Abstract
Patients with increased body mass index (BMI) are often denied reduction mammoplasty due to concern for high morbidity. There is a paucity of evidence identifying high BMI as a predictor of poor long-term outcomes in reduction mammoplasty. In this study, we investigated the influence of BMI on long-term patient satisfaction following reduction mammoplasty.
All patients undergoing reduction mammoplasty over a 12-year period at a single institution were included in the study. A retrospective chart review was conducted to extract demographics, operative data, and postoperative course including complications. Patients were classified into 4 categories based on BMI (normal (<25), overweight (25–29.9), obese (30–39.9), and morbidly obese (≥40)). Patient satisfaction was assessed using a customized survey which was administered over the phone. Only patients with complete medical records who participated in the survey were included.
The 70 patients met the inclusion criteria for the study. Median time from surgery to survey was 6 years. Overall satisfaction after reduction mammoplasty was high, 5 on a 5-point Likert scale. The amount of breast tissue resected correlated with patient BMI (P <.01). There was no statistical difference in satisfaction across BMI classes. Furthermore, high BMI (obese, and morbidly obese) was not associated with higher postoperative complications (P = .70). Those with a high overall satisfaction score had a significantly greater self-reported aesthetic score compared to those with low and mid satisfied scores (P <.01).
Following reduction mammoplasty, patients report high satisfaction which is sustained over several years. Obesity is not associated with a higher incidence of complications or lower satisfaction. Our data suggest that patients with a high BMI should not be denied reduction mammoplasty out of concern for higher complication rate or reduced patient satisfaction due to BMI alone, but reduction mammoplasty should be considered in the setting of overall health counseling.
Keywords: body mass index (BMI), breast reduction, mammoplasty, patient-related outcomes, satisfaction
1. Introduction
Macromastia, or breast hypertrophy, can cause disabling physical symptoms in women, and emotional burden.[1] Reduction mammoplasty is the preferred procedure to alleviate symptoms in these patients.[2–4] Despite the proven benefits to patients, there is a hesitation in performing reduction mammoplasty in the obese (body mass index (BMI) >30) population and some insurers require the patient to lose weight in order to reach a permissible maximum weight (20% over their ideal body weight)[5] before approving the procedure. This may be due to the overwhelming evidence describing an association between obesity (BMI >30) and increased postoperative complication rates,[6–11] with the postoperative risk even greater in those classed as morbidly obese (BMI >40),[12,13] with very few studies contradicting this maxim.[14,15] There is also the consideration of whether the macromastia and patient symptoms are sequelae of increased BMI, and if breast reduction surgery poses the best treatment option.
However, reports often describe the complications after reduction mammoplasty as minor with little effect on aesthetic outcomes.[9,10,16] Indeed, increased preoperative BMI has been correlated with high satisfaction following reduction mammoplasty, however, this did not include the morbidly obese (BMI >40).[17] Given these findings, it can be argued that potential complication rate or dissatisfaction should not prevent those with high BMIs from undergoing breast reduction surgery.[10,14] Additionally, most existing studies have been limited in scope to a 1-year postoperative period and are thus unable to measure the long-term impact of reduction mammoplasty on patient satisfaction.[18,19]
Previous studies have used a plethora of instruments to measure improvement in quality of life and patient satisfaction following reduction mammoplasty.[20–26] We aim to assess the influence of BMI in long-term patient satisfaction following reduction mammoplasty with the use of a customized questionnaire. In addition, we aim to provide further clarification of the relationship between obesity (BMI >30) and complications following reduction mammoplasty.
2. Methods
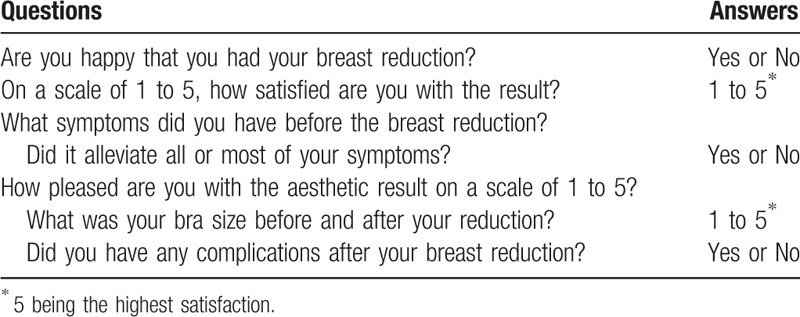
A single-site retrospective review was performed on patients who had undergone reduction mammoplasty at the University of Maryland Medical Center from 2006 to 2013. Potential participants were identified using the CPT code 19318 (reduction mammoplasty). Only patients with 5 or more years of post-reduction follow-up were included. Patients who had oncologic reductions were deceased or did not have functional telephone numbers were excluded from the study. Eligible patients were then surveyed using a customized questionnaire to assess long-term outcomes after reduction mammoplasty. The questionnaire (Table 1) included descriptive, open questions in order to capture patient perception of their pre- and post-operative experience. The questionnaire was designed to be brief to increase compliance and response rate. In our first stage of recruitment, letters were mailed to potential participants with information on the study and the opportunity to opt out. Then the patients were contacted by telephone to participate in our specialized survey during the phone call. The study protocol was approved by our Institutional Review Board.
