Abstract
Overall, asthma mortality rates have declined dramatically in the last 30 years, due to improved diagnosis and to better treatment, particularly in the 1990s following the more widespread use of inhaled corticosteroids (ICSs). The impact of ICS on other long-term outcomes, such as lung function decline, is less certain, in part because the factors associated with these outcomes are incompletely understood. The purpose of this review is to evaluate the effect of pharmacological interventions, particularly ICS, on asthma progression and mortality. Furthermore, we review the potential mechanisms of action of pharmacotherapy on asthma progression and mortality, the effects of ICS on long-term changes in lung function, and the role of ICS in various asthma phenotypes.
Overall, there is compelling evidence of the value of ICS in improving asthma control, as measured by improved symptoms, pulmonary function and reduced exacerbations. There is, however, less convincing evidence that ICS prevents the decline in pulmonary function that occurs in some, although not all, patients with asthma. Severe exacerbations are associated with a more rapid decline in pulmonary function, and by reducing the risk of severe exacerbations, it is likely that ICS will, at least partially, prevent this decline. Studies using administrative databases also support an important role for ICS in reducing asthma mortality, but the fact that asthma mortality is, fortunately, an uncommon event makes it highly improbable that this will be demonstrated in prospective trials.
Short abstract
There is compelling evidence of the value of ICS in improving asthma control and indirect evidence that ICS prevents lung function decline by preventing severe exacerbations. Registry-based studies support the role of ICS in reducing asthma mortality. http://bit.ly/2VcNjaz
Introduction
Asthma deaths have been described from antiquity [1]. Henry Hyde Salter (himself suffering from asthma) wrote, in 1860, that the natural history of asthma is that while very young patients tend to recover and are at low risk of death, in those older than 45 years there is a progressive worsening of the disease, increasing the risk of death [2].
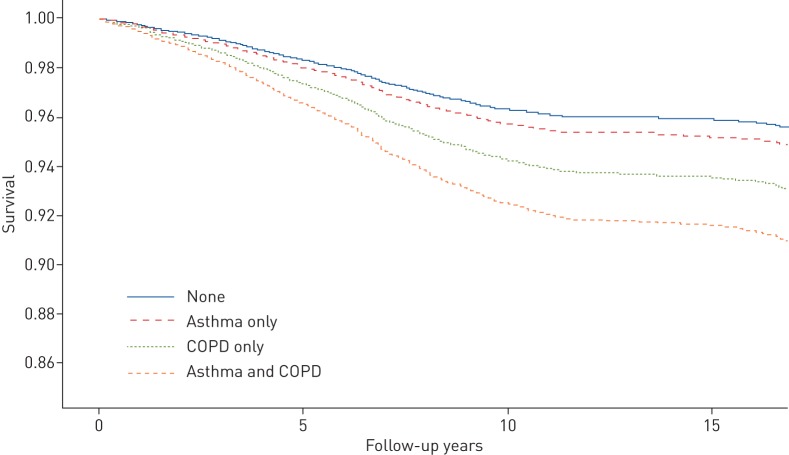
Smoking [3] and chronic obstructive pulmonary disease (COPD) [4] are known to be associated with increased mortality, mainly due to nonrespiratory causes. While there is no doubt that asthma deaths occur and epidemics of asthma mortality have been reported in some countries from the 1950s through to the 1980s, likely caused by overuse of inhaled β2-agonists [5], an unanswered question is whether patients whose asthma develops early in life have increased mortality risk due to asthma itself or other diseases. Reasons for this uncertainty include the heterogeneity of asthma, its frequent association with other diseases and the poor accuracy of certified causes of death [6]. Some long-term studies, conducted in patients followed from asthma diagnosis, concluded that asthma itself, without concomitant risk factors such as smoking or reduced lung function, is not associated with reduced survival compared with age-matched controls [7–14]. In contrast, patients with late-onset asthma and elderly patients with asthma [15] appear to have increased mortality risk, particularly when associated with other diseases, mainly COPD (figure 1) or reduced lung function [8–11, 13].
