Abstract
To compare the efficacy of curettage and bone grafting combined with elastic intramedullary nailing (EIN) vs curettage and bone grafting in the treatment of long bone cysts in children and to clarify the necessity of using EIN in the treatment of bone cysts.
Sixty-two patients were involved in this study from Jan. 2009 to Sept. 2017 (43 males, 19 females; 27 humeri, 35 femurs); the patients were assigned to an EIN group, comprising 30 patients who underwent curettage and bone grafting combined with EIN, or to a non–elastic intramedullary nailing (NEIN) group, comprising 32 patients who underwent curettage and bone grafting alone. The prognosis of the 2 groups was assessed with reference to the standard of Capanna.
No statistically significant differences in sex, age, location, activity, pathological fracture, cyst volume, operative time and intraoperative blood loss were found between the 2 groups (P > .05). The effective rate was 90.0% in the EIN group and 68.8% in the NEIN group, and the difference was statistically significant (P < .05).
Compared to simple curettage and bone grafting, curettage and bone grafting combined with EIN treatment can significantly improve the prognosis of children with bone cysts. It is recommended that EIN be added to bone cyst curettage and bone grafting.
Keywords: bone cyst, bone grafting, elastic intramedullary nailing
1. Introduction
Simple bone cysts, also known as solitary bone cysts, are common benign bone cysts in children and adolescents. These cysts usually occur in extremity long-bone metaphyses. The average age of onset is 8 to 14 years old.[1–5] Simple bone cysts mostly occur in males, and the male-to-female ratio is 2:1 to 4:1[1–3,6,7]; pain caused by intercurrent pathological fracture is often the first symptom, and 63% to 87%[1,3] of cysts are combined with pathological fracture before surgery. According to the Neer evaluation criterion, bone cysts can be divided into a latent stage and an active stage, in which the active stage accounts for 37.9% to 57.9%. The prognosis of the active stage is often worse than that of the latent stage.[8–10] Although simple bone cysts are a benign disease, they often occur in the long bones of extremities and are easily combined with pathological fractures that lead to limb activity disorders. Therefore, it is urgent to explore a scientific and effective treatment.
At present, the treatment for simple bone cysts is mainly invasive therapy, including intracavitary injection therapy and operative treatment. Intracavitary injection therapy mainly includes hormone injection and autologous red bone marrow injection, and operative treatment mainly includes cyst-wall clearance, bone grafting, drilling decompression and intramedullary nail fixation. Single treatment or multiple treatments can be adopted. Among these approaches, curettage and bone grafting are common operative treatments; however, the postoperative effect is not satisfactory, and the reason may be related to the lack of continuous cystic cavity drainage after surgery. Elastic intramedullary nailing (EIN) has unique advantages: it not only can continue the drainage of the cystic cavity but also may effectively prevent pathological fracture or fracture displacement and reduce the immobile period of the affected limb. The aim of this study was to explore whether the use of EIN during curettage and bone grafting can effectively improve prognosis.
2. Materials and methods
2.1. Objective of the study
From Jan. 2009 to Sept. 2017, 62 children with bone cysts were recruited from the Children's Hospital affiliated with Chongqing Medical University. The operation methods were curettage and bone grafting combined with EIN or simple curettage and bone grafting. The postoperative follow-up time was from 12 to 93 months (27 months on average). The study was approved by the ethics committee of our hospital, and study subjects’ informed consent was obtained.
2.2. Study methods
2.2.1. Inclusion criteria
-
(1)
The cyst was a primary simple bone cyst;
-
(2)
No other treatment was performed before the operation (such as hormone injection, autologous red bone marrow injection, and drilling decompression);
-
(3)
The operative method was curettage + bone grafting or cyst curettage + bone grafting + EIN;
-
(4)
The bone cyst was confirmed by postoperative pathological examination;
-
(5)
The focus was located in the humerus or femur;
-
(6)
The age of onset was less than 18 years old;
-
(7)
The postoperative follow-up time was 1 year or more.
2.2.2. Surgical method and grouping
This study was divided into an EIN group and a non-elastic intramedullary nailing (NEIN) group.
