Abstract
Background:
The purpose of this study is to evaluate the rate of dysphagia between zero-profile spacer versus cage-plate for the treatment of multilevel cervical spondylotic myelopathy (CSM).
Methods:
The authors searched electronic databases for relevant studies that compared the clinical effectiveness of zero-profile spacer versus cage-plate for the treatment of patients with multilevel CSM. The following outcome measures were extracted: the Japanese Orthopaedic Association (JOA) scores, Neck Disability Index (NDI) score and fusion rate, dysphagia rate, adjacent segment degeneration, and cervical lordosis. Newcastle-Ottawa Quality Assessment Scale was used to evaluate the quality of each study. Data extraction and quality assessment were conducted, and RevMan 5.2 was used for data analysis.
Results:
A total of 10 studies were included in our meta-analysis. Our pooled data revealed that zero-profile spacer was associated with decreased dysphagia rate at postoperatively 1, 3, and 6 months, and the final follow-up when compared with cage-plate group. No significant difference was observed in terms of postoperative JOA score, NDI score, and fusion rate. Compared with zero-profile spacer, the postoperative adjacent segment degeneration was significant higher in cage-plate. Pooled data from the relevant studies revealed that cervical lordosis was significantly lower in zero-profile spacer compared with cage-plate.
Conclusions:
Our meta-analysis reveals zero-profile spacer is better than the cage-plate in terms of dysphagia. This suggests zero-profile spacer is a superior alternative invention for the treatment of multilevel CSM to reduce the risk of dysphagia.
Keywords: cage-plate, cervical spondylotic myelopathy, zero-profile spacer
1. Introduction
Cervical spondylotic myelopathy (CSM) is a clinically symptomatic condition associated with degeneration of intervertebral discs and adjacent vertebral structures. The degeneration of the intervertebral disc, uncovertebral joint, facet joint, posterior longitudinal ligament, and ligamentum flavum causes spinal cord compression and cervical myelopathy.[1] At present, patients diagnosed with single-level symptomatic CSM were often recommended to receive anterior cervical decompression and fusion (ACDF).[2–5] However, ACDF for multilevel CSM means a long cervical plate and may be associated with longer operative times, and also complications such as breakage or loosening of plate and screws, trachea-esophageal injury, neurovascular injury, and postoperative dysphagia.[6,7]
To reduce the dysphagia complication, the zero-profile anchored spacer had been advocated for multilevel CSM. The device generally consists of a polyetheretherketone cage with self-locking clips or screws passing through the spacer into the endplates of the adjacent vertebral bodies.[8] Zero-profile cage utilizes an integrated, low-profile plate design to avoid plate-to-soft tissue impact, reducing dysphagia incidence and other plate-associated complications. Satisfactory clinical and fusion outcomes have been reported using this device in ACDF for multilevel CSM.[9]
There is, at present, no consensus concerning the superiority of zero-profile spacer versus cage-plate regarding the incidence of dysphagia in the treatment of multilevel CSM.[10,11] To further clarify controversies in the current literature, we performed present meta-analysis to evaluate the rate of dysphagia between zero-profile spacer versus cage-plate after ACDF for the patients with multilevel CSM.
2. Materials and methods
2.1. Search strategy and study selection
Electronic databases, including MEDLINE, EMBASE, Cochrane Controlled Trial Register, and ISI Web of Knowledge (all databases) were searched for relevant reports published up to May 31, 2018. The MeSH Terms and Other Term used for our searches included “anterior cervical fusion,” “anterior plate,” “anterior cervical discectomy and fusion,” “ACDF,” “interbody fusion,” “low profile,” “zero profile,” “zero-p,” “anchored fusion,” “anchored spacer device,” and “stand alone.” The conjunctions “AND” and “OR” were used during the literature retrieval. We restricted the language to English. Reference lists of all included studies were scanned to identify additional potentially relevant studies. Two reviewers independently screened the titles and abstracts of identified papers, and full-text copies of all potentially relevant studies were obtained.
2.2. Inclusion and exclusion criteria
Two authors reviewed the articles, including randomized controlled trials (RCTs) and retrospective or prospective studies, in detail. The inclusion criteria for this study were as follows: all patients with multilevel CSM undergoing ACDF involving 2 or more levels; studies involving 2 cervical fusion groups: zero-profile versus cage-plate; a follow-up time of no less than 12 months. The following articles were excluded: meeting abstracts, review articles, editorial comments, letters, technical reports, case reports, biomechanical studies, and animal experiments; studies that did not meet the inclusion criteria; articles considered as duplicate publications.
