickDASH scores, which correspond to a 1-standard-deviation increase on the PROMIS instruments. Patient age and care provider were included as covariates in all models, and each model was run for all patients across all clinical visit types. We controlled for care provider because it was an attribute of our study design and patient age because we found it to be associated with satisfaction in our previous research4. As a sensitivity analysis, we re-ran the regression model for overall satisfaction, treating it as continuous, transforming it as 100 − Y, applying a negative binomial outcome model, and adjusting for sex and race in addition to patient age and surgeon. Similarly, the models were repeated in the subset of new-patient and return-patient visits. Significance was assessed at p ≤ 0.05, and all tests were 2-sided. Statistical analysis was conducted using R version 3.3.0 (R Foundation for Statistical Computing)16.
Results
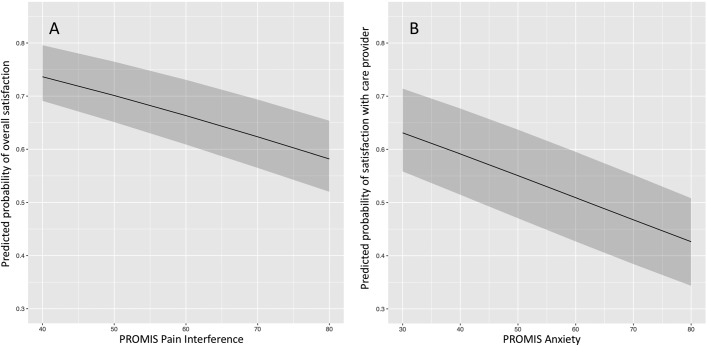
During the study period, 1,160 unique patient visits met the inclusion criteria, of which 661 were new patient visits and 499 were return patient visits. Details with regard to the demographic information of the respondents and the functional, psychological, and satisfaction scores are shown in Table I. The distribution of the overall Press Ganey scores of the study participants is shown as a histogram in Figure 1.
Fig. 1.
Histogram showing the distribution of overall Press Ganey scores in the study population.
TABLE I.
Descriptive Summary of Patient Characteristics*
| Variable | All (N = 1,160) | New (N = 661) | Return (N = 499) |
| Age (yr) | |||
| Mean and standard deviation | 53.1 ± 15.2 | 53.0 ± 15.2 | 53.2 ± 15.3 |
| Median (interquartile range) | 56 (41, 65) | 55 (40, 65) | 57 (43, 64) |
| Range | 18 to 84 | 18 to 83 | 18 to 84 |
| Male sex | 446 (38%) | 251 (38%) | 195 (39%) |
| Race | |||
| White | 1,057 (91%) | 598 (90%) | 459 (92%) |
| Black | 5 (0%) | 2 (0%) | 3 (1%) |
| Other | 78 (7%) | 47 (7%) | 31 (6%) |
| Hispanic or Latino ethnicity | 58 (5%) | 35 (5%) | 23 (5%) |
| PROMIS Anxiety CAT | |||
| Mean and standard deviation | 50.5 ± 9.4 | 50.8 ± 9.3 | 49.9 ± 9.4 |
| Median (interquartile range) | 51 (46, 56) | 51 (46, 56) | 51 (44, 56) |
| Range | 33 to 85 | 33 to 78 | 33 to 85 |
| PROMIS Pain Interference CAT | |||
| Mean and standard deviation | 56.4 ± 7.8 | 56.7 ± 7.8 | 55.9 ± 7.8 |
| Median (interquartile range) | 56 (53, 62) | 56 (53, 62) | 56 (53, 61) |
| Range | 39 to 81 | 39 to 80 | 39 to 81 |
| PROMIS Physical Function CAT | |||
| Mean and standard deviation | 46.8 ± 9.4 | 46.8 ± 9.1 | 46.7 ± 9.6 |