The surgical methods of the NEIN group were as follows: after the administration of anesthesia, the children were maintained in the supine position and strictly sterilized and draped after location of the focus by the C-arm; the skin, subcutaneous tissue and deep fascia were incised, with attention paid to protecting the peripheral nerves. The periosteum and the focus were exposed layer by layer. The periosteum was gently peeled off to expose the cortex of the focus, followed by aspiration of the fluid in the cystic cavity for examination. The focal cortex was drilled, and a rectangular bone window was chiseled into the cyst wall; the cyst focus was cleared as far as possible without damaging the epiphysis. Next, the cyst wall was rinsed with a large amount of normal saline after inactivation with anhydrous alcohol, and the medullary cavity of the upper and lower sides of the cystic cavity was drilled through. The autogenous bone/allogeneic bone/artificial bone were arranged tightly along the gravity line of the trabecular bone to fill the cystic cavity, and the filling was satisfactory under the C-arm. After correctly counting the medical appliances, we used 1% povidone iodine and normal saline to clean the incision and sutured the wound layer by layer. Subcutaneous tissue and intracutaneous tissue were continuously sutured with the absorbable thread, 1 drainage tube was placed subcutaneously, and the brace was fixed externally.
The surgical method in the EIN group was similar to that in the NEIN group. After curettage and bone grafting, under direct vision, 1 or 2 elastic intramedullary nails (2.5 to 4.0 mm, Sanatmetal, Hungary) were inserted from the metaphysis, fixed to the medullary cavity and passed through the cystic cavity. The length and diameter of the elastic intramedullary nail were determined by measuring the humerus or femur on anteroposterior and lateral X-ray films before surgery. The diameter of the nails was selected such that 2 nails would occupy approximately two-thirds of the medullary canal[23] (or 1 nail would occupy approximately half of the medullary canal), and their tips did not damage the growth plates of the bones.
2.2.3. Evaluation criteria
Bone cysts were divided into an active stage and latent stage according to the Neer[11] criteria before the operation.
-
(1)
Active stage: the cyst was close to the epiphyseal line, and the distance was less than 0.5 cm;
-
(2)
Latent stage: the cyst was relatively far from the epiphyseal line, and the distance was more than 0.5 cm.
According to the criteria of Capanna,[12] the prognosis was divided into three categories: cured, partially healed and ineffective.
-
(1)
Cured: cystic cavities were completely filled with bone substance without any residue, accompanied by thickening of the bone cortex;
-
(2)
Partially healed: most of the cystic cavities were filled by bone substance and cured; the bone cortex margin was thickened, but a small part of the transparent areas remained;
-
(3)
Ineffective: relapse or no response, i.e., there was a large area of osteolysis, and the cortical bone in the cyst wall was thin or showed no obvious change in the cyst after treatment;
2.2.4. Evaluation content and methods
-
(1)
Preoperation: the patient sex, patient age, disease location, cyst volume (the cyst volume was measured and calculated by Gobel's method of measuring and calculating the volume of the bone tumor in pediatric sarcomas in 1987[13]), whether there was pathological fracture or not and other characteristics were obtained by case history and imaging data;
-
(2)
During the operation: operative time, intraoperative blood loss and operation methods were recorded.
-
(3)
Postoperation: whether there was wound infection, recurrent fracture, or a focused prognosis was determined through imaging, out-patient case reviews and telephone follow-up.
2.2.5. Statistical method
Statistical analyses were carried out with IBM SPSS statistics 19.0 for Windows (IBM Corp., Armonk, NY) The Wilcoxon rank sum test was used for orderly graded data of the postoperative curative effect. The chi-square test was used for categorical data of gender and location. Age, cyst volume, intraoperative blood loss, operative time and healing time and other measuring data were tested by two-independent-sample t-tests. P < .05 was considered statistically significant.