Table 1.
Survey questions on long-term outcomes following reduction mammoplasty.
Patients who underwent reduction mammoplasty at the University of Maryland Medical Center from 2006 to 2013 were identified and mailed letters in the first stage of recruitment. 206 patients progressed to the second stage and were able to be contacted by telephone. Of those, 52 declined to participate in the survey, resulting in a survey response rate of 74.8% (n = 154). Patients who had incomplete medical records were then excluded, leaving a final total of 70 female subjects who underwent reduction mammoplasty for non-oncological indications.
Overall and aesthetic satisfaction were also surveyed following the procedure and assessed with a 5-point Likert scale with 2 verbal anchors (1 = dissatisfied, 5 = very satisfied). Patient demographics, perioperative course, and postoperative complications were extracted from electronic medical records. Preoperative BMI was classified according to the World Health Organisation Clinical Guidelines adopted by the National Institute of Health.[27] The data were tabulated in Microsoft Excel (Microsoft 2016, Redmond, Washington) and analysis completed with IBM SPSS Software Version 24.0 (IBM Corp, Armonk, NY). Differences in continuous data were evaluated with the analysis of variance (ANOVA) and Kruskal–Wallis tests. The χ-squared test was used to calculate significance in difference between categorical data. Statistical significance was determined by a value of P ≤.05.
3. Results
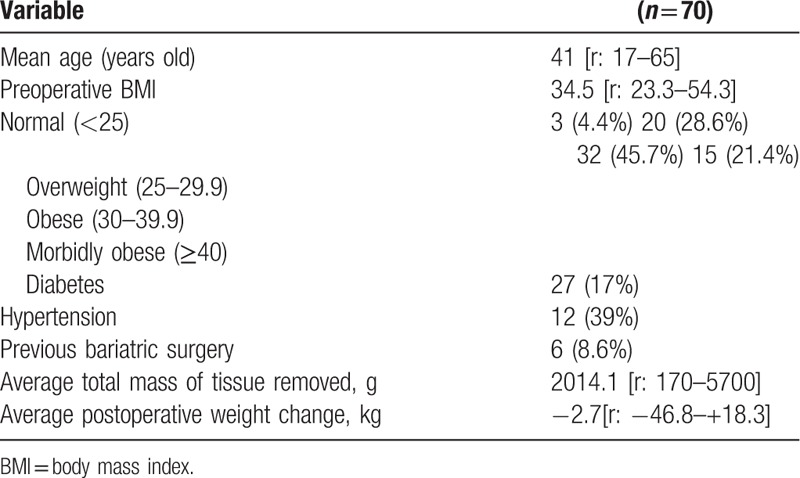
A total of 70 female subjects who underwent reduction mammoplasty for non-oncological indications were included in this study. A summary of participant demographics can be found in Table 2. The median follow-up time was 6 years [range: 5–12 years]. The average preoperative BMI classification was also the most prevalent within our study: obese. The majority of patients lost weight following reduction mammoplasty (53%), with an average weight loss of 2.7 kg (6.0lbs) per person. The most common preoperative symptoms were back pain (80%) and shoulder grooving (49%). Other symptoms that were reported included posture problems (34%), rash (34%), and difficulty breathing (11%). After reduction mammoplasty, 78.6% of participants reported that preoperative symptoms were completely or mostly resolved and 71.4% stated that there was no recurrence in symptoms. 93% of patients were happy with their surgery. The median aesthetic and overall satisfaction scores on a 5-point Likert scale were high (4 and 5, respectively).
Table 2.
Patient characteristics.
