Abstract
Tinnitus is a prevalent condition among different populations. As the nature of tinnitus is subjective, self-reported measures have been validated and utilized to assess psychometric properties of tinnitus patients. Without exception, Chinese clinicians have administered these measures to patients in mainland China after cross-cultural adaptation. However, shortcomings of these Mandarin measures limited the widespread use of them. Measures which can be fully adapted to the context of Chinese tinnitus patients are still needed. The objective of this study was to evaluate the reliability and validity of the Mandarin Tinnitus Primary Function Questionnaire (TPFQ-M) in a Chinese population.
In this observational questionnaire study, we recruited 350 subjects with primary tinnitus from hearing clinics of West China Hospital and administered the TPFQ-M, Mandarin Tinnitus Handicap Inventory (THI-M), and a systematic hearing test battery.
The subjects finished the TPFQ-M within 3 minutes. Exploratory and confirmatory factor analyses demonstrated that a 4-factor model was close to fit. The Cronbach alpha of TPFQ-M was 0.925, and test-retest reliability was reasonable with a 7-day test interval (ICC = 0.857, P < .001; 95% CI: 0.764–0.915). Test-retest reliabilities of subdomains were not parallel to each other, with 0.612 for Emotion, 0.766 for Sleep, 0.860 for Concentration, and 0.897 for Hearing. The convergent validity of TPFQ-M compared to the THI-M was moderate (r = 0.705, P < .001; 95% CI: 0.647–0.754).
The TPFQ-M, which shows high internal consistency and good factor structure, is simple and relatively easy to administer in busy clinics. Additional in-depth research involving multiple centers in mainland China is warranted.
Keywords: adult, questionnaire, reliability, tinnitus, validity
1. Introduction
Tinnitus is a sound that individuals perceive in their ears or heads without an external sound source, affecting a large population, with a prevalence rate of 10% to 15% in adults.[1,2] In most cases, tinnitus can give rise to health-related concerns, with predominantly negative effects, such as depression, anxiety, insomnia, attention problems, and even suicide attempts.[3–6] Hence, for the past several decades, researchers have focused on the etiology and treatment of tinnitus. Until now, any etiological hypothesis, however, could not overwhelm the others unanimously. To be specific, there are three hypotheses of tinnitus mechanism, namely, cochlear tinnitus, peripheral-dependent central tinnitus, and peripheral-independent central tinnitus.[7] These present different cellular or neural changes from cochlear to central auditory systems. A wide range of treatments for tinnitus relief have been developed,[8] including cognitive behavior therapy, sound therapy, masking with customized noise or music, and medications. However, as clinicians and patients prefer more significant outcomes, the more precise measures are warranted.
The assessment of tinnitus plays a vital role in the diagnosis, treatment, and monitoring. As the nature of primary tinnitus is subjective, self-reported measures prevailed swiftly in the past 2 decades, whereas objective measures have not been established to date. Apparently, tinnitus measures should be multi-domain, encompassing psychometric parameters, in which not only symptoms and feelings are considered, but also treatment-related changes.[9] Apart from the limitations of self-reported measures, such as exaggerating symptoms or underreporting severities, current self-reported questionnaires of tinnitus are relatively reliable, valid, and adapted to the local population.
To achieve a multi-domain approach, these measures employ more than one item for each domain to maintain high reliability and validity. To our knowledge, no less than 20 of self-rating questionnaires have been utilized in clinical practice globally, which include the Tinnitus Questionnaire (TQ),[10] Tinnitus Handicap Inventory (THI),[11] Tinnitus Reaction Questionnaire (TRQ),[12] Tinnitus Handicap Questionnaire (THQ),[13] and Tinnitus Functional Index (TFI).[14] These measures maintain a host of selected and validated subdomains, such as emotion, concentration distraction, sleep disturbance, hearing perception difficulties, general impact on daily work or leisure, and patients’ views of tinnitus, effectively appraising psychometric characteristics of tinnitus patients. Researchers and clinicians have translated these tinnitus measures, including but not limited to measures mentioned above, into different languages and evaluated severities of tinnitus patients with them.
No large-scale epidemiological study of tinnitus patients in mainland China has been conducted to date, and thus we are unable to present detailed characteristics of Chinese tinnitus patients. According to some published papers related to tinnitus assessments[15–17] and treatments,[18] these patients share similar primary symptoms as those of other countries such as emotions, sleep, concentration,[3] and hearing problems.[19] However, we observed certain distinct features in Chinese tinnitus patients. In addition, patients prefer to seek medical help in larger hospitals as local primary healthcare centers are limited.[20] In addition, patients do not receive adequate health education due to a lack of tinnitus clinics and doctors who are specialized in tinnitus. Therefore, physicians have employed self-reporting tinnitus measures in assessing this particular condition in mainland China in the past decade. A total of 5 self-reported tinnitus measures in English have been translated and validated into six Mandarin versions to date, including two versions of THI,[21,22] THI-12,[23] THQ,[24] Tinnitus Activity Questionnaire (TAQ),[25] and Tinnitus Questionnaire (TQ).[26] One Mandarin clinician-rated instrument was also developed, consisting of six items, named Tinnitus Evaluation Questionnaire (TEQ).[27] Among these Mandarin questionnaires, except for THI, which is the first tinnitus questionnaire administrated in China, none have thrived due to various specific disadvantages.
First, except for the Mandarin version of TQ, other tinnitus measures do not exhibit a factorial structure or have vague factorial constructs that are not suitable for precise evaluation of tinnitus. The Mandarin versions of THI (THI-M) and TEQ are not multi-factor. Subdomains of the Mandarin versions of TAQ, THI-12, and THQ overlapped during cross-adaptation. Hence, Physicians only can obtain overall scores for their patients’ status actually.
Second, the response burden of most measures is heavy in busy clinics. More than 20 items are included in THI, TAQ, THQ, and TQ, particularly 52 items of TQ. Although the content of a measure is more relevant than its intrinsic length,[28] these lengthy measures could not be efficiently administered in extremely busy clinics of mainland China where a specialist has to see more than 100 outpatients each day.[29]
Third, some measures employed idioms or words that are more frequently used in the English context such as “feel insecure” in THI and THQ, “enjoy life” in THI, TRQ, and TFI, and “quiet resting activities” in TFI. Instead, in mainland China, “feel secure” or “feel insecure” is mostly used to describe the circumstances of the surrounding, and rarely for a personal life; “enjoy life” is often replaced by the word “happy”. In accordance with habits of Mandarin, putting two words that overlap in meaning in one phrase would lead to misunderstanding, hence, “resting activities” would be preferred rather than “quiet resting activities”. Moreover, the TEQ introduced doctors’ judgments during initial tinnitus evaluation, which should be assessed for its accuracy for tinnitus evaluation and acceptance by clinicians and patients.