| Median (interquartile range) | 48 (40, 53) | 48 (40, 53) | 48 (40, 53) |
| Range | 15 to 73 | 15 to 73 | 23 to 73 |
| PROMIS Upper Extremity CAT | |||
| Mean and standard deviation | 37.3 ± 10 | 38.1 ± 10.2 | 36.5 ± 9.6 |
| Median (interquartile range) | 37 (30, 42) | 37 (31, 44) | 36 (30, 41) |
| Range | 15 to 56 | 15 to 56 | 15 to 56 |
| QuickDASH | |||
| Mean and standard deviation | 36.5 ± 22.3 | 36.2 ± 22.4 | 36.8 ± 22.3 |
| Median (interquartile range) | 34 (18, 52) | 34 (18, 51) | 34 (20, 52) |
| Range | 0 to 98 | 0 to 98 | 0 to 93 |
| Press Ganey survey raw score | |||
| Mean and standard deviation | 89.3 ± 13.5 | 88.3 ± 14.6 | 90.6 ± 11.9 |
| Median (interquartile range) | 94.8 (83.1, 100.0) | 94.2 (81.2, 100.0) | 95.4 (85.4, 100.0) |
| Range | 12.9 to 100.0 | 12.9 to 100.0 | 35.4 to 100.0 |
| Overall satisfaction | 780 (67%) | 430 (65%) | 350 (70%) |
| Satisfaction with care provider | 634 (55%) | 341 (52%) | 293 (59%) |
There were missing values for the following: 20 for race (14 new visits and 6 return visits); 29 for ethnicity; 44 for PROMIS Anxiety CAT, PROMIS Pain Interference CAT, and PROMIS Physical Function CAT; 430 for PROMIS Upper Extremity CAT; 104 for QuickDASH; and 4 for satisfaction with care provider.
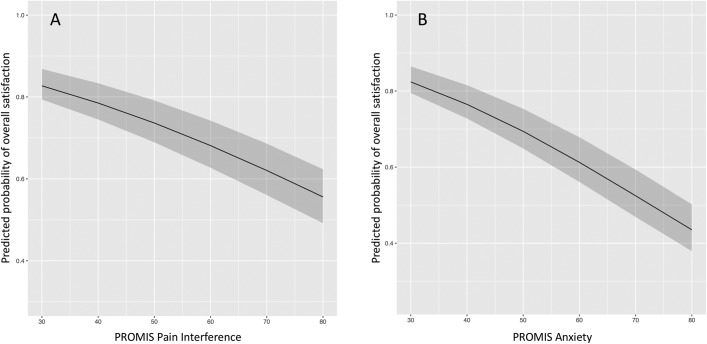
Table II shows the results of the logistic regression models comparing the pre-visit patient-reported outcome metrics with overall satisfaction and with satisfaction with the care provider for all visit types. For every 10-point increase in PROMIS Pain Interference (more self-reported pain interference), there was a 17% decrease in the odds of overall satisfaction (OR, 0.83 [95% CI, 0.71 to 0.98]; p = 0.03). Similarly, there was an association between anxiety and patient satisfaction with their care provider, whereby a 10-point increase in PROMIS Anxiety (higher self-reported anxiety) was associated with a 16% decrease in the odds of perfect satisfaction with the care provider (OR, 0.84 [95% CI, 0.72 to 0.97]; p = 0.02). The relationship between overall satisfaction and PROMIS Pain Interference is shown in Figure 2-A. The relationship between satisfaction with the care provider and PROMIS Anxiety is shown in Figure 2-B. None of the physical function measures were associated with overall satisfaction or satisfaction with the care provider.
Fig. 2.
Predicted probability (solid lines) with 95% CIs (shaded areas) of patient satisfaction based on pre-visit patient-reported outcome score, in all patients (visit types). Fig. 2-A PROMIS Pain Interference compared with overall satisfaction. Fig. 2-B PROMIS Anxiety compared with satisfaction with care provider.
TABLE II.
