Abstract
Objectives
CVS, the largest US pharmacy chain, discontinued selling tobacco products in 2014; meanwhile, Family Dollar and Dollar General, the two largest dollar store chains, began selling tobacco in 2012 and 2013, respectively. The purpose of this study is to evaluate the differential change in tobacco retailer density (TRD) by rurality throughout 12 Southeastern US states.
Methods
Tobacco retailer density was calculated for CVS and dollar store locations and combined to represent retailer density change before and after policy changes. Bivariate analyses were conducted to compare the corporate-initiated changes in county-level retailer density across rurality categories.
Results
Findings suggest a statistically significant difference (p < 0.0001) between TRD effect and rurality. Urban counties together experienced a retailer density increase of 0.4 stores per 10 k adult population, while rural counties reported a TRD increase of 2.6—eight (8) times the increase in urban areas.
Conclusions
Recent corporate policy changes on tobacco sales have increased access to tobacco retailers in rural counties considerably more than in urban counties, contributing to further disparities. CVS pharmacies discontinuing tobacco sales caused a decrease in retail density in urban areas, and the decision of the dollar stores locations initiating tobacco sales resulted in a greater burden to rural and small-metro counties.
1. Introduction
Smoking remains the leading cause of preventable death and disease in the U.S. (Health CO on S and. Smoking and Tobacco Use, 2018) Since the 1964 Surgeon General's Report on the dangers of smoking, rates have declined from 42% to 16% (Health CO on S and. Smoking and Tobacco Use, 2018; Holford et al., 2014), but decreases have been disproportionately concentrated in urban areas (Doogan et al., 2017). Rural Americans are more likely to use tobacco than their urban or suburban counterparts and are more likely to be exposed to tobacco smoke (Vander Weg et al., 2011). Policy-level tobacco control and regulatory factors have been more effective in urban areas, contributing to the increased tobacco-related disparities between urban and rural communities (Doogan et al., 2017; Vander Weg et al., 2011; Ziller et al., 2019). As a result of successful tobacco control policies that have reduced marketing and advertising of tobacco products, retail outlets are considered the last frontier for the tobacco industry to market its products (Robertson et al., 2015). Compared to their urban counterparts, rural populations have reported greater exposure to tobacco advertising in the retail outlets they visit, including convenience stores, gas stations, grocery stores, and big box stores (Bernat and Choi, 2018).
CVS, the largest U.S. pharmacy chain, made headlines in 2014 when it discontinued the sale of tobacco products in its ~8000 pharmacies, citing a commitment to health promotion and provision of community healthcare services, and demonstrating that private retailers can play a meaningful role in changing tobacco-use behaviors (Polinski et al., 2017). In less ceremonious fashion, Family Dollar and Dollar General, the two largest dollar store chains, began selling tobacco in 2012 and 2013, respectively, at their combined ~19,000 stores, declaring they were responding to consumer demand (Newsmax, 2014). Dollar stores draw their customer base from lower income individuals, and have opened new stores at record pace since the U.S. housing market crash, specifically targeting small towns in rural areas (Meyersohn, 2017).
Higher tobacco retailer density (TRD) is known to be associated with higher smoking rates, a higher number of cigarettes smoked per day, increased rates of new and experimental smoking (Chuang et al., 2005; McCarthy et al., 2009), and is associated with lower life expectancy and higher mortality (Galiatsatos et al., 2017). This increase in access to tobacco due to the corporate decisions of the dollar stores, which far outnumber CVS locations, has been found to be associated with the tobacco use patterns of pregnant mothers in the Southeast (Hall et al., 2019).
In the current study, we aim to determine how the aforementioned corporate policy changes of CVS and the dollar stores may be associated with increasing disparities for another vulnerable population—residents of rural areas. Specifically, we evaluated the differential change in county-level TRD (retailers per 10,000 adults) resulting from implementation of these three corporation's policy changes between urban, rural and small-metro areas in 12 Southeastern U.S. states. The U.S. Southeast is home to nearly 10,000 dollar store locations as of 2018, more than three times the number of CVS locations. Additionally, the Southeast has some of the highest rates of smoking and tobacco-related cancer mortality (Mokdad et al., 2017). It is the region with the most concentrated rural poverty (HAC, 2012), and where some of the highest rural-urban cancer disparities persist (Yao et al., 2017). Rural counties in the Southeast exhibit multiple disparities compared with urban counties, e.g., having higher unemployment and poverty, and lower income lower education rates.