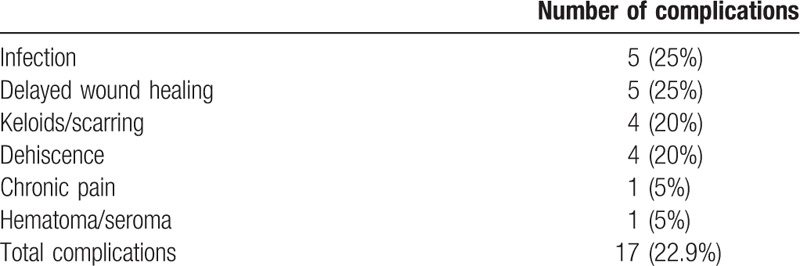
Complications were identified in 17 patients (24%). Most were local wound healing complications and are listed in Table 3. The most common complications were infection (n = 5) and delayed wound healing (n = 5).
Table 3.
Complications following reduction mammoplasty.
3.1. Preoperative BMI analysis (Table 4)
Table 4.
Breast reduction outcomes across different body mass index (BMI) groups.
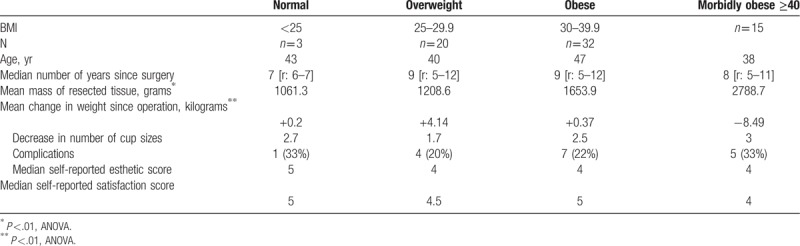
The cohort was subdivided according to BMI to create 4 groups: normal (<25), overweight (25–29.9), obese (30–39.9), and morbidly obese (≥40). Those with a high BMI had significantly larger amounts of breast tissue resected than the groups with lower BMIs, i.e. the higher the BMI, the greater the mass of breast tissue resected (P <.01, ANOVA). Additionally, those with morbidly obese patients lost more weight since surgery than other BMI groups (P <.01, ANOVA).
No statistical difference was found between the BMI groups for complication rate (P = .79, χ-squared test), median overall satisfaction (P = .70, Kruskal–Wallis test) or median aesthetic satisfaction (P = .31, Kruskal–Wallis test).
3.2. Satisfaction analysis (Table 5)
Table 5.
Breast reduction outcomes according to satisfaction score.
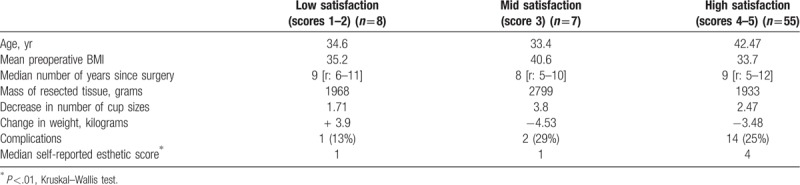
The study group was also separated according to overall satisfaction on the 5-point Likert scale to give 3 categories: low (scores 1–2), mid (score 3), and high (scores 4–5) satisfaction. There was significance between self-reported satisfaction and aesthetic scores, as those with high satisfaction also reported a higher aesthetic satisfaction than low and mid overall satisfaction scores (P <.01, Kruskal–Wallis test). There were no differences between satisfaction groups and BMI (P = .07, ANOVA), weight change (P = .314, ANOVA), or complication rate (P = .78, χ-squared test).
4. Discussion
Reduction mammoplasty can improve the quality of life for patients with macromastia by alleviating physical symptoms, increasing psychosocial wellbeing, and enhancing functional status;[2–4,22] however, these reports result from short term studies that possess limited follow-up. Our study provides a 12-year perspective of patient outcomes following reduction mammoplasty. It demonstrates that women who undergo reduction mammoplasty have high levels of satisfaction that is sustained for 12 years postoperatively, as well as resolution of physical symptomatology.
We did not find any difference in postoperative complication rate or satisfaction between BMI groups. This conflicts with most of the current literature[7–10] that describes increased postoperative complications in patients with high BMI classifications. The literature also describes longer operative times and increased hospitalization costs in those with larger body habitus. However, it provides evidence to those who advocate for reduction mammoplasty in the obese population;[14] the long-term benefits of breast reduction surgery (high patient satisfaction, resolution of symptoms) appear to exceed the risks of postoperative complications and increased healthcare burden. Additionally, we found that those with an increased BMI had a larger mass of breast tissue resected which correlates with the literature.[20] Interestingly, patients with a morbidly obese BMI reported a greater weight loss than other BMI groups, perhaps due to their renewed capacity for exercise. Although caution must be taken when interpreting these results given the larger interval between the operation and survey completion and the influence of external factors that influence weight, such as emotional state and socioeconomics.
