Supplemental Digital Content is available in the text
Keywords: Endometrial cancer, Endometrial hyperplasia, Menopause, Vaginal estrogen
Abstract
Objective:
The aim of the study was to systematically review studies that evaluated endometrial hyperplasia or cancer incidence with unopposed vaginal estrogens.
Methods:
PubMed and EMBASE were searched from inception to August 2017 for relevant articles and abstracts. Bibliographies of review articles and abstracts of major women's health medical meetings were examined. Eligible studies (independently reviewed by 4 authors) had to report menopausal vaginal estrogen use and endometrial histology, or incidence of endometrial hyperplasia or cancer.
Results:
Of 5,593 abstracts from the literature search and 47 articles from other sources, 36 articles and 2 abstracts were eligible, describing 20 randomized controlled studies, 8 interventional studies, and 10 observational studies. Collectively, the studies did not support an increased risk of endometrial hyperplasia or cancer with low-dose vaginal estrogens. Rates of endometrial cancer and hyperplasia were 0.03% and 0.4%, respectively, from 20 randomized controlled trials (2,983 women) of vaginal estrogens. Overall, reports of endometrial hyperplasia were observed with various doses and durations and appeared sporadic (except 1.25 mg conjugated equine estrogens), consistent with endometrial hyperplasia rates in the general population. A Denmark registry study was an exception and may be of limited applicability to the United States. The Women's Health Initiative Observational Study showed no association (1.3 cases/1,000 women-years with vaginal estrogens versus 1.0/1,000 women-years for nonuse).
Conclusion:
This systematic review supports the use of low-dose vaginal estrogens for treating vulvar and vaginal atrophy in menopausal women without a concomitant progestogen. This review does not support increased endometrial hyperplasia or cancer risk with low-dose, unopposed vaginal estrogens; however, longer-term, real-world data are needed.
More than two million women in the United States are estimated to use vaginal estrogen products to treat symptomatic vulvar and vaginal atrophy.1-3 Because most women do not use vaginal estrogens with concomitant progestogen, examination of the impact of unopposed vaginal estrogens on the endometrium is an important safety parameter. Although it may be well accepted that local unopposed vaginal estrogens do not have the same stimulatory effects on the endometrium as unopposed oral estrogens, a lesser association between vaginal estrogen use and endometrial hyperplasia or cancer has not been systemically reviewed in published studies. A systematic review of the published clinical evidence to examine the endometrial safety of vaginal estrogens would enhance future development of novel, safe, and effective, low-dose vaginal estrogen products. The objective of this systematic review was to assess the endometrial safety of low-dose vaginal estrogens in menopausal women in the published medical literature.
METHODS
Literature search methodology
The concept of this review was based on a request from the US Food and Drug Administration to research and review the risk of endometrial hyperplasia or cancer with the use of vaginal estrogens. A systematic search of PubMed, EMBASE, and Clinicaltrials.gov was conducted from inception to August 2017 for journal articles, conference abstracts, and study data reporting any use of vaginal estrogens in menopausal women published in the English language. Keywords used for PubMed were vaginal and (estrogen or oestrogen or estradiol or oestradiol). Keywords used for EMBASE were (uterine or endometri∗) and (cancer or carcinoma or hyperplasia or proliferation) and vagin∗ and (estrogen(s) or estradiol) and (menopaus∗ or postmenopaus∗) excluding reviews and articles with rats, mouse, mice, and dogs in the title. A separate literature search of these databases was conducted for studies of vaginal dehydroepiandrosterone (DHEA; prasterone) in postmenopausal women using the keywords vaginal and prasterone.
Bibliographies of review articles were inspected for studies of vaginal estrogen use in menopausal women that may have not appeared in the literature search results. Review articles examined included those published in the last 10 years that focused on vaginal atrophy, vaginal estrogen use, or menopausal hormone therapy. Bibliographies of the most recent Cochrane reviews for vaginal estrogen use outcomes were also reviewed. Relevant articles were also included if mentioned in the Results and Discussion of relevant full text articles or when consulting with experts in the field.
The published abstracts of major medical meetings in women's health (The North American Menopause Society, the American College of Obstetricians and Gynecologists, and the International Menopause Society) were reviewed for relevant published abstracts from the previous 5 years. Abstracts from The North American Menopause Society and American College of Obstetricians and Gynecologists were searched in EMBASE using the keyword endometr∗, whereas the pdf files of abstracts from the International Menopause Society published in the Climacteric journal were manually searched. Any abstracts with reports of endometrial data in menopausal women using vaginal estrogens, for which the full article was not yet published, were included.
Clinicaltrials.gov was searched for studies of any vaginal estrogen use in menopausal women to determine if any completed studies were not published and/or had data posted on the clinicaltrials.gov Web site.
Inclusion criteria
Abstracts were independently reviewed by four reviewers (G.D.C., S.G., K.O., S.M.), who initially determined from the title/abstract if the article met eligibility criteria for full-text review, which included studies using vaginal estrogens in menopausal women for any reason (eg, vulvar and vaginal atrophy, urinary incontinence, pelvic organ prolapse, and recurrent urinary tract infections). Endometrial histology was required to identify cases of endometrial cancer or endometrial hyperplasia, except for larger cohort studies in which incidence rates were reported. Citations were included for full-text review if it was not stated or clear from the abstract if any endometrial histologic data were reported, including but not limited to endometrial cancer, hyperplasia, or proliferation.
From the full text review, primary studies were eligible for review if they reported endometrial histology data obtained from a biopsy in menopausal women using vaginal estrogens, or incidence of endometrial cancer and/or hyperplasia in menopausal women who used vaginal estrogens from larger cohort studies. Articles were excluded if they reported no use of vaginal estrogen, use of vaginal ring with a progestogen, exclusive use of estriol or other non-US-approved estrogen, no endometrial histology, or unrelated content. General reviews or editorials, abstracts of studies now fully published, or duplicate publications were also excluded. No studies reporting endometrial histology in women using vaginal estrogens were excluded.
