Abstract
Background
The relationship between a clinician and their client—the “therapeutic alliance” is a robust predictor of outcome in healthcare settings; yet, few interventions to improve alliance have been tested. Motivational interviewing is a client-centered approach that embodies many principles and strategies consistent with a strong therapeutic alliance.
Purpose
To examine whether alliance is enhanced by training dietitians to deliver a motivational interviewing informed health behavior change intervention (“Eating as Treatment”; EAT) as part of routine consultations with patients with head and neck cancer. The predictive ability of motivational interviewing techniques was also assessed.
Methods
A secondary analysis of the EAT stepped-wedge cluster-randomized controlled trial was conducted. Patients with head and neck cancer undergoing radiotherapy (n = 307) were treated by radiotherapy dietitians (n = 29) during the control (Treatment as Usual) or intervention (EAT) phase. Alliance was rated during the first and final weeks of radiotherapy, and again 4 and 12 weeks post-radiotherapy. Dietetic sessions were audiotaped. Week one sessions were objectively rated for dietitians’ use of motivational interviewing techniques.
Results
Generalized linear-mixed effects regressions found no effect of EAT on dietitian-rated alliance (p = .237). After excluding outliers, patient-rated alliance was 0.29 points lower after EAT training (p = .016). Post hoc analyses revealed lower patient ratings on perceived support and dietitian confidence. Hierarchical multiple regressions found that no specific motivational interviewing techniques predicted patient-rated alliance. Dietitian acknowledgment of patient challenges was related to dietitian-rated alliance (β =.15, p =.035).
Conclusions
Patient and dietitian ratings of alliance were high after EAT training, but not significantly improved. Further research is needed to better understand the differential impact of intervention training and delivery on patient and clinician ratings of therapeutic alliance.
Clinical Trial information
Trial registration number ACTRN12613000320752
Keywords: Alliance, Motivational interviewing, Cancer • Nutrition, Eating as treatment
Training dietitians to deliver a new health behaviour change intervention affected the strength of their working relationship with head and neck cancer patients.
Introduction
The relationship between a clinician and their client—the “therapeutic alliance,” also known as the working or helping alliance, is one of the most studied concepts in the psychotherapy research literature [1–4]. One likely reason for the interest is the often-cited link between the quality of the therapeutic alliance and therapy outcomes across a variety of therapeutic approaches and client presentations within psychotherapy [2, 5, 6] and more recently, within behavioral medicine [7, 8]. Meta-analyses on the effect of therapeutic alliance on patient outcomes within psychotherapy [1, 6] and medical settings [7] have produced medium to large effect sizes, with other research suggesting that the proportion of variance in outcome explained by alliance may be as large as 14.7% [9]. However, despite the wealth of research into the therapeutic alliance, and the demonstrated link between alliance and client outcomes, there remains relatively little evidence on how best to build and maintain the therapeutic alliance [10, 11].
Whilst no single, generally agreed upon definition of the therapeutic alliance exists [1, 12, 13], many researchers follow Bordin’s [14] conceptualization of alliance. According to Bordin, the alliance consists of three features: agreement on therapeutic goals, consensus on the tasks of therapy, and the development of a bond between client and therapist. Numerous measures of therapeutic alliance have been developed, and several measurement issues noted. First is the need to consider from whose perspective alliance is being measured (the client, the therapist, or an external observer) as client and therapist ratings of the alliance may be incongruent [1], and client ratings tend to be stronger predictors of therapeutic outcome [2]. Second, given that alliance fluctuates over time, it is necessary to consider the point in therapy at which alliance is measured: earlier measures of alliance are favored, as they have been found to be particularly predictive of outcome [2]. Not surprisingly, whilst most research only measures alliance at a single time point, outcome is more dependably predicted when alliance is measured at multiple time points [9].
Several therapist variables influence the therapeutic alliance. Ackerman and Hilsenroth [15] reviewed 25 studies that investigated therapist variables related to therapeutic alliance and found alliance to be related to both therapist personal attributes (e.g., being open, warm, flexible, honest, respectful, and confident) and also therapist techniques (e.g., exploration, reflection, accurate interpretation, being supportive, affirming, and attending to the patient’s experience). Such findings have led to recommendations that clinicians be trained in alliance-fostering techniques (e.g., Refs. 1, 2, 7, 13, and 16). Conversely, it has been argued that due to the interpersonal nature of the alliance, it may not be possible to teach therapists the ability to form strong alliances [17]. It is not surprising then that efforts to train therapists to improve alliance have been met with mixed results—with some (e.g., Refs. 18 and 19), but not others (e.g., Refs. 17, 20, and 21), demonstrating improvement in alliance post-training. Possible explanations for the mixed results include methodological limitations (e.g., small sample sizes), potential difficulties in manualizing relational aspects of the alliance [17], and the possibility that some elements of the alliance (e.g., goal setting) may be more easily trained than other elements (e.g., bond development [22]).
Motivational interviewing [23] is a client-centered approach that encourages change by allowing clients to explore and resolve ambivalence in an accepting and compassionate therapeutic relationship. At its core, motivational interviewing suggests certain features of therapy (specifically collaboration, acceptance, compassion, and eliciting the client’s intrinsic motivation for change) to be critical for promoting behavior change [24]. Techniques used include asking open-ended questions, informing and advising (with permission), reflective listening, affirming, and summarizing. Numerous systematic reviews and meta-analyses have presented evidence for the effectiveness of motivational interviewing in various healthcare settings [25–29]. Although motivational interviewing was initially developed to be used in 30 to 60 min therapy sessions to address problem drinking, it has been adapted in various (often shortened) forms to address a wide variety of health behaviors including pain management, diabetes control, physical activity, and diet [30].
Given the emphasis motivational interviewing has on alliance-related behaviors such as collaboration and respect, it appears to be an excellent psychosocial model for building the therapeutic alliance [31–33]. The results of several studies support this proposition. Boardman et al. [24] found that motivational interviewing spirit (collaboration, empathy, and egalitarianism) significantly predicted working alliance in a smoking cessation trial. Similarly Moyers et al. [34] found that motivational interviewing-consistent interpersonal skills were significantly related to the alliance-related construct of client involvement in a substance abuse trial. Looking at an adaptation of motivational interviewing (motivational enhancement therapy), Crits-Christoph et al. [33] found greater use of motivational enhancement therapy techniques to be associated with higher levels of alliance. Furthermore, it has been suggested that motivational interviewing may be particularly useful in improving the alliance of clinicians with only limited counseling experience [33].
The present study is a secondary analysis of data from a stepped-wedge cluster-randomized controlled trial of a dietitian-delivered health behavior change intervention (Eating As Treatment [EAT [35]]). The EAT Intervention builds from a successful pilot [36] and is designed to be integrated into brief oncology dietetic consultations. It was developed with the aim of reducing malnutrition in patients with head and neck cancer undergoing radiotherapy. EAT incorporates behavior change principles and strategies drawn from motivational interviewing and cognitive behavior therapy, with a view to encourage patients to maintain their nutrition, [35] despite a range of factors that hinder oral intake (including local tumor effects and side effects of radiotherapy [37]). Accordingly, The EAT trial afforded a unique opportunity to assess therapeutic alliance between “real-world” oncology dietitians and their patients during routine care and after being trained in motivational interviewing consistent principles and strategies.