2.3. Quality assessment of included studies
Risk of bias assessment was performed using the checklist proposed by Cowley[12] for nonrandomized studies. The items were scored with “yes,” “no,” or “unclear.” A Furlan score of 6 or more out of a possible 12, or a Cowley score of 9 or more out of a possible 17, was considered to reflect “high methodological quality.” These studies were independently evaluated by 2 reviewers, and any discrepancies were resolved by discussion and consensus.
2.4. Data extraction
The data were extracted by 2 reviewers independently from each included study based on the following items: basic characteristics, including country, study design, age, enrolled number, and length of follow-up; function outcomes including postoperative Japanese Orthopedic Association (JOA) score, Neck Disability Index (NDI) score, and percentage of clinical success; radiological outcomes including postoperative total and segmental cervical lordosis, and disc height; complication types and complication rates. Any disagreement between the reviewers was resolved by discussion.
2.5. Data analysis
We performed all meta-analyses with the Review Manager software (RevMan Version 5.2; Cochrane Collaboration, Oxford, UK). Heterogeneity was tested using chi-square test and quantified by calculating I2 statistic, for which P < .1 and I2 < 50% was considered to be statistically significant. For the pooled effects, weighted mean difference (WMD) or standard mean difference (SMD) was calculated for continuous variables according to the consistency of measurement units, and odds ratio (OR) was calculated for dichotomous variables. Continuous variables are presented as mean differences and 95% confidence intervals (CIs), whereas dichotomous variables are presented as ORs and 95% CI. Random-effects or fixed-effects models were used depending on the heterogeneity of the studies included.
3. Results
The process of identifying relevant studies is summarized in Fig. 1. From the selected databases, 436 references were obtained. By screening the titles and abstracts, 415 references were excluded due to duplicates, irrelevant studies, case reports, not comparative studies, and review articles. The remaining potentially relevant 25 studies underwent a detailed and comprehensive evaluation. Finally, 10 studies were included in our meta-analysis.[13–22] The characteristics of these studies are summarized in Table 1.
Figure 1.
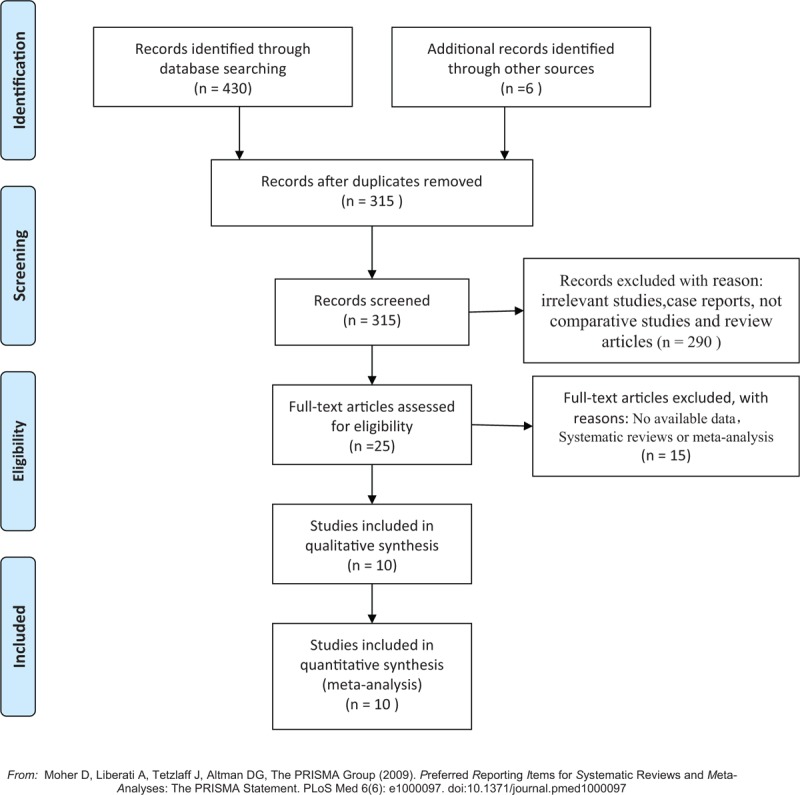
The flow chart shows the article selection process we performed.