Studies reporting endometrial cancer/histology data were summarized into tables by type of trial (randomized controlled trials [RCTs]; prospective, interventional studies; prospective observational studies; and retrospective observational/registry studies). In studies that use vaginal cream, the actual estrogen dose was provided in addition to vaginal cream weights for comparison purposes.
RESULTS
A total of 5,593 abstracts were identified from the literature search and 47 studies from other sources (not found in the literature searches); of these a total of 284 full text articles were reviewed (Fig. 1). Of the full-text articles and abstracts reviewed, 36 articles and 2 abstracts reported endometrial histology or endometrial cancer with use of vaginal estrogens in menopausal women and were included for critical review and interpretation. Twenty were RCTs,4-24 eight were prospective, interventional studies,25-32 two were prospective observational studies,33,34 and eight were retrospective observational studies.35-41
FIG. 1.
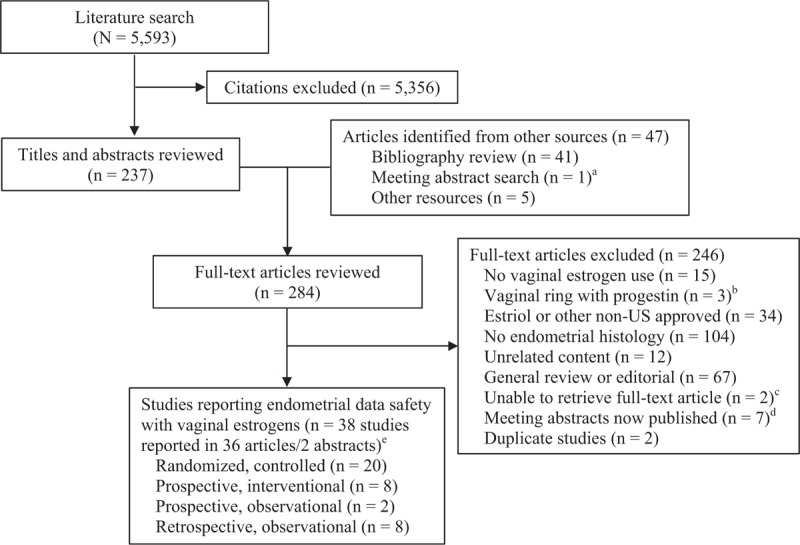
Identification, screening, and selection of articles reporting endometrial histology in menopausal women using vaginal estrogens. aMeeting abstracts from a search of major women's health meetings in the past 5 years for studies that were not found in the literature search results. bVaginal ring with progestin included studies of vaginal rings resulting in systemic levels of estrogen to treat vasomotor symptoms so that a progestin had to be given. cOne article was published in 1979 and did not mention endometrial data in the abstract, and the other was published in 1963 with no abstract available. dMeeting abstracts with a full publication, with no endometrial data, or not relevant. eDoes not include estriol studies; comparative studies with estriol were included, but only data for other vaginal estrogens were summarized.
The most common reason for study exclusion (Fig. 1) was no reported endometrial histology data (n = 104), followed by types of studies (ie, reviews/ editorials; n = 67), studies of estriol or other ex-US-approved estrogen (n = 34), and no vaginal estrogen use (n = 15). Two studies (reported in three articles) of a vaginal ring use that contained data on endometrial histology were excluded because the ring was developed to achieve systemic estradiol levels for the treatment of menopausal symptoms including hot flushes, and a progestin was included in the study to be given for 12 days of each 28-day cycle to prevent endometrial hyperplasia.42-44 Two studies could not be retrieved; one was published in 1979 and did not mention endometrial data in the abstract,45 and the other was published in 1963 and did not have an abstract available.46
Randomized controlled trials
Endometrial histology was reported in 20 RCTs (Table 1, Supplemental Table 1, Supplemental Digital Content 1) of menopausal women who used various doses and durations of vaginal estrogen creams, tablets, inserts, or rings (multiple products were used in some studies). From a total of 2,983 unique women exposed to vaginal estrogen products for up to 1 year (66 women were exposed to multiple doses), 1 case of endometrial cancer (0.03%) and 12 cases of hyperplasia (0.4%; including a case of hyperplasia in an endometrial polyp) were detected.
TABLE 1.
