Abstract
Background
During emergency medicine (EM) training, residents are exposed to a wide spectrum of patient complaints. We sought to determine how resident clinical experience changes based on training level in relation to the patient acuity levels, chief complaints, and dispositions.
Methods
We performed a retrospective chart review of patients seen at a safety‐net, academic hospital in Los Angeles from July 1, 2015, to June 30, 2016. Resident postgraduate year (PGY) level and specialty, patient acuity (based on the Emergency Severity Index), chief complaint (based on one of 30 categories), and disposition were abstracted. Our primary objective was to examine the progression of EM resident experience throughout the course of training. As a secondary objective, we compared the cases seen by EM and off‐service PGY‐1s.
Results
A total of 49,535 visits were examined, and of these, 32,870 (66.4%) were in the adult ED (AED) and 16,665 (33.6%) were in the pediatric ED (PED). The median acuity level was 3, and 27.4% of AED patients and 7.3% of PED patients were admitted. Data from 126 residents were analyzed. This included 94 PGY‐1 residents (16 EM and 78 off‐service), 16 PGY‐2 EM, and 16 PGY‐3 EM residents. Residents of different training levels evaluated different types of patients. Senior EM residents were more likely to care for higher‐acuity patients than junior EM residents. EM PGY‐3s saw higher percentages of acuity level 1 and 2 patients (2.3 and 37.8%, respectively, of their total patients) than EM PGY‐1s (0.3 and 18.7%, respectively). Conversely, EM PGY‐1s saw higher percentages of acuity level 4 and 5 patients (27.9 and 1.6%, respectively) compared to EM PGY‐3s (10.7 and 0.7%, respectively). There was a significant linear trend for increasing acuity with training year among EM residents (p < 0.001). EM PGY‐1s saw more patients than off‐service PGY‐1s with slightly higher acuities and admission rates.
Conclusion
The clinical experience of EM residents varies based on their level of training. EM residents show a progression throughout residency and are more likely to encounter higher volumes of patients with higher acuity as they progress in their training. When designing EM residency curriculums, this is a model of an EM residency program.
Residents who work in the emergency department (ED) see a variety of patients with varying acuity levels, chief complaints, and diagnoses.1, 2, 3, 4, 5, 6, 7, 8, 9 Emergency medicine (EM) residents often have some control over the number and types of patients they evaluate, since residents in the ED may choose to assign themselves to patients or leave them for their coresidents to see. This may lead to variation in clinical experience among EM residents.
Multiple studies have evaluated the clinical experiences of EM residents, typically focusing on factors such as resident productivity, procedural experience, and types of patients seen.1, 2, 3, 4, 5, 6, 7, 8, 9 Residents see more patients per hour1, 2, 3 and generate more RVUs per hour4 as they progress in their training. They also see more patients per hour when they work shorter shifts.5 While productivity generally increases as residents progress in their training,1, 2, 3 interestingly, a study by Henning et al.6 found that while EM interns increase productivity significantly over the course of a year, senior EM residents’ productivity did not change significantly. Procedural experience varies among different residency types and settings.7 Residents may not be exposed to all important pathology. In fact, in a study by Langdorf et al.,3 participating residents did not see a large number of core EM diagnoses during a 9‐month study period. Another study compared types of patients seen by EM and pediatric residents in a pediatric ED and found that EM residents see more surgical patients, while pediatric residents see more medical patients.8 Finally, two studies compared the training experiences of EM residents in urban versus rural training environments and found that overall experiences were similar with the exception that patients in urban training sites had overall higher acuities, and residents at these sites performed more procedures.9, 10 Despite this body of literature evaluating EM training experience, none to our knowledge have quantified differences among the types of patients seen by residents based on their training level.
The aim of our study was to evaluate the clinical experiences of residents in the ED based on their level of training. We hypothesized that residents at different training levels see different types of patients in the ED with varied acuity levels, chief complaints, and resulting dispositions. Our primary objective was to examine the progression of EM resident experience throughout the course of training. As a secondary objective, we compared the cases seen by EM and off‐service postgraduate year (PGY)‐1s.