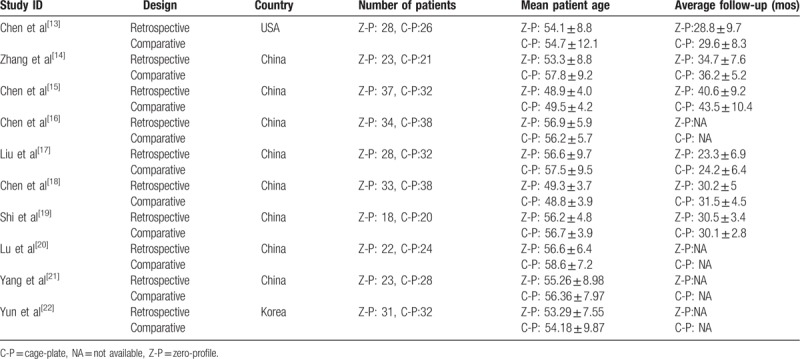
Table 1.
Characteristics of included studies.
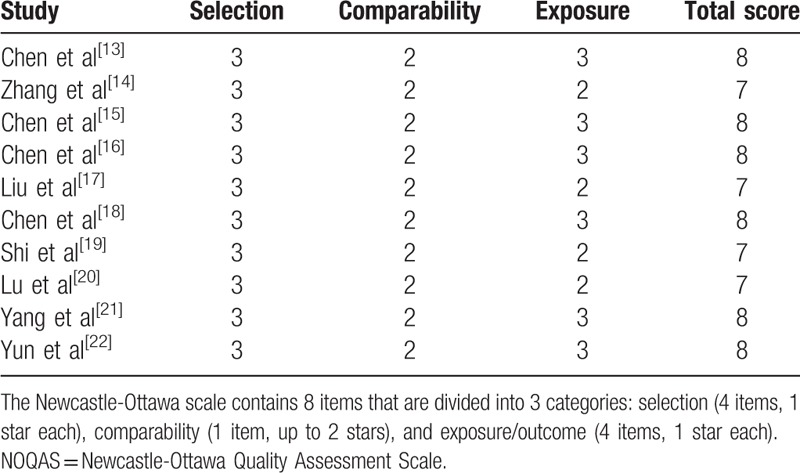
3.1. Quality assessment
Newcastle-Ottawa Quality Assessment Scale was used to evaluate the quality of each study. This scale for nonrandomized case controlled studies and cohort studies had a maximum of 9 points, which included the quality of selection, comparability, exposure, and outcomes for study participants. Of these studies, 6 scored 8 points and 4 scored 7 points. Therefore, the quality of each study was relatively high (Table 2).
Table 2.
Quality assessment of included studies in the meta-analysis according to NOQAS.
3.2. Clinical outcome
3.2.1. Postoperative JOA
Postoperative JOA scores were reported in 7 studies. No significant difference in postoperative visual analog scale score was found between zero-profile spacer and cage-plate groups (WMD −0.06; 95% CI −0.26, 0.13; I2 = 0%; P = .51) (Fig. 2).
Figure 2.
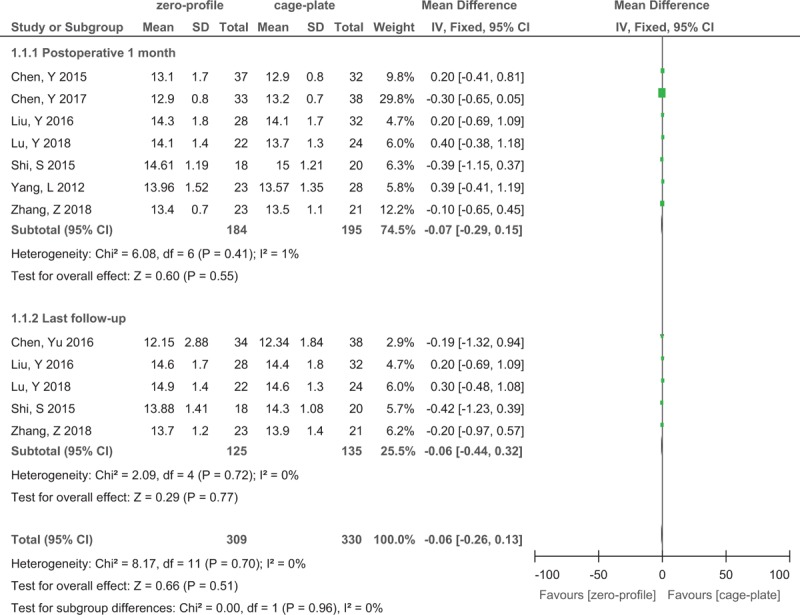
Forest plot of postoperative JOA scores between zero-profile spacer and cage-plate groups. JOA = Japanese Orthopaedic Association.