Association Between Patient-Reported Outcome Measures and Satisfaction in All Patients
| Satisfaction Measure | Outcome Measure | OR* | P Value |
| Overall satisfaction | PROMIS Physical Function CAT | 1.12 (0.98 to 1.28) | 0.10 |
| PROMIS Upper Extremity CAT | 1.04 (0.89 to 1.22) | 0.62 | |
| QuickDASH | 0.99 (0.93 to 1.05) | 0.75 | |
| PROMIS Anxiety CAT | 0.87 (0.74 to 1.02) | 0.09 | |
| PROMIS Pain Interference CAT | 0.83 (0.71 to 0.98) | 0.03 | |
| Satisfaction with surgeon (care provider) | PROMIS Physical Function CAT | 1.09 (0.96 to 1.24) | 0.20 |
| PROMIS Upper Extremity CAT | 1.00 (0.86 to 1.17) | 0.95 | |
| QuickDASH | 0.99 (0.93 to 1.04) | 0.62 | |
| PROMIS Anxiety CAT | 0.84 (0.72 to 0.97) | 0.02 | |
| PROMIS Pain Interference CAT | 0.93 (0.79 to 1.09) | 0.36 |
The values are given as the OR, with the 95% CI in parentheses; these were for every 10-point increase in the outcome measure. The ORs were from the univariate logistic regression model comparing each patient-reported outcome measure with the Press Ganey overall patient satisfaction and with the Care Provider (CP) subdomain of the Press Ganey survey, in all patient visit types. For the PROMIS Physical Function and Upper Extremity CATs, a higher score indicates more function. For the QuickDASH and PROMIS Anxiety and Pain Interference CATs, a higher score indicates more disability (QuickDASH), more anxiety, or more pain interference.
Among new patients only, Table III shows the results of the logistic regression models comparing the pre-visit patient-reported outcome metrics with overall satisfaction and with satisfaction with the care provider. A significant positive association was found between higher levels of physical function and patient satisfaction, whereby a 10-point increase in the PROMIS Physical Function score increased the odds of reporting satisfaction with the care provider by 22% (OR, 1.22 [95% CI, 1.02 to 1.47]; p = 0.03). The relationship between satisfaction with the care provider and PROMIS Physical Function is shown in Figure 3. Among new patients, neither pain interference nor anxiety were associated with overall satisfaction or satisfaction with the care provider.
Fig. 3.
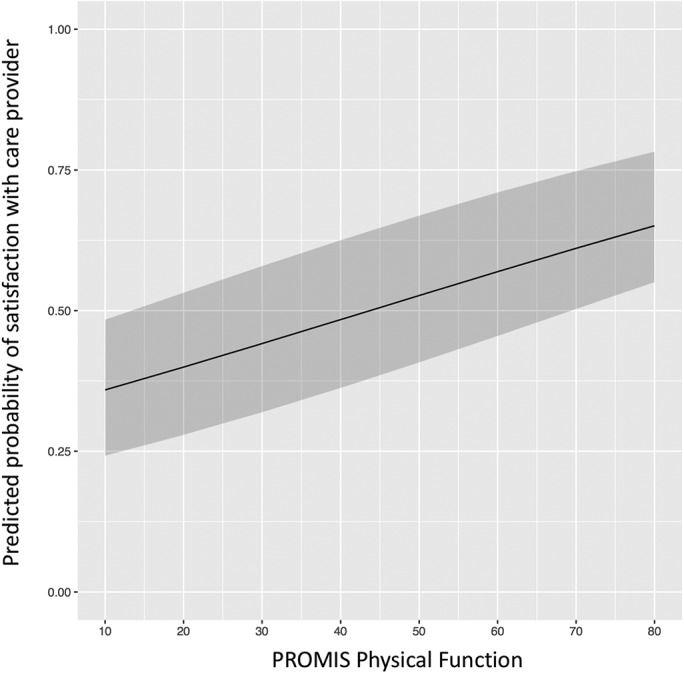
Predicted probability (solid line) with 95% CI (shaded area) of patient satisfaction based on pre-visit PROMIS Physical Function score, in new patients only.
TABLE III.
Association Between Patient-Reported Outcome Measures and Satisfaction in New Patient Visits
| Satisfaction Measure | Outcome Measure | OR* | P Value |
| Overall satisfaction | PROMIS Physical Function CAT | 1.18 (0.98 to 1.42) | 0.07 |
| PROMIS Upper Extremity CAT | 0.91 (0.74 to 1.13) | 0.39 | |
| QuickDASH | 1.02 (0.95 to 1.10) | 0.60 | |
| PROMIS Anxiety CAT | 1.01 (0.83 to 1.23) | 0.94 | |
| PROMIS Pain Interference CAT | 0.92 (0.74 to 1.14) | 0.45 | |
| Satisfaction with surgeon (care provider) | PROMIS Physical Function CAT | 1.22 (1.02 to 1.47) | 0.03 |
| PROMIS Upper Extremity CAT | 0.98 (0.80 to 1.21) | 0.86 | |
| QuickDASH | 0.97 (0.90 to 1.04) | 0.39 | |
| PROMIS Anxiety CAT | 0.84 (0.69 to 1.02) | 0.08 | |
| PROMIS Pain Interference CAT | 0.88 (0.71 to 1.09) | 0.23 |
The values are given as the OR, with the 95% CI in parentheses; these were for every 10-point increase in the outcome measure. The ORs were from the univariate logistic regression model comparing each patient-reported outcome measure with the Press Ganey overall patient satisfaction and with the Press Ganey Care Provider (CP) subdomain in new patient visits only. For the PROMIS Physical Function and Upper Extremity CATs, a higher score indicates more function. For the QuickDASH and PROMIS Anxiety and Pain Interference CATs, a higher score indicates more disability (QuickDASH), more anxiety, or more pain interference.