FIGURE 1.
Results from Cox proportion hazard models. Curves are adjusted for sex, age, body mass index, education, race/ethnicity and smoking status at baseline. COPD: chronic obstructive pulmonary disease. Reproduced from [8] with permission.
Overall, asthma mortality has declined in the last 30 years [16], due in part to improved diagnosis and more accurate certification of death, but also due to better treatment, particularly with the introduction of inhaled corticosteroids (ICSs) [6]. However, no randomised controlled trial (RCT) has demonstrated improved survival as either a primary or secondary outcome in patients with asthma treated with ICS; the only evidence has come from registry-based studies [17, 18]. The purpose of this review is to evaluate the strength of the evidence of the effect of pharmacological interventions, particularly ICS, on asthma progression and mortality.
Natural history of asthma
Describing the natural history of asthma poses the same challenges as defining asthma. This is due to the heterogeneity of the airway diseases unified under the “asthma” label [19]. Thus, the natural history may follow different paths of disease progression, including lung function decline, remission, reoccurrence, morbidity and mortality.
Information on asthma's natural history mainly comes from three types of studies: 1) studies of patients with predominantly severe or difficult-to-treat asthma, conducted in specialised hospital clinics; 2) cohorts of individuals with asthma, both children and adults, enrolled in prospective population studies alongside healthy individuals; and 3) registry-based studies using data retrieved from hospital, prescription and mortality records. Data from interventional studies can also contribute to knowledge of natural history, although such studies are usually too short to be extrapolated to a lifetime perspective. While studies from specialised departments often include well-characterised patients, they select a subgroup of individuals with the most severe asthma, representing <10% of the asthma population, who may have a much worse prognosis than the majority of individuals, with milder asthma, who use intermittent treatment and who have infrequent exacerbations [20]. General population cohort studies (and in particular registry-based studies) can be criticised for an uncertain diagnosis and poor characterisation of the participants, as they do not always include clinically important variables such as lung function, daily symptoms and biomarkers, e.g. eosinophils or exhaled nitric oxide fraction (FENO). However, in recent years, a number of well-designed childhood asthma cohorts have cast new light on the progression of asthma from childhood to adolescence and even adulthood, with some of these cohorts including individuals who have reached their 50s [21].
Natural history of lung function in childhood asthma
Childhood studies suggest that at the time of diagnosis, as a group, children with asthma already have reduced forced expiratory volume in 1 s (FEV1) and FEV1/forced vital capacity (FVC) ratio. Longitudinal observations have identified several trajectories that differ from normal, in terms of maximal FEV1, the duration of the FEV1 plateau during early adulthood and the age at onset of FEV1 decline. In one study, only 25% of children had a normal pattern of lung function development, whereas 26% had reduced growth and an early decline, 23% had reduced growth only, and 26% had normal growth and an early decline [22].
In another cohort, children with the most severe symptoms had reduced lung function both at the age of 10 years and when they reached their 50s. However, lung function decline (FEV1 and FEV1/FVC ratio) between 20 and 50 years of age was no faster than in the control group without asthma, and was not related to initial asthma severity [23]. A similar pattern was observed in still another cohort, where children were followed from the age of 10–15 to 60–65 years [24]. Thus, it seems that childhood asthma mostly exerts its deleterious impact on lung function during the growth phase [25]. Factors that predict suboptimal development resulting in poorer lung function in adulthood include low baseline FEV1, severe and persistent symptoms, early sensitisation, lower bronchodilator response, airway hyperresponsiveness (AHR), and male sex.
The effect of active smoking on lung function in individuals with childhood asthma and early-onset asthma has been a subject of debate [26–28]. Some studies suggest that the role of smoking with regard to driving lung function impairment is small in this group [29]. Other studies suggest that smoking only plays an important role in those with nonatopic asthma [30], whereas still other studies suggest a synergistic effect of atopy and smoking resulting in chronic airflow limitation [31].