3.2.2. Postoperative NDI
Postoperative NDI were reported in 8 studies. There was no significant difference between zero-profile spacer and cage-plate groups (WMD −0.02; 95% CI −0.35, 0.32; I2 = 0%; P = .93) (Fig. 3).
Figure 3.
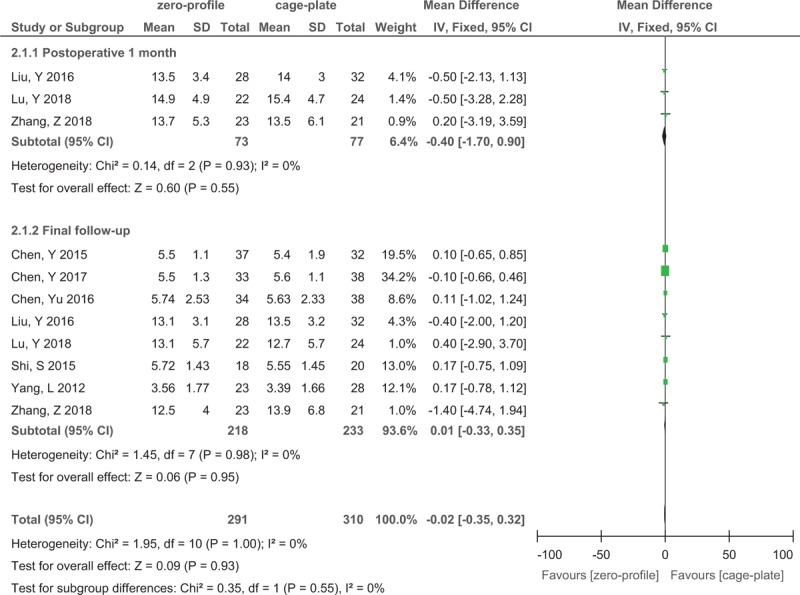
Forest plot of postoperative NDI between zero-profile spacer and cage-plate groups. NDI = Neck Disability Index.
3.2.3. Postoperative cervical lordosis
Postoperative cervical lordosis was reported in 10 studies. Pooled data from the 10 relevant studies revealed cervical lordosis was significantly lower in zero-profile spacer compared with cage-plate at final follow-up (WMD −0.87; 95% CI −1.73, −0.06; I2 = 26%; P = .04) (Fig. 4).
Figure 4.
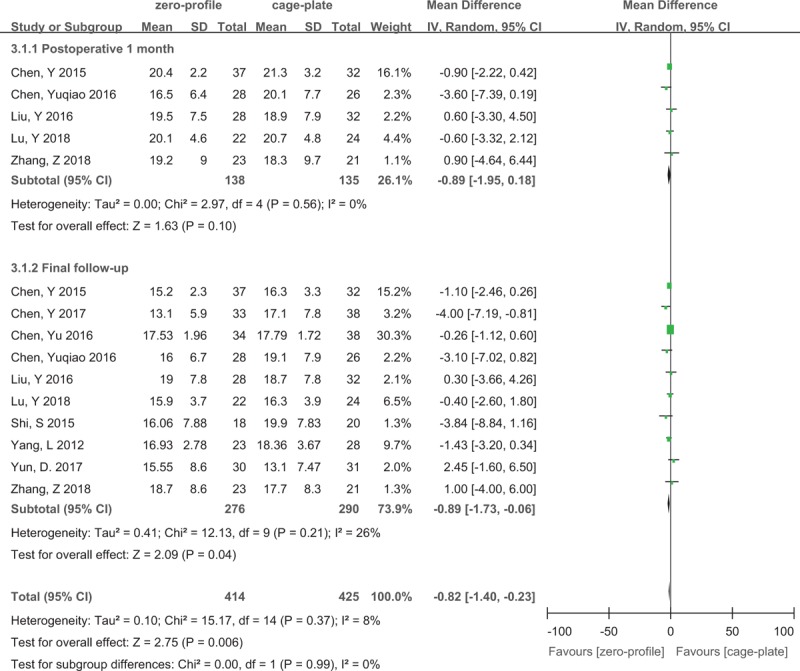
Forest plot of postoperative cervical lordosis between zero-profile spacer and cage-plate groups.
3.2.4. Fusion rate
Nine studies reported fusion rate. Pooled estimates revealed no significant difference between the 2 groups with no evidence of statistical heterogeneity (OR 0.77; 95% CI 0.35, 1.66; I2 = 0%; P = .5) (Fig. 5).