Methods
Study Design
This was a retrospective chart review conducted at Harbor–UCLA Medical Center, including data from July 1, 2015, to June 30, 2016. Electronic medical records for all patients seen in the adult or pediatric ED who were seen by a resident during this time frame were reviewed. For each patient encounter, a predetermined data collection form was completed including: resident PGY level, gender and specialty, patient acuity level, chief complaint, and disposition. Acuity was classified based on the Emergency Severity Index.11, 12, 13 The chief complaint recorded by the triage nurse was categorized into one of 30 categories determined by the study team based on previously published data of the most common chief complaints.14, 15 Categorization was reviewed by a second investigator and any discrepancies were reviewed by a third investigator. Resident shift schedules were reviewed and tabulated for the number of adult and pediatric shifts to calculate the number and types of patients seen in each environment. As many patients seen by PGY‐1s are supervised by an upper‐level EM resident, both the PGY‐1 and the upper‐level resident were given credit for patients they saw together. Only the first resident of each year to see the patient was considered in the analysis, so residents who assumed care of a patient in sign‐out were not credited with the encounter.
Study Setting and Population
Harbor–UCLA Medical Center is a large, urban, academic safety‐net hospital, located in Los Angeles with nearly approximately 90,000 ED visits per year. Harbor–UCLA Medical Center serves a diverse county population made up of approximately 55% Latino, 20% African American, 18% Caucasian, and 7% other patients with a large percentage of non–English‐speaking patients. The hospital includes adult, pediatric, and psychiatric EDs. For this study, patients presenting primarily to the psychiatric ED were not included (i.e., those who were not seen or only had a medical screening exam in adult ED [AED] or pediatric ED [PED]), while patients with psychiatric complaints who were seen in the AED or PED were included in the study. The remaining patient encounters to the AEDs and PEDs were reviewed for the period between July 1, 2015, and June 30, 2016. Patients were excluded from analysis if they were not seen by an intern or ED resident (i.e., patients only seen by attending physicians, nurse practitioners or off‐service upper‐year rotating residents) since the primary aim of the study was to evaluate the experience of EM residents. Off‐service interns were included in the study because they regularly work under the supervision of upper‐level EM residents, while more senior off‐service rotators do not.
At the time of our study, Harbor–UCLA's EM residency program consisted of 3 years of training with 16 residents per year. The AED has off‐service rotating residents from multiple departments, including internal medicine, psychiatry, orthopedics, combined internal medicine and pediatrics, and family medicine. The PED is primarily staffed by EM, pediatrics, and family medicine residents. Off‐service upper‐level residents rotating in the ED were excluded as we expected the heterogeneity of their training experience to make it difficult to draw generalizable conclusions about their ED experience. Shifts in the AED average 9.5 hours, with 6.5 hours devoted to seeing new patients, 2 hours for sign out and teaching and 1 hour for cleanup and note writing time at the end of the shift, while shifts in the PED average 8.5 hours, which is entirely dedicated to patient care with the exception of 30 minutes of cleanup and note writing time at the end of the shift. A typical AED shift has one PGY‐2 and ‐3 resident and often a PGY‐1. During signouts PGY‐2s receive signouts on more active patients while PGY‐3s receive signouts on patients that have been dispositioned or with less active issues. EM and off‐service residents from all levels of training are encouraged to see a wide range of types of patients to gain a variety of clinical experiences. Residents are not restricted in the types of patients they see with the exception of trauma activated patients who are only seen by PGY‐2s and ‐3s. At the time of the study, there were no lower‐acuity areas of the ED covered by residents; however, there was a fast‐track area managed by nurse practitioners. As a result, residents naturally saw a selection of different acuity patients on shifts. Attending physicians do not see patients primarily except during weekly resident conference, and that data were excluded from analysis.
Confidentiality and Ethics Approval
The study was approved by the Los Angeles Biomedical Research Institute Institutional Review Board. Residents and patients were deidentified to protect confidentiality prior to analysis.