The Tinnitus Primary Function Questionnaire (TPFQ) that was developed in 2014[30] has been translated into other languages[31] and possesses a number of advantages. First, the TPFQ is a factorial structure that reveals subdomains traits of patients, namely, concentration (items 1 to 3), emotion (items 4 to 6), hearing (items 7 to 9), and sleep (items 10 to 12). Second, this questionnaire consists of 12 items only, which may be easily completed in a busy clinic. Third, this test hardly employs jargon, idioms, or vernacular terms and presents the specific context of English-speaking countries such as “feel insecure” in THI and THQ, “enjoy life” in THI, TRQ, and TFI, and “quiet resting activities” in TFI. Fourth, it is efficient and sensitive in assessing treatment-related changes than other measures not focusing on outcomes evaluation, which has been discussed in the original paper.[30] The loudness assessment, however, is not included in this brief questionnaire.
Generally, the TPFQ has a brief and multi-factor structure that could be easy to understand and answer. Hence, it could be one of the measures addressing issues that are related to clinicians with the extensive outpatient workload and decreasing the response burden of tinnitus patients in mainland China. However, the TPFQ is generally administered in English. The present study aimed to translate the original English version of TPFQ into Mandarin and to estimate its reliability and validity.
2. Materials and methods
2.1. Subjects
All of the subjects recruited to the study were diagnosed with primary tinnitus[32] and consulted the hearing clinic of West China Hospital of Sichuan University in Sichuan Province of China from July 15, 2017 to October 14, 2017 and December 13, 2017 to September 21, 2018. The university hospital is the largest tertiary teaching hospital in southwest China. Sample size determination was based on the subject-to-item ratio of 10:1.[33] The inclusion criteria were:
-
1.
chief complaint of tinnitus, with or without association with sensorineural hearing loss;
-
2.
age ≥ 18 years old;
-
3.
subjects with good adherence; and
-
4.
when tinnitus is intermittent, episodes last for at least 5 minutes, and occur more than once per week.[34]
We excluded tinnitus subjects with the following conditions:
-
1.
hyperacusis;
-
2.
mental disorders or any other condition that may lead to poor adherence; and
-
3.
ear disorders such as infections, effusion involving the middle ear, cholesteatoma, or otosclerosis.
All patients initially underwent detailed consultations and physical examinations including otoscopy and tuning fork tests by a senior ENT attending doctor or a consultant in the clinic to determine if they met the inclusion criteria. When the inclusion criteria met, patients voluntarily signed informed consent. The participants were free to withdraw from the study at any point during the investigation. Upon collection of informed consent, the subjects completed the THI-M[22] and TPFQ-M. The subjects were subjected to a battery of hearing tests to reconfirm their ears’ conditions and hearing levels, consisting of pure tone audiometry, transient evoked otoacoustic emission (TEOAE), tympanometry and speech recognition score. We defined hearing loss a condition with an average pure-tone hearing threshold (500, 1K, 2K, and 4K Hz) greater than 25 dB (decibel) HL (hearing level) in any ear. The loudness of tinnitus was measured by an 11-point scale ranged from 0 to 10, with 0 for “very faint” and 10 for “very loud”. Patients freely selected a type tinnitus therapy based on doctors’ advice, which included sound masking, tinnitus consultation, medication, or hearing aids. Some subjects had to wait for 1 week for a tinnitus consult. Thus, before treatment initiation, they completed the questionnaires for the second time in the clinic or electronically by email or We Chat (a social media application, Tencent, Shenzhen, Guangdong Province, China).[35]
The Ethics Committee of West China Hospital of Sichuan University (2017–113) approved the observational study. This study was also registered with the Chinese Clinical Trial Registry (ChiCTR) network, which is an affiliated partner of WHO clinical trials registry platform (ChiCTR-OOC-17011897).
2.2. Questionnaire translation
There is currently no consensus in the cross-cultural adaptation of questionnaires between different languages; however, forward-backward translation of a questionnaire to the target language is a prevailing method in academia.[36] We followed this approach to generate our TPFQ-M as well and reviewed our translation process of TPFQ-M in terms of Epstein's paper as a checklist to guide the cross-cultural adaptation. The following six steps were employed.
2.3. Preparation
Before translation, we established a 10-person panel, including two audiologists, two otolaryngologists, 2 research assistants, and 4 Chinese linguists of the English language. All members of the panel were Chinese-English bilinguals, and their mother tongue was Chinese. We also obtained permission from the author to translate the TPFQ. One audiologist was in charge of the entire procedure.
2.4. Forward translation
One ENT doctor, 1 linguist, and 1 assistant independently translated the TFPQ to Mandarin (Versions 1.1, 1.2, and 1.3). They were asked to retain meanings of the original TPFQ without jargons, idioms, or vernacular terms.
2.5. Backward translation
The other 3 linguists, who have no any background in tinnitus questionnaire research, blindly translated the 3 Mandarin versions back into English (Version 1.1b, Version1.2b, and Version1.3b). We did not reconcile the target language versions before backward translation, aiming to get more different versions of backward translations. In addition, the backward translators were also Chinese-English bilinguals, but at least with 1-year lived experience in an English-speaking country, so they were proficient in English and understood the similarities and differences between Chinese and English cultures.[37] As a result, the linguistic and cultural appropriateness of backward translation versions could also be guaranteed.
2.6. Committee review
The rest members of the panel, which consisted of 2 audiologists, an otolaryngologist, and a research assistant, as well as 2 previous translators in step 3, compared the translation reports to select the best equivalent item, both in terms of concept and meaning. The audiologist in charge chaired this multidisciplinary review process. In the process of comparison, the 3 backward translation versions (Version 1.1b, 1.2b, and 1.3b) were first compared with the 3 forward translation versions (Versions 1.1, 1.2, and 1.3), and then compared with the original English version. All members discussed these twelve items one by one. The discrepancies of forward and backward translations were identified and resolved. All translations were consolidated into one Mandarin version. The similar committee review method has been employed by other studies related to cross-cultural adaptation of self-reported questionnaires.[38–40] We cut out the expression “I feel like” in item 1 due to potential uncertainty as Chinese use this phrase to present a fact and not an either-or condition. One directly translated item 3 with the same double-negation pattern, in which “undisturbed” and “worst” were used in the English version, whereas the other paraphrased it in a positive sentence, “…tinnitus keeps disturbing me…”. We selected the latter because individuals with a different educational background can readily understand this phrase. We also altered the negative word “worst” into an affirmative sentence as “…tinnitus leads to emotional instability” instead of “emotional peace” in item 4, and into “…tinnitus interferes with my understanding of other's speech” in item 9. In addition, “depressed” is not a common word in the Chinese culture and is only used when he or she has developed mental health problems. Thus, we transformed the term “depressed” into “very unhappy” in item 5, which is more similar to everyday Chinese speech. Upon modification, translators not involved in the committee translated these 5 problematic items, not the entire questionnaire, back into English.[40] The committee review process was undertaken again and repeated until the committee believed these changes did not ruin the conceptual, item and semantic equivalence between the Mandarin version and the original English version. Meanwhile, we corresponded with Richard Tyler by email for technical issues. Upon reaching a consensus, we generated a version of the pre-TPFQ-M (Version 2.0).