Figure 5.
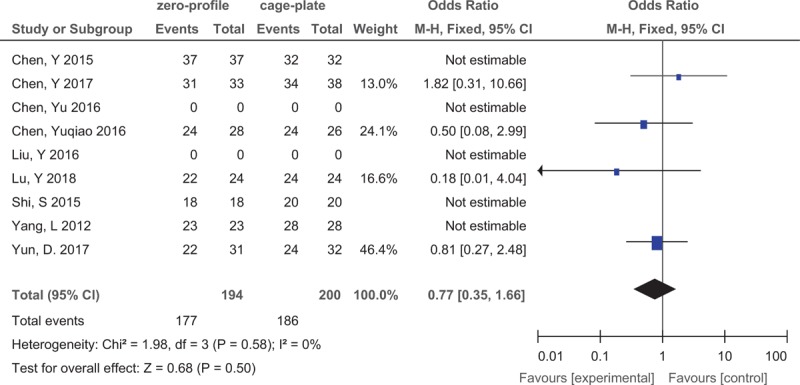
Forest plot of postoperative fusion rate between zero-profile spacer and cage-plate groups.
3.2.5. Adjacent segment degeneration
Five studies reported adjacent segment degeneration. Pooled data from the 5 relevant studies revealed a significant difference with no evidence of statistical heterogeneity (OR 0.44; 95% CI 0.2, 0.96; I2 = 0%; P = .04) (Fig. 6).
Figure 6.
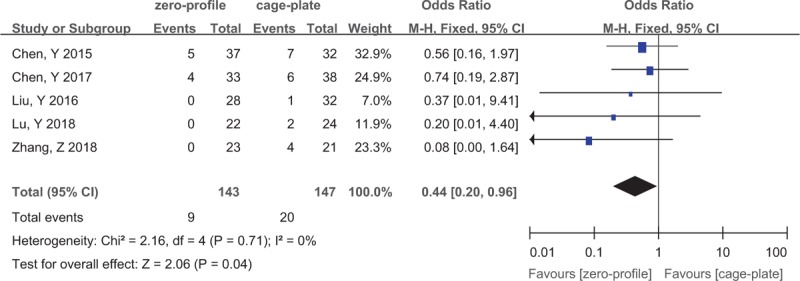
Forest plot of postoperative adjacent segment degeneration rate between zero-profile spacer and cage-plate groups.
3.2.6. Dysphagia
All studies reported dysphagia. Pooled data revealed no significant difference between the 2 groups in postoperative 48 hours (OR 0.67; 95% CI 0.41, 1.11; I2 = 0%; P = .12) (Fig. 7). However, pooled data from the relevant studies revealed that a significantly low rate was found in the zero-profile spacer group compared with cage-plate group with no evidence of statistical heterogeneity at postoperative 1 month (I2 = 0%; P = .002), 3 months (I2 = 0%; P = .0001), 6 months (I2 = 0%; P = .002), and the final follow-up (I2 = 34%; P = .004) (Fig. 7).
Figure 7.
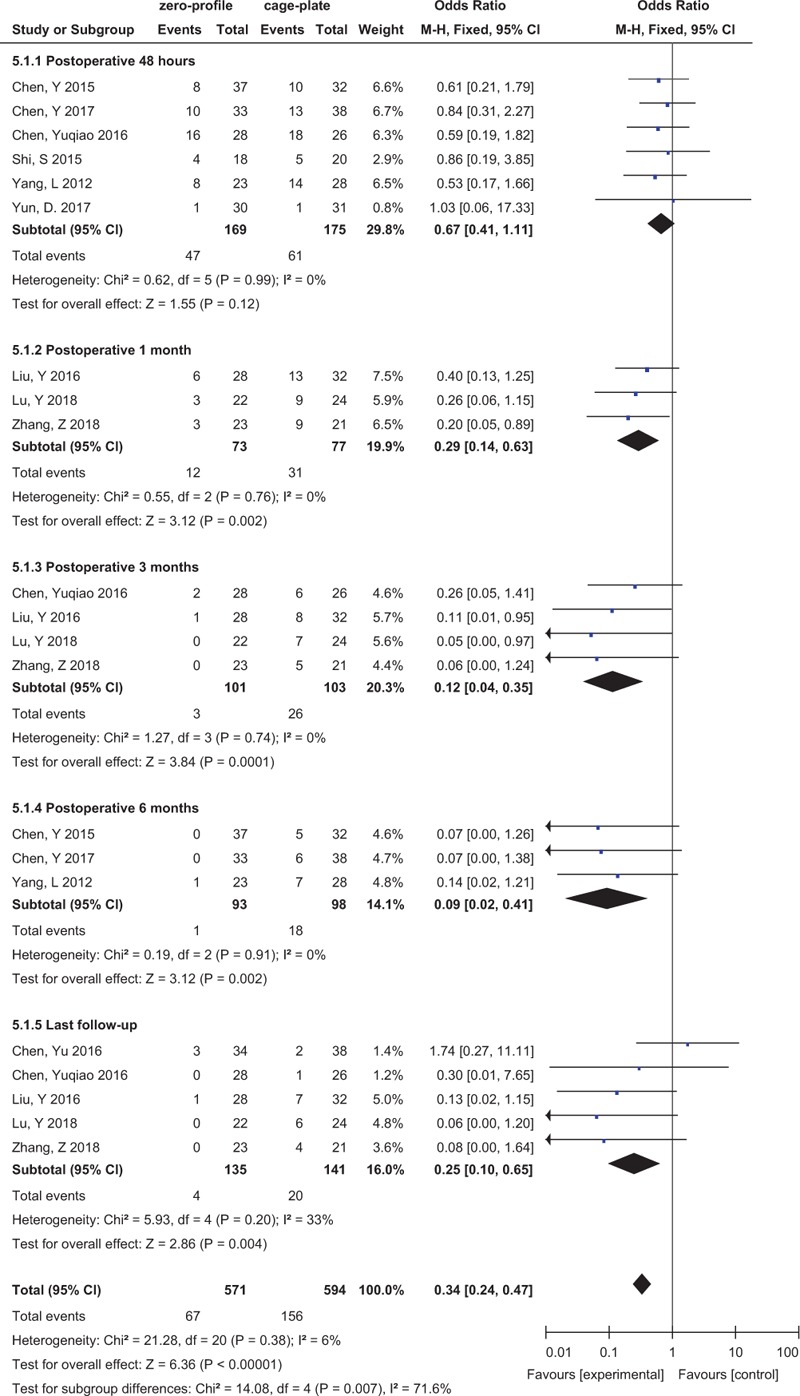
Forest plot of postoperative dysphagia rate between zero-profile spacer and cage-plate groups.
4. Discussion
Anterior cervical decompression and fusion has been commonly regarded as 1 of the gold-standard operation for CSM when conservative treatment fails.[23] An anterior cervical plate is widely used in ACDF to enhance the interbody fusion rate, and increase the cervical stability and avoid subsidence or graft dislocation.[24,25] However, the application of anterior cervical plate is closely associated with several postoperative complications including neck pain, hoarseness, and dysphagia. Zero-profile implant is a stand-alone anchored spacer designed to minimize these complications, simultaneously providing adequate stability and avoiding the implant contact with the anterior soft tissue.[8] Although several relevant studies comparing the zero-profile spacer and cage-plate have been reported,[13,14,17,18,20,22] it remains ambiguous on which method, zero-profile or cage-plate, is superior. Therefore, we conducted a meta-analysis to evaluate which device is the optimal implant for cervical fusion.