Clinical trials (n = 37) that evaluated endometrial histology with vaginal estrogen use in menopausal women
| Study type | Type of vaginal estrogen/dose | Total number of women | Study duration | Total endometrial hyperplasia or cancer cases |
| RCT 20 trials4-24 | CEE or SCE-A creams 0.3-1.25 mg | 1,064 in 8 studies4-11 | 2-52 wks | Simple (n = 1) and complex (n = 1) hyperplasia with 1.25 mg CEE at 24 wk4Simple hyperplasia (n = 2) with 0.625 mg CEE at 2 wk11No EC or hyperplasia with SCE-A |
| Estrogen tablets25-50 μg | 490 in 8 studies4,8,12-17 | 3-52 wks | Simple hyperplasia without atypia with 25 μg at 3 wk (n = 2)13 and 12 wk (n = 1)12 No EC or hyperplasia at 52 wk | |
| Estrogen tablets10 μg | 297 in 2 studies12,18,19 | 12 wk; 52 wk | Complex hyperplasia (n = 1) occurring after 9 days of exposure18Single Gr 2, stage 1B endometrioid adenocarcinoma after 324 days of exposure18,19 | |
| Estrogen softgel inserts4, 10, 25 μg | 572 in 1 study20 | 12 wk | No EC or hyperplasia at 12 wk | |
| Estrogen rings (estradiol and estriol)7.5-400 μg/day | 626 in 6 studies7,16,21-24 | 12-48 wk | Hyperplasia with atypia (n = 3; 2 with estriol rings) at 12 wk21Endometrial polyp with hyperplasia (n = 1) at 12 wk with estradiol ring7 | |
| Prospective interventional8 trials25-32 | CEE or estradiol creams0.3-0.625 mg/day (CEE)10 μg/g (estradiol) | 32 in 3 studies25-27 | 12 wk–24 mo | No EC or hyperplasia |
| Estrogen tablet/ovules10-50 μg/day | 729 in 5 studies28-32 | 3-52 wk | No ECSimple glandular hyperplasia (n = 2) with 25 μg at 6 mos28Cystic hyperplasia (n = 1) with 25 μg at 6 mo28Possible hyperplasia in a polyp with 10 μg at 52 wk,30 reported as a case of complex hyperplasia without atypia in the Vagifem prescribing information47 | |
| Prospective observational2 trials33,34 | Estrogen cream, 25 μg estradiol tablets | 45,663 women33and 8,170 women-years34 | Median follow-up, 7.2 years (WHI Study) | Endometrial cancer incidence (VE use vs nonuse):1.3-1.7 vs 1.0-2.0/1,000 women-years33,34Endometrial cancer risk (VE use vs nonuse):HR: 1.47 (95% CI, 0.75-2.90); WHI study33 |
| Retrospective observational8 trials (in 7 articles)35-41 | Cream, tablets, or rings | ∼1.5 Million | 1-29 yr | Endometrial hyperplasia/cancer incidence (VE use vs nonuse): 9.96-10.25 vs 9.96/10,000 women-years36 1.3% vs 1.2%37 7%-9% vs 8-10%40Endometrial cancer risk (VE use vs nonuse): OR: 1.11 (95% CI, 0.47-2.65); US study37 RR: 1.96 (95% CI, 1.77-2.17); Danish study35 OR: 1.4 (95% CI, 1.0-2.0); Swedish study; 93% of women treated with estriol/dienestrol 38 Older US studies (use of higher VE doses) OR: 2.30 (95% CI, 1.1-4.6)39 OR: 0.90 (95% CI, 0.29-4.28)40 OR: 0.82 (95% CI, 0.46-3.20)40 RR: 0.7 (95% CI, 0.1-3.6)41 |
CI, confidence interval; CEE, conjugated equine estrogen; EC, endometrial cancer; HR, hazard ratio; OR, odds ratio; RR, risk ratio; SCE-A, synthetic conjugated estrogens-A; RCT, randomized controlled trial; VE, vaginal estrogen.
Conjugated equine estrogen creams
Vaginal conjugated equine estrogens (CEEs) cream or synthetic conjugated estrogens-A cream were evaluated in 1,064 women from eight RCTs, with doses ranging from 0.3 to 1.25 mg and with durations of 2 to 52 weeks.4-11
CEEs cream at 2 g (equivalent to 1.25 mg of CEE) were evaluated in a 24-week study in which women (n = 79) applied the vaginal cream daily for 21 days, and withheld treatment for 7 days.4 Of the 28 women with biopsies of sufficient tissue at 24 weeks, there were two cases (2/28; 7.1%) of endometrial hyperplasia: one (3.6%) woman had simple hyperplasia without atypia and one (3.6%) woman had complex hyperplasia without atypia; there were no endometrial cancers.
In other studies, no cases of endometrial hyperplasia or cancer were reported with daily 1.25 mg CEE cream for 3 weeks (n = 7),6 1.25 mg CEE cream three times per week for 12 weeks (n = 67),7 or 0.625 mg CEE cream daily for 2 weeks then twice weekly for 10 weeks (n = 26).8 In a 12-week study of synthetic conjugated estrogens-A 1.25 mg (n = 161) or 0.625 mg (n = 150) versus placebo, no cases of endometrial hyperplasia or cancer were reported.9
Two studies used 0.625 mg CEE cream in women before hysterectomy. In one study, women received the CEE cream daily for 2 weeks before hysterectomy (n = 150); two cases of simple hyperplasia (2/150; 1.3%) were identified.11 In a similar trial of 4 to 8 weeks duration of 0.625 mg CEE inserted vaginally (n = 8) for 2 weeks and then twice weekly before hysterectomy for vaginal wall prolapse, no cases of endometrial hyperplasia or cancer were reported.10
A 12-month RCT (n = 423) also evaluated a lower dose of 0.3 mg CEE cream administered twice weekly or once daily for 21 days and off for 7 days.5 No cases of endometrial hyperplasia or cancer were observed in the study.5
Estradiol tablets
Vaginal estradiol tablets, with doses ranging from 10 to 50 μg, were evaluated in 10 studies in 721 unique women with durations ranging from 3 weeks to 2 years.4,8,12-19 Of these, 66 women were exposed to multiple doses as part of crossover study designs in two RCTs.
Eight RCTs evaluated vaginal estradiol tablets at 25 μg4,8,12-17; one trial also included an estradiol vaginal tablet of 50 μg evaluated in 20 women.14 Out of a total of 490 women exposed to 25 μg for 3 to 52 weeks, there were three reports of endometrial hyperplasia, two cases after 3 weeks of treatment, and one after 12 weeks.12,13 There were no reports of endometrial hyperplasia or endometrial cancer in women exposed to 50 μg.14
One report of simple hyperplasia without atypia (1/32; 3.1%) was observed in a woman treated with a 25-μg vaginal estradiol tablet after 12 weeks of therapy; no other endometrial hyperplasia or malignancy was found at week 52.12 In a study of women who used a 25-μg vaginal estradiol tablet for 3 weeks before genital prolapse surgery without baseline biopsies, 2 of 22 (9.1%) women had “simple hyperplastic endometrium without epithelial atypia,” with normal atrophic endometrium observed 1 month later in both women.13
Studies with lower doses of vaginal estradiol were also reported. Two RCTs evaluated a vaginal 10-μg estradiol tablet in a total of 297 women for 12 to 52 weeks.12,18,19 The first study was of 12 weeks duration and no endometrial hyperplasia or cancer was observed for the vaginal estradiol tablet (10 μg; n = 92).12 The second study was a 52-week RCT (n = 205), which identified one case of endometrial cancer after 324 days of drug use and one case of complex endometrial hyperplasia without atypia after 9 days of drug use.18,19
Data from the 52-week RCT19 were pooled with the data from a separate, open-label, 52-week study30 (described below in the section on the prospective, interventional studies) to evaluate the incidence rate of endometrial hyperplasia and carcinoma.18 The combined incidence of endometrial cancer and hyperplasia in 541 women who used the 10-μg vaginal tablet was 0.52% (95% confidence interval [CI], 0.06%-1.86%).18
Estradiol softgel inserts
A 12-week, RCT evaluated 4, 10, and 25 μg of solubilized estradiol in softgel capsule. Of the 572 women treated, no cases of endometrial hyperplasia or cancer were observed for any of the doses.20
Estradiol rings
Vaginal estrogen rings, with doses ranging from 7.5 to 400 μg/day, were evaluated in a total of 626 women in 6 studies with durations ranging from 12 to 48 weeks.7,16,21-24 In a 6-month cross-over study of an estradiol vaginal ring (7.5 μg/day for 3 months) and vaginal estriol cream (0.5 mg), endometrial hyperplasia with atypia was found in one woman (1/82; 1.2%) who used the ring in the cream-ring sequence of the crossover and two women in the estriol cream group (2/82; 2.4%).21 Nachtigall7 also reported one woman (1/129) who had an endometrial polyp with hyperplasia after 12 weeks of using a vaginal estradiol ring releasing 7.5 μg/day.