2.7. Field testing
We administered the pre-TPFQ-M to 10 individuals with tinnitus, 5 patients, and 5 clinicians. Three patients experienced difficulty in understanding item 4, which included the phrase “emotional instability.” Therefore, we used the same structure, “…tinnitus keeps disturbing me…” as that of item 3 and transferred “emotional instability” into “emotional stability”. This item was revised as “…tinnitus keeps disturbing me to retain emotional stability,” Although all of the clinicians and other patients completed the pre-TPFQ-M without difficulty, they claimed the word of “speech” in Hearing subdomain was too formal and quite confusing compared to daily speech, as the term “talking” is more commonly used in Chinese speech. The sample size of the pre-testing was small, but the pilot subjects had a broad educational background from primary school to PhD, with a mean age of 45.4 ± 16.6 years.
2.8. Final version
We confirmed these modifications in pre-testing and reviewed the final version in terms of grammar and sentence construction, resulting in the final version of TPFQ-M (Version 3.0).
2.9. Scoring
2.9.1. TPFQ (Mandarin version)
The subjects rated each item using a scale of 0 to 100, with 0 for completely disagree and 100 for completely agree. The authors summed the scores of answers in each item (maximum of 12 items), and then calculated the mean by dividing the number of answered items. Subdomain average scores were computed using the same approach. To obtain more complete data, we established an approach in that if the number of items of each subdomain subjects scored was less than two, and then the corresponding score of the subdomain was not valid. No invalid subdomain scores were deleted in this study.
2.9.2. THI (Mandarin version)
In 25-item THI-M, 3 response options were provided to the subjects (yes, 4 points; sometimes, 2 points; no, 0 points) that were related to the functional, emotional, and catastrophic impacts of tinnitus. The overall THI-M score was computed by calculating the sum of the scores from the 25 items, ranging from 0 to 100.
2.10. Statistical analysis
The data were stored and analyzed using Excel 2010 (Microsoft, Redmond, WA), IBM SPSS 24 and SPSS AMOS 25 (IBM, Armonk, NY). The factor structure of TPFQ-M was evaluated using Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA), convergent validity was assessed by Spearman's correlation due to the skewed distribution of the data, and the internal consistency reliability of the TPFQ-M was reviewed using Cronbach alpha and test-retest reliability with intraclass correlation coefficient (ICC).[41] Two rounds of enrollments were utilized. The subjects of the first round (subsample 1) were for EFA, whereas the second round of patients (subsample 2) was employed for CFA.
During EFA, we employed the screen test[42] for cross-validation. If the number of factors extracted from EFA and the screen test was contradictory, then EFA was run multiple times below and above the predicted number of factors. Principal axis factoring was selected as the extraction method because of its versatile applicability in normal or non-normal distributed data[43] compared to principal component analysis for data reduction, and varimax rotation was employed to gain simpler and easy-to-interpret results. A loading cut-off value of 0.32 was selected to display the rotation results.[44]
The test model of CFA was constructed following the factorial structure obtained from EFA. We used the marker indicator approach, wherein the unstandardized factor loading of one observed variable in each factor was fixed to a value of 1.0, and the ratio of CMIN to degrees of freedom (df) (relative Chi-square, CMIN/df) and goodness-of-fit indexes were selected to evaluate the model fit based on maximum likelihood estimation. The significance level was 0.05. The dispersion of quantitative data with normal distribution was presented by standard deviation, whereas the 95% confidence interval (95% CI) was used to represent that of a set of data with skewed distribution.
3. Results
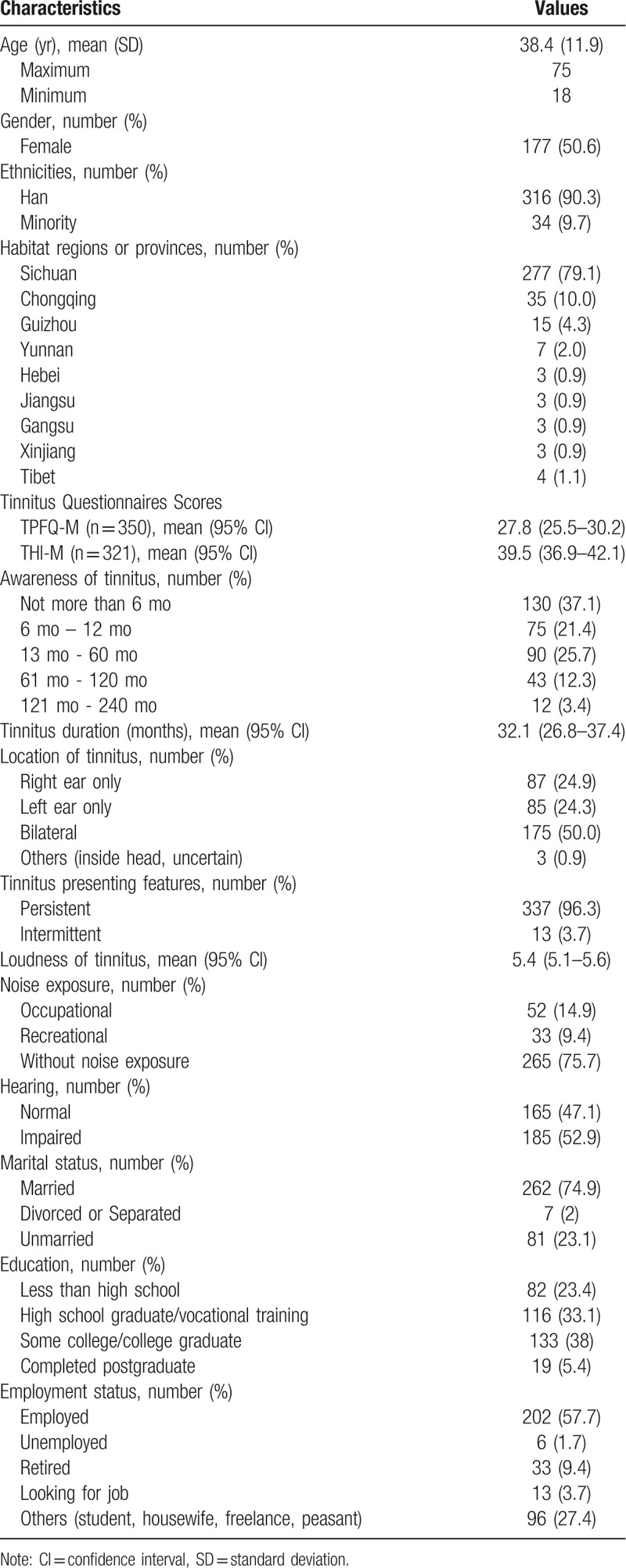
We recruited a total of 361 patients with primary tinnitus, consisting of 141 in the first enrollment and 220 in the second round. Approximately 40 subjects have incomplete information, from which 11 subjects without or with partial hearing tests results excluded, 29 subjects without THI-M scores only included. The subjects completed the TPFQ-M and THI-M in an average of 142 seconds (95% CI: 132–152), and 464 seconds (95% CI: 414–515), respectively. Table 1 shows the baseline characteristics of the study participants. Half of the subjects were females. The proportions of bilateral tinnitus perception were 50%. Nearly 40% of the subjects presented a tinnitus history of fewer than six months. The majority of the patients has no history of noise exposure, whereas the rate of occupational noise exposure was nearly two-fold higher compared to the recreational noise exposure rate (9.4%). The percentage of hearing-impaired subjects was marginally higher than those with normal hearing.