Natural history of lung function in adult-onset asthma
Most studies in adults show that, as a group, individuals with asthma have a lower FEV1 and FEV1/FVC ratio than healthy individuals. Predictors of reduced lung function include adult-onset, long-standing disease, severe symptoms, frequent exacerbations, smoking, ongoing exposure to allergens and occupational agents, chronic mucus hypersecretion, and high levels of AHR, IgE and eosinophils [26]. Some of these predictors have been reproduced in longitudinal studies, where the outcome has been lung function decline. The initial focus of these analyses was whether lung function declines faster in those with asthma than in healthy individuals, including the role of smoking [32, 33]. More recent longitudinal studies identified potentially modifiable characteristics related to faster FEV1 decline, including high frequency and severity of exacerbations [34, 35], and elevated FENO and eosinophils [36–38].
Earlier studies did not differentiate between childhood-onset versus adult-onset asthma [39]. This is relevant, as adult-onset asthma, in addition to a poorer response to therapy, seems to be associated with a higher risk of disease progression, including faster FEV1 decline [40–42]. Furthermore, the presence of airflow limitation at baseline in individuals with asthma, a condition sometimes labelled asthma–COPD overlap (ACO), is also associated with faster FEV1 decline, in particular in those with onset of asthma after the age of 40 years [13]. In contrast, both early-onset asthma without airflow limitation at baseline and ACO with early-onset asthma are associated with subsequent normal FEV1 decline [13].
Mortality in asthma
Most deaths from asthma are preventable. While asthma mortality has reduced substantially over the last few decades in most countries, asthma deaths still occur and are strongly related to social deprivation, even in developed countries [43, 44]. This suggests poor access to healthcare/medications and low adherence to ICS are important modifiable factors. In addition, studies from both before and after the introduction of ICS suggest that the overuse of potent inhaled β2-agonists increases asthma mortality [5].
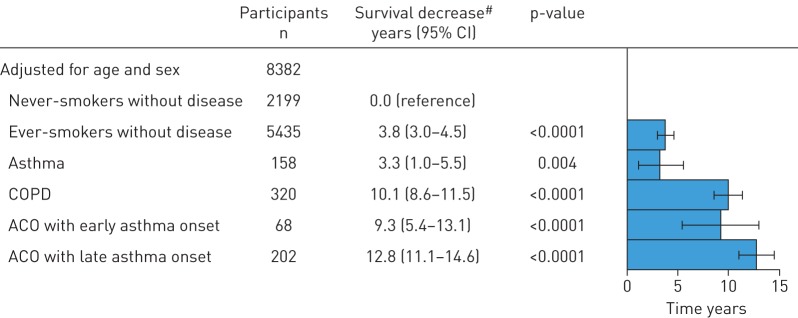
Patient characteristics related to increased risk of death in asthma include similar factors to those related to rapid lung function decline. Thus, severe and difficult-to-treat asthma, late-onset asthma, current smoking, presence of chronic airflow limitation, eosinophilia, bronchial hypersecretion, AHR, aspirin sensitivity, previous intensive care unit admissions, and the presence of heart disease have been related to poorer survival [7, 45–48]. Recently it has become clear that individuals with characteristics of both asthma and COPD (ACO) have reduced survival. In the Copenhagen City Heart Study, life expectancy compared with healthy never-smokers was reduced by ∼9 years in those with ACO and early-onset asthma, and by ∼13 years in those with ACO and late-onset asthma, whereas it was only reduced by 3 years in individuals with asthma, preserved lung function and low tobacco exposure (figure 2) [13]. In a Danish cohort, females with ACO showed higher mortality compared with those with asthma or COPD alone [49].
FIGURE 2.