Our meta-analysis demonstrates that there was no significant difference in terms of postperative JOA score, NDI score, and fusion rate between zero-profile and cage-plate. Compared with cage-plate group, postoperative dysphagia rate was significantly lower in the zero-profile spacer group. Pooled data from the relevant studies revealed a significant difference in postoperative adjacent segment degeneration and cervical lordosis.
The JOA and NDI scores were often used to evaluate the improvement of nerve function. Our study shows that there was no statistically difference in JOA scores, and also NDI scores between zero-profile and cage-plate. Our findings are in line with previous studies confirming that surgical management of multilevel CSM by zero-profile or cage-plate shows no significant differences in terms of achieved nerve improvement.[26,27] Hence, these results suggest that both procedures can have sufficient decompression and improve the patients’ neurological function.
Dysphagia is 1 of the most concerning postoperative complication after ACDF with anterior plate fixation, especially after multilevel surgeries. The exact etiology of dysphagia remained unknown. Previous study reported that esophageal injury, postoperative soft tissue edema, adhesive formations around implanted cervical plates, and postoperative hematoma may be the possible reasons for dysphagia-related symptoms.[28,29] In addition, with the raise of fused segment, the risk of dysphagia increases.[10] Cho et al[30] found that the rate of postoperative dysphagia could be as high as 71% within the first 2 weeks after surgery, which gradually decreased during the following months. The results of this meta-analysis suggested that the zero-profile group was associated with lower incidence of dysphagia at postoperative 1, 3, and 6 months, and final follow-up, when compared with the cage-plate group. Recently, a meta-analysis performed by Tong et al[27] revealed that significantly lower dysphagia rates were observed in the zero-profile group at postoperative 2, 3, and 6 months. Our finding was comparable with previous studies.[27] However, our study revealed no significant difference between the 2 groups at postoperative 48 hours. At the early stage (2 weeks postoperatively), it could partly be attributed to longer intraoperative esophagus retraction time and greater retraction extent to fix the anterior plates.