Table 1.
Baseline characteristics of subjects (n = 350).
3.1. Exploratory factor analysis
EFA is used to reveal latent data constructs and assists researchers in deciding how many factors to retain. The subjects-to-variable ratio was 10.8 (130 subjects/12 items = 10.8), which achieved the recommended ratio of 5:1 for factor analysis.[45] First, Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy was conducted to determine the suitability of the data for EFA. If KMO > 0.7, then the EFA is acceptable. The KMO of the present study was 0.848, which is greater than 0.7. Moreover, Bartlett test of sphericity indicated a significant statistical difference (χ2 = 1511.235, P < .001), which was used to test the null hypothesis (if the null hypothesis is rejected, EFA is available). Both KMO and Bartlett test revealed that EFA is suitable to our data. We adopted the Kaiser criterion (the cut-off value of an eigenvalue > 1.0)[46] for deciding the number of factors. After factor rotation, the Concentration and Hearing components were combined into one factor (Table 2), with factor loadings of 0.604 to 0.897, respectively. Three factors explained a cumulative variance of 75.96% (Table 3). However, the scree plot demonstrated four factors (Fig. 1), which disagreed with the predicted 3-factor model.
Table 2.
Rotated component matrix showing factor loadings (n = 130).
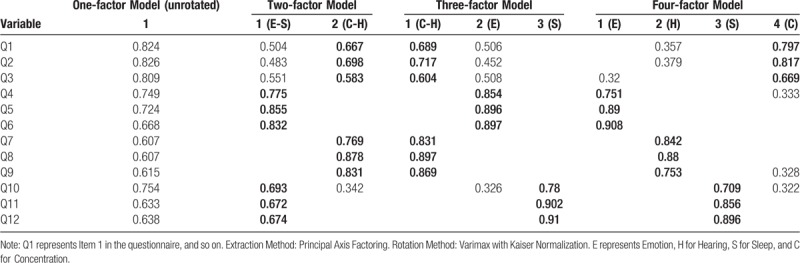
Table 3.
Total variance explained of TPFQ-M in exploratory factor analysis (n = 130).
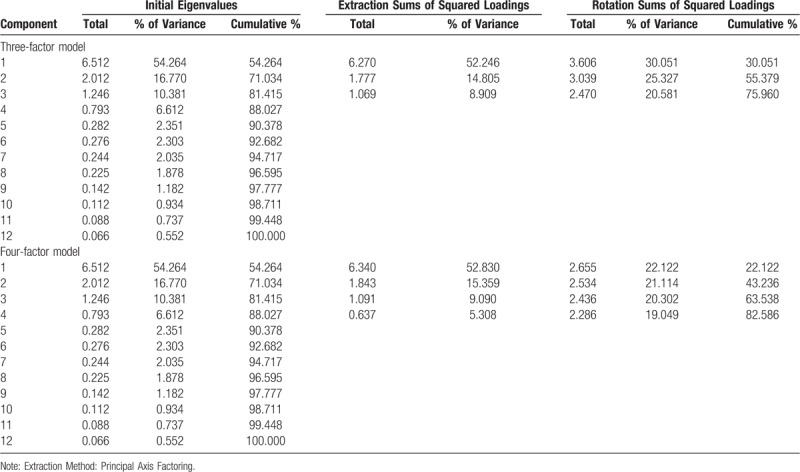
Figure 1.
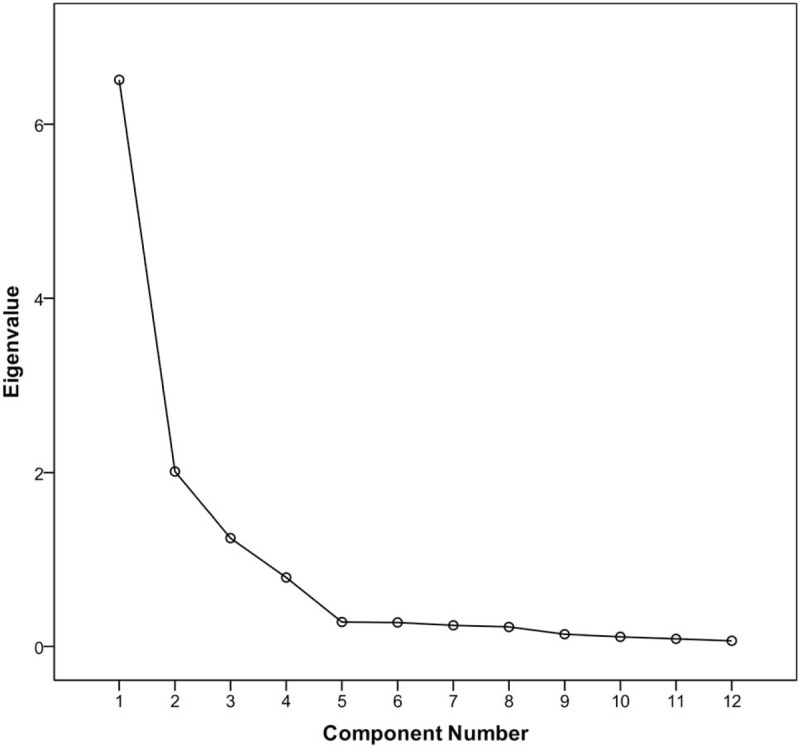
The point where the slope of the curve above is clearly leveling off at component 5 indicates the 4 factors that should be generated by the screen test (n = 130).
This discrepancy was assessed by retesting EFA at different fixed factors, including 1, 2, and 4 factors (Table 2). In the 1-factor model, the factor loadings were relatively acceptable, ranging from 0.607 to 0.824, whereas 74% of the nonredundant residuals with absolute values were >0.05 at reproduced correlations, which should be < 50% in a good fit.[47] These findings indicate that the 1-factor and the 2-factor model were inappropriate for our analysis. All items had cross-loadings in both factors,[33] which was >0.32 after rotation. Furthermore, 51% of the nonredundant residuals had absolute values >0.05. In the 4-factor model, none of the residuals with absolute values were >0.05, thereby satisfying the above criterion. The cross-loadings of the items still appeared in the 3- and 4-factor models, but the values of item cross-loadings were relatively low in the latter, all below 0.4. According to the EFA, both the 3- and 4-factor models of the TPFQ-M were acceptable; however, which one was optimal required further confirmation.