Survival decrease in six subgroups of the Copenhagen City Heart Study, defined by smoking and presence of airway disease. COPD: chronic obstructive pulmonary disease; ACO: asthma–COPD overlap. #: bias-corrected bootstrap estimates based on Makuch–Ghali curves. Reproduced and modified from [13] with permission.
Earlier epidemiological studies, based on longitudinally followed cohorts or on health registries, have consistently shown that individuals with asthma from the general community, as a group, have a higher risk of death than healthy individuals (hazard ratio 1.5) [46, 50]. The increased risk is caused by higher mortality from respiratory diseases, including COPD and pneumonia. It has also been debated whether asthma, like COPD, also predisposes individuals to a higher risk of developing ischaemic heart disease and lung cancer. However, a study focusing on the long-term prognosis of smokers and never-smokers with asthma suggests that these associations may have been caused by inadequate adjustment for smoking, social status and, in the case of heart disease, cardiovascular risk factors [14, 51].
Changing concepts in asthma diagnosis, severity assessment and treatment, and their effects on asthma progression and mortality
The first guidelines on asthma diagnosis and management were published in the late 1980s [52–55]. The development of these documents was stimulated by an increase in asthma-related mortality in several countries (particularly New Zealand [5]), and a marked increase in asthma prevalence in many countries in the 1970s and 1980s [56]. These were consensus statements, rather than formal evidence-based clinical practice guidelines, but all identified the need to establish the diagnosis of asthma using objective criteria to document variable lung function, which has not changed over time, and recommended treatment options based on the perceived severity of the disease. The objectives of treatment were to improve symptom control and lung function. The importance of airway inflammation in asthma pathogenesis had already been identified [57], but the early documents did not emphasise the benefits of anti-inflammatory treatments, and as a result medications that rapidly improved symptoms and lung function, particularly inhaled β2-agonists, were the focus of treatment, especially for patients with mild-to-moderate asthma.
The effects of an over-reliance on inhaled β2-agonists were profound [58]. The most commonly used are inhaled short-acting β2-agonists (SABAs), which with regular use as the only treatment for asthma are now known to promote eosinophilic airway inflammation [59], cause a deterioration of asthma control [60] and in some instances increase the risk of asthma mortality [61]. The increase in asthma mortality risk is also seen when inhaled long-acting β2-agonists (LABAs) are used as the only treatment [62].
A paradigm change in asthma management has occurred, in that management now focuses on overall asthma control, consisting of two domains: 1) achieving current asthma control and 2) minimising future risk, particularly of severe exacerbations, but also of loss of lung function, and side-effects of medications. Asthma severity is now defined by the level of treatment needed to control the disease [63], rather than, as previously, a complex algorithm of symptoms, lung function and reliever use, which did not take treatment requirements into consideration. In addition, there is an improved understanding of the role of airway inflammation in causing the manifestations of asthma, including symptoms, variable airflow obstruction and severe exacerbations. Indeed, severe exacerbations have not only been recognised as a vitally important target for treatment, but are also associated with progression of asthma and a more rapid decline in lung function [35].
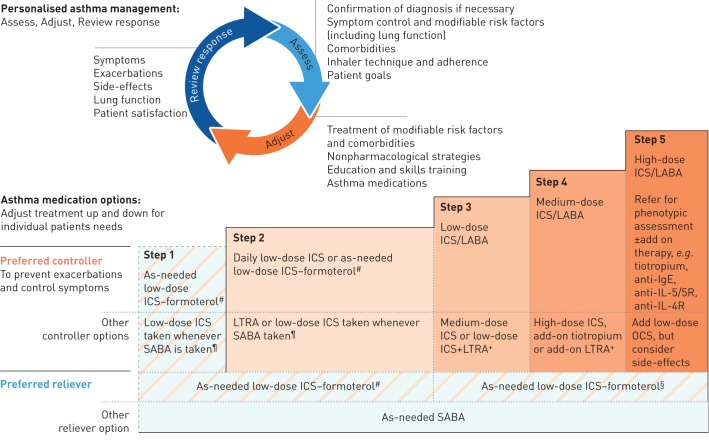
These changes resulted in an enhanced appreciation of the pivotal role for ICS in asthma management. ICS treatment is known to improve all manifestations of asthma and to reduce asthma mortality [17], and over the past decade maintenance ICS treatment has been recommended for all patients with symptoms requiring reliever use two or more times per week. More recently, because of an increased understanding that patients considered to have mild asthma have greater morbidity than previously appreciated [64], ICSs are now recommended as a treatment option for all patients [6]. Also, the use of ICS/rapid-onset β2-agonist as a reliever medication for all patients with asthma, in preference to SABA alone, has been another very recent addition to treatment recommendations (figure 3) [65].