Prospective interventional studies
Eight prospective interventional studies (Table 1 and Supplemental Table 2, Supplemental Digital Content 2) reported endometrial histology in 761 menopausal women who used vaginal estrogen creams (n = 3) or tablets/ovules (n = 5). Three studies evaluated vaginal CEE (0.3-0.625 mg per day) or estradiol (10 μg/g) cream in 32 women ranging in duration from 12 weeks to 24 months.25-27 An estradiol ovule (50 μg/day) was evaluated in nine women for 3 weeks; a 25-μg estradiol tablet in 384 women with durations ranging from 12 to 24 weeks; and a 10-μg estradiol tablet in 336 women for 52 weeks.28-32
No cases of endometrial cancer were reported in any of the prospective, interventional studies. Two cases (2/266; 0.75%) of simple glandular hyperplasia and one case (1/266; 0.38%) of cystic hyperplasia were reported following treatment with 25-μg estradiol tablets used for 6 months, although biopsies were not taken before the start of estrogen treatment.28
A 52-week, open-label study of the 10-μg estradiol tablet (n = 336) reported an estimated incidence of endometrial hyperplasia of 0 (95% CI, 0-0.011).30 For one woman, one pathologist scored the biopsy as a polyp of hyperplastic type while two other pathologists scored it as complex hyperplasia without atypia; a hysteroscopy performed after trial completion revealed a benign fibrous polyp with no sign of hyperplasia.30 In the prescribing information for the 10-μg estradiol tablet, this hyperplastic polyp was reported as a case of complex hyperplasia without atypia (1/297; 0.34%).47
Prospective observational studies
Two prospective observational studies reported endometrial histology or cancer in menopausal women who used vaginal estrogen products (Table 1 and Supplemental Table 3, Supplemental Digital Content 3).33,34,48 The first study was a cohort study (n = 45,663 analyzed women; n = 3,003 women with an intact uterus who took vaginal estrogens) with a 2-year median duration of estrogen use, as part of the Women's Health Initiative (WHI)-Observational Study (1993-2005) and Extension Study (2005-2010).33 Although the study did not specify the type of vaginal estrogen used, products available before 2010 in the United States were estradiol tablets containing 25-μg estradiol49 and creams dispensed with 0.3 to 1.25 mg CEE.50 In the WHI-Observational Study, 11 cases of endometrial cancer were identified in 3,003 vaginal estrogen users versus 222 cases in 29,430 nonusers (2-year median duration), resulting in an incidence of 1.3/1,000 women-years for vaginal estrogen users and 1.0/1,000 women-years for nonusers.33 Based on these data, risk of endometrial cancer did not statistically significantly increase with use of vaginal estrogens relative to nonusers (hazard ratio [HR] 1.47; 95% CI, 0.75-2.90).33
The second study was an analysis of prospective data collected at a single site from 1976 to 1977 and retrospective data from 1975 for a total of 8,170 women-years including 574 women-years of women who used vaginal estrogen cream.34 The incidence rate of endometrial cancer in vaginal estrogen cream users was numerically lower (1.7 per 1,000 women-years) than in nonusers (2 per 1,000 women-years) and in oral estrogen users (3.8 per 1,000 women-years).34
Retrospective observational studies
Eight studies reported the incidence of endometrial cancer and/or hyperplasia in retrospective, observational/registry studies of ∼1.5 million menopausal women who used vaginal estrogens from 1 to 29 years (Table 1 and Supplemental Table 4, Supplemental Digital Content 4). Two studies were from large registries or databases,35,36 one a case-control study from a large database,37 and five were smaller case-control studies.38-41 In two of the studies, vaginal estrogen was specified as cream,40 and in another as cream, tablets, or ring,37 whereas in the other five studies,35,36,38,39,41 type of vaginal estrogen was not specified.
One Danish study35 and an older, smaller, case-control US study (n = 167 cases and 903 controls)39 identified an increased risk of endometrial cancer. The Danish Sex Hormone Register Study (n = 914,595) found a statistically significant increase in any endometrial cancer with vaginal estrogen use (product type or dose not stated) versus nonuse (risk ratio, 1.96; 95% CI, 1.77-2.17), and that the association did not vary by type of tumor (ie, estrogen [type I] or nonestrogen [type II] dependent).35 The case-control US study evaluated data collected between 1977 and 1979 and found an increased risk of endometrial cancer with vaginal estrogen use compared with nonuse (odds ratio [OR], 2.30; 95% CI, 1.1-4.6).39
The six other retrospective observational studies did not find an increased risk of endometrial hyperplasia or cancer with vaginal estrogen use compared with no use, as shown by incidence and ORs (Supplemental Table 4, Supplemental Digital Content 4). Incidence of endometrial hyperplasia and cancer for vaginal estrogen use versus nonuse was 9.96 to 10.25 versus 9.96/10,000 women-years in the large Kaiser Permanente Northern California membership database cohort study,36 1.3% versus 1.2% in the North Carolina Medicaid cohort study,37 and 7% to 9% versus 8% to 10% in two case-control studies from Yale-New Haven Hospital.40 ORs for risk of endometrial cancer showed no statistically significant increase with vaginal estrogen use versus nonuse in studies of the United States37,40,41 and Sweden38 (Supplemental Table 4, Supplemental Digital Content 4).