3.2. Confirmatory factor analysis
Next, we tested the 3-factor and 4-factor model solutions using subsample 2 of 220 patients in the CFA, respectively. Naming of the factors was the same as that of the original TPFQ (Fig. 2).
Figure 2.
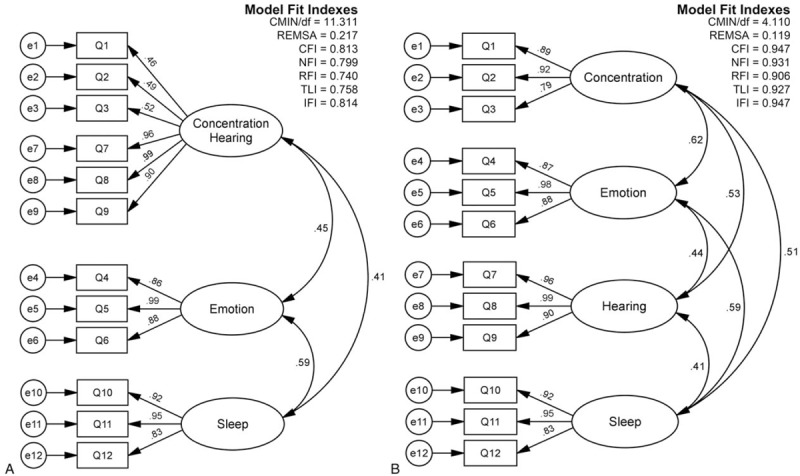
In each CFA pattern, the loadings of items are observed on the left side of the graph, whereas the correlation coefficients between subscales coming along with the curved double-arrow lines are shown on the right (n = 220). A reveals the solution of a 3-factor structure. B demonstrates the 4-factor model. On the top right, model fit indexes are marked, respectively.
In the 3-factor model, the ratio of CMIN/df was 11.311 higher than the cut-off value of 2.[48] In addition, the root mean square error of approximation (RMSEA) was 0.217. If the value of RMSEA <0.08 reflects adequate fit, then values between 0.08 and 0.10 demonstrate a mediocre fit while those >0.1 indicate an inadequate fit.[43] Even though the differences in covariances of the three factors were statistically significant (P < .001) from one another, the comparative fit index (CFI, <0.9 poor fit), normed fit index (NFI, <0.9 poor fit), relative fit index (RFI, <0.9 poor fit), Tucker-Lewis coefficient (TLI, <0.9 poor fit), and incremental fit index (IFI, <0.9 poor fit)[49,50] were apparently indicative of an inappropriate fit, whose values were relatively far from 1 (Fig. 2A). The loadings of items 1 to 3 were <0.6, indicating the least variance in factor one compared to that of the other 3 items (items 7 to 9) that were ≥0.9 in the same factor. Therefore, the 3-factor structure was inappropriate for tinnitus evaluation.
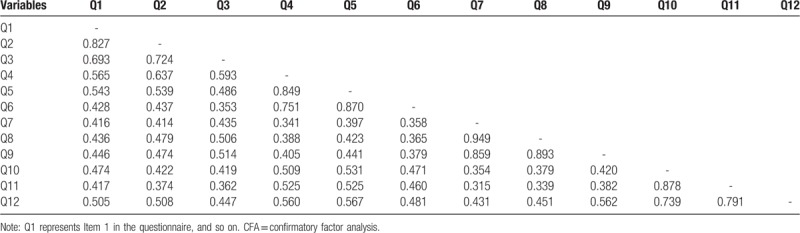
Conversely, the value of CMIN/df markedly decreased and was 4.11, which is still higher than 2, in the 4-factor model. The values of CFI, NFI, RFI, TLI, and IFI were close to 1 (all above 0.9). The RMSEA value significantly decreased to 0.119, which is slightly higher than 0.1, indicating a reasonable model fit.[51] Furthermore, there were statistically significant differences among the four factors (P < .001), including the concentration and hearing components (P < .001). Overall, the indexes of the four-factor model indicated an acceptable fit (Fig. 2B). The correlations of all items were also demonstrated in Table 4.
Table 4.
Correlations between all variables in the CFA (n = 220).
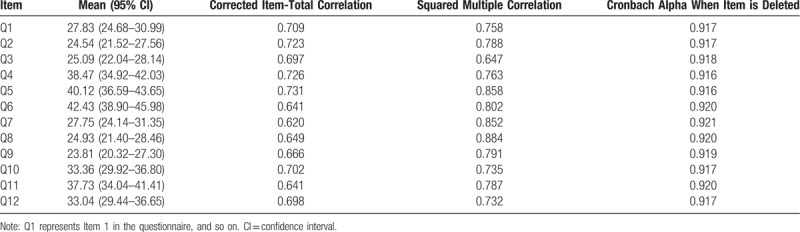
3.3. Reliability
The Cronbach alpha of the 12-item TPFQ-M, which had a sample size of 350 subjects, revealed internal consistency (0.925). The values of item-total correlation were between 0.620 and 0.731 (Table 5), indicating that the TPFQ-M has good internal consistency. The values of Cronbach alpha for subscales were also calculated (Concentration, 0.913; Emotion, 0.937; Hearing, 0.953; Sleep, 0.921).
Table 5.
Item-total correlation of TPFQ-M (n = 350).
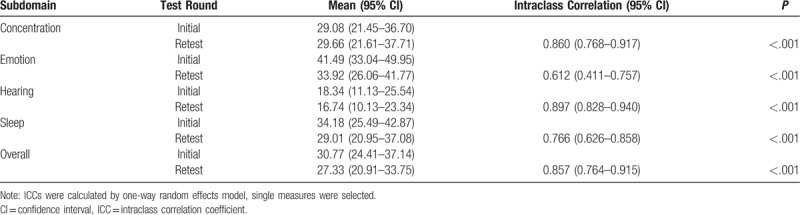
3.4. Test-retest reliability
Fifty-two patients completed the TPFQ-M twice at a 7-day interval (mean: 7.8 days; 95% CI: 6.5–9.1), while waiting for tinnitus consulting. They finished the TPFQ-M in the clinic, online or via social media. The Spearman-Brown correlation of ICC was used to assess test-retest reliability for data outside the normal distribution. The overall ICC of TPFQ-M was 0.857 (Table 6).
Table 6.
Test-retest reliability of TPFQ-M evaluated by ICC (n = 52).
3.5. Convergent validity
Convergent validity reveals the correlation among relevant measures with the same construct or a highly related construct.[52] Due to the absence of a gold standard for assessing tinnitus, we employed the THI, which has been widely accepted worldwide, for convergent validity evaluation, compared to the TPFQ-M. We examined the correlation of the TPFQ-M and the Mandarin version of THI[22] based on their total scores in all subjects using Spearman analysis, which demonstrated moderate correlation (r = 0.705, P < .001; 95% CI: 0.647–0.754).