Satisfaction was independent of BMI, weight change, or complications. This is in contrast to Corridi et al[28] who found that patients were dissatisfied with breast appearance following massive weight loss with or without preceding breast reduction surgery, suggesting that postoperative weight loss can influence patients’ aesthetic assessment of their breasts. It is also possible that our lower-than-expected complication rates for obese and morbidly obese patients[7–10] may influence the reported satisfaction. Additionally, in contrast to the literature which details hematoma, delayed wound healing and partial or complete nipple loss as common complications following reduction mammoplasty in obese patients, the majority of complications within our cohort were minor. It is possible that the resolution of preoperative symptoms and functional restoration compensate for any potential minor complication suffered. In fact, Nguyen et al[29] found that patients still reported high patient satisfaction despite experiencing a complication rate and major complications, such as decreased nipple sensitivity. We acknowledge that patients within the morbidly obese BMI classification (≥40) may also benefit from bariatric surgery and weight loss programs before breast reduction. Although weight loss is essential for improvement of overall health, it does not guarantee alleviation of macromastia symptoms[30] but can convert patients into insurance eligible candidates for reduction mammoplasty. Therefore, surgeons also face the task of deciding the best treatment pathway for patients, and whether weight loss is advisable before reduction surgery.
Patients with low satisfaction scores cited reasons of: amount of breast tissue removed (too much or too little), return of hypertrophy or poor aesthetic outcome. Conversely, those with high overall satisfaction had significantly higher self-reported aesthetic satisfaction, that is, how well the patient perceives their breasts to look impacts how happy they are after surgery, which is not a new notion.[23,31] Previous studies have reported patient outcomes following reduction mammoplasty at different time points and found that satisfaction is stable in the immediate and shot-term postoperative period.[18,19] This is supported by our finding of high overall and aesthetic satisfaction present even 12 years after breast reduction. Thus, demonstrating that reduction mammoplasty has a clinically important and robust benefit.
Our study can be separated into 2 portions: the questionnaire and the chart review; the former is limited due by potential recall bias, and the latter by its retrospective nature. Furthermore, our study only assesses postoperative patient satisfaction, while prior studies compare preoperative survey results to postoperative results.[19,20,28] Due to the retrospective nature of the review, we did not have the opportunity to survey patients before their surgeries. Although a high response rate was achieved, a smaller subset of patients was included in this study due to incomplete medical records thus limiting the external validity of the results. Additionally, there was a low sample size overall and within the subgroups, thus, decreasing our statistical power and ability to assess the impact of BMI on outcomes. Thus, caution must be taken when drawing conclusions. Another significant limitation is the use of a non-validated questionnaire. Although the BREAST-Q[32] is commonly used to evaluate patient-reported outcomes after reduction mammoplasty, we chose to implement a novel survey with questions that were tailored to capture all symptoms and the complete patient experience following reduction mammoplasty and allow a holistic evaluation of long-term outcomes. Elements were based on key themes in the BREAST-Q (excluding sexual functioning due to the impersonal nature of phone calls when discussing sensitive issues) and a 5-point Likert scale is used instead of the 4-point score. Through our qualitative-style questions, we were able to collect descriptive patient experiences. We found that all the issues raised by the patients in our study are incorporated within the BREAST-Q, highlighting its potential efficacy in assessing long term patient-related outcomes, and an avenue for further research. Additionally, our aim was to create a more focused survey that could easily be administered over the telephone to increase survey compliance and response rate, which the novel survey achieved (74.8%).
Patients with breast hypertrophy experience high levels of satisfaction after reduction mammoplasty independent of BMI. Additionally, satisfaction was not impacted by postoperative complications, or amount of breast tissue resected. Complication rates were not significantly different between different BMI groups. We advocate against the exclusion of patients from breast reduction surgery due to BMI alone and fear of increased complication rate strictly based on BMI; instead BMI must form part of the patient's overall health assessment and treatment plan, wherein a responsible preoperative counseling should include recommendation for weight loss before an elective procedure such as breast reduction for obese patients.
Author contributions
Conceptualization: Jennifer Bai, Adekunle Elegbede, Chinezimuzo Ihenatu, Arthur Nam, Sheri Slezak, Yvonne Rasko.