The primary aim of the current analysis is to explore whether therapeutic alliance improved after dietitians were trained in EAT. We hypothesized that alliance would be rated higher (by both dietitians and patients) when EAT principles and strategies were used to inform the delivery of dietetic intervention (i.e., after training) relative to routine delivery of dietetic intervention (i.e., before training). To best inform alliance training pedagogy, a secondary aim was to explore the relationship between motivational interviewing skills and therapeutic alliance.
Methods
A detailed account of the parent EAT trial is reported elsewhere [35] and summarized below.
Study Design—The EAT Trial
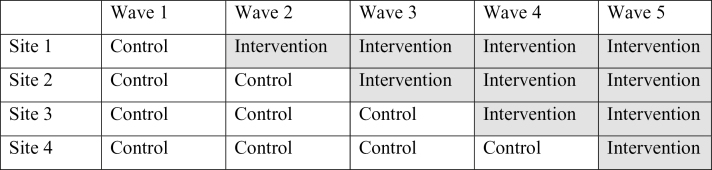
The EAT trial employed a stepped-wedge cluster-randomized controlled design [35]. Participants were recruited for the study in waves so that each cluster contributed data under both the control and intervention conditions (Fig. 1). As the EAT trial involved training dietitians in a new practice paradigm, a cluster-randomized design was considered preferable to a standard randomized design as it limits the contamination between groups that would occur if dietitians were required to ignore new intervention principles acquired when treating control participants. A stepped-wedge, cluster-randomized, controlled trial was considered preferable to a standard, parallel, cluster-randomized controlled trial as the former provides the same level of evidence as the latter with the advantage of requiring fewer trial sites [38]. Sites were recruited through the Trans-Tasman Radiation Oncology Group—a cancer clinical trial group that works with treatment providers across Australia and New Zealand to facilitate the development and conduct of radiotherapy-related clinical trials. The order of movement to the intervention condition randomized using a uniform random number generator in STATA.
Fig. 1·.
Sequence of intervention roll-out in the stepped-wedge design.
Participants
Staff and patients from the radiotherapy departments of five Australian hospitals participated in the EAT trial. At one of the sites, two hospitals were combined to represent one step in the stepped-wedge design because of the overlap of dietetic services in those hospitals.
Patients
A total of 307 patients were recruited to the EAT trial. Eligible patients were those aged 18 years or over, with a diagnosis of head and neck cancer, undergoing curative radiation therapy, available for follow-up for at least 6 months and capable of providing written informed consent. Patients who were unlikely to satisfactorily complete questionnaires due to an inability to communicate in English or the presence of organic brain disease were excluded. Hospital research officers approached eligible participants, explained the study to them, and obtained written informed consent. As shown in Table 1, most participants were men (79.4%) and the average age of participants was 58.4 years. The number of dietetic appointments attended by control participants (M = 10.13, SE = 0.23) was comparable to intervention participants (M =10.8, SE = 0.37). Radiotherapy prescription (Gy: M = 68, SD = 4 vs. M = 68, SD = 3) and duration—approximately 7 weeks (fraction number: M = 34, SD = 2 vs. M = 34, SD = 2) were also comparable across groups.
Table 1.
Week one patient characteristics for each phase
| Characteristic | Intervention phase | |
|---|---|---|
| Control | Intervention | |
| (n = 151) | (n = 155) | |
| Sex, n (%) | ||
| Male | 126 (83) | 117 (76) |
| Female | 25 (17) | 38 (24) |
| Age, M (SD) | 58.5 (10.0) | 58.3 (10.7) |
| PHQ-9, M (SD) | 4.3 (5.1) | 4.2 (4.2) |
| PG-SGA, M (SD) | 5.4 (5.2) | 5.5 (4.9) |
| Country of birth, n (%) | ||
| Australia | 100 (66) | 97 (62) |
| UK and Ireland | 13 (9) | 25 (16) |
| Other | 38 (25) | 33 (21) |
| Marital status, n (%) | ||
| Married/defacto | 102 (67) | 90 (58) |
| Single/other | 49 (33) | 65 (42) |
| Highest education, n (%) | ||
| Up to year 9 | 22 (15) | 21 (14) |
| School Certificate | 32 (21) | 36 (23) |
| High School Certificate | 20 (13) | 27 (17) |
| TAFE/other | 46 (30) | 36 (23) |
| University degree | 31 (21) | 35 (23) |
| Employment, n (%) | ||
| Full-time | 79 (52) | 73 (47) |
| Part-time/casual | 12 (8) | 18 (11) |
| Retired | 41 (27) | 40 (26) |
| No job | 10 (7) | 9 (6) |
| Other | 9 (6) | 15 (10) |
M Mean; n Number; PG-SGA Patient-Generated Subjective Global Assessment; PHQ-9 Patient Health Questionnaire; SD Standard Deviation; TAFE Technical and Further Education.
Dietitians
Twenty-nine radiotherapy dietitians provided treatment to participants enrolled in the EAT trial. Due to staff turnover across the 30 months, the study was conducted, not all dietitians saw patients across both the control and intervention phases: 13 dietitians saw patients in both phases, 11 dietitians only saw patients during the control phase, and 5 dietitians only saw patients during the intervention phase. For dietitians who took part in the intervention phase (n = 18), all had attained bachelor level qualifications, 8 had completed postgraduate level training in nutrition and dietetics (e.g., Masters and Postgraduate Diploma), and length of experience working with patients with head and neck cancer ranged from a few months to more than 20 years. Demographic information was not available for the dietitians who only saw patients in the control phase (n = 11).
EAT Intervention
Maintaining adequate nutrition during radiotherapy is important to achieve positive treatment outcomes; however, this is complicated by a range of barriers encountered by patients with head and neck cancer (e.g., mucositis, loss of appetite, and pain [37]). The EAT intervention [35] combines principles and strategies from motivational interviewing and cognitive behavior therapy to help dietitians improve the motivation for patients to maintain their nutrition during radiotherapy treatment, whilst also providing practical behavior change strategies to assist patients reach their dietary goals. The intervention is guided by four principles stating that behavior change is more likely to occur if (a) people argue for the behavior themselves; (b) it is part of a concrete plan they devise for themselves; (c) it is recorded externally; and (d) they feel it is important, achievable and is being monitored. Dietitians were trained in techniques (e.g., eliciting motivation for change) to enable them to conduct their sessions in a manner consistent with these principles. In line with the motivational interviewing technique of facilitating discrepancy [23], dietitians were also trained to hold a specific conversation with patients (“Eat to Live”) in which patients were invited to reflect on the (in)consistency of their current eating behaviors, their continued treatment efforts, and desire to survive cancer. The intervention was delivered as part of routine face-to-face consultations delivered by dietitians at participating hospital sites. A full description of the intervention has been detailed elsewhere [35].