Data Analysis
Data was exported from the Cerner electronic health record into Excel 2013 (Microsoft Corp.). Subsequent deidentification, manipulation, and analysis was done in STATA IC 15 (StataCorp). All data points were exported in an automated fashion by queries created and validated by an investigator who is familiar with the data structure of our system. The queries were compared to the results of manual chart review and modified until no further discrepancies were found. Significant trends in the number of patients seen, acuity levels, and the proportion of patients admitted versus discharge by class year were determined by linear and logistic regression models. Median acuity levels between EM and off‐service PGY‐1 residents were compared by the Wilcoxon rank‐sum test.
Results
Patient Characteristics
A total of 49,535 patient visits were included in the analysis (Figure 1). Crediting both the intern and the supervising upper‐level resident who saw a patient together resulted in 56,669 resident–patient encounters for analysis. The demographics and dispositions of the included patient encounters are shown in Table 1.
Figure 1.
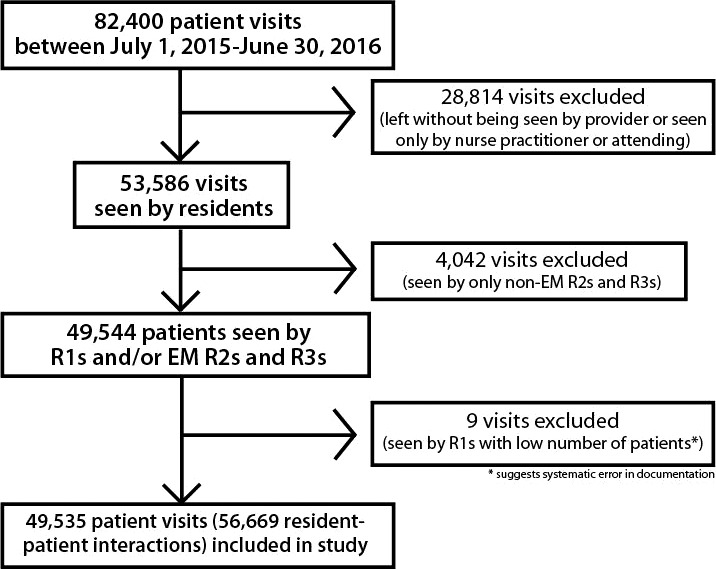
Study flow diagram.
Table 1.
Patient Characteristics
| AED | PED | |
|---|---|---|
| Demographics | ||
| Total visits | 32,870 | 16,665 |
| Mean age (years) | 49.5 | 9.1 |
| Median age (years) | 50 | 8 |
| Male, n (%) | 16,953 (51.6) | 8,739 (52.4) |
| Acuity level | ||
| Median acuity level | 3 | 3 |
| Dispositions, n (%)a | ||
| Discharged | 22,100 (67.2) | 14,916 (89.5) |
| Admitted | 9,012 (27.4) | 1,218 (7.3) |
| Transferred to other evaluation area at this facilityb | 668 (2.0) | 255 (1.5) |
| Interfacility transfer | 590 (1.8) | 138 (0.8) |
| Expired | 133 (0.4) | 3 (0.0) |
AED = adult ED; PED = pediatric ED.
Does not sum to total because of some missing dispositions, rare dispositions such as erroneous registration.
Transferred to other area of the hospital includes the psychiatric ED, labor, and delivery, etc.
Resident Characteristics
A total of 126 residents were included in the study: 16 EM PGY‐1s, 78 off‐service PGY‐1s, 16 PGY‐2s, and 16 PGY‐3s. Data from 13 non‐EM interns were excluded because of extremely low numbers of patients seen per shift, suggesting incomplete data from not signing up for patients in the electronic health record. Number of males in each PGY group were as follows: five (31.2%) EM PGY‐1s, 47 (60.3%) off‐service PGY‐1s, 11 (68.9%) EM PGY‐2s, and nine (56.3%) EM PGY‐3s. EM PGY‐1s spent slightly less of their total shifts in the AED (47.9%) compared to the PED, while off‐service interns, EM PGY‐2s and EM PGY‐3s spent more of their time in the AED (83.7, 79.3, and 80.2%, respectively).