Data curation: Ledibabari Mildred Ngaage, Jennifer Bai, Chinezimuzo Ihenatu, Sheri Slezak, Yvonne Rasko.
Formal analysis: Ledibabari Mildred Ngaage, Selim Gebran, Adekunle Elegbede, Arthur Nam, Yvonne Rasko.
Investigation: Ledibabari Mildred Ngaage, Adekunle Elegbede, Sheri Slezak, Yvonne Rasko.
Methodology: Jennifer Bai, Selim Gebran, Chinezimuzo Ihenatu, Arthur Nam, Yvonne Rasko.
Project administration: Ledibabari Mildred Ngaage, Yvonne Rasko.
Resources: Arthur Nam, Sheri Slezak, Yvonne Rasko.
Software: Selim Gebran.
Supervision: Adekunle Elegbede, Sheri Slezak, Yvonne Rasko.
Validation: Ledibabari Mildred Ngaage, Selim Gebran, Adekunle Elegbede, Chinezimuzo Ihenatu, Arthur Nam, Yvonne Rasko.
Writing – original draft: Ledibabari Mildred Ngaage, Jennifer Bai.
Writing – review & editing: Ledibabari Mildred Ngaage, Jennifer Bai, Selim Gebran, Adekunle Elegbede, Chinezimuzo Ihenatu, Arthur Nam, Sheri Slezak, Yvonne Rasko.
Footnotes
Abbreviation: BMI = body mass index.
The authors report no conflicts of interest.
References
- [1].Kerrigan CL, Collins ED, Striplin D, et al. The health burden of breast hypertrophy. Plast Reconstr Surg 2001;108:1591–9. [DOI] [PubMed] [Google Scholar]
- [2].Chadbourne EB, Zhang S, Gordon MJ, et al. Clinical outcomes in reduction mammaplasty: a systematic review and meta-analysis of published studies. Mayo Clin Proc 2001;76:503–10. [DOI] [PubMed] [Google Scholar]
- [3].Boschert MT, Barone CM, Puckett CL. Outcome analysis of reduction mammaplasty. Plast Reconstr Surg 1996;98:451–4. [DOI] [PubMed] [Google Scholar]
- [4].Raispis T, Zehring RD, Downey DL. Long term functional results after reduction mammoplasty. Ann Plast Surg 1995;34:113–6. [DOI] [PubMed] [Google Scholar]
- [5].Nguyen JT, Wheatley MJ, Schnur PL, et al. Reduction mammaplasty: a review of managed care medical policy coverage criteria. Plast Reconstr Surg 2008;121:1092–100. [DOI] [PubMed] [Google Scholar]
- [6].Ngaage LM, Ngaage KC, Ngaage DL. The challenges of the postoperative care of obese patients. Analg Resusc: Curr Res 2015;4:2doi:10.4172/2324-903X.1000135. [Google Scholar]
- [7].Wirthmann AE, Welsch L, Wellenbrock SV, et al. Reduction mammoplasty in adolescents and elderly: a ten year case series analyzing age related outcome with focus on safety and complications. J Plast Reconstr Aesthet Surg 2018;71:377–83. [DOI] [PubMed] [Google Scholar]
- [8].Chen CL, Shore AD, Johns R, et al. The impact of obesity on breast surgery complications. Reconstr Surg 2011;128:395e–402e. [DOI] [PubMed] [Google Scholar]
- [9].Shah R, Al-Ajam Y, Stott D, et al. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthetic Surg 2011;64:508–14. [DOI] [PubMed] [Google Scholar]
- [10].Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified. J Plast Reconstr Aesthetic Surg 2009;62:195–9. [DOI] [PubMed] [Google Scholar]
- [11].Chun YS, Schwartz MA, Gu X, et al. Body mass index as a predictor of postoperative complications in reduction mammoplasty. Plast Reconstr Surg 2012;129:228e–33e. [DOI] [PubMed] [Google Scholar]
- [12].Fisher JP, Cleveland EC, Shang EK, et al. Complications following reduction mammoplasty: a review of 3538 cases from the 2005-2010 NSQIP data sets. Aesth Surg J 2014;34:66–73. [DOI] [PubMed] [Google Scholar]
- [13].Gamboa-Bobadilla GM, Killingsworth C. Large-volume reduction mammaplasty: the effect of body mass index on postoperative complications. Ann Plast Surg 2007;58:246–9. [DOI] [PubMed] [Google Scholar]
- [14].Roehl K, Craig ES, Gómez V, et al. Breast reduction: safe in the morbidly obese. Plast Reconstr Surg 2008;122:370–8. [DOI] [PubMed] [Google Scholar]
- [15].Kalliainen LK. ASPS Health Policy Committee. ASPS clinical practice guidelines summary on reduction mammoplasty. Plast Reconstr Surg 2012;130:785–9. [DOI] [PubMed] [Google Scholar]