FIGURE 3.
The Global Initiative for Asthma stepwise asthma treatment strategy for adults and adolescents ≥12 years of age. ICS: inhaled corticosteroid; SABA: short-acting β2-agonist; LTRA: leukotriene receptor agonist; LABA: long-acting β2-agonist; IL: interleukin; R: receptor; OCS: oral corticosteroid. #: off-label (data only with budesonide–formoterol); ¶: off-label (separate or combination ICS and SABA inhalers); +: consider adding house dust mite sublingual immunotherapy for sensitised patients with allergic rhinitis and forced expiratory volume in 1 s >70% predicted; §: low-dose ICS–formoterol is the reliever for patients prescribed budesonide–formoterol or beclometasone dipropionate–formoterol maintenance and reliever therapy. Reproduced from [65] with permission.
A result of this focus on ICS use, either as monotherapy for mild asthma or together with LABA in a single inhaler for patients with moderate-to-severe disease, is that the risks of severe asthma exacerbations and associated emergency department visits or hospitalisation have declined, both in clinical trials where these treatment options have been studied [66–68] and in real-world settings. A study from Ontario, Canada, reported an almost 50% reduction in emergency department visits for asthma between 2003 and 2013 [69], with overall asthma mortality decreasing in countries where this has been measured [43, 70].
Effect of current medications on severe asthma progression and mortality
Most patients can achieve satisfactory control of their asthma from an ICS with or without a LABA. However, 5–10% have severe disease, requiring extensive treatment to achieve control or remaining uncontrolled despite such treatment [71, 72]. This subgroup accounts for the majority of morbidity and mortality due to asthma, and for 60% of the total healthcare costs attributable to asthma. Furthermore, patients with a recent history of an asthma exacerbation have particularly high annual healthcare costs, estimated to be three times those of patients with severe asthma and no history of an exacerbation [73].
Severe asthma is heterogeneous with respect to the clinical problem, nature of lung function impairment and underlying pathology [74]. It is often complex, as many patients have a clinically severe condition primarily because the diagnosis is incorrect, or due to issues with inhaler technique or treatment adherence. Other patients have persistent asthma-like symptoms primarily driven by comorbid factors. The international European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines on severe asthma acknowledge these difficulties and have produced the most widely accepted definition [71]. This is “asthma which requires treatment [with guideline-suggested medications for Global Initiative for Asthma stages 4–5 asthma (high-dose ICS and LABA or leukotriene modifier/theophylline) for the previous year or systemic corticosteroid for ≥50% of the previous year] to prevent it from becoming ‘uncontrolled’ or which remains ‘uncontrolled’ despite this therapy”. The diagnosis of asthma should be confirmed and comorbidities addressed before making a diagnosis of severe asthma.
An important aspect of the ERS/ATS definition is that different criteria for uncontrolled asthma are identified and no assumptions are made about the involvement of pathophysiological pathways. This is important as it is increasingly clear that different mechanisms drive different aspects of the clinical problem [74]. For example, symptoms likely reflect airway dysfunction, comorbidities and psychological factors more closely than underlying type 2 high airway inflammation, whereas severe exacerbations more closely reflect bronchodilator unresponsive airflow limitation due to eosinophilic, type 2 high airway inflammation. The mechanisms driving progressive loss of lung function are less clear, but neutrophilic and type 2 high airway inflammation may be contributory [36, 75]. Therapeutic interventions also impact clinical problems differently, with LABAs having a proportionately bigger impact on symptoms and lung function than exacerbations (particularly more severe events), whereas the opposite is true for ICS or a step-up in ICS dose [76].