4. Discussion
To date, besides our Mandarin version, another Hindi version of TPFQ (TPFQ-H)[31] is currently available. The current study was designed to determine the reliability and validity of the TPFQ-M. The results of the present study indicate that the TPHQ-M can be administered to Chinese tinnitus patients in clinical practice in mainland China.
We translated the original English version into Chinese-Mandarin using the forward-backward method. As mentioned in the Methods, we focused largely on the equivalence of contents and meaning of items between 2 versions, rather than word-by-word translation. First, we produced the Mandarin-target version with non-medical background linguists to retain the concept. Similarly, recent reports have shown that the participation of linguists and clinicians helps ensure that the translations of questionnaires retain both cultural and conceptual equivalence. Second, translators with medical backgrounds merged pre-versions into one Mandarin-target version, preventing the overuse of obscure medical terms and the inaccurate use of words to describe tinnitus-related distress. We reported the forward-and-backward translation procedure based on Epstein review. Our findings indicate that this review of cross-cultural adaptation different guidelines reduces bias during translation. Using this guide can also ensure the quality and comparability of different studies of hearing-related questionnaires from a variety of regions and countries.
To confirm whether TPFQ-M employs a distinct factor structure that varies from the original TPFQ, we administered EFA and CFA for cross-checking in independent samples. Initially, three factors extracted from EFA differed from the four factors observed in the scree plot test. Some researchers argued that the Kaiser criterion may lead to overestimations of the number of factors extracted.[33,47] Then, we retested the EFA at 1-, 2-, and 4-factor structures, respectively. Our metrics indicate that the 1- and 2-factor models were not a good fit. The other 2 models were derived from the CFA. In the 3-factor model, the correlations between the Concentration-Hearing factor and the 2 other factors were relatively low (Fig. 2A), and discriminant capabilities were observed due to significant covariance differences, whereas the model fit indexes overturned this model, failing to meet the standard of a good fit (Fig. 2A). The low correlations and the significant covariance between Concentration and Hearing were supported as two independent factors in the 4-factor model. The goodness-of-fit indexes confirmed our results and indicated that the 4-factor construct was highly reliable (Fig. 2B).
However, studies have demonstrated that chronic tinnitus could interfere with patients’ concentration abilities,[53] and tinnitus with hearing loss could lead to poor quality of life (including concentration).[19] Two issues are often hard to distinguish rather than two sides of a problem. Whether the impacts of tinnitus on concentration outweigh that of hearing loss on concentration remains unclear. The four-factor theory of the original TPFQ was generated from the international classification of functioning, disability, and health of the World Health Organization.[30] Tyler et al. pointed out that tinnitus interferes with the primary functions (concentration, emotion, hearing, and sleep) of an individual, which are then related to social interactions, work, and daily life. The TPFQ-M retained the same four-factor structure and discriminated these components in the Chinese study population. We observed that the TPFQ-M could theoretically employ Concentration and Hearing as 2 factors, namely, Emotion, followed by Hearing, Sleep, and Concentration. We also followed the same order of typesetting as the TPFQ.
The reliability of a measure is another critical point. We found that the TPFQ-M had excellent reliability and high item-total correlations. Cronbach alpha of TPFQ-M was 0.925, indicating that TPFQ-M could produce similar results using the same context. It was marginally higher than Cronbach alpha of the original TPFQ (α = 0.89). The subscale values of Cronbach alpha (Concentration 0.913, Emotion 0.937, Hearing 0.953, and Sleep 0.921) were all >0.9 compared to that of the original TPFQ (0.86, 0.9, 0.9, and 0.93). The cross-culture translation may contribute to the observed high internal consistency, which maintained the conceptual equivalence of the original TPFQ, which is due to the considerable reduction in random errors.
In addition, the original TPFQ did not report the test-retest reliability. We estimated the test-retest reliability of TPFQ-M by ICC instead of Pearson correlation, which is commonly used in other similar researches on test reliability. In fact, Pearson correlation is frequently used to measure the mean differences between two variables, whereas the ICC is employed to measure similarity in the resulting units of the same group. Therefore, it is more appropriate to employ the ICC in evaluating test-retest reliability. According to the Landis and Koch classification,[54] test-retest reliability may be described as excellent (0.8 < ICC ≤ 1), good (0.6 < ICC ≤ 0.8), fair (0.4 < ICC ≤ 0.6), poor (0.2 < ICC ≤ 0.4), or bad (0 < ICC ≤ 0.2). The overall test-retest ability of TPFQ-M was excellent. Among the subdomains, Emotion acquired the lowest test-retest reliability (Table 6). A possible explanation for this might be that after patients with tinnitus see a doctor, the anxiety or worry about tinnitus is relived considerably because patients might think they have found a specialist that could help them before treatment initiation; and these mental suggestions generated from patients themselves increase their confidence to fight with tinnitus. Nevertheless, emotional symptoms caused by tinnitus are unavoidable issues that need to be addressed. Tinnitus may not directly result in suicide,[55] whereas emotional distress was associated with tinnitus severity, which is highly correlated with suicide ideation in adults with tinnitus.[56] In a multi-domain measure, researchers should retain this domain as an early detector or indicator of outcomes in mental signs of tinnitus sufferers.
In original TPFQ, the authors calculated the construct validity by comparing it with other four questionnaires, namely, Pittsburgh Sleep Quality Index (PSQI), Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI), and THQ. The relevant domains among these different measures showed moderate to high correlations, whereas low correlations were observed in the irrelevant domains. The authors obtained convincing results on the construct validity of TPFQ. TPFQ was utilized in a clinical trial to measure the severity and outcomes of tinnitus.[57] However, a comparison between TPFQ and THQ in the original study of TPFQ (Tyler et al, 2014), instead of THI, may have narrowed the coverage of TFPQ. For this purpose, we estimated the convergent validity of TPFQ-M compared to THI-M, which has been extensively utilized in China. The correlation between TPFQ-M and THI-M was 0.705, which was acceptable, and slightly lower than the corresponding figure of 0.77 between TPFQ and THQ presenting in the original paper. Since the funding in the present study was limited that does not allow sufficient financial support to complete other relevant measures, we dropped these measures for other concurrent validity.
Overall, we developed a new tinnitus tool, TPFQ-M, which shows high internal consistency and good factor structure in relation to language requirements for Chinese subjects and cost-effectiveness for completion, indicating that it may be potentially utilized in a busy clinic in China. If this measure is used in clinical practice in mainland China, we believe that clinicians or audiologists can at least get the following benefits. For one thing, they could quickly obtain the status of the four main dimensions of tinnitus patients. For another, because of the reduction of evaluation time, the communication time between doctors and patients is relatively increased, which makes sense for Chinese doctors.[29] In addition, this measure enriches the tinnitus measures that are currently available in mainland China, giving physicians who treat tinnitus an alternative.