2. Methods
The addresses of CVS and dollar store locations in 12 Southeastern states (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia and West Virginia) were obtained from the respective corporate websites (December 2017–January 2018). County-level population estimates of individuals ≥18 years were obtained for 2016 from the American Community Survey. TRD (stores per 10,000 adults) was calculated by county for CVS and dollar store locations. County-level TRD change (related to the decisions between 2012 and 2014 by Family Dollar, Dollar General and CVS) was calculated to test whether: (1) the initiation of tobacco sales by dollar stores was associated with density increase, and (2) the discontinuation of tobacco sales by CVS resulted in density decrease (i.e., the difference between the CVS retail density and the dollar store retail density). Counties were assigned to one of three rurality categories according to the rural-urban classification scheme of the National Center for Health Statistics (Ingram and Franco, 2014) as follows: urban (population ≥1million), small-metro (population <1 million–≥50,000), and rural counties which are not in a metropolitan statistical area (population <50,000) (Ingram and Franco, 2014). Descriptive and bivariate statistics, analysis of variance (ANOVA, aov in R v.3.4.2) with Tukey post-hoc, were conducted to compare the corporate-initiated changes in county-level TRD across rurality categories which occurred between 2012 and 2014 (Fig. 1) and to identify counties with the largest TRD changes.
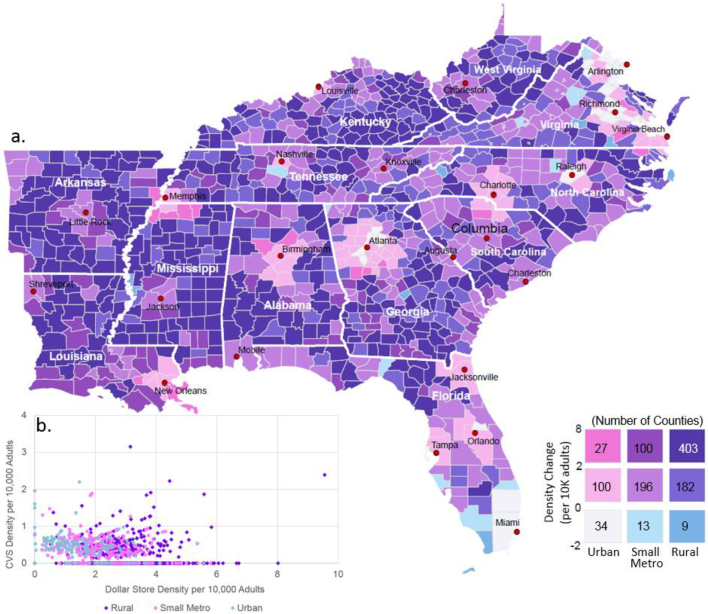
Fig. 1.
(a) Bivariate Choropleth map: Corporate-initiated changes in tobacco retail density occurring between 2012 and 2014 in urban, small-metro, and rural counties of the Southeastern United States. Urban-Rural Classification Scheme for counties from the National Center for Health Statistics, six levels categorized as follows: 1–2 as urban, 3–4 as small-metro, and 4–6 as rural. Purple indicates higher level of burden in both density change and rurality. b) County level change in retailer density caused by corporate tobacco sales decisions. Seven urban counties had no Family Dollar or Dollar General stores whereas 361 rural counties had no CVS stores.
3. Results
In the Southeastern U.S., overall TRD increased by 1.17 stores/10,000 on average from 2012 and 2014, following the dollar store corporate decisions to initiate tobacco sales, despite the CVS decision to discontinue sales. The CVS decision alone would have caused a decrease of 0.45 stores/10,000. The level of increase in TRD was not experienced equally across all counties (Fig. 1a). Urban and small-metro counties saw a retailer density increase of 0.4 and 1.3 stores/10,000, respectively, whereas rural counties experienced a TRD increase of 2.6 stores/10,000–six times the increase in urban areas. Only 31 of the region's 1063 counties experienced a decrease in TRD following the aforementioned corporate policy changes, resulting from a greater number of CVS than dollar store locations in those counties; 25 counties experienced no change (due to an equal number of CVS and dollar store locations or no stores in those counties), and 1007 counties experienced an increase in TRD. Most counties experiencing a decrease in TRD were urban (68%) or suburban (26%) (i.e. small-metro counties adjacent to urban) compared to rural (6%) (Fig. 1). Across the U.S. Southeast, 77% of the rural residents resided in a county which experienced a TRD increase >2.0 (the median), while only 2% of urban residents experienced this increase.