We believe that our result of meta-analysis is affected by several reasons. Firstly, in this meta-analysis, most of the studies selected were not RCTs, although it did not influence the credibility of the results. Secondly, only 10 studies were included, and their sample sizes were relatively small. Finally, most studies originated from China, and there may be demography bias. Due to these limitations, the combined results of this meta-analysis should be cautiously accepted, and high-quality RCTs with long-term follow-up and large sample size are needed.
5. Conclusions
In conclusion, our meta-analysis reveals zero-profile spacer is better than the cage-plate in terms of dysphagia. This suggests zero-profile spacer is a superior alternative invention for the treatment of multilevel CSM to reduce the risk of dysphagia. This requires further validation and investigation in larger sample-size prospective and randomized studies.
Author contributions
Conceptualization: Zhongmeng Yang.
Data curation: Yao Zhao, Jiaquan Luo.
Formal analysis: Yao Zhao.
Investigation: Zhongmeng Yang, Jiaquan Luo.
Methodology: Zhongmeng Yang, Yao Zhao.
Supervision: Jiaquan Luo.
Writing – original draft: Zhongmeng Yang.
Writing – review & editing: Jiaquan Luo.
Footnotes
Abbreviations: ACDF = anterior cervical decompression and fusion, CI = confidence intervals, CSM = cervical spondylotic myelopathy, JOA = Japanese Orthopaedic Association, NDI = Neck Disability Index, RCT = randomized controlled trial, WMD = weighted mean difference.
ZY and YZ equally contributed to this work.
This study was supported by Natural Science Foundation of Tibet Autonomous Region (No. XZ2018ZRG-117), Zhuhai medical and health science and technology plan project P.R. China (No. 20171009E030008).
The authors declare that they have no competing interests.
References
- [1].Edwards CN, Riew KD, Anderson PA, et al. Cervical myelopathy: current diagnostic and treatment strategies. Spine J 2003;3:68–81. [DOI] [PubMed] [Google Scholar]
- [2].Lau D, Chou D, Mummaneni PV. Two-level corpectomy versus three-level discectomy for cervical spondylotic myelopathy: a comparison of perioperative, radiographic, and clinical outcomes. J Neurosurg Spine 2015;23:280–9. [DOI] [PubMed] [Google Scholar]
- [3].Guan L, Hai Y, Yang JC, et al. Anterior cervical discectomy and fusion may be more effective than anterior cervical corpectomy and fusion for the treatment of cervical spondylotic myelopathy. BMC Musculoskelet Disord 2015;16:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Luo J, Cao K, Huang S, et al. Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J 2015;24:1621–30. [DOI] [PubMed] [Google Scholar]
- [5].Quinn JC, Kiely PD, Lebl DR, et al. Anterior surgical treatment of cervical spondylotic myelopathy: review article. HSS J 2015;11:15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Shamji MF, Massicotte EM, Traynelis VC, et al. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Spine (Phila Pa 1976) 2013;38:S195–209. [DOI] [PubMed] [Google Scholar]
- [7].Liu Y, Hou Y, Yang L, et al. Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012;37:E1450–8. [DOI] [PubMed] [Google Scholar]
- [8].Scholz M, Reyes PM, Schleicher P, et al. A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976) 2009;34:156–60. [DOI] [PubMed] [Google Scholar]
- [9].Miao J, Shen Y, Kuang Y, et al. Early follow-up outcomes of a new zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech 2013;26:E193–7. [DOI] [PubMed] [Google Scholar]
- [10].Vanek P, Bradac O, Delacy P, et al. Anterior interbody fusion of the cervical spine with Zero-P spacer: prospective comparative study-clinical and radiological results at a minimum 2 years after surgery. Spine (Phila Pa 1976) 2013;38:E792–7. [DOI] [PubMed] [Google Scholar]
- [11].Wang Z, Jiang W, Li X, et al. The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J 2015;24:148–54. [DOI] [PubMed] [Google Scholar]
- [12].Cowley DE. Prostheses for primary total hip replacement. A critical appraisal of the literature. Int J Technol Assess Health Care 1995;11:770–8. [DOI] [PubMed] [Google Scholar]