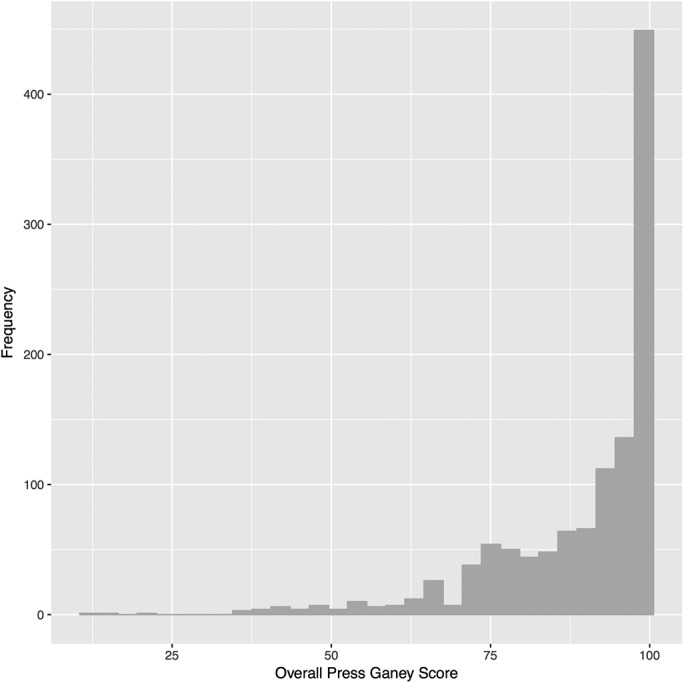
Among return patients only, Table IV shows the results of logistic regression models comparing the pre-visit patient-reported outcome metrics with overall satisfaction and with satisfaction with the care provider. There was a negative association of both pain interference (OR, 0.76 [95% CI, 0.58 to 0.98]; p = 0.04) and anxiety (OR, 0.69 [95% CI, 0.53 to 0.89]; p < 0.01) with overall patient satisfaction. These relationships between overall satisfaction and PROMIS Pain Interference and Anxiety are shown in Figures 4-A and 4-B. The sensitivity analysis for overall satisfaction demonstrated consistent results (data not shown).
Fig. 4.
Predicted probability (solid lines) with 95% CIs (shaded areas) of patient satisfaction based on pre-visit patient-reported outcome score, in return patients only. Fig. 4-A PROMIS Pain Interference. Fig. 4-B PROMIS Anxiety.
TABLE IV.
Association Between Patient-Reported Outcome Measures and Satisfaction in Return Patient Visits
| Satisfaction Measure | Outcome Measure | OR* | P Value |
| Overall satisfaction | PROMIS Physical Function CAT | 1.05 (0.85 to 1.29) | 0.66 |
| PROMIS Upper Extremity CAT | 1.26 (0.97 to 1.64) | 0.09 | |
| QuickDASH | 0.95 (0.87 to 1.04) | 0.27 | |
| PROMIS Anxiety CAT | 0.69 (0.53 to 0.89) | <0.01 | |
| PROMIS Pain Interference CAT | 0.76 (0.58 to 0.98) | 0.04 | |
| Satisfaction with surgeon (care provider) | PROMIS Physical Function CAT | 0.95 (0.79 to 1.16) | 0.63 |
| PROMIS Upper Extremity CAT | 1.03 (0.81 to 1.31) | 0.81 | |
| QuickDASH | 1.01 (0.93 to 1.10) | 0.83 | |
| PROMIS Anxiety CAT | 0.86 (0.67 to 1.09) | 0.20 | |
| PROMIS Pain Interference CAT | 1.05 (0.82 to 1.33) | 0.71 |
The values are given as the OR, with the 95% CI in parentheses; these were for every 10-point increase in the outcome measure. The ORs were from univariate logistic regression model comparing each patient-reported outcome measure with the Press Ganey overall patient satisfaction and with the Press Ganey Care Provider (CP) subdomain in return patient visits only. For the PROMIS Physical Function and Upper Extremity CATs, a higher score indicates more function. For the QuickDASH, PROMIS Anxiety and Pain Interference CAT, a higher score indicates more disability (QuickDASH), more anxiety, or more pain interference.