Main Results
There was a significant linear increase in the number of patients seen by EM residents over the course of their training in the adult but not the pediatric EDs (Table 2). In an average AED shift, EM PGY‐1s saw 4.8 patients (0.7 patients/hour), PGY‐2s saw 7.8 patients (1.2 patients/hour), and PGY‐3 saw 8.2 patients (1.3 patients/hour). In an average PED shift, EM PGY‐1s saw 8.6 patients (1.1 patient/hour), PGY‐2s saw 11.3 patients (1.4 patients/hour), and PGY‐3 saw 9.9 patients (1.2 patients/hour). Patients/hour data only reflects new patients/hour seen during clinical hours of the shift (excludes education, signout, and end‐of‐shift note writing/cleanup time) and does not include patients received in signout, which make up a significant portion of resident workload, or any fast track patients, who were only seen by nurse practitioners at the time of the study. The number of patients seen per shift increased significantly from the EM PGY‐1 to the PGY‐2 years (p < 0.001) but not between the PGY‐2 and PGY‐3 years (p < 1).
Table 2.
Number of Patients Seen by EM PGY Year
| PGY‐1a | PGY‐2 | PGY‐3 | p‐value | |
|---|---|---|---|---|
| Patients seen during year per resident | 469 (±99) | 1,332 (±192) | 1,383 (±151) | |
| Adult patients seen | 152 (±32) | 969 (±130) | 1,065 (±158) | |
| Pediatric patients seen | 318 (±85) | 363 (±81) | 317 (±58.5) | |
| Patients per shift | 6.6 (±1.3) | 8.5 (±1.0) | 8.6 (±0.9) | <0.001b |
| Patients per AED shift | 4.5 (±0.9) | 7.8 (±0.8) | 8.2 (±1.0) | <0.001b |
| Patients per PED shift | 8.6 (±2.1) | 11.3 (±2.6) | 9.9 (±1.4) | 0.1a |
Data are reported as mean (±SD).
Only includes EM PGY‐1 encounters and does not include off‐service PGY‐1 encounters.
Significance of the provider's PGY in a linear regression model for the number of patients seen per shift.
Patient acuity levels seen by each PGY group in the combined AED and PED settings are shown in Table 3. There was a significant linear trend for higher acuity patients (lower ESI score) over the course of residency among EM residents (p < 0.0001). This trend in increasing acuity remained significant at p < 0.001 when comparing just EM PGY‐1s to EM PGY‐2s and just PGY‐2s to PGY‐3s. PGY‐3s saw the highest percentage of acuity level 1 patients, followed by PGY2s (p < 0.001). EM PGY‐1s saw the highest percentage of acuity level 4 and 5 patients compared with senior EM residents.
Table 3.
Acuity by PGY Level
| Acuity Level, ESI Scorea | Total Patientsb | PGY‐1c | PGY‐2 | PGY‐3 | p‐value among EM residents | |
|---|---|---|---|---|---|---|
| EM | Off‐service | |||||
| Median (IQR) | 3 (2–3) | 3 (3–4) | 3 (2–3) | 3 (2–3) | 3 (2–3) | <0.001d |
| 1 | 955 (1.9) | 19 (0.3) | 14 (0.3) | 440 (2.1) | 511 (2.3) | <0.001e |
| 2 | 15,633 (31.6) | 1,402 (18.7) | 1,695 (29.8) | 7,319 (34.2) | 7,875 (37.8) | <0.001e |
| 3 | 24,377 (49.2) | 3,823 (50.9) | 2,937 (51.6) | 10,432 (48.9) | 10,949 (49.5) | <0.5e |
| 4 | 7,485 (15.1) | 2,096 (27.9) | 906 (15.9) | 2,696 (12.6) | 2,365 (10.7) | <0.001e |
| 5 | 488 (1.0) | 121 (1.6) | 70 (1.2) | 179 (0.84) | 148 (0.7) | <0.5e |
Data are reported as n (%) unless otherwise reported.
ESI = Emergency Severity Index; IQR = interquartile range.
ESI Score, 1 is the most acute.
Actual number of patient visits, includes total number of patients who had acuity data available.
Number of resident–patient interactions, crediting both the PGY‐1 and the supervising PGY‐2 or PGY‐3 with the encounter.
Includes only EM residents and refers to the significance of PGY on the ESI in a linear regression model.
Refers to the significance of PGY on the proportion with that ESI score in a logistic regression model.