3. Results
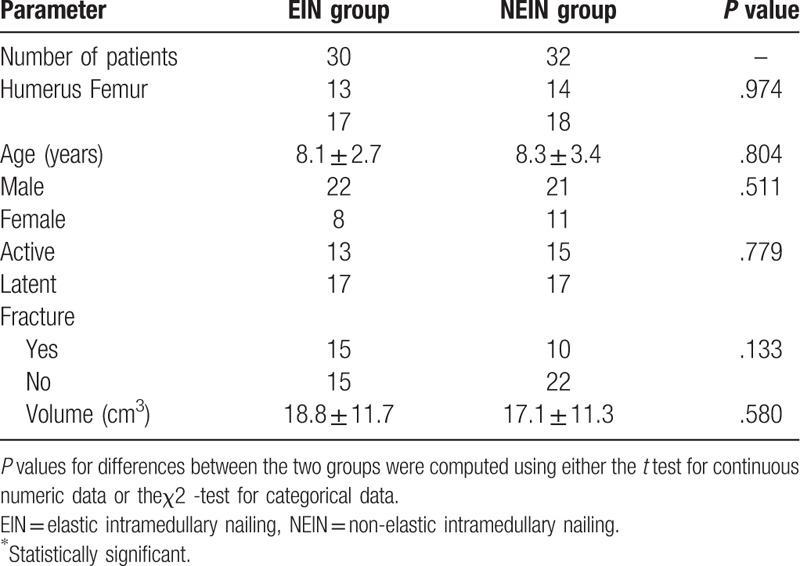
From Jan. 2009 to Sept. 2017, 62 patients in our hospital were treated with curettage and bone grafting with (or without) elastic intramedullary nails, and their postoperative pathological examination results confirmed the diagnosis of bone cysts. The patients were divided into an EIN group (n = 30) and NEIN group (n = 32), among which there were 22 males and 8 females in the EIN group and 21 males and 11 females in the NEIN group; an average age of 8.1 years in the EIN group and 8.3 years in the NEIN group. Thirteen humeral cysts and 17 femoral cysts were included in the EIN group, and 14 humeral cysts and 18 femoral cysts were included in the NEIN group. In the EIN group, 13 patients were at the latent stage, and 17 patients were at the active stage; in the NEIN group, 15 patients were at the latent stage, and 17 patients were at the active stage. There were 15 cases of pathological fracture and 15 cases of nonpathological fracture in the EIN group, and there were 10 cases of pathological fracture and 22 cases of nonpathological fracture in the NEIN group; the average cyst volume in the EIN group was 18.8 cm3, and that in the NEIN group was 17.1 cm3. There were no significant differences in sex, age, location, activity, pathological fracture, or cyst volume between the 2 groups (see Table 1).
Table 1.
Comparison of general data between the 2 groups of pediatric patients.
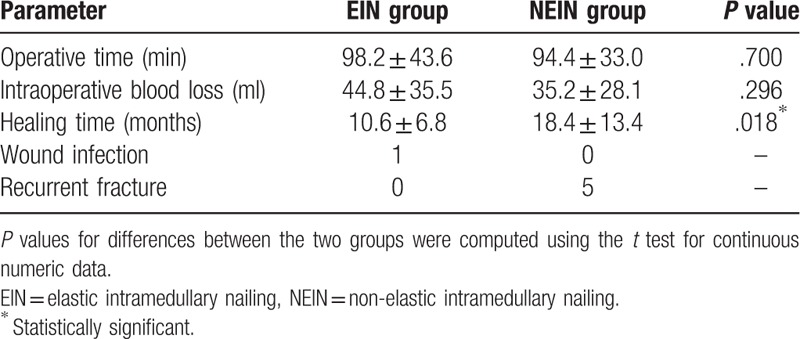
The average operative time was 98.2 minutes in the EIN group and 94.4 minutes in the NEIN group (P = .700); the intraoperative blood loss was 35.2 ml in the EIN group and 35.2 ml in the NEIN group (P = .296). One case of postoperative wound infection was noted in the EIN group, which was improved after treatment with debridement and anti-infection agents, and no wound infections were observed in the NEIN group; furthermore, there were no cases of recurrent fractures in the EIN group and 5 cases of recurrent fractures in the NEIN group (see Table 2).
Table 2.
Comparison of intraoperative and postoperative conditions.