The one-way ANOVA revealed a large and statistically significant difference in TRD change by rural-urban category (Table 1). The decision by CVS to discontinue tobacco sales resulted in a greater benefit to urban and small-metro counties as compared with rural counties. Conversely, the result of dollar stores initiating tobacco sales was associated with a greater TRD burden to rural and small-metro counties. Of the residents in the counties experiencing a decrease in TRD, 89% were urban, and only 0.9% were rural. In addition, 99% of rural residents live in counties that experienced an increase in TRD. The distribution of CVS and dollar stores is dissimilar: CVS has 48% of its locations in urban counties, while dollar stores have only 21% of their stores in urban areas.
Table 1.
Analysis of variance of retailer density change from pre- to post policy change period among rurality categories. Rurality classifications of Southeast US counties and corporate policy initiated change in tobacco retailer density (from 2012 to 2014).
| Variable | Source | df | SS | MS | F-value | P-value |
|---|---|---|---|---|---|---|
| Density change | Between groups | 2 | 431.9 | 215.94 | 166.8 | <0.001 |
| Within groups | 1060 | 1372.1 | 1.29 | |||
| Post-hoc comparisons of means | Difference | P-value | ||||
| Rural – Urban | 1.669 | 0.000 | ||||
| Rural – Small Metro | 0.957 | 0.000 | ||||
| Small Metro – Urban | 0.712 | 0.000 | ||||
| Dollar-stores density | Between groups | 2 | 329.4 | 164.71 | 154.1 | <0.001 |
| Within groups | 1060 | 1133.1 | 1.07 | |||
| Post-hoc comparisons of means | Difference | P-value | ||||
| Rural – Urban | 1.480 | 0.000 | ||||
| Rural – Small Metro | 0.804 | 0.000 | ||||
| Small Metro – Urban | 0.676 | 0.000 | ||||
| CVS density | Between groups | 2 | 7.4 | 3.67 | 30.1 | <0.001 |
| Within groups | 1060 | 129.5 | 0.12 | |||
| Post-hoc comparisons of means | Difference | P-value | ||||
| Rural – Urban | −0.189 | 0.000 | ||||
| Rural – Small Metro | −0.154 | 0.000 | ||||
| Small Metro – Urban | −0.036 | 0.547 | ||||
df: degrees of freedom, SS: sum of squares, MS: mean squares.
4. Discussion and conclusions
To our knowledge, our report is the first to describe the differential changes in TRD due to corporate decisions by major retailers to either discontinue or start selling tobacco products. The CVS decision to discontinue tobacco sales reduced TRD in the Southeast by 0.4 stores per 10,000 adults. The decisions by the dollar stores to sell tobacco have increased density of tobacco retailers by 1.5 stores per 10,000, and most concerning, the increase was disproportionate in rural communities. Findings suggest that half of the counties with the greatest decrease in TRD were wealthy urban counties in northwest Virginia near Washington D.C. (e.g., Fairfax and Stafford Counties, VA) while other counties with decreases were large urban centers and suburbs (e.g., Miami-Dade County, FL; Fulton and Forsyth Counties, GA). There was a small number of wealthy but rural vacation destinations experiencing a decrease in TRD (e.g., Dare County, NC which includes the Outer Banks and Monroe County, FL, home of the Florida Keys). However, the ten communities with the largest increases were all rural counties with increases >6 stores per 10,000 adults.
Other retail outlets may have opened or closed in this time period, however no other similarly sized national company made a corporate level policy change related to tobacco during this period. County-level analyses can mask the potential TRD changes to individual neighborhoods and population sub-groups. Future studies should use greater geographic precision to examine neighborhood level tobacco-related outcomes related to the changes in access to tobacco products, including initiation age of tobacco, access to adolescents, and changes in smoking frequency.