EM PGY‐1 residents saw significantly more patients per shift than their off‐service PGY‐1 counterparts in the adult (p < 0.001) but not the pediatric EDs (p < 0.2). On average EM PGY‐1s saw 6.6 patients per shift, 4.47 (0.7 patients/hour) in the AED and 8.6 (1.1 patients/hour) in the PED, while off‐service PGY‐1s saw 3.6 patients per shift, 2.76 (0.4 patients/hour) in the AED and 7.4 (0.9 patients/hour) in the PED. These levels of significance were similar in a sensitivity analysis including the 13 off‐service PGY1 residents who had been excluded based on the assumption of a systemic error in signing up for patients. The median acuity of patients seen by both EM and off‐service PGY‐1 residents was 3, but because of the large sample size, the acuity of patients seen by the EM PGY‐1s was significantly greater (p < 0.0001). This difference was so small that it becomes nonsignificant when AED and PED visits were analyzed separately. EM PGY‐1s admitted a significantly higher percentage of patients than their off‐service PGY‐1 counterparts (p < 0.001); however, in a model accounting for the balance of adult versus pediatric shifts, this difference became insignificant (p < 0.5).
The most common chief complaints are shown in Table 4. Over the course of their residency, EM residents saw a significantly greater proportion of trauma patients and significantly lesser proportion of patients with musculoskeletal complaints when accounting for the distribution of adult versus pediatric shift. The most over‐ and underrepresented chief complaints (i.e., complaints seen disproportionately more by a given PGY group than the overall prevalence of the complaint) are shown in Figure 2.
Table 4.
Most Common Chief Complaints by PGY Group
| Overall‐ n(%) | p‐valuea | EM PGY‐1 | Off‐service PGY‐1 | PGY‐2 | PGY‐3 |
|---|---|---|---|---|---|
| Abdominal (Abd) pain, 7,231 (14.6%) | 0.86 | Abd pain, 884 (11.8%) | Abd pain, 926 (16.3%) | Abd pain, 3,207 (15.0%) | Abd pain, 3,517 (15.9%) |
| Other, 5,983 (12.1%) | 0.48 | Other, 720 (9.6%) | Other, 650 (11.4%) | Other, 2,713 (12.7%) | Other, 2,709 (12.2%) |
| Trauma, 4,007 (8.1%) | 0.001 | URI/throat, 690 (9.2%) | MSK, 414 (7.3%) | Trauma, 1,769 (8.3%) | Trauma, 1,833 (8.3%) |
| Musculoskeletal (MSK), 3,487 (7.0%) | 0.005 | Fever, 667 (8.9%) | Chest pain, 393 (6.9%) | Chest pain, 1,513 (7.1%) | Chest pain, 1,628 (7.4%) |
| Upper respiratory infection (URI)/throat, 2,894 (5.9%) | 0.74 | MSK, 663 (8.9%) | URI/throat, 365 (6.4%) | MSK, 1,466 (6.9%) | MSK, 1,410 (6.4%) |
Data are reported as n (%).
p‐value refers to the difference in proportion of patients seen with that chief complain between EM PGY groups
Figure 2.
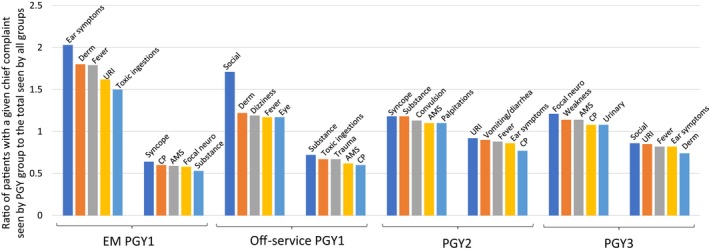
Most over‐ and underrepresented chief complaints seen by each PGY.
Dispositions by PGY levels are summarized in Table 5. In a logistic regression model accounting for the distribution of pediatric and adult shifts, EM residents saw a significantly decreasing proportion of patients who were discharged and significantly increasing proportion of those were admitted or died. The majority of patients who expired were seen by PGY‐2s and PGY‐3s. The proportion of patients who were admitted increased significantly from the EM PGY‐1 to the PGY‐2 years (p < 0.001) but not between the PGY‐2 and PGY‐3 years (p < 0.5).