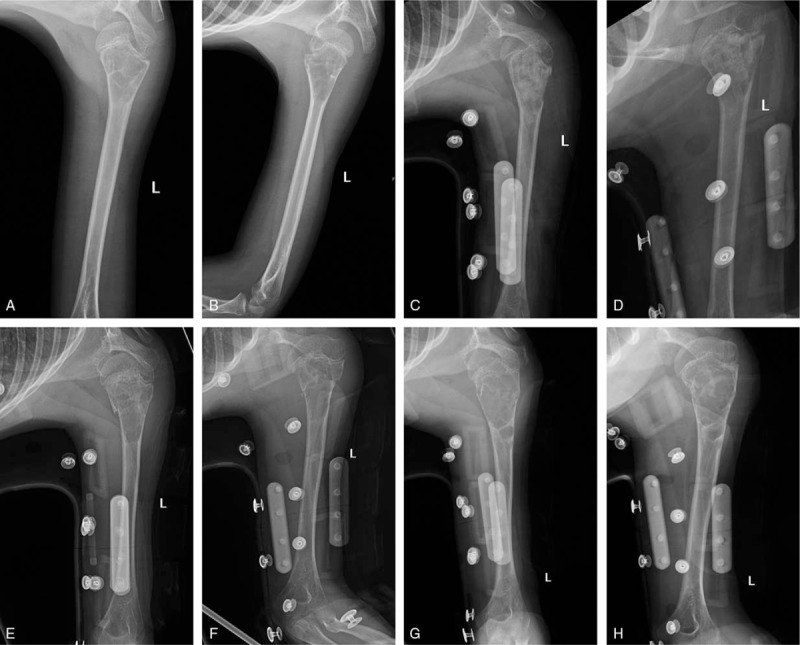
In the EIN group, 17 cases were cured, 10 cases were partially healed, and 3 cases were ineffective. The effective rate was 90.0% (effective rate = (cured + partially cured) / total number of people). In the NEIN group, 10 cases were cured, 12 cases were partially healed, and 10 cases were ineffective. The effective rate was 68.8%. There was a significant difference in curative effects between the two groups (P = .013). The effective rate in the EIN group was higher than that in the NEIN group (see Table 3). The typical cases of the EIN group are shown in Figure 1, and the typical cases of the NEIN group are shown in Figure 2.
Table 3.
Comparison of curative effects between the 2 groups of pediatric patients.
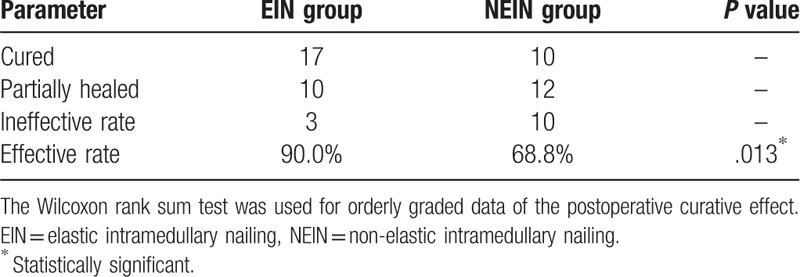
Figure 1.
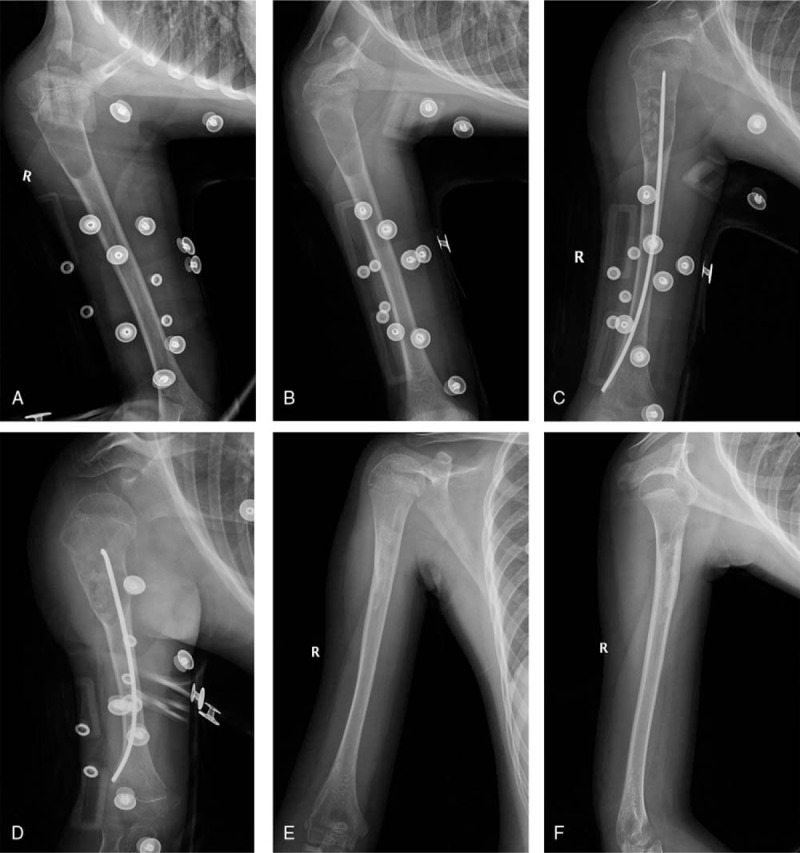
Elastic nail group. Note: EIN group, male patient, 9 years and 2 months old. A and B show before the operation, and it can be seen that for the cystic cavity of the right proximal femur, the volume was approximately 16 cm3, and the cyst was at the active stage. C and D were obtained 3 day after the operation, and high-density bone implant filling can be seen in the focus. One elastic nail can be seen in the medullary cavity. E and F show the results of follow-up for 1 year after the operation; the bone cyst was cured completely, the bone cortex was thickened, and no obvious deformity was found in the original focus.