EAT Procedure
The control phase for the EAT trial was treatment as usual in which dietitians delivered routine dietetic care with no changes to the usual care provided to patients. As sites moved into the intervention phase, a team of instructors provided dietitians with a 2 day, 12 hr workshop in EAT, and 1 day “shadowing” clinicians during regular practice to support “real-world” implementation. The initial training was supported by a booster training session and regular supervision with a clinical psychologist. Individual telephone supervision and coaching sessions were scheduled to occur fortnightly for between 30 and 60 minutes for 2 months (commencing the week after training where possible). Following the 2 month booster training, session frequency reduced to monthly, but could remain fortnightly as needed (e.g., dietitian request). Supervision and coaching sessions comprised both global support/troubleshooting and specific feedback based on shared discussion and evaluation of session recordings. For simplicity, hereafter, “EAT Training” will be used to refer to the entire training package (initial training, booster training, and supervision/coaching sessions). A full description of training and support is detailed elsewhere [35, 39].
Measurement
Patients were assessed on a range of validated measures during the first and last weeks of radiotherapy, and again 4 and 12 weeks post-radiotherapy (only those relevant to the present secondary analysis are detailed here). In addition (and with patient consent), dietitians were asked to audio record all dietetic sessions with trial patients. For the current study, all week one session recordings were rated by an independent assessor (blind to treatment allocation) on the dietitian’s use of motivational interviewing techniques. The focus on week one sessions for the current analysis was due to the demonstrated link between early alliance and patient outcome [2].
Therapeutic alliance
Patients and dietitians rated therapeutic alliance at each assessment point using the Agnew Relationship Measure—Five Item Version [40]. This 5-item questionnaire was developed to track therapeutic alliance in busy clinical settings [40]. It uses items from the Bond, Partnership, and Confidence domains in the original 28-item Agnew Relationship Measure. Participants and clinicians (on parallel forms) rated their agreement with a series of statements describing different elements of the therapeutic alliance. Responses were recorded on a 7-point Likert scale anchored from 1 (strongly disagree) to 7 (strongly agree), with higher scores indicating a stronger alliance. A core alliance score was derived by calculating the mean of the five items. The Agnew Relationship Measure—Five Item Version has acceptable levels of alternative forms of reliability and internal consistency [40] and the parent 28-item version has strong concurrent validity relative to the Working Alliance Inventory—one of the most commonly implemented measures of therapeutic alliance [41]. In the present study, Cronbach’s alpha was .90 for the dietitian form and .78 for the patient form.
Dietitian use of motivational interviewing techniques
Dietitians’ use of motivational interviewing techniques during week one of radiotherapy was evaluated using the Behavior Change Counseling Index [42]. Relative to other standardized fidelity measures (e.g., the Motivational Interviewing Treatment Integrity Code [43]), the Behavior Change Counseling Index is less complex and requires less training. The Behavior Change Counseling Index is an 11-item inventory developed to assess the use of motivational interviewing skills in behavior change counseling, an adaptation of motivational interviewing used in brief healthcare consultations [42]. A blinded assessor rated the degree to which dietitians exhibited each item (e.g., the practitioner invites the patient to talk about behavior change; the practitioner asks questions to elicit how the patient thinks and feels about the topic; when the practitioner provides information, it is sensitive to patient concerns and understanding), using a 5-point Likert scale anchored from 0 (not at all) to 4 (a great deal). The mean score of all applicable items was calculated to produce an overall score. The index generated scores between 0 and 4, with higher scores indicating a greater use of motivational interviewing techniques. The Behavior Change Counseling Index has acceptable levels of face validity and reliability [42]. In the present study, Cronbach’s alpha was .76.
Statistical Analyses
All analyses were conducted using the full sample of providers. To verify that the EAT training changed the practice of dietitians, an independent-samples t-test was conducted to compare the use of motivational interviewing techniques in week one sessions by dietitians in the control and intervention phases. Following Ardito and Rebellino’s [5] suggestion that alliance research should pay attention to the level of agreement between client and clinician ratings of alliance, the relationship between patient-rated alliance and dietitian-rated alliance was investigated using the Pearson product-moment correlation coefficient.
The effect of training (EAT vs. treatment as usual) on both patient and dietitian ratings of the therapeutic alliance was then assessed using generalized linear-mixed effects regression models. In line with the intention to treat principle, all participants were included in the analysis. For each alliance outcome (patient-rated alliance and dietitian-rated alliance), we included a fixed effect for site (to account for differences in the average level of the outcome across sites), a fixed effect for study wave (to account for calendar time), and a fixed effect indicator variable for intervention group (either EAT or treatment as usual). As therapeutic alliance was assessed on four occasions, a random effect for participant and a fixed effect for assessment time point were also included. To allow for any different trajectories of alliance scores over time depending on intervention group, an interaction term for intervention group by time point was also included. However, as this interaction was found to be nonsignificant, it was removed from the model.
For the dietitian-rated therapeutic alliance, one potential outlier was identified, but as the exclusion of the outlier did not alter the pattern of results, the results for the entire sample are presented. For the patient-rated therapeutic alliance, three potential outliers (all with scores 7.5 SD lower than the mean) were identified in the control phase. As the exclusion of the outliers altered the pattern of results, the results for both the entire sample and the sample excluding the outliers are presented.
To analyze whether individual motivational interviewing techniques were related to alliance, hierarchical multiple regressions were performed to assess the ability of each Behavior Change Counseling Index item to predict alliance (both patient-rated and dietitian-rated) after controlling for the influence of site, wave, and the other Behavior Change Counseling Index items. Analyses were conducted using IBM SPSS 24.0.
Results
Dietitians in the intervention phase (M = 1.80, SD = 0.44) were rated as exhibiting more motivational interviewing techniques in week one sessions than dietitians in the control phase (M = 1.33, SD = 0.36; p < .001). The magnitude of the differences in the means (mean difference = −0.46, 95% CIs [−0.57, −0.36]) indicated a large effect of EAT training on use of motivational interviewing techniques. There was also a small, positive correlation between patient and dietitian ratings of alliance, r = .096, n = 817, p < .001.
Effect of EAT Training on Therapeutic Alliance
Dietitian-rated alliance
The crude and adjusted mean dietitian-rated therapeutic alliance scores are presented in Table 2. Adjusting for assessment time point, site, and wave, no significant difference was found between mean dietitian-rated therapeutic alliance scores in the intervention phase compared with the control phase (adjusted mean scores control vs. intervention: 6.47 vs. 6.27; β = −0.19, 95% CIs [−0.52, 0.13], p = 0.237).
Table 2.