Our study has a number of limitations. First, our study involved a single site and utilized a sample population. Second, individuals with tinnitus, who were not going to the hospital for consultations, were not included in our study. Third, other relevant psychometric measures were not employed for comparison, specifically measures related to depression, anxiety, sleep and quality of life. Fourth, the severity grading of the TPFQ-M also requires subsequent research support. We suggest that clinicians consider these limitations when using the TPFQ-M for their patients. We plan to further assess the validity of our tool using individuals with tinnitus from different regions of mainland China.
5. Conclusions
The evaluation of tinnitus remains a challenge to the fields of otolaryngology, audiology, psychology, and other related medical disciplines. Any tools or methods for testing psychometric characteristics and severities of tinnitus must be universally accurate and reliable. The validity of a test based on its reliability. The TPFQ-M has not only excellent reliability and test-retest reliability but also strong enough convergent validity, but discriminant validity and responsiveness were not obtained from this study. Thus, we recommend that TPFQ-M be utilized with a limited scope; for instance, only in some key hospitals or research centers where qualified clinicians are available until additional investigations of its adaptability in mainland China have been completed.
Acknowledgments
We thank the staff members of the hearing lab and the school of languages and literature for their contributions to the research. We also appreciate Mr. Yan Xu for his review of our data analysis.
Author contributions
Conceptualization: Tao Lu, Gang Li, Yun Zheng.
Formal analysis: Tao Lu.
Funding acquisition: Yun Zheng.
Investigation: Tao Lu, Jiehai Liu, Gang Li, Ting Xiang, Ying Ma, Juan Zhong, Jiamei Chen, Yurui He, Hemei Huang, Zongyun Zhang, Pan Liu.
Methodology: Tao Lu, Jiehai Liu, Yun Zheng.
Project administration: Tao Lu.
Supervision: Yun Zheng.
Validation: Gang Li, Yun Zheng.
Visualization: Tao Lu.
Writing – original draft: Tao Lu.
Writing – review & editing: Tao Lu, Jiehai Liu.
Footnotes
Abbreviations: CFA = confirmatory factor analysis, CFI = comparative fit index, EFA = exploratory factor analysis, ICC = intraclass correlation coefficient, IFI = incremental fit index, KMO = Kaiser-Meyer-Olkin, NFI = normed fit index, RFI = relative fit index, RMSEA = root mean square error of approximation, TAQ = tinnitus activity questionnaire, TEQ = tinnitus evaluation questionnaire, TFI = tinnitus functional index, THI = tinnitus handicap inventory, THI-M = the Mandarin version of the Tinnitus Handicap Inventory, THQ = tinnitus handicap questionnaire, TLI = Tucker-Lewis Coefficient, TPFQ = Tinnitus Primary Function Questionnaire, TPFQ-M = the Mandarin version of the Tinnitus Primary Function Questionnaire, TQ = Tinnitus Questionnaire, TRQ = tinnitus reaction questionnaire.
This work was supported by grant from the Health Commission of Sichuan Province of China (18PJ075).
The authors have no conflicts of interest.
References
- [1].Shargorodsky J, Curhan GC, Farwell WR. Prevalence and characteristics of tinnitus among US Adults. Am J Med 2010;123:711–8. [DOI] [PubMed] [Google Scholar]
- [2].Park RJ, Moon JD. Prevalence and risk factors of tinnitus: the Korean National Health and Nutrition Examination Survey 2010-2011, a cross-sectional study. Clin Otolaryngol 2014;39:89–94. [DOI] [PubMed] [Google Scholar]
- [3].Durai M, Searchfield G. Anxiety and depression, personality traits relevant to tinnitus: a scoping review. Int J Audiol 2016;55:605–15. [DOI] [PubMed] [Google Scholar]
- [4].Miguel GS, Yaremchuk K, Roth T, et al. The effect of insomnia on tinnitus. Ann Otol Rhinol Laryngol 2014;123:696–700. [DOI] [PubMed] [Google Scholar]
- [5].Pridmore S, Walter G, Friedland P. Tinnitus and suicide: recent cases on the public record give cause for reconsideration. Otolaryngol Head Neck Surg 2012;147:193–5. [DOI] [PubMed] [Google Scholar]
- [6].Seo JH, Kang JM, Hwang SH, et al. Relationship between tinnitus and suicidal behaviour in Korean men and women: a cross-sectional study. Clin Otolaryngol 2016;41:222–7. [DOI] [PubMed] [Google Scholar]
- [7].Norena AJ. Revisiting the cochlear and central mechanisms of tinnitus and therapeutic approaches. Audiol Neurootol 2015;20Suppl 1:53–9. [DOI] [PubMed] [Google Scholar]
- [8].Zenner HP, Delb W, Kroner-Herwig B, et al. A multidisciplinary systematic review of the treatment for chronic idiopathic tinnitus. Eur Arch Otorhinolaryngol 2017;274:2079–91. [DOI] [PubMed] [Google Scholar]
- [9].Meikle MB, Stewart BJ, Griest SE, et al. Tinnitus outcomes assessment. Trends Amplif 2008;12:223–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hallam RS, Jakes SC, Hinchcliffe R. Cognitive variables in tinnitus annoyance. Br J Clin Psychol 1988;27(Pt 3):213–22. [DOI] [PubMed] [Google Scholar]
- [11].Newman CW, Jacobson GP, Spitzer JB. Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg 1996;122:143–8. [DOI] [PubMed] [Google Scholar]
- [12].Wilson PH, Henry J, Bowen M, et al. Tinnitus reaction questionnaire: psychometric properties of a measure of distress associated with tinnitus. J Speech Hear Res 1991;34:197–201. [PubMed] [Google Scholar]
- [13].Kuk FK, Tyler RS, Russell D, et al. The psychometric properties of a tinnitus handicap questionnaire. Ear Hear 1990;11:434–45. [DOI] [PubMed] [Google Scholar]
- [14].Henry JA, Griest S, Thielman E, et al. Tinnitus Functional Index: development, validation, outcomes research, and clinical application. Hear Res 2016;334:58–64. [DOI] [PubMed] [Google Scholar]
- [15].Xu Y, Yao J, Zhang Z, et al. Association between sleep quality and psychiatric disorders in patients with subjective tinnitus in China. Eur Arch Otorhinolaryngol 2016;273:3063–72. [DOI] [PubMed] [Google Scholar]
- [16].Xu J, Zheng Y, Meng Z, et al. The relationship between tinnitus severity and anxiety. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi (Chinese) 2012;26:729–32. [PubMed] [Google Scholar]
- [17].Mao K, Jiang W, Feng Y. Preliminary investigation of psychologic factors in 76 tinnitus patients. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi (Chinese) 2011;25:732–4. [PubMed] [Google Scholar]