Figure 2.
Nonelastic nail group. Note: NEIN group, female patient, 8 years and 5 months old. A and B show before the operation, and it can be seen that in the cystic cavity of the left proximal humerus, the volume was approximately 19 cm3, and the cyst was at the active stage. C and D were obtained 1 day after the operation, and high-density bone implant filling can be seen in the focus. E and F were recurrent fractures caused by trauma 3 years after the operation. The bone cortex of the left proximal humerus is thin, the bone cortex is discontinuous, and the distal fracture is slightly displaced to the radial side without obvious angulation. G and H show the re-examination results 5 years after the operation; the cyst cavity still exists in the proximal humerus and the bone cortex is still thinning. The bone cortex at the original fracture is basically continuous.
4. Discussion
Many methods are available to treat simple bone cysts, but the best method has not yet been determined. As a traditional surgical method, different treatment effects have been reported for curettage and bone grafting. In this research, the traditional curettage and bone grafting method was used for patients in the NEIN group, and in the postoperative follow-up, 22 cases showed a significant treatment effect while 10 cases exhibited recurrence, reflecting a poor treatment effect, with an effective rate of 68.8%. Oppenheim et al[14] obtained a similar result in his research in which 37 children with simple bone cysts who underwent curettage and bone grafting were followed up for 4 years, 16 of whom experienced recurrence, yielding a total recurrence rate of 43.2%. In this study, 12 cases were in the active stage and 25 cases were in the latent stage, and the recurrence rate was higher in the active-stage cases than that in latent-stage cases and higher in children younger than 10 years than that in children older than 10 years. In particular, 7 of the 8 children younger than 10 years old in the active stage recrudesced. Penimalli et al[15] included 19 children with bone cysts who underwent curettage and bone grafting, and 14 patients recrudesced after the operation, with a total recurrence rate as high as 73.7%. However, some studies have reached different conclusions. In the study of Kokavec et al,[16] 19 patients with bone cysts were all treated with curettage and bone grafting, and only 3 patients recrudesced during the follow-up after surgery, yielding an effective rate of 84.2%. Traub et al[9] included 8 cases of bone cysts and used curettage and bone grafting for treatment. During the 5-year follow-up after the operation, no patients recrudesced, yielding an effective rate of 100%. Other related studies have also achieved good curative effects.[17–21]
In the past decade, EIN has become popular in the treatment of bone cysts due to its satisfactory effect in long bone fractures in children. In 2000, Roposch et al[22] reported that among 32 pediatric patients, only 2 cases exhibited recurrence, and the effective rate was 93.8%. EIN also resulted in a good effect in the studies of Li et al[3] and De Sanctis et al.[23] Moreover, Mavčič et al[24] reported that the use of EIN for bone cysts not only improved the cure rate by reducing recurrence but also prevented pathological fractures as confirmed in his research in which no patients suffered pathological fracture in the EIN group, while 5 cases sustained pathological fractures after surgery in the NEIN group. However, some studies have also shown that the recurrence rate of bone cysts treated with EIN alone is high. Traub et al[24] included 8 children treated with EIN alone in their research, and 4 children recrudesced during the 5-year follow-up, with an effective rate of only 50%.
Compared with curettage and bone grafting alone, can the combination of this method with EIN provide better outcomes? In this research, the combination of curettage and bone grafting with EIN was used in 30 pediatric patients, and 27 cases experienced a positive treatment effect while 3 cases experienced recurrence, yielding an effective rate of 90.0%, which is significantly higher than that in the NEIN group. Hou et al[25] reached a similar conclusion in their study of 19 patients, including 7 in the EIN group and 12 in the NEIN group. In the postoperative follow-up, the effective rate was 85.7% in the EIN group compared with 66.7% in the NEIN group. In addition, with the combination of curettage and bone grafting and EIN, Luo et al[26] also achieved a good effect in treating bone cysts.