Crude and adjusteda mean dietitian- and patient-rated alliance by intervention phase in the samples including and excluding outliers
| Dietitian | Patient | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Including outliersb (Control n = 24, Intervention n = 18) |
Including outliers (Control n = 151, Intervention n = 155) |
Excluding outliers (Control n = 148, Intervention n = 155) |
|||||||
| Intervention phase | Crude M (SD) | Adjusted M (SE) | Observed range (possible range) | Crude M (SD) | Adjusted M (SE) | Observed range (possible range) | Crude M (SD) | Adjusted M (SE) | Observed range (possible range) |
| Control | 5.96 (0.89) | 6.47 (0.14) | 2.40–7.00 (1.00–7.00) |
6.64 (0.75) | 6.89 (0.11) | 1.00–7.00 (1.00–7.00) |
6.68 (0.57) | 6.96 (0.10) | 4.00–7.00 (1.00–7.00) |
| Intervention | 6.32 (0.86) | 6.27 (0.09) | 2.00–7.00 (1.00–7.00) |
6.67 (0.62) | 6.68 (0.07) | 3.20–7.00 (1.00–7.00) |
6.67 (0.62) | 6.67 (0.07) | 3.20–7.00 (1.00–7.00) |
aMean scores adjusted for time point, site, and wave.
bThe single outlier did not affect the pattern of results, entire sample presented.
Patient-rated alliance
The crude and adjusted mean patient-rated therapeutic alliance scores (entire sample and after excluding outliers) are also presented in Table 2. With outliers included, no significant difference was found between mean patient-rated therapeutic alliance scores for patients in the intervention phase compared with the control phase (adjusted mean scores control vs. intervention: 6.89 vs. 6.68; β = −0.21, 95% CIs [−0.46, 0.04], p = .101). However, when the three outliers were excluded, the mean patient-rated therapeutic alliance score was 0.29 points lower for participants in the intervention phase, compared with the control phase (adjusted mean scores control vs. intervention: 6.96 vs. 6.67; β = −0.29, 95% CIs [−0.52, −0.05], p = .016).
Given this unexpected result, a series of post hoc exploratory generalized linear-mixed effects regression models were performed for each of the individual therapeutic alliance items (controlling for site, wave, and assessment time point) to assess which therapeutic alliance item(s) were rated lower by intervention relative to control participants. The results are presented in Table 3. In summary, the analyses indicated that intervention patients rated alliance significantly lower than control patients on therapeutic alliance items 1 (“My dietitian is supportive”), 4 (“I have confidence in my dietitian and his/her techniques”), and 5 (“My dietitian is confident in him/herself and his/her techniques”).
Table 3.
Post hoc generalized linear mixed effects regressions for effects of Eating As Treatment training on individual patient-rated alliance items
| Intervention phase | ||||||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | 95% CI | ||||||
| Therapeutic Alliance itema | Crude M (SD) | Adjusted M (SE) | Crude M (SD) | Adjusted M (SE) | β | p | Lower limit | Upper limit |
| 1. Support | 6.74 (0.75) | 6.72 (0.06) | 6.71 (0.74) | 6.97 (0.10) | −.24 | .032* | −0.46 | −0.02 |
| 2. Agree | 6.66 (0.81) | 6.64 (0.08) | 6.67 (0.72) | 6.87 (0.11) | −.24 | .072 | −0.50 | 0.02 |
| 3. Partnership | 6.40 (1.57) | 6.56 (0.16) | 6.55 (1.36) | 6.83 (0.24) | −.27 | .318 | −0.81 | 0.27 |
| 4. Patient confidence | 6.69 (0.79) | 6.62 (0.09) | 6.63 (0.91) | 7.13 (0.14) | −.50 | .002* | −0.81 | −0.19 |
| 5. Dietitian confidence | 6.71 (0.80) | 6.79 (0.07) | 6.78 (0.61) | 7.03 (0.10) | −.24 | .039* | −0.46 | −0.01 |
Mean scores adjusted for time point, site, and wave.
aItem 1, “My dietitian is supportive”; Item 2, “My dietitian and I agree about how to work together”; Item 3, “My dietitian and I have difficulty working jointly as a partnership”; Item 4, “I have confidence in my dietitian and his/her techniques”; and Item 5, “My dietitian is confident in him/herself and his/her techniques.”
*p < .05.
Relationship Between Specific Motivational Interviewing Techniques and Therapeutic Alliance
Dietitian-rated alliance
In Step 1 of the hierarchical multiple regression (presented in Table 4), site and wave were found to significantly account for 19.7% of the variance in dietitian-rated alliance (p < .001). After entry of all Behavior Change Counseling Index items at Step 2, the total variance explained by the model as a whole was 25.4% (p < .001). The Behavior Change Counseling Index items explained an additional 5.7% of the variance in dietitian-rated alliance, after controlling for site and wave; however, this increase was not significant (p = .270). In the final model, only Behavior Change Counseling Index item 8 (“Practitioner acknowledges challenges about change that the patient faces”) had demonstrated a significant relationship with dietitian-rated alliance (β = .15, p = .035).
Table 4.
Hierarchical multiple regression analysis predicting dietitian-rated alliance
| Variable | B | SE B | β | t | p | R 2 | R 2∆ |
|---|---|---|---|---|---|---|---|
| Step 1 | .20* | .20* | |||||
| Wave | 0.06 | 0.04 | .10 | 1.43 | .155 | ||
| Site 2 vs. Site 1 | −0.46 | 0.23 | −.24 | −2.01 | .046* | ||
| Site 3 vs. Site 1 | −1.31 | 0.24 | −.65 | −5.56 | <.001* | ||
| Site 4 vs. Site 1 | −0.83 | 0.27 | −.30 | −3.12 | .002* | ||
| Site 5 vs. Site 1 | −0.88 | 0.24 | −.40 | −3.63 | <.001* | ||
| Step 2 | .25 | .06 | |||||
| Wave | 0.08 | 0.05 | .14 | 1.74 | .083 | ||
| Site 2 vs. Site 1 | −.039 | 0.24 | −.21 | −1.63 | .105 | ||
| Site 3 vs. Site 1 | −1.23 | 0.25 | −.61 | −5.04 | <.001 | ||
| Site 4 vs. Site 1 | −0.85 | 0.28 | −.31 | −3.07 | .003 | ||
| Site 5 vs. Site 1 | −0.89 | 0.25 | −.41 | −3.55 | <.001 | ||
| BECCI 1 | −0.09 | 0.15 | −.05 | −0.66 | .513 | ||
| BECCI 2 | 0.05 | 0.06 | .05 | 0.73 | .464 | ||
| BECCI 3 | −0.11 | 0.09 | −.10 | −1.24 | .217 | ||
| BECCI 4 | −0.04 | 0.08 | −.04 | −0.48 | .632 | ||
| BECCI 5 | −0.13 | 0.11 | −.10 | −1.20 | .231 | ||
| BECCI 6 | −0.08 | 0.08 | −.09 | −1.10 | .271 | ||
| BECCI 7 | 0.22 | 0.14 | .10 | 1.52 | .131 | ||
| BECCI 8 | 0.15 | 0.07 | .16 | 2.12 | .035* | ||
| BECCI 9 | −0.05 | 0.08 | −.06 | −0.62 | .539 | ||
| BECCI 10 | 0.00 | 0.08 | .00 | 0.05 | .958 | ||
| BECCI 11 | 0.03 | 0.05 | .04 | 0.53 | .595 |
BECCI Behavior Change Counseling Index.
*p < .05.