- [18].Cai Y, Zhou Q, Yang H, et al. Logistic regression analysis of factors influencing the effectiveness of intensive sound masking therapy in patients with tinnitus. BMJ Open 2017;7:e018050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Joo YH, Han KD, Park KH. Association of hearing loss and tinnitus with health-related quality of life: the Korea National Health and Nutrition Examination Survey. PLoS One 2015;10:e0131247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Li X, Lu J, Hu S, et al. The primary health-care system in China. Lancet 2017;390:2584–94. [DOI] [PubMed] [Google Scholar]
- [21].Shi QL, Bu XK, Wang JG. Translation and application of tinnitus handicap inventory in Chinese version. Acta Universitis Medicinalis Nanjing (Chinese) 2007;27:476–9. [Google Scholar]
- [22].Meng Z, Zheng Y, Liu S, et al. Reliability and validity of the chinese (mandarin) tinnitus handicap inventory. Clin Exp Otorhinolaryngol 2012;5:10–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Jian Y, Yu F, Zhong SC, et al. The clinical application of tinnitus handicap index (THI-12) Chinese version. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi (Chinese) 2016;30:907–10. [DOI] [PubMed] [Google Scholar]
- [24].Xin Y, Tao LY, Wang J, et al. Translation and Application of Tinnitus Handicap Questionnaire. Journal Audiol Speech Pathol (Chinese) 2015;23:457–61. [Google Scholar]
- [25].Pan T, Richard T, Song Y, et al. Investigation of the influence of tinnitus to patients in their daily life and the reliability test of tinnitus activity questionnaire. Chin Arch Otolaryngol Head Neck Surg 2011;18:667–70. [Google Scholar]
- [26].Meng Z, Chen Z, Xu K, et al. Psychometric properties of a Mandarin version of the tinnitus questionnaire. Int J Audiol 2016;55:366–74. [DOI] [PubMed] [Google Scholar]
- [27].Liu P, Xu GL, Li M, et al. Study on reliability and validity of the Tinnitus Evaluation Questionnaire. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi (Chinese) 2012;47:716–9. [PubMed] [Google Scholar]
- [28].Rolstad S, Adler J, Ryden A. Response burden and questionnaire length: is shorter better? A review and meta-analysis. Value Health 2011;14:1101–8. [DOI] [PubMed] [Google Scholar]
- [29].Li Q, Xie P. Outpatient workload in China. Lancet 2013;381:1983–4. [DOI] [PubMed] [Google Scholar]
- [30].Tyler R, Ji H, Perreau A, et al. Development and validation of the tinnitus primary function questionnaire. Am J Audiol 2014;23:260–72. [DOI] [PubMed] [Google Scholar]
- [31].Shaurya C, Ravichandran A, Kumar S. Transadaptation and standardization of tinnitus primary function questionnaire in hindi. Int Tinnitus J 2018;22:23–9. [DOI] [PubMed] [Google Scholar]
- [32].Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg 2014;1512 Suppl:S1–40. [DOI] [PubMed] [Google Scholar]
- [33].Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval 2005;10: [Google Scholar]
- [34].Henry JA, Dennis KC, Schechter MA. General review of tinnitus: Prevalence, mechanisms, effects, and management. J Speech Lang Hear R 2005;48:1204–35. [DOI] [PubMed] [Google Scholar]
- [35].Thorpe JM, Smith D, Kuzla N, et al. Does mode of survey administration matter? Using measurement invariance to validate the mail and telephone versions of the bereaved family survey. J Pain Symptom Manage 2016;51:546–56. [DOI] [PubMed] [Google Scholar]
- [36].Epstein J, Santo RM, Guillemin F. A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. J Clin Epidemiol 2015;68:435–41. [DOI] [PubMed] [Google Scholar]
- [37].Hall DA, Zaragoza Domingo S, Hamdache LZ, et al. A good practice guide for translating and adapting hearing-related questionnaires for different languages and cultures. Int J Audiol 2017;57:161–75. [DOI] [PubMed] [Google Scholar]
- [38].Zam T, Dzulkarnain A, Rahmat SB, et al. Translation, adaptation and cross-cultural validation of hearing handicap inventory for adult in malay language. J Audiol Otolahead of print 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Parent-Vachon M, Parnell LK, Rachelska G, et al. Cross-cultural adaptation and validation of the Questionnaire for Pruritus Assessment for use in the French Canadian burn survivor population. Burns 2008;34:71–92. [DOI] [PubMed] [Google Scholar]
- [40].Su CT, Parham LD. Generating a valid questionnaire translation for cross-cultural use. Am J Occup Ther 2002;56:581–5. [DOI] [PubMed] [Google Scholar]
- [41].Bartko JJ. The intraclass correlation coefficient as a measure of reliability. Psychol Rep 1966;19:3–11. [DOI] [PubMed] [Google Scholar]
- [42].Cattell RB. Factor analysis: An introduction to essentials. II. the role of factor analysis in research. Biometrics 1965;21:405–35. [PubMed] [Google Scholar]
- [43].Fabrigar LR, Wegener DT, MacCallum RC, et al. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods 1999;4:272–99. [Google Scholar]
- [44].Yong AG, Pearce S. A beginner's guide to factor analysis focusing on exploratory factor analysis. Tutor Quant Methods Psychol 2013;9:79–94. [Google Scholar]
- [45].Osborne JW, Costello AB. Sample size and subject to item ratio in principal components analysis. Pract Assess Res Eval 2004;9: [Google Scholar]
- [46].Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas 1960;20:141–51. [Google Scholar]
- [47].Field A. Discovering Statistic Using SPSS. Third ed.London: SAGE; 2009. [Google Scholar]
- [48].Marsh HW, Hocevar D. Application of confirmatory factor analysis to the study of self-concept: First- and higher order factor models and their invariance across groups. Psychol Bull 1985;97:562–82. [Google Scholar]
- [49].Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1–55. [Google Scholar]
- [50].Bentler PM. Comparative fit indexes in structural models. Psychol Bull 1990;107:238–46. [DOI] [PubMed] [Google Scholar]
- [51].Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res 1992;21:230–58. [Google Scholar]
- [52].Carlson KD, Herdman AD. Understanding the impact of convergent validity on research results. Organ Res Methods 2010;15:17–32. [Google Scholar]
- [53].Gudwani S, Munjal SK, Panda NK, et al. Association of chronic subjective tinnitus with neuro- cognitive performance. Int Tinnitus J 2017;21:90–7. [DOI] [PubMed] [Google Scholar]
- [54].Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- [55].Martz E, Jelleberg C, Dougherty DD, et al. Tinnitus, depression, anxiety, and suicide in recent veterans: a retrospective analysis. Ear Hear 2018;39:1046–56. [DOI] [PubMed] [Google Scholar]
- [56].Han KM, Ko YH, Shin C, et al. Tinnitus, depression, and suicidal ideation in adults: a nationally representative general population sample. J Psychiatr Res 2018;98:124–32. [DOI] [PubMed] [Google Scholar]
- [57].Rojas-Roncancio E, Tyler R, Jun HJ, et al. Manganese and Lipoflavonoid Plus((R)) to treat tinnitus: a randomized controlled trial. J Am Acad Audiol 2016;27:661–8. [DOI] [PubMed] [Google Scholar]