Discussion
The main finding of this study is that antecedent levels of patient-reported physical function, pain interference, and anxiety are associated with the PGMP score of patient satisfaction in a hand clinic patient population. Among all visit types, patient satisfaction was lower in patients with more self-reported pain as measured by the PROMIS Pain Interference metric and more self-reported anxiety as measured by the PROMIS Anxiety metric. Among new patients presenting to a hand and upper-extremity clinic, lower self-reported physical function was associated with lower satisfaction with their care provider. In our model, this effect was relatively large, whereby a 10-point increase (more function) in the PROMIS Physical Function CAT score was associated, on average, with a 22% increase in the likelihood of a patient being satisfied. Similarly, among return patient visits, patient satisfaction was lower in patients exhibiting increased pain interference and anxiety.
This study is in concert with prior investigations that have demonstrated associations of patient demographic characteristics, function measures, psychological distress measures, with patient satisfaction. Within the hand patient population, Lozano Calderón et al. demonstrated that decreased function correlated with less satisfaction. However, in contrast to the present study, pain was not associated with satisfaction5. Vranceanu and Ring found an association of psychological factors such as depression and catastrophizing with satisfaction in hand patients17. In a recent literature review, Marks et al. found that pain was the factor most highly correlated with satisfaction after hand surgery18.
These relationships of demographic and psychosocial characteristics with patient satisfaction are found in other orthopaedic subspecialties, as well as other medical specialties. For example, in studying spine patients, Abtahi et al. showed an association between psychological distress and patient satisfaction7. In the arthroplasty literature, Bourne et al. found that preoperative pain was significantly associated with dissatisfaction after primary total knee arthroplasty19. In a prospective study of 491 patients who had undergone a foot or ankle surgical procedure, Dawson et al. found that pain significantly influenced satisfaction20. Beyond orthopaedics, prior studies have shown that age, ethnicity, education level, and employment status can be associated with patient satisfaction8-14.
This study had several limitations. It was performed in a hand and upper-extremity clinic at a single academic center, and therefore its conclusions may not be generalizable to all populations. Most importantly, each patient was only assessed once for both the functional and psychological measures and the patient satisfaction score. No comments or conclusions can or should therefore be made regarding the interplay between treatment, clinical outcome, satisfaction, pain, and anxiety with regard to the return patient visits included in this study. This reflects the current framework within which the Press Ganey survey assesses and reports patient satisfaction to subscribing institutions (i.e., the survey does not attempt or claim to assess satisfaction with clinical outcome). More specifically, it is not possible to draw conclusions with regard to the effect of treatment in this manner.
Both the assessment and definition of patient satisfaction in the peer-reviewed literature vary widely. In this study, we utilized the PGMP survey and its care provider subdomain to assess patient satisfaction and employed definitions of patient satisfaction based on prior peer-reviewed literature. Use of the Press Ganey survey is highly prevalent in the United States and likely adds to the strength of this study, yet we urge caution when comparing study results when the methods by which patient satisfaction has been assessed and/or defined differ. Illustrating this difficulty, a strict numerical definition or cut-point that identifies patients as unsatisfied or satisfied using the Press Ganey survey is difficult to ascertain and remains open to debate. In this study, for example, a threshold of the 33rd percentile of the study population was utilized a priori to define satisfaction based on a peer-reviewed precedent4. Still, given the potential for a Type-I error inherent to multiple hypothesis testing and the lack of current consensus with regard to thresholds for defining patient satisfaction in particular with regard to the Press Ganey survey, we urge careful consideration of such thresholds when interpreting and designing studies in this arena.