Patient-rated alliance
In Step 1 of the regression (presented in Table 5), site and wave were found to account for 2.8% of the variance in patient-rated alliance (p =.382). After entry of all Behavior Change Counseling Index items at Step 2, the total variance explained by the model as a whole was 8.1% (p = .506). The Behavior Change Counseling Index items explained an additional 5.3% of the variance in patient-rated alliance, after controlling for site and wave; however, this increase was not significant (p = .531). In the final model, none of the individual Behavior Change Counseling Index items were statistically significantly associated with patient-rated alliance.
Table 5.
Hierarchical multiple regression analysis predicting patient-rated alliance
| Variable | B | SE B | β | t | p | R 2 | R 2∆ |
|---|---|---|---|---|---|---|---|
| Step 1 | .03 | .03 | |||||
| Wave | 0.00 | 0.33 | .00 | 0.03 | .998 | ||
| Site 2 vs. Site 1 | −0.14 | 0.20 | −.10 | −0.72 | .473 | ||
| Site 3 vs. Site 1 | −0.26 | 0.20 | −.17 | −1.30 | .199 | ||
| Site 4 vs. Site 1 | −0.18 | 0.23 | −.09 | −0.79 | .429 | ||
| Site 5 vs. Site 1 | −0.40 | 0.21 | −.24 | −1.92 | .056 | ||
| Step 2 | .08 | .05 | |||||
| Wave | 0.03 | 0.04 | .07 | 0.82 | .413 | ||
| Site 2 vs. Site 1 | −0.11 | 0.21 | −.07 | −0.51 | .613 | ||
| Site 3 vs. Site 1 | −0.17 | 0.21 | −.11 | −0.81 | .417 | ||
| Site 4 vs. Site 1 | −0.21 | 0.24 | −.10 | −0.88 | .380 | ||
| Site 5 vs. Site 1 | −0.39 | 0.22 | −.23 | −1.80 | .074 | ||
| BECCI 1 | 0.09 | 0.12 | .06 | 0.74 | .457 | ||
| BECCI 2 | 0.05 | 0.05 | .07 | 0.98 | .328 | ||
| BECCI 3 | −0.03 | 0.08 | −.03 | −0.35 | .724 | ||
| BECCI 4 | 0.00 | 0.07 | .00 | 0.04 | .971 | ||
| BECCI 5 | −0.16 | 0.09 | −.16 | −1.80 | .073 | ||
| BECCI 6 | −0.03 | 0.06 | −.05 | −0.52 | .602 | ||
| BECCI 7 | 0.11 | 0.12 | .07 | 0.91 | .365 | ||
| BECCI 8 | −0.03 | 0.06 | −.04 | −0.49 | .626 | ||
| BECCI 9 | −0.00 | 0.07 | −.00 | −0.04 | .966 | ||
| BECCI 10 | −0.03 | 0.07 | −.04 | −0.46 | .644 | ||
| BECCI 11 | −0.03 | 0.05 | −.07 | −0.71 | .479 |
BECCI Behavior Change Counseling Index.
*p < .05.
Discussion
The primary aim of the present study was to evaluate whether training dietitians in a motivational interviewing informed health behavior change intervention (EAT) resulted in higher levels of therapeutic alliance between dietitians and their patients. It was hypothesized that alliance (as rated by both dietitians and patients) would be higher in the intervention phase of the study compared with the control phase. Although we did see a significant increase in dietitian demonstration of motivational interviewing consistent skills, contrary to expectation, a corresponding increase in therapeutic alliance was not observed. Rather, we found that dietitian-rated alliance remained stable and ratings of therapeutic alliance may have been lower for patients in the intervention relative to the control phase. Regarding our secondary aim of exploring whether discrete motivational interviewing skills predicted therapeutic alliance, only one of the 11 skills assessed emerged as a significant predictor—of dietitian- (but not patient-) rated alliance.
Therapeutic Alliance and the EAT Intervention
The observed disparity between clinician and client ratings of therapeutic alliance is common, and consistent with the low to moderate relationship typically observed [44]. As per evidence suggesting a level of divergence in ratings of therapeutic alliance depending on the perspective of the rater (clinician vs. client vs. observer [44, 45]), our findings suggest that training dietitians in the EAT intervention had a differential impact on dietitian and patient perception of the therapeutic alliance. Of note, prior research has demonstrated that in-session difficulties experienced by the clinician (e.g., anxiety, negative reactions to patients) can affect patient but not clinician ratings of therapeutic alliance [46]. Conversely, in-session “flow” (feeling stimulated, inspired, and engrossed) can improve clinician-rated alliance, but client ratings remain unchanged [46]. As perceived skill [47] and clinician confidence [48] have been linked to positive client ratings of therapeutic alliance [47], it is reasonable to extrapolate that changes in clinician anxiety and/or confidence when working within the new paradigm of EAT may have contributed to the observed (albeit minor) reduction in patient-rated alliance. Indeed, exploratory post hoc analyses demonstrated that intervention patients felt less confident in their dietitian and felt their dietitian was less confident in their own skills. It is also interesting to consider whether changes in clinician anxiety and/or confidence would have influenced the perceived “flow” of sessions, thereby preventing the expected increase in dietitian-rated alliance.
Of note, the strength of the supervisory relationship can have a powerful and positive impact on clinician rating of therapeutic alliance (e.g., by reducing anxiety and/or increasing self-efficacy [49]). Given that supervision was integral to training in the current trial, it is also possible that difficulties in the supervisory relationship contributed to our inability to detect the expected increase in dietitian-rated alliance. We suspect that this is unlikely the case (given the observed high ratings of therapeutic alliance), but nonetheless is an important consideration for future research. In summary, further research is needed to understand how best to prevent unintended consequences of training from undermining therapeutic alliance—especially since therapeutic alliance can have a profound impact on client outcome [1].
EAT techniques (and/ or their delivery) may also have contributed to the possible reduction in patient-rated alliance during the intervention phase. Although motivational interviewing can enhance alliance [24, 33, 34], certain techniques may have a less faciliatory role. Specifically, as the overall focus of the parent EAT trial was patient behavior change (not alliance improvement), one of the techniques used during the intervention phase to facilitate change was highlighting any discrepancy between the patients’ current nutrition-related behavior(s) and their overall goal of survival (the “Eat to Live” conversation). It is important that this conversation is held in a way that does not confront the patient and undermine the spirit of motivational interviewing [23]. As this conversation was exclusive to the intervention phase, if dietitians had difficulty with this, intervention patients may have felt less supported than their control counterparts and therefore rated alliance lower. Conversely, the natural (and expected) discomfort that arises when a discrepancy is highlighted [23], although useful to promote change [50], may adversely affect how supported the patient feels.
Indeed, post hoc analyses suggest that patients in the intervention phase rated their dietitians lower on the therapeutic alliance item relating to dietitian supportiveness. Accordingly, our findings may reflect either the negative impact of “confrontation” on patient-rated therapeutic alliance—an effect observed after as few as two instances of this behavior [24] or the natural discomfort that arises when a discrepancy is strategically highlighted [23]. Either way, it points to the importance of better understanding the factors that may contribute to therapist use of “confrontation” and/or undermine the spirit of motivational interviewing with a view to not only minimize this behavior, but also how best to identify and address potential ruptures in therapeutic alliance (especially when delivering an unfamiliar/new intervention).