DISCUSSION
Clinical evidence from this systematic review does not support an increased risk of endometrial hyperplasia or endometrial cancer with low-dose unopposed vaginal estrogen use. Sporadic reports of endometrial hyperplasia were not associated with a specific dose or duration, with the exception of the highest CEE dose of 1.25 mg used 21 days on/7 days off which appears to be associated with an increased risk of endometrial hyperplasia (2 cases in 28 women).4
The well-established dose effect of endometrial hyperplasia seen with higher doses of oral estrogen products51,52 was not observed with lower doses of vaginal estradiol. Although older studies, which typically evaluated higher vaginal estrogen doses, were not powered to detect endometrial cancer because of small sample size and short duration, they were powered to detect endometrial hyperplasia, a signal that was not detected with low-dose vaginal estrogen products. Overall, the sporadic reports of endometrial hyperplasia observed (∼0.4% in RCTs) appear to be consistent with background rates of endometrial hyperplasia in the general population.53
Of the 38 studies reviewed, only two retrospective observational studies showed an increased risk of endometrial cancer with vaginal estrogens use compared with nonuse. The first was a study reporting data from 1977 to 1979 from a single center in the United States, which observed an increase in endometrial cancer (OR, 2.30; 95% CI, 1.1-4.6).39 This increase may be due to higher-dose vaginal products used in the 1970s compared with lower-dose products currently available. The second larger study from Denmark also found an association between vaginal estrogen use and increased endometrial cancer risk (risk ratio, 1.96; 95% CI 1.77-2.17).35 The findings of the Danish study may, however, be of limited applicability to the United States, as the study had a low background rate of endometrial cancer, longer duration of different rates of vaginal estrogen use, and evaluated different vaginal estrogen products (including estriol and dienestrol) with more frequent use and higher dosing regimens.35 The study also reports an association between vaginal estrogen use and type II (ie, nonestrogen-dependent) endometrial cancer, which suggests ascertainment bias in users of vaginal estrogen products versus nonusers. Prior systemic estrogen use in this study may also be a confounding factor as women with a history of systemic estrogen use were included if duration of vaginal estrogen use exceeded duration of systemic estrogen use.35
The most recent US data were from the WHI Observational Study, which examined real-world use of higher-dose vaginal estrogen products with systemic absorption and reported no increased risk of endometrial cancer with vaginal estrogen use (HR, 1.47; 95% CI, 0.75-2.90).33 Women with previous systemic exposure were excluded from this analysis,33 in contrast to the Danish observational study.35 Since the literature search for this review, an analysis of the large Nurses’ Health Study cohort was published and found results similar to those of the WHI Observational Study.54 No increased risk of endometrial cancer was found in women who used vaginal estrogens versus women who did not use them (HR, 1.62; 95% CI, 0.88-2.97).54
Vaginal prasterone (DHEA) is postulated to be converted intracellularly into estrogens and/or androgens depending on the expression of appropriate steroid-forming and steroid-inactivating enzymes.55,56 Estradiol levels are, however, reported to increase with DHEA use in postmenopausal women.57 Thus, we examined the endometrial histology with prasterone separately. No cases of endometrial hyperplasia or endometrial cancer were observed after exposure to prasterone either daily or twice a week for up to 12 weeks or a year (Supplemental Table 5, Supplemental Digital Content 5).55,58-61
Limitations of this systematic review include the limited number of studies systematically evaluating endometrial hyperplasia and cancer with the use of vaginal estrogens. The RCTs and prospective interventional trials were of short duration and of limited sample size, possibly leading to unpowered studies given the relatively infrequent incidence of endometrial hyperplasia and cancer. Although the observational trials have a greater number of samples and longer follow-up duration, they lack randomization and have potential confounding factors, possibly skewing the results. Despite these limitations, the collective reports of endometrial hyperplasia and endometrial cancer in the large number of women studied who used vaginal estrogens does not support an increased risk of these endometrial pathologies.
Estrogen dose and duration of use can influence the risk of endometrial cancer in systemic estrogen users.62-64 For vaginal products, placement of the estrogen within the vagina (lower vs upper part) may also affect the amount of estrogen reaching the endometrium, and thus, possibly impact endometrial hyperplasia or cancer risk, given the significant anatomic differences of the vascular and lymphatic supplies to the lower and upper vagina. Studies by Cicinelli et al65,66 found that placement of estrogen products in the upper third of the vagina had preferential distribution of estrogen to the uterus, also known as the “first uterine pass effect,” which was mediated by the close proximity of veins and arteries. Whereas when estrogen products are placed in the lower third of the vagina, the transfer of estrogen to the uterus is minimal, which may limit the risk of hyperplasia.65 Therefore, products administered to the lower part of the vagina may have less of an effect on the endometrium than products administered to the upper part of the vagina.65
CONCLUSIONS
The evidence assessed as part of this systematic literature review does not support an increased risk of endometrial hyperplasia or endometrial cancer with vaginal estrogens. Longer-term data may help confirm the endometrial safety profile of vaginal estrogens found in this systematic review.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Acknowledgments
The authors acknowledge the medical writing support provided by Dominique Verlaan, PhD, CMPP (Precise Publications, LLC), which was funded by TherapeuticsMD.