It is especially critical to note that this study did not assess patient satisfaction with any outcome of the treatment provided, nor does the Press Ganey survey address this related but distinct concept.
In addition, the low response rate and responder bias seen with patient satisfaction surveys should be considered a limitation of this study and are additional concerns, broadly, when interpreting patient satisfaction scores21. Accounting for such non-response bias, if present, may provide a more comprehensive assessment and understanding of the interactions of physical and mental health with patient satisfaction. Currently, this does not appear to be a component of the reporting of the Press Ganey survey results provided to institutions for utilization. Although patient satisfaction survey data are by their very nature incomplete and censored because of non-response bias, they are commonly being used and interpreted without regard for these considerations. In this light, we consider the current observational study design reflective of the current use of broad-based satisfaction survey data in the United States.
Furthermore, this study did not comprehensively evaluate each patient’s psychological state, and we limited the psychological assessment to 2 metrics involving pain interference and anxiety. Although the PROMIS metrics utilized are valid measures of these psychological domains, there are various methods that can be employed to assess patient pain, anxiety, self-efficacy, catastrophizing, social support, and other psychological characteristics to gain a deeper understanding of the relationship of patient satisfaction to such measures.
Despite controversy, patient satisfaction is increasingly used as a metric to evaluate quality and value within the U.S. health-care system. The routine measurement of patients’ satisfaction with their care has become more ubiquitous as legislative changes to reimbursement models take effect. In turn, health-care provider rating systems also likely reflect the changing expectations of our patients, who are increasingly more informed and engaged participants in the modern health-care marketplace. As these data become more available, the judicious application of patient satisfaction metrics to inform policy decisions can be a complex endeavor. This is especially true in light of the fact that patient satisfaction can be influenced by variables unrelated to the quality of medical care provided.
Finally, this study builds upon other work and further supports the assertion that the biopsychosocial model of health is pertinent to orthopaedic surgery22. The biopsychosocial model was originally introduced by psychiatrist George Engel in 197723. Rooted in medical anthropology, this model postulates that the effect that a disease state has on a patient is determined by more than just biological factors and that, in particular, psychological and social factors have strong influences on health24.
An appreciation of the multifaceted interplay between these biological, psychological, and social elements is essential if we are to help patients to improve their health outcomes as well as satisfaction with the care provided. Moreover, orthopaedic surgeons must recognize that patient satisfaction is being used to assess the quality of care that we provide, despite the complexity surrounding its appropriate application. Systematic efforts to improve patient satisfaction may be informed by the identification of patients less likely to be satisfied with the care they have received. As this study highlights, a more complete understanding of the factors that affect patient satisfaction is needed to accurately assess health-care quality and value.
Footnotes
Investigation performed at the Department of Orthopaedics and the Division of Epidemiology, Department of Internal Medicine, University of Utah, Salt Lake City, Utah
Disclosure: This investigation was supported by the University of Utah Study Design and Biostatistics Center. Funding was partly provided by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764). The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/E937).
References
- 1.Gershon R, Rothrock NE, Hanrahan RT, Jansky LJ, Harniss M, Riley W. The development of a clinical outcomes survey research application: Assessment Center. Qual Life Res. 2010. June;19(5):677-85. Epub 2010 Mar 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Graham B, Green A, James M, Katz J, Swiontkowski M. Measuring patient satisfaction in orthopaedic surgery. J Bone Joint Surg Am. 2015. January 7;97(1):80-4. [DOI] [PubMed] [Google Scholar]
- 3.Press Ganey. Census-based surveying (medical practice/ambulatory). 2016. http://www.pressganey.com/solutions/patient-experience/census-based-surveying/census-based-surveying-medical-practice_ambulatory. Accessed 2018 Aug 7.