The role of measurement issues also needs to be considered. The Agnew Relationship Measure—Five Item Version was chosen for the present trial given its brevity, to limit the burden placed on patients completing numerous questionnaires as part of the parent EAT trial. However, two of the five items refer to confidence. Therefore, if patient-rated alliance is already sensitive to changes in clinician anxiety/confidence [46], the Agnew Relationship Measure—Five Item Version may not provide the most accurate assessment of therapeutic alliance—especially in settings where clinicians have been trained to deliver new practice techniques. Accordingly, future research that involves clinician training may be better served by an alliance measure less dependent on confidence, such as the 6-item Session Alliance Inventory [51]. Objective assessment of the supervisor–supervisee relationship is also an important consideration for future research.
Discrete Skills and Therapeutic Alliance
Contrary to evidence linking both patient centered communication (e.g., active listening and open-ended questions [52]) and motivational interviewing-related variables (e.g., exploration, reflection, responsiveness, and flexibility) to positive therapeutic alliance [15], we found little evidence to suggest that increased application of individual motivational interviewing skills benefitted the therapeutic alliance. Of the 11 skills assessed, we found that dietitian acknowledgment of patient challenges was the only skill to be associated with improved alliance (at least as rated by dietitians). Within oncology, there is evidence to suggest that clinician ratings of therapeutic alliance are more strongly influenced by “bond” relative to client ratings [53]. We can therefore speculate that in the current trial, being attentive to patient experience in this manner may have served to strengthen dietitian-rated therapeutic alliance by enhancing the perceived bond with their patient. However, further research is needed.
Findings from addiction treatment settings suggest that it may be the overall “spirit” of motivational interviewing, relative to discrete motivational interviewing consistent skills that is most strongly related to therapeutic alliance [24, 34]. Indeed, as per the current findings, prior research has demonstrated that motivational interviewing–consistent communication skills (e.g., affirming, asking open questions, reflecting, and summarizing) were not significant predictors of therapeutic alliance—as indexed either by observer [24, 34] or client-rated indices [33]. Rather, it was the interpersonal elements of motivational interviewing, the “spirit” (e.g., empathy, acceptance, respect, warmth, genuineness, and collaboration)—a variable not directly assessed by the Behavior Change Counseling Index [42] that had a profound influence on therapeutic alliance [24, 34]. This finding may be of particular relevance when interpreting the current results due to the high prevalence of substance misuse within adults diagnosed with head and neck cancer (e.g., Ref. 54). Other notable predictors of therapeutic alliance that may help explain the remaining variation in patient and dietitian ratings of alliance include attachment style [55, 56], clinician skill/ competence [57], and patient adherence to treatment [7]. Evidently, further information is needed to clarify the relative contribution of intervention elements, clinician variables, and patient characteristics to the therapeutic alliance—especially within healthcare settings outside of addiction.
Strengths and Limitations
To the best of our knowledge, this is the first large-scale, multisite assessment of therapeutic alliance between real-world oncology dietitians and their patients. Therapeutic alliance was assessed under conditions of both routine care and following training in a health behavior change intervention. We therefore contribute unique insight into the relationship between clinician behavior change and therapeutic alliance within a real-world setting. We also addressed several methodological issues noted in previous alliance research. Firstly, alliance has typically been measured at only one point in time, thereby limiting the dependability of the measurement since alliance fluctuates over time [5, 9]. Accordingly, in the current study, alliance was assessed at four key therapeutic intervals. Secondly, assessment of therapeutic alliance (particularly within medical settings) tends to focus on the perspective of the client [53]. As the level of agreement between client and clinician ratings may influence the outcome of psychological interventions [58], it is important to consider both perspectives. To the best of our knowledge, within medical settings, ours is one of the first studies [alongside [53]] to assess therapeutic alliance from both sides of the therapeutic encounter. Finally, our assessment of clinician behavior (i.e., application of motivational interviewing skills) is derived from the gold standard method [59] of independent, observer ratings of audio recorded consultations using a validated assessment tool (the Behavior Change Counseling Index).
Although of benefit for informing real-world practice, the translational design of the current study also meant that some dietitians only took part in one (not both) of the trial phases. Accordingly, between-group differences on dietitian characteristics (such as previous training or experience) may have obscured or confounded results. This is an artifact of conducting research in a real-world setting, and it is hoped that any loss of internal validity in the study is offset by the enhanced generalizability of the results. Our findings, like much of the alliance literature [33], may also be complicated by ceiling effects, with patients in both the control and intervention groups rating alliance very high (adjusted means 6.96 and 6.67, respectively, out of a possible seven). Although it is possible that these ratings accurately reflect the experience of alliance by patients and dietitians, the potential role of social desirability bias [60] must be acknowledged. However, despite the efforts of multiple research groups to reduce this effect, little progress has been made [11]. It is also important to acknowledge that the current study may or may not have been adequately powered for these secondary outcomes (power calculations were performed for the primary outcome of the original analysis). Accordingly the potential influence of type 2 error must be considered when interpreting the current pattern of results. Finally, although we did see a significant change in dietitian behavior during the week one sessions rated, the degree of change may have been insufficient to achieve overall consistency with motivational interviewing principles. Indeed, although a large effect of training on week one Behavior Change Counseling Index scores was apparent (eta squared = .250), inspection of the mean Behavior Change Counseling Index score (1.80) suggests that clinicians tended to implement skills between “minimally” and “to some extent” during their consultations (compared with higher ratings of “a good deal” or “a great extent”). In time, it is possible that with more practice (and possibly increased confidence), the dietitians might use the motivational interviewing techniques more often and alliance improve. Future research could evaluate if this is the case.
Implications and Future Directions
In conclusion, we did not find evidence to suggest that therapeutic alliance was improved by training dietitians in motivational interviewing techniques. Possible explanations for this include a lack of dietitian confidence in using the new techniques, the ceiling effects evident in the alliance data, and the natural discomfort that arises when clinicians strategically “develop discrepancy.” Although patient ratings of alliance were slightly lower in the EAT phase compared with the control phase, this did not appear to be a clinically significant reduction (ratings during EAT were still very high), and the lower ratings may have been due to the choice of measurement instrument. Results did however show that the motivational interviewing technique of acknowledging patient challenges was significantly and positively related to dietitian-rated alliance, and thus would appear to be worthy of inclusion in any future efforts to foster therapeutic alliance. Further studies on the use of motivational interviewing (both overall spirit and individual techniques) by dietitians (and indeed clinicians more generally) to enhance alliance are warranted and should ensure the use of appropriate, sensitive alliance measures.
Acknowledgments
The current study is a secondary analysis of a trial (The EAT Trial) funded by the National Health and Medical Research Council of Australia (APP1021018; 2011/ 3654).
Compliance With Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Rebecca Murray, Amanda Baker, Sean Halpin, Ben Britton, Kristen McCarter, Kerrin Palazzi, and Alison K. Beck declare that they have no conflict of interest.