Two possible explanations may account for the differences among study results, including small sample sizes and excessive confounding factors. The advantage of this study is that it used direct control between groups with large sample sizes, and therefore, the conclusion is relatively reliable. The prognosis of simple bone cysts is affected not only by the operation method but also by factors such as sex, age of onset, location of onset, lesion activity and capsule volume.[8,10,25,27,28] In this study, there was no significant difference between the 2 groups in gender, age of onset, location of onset, lesion activity, pathological fracture and capsule volume, which excludes the influence of other confounding factors on the results. However, this study was a retrospective case analysis, and the study group and the control group were not randomly divided, making it somewhat deficient.
The results of this study show that EIN combined with curettage and bone grafting can significantly improve the effective rate of bone cyst treatment compared with curettage and bone grafting alone. The reason may be that elastic intramedullary nails can maintain a continuously open capsule cavity, thus effectively reducing the pressure in the capsule cavity and creating favorable conditions for healing.
Therefore, the use of EIN can effectively improve the prognosis of bone cysts without serious complications after surgery. Accordingly, EIN should be added as a standard procedure in the treatment of curettage and bone grafting in children with simple bone cysts.
Author contributions
Conceptualization: Ke Zhang, ZhongLiang Wang.
Data curation: Ke Zhang, Zheng Zhang.
Formal analysis: Ke Zhang.
Funding acquisition: Ke Zhang, ZhongLiang Wang.
Investigation: Ke Zhang, Zheng Zhang.
Methodology: Ke Zhang, ZhongLiang Wang, Zheng Zhang.
Project administration: Ke Zhang, ZhongLiang Wang.
Resources: Ke Zhang, ZhongLiang Wang.
Software: Ke Zhang.
Supervision: Ke Zhang, ZhongLiang Wang.
Validation: Ke Zhang.
Visualization: Ke Zhang.
Writing – original draft: Ke Zhang.
Writing – review & editing: Ke Zhang, ZhongLiang Wang, Zheng Zhang.
Footnotes
Abbreviations: NTEN = non-titanium elastic intramedullary nailing, TEN = titanium elastic intramedullary nailing.
The researcher declares no conflicts of interest.
References
- [1].Erol B, Onay T, Topkar OM. A comparative study for the treatment of simple bone cysts of the humerus. J Pediatr Orthop B 2017;26:5–13. [DOI] [PubMed] [Google Scholar]
- [2].Solooki S, Keikha Y, Vosoughi AR. Can ethanol be used as an adjuvant to extended curettage in order to reduce the recurrence rate of aneurysmal bone cyst? Rev Bras Ortop (English Edition) 2017;52:349–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Li W, Xu R, Du M. Comparison of titanium elastic intramedullary nailing versus injection of bone marrow in treatment of simple bone cysts in children: A retrospective study. Bmc Musculoskel Dis 2016;17:343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Wilke B, Houdek M, Rao RR. Treatment of unicameral bone cysts of the proximal femur with internal fixation lessens the risk of additional surgery. Orthopedics 2017;40:e862–7. [DOI] [PubMed] [Google Scholar]
- [5].Jamshidi K, Mirkazemi M, Izanloo A. Locking plate and fibular strut-graft augmentation in the reconstruction of unicameral bone cyst of proximal femur in the paediatric population. Int Orthop 2018;42:169–74. [DOI] [PubMed] [Google Scholar]
- [6].Shirai T, Tsuchiya H, Terauchi R. Treatment of a simple bone cyst using a cannulated hydroxyapatite pin. Medicine 2015;94:e1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Higuchi T, Yamamoto N, Shirai T. Treatment outcomes of the simple bone cyst. Medicine 2018;97:e572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rougraff BT, Kling TJ. Treatment of active unicameral bone cysts with percutaneous injection of demineralized bone matrix and autogenous bone marrow. J Bone Joint Surg Am 2002;84-A:921–9. [DOI] [PubMed] [Google Scholar]