Footnotes
Data Presentation: Presented at the 2018 Endocrine Society Annual Meeting, March 17-20, 2018, Chicago, IL and at the American College of Obstetricians and Gynecologists Annual Meeting, April 27-30, 2018, Austin, TX.
Funding/support: None reported.
Financial disclosure/conflicts of interest: Dr Constantine consults for pharmaceutical companies including but not limited to TherapeuticsMD and has stock options from TherapeuticsMD. Dr Lapane consults for TherapeuticsMD. Dr Liu consults for Allergan, Bayer Healthcare, Pfizer, and TherapeuticsMD; and has received research support (paid to UH Cleveland Medical Center) from AbbVie, Allergan, Bayer Healthcare, Ferring, and Palatin. Dr Ohleth is the owner of Precise Publications. Drs Graham, Bernick, and Mirkin are employees of TherapeuticsMD with stock/stock options. Dr Bernick is also a Board member of TherapeuticsMD.
REFERENCES
- 1.US Census Bureau. Age and sex composition: 2010 Census Briefs. Issued May 2011. Available at http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf Accessed April 14, 2015. [Google Scholar]
- 2.Simon JA, Kokot-Kierepa M, Goldstein J, Nappi RE. Vaginal health in the United States: results from the vaginal health: insights, views & attitudes survey. Menopause 2013; 20:1043–1048. [DOI] [PubMed] [Google Scholar]
- 3.Kingsberg S, Krychman M, Graham S, Bernick B, Mirkin S. The Women's EMPOWER Survey: identifying women's perceptions on vulvar and vaginal atrophy (VVA) and its treatment. J Sex Med 2017; 14:413–424. [DOI] [PubMed] [Google Scholar]
- 4.Rioux JE, Devlin C, Gelfand MM, Steinberg WM, Hepburn DS. 17β-Estradiol vaginal tablet versus conjugated equine estrogen vaginal cream to relieve menopausal atrophic vaginitis. Menopause 2000; 7:156–161. [DOI] [PubMed] [Google Scholar]
- 5.Bachmann G, Bouchard C, Hoppe D, et al. Efficacy and safety of low-dose regimens of conjugated estrogens cream administered vaginally. Menopause 2009; 16:719–727. [DOI] [PubMed] [Google Scholar]
- 6.Luisi M, Franchi F, Kicovic PM. A group-comparative study of effects of Ovestin cream versus Premarin cream in post-menopausal women with vaginal atrophy. Maturitas 1980; 2:311–319. [DOI] [PubMed] [Google Scholar]
- 7.Nachtigall LE. Clinical trial of the estradiol vaginal ring in the US. Maturitas 1995; 22 suppl:S43–S47. [DOI] [PubMed] [Google Scholar]
- 8.Manonai J, Theppisai U, Suthutvoravut S, Udomsubpayakul U, Chittacharoen A. The effect of estradiol vaginal tablet and conjugated estrogen cream on urogenital symptoms in postmenopausal women: a comparative study. J Obstet Gynaecol Res 2001; 27:255–260. [DOI] [PubMed] [Google Scholar]
- 9.Freedman M, Kaunitz AM, Reape KZ, Hait H, Shu H. Twice-weekly synthetic conjugated estrogens vaginal cream for the treatment of vaginal atrophy. Menopause 2009; 16:735–741. [DOI] [PubMed] [Google Scholar]
- 10.Rahn DD, Good MM, Roshanravan SM, et al. Effects of preoperative local estrogen in postmenopausal women with prolapse: a randomized trial. J Clin Endocrinol Metab 2014; 99:3728–3736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vesna A, Neli B. Benefit and safety of 28-day transdermal estrogen regimen during vaginal hysterectomy (a controlled trial). Maturitas 2006; 53:282–298. [DOI] [PubMed] [Google Scholar]
- 12.Bachmann G, Lobo RA, Gut R, Nachtigall L, Notelovitz M. Efficacy of low-dose estradiol vaginal tablets in the treatment of atrophic vaginitis: a randomized controlled trial. Obstet Gynecol 2008; 111:67–76. [DOI] [PubMed] [Google Scholar]
- 13.Felding C, Mikkelsen AL, Clausen HV, Loft A, Larsen LG. Preoperative treatment with oestradiol in women scheduled for vaginal operation for genital prolapse. A randomised, double-blind trial. Maturitas 1992; 15:241–249. [DOI] [PubMed] [Google Scholar]
- 14.Mattsson LA, Cullberg G, Eriksson O, Knutsson F. Vaginal administration of low-dose oestradiol—effects on the endometrium and vaginal cytology. Maturitas 1989; 11:217–222. [DOI] [PubMed] [Google Scholar]
- 15.Mettler L, Olsen PG. Long-term treatment of atrophic vaginitis with low-dose oestradiol vaginal tablets. Maturitas 1991; 14:23–31. [DOI] [PubMed] [Google Scholar]
- 16.Weisberg E, Ayton R, Darling G, et al. Endometrial and vaginal effects of low-dose estradiol delivered by vaginal ring or vaginal tablet. Climacteric 2005; 8:83–92. [DOI] [PubMed] [Google Scholar]
- 17.Cardozo LD, Wise BG, Benness CJ. Vaginal oestradiol for the treatment of lower urinary tract symptoms in postmenopausal women—a double-blind placebo-controlled study. J Obstet Gynaecol 2001; 21:383–385. [DOI] [PubMed] [Google Scholar]
- 18.Simon J, Nachtigall L, Ulrich LG, Eugster-Hausmann M, Gut R. Endometrial safety of ultra-low-dose estradiol vaginal tablets. Obstet Gynecol 2010; 116:876–883. [DOI] [PubMed] [Google Scholar]
- 19.Simon J, Nachtigall L, Gut R, Lang E, Archer DF, Utian W. Effective treatment of vaginal atrophy with an ultra-low-dose estradiol vaginal tablet. Obstet Gynecol 2008; 112:1053–1060. [DOI] [PubMed] [Google Scholar]