Table 5.
ED Disposition by PGY Level
| Disposition | Total Patientsa | PGY‐1 | PGY‐2 | PGY‐3 | p‐value Among EM Residentsb | |
|---|---|---|---|---|---|---|
| EM | Off‐service | |||||
| Discharged | 37,016 (74.7) | 6,392 (85.0) | 4,419 (77.6) | 15,542 (72.9) | 15,834 (71.6) | <0.001 |
| Admitted | 10,230 (20.7) | 872 (11.6) | 1,034 (18.2) | 4,745 (22.3) | 5,196 (23.5) | <0.001 |
| Interhospital transfer | 728 (1.5) | 72 (1.0) | 87 (1.5) | 328 (1.5) | 375 (1.7) | <0.001 |
| To other evaluation area at this facility | 923 (1.9) | 114 (1.5) | 107 (1.9) | 416 (2.0) | 431 (2.0) | <0.001 |
| Expired | 136 (0.3) | 1 (0.0) | 3 (0.1) | 63 (0.3) | 72 (0.3) | <0.001 |
Data are reported as n (%).
Includes total number of patients who had disposition data available.
p‐value is for the comparison of EM residents only and refers to the linear trend over the course of training for the proportion with that disposition in a logistic regression model.
Discussion
Residency training is based on experiential growth in the knowledge and breadth of EM. Assuring that residents gain experience to master the knowledge and clinical skills necessary to practice EM is a primary goal of EM residency programs. Residents are encouraged to reach milestones throughout their training with graduated responsibilities and expectations as they advance in training.
Our study demonstrates not only that residents see more patients as they progress from PGY‐1 year to upper level years, as has been shown in prior literature,1, 2, 3 but also that residents at different training levels select different types of patients in the ED in terms of chief complaints and acuity levels. Our data support the desired clinical growth that residencies strive for, that EM residents further in their training see higher‐acuity patients and patients with more acute chief complaints. This difference was most pronounced between PGY‐1s and upper‐level residents, as one might expect. PGY‐2s and PGY‐3s saw similar numbers of patients per shift but saw higher‐acuity patients during the PGY‐3 year. While PGY‐2s and ‐3s saw similar numbers of patients, it is important to note that PGY‐2s tend to have more supervision, while PGY‐3s are more independent in their decision making and take on more of a leadership and teaching role in the ED. In our department, PGY‐3s are responsible for helping to manage patient flow for their team (keeping track of all the patients on the team, accepting patient transfers, and triaging patients), which may impact the number of patients they see and contribute to our findings. PGY‐2s do not begin to supervise PGY‐1s and medical students until the last few months of their PGY‐2 year, while PGY‐3s are responsible for this supervision throughout the year. This additional teaching and supervision time may impact the number of patients seen by PGY‐3s. Finally, PGY‐2s and PGY‐3s receive different types of patients in signout. PGY‐2s receive signouts for more active patients, while PGY‐3s receive signout on patients that have been dispositioned with less active issues. While the resident who receives a patient in signout is not credited for that patient in this study, patients that are signed out may impact the numbers of types of patients seen by PGY‐2s and ‐3s. We found that EM PGY‐1s see higher volumes of patients than off‐service PGY‐1s. This difference was only statistically significant in the AED. Additionally, EM PGY‐1s tend to see higher‐acuity patients and a higher percentage of patients who are admitted; however, these differences are small enough that they are only statistically significant when analyzing AED and PED data as a whole. EM PGY‐1s tend to favor patients with chief complaints that are generally thought to be less emergent, such as ear symptoms and skin symptoms, while they select relatively fewer patients with more critical chief complaints, such as syncope and chest pain. These findings appear to be secondary to the fact that EM PGY‐1s spend a higher percentage of their total time working in the PED (approximately 50%) where patients tend to present with less emergent chief complaints as compared to off‐service PGY‐1s (approximately 14%). It is important to note that EM PGY‐1s spend a total of 3 months rotating through the ED, while off‐service PGY‐1s only spend 1 month on average. Additionally, EM PGY‐1s typically have experience rotating through the ED as medical students, while off‐service PGY‐1s may not. Hence, it is likely that EM PGY‐1 experience level and comfort with ED logistics impact the numbers of types of patients seen.