- 4.Abtahi AM, Presson AP, Zhang C, Saltzman CL, Tyser AR. Association between orthopaedic outpatient satisfaction and non-modifiable patient factors. J Bone Joint Surg Am. 2015. July 1;97(13):1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lozano Calderón SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg Am. 2008. March;33(3):303-7. [DOI] [PubMed] [Google Scholar]
- 6.Vranceanu AM, Jupiter JB, Mudgal CS, Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010. June;35(6):956-60. Epub 2010 Apr 9. [DOI] [PubMed] [Google Scholar]
- 7.Abtahi AM, Brodke DS, Lawrence BD, Zhang C, Spiker WR. Association between patient-reported measures of psychological distress and patient satisfaction scores after spine surgery. J Bone Joint Surg Am. 2015. May 20;97(10):824-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen Thi PL, Briançon S, Empereur F, Guillemin F. Factors determining inpatient satisfaction with care. Soc Sci Med. 2002. February;54(4):493-504. [DOI] [PubMed] [Google Scholar]
- 9.Rogers F, Horst M, To T, Rogers A, Edavettal M, Wu D, Anderson J, Lee J, Osler T, Brosey L. Factors associated with patient satisfaction scores for physician care in trauma patients. J Trauma Acute Care Surg. 2013. July;75(1):110-4; discussion 114–5. [DOI] [PubMed] [Google Scholar]
- 10.Sun BC, Adams J, Orav EJ, Rucker DW, Brennan TA, Burstin HR. Determinants of patient satisfaction and willingness to return with emergency care. Ann Emerg Med. 2000. May;35(5):426-34. [PubMed] [Google Scholar]
- 11.Young GJ, Meterko M, Desai KR. Patient satisfaction with hospital care: effects of demographic and institutional characteristics. Med Care. 2000. March;38(3):325-34. [DOI] [PubMed] [Google Scholar]
- 12.Rahmqvist M, Bara AC. Patient characteristics and quality dimensions related to patient satisfaction. Int J Qual Health Care. 2010. April;22(2):86-92. Epub 2010 Feb 3. [DOI] [PubMed] [Google Scholar]
- 13.Boudreaux ED, Ary RD, Mandry CV, McCabe B. Determinants of patient satisfaction in a large, municipal ED: the role of demographic variables, visit characteristics, and patient perceptions. Am J Emerg Med. 2000. July;18(4):394-400. [DOI] [PubMed] [Google Scholar]
- 14.Harris I, Dao AT, Young J, Solomon M, Jalaludin BB, Rae H. Factors predicting patient satisfaction following major trauma. Injury. 2007. September;38(9):1102-8. Epub 2007 Aug 13. [DOI] [PubMed] [Google Scholar]
- 15.Gummesson C, Ward MM, Atroshi I. The shortened Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006. May 18;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.R Foundation for Statistical Computing. R: a language and environment for statistical computing. 2016. https://www.R-project.org/. Accessed 2018 Aug 7.
- 17.Vranceanu AM, Ring D. Factors associated with patient satisfaction. J Hand Surg Am. 2011. September;36(9):1504-8. Epub 2011 Jul 27. [DOI] [PubMed] [Google Scholar]
- 18.Marks M, Herren DB, Vliet Vlieland TP, Simmen BR, Angst F, Goldhahn J. Determinants of patient satisfaction after orthopedic interventions to the hand: a review of the literature. J Hand Ther. 2011. Oct-Dec;24(4):303-12.e10; quiz 312. Epub 2011 Jun 17. [DOI] [PubMed] [Google Scholar]
- 19.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010. January;468(1):57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dawson J, Boller I, Doll H, Lavis G, Sharp RJ, Cooke P, Jenkinson C. Factors associated with patient satisfaction with foot and ankle surgery in a large prospective study. Foot (Edinb). 2012. September;22(3):211-8. Epub 2012 Jun 6. [DOI] [PubMed] [Google Scholar]
- 21.Presson AP, Zhang C, Abtahi AM, Kean J, Hung M, Tyser AR. Psychometric properties of the Press Ganey® outpatient medical practice survey. Health Qual Life Outcomes. 2017. February 10;15(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayers DC, Franklin PD, Ring DC. The role of emotional health in functional outcomes after orthopaedic surgery: extending the biopsychosocial model to orthopaedics: AOA critical issues. J Bone Joint Surg Am. 2013. November 6;95(21):e165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977. April 8;196(4286):129-36. [DOI] [PubMed] [Google Scholar]
- 24.Vranceanu AM, Ring D. Value of psychological evaluation of the hand surgical patient. J Hand Surg Am. 2008. Jul-Aug;33(6):985-7. [DOI] [PubMed] [Google Scholar]