Rural Americans are at a greater risk for tobacco-related illness than urban Americans (Doogan et al., 2017). Greater tobacco retail density is associated with greater health disparities, disproportionately burdening rural counties. The current study did not examine whether change in TRD was related to an actual increased use of tobacco products on a per-capita basis. There is concern that the dollar stores' decisions to start selling tobacco products may be exacerbating urban-rural disparity, although dollar stores alone are not the cause for urban-rural tobacco use disparities. Smoking regulations, such as smoke-free workspaces, mostly benefit urban communities, where tobacco use has declined disproportionately. Rural Americans are less likely to receive adequate protection from second-hand smoke, and smoking cessation interventions have been less effective in rural areas (Griffin et al., 2015). State governments have an opportunity to invest billions of dollars from tobacco taxes and legal settlements in tobacco control and prevention initiatives. To date, no state in the US has funded its tobacco prevention program to the level recommended by the U.S. Centers for Disease Control (State Tobacco Settlement, 2017).
Addressing the disparities in tobacco retailers density will require fully funding comprehensive tobacco control and prevention strategies (Ziller et al., 2019). Comprehensive evidence-based tobacco control strategies have shown to increase the effectiveness of counter-marketing campaigns in rural areas (Hahn et al., 2015). Combining telehealth smoking cessation programs with high-impact media campaigns has the potential to increase the reach and effectiveness of smoking cessation interventions in rural communities (Carlson et al., 2012). Policy strategies, such as increasing the price of cigarettes, can protect public health and benefit vulnerable communities (Henriksen et al., 2017) because increasing the price of cigarette packs reduces smoking (Chaloupka et al., 2012; World Health Organization, 2015). However, all 12 Southeastern states in this study have state tobacco excise taxes below the national average. In addition, state and local governments have the authority to utilize carefully crafted licensing laws to reduce density of tobacco retailers in vulnerable communities (Ackerman et al., 2017).
Funding
There are no funding sources to report.
Declaration of Competing Interest
None declared.
References
- Ackerman A., Etow A., Bartel S., Ribisl K.M. Reducing the density and number of tobacco retailers: policy solutions and legal issues. Nicotine Tob. Res. 2017;19(2):133–140. doi: 10.1093/ntr/ntw124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernat D.H., Choi K. Differences in cigarette use and the tobacco environment among youth living in metropolitan and nonmetropolitan areas. J. Rural. Health. 2018;34(1):80–87. doi: 10.1111/jrh.12194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson L.E., Lounsberry J.J., Maciejewski O., Wright K., Collacutt V., Taenzer P. Telehealth-delivered group smoking cessation for rural and urban participants: feasibility and cessation rates. Addict. Behav. 2012;37(1):108–114. doi: 10.1016/j.addbeh.2011.09.011. [DOI] [PubMed] [Google Scholar]
- Chaloupka F.J., Yurekli A., Fong G.T. Tobacco taxes as a tobacco control strategy. Tob. Control. 2012;21(2):172–180. doi: 10.1136/tobaccocontrol-2011-050417. [DOI] [PubMed] [Google Scholar]
- Chuang Y.-C., Cubbin C., Ahn D., Winkleby M.A. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. J. Epidemiol. Community Health. 2005;59(7):568–573. doi: 10.1136/jech.2004.029041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dollar-Store Chains Find Smokers Are Some of Their Best Shoppers. Newsmax. https://www.newsmax.com/finance/dollar-store-retail-tobacco-cigarette/2014/11/05/id/605459/. Published November 5, 2014. Accessed March 9, 2018.
- Doogan N.J., Roberts M.E., Wewers M.E. A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Prev. Med. 2017;104:79–85. doi: 10.1016/j.ypmed.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galiatsatos P, Kineza C, Hwang S, et al. Neighbourhood characteristics and health outcomes: evaluating the association between socioeconomic status, tobacco store density and health outcomes in Baltimore City. Tob Control. November 2017:tobaccocontrol-2017-053945. doi:10.1136/tobaccocontrol-2017-053945. [DOI] [PMC free article] [PubMed]
- Griffin E., Moon G., Barnet R. Examining the significance of urban–rural context in tobacco quitline use: does rurality matter? Int J Public Health. 2015;60(3):327–333. doi: 10.1007/s00038-014-0634-y. [DOI] [PubMed] [Google Scholar]
- HAC. Rural Research Brief: Poverty in Rural America. 2012. http://www.ruralhome.org/storage/research_notes/rrn_poverty.pdf.