Over the past 30 years, studies have shown that EM residents progress in their productivity and patient load over the course of their residencies.1, 2, 3, 4 Our study adds to this body of knowledge by demonstrating that the types of patients that residents choose to see also change over the course of their residency training. Educators can use this information to help coach residents at different training levels to expand the types of patients they see.
Future studies are needed to verify the trends observed in our study. It would be beneficial to perform a similar study over a longer time period at additional residency sites. In addition, given that we found that EM PGY‐2s and PGY‐3s see similar numbers and types of patients, we plan to perform a future study to assess resident autonomy.
Limitations
While this study is robust in its use of a large sample of an entire year of patient data, it is limited to a single year in a single residency program. We included a total of 126 residents over a 1‐year period, of whom 78 were off‐service interns who generally only rotate for 1 month in the AED or PED. On each team on a given AED shift, there is only one PGY‐1 resident, so off‐service PGY‐1s are not working during the same shifts as EM PGY‐1s and thus should not alter selection of their patients. However, EM PGY–2s only supervise PGY1s during the last few months of their PGY2 year, so this could potentially impact types of patients they see. While PGY‐1s are advised to see a range of types of patients, it is possible that they could gravitate toward certain types of patients (for example, an orthopedic intern may be interested in seeing patients with orthopedics injuries), which could impact the types of patients seen by the supervising senior residents. Different EM programs have different number of off‐service PGY‐1 rotators, so this could limit the generalizability of our secondary analysis comparing EM PGY‐1s to off‐service PGY‐1s. Given that each EM class size only consists of 16 residents, it is possible that differences observed between resident classes may be a result of differences in residents within individual classes as opposed to differences in levels of training. Also, the nature of patient flow in our department will be different from other departments. In our program, PGY‐3s supervise PGY‐1 and medical student encounters in the adult ED, while PGY‐2s are only allowed to supervise PGY‐1s and medical students in the last few months of their PGY‐2 year. Also, PGY‐2s take signout on patients whose evaluation is still in progress, while PGY‐3s assume care of those whose disposition is settled. These systematic differences in responsibilities between R‐2s and R‐3s would influence the number of type of patients they would independently see de novo. We excluded 56 upper‐level off‐service residents because we felt that their advanced level of training in different specialties was too heterogenous to categorize as a group and to compare this data to that of upper‐level EM residents. Upper‐level off‐service residents do not see any trauma‐activated patients but are otherwise allowed to choose to see any patients they wish to see. Based on our observations, upper‐level off‐service residents tend to see a range of types of patients. However, it is possible that the patients selected by this group could impact the patients selected by ED residents.
Another limitation of the study is that some data in the medical records were unavailable and may have affected the results if it were included. For example, 597 (1.2%) of patients had unknown acuity levels, and 502 (1.0%) of patients had unknown dispositions. This is an inherent problem with reviewing medical records as not all data are properly recorded and thus was unavoidable in the study. However, Cerner was implemented at our institution in October 2014, and electronic records are ideal for large‐volume chart review. In general, resident groups saw similar numbers of these patients with missing data. As 5,983 (12.1%) of patients had chief complaints that did not fall into one of the preset chief complaints, they were reported as “other.” If we had included more categories of chief complaints, we would have reduced the number of other diagnoses. However, our list was based on previously published literature and designed to be a useable length. Finally, this study was conducted at a single county institution with particular challenges such as limited resources and language barriers, so the results may not be generalizable to other residency programs with different curriculums patient populations and nuances in ED flow.
Conclusions
Our study shows that the clinical experience of emergency medicine residents varies based on their level of training. Emergency medicine residents show a progression throughout residency and are more likely to encounter higher volumes of patients with higher acuity as they progress in their training. Emergency medicine PGY‐1s tend to see a higher volume of patients with higher acuities and higher admission rates than off‐service interns, which is not surprising given their increased time and experience in the ED. Future multi‐institution studies over longer periods of time would help verify this trend. When designing emergency medicine residency curriculums, this a model of an emergency medicine residency program.