Authors’ Contributions Rebecca conducted the study and drafted the manuscript in partial fulfillment of the requirements for a Masters of Clinical Psychology degree, under the supervision of Amanda and Sean (i.e. all made substantial contributions to conception, design, acquisition of data and manuscript preparation). Ben and Kristen made significant contributions to study conception and design. Kerrin made significant contributions to the analysis of data. Alison made significant contributions to the study design, interpretation of study findings and critically revising the manuscript. All authors contributed to the revision of the manuscript and gave final approval of the version to be published.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Coordinating ethics for The EAT Trial was granted by Hunter New England Health (HREC/12/HNE/108; HNEHREC: 12/04/18/4.06). Approval was also received from the following committees: Central Adelaide Local Health Network (HREC/13/RAH/75; SSA/13/RAH/102); Sir Charles Gairdner Group HREC (2012-136); Peter MacCallum Cancer Center Ethics (SSA/13/PMCC/19); Western Sydney Local Health District Research Governance (SSA/13/WMEAD/110); Metro South Hospital and Health Service (SSA/13/QPAH/240 and SSA/13/QPAH/241).
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy (Chic). 2011; 48:9–16. [DOI] [PubMed] [Google Scholar]
- 2. Castonguay LG, Constantino MJ, Holtforth MG. The working alliance: Where are we and where should we go?Psychotherapy (Chic). 2006;43:271–279. [DOI] [PubMed] [Google Scholar]
- 3. Horvath AO. The alliance. Psychother Theor Res Pract Train. 2001;38:365–372. [Google Scholar]
- 4. Wampold BE, Imel ZE.. The Great Psychotherapy Debate: The Evidence for What Makes Psychotherapy Work. 2nd ed. New York: Routledge; 2015. [Google Scholar]
- 5. Ardito RB, Rabellino D. Therapeutic alliance and outcome of psychotherapy: Historical excursus, measurements, and prospects for research. Front Psychol. 2011;2:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Flückiger C, Del Re AC, Wampold BE, Symonds D, Horvath AO. How central is the alliance in psychotherapy? A multilevel longitudinal meta-analysis. J Couns Psychol. 2012;59:10–17. [DOI] [PubMed] [Google Scholar]
- 7. Fuertes JN, Toporovsky A, Reyes M, Osborne JB. The physician-patient working alliance: Theory, research, and future possibilities. Patient Educ Couns. 2017;100:610–615. [DOI] [PubMed] [Google Scholar]
- 8. Ferreira PH, Ferreira ML, Maher CG, Refshauge KM, Latimer J, Adams RD. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Phys Ther. 2013;93:470–478. [DOI] [PubMed] [Google Scholar]
- 9. The Dependability of Alliance Assessments: The Alliance–Outcome Correlation is Larger Than You Might Think [press release]. US: American Psychological Association; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sharpless BA, Muran CJ, Barber JP. Coda: Recommendations for practice and training. In: Muran JC, Barber JP, eds. The Therapeutic Alliance: An Evidence-Based Guide to Practice. New York: Guilford Press; 2010:341–354. [Google Scholar]
- 11. Bickman L, de Andrade AR, Athay MM, et al. . The relationship between change in therapeutic alliance ratings and improvement in youth symptom severity: Whose ratings matter the most?Adm Policy Ment Health. 2012;39:78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Samstag LW. The working alliance in psychotherapy: An overview of the invited papers in the special section. Psychotherapy (Chic). 2006;43:300–307. [DOI] [PubMed] [Google Scholar]
- 13. Baldwin SA, Wampold BE, Imel ZE. Untangling the alliance-outcome correlation: Exploring the relative importance of therapist and patient variability in the alliance. J Consult Clin Psychol. 2007;75:842–852. [DOI] [PubMed] [Google Scholar]
- 14. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theor Res Pract Train. 1979;16:252–260. [Google Scholar]
- 15. Ackerman SJ, Hilsenroth MJ. A review of therapist characteristics and techniques positively impacting the therapeutic alliance. Clin Psychol Rev. 2003;23:1–33. [DOI] [PubMed] [Google Scholar]
- 16. Norcross JC, Wampold BE. Evidence-based therapy relationships: Research conclusions and clinical practices. Psychotherapy (Chic). 2011;48:98–102. [DOI] [PubMed] [Google Scholar]
- 17. Crits-Christoph P, Gibbons MBC, Crits-Christoph K, Narducci J, Schamberger M, Gallop R. Can therapists be trained to improve their alliances? A preliminary study of alliance-fostering psychotherapy. Psychother Res. 2006;16:268–281. [Google Scholar]
- 18. Hilsenroth MJ, Ackerman SJ, Clemence AJ, Strassle CG, Handler L. Effects of structured clinician training on patient and therapist perspectives of alliance early in psychotherapy. Psychother Theor Res Pract Train. 2002;39:309–323. [Google Scholar]
- 19. Bambling M, King R, Raue P, Schweitzer R, Lambert W. Clinical supervision: Its influence on client-rated working alliance and client symptom reduction in the brief treatment of major depression. Psychother Res. 2006;16:317–331. [Google Scholar]
- 20. Preliminary Results of a Video-Assisted Psychotherapist Workshop in Alliance Strategies. US: Educational Publishing Foundation; 2011. doi: 10.1037/a0022184 [DOI] [PubMed] [Google Scholar]
- 21. Meystre C, Bourquin C, Despland JN, Stiefel F, de Roten Y. Working alliance in communication skills training for oncology clinicians: A controlled trial. Patient Educ Couns. 2013;90:233–238. [DOI] [PubMed] [Google Scholar]
- 22. Summers RF, Barber JP. Therapeutic alliance as a measurable psychotherapy skill. Acad Psychiatry. 2003;27: 160–165. [DOI] [PubMed] [Google Scholar]
- 23. Miller WR, Rollnick S.. Motivational Interviewing: Helping People Change. 3rd ed. New York: Guildford Press; 2013. [Google Scholar]
- 24. Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS. Using motivational interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance?J Subst Abuse Treat. 2006;31:329–339. [DOI] [PubMed] [Google Scholar]
- 25. Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–312. [PMC free article] [PubMed] [Google Scholar]
- 26. Heckman CJ, Egleston BL, Hofmann MT. Efficacy of motivational interviewing for smoking cessation: A systematic review and meta-analysis. Tob Control. 2010;19:410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. O’Halloran PD, Blackstock F, Shields N, et al. . Motivational interviewing to increase physical activity in people with chronic health conditions: A systematic review and meta-analysis. Clin Rehabil. 2014;28:1159–1171. [DOI] [PubMed] [Google Scholar]
- 28. VanBuskirk KA, Wetherell JL. Motivational interviewing with primary care populations: A systematic review and meta-analysis. J Behav Med. 2014;37:768–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lundahl B, Moleni T, Burke BL, et al. . Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. 2013;93:157–168. [DOI] [PubMed] [Google Scholar]