- 20.Constantine G, Simon JA, Pickar JH, et al. The REJOICE trial: a phase 3 randomized, controlled trial evaluating the safety and efficacy of a novel vaginal estradiol soft-gel capsule for symptomatic vulvar and vaginal atrophy. Menopause 2017; 24:409–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barentsen R, Van de Weijer PH, Schram JH. Continuous low dose estradiol released from a vaginal ring versus estriol vaginal cream for urogenital atrophy. Eur J Obstet Gynecol Reprod Biol 1997; 71:73–80. [DOI] [PubMed] [Google Scholar]
- 22.Henriksson L, Stjernquist M, Boquist L, Cedergren I, Selinus I. A one-year multicenter study of efficacy and safety of a continuous, low-dose, estradiol-releasing vaginal ring (Estring) in postmenopausal women with symptoms and signs of urogenital aging. Am J Obstet Gynecol 1996; 174:85–92. [DOI] [PubMed] [Google Scholar]
- 23.Pinkerton JV, Shifren JL, La VJ, Rosen A, Roesinger M, Siddhanti S. Influence of raloxifene on the efficacy of an estradiol-releasing ring for treating vaginal atrophy in postmenopausal women. Menopause 2003; 10:45–52. [DOI] [PubMed] [Google Scholar]
- 24.Vartiainen J, Wahlstrom T, Nilsson CG. Effects and acceptability of a new 17 beta-oestradiol-releasing vaginal ring in the treatment of postmenopausal complaints. Maturitas 1993; 17:129–137. [DOI] [PubMed] [Google Scholar]
- 25.Handa VL, Bachus KE, Johnston WW, Robboy SJ, Hammond CB. Vaginal administration of low-dose conjugated estrogens: systemic absorption and effects on the endometrium. Obstet Gynecol 1994; 84:215–218. [PubMed] [Google Scholar]
- 26.Santen RJ, Pinkerton JV, Conaway M, et al. Treatment of urogenital atrophy with low-dose estradiol: preliminary results. Menopause 2002; 9:179–187. [DOI] [PubMed] [Google Scholar]
- 27.Semmens JP, Tsai CC, Semmens EC, Loadholt CB. Effects of estrogen therapy on vaginal physiology during menopause. Obstet Gynecol 1985; 66:15–18. [PubMed] [Google Scholar]
- 28.Mainini G, Scaffa C, Rotondi M, Messalli EM, Quirino L, Ragucci A. Local estrogen replacement therapy in postmenopausal atrophic vaginitis: efficacy and safety of low dose 17beta-estradiol vaginal tablets. Clin Exp Obstet Gynecol 2005; 32:111–113. [PubMed] [Google Scholar]
- 29.Manonai J, Theppisai U, Chittacharoen A. Effect and safety of 17 beta-estradiol vaginal tablet in postmenopausal women with urogenital symptoms. J Med Assoc Thai 2001; 84:1015–1020. [PubMed] [Google Scholar]
- 30.Ulrich LS, Naessen T, Elia D, Goldstein JA, Eugster-Hausmann M. Endometrial safety of ultra-low-dose vagifem 10 microg in postmenopausal women with vaginal atrophy. Climacteric 2010; 13:228–237. [DOI] [PubMed] [Google Scholar]
- 31.Van Haaften M, Donker GH, Sie-Go DM, Haspels AA, Thijssen JH. Biochemical and histological effects of vaginal estriol and estradiol applications on the endometrium, myometrium and vagina of postmenopausal women. Gynecol Endocrinol 1997; 11:175–185. [DOI] [PubMed] [Google Scholar]
- 32.Yumru AE, Bozkurt M, Inci CE, Baykan G. The use of local 17beta-oestradiol treatment for improving vaginal symptoms associated with post-menopausal oestrogen deficiency. J Int Med Res 2009; 37:198–204. [DOI] [PubMed] [Google Scholar]
- 33.Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women's Health Initiative Observational Study. Menopause 2018; 25:11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gambrell RD, Jr, Massey FM, Castaneda TA, Ugenas AJ, Ricci CA. Reduced incidence of endometrial cancer among postmenopausal women treated with progestogens. J Am Geriatr Soc 1979; 27:389–394. [DOI] [PubMed] [Google Scholar]
- 35.Mørch LS, Kjaer SK, Keiding N, Lokkegaard E, Lidegaard O. The influence of hormone therapies on type I and II endometrial cancer: a nationwide cohort study. Int J Cancer 2016; 138:1506–1515. [DOI] [PubMed] [Google Scholar]
- 36.Gunnison KM, Tucker LY, Postlethwaite DA, Pruett KM. Topical vaginal estrogen use and risk of endometrial hyperplasia or cancer. Obstet Gynecol 2015; 125:8S. [Google Scholar]
- 37.Neidecker MV, Camacho F, Balkrishnan R. Endometrial carcinoma risk of vaginal estrogen in medicaid women with atrophic vaginitis. Value Health 2009; 12:A38. [Google Scholar]
- 38.Weiderpass E, Baron JA, Adami HO, et al. Low-potency oestrogen and risk of endometrial cancer: a case-control study. Lancet 1999; 353:1824–1828. [DOI] [PubMed] [Google Scholar]
- 39.Kelsey JL, LiVoisi VA, Holford TR, et al. A case-control study of cancer of the endometrium. Am J Epidemiol 1982; 116:333–342. [DOI] [PubMed] [Google Scholar]
- 40.Horwitz RI, Feinstein AR. Intravaginal estrogen creams and endometrial cancer: no causal association found. JAMA 1979; 241:1266–1267. [PubMed] [Google Scholar]
- 41.Gray LA, Sr, Christopherson WM, Hoover RN. Estrogens and endometrial carcinoma. Obstet Gynecol 1977; 49:385–389. [PubMed] [Google Scholar]
- 42.Al-Azzawi F, Lees B, Thompson J, Stevenson JC. Bone mineral density in postmenopausal women treated with a vaginal ring delivering systemic doses of estradiol acetate. Menopause 2005; 12:331–339. [DOI] [PubMed] [Google Scholar]