AEM Education and Training 2019;3:243–250
Presented at the American College of Emergency Physicians Scientific Assembly, Washington, DC, October 30, 2017.
The authors have no relevant financial information or potential conflicts to disclose.
Author contributions: AD contributed to study concept and design, data acquisition, analysis and interpretation of data, drafting and revision of the manuscript, and statistical expertise; KY contributed to data acquisition, analysis and interpretation of data, and drafting and revision of the manuscript; DL contributed to analysis and interpretation of data and revision of the manuscript; RJF contributed to study concept and design, data acquisition, analysis and interpretation of data, revision of the manuscript, and statistical expertise; JJ contributed to study concept and design, analysis and interpretation of data, and revision of the manuscript; and DAT contributed to study concept and design, analysis and interpretation of data, and revision of the manuscript.
References
- 1. DeBehnke D, O'Brien S, Leschke R. Emergency medicine resident work productivity in an academic emergency department. Acad Emerg Med 2000;7:90–2. [DOI] [PubMed] [Google Scholar]
- 2. Deveau J, Lorenz J, Hughs M, et al. Emergency medicine work productivity and procedural accomplishment. J Am Osteopath Assoc 2003;103:291–6. [PubMed] [Google Scholar]
- 3. Langdorf M, Strange G, Macneil P. Computerized tracking of emergency medicine resident clinical experience. Ann Emerg Med 1990;19:764–73. [DOI] [PubMed] [Google Scholar]
- 4. Brennan DF, Silvestri S, Sun JY, Papa L. Progression of emergency medicine resident productivity. Acad Emerg Med 2007;14:790–4. [DOI] [PubMed] [Google Scholar]
- 5. Jeanmonod R, Jeanmonod D, Ngiam R. Resident productivity: does shift length matter? Am J Emerg Med 2008;26:789–91. [DOI] [PubMed] [Google Scholar]
- 6. Henning DJ, McGillicuddy DC, Sanchez LD. Evaluating the effect of emergency residency training on productivity in the emergency department. J Emerg Med 2010;45:414–8. [DOI] [PubMed] [Google Scholar]
- 7. Hayden SR, Panacek EA. Procedural competency in emergency medicine: the current range of resident experience. Acad Emerg Med 1999;6:728–35. [DOI] [PubMed] [Google Scholar]
- 8. Whiteman PJ, Foltin GL. Physician bias during patient selection in the pediatric emergency department. Pediatr Emerg Care 1998;14:332–3. [PubMed] [Google Scholar]
- 9. Wadman MC, Fago B, Hoffman LH, Tran TP, Muelleman RL. A comparison of emergency medicine resident clinical experience in a rural versus urban emergency department. Rural Remote Health 2010;10:1442. [PubMed] [Google Scholar]
- 10. Waymack JR, Markwell S, Milbrandt JC, Clark TR. Comparison of rates of emergency department procedures and critical diagnoses in metropolitan and rural hospitals. Rural Remote Health 2015;15:3298. [PubMed] [Google Scholar]
- 11. Wuerz RC, Milne LW, Eitel DR, Travers D, Gilboy N. Reliability and validity of a new five‐level triage instrument. Acad Emerg Med 2000;7:236–42. [DOI] [PubMed] [Google Scholar]
- 12. Wuerz RC. Emergency Severity Index triage category is associated with six‐month survival. ESI Triage Study Group. Acad Emerg Med 2001;8:61–4. [DOI] [PubMed] [Google Scholar]
- 13. Wuerz RC, Travers D, Gilboy N, Eitel DR, Rosenau A, Yazhari R. Implementation and refinement of the Emergency Severity Index. Acad Emerg Med 2001;8:170–6. [DOI] [PubMed] [Google Scholar]
- 14. Malmström T, Torkki P, Valli J, Malmström R. Patient flow analysis of Hyvinkää Hospital joint emergency unit. Finnish Med J 2012;5:345–51. [Google Scholar]
- 15. Malmström T, Huuskonen O, Torkki P, Malmström R. Structured classification for ED presenting complaints ‐ from free text field‐based approach to ICPC‐2 ED application. Scand J Trauma Resusc Emerg Med 2012;20:76. [DOI] [PMC free article] [PubMed] [Google Scholar]