- [13].Chen Y, Lu G, Wang B, et al. A comparison of anterior cervical discectomy and fusion (ACDF) using self-locking stand-alone polyetheretherketone (PEEK) cage with ACDF using cage and plate in the treatment of three-level cervical degenerative spondylopathy: a retrospective study with 2-year follow-up. Eur Spine J 2016;25:2255–62. [DOI] [PubMed] [Google Scholar]
- [14].Zhang Z, Li Y, Jiang W. A comparison of zero-profile anchored spacer (ROI-C) and plate fixation in 2-level noncontiguous anterior cervical discectomy and fusion- a retrospective study. BMC Musculoskelet Disord 2018;19:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chen Y, Chen H, Cao P, et al. Anterior cervical interbody fusion with the Zero-P spacer: mid-term results of two-level fusion. Eur Spine J 2015;24:1666–72. [DOI] [PubMed] [Google Scholar]
- [16].Chen Y, Chen H, Wu X, et al. Comparative analysis of clinical outcomes between zero-profile implant and cages with plate fixation in treating multilevel cervical spondilotic myelopathy: a three-year follow-up. Clin Neurol Neurosur 2016;144:72–6. [DOI] [PubMed] [Google Scholar]
- [17].Liu Y, Wang H, Li X, et al. Comparison of a zero-profile anchored spacer (ROI-C) and the polyetheretherketone (PEEK) cages with an anterior plate in anterior cervical discectomy and fusion for multilevel cervical spondylotic myelopathy. Eur Spine J 2016;25:1881–90. [DOI] [PubMed] [Google Scholar]
- [18].Chen Y, Liu Y, Chen H, et al. Comparison of curvature between the zero-P spacer and traditional cage and plate after 3-level anterior cervical discectomy and fusion: mid-term results. Clin Spine Surg 2017;30:E1111–6. [DOI] [PubMed] [Google Scholar]
- [19].Shi S, Liu Z, Li X, et al. Comparison of plate-cage construct and stand-alone anchored spacer in the surgical treatment of three-level cervical spondylotic myelopathy: a preliminary clinical study. Spine J 2015;15:1973–80. [DOI] [PubMed] [Google Scholar]
- [20].Lu Y, Bao W, Wang Z, et al. Comparison of the clinical effects of zero-profile anchored spacer (ROI-C) and conventional cage-plate construct for the treatment of noncontiguous bilevel of cervical degenerative disc disease (CDDD). Medicine 2018;97:e9808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Yang L, Gu Y, Liang L, et al. Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical diskectomy and fusion. Orthopedics 2012;35:e1503–10. [DOI] [PubMed] [Google Scholar]
- [22].Yun DJ, Lee SJ, Park SJ, et al. Use of a zero-profile device for contiguous 2-level anterior cervical diskectomy and fusion: comparison with cage with plate construct. World Neurosurg 2017;97:189–98. [DOI] [PubMed] [Google Scholar]
- [23].Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607–24. [PubMed] [Google Scholar]
- [24].Bose B. Anterior cervical instrumentation enhances fusion rates in multilevel reconstruction in smokers. J Spinal Disord 2001;14:3–9. [DOI] [PubMed] [Google Scholar]
- [25].Kaiser MG, Haid RJ, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002;50:229–36. 236-238. [DOI] [PubMed] [Google Scholar]
- [26].Xiao S, Liang Z, Wei W, et al. Zero-profile anchored cage reduces risk of postoperative dysphagia compared with cage with plate fixation after anterior cervical discectomy and fusion. Eur Spine J 2017;26:975–84. [DOI] [PubMed] [Google Scholar]
- [27].Tong MJ, Xiang GH, He ZL, et al. Zero-profile spacer versus cage-plate construct in anterior cervical diskectomy and fusion for multilevel cervical spondylotic myelopathy: systematic review and meta-analysis. World Neurosurg 2017;104:545–53. [DOI] [PubMed] [Google Scholar]
- [28].Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–7. [DOI] [PubMed] [Google Scholar]
- [29].Tasiou A, Giannis T, Brotis AG, et al. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg 2017;3:444–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cho SK, Lu Y, Lee DH. Dysphagia following anterior cervical spinal surgery: a systematic review. Bone Joint J 2013;95-B:868–73. [DOI] [PubMed] [Google Scholar]