- 30. Rollnick S, Allison J, Ballasiotes S, et al. . Variations on a theme: Motivational interviewing and its adaptations. In: Miller WR, Rollnick S, eds. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002:270–283. [Google Scholar]
- 31. Kelly TM. The therapeutic alliance and psychosocial interventions for successful treatment of addiction. Psychiatr Times. 2015;32:33–36. [Google Scholar]
- 32. Zerler H. Motivational interviewing and suicidality. In: Arkowitz H, Westra HA, Miller WR, Rollnick S, eds. Motivational Interviewing in the Treatment of Psychological Problems. New York: Guildford Press; 2008:173–193. [Google Scholar]
- 33. Crits-Christoph P, Gallop R, Temes CM, et al. . The alliance in motivational enhancement therapy and counseling as usual for substance use problems. J Consult Clin Psychol. 2009;77:1125–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moyers TB, Miller WR, Hendrickson SML. How does motivational interviewing work? Therapist interpersonal skill predicts client involvement within motivational interviewing sessions. J Consult Clin Psychol. 2005;73:590–598. [DOI] [PubMed] [Google Scholar]
- 35. Britton B, McCarter K, Baker A, et al. . Eating As Treatment (EAT) study protocol: A stepped-wedge, randomised controlled trial of a health behaviour change intervention provided by dietitians to improve nutrition in patients with head and neck cancer undergoing radiotherapy. BMJ Open. 2015;5:e008921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Britton B, Baker A, Clover K, McElduff P, Wratten C, Carter G. Heads up: A pilot trial of a psychological intervention to improve nutrition in head and neck cancer patients undergoing radiotherapy. Eur J Cancer Care. In Press; 2017. doi: 10.1111/ecc.12502. [DOI] [PubMed] [Google Scholar]
- 37. Gorenc M, Kozjek NR, Strojan P. Malnutrition and cachexia in patients with head and neck cancer treated with (chemo)radiotherapy. Rep Pract Oncol Radiother. 2015;20:249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials. 2007;28:182–191. [DOI] [PubMed] [Google Scholar]
- 39. Beck AK, Baker A, Britton B, et al. . Fidelity considerations in translational research: Eating as treatment–a stepped wedge, randomised controlled trial of a dietitian delivered behaviour change counselling intervention for head and neck cancer patients undergoing radiotherapy. Trials. 2015;16:465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cahill J, Stiles WB, Barkham M, et al. . Two short forms of the agnew relationship measure: The ARM-5 and ARM-12. Psychother Res. 2012;22:241–255. [DOI] [PubMed] [Google Scholar]
- 41. Stiles WB, Agnew-Davies R, Barkham M, et al. . Convergent validity of the agnew relationship measure and the working alliance inventory. Psychol Assess. 2002;14:209–220. [DOI] [PubMed] [Google Scholar]
- 42. Lane C, Huws-Thomas M, Hood K, Rollnick S, Edwards K, Robling M. Measuring adaptations of motivational interviewing: The development and validation of the behavior change counseling index (BECCI). Patient Educ Couns. 2005;56:166–173. [DOI] [PubMed] [Google Scholar]
- 43. Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28:19–26. [DOI] [PubMed] [Google Scholar]
- 44. Shick Tryon G, Collins Blackwell S, Felleman Hammel E. A meta-analytic examination of client–therapist perspectives of the working alliance. Psychother Res. 2007;17:629–642. [Google Scholar]
- 45. Berry K, Gregg L, Hartwell R, Haddock G, Fitzsimmons M, Barrowclough C. Therapist-client relationships in a psychological therapy trial for psychosis and substance misuse. Drug Alcohol Depend. 2015;152:170–176. [DOI] [PubMed] [Google Scholar]
- 46. Nissen-Lie HA, Havik OE, Høglend PA, Rønnestad MH, Monsen JT. Patient and therapist perspectives on alliance development: Therapists’ practice experiences as predictors. Clin Psychol Psychother. 2015;22:317–327. [DOI] [PubMed] [Google Scholar]
- 47. Bachelor A. Clients’ and therapists’ views of the therapeutic alliance: Similarities, differences and relationship to therapy outcome. Clin Psychol Psychother. 2013;20:118–135. [DOI] [PubMed] [Google Scholar]
- 48. De Vries AM, de Roten Y, Meystre C, Passchier J, Despland JN, Stiefel F. Clinician characteristics, communication, and patient outcome in oncology: A systematic review. Psychooncology. 2014;23:375–381. [DOI] [PubMed] [Google Scholar]
- 49. Kristina DM, LG W, Ren L, Jessica G. Investigating supervisory relationships and therapeutic alliances using structural equation modeling. Couns Educ Superv. 2016;55:263–277. [Google Scholar]
- 50. Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Falkenström F, Hatcher RL, Skjulsvik T, Larsson MH, Holmqvist R. Development and validation of a 6-item working alliance questionnaire for repeated administrations during psychotherapy. Psychol Assess. 2015;27:169–183. [DOI] [PubMed] [Google Scholar]
- 52. Pinto RZ, Ferreira ML, Oliveira VC, et al. . Patient-centred communication is associated with positive therapeutic alliance: A systematic review. J Physiother. 2012;58:77–87. [DOI] [PubMed] [Google Scholar]
- 53. Bar-Sela G, Mitnik I, Lulav-Grinwald D. Perceptions of the working alliance among medical staff and cancer patients. Palliat Support Care. 2016;14:199–203. [DOI] [PubMed] [Google Scholar]
- 54. Maasland DH, van den Brandt PA, Kremer B, Goldbohm RA, Schouten LJ. Alcohol consumption, cigarette smoking and the risk of subtypes of head-neck cancer: Results from the Netherlands Cohort Study. BMC Cancer. 2014;14:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Steel C, Macdonald J, Schroder T. A systematic review of the effect of therapists’ internalized models of relationships on the quality of the therapeutic relationship. J Clin Psychol. 2018;74:5–42. [DOI] [PubMed] [Google Scholar]
- 56. Smith AE, Msetfi RM, Golding L. Client self rated adult attachment patterns and the therapeutic alliance: A systematic review. Clin Psychol Rev. 2010;30:326–337. [DOI] [PubMed] [Google Scholar]
- 57. McGuire AB, White DA, Bartholomew T, et al. . The relationship between provider competence, content exposure, and consumer outcomes in illness management and recovery programs. Adm Policy Ment Health. 2017;44:81–91. [DOI] [PubMed] [Google Scholar]
- 58. Marmarosh CL, Kivlighan DM Jr. Relationships among client and counselor agreement about the working alliance, session evaluations, and change in client symptoms using response surface analysis. J Couns Psychol. 2012;59:352–367. [DOI] [PubMed] [Google Scholar]
- 59. Bellg AJ, Borrelli B, Resnick B, et al. ; Treatment Fidelity Workgroup of the NIH Behavior Change Consortium. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH behavior change consortium. Health Psychol. 2004;23:443–451. [DOI] [PubMed] [Google Scholar]
- 60. Joosten E, de Weert G, Sensky T, van der Staak C, de Jong C. Effect of shared decision-making on therapeutic alliance in addiction health care. Patient Prefer Adherence. 2008;2:277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]