- [9].Traub F, Eberhardt O, Fernandez FF. Solitary bone cyst: A comparison of treatment options with special reference to their long-term outcome. Bmc Musculoskel Dis 2016;17:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Glowacki M, Byrne A, Ignys O, et al. Evaluation of volume and solitary bone cyst remodeling using conventional radiological examination. Skeletal Radiol 2010;39:251–9. [DOI] [PubMed] [Google Scholar]
- [11].Neer NCS, Francis KC, Marcove RC. Treatment of unicameral bone cyst. A follow-up study of one hundred seventy-five cases. J Bone Joint Surg Am 1966;48:731. [PubMed] [Google Scholar]
- [12].Capanna R, Monte AD, Gitelis S. The natural history of unicameral bone cyst after steroid injection. Clin Orthop Relat RD 1982 204–11. [PubMed] [Google Scholar]
- [13].G Bel V, J Rgens H, Etsp Ler G. Prognostic significance of tumor volume in localized Ewing's sarcoma of bone in children and adolescents. J Cancer Res Clin 1987;113:187–91. [DOI] [PubMed] [Google Scholar]
- [14].Oppenheim WL, Galleno H. Operative treatment versus steroid injection in the management of unicameral bone cysts. J Pediatr Orthop 1984;4:1–7. [DOI] [PubMed] [Google Scholar]
- [15].Pentimalli G, Tudisco C, Scola E. Unicameral bone cysts? Comparison between surgical and steroid injection treatment. Arch Orthop Trauma Surg 1987;106:251–6. [DOI] [PubMed] [Google Scholar]
- [16].Kokavec M, Fristakova M, Polan P. Surgical options for the treatment of simple bone cyst in children and adolescents. Isr Med Assoc J 2010;12:87–90. [PubMed] [Google Scholar]
- [17].Yildirim C, Akmaz I, Sahin O. Simple calcaneal bone cysts: a pilot study comparing open versus endoscopic curettage and grafting. J Bone Joint Surg Br 2011;93:1626–31. [DOI] [PubMed] [Google Scholar]
- [18].Sponer P, Urban K, Urbanová E. Behaviour of nonresorbable bioactive glass–ceramic implanted into long bone defects: comparison with cancellous allografts. Arch Orthop Trauma Surg 2009;129:1353–60. [DOI] [PubMed] [Google Scholar]
- [19].Çelik S, Uludağ A, Tosun HB. Unicameral (simple) and aneurysmal bone cysts: The effect of insufficient curettage on recurrence. Pan Afr Med J 2016;24:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hou T, Wu Z, Xing J. Tissue-engineered bone treating simple bone cyst--a new strategy. J Surg Res 2016;200:544–51. [DOI] [PubMed] [Google Scholar]
- [21].Teoh KH, Watts AC, Chee YH. Predictive factors for recurrence of simple bone cyst of the proximal humerus. J Orthop Surg (Hong Kong) 2010;18:215–9. [DOI] [PubMed] [Google Scholar]
- [22].Roposch A, Saraph V, Linhart WE. Flexible intramedullary nailing for the treatment of unicameral bone cysts in long bones. J Bone Joint Surg Am 2000;82-A:1447–53. [DOI] [PubMed] [Google Scholar]
- [23].De Sanctis N, Andreacchio A. Elastic stable intramedullary nailing is the best treatment of unicameral bone cysts of the long bones in children? Prospective long-term follow-up study. J Pediatr Orthop 2006;26:520–5. [DOI] [PubMed] [Google Scholar]
- [24].Mavčič B, Saraph V, Gilg MM. Comparison of three surgical treatment options for unicameral bone cysts in humerus. J Pediatr Orthop B 2019;28:51–6. [DOI] [PubMed] [Google Scholar]
- [25].Hou H, Wu K, Wang C. Treatment of unicameral bone cyst. J Bone Joint Surg Am 2010;92:855–62. [DOI] [PubMed] [Google Scholar]
- [26].Luo L, Lu X, Ge J. Elastic stable intramedullary nailing for treatment of benign lesions of humerus complicating by pathological fracture in children. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013;27:21–4. [PubMed] [Google Scholar]
- [27].Flont P, Kolacinska-Flont M, Niedzielski K. Factors predictive of positive response to steroid therapy in simple bone cysts: an old trick that still works. Int Orthop 2013;37:1519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yandow SM, Marley LD, Fillman RR. Precordial doppler evaluation of simple bone cyst injection. J Pediatr Orthoped 2009;29:196–200. [DOI] [PubMed] [Google Scholar]