- Hahn E.J., Rayens M.K., Adkins S., Begley K., York N. A controlled community-based trial to promote smoke-free policy in Rural communities. J. Rural. Health. 2015;31(1):76–88. doi: 10.1111/jrh.12087. [DOI] [PubMed] [Google Scholar]
- Hall J, Cho HD, Maldonado-Molina M, George T, Shenkman E, Salloum R. Association of Rates of Smoking During Pregnancy with Corporate Tobacco Sales Policies. JAMA Pediatr. 2019;in press. [DOI] [PMC free article] [PubMed]
- Health CO on S and. Smoking and Tobacco Use; 50th Anniversary Surgeon General's Report. Smoking and Tobacco Use. http://www.cdc.gov/tobacco/data_statistics/sgr/2012/. Published March 6, 2018. Accessed March 12, 2018.
- Henriksen L., Andersen-Rodgers E., Zhang X. Neighborhood variation in the Price of cheap tobacco products in California: Results from healthy Stores for a Healthy Community. Nicotine Tob. Res. 2017;19(11):1330–1337. doi: 10.1093/ntr/ntx089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holford T.R., Meza R., Warner K.E. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964-2012. JAMA. 2014;311(2):164–171. doi: 10.1001/jama.2013.285112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram D.D., Franco S.J. 2013 NCHS urban-Rural classification scheme for counties. Vital Health Stat. 2014;2(166):1–73. [PubMed] [Google Scholar]
- McCarthy W.J., Mistry R., Lu Y., Patel M., Zheng H., Dietsch B. Density of tobacco retailers near schools: effects on tobacco use among students. Am. J. Public Health. 2009;99(11):2006–2013. doi: 10.2105/AJPH.2008.145128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyersohn N. Dollar General is opening 900 new stores next year. CNNMoney. http://money.cnn.com/2017/12/07/news/companies/dollar-general-store-openings/index.html. Published December 7, 2017. Accessed March 13, 2018.
- Mokdad A.H., Dwyer-Lindgren L., Fitzmaurice C. Trends and patterns of disparities in cancer mortality among US counties, 1980-2014. JAMA. 2017;317(4):388–406. doi: 10.1001/jama.2016.20324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polinski J.M., Howell B., Gagnon M.A., Kymes S.M., Brennan T.A., Shrank W.H. Impact of CVS Pharmacy's discontinuance of tobacco sales on cigarette purchasing (2012–2014) Am. J. Public Health. 2017;107(4):556–562. doi: 10.2105/AJPH.2016.303612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson L., McGee R., Marsh L., Hoek J.A. Systematic review on the impact of point-of-Sale tobacco promotion on smoking. Nicotine Tob. Res. 2015;17(1):2–17. doi: 10.1093/ntr/ntu168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State Tobacco Settlement. Campaign for Tobacco-Free Kids. https://www.tobaccofreekids.org/what-we-do/us/statereport. Published June 7, 2017. Accessed March 9, 2018.
- Vander Weg M.W., Cunningham C.L., Howren M.B., Cai X. Tobacco use and exposure in rural areas: findings from the behavioral risk factor surveillance system. Addict. Behav. 2011;36(3):231–236. doi: 10.1016/j.addbeh.2010.11.005. [DOI] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2015. WHO Report on the Global Tobacco Epidemic 2015: Raising Taxes on Tobacco. [Google Scholar]
- Yao N., Alcalá H.E., Anderson R., Balkrishnan R. Cancer disparities in Rural Appalachia: incidence, early detection, and survivorship. J. Rural. Health. 2017;33(4):375–381. doi: 10.1111/jrh.12213. [DOI] [PubMed] [Google Scholar]
- Ziller E.C., Lenardson J.D., Paluso N.C., Talbot J.A., Daley A. Rural–urban differences in the decline of adolescent cigarette smoking. Am. J. Public Health. 2019;109(5):771–773. doi: 10.2105/AJPH.2019.304995. [DOI] [PMC free article] [PubMed] [Google Scholar]