- [16].Sutinen M, Eskelinen E, Kääriäinen M. Overweight is associated with increased incidence of minor complications after reduction mammoplasty: a retrospective analysis of 453 consecutive cases. Scand J Surg 2018;107:230–5. [DOI] [PubMed] [Google Scholar]
- [17].Radosa JC, Radosa MP, Baum S, et al. Reduction mammaplasty for symptomatic macromastia: which factors influence the post-operative outcome. Arch Gynecol Obstet 2013;287:715–22. [DOI] [PubMed] [Google Scholar]
- [18].Cohen WA, Homel P, Patel NP. Does time affect patient satisfaction and health-related quality of life after reduction mammoplasty. Eplasty 2016;16:e7. [PMC free article] [PubMed] [Google Scholar]
- [19].Cabral IV, da Silva Garcia E, Sobrinho RN, et al. Use of the BREAST-Q™ survey in the prospective evaluation of reduction mammaplasty outcomes. Aesthetic Plast Surg 2018;42:388–95. [DOI] [PubMed] [Google Scholar]
- [20].Gonzalez MA, Glickman LT, Aladegbami B, et al. Quality of life after breast reduction surgery: a 10-year retrospective analysis using the Breast Q questionnaire: does breast size matter. Ann Plast Surg 2012;69:361–3. [DOI] [PubMed] [Google Scholar]
- [21].Chao JD, Memmel HC, Redding JF, et al. Reduction mammaplasty is a functional operation, improving quality of life in symptomatic women: A prospective, single-center breast reduction outcome study. Plast Reconstr Surg 2002;110:1644–52. [DOI] [PubMed] [Google Scholar]
- [22].Thoma A, Sprague S, Veltri K, et al. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg 2007;120:13–26. [DOI] [PubMed] [Google Scholar]
- [23].Klassen A, Fitzpatrick R, Jenkinson C, et al. Should breast reduction surgery be rationed? A comparison of the health status of patients before and after treatment: postal questionnaire survey. Br Med J 1996;313:454–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Tykka E, Asko-Seljavaara S, Hietanen H. Patients’ satisfaction with breast reconstruction and reduction mammoplasty. Scand J Plast Reconstr Surg Hand Surg 2002;35:399–405. [DOI] [PubMed] [Google Scholar]
- [25].Blomqvist LMD, Brandberg YP. Three-year follow-up on clinical symptoms and health-related quality of life after reduction mammaplasty. Plast Reconstr Surg 2004;114:49–54. [DOI] [PubMed] [Google Scholar]
- [26].Jones SA, Bain JR. Review of data describing outcomes that are used to assess changes in quality of life after reduction mammaplasty. Plast Reconstr Surg 2001;108:62–7. [DOI] [PubMed] [Google Scholar]
- [27].NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda (MD): National Heart, Lung, and Blood Institute; 1998 Sep. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2003/ Accessed June 12, 2019. [Google Scholar]
- [28].Coriddi M, Koltz PF, Gusenoff JA. Reduction mammaplasty, obesity, and massive weight loss: temporal relationships of satisfaction with breast contour. Plast Reconstr Surg 2011;128:643–50. [DOI] [PubMed] [Google Scholar]
- [29].Nguyen JT, Palladino H, Sonnema AJ, et al. Long-term satisfaction of reduction mammoplasty for bilateral symptomatic macromastia in younger patients. J Adolesc Health 2013;53:112–7. [DOI] [PubMed] [Google Scholar]
- [30].Geiker NR, Horn J, Astrup A. Preoperative weight loss program targeting women with overweight and hypertrophy of the breast - a pilot study. Clin Obes 2017;7:98–104. [DOI] [PubMed] [Google Scholar]
- [31].Gardikiotis I, Azoicai D, Popa M, et al. The impact of body image and self-perceived physical ability on the well-being after mastectomy without reconstruction. J Surg 2015;11:143–9. [Google Scholar]
- [32].Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 2009;124:345–53. [DOI] [PubMed] [Google Scholar]