- 43.Buckler H, Al-Azzawi F. The effect of a novel vaginal ring delivering oestradiol acetate on climacteric symptoms in postmenopausal women. BOG 2003; 110:753–759. [PubMed] [Google Scholar]
- 44.Al-Azzawi F, Buckler HM. Comparison of a novel vaginal ring delivering estradiol acetate versus oral estradiol for relief of vasomotor menopausal symptoms. Climacteric 2003; 6:118–127. [PubMed] [Google Scholar]
- 45.Gordon WE, Hermann HW, Hunter DC. Safety and efficacy of micronized estradiol vaginal cream. South Med J 1979; 72:1252–1253. [DOI] [PubMed] [Google Scholar]
- 46.Timonen S, Tervila L. Uterine carcinoma and oestrogen reaction in vaginal smear. Ann Chir Gynaecol Fenn 1963; 52:143–147. [PubMed] [Google Scholar]
- 47.Vagifem (estradiol vaginal tablets) Prescribing Information. Bagsvaerd, Denmark: Novo Nordisk Pharmaceuticals Inc; 2012. [Google Scholar]
- 48.Gambrell RD., Jr The prevention of endometrial cancer in postmenopausal women with progestogens. Maturitas 1978; 1:107–112. [DOI] [PubMed] [Google Scholar]
- 49.Novo Nordisk. Vagifem 10 mcg to replace Vagifem® 25 mcg formulation for atrophic vaginitis due to menopause. Available at: http://press.novonordisk-us.com/News-Releases?item=122607 June 1, 2018. [Google Scholar]
- 50.Premarin (conjugated estrogens) Vaginal Cream Prescribing Information. Philadelphia, PA: Wyeth Pharmaceuticals Inc; 2016. [Google Scholar]
- 51.Pickar JH, Yeh IT, Wheeler JE, Cunnane MF, Speroff L. Endometrial effects of lower doses of conjugated equine estrogens and medroxyprogesterone acetate: two-year substudy results. Fertil Steril 2003; 80:1234–1240. [DOI] [PubMed] [Google Scholar]
- 52.Key TJ, Pike MC. The dose-effect relationship between ’unopposed’ oestrogens and endometrial mitotic rate: its central role in explaining and predicting endometrial cancer risk. Br J Cancer 1988; 57:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reed SD, Newton KM, Clinton WL, et al. Incidence of endometrial hyperplasia. Am J Obstet Gynecol 2009; 200:678.e1–678.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bhupathiraju SN, Grodstein F, Stampfer MJ, et al. Vaginal estrogen use and chronic disease risk in the Nurses’ Health Study. Menopause 2018; [Epub ahead of print, Dec 17]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Portman DJ, Labrie F, Archer DF, et al. Lack of effect of intravaginal dehydroepiandrosterone (DHEA, prasterone) on the endometrium in postmenopausal women. Menopause 2015; 22:1289–1295. [DOI] [PubMed] [Google Scholar]
- 56.Luu-The V, Zhang Y, Poirier D, Labrie F. Characteristics of human types 1, 2 and 3 17 beta-hydroxysteroid dehydrogenase activities: oxidation/reduction and inhibition. J Steroid Biochem Mol Biol 1995; 55:581–587. [DOI] [PubMed] [Google Scholar]
- 57.Intrarosa (prasterone insert) Prescribing Information. Waltham, MA: AMAG Pharmaceuticals; 2018. [Google Scholar]
- 58.Bouchard C, Labrie F, Derogatis L, et al. Effect of intravaginal dehydroepiandrosterone (DHEA) on the female sexual function in postmenopausal women: ERC-230 open-label study. Horm Mol Biol Clin Investig 2016; 25:181–190. [DOI] [PubMed] [Google Scholar]
- 59.Labrie F, Archer D, Bouchard C, et al. Intravaginal dehydroepiandrosterone (prasterone), a physiological and highly efficient treatment of vaginal atrophy. Menopause 2009; 16:907–922. [DOI] [PubMed] [Google Scholar]
- 60.Archer DF, Labrie F, Bouchard C, et al. Treatment of pain at sexual activity (dyspareunia) with intravaginal dehydroepiandrosterone (prasterone). Menopause 2015; 22:950–963. [DOI] [PubMed] [Google Scholar]
- 61.Bouchard C, Labrie F, Archer DF, et al. Decreased efficacy of twice-weekly intravaginal dehydroepiandrosterone on vulvovaginal atrophy. Climacteric 2015; 18:590–607. [DOI] [PubMed] [Google Scholar]
- 62.Grady D, Gebretsadik T, Kerlikowske K, Ernster V, Petitti D. Hormone replacement therapy and endometrial cancer risk: a meta-analysis. Obstet Gynecol 1995; 85:304–313. [DOI] [PubMed] [Google Scholar]
- 63.Trabert B, Wentzensen N, Yang HP, et al. Is estrogen plus progestin menopausal hormone therapy safe with respect to endometrial cancer risk? Int J Cancer 2013; 132:417–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Epstein E, Lindqvist PG, Olsson H. A population-based cohort study on the use of hormone treatment and endometrial cancer in southern Sweden. Int J Cancer 2009; 125:421–425. [DOI] [PubMed] [Google Scholar]
- 65.Cicinelli E, Di NE, De ZD, et al. Placement of the vaginal 17beta-estradiol tablets in the inner or outer one third of the vagina affects the preferential delivery of 17beta-estradiol toward the uterus or periurethral areas, thereby modifying efficacy and endometrial safety. Am J Obstet Gynecol 2003; 189:55–58. [DOI] [PubMed] [Google Scholar]
- 66.Cicinelli E, De Ziegler D, Morgese S, Bulletti C, Luisi D, Schonauer LM. First uterine pass effect is observed when estradiol is placed in the upper but not lower third of the vagina. Fertil Steril 2004; 81:1414–1416. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