The high level of morbidity, healthcare costs and treatment-related side-effects in severe asthma mean that there is large unmet need for alternative therapies. Treatment should target the pathophysiological mechanism responsible for the clinical problem and should be adapted for each individual patient. One particularly fruitful area of development has been the use of monoclonal antibodies targeting type 2 cytokines involved in the development of type 2 high airway inflammation [72]. These treatments have a large impact on exacerbation frequency but a less impressive effect on symptoms and lung function. The first of these, anti-IgE (omalizumab), is now known to be particularly effective in patients with evidence of type 2 airway inflammation [77]. A number of newer approaches, including anti-interleukin (IL)-5 (mepolizumab, reslizumab), anti-IL-5 receptor (benralizumab) and anti-IL-4 receptor α (dupilumab which blocks IL-4 and IL-13), have been approved by regulatory authorities for treatment of severe eosinophilic asthma.
A recent large epidemiological study has shown that most patients with severe asthma transition to less severe disease over time [78]. Low socioeconomic class, comorbidity and high medication use were all identified as predictors of remaining severe. Clinical trials of biological agents in severe asthma have shown that symptoms improve markedly with placebo treatment within the first month or so, but little thereafter (table 1) [79–86]. The effect of biological treatment on top of this is modest, implying that factors not related to inflammation, such as comorbidities, are driving many residual symptoms. The findings of high correlation between the presence of obesity and a high Hospital Anxiety and Depression Scale score and reported symptoms in severe asthma are also consistent with this [87].
TABLE 1.
Summary of the effect of treatment on pre-bronchodilator forced expiratory volume in 1 s (FEV1), asthma exacerbations and mortality
| Study [ref.] | Subjects n | Duration weeks | Asthma severity# | Treatment group | Change from baseline in pre-bronchodilator FEV1 mL | Exacerbations¶ | Mortality %+ | |
| Overall | ED and hospitalisation | |||||||
| Busseet al. [79] | 36 010 | 26 | Moderate | ICS | Not reported | 11.7% | 0.60% | 0 |
| ICS/LABA | Not reported | 9.8% | 0.66% | 0 | ||||
| DREAM [80] | 616 | 52 | Severe | Placebo | 60 | 2.40 | 0.43 | 0 |
| Mepolizumab | 115–140 | 1.15–1.46 | 0.17–0.25 | 1 | ||||
| MENSA [81] | 576 | 32 | Severe | Placebo | 86 | 1.74 | 0.20 | 1 |
| Mepolizumab | 183–186 | 0.83–0.93 | 0.08–0.14 | 0 | ||||
| MUSCA [82] | 551 | 24 | Severe | Placebo | 56 | 1.21 | 0.10 | 0 |
| Mepolizumab | 176 | 0.51 | 0.03 | 0 | ||||
| CALIMA [83] | 1306 | 56 | Severe | Placebo | 215§ | 0.93§ | 0.04§ | 0 |
| Benralizumab | 330–340§ | 0.60–0.66§ | 0.04–0.05§ | 0 | ||||
| SCIROCCO [84] | 1205 | 48 | Severe | Placebo | 239§ | 1.33§ | 0.18§ | 0 |
| Benralizumab | 345–398§ | 0.65–0.73§ | 0.06–0.11§ | 0 | ||||
| Castroet al. [85] | 953 | 52 | Severe | Placebo | 120 | 1.81 | 0.12 | 0 |
| Reslizumab | 220 | 0.84 | 0.077 | 0 | ||||
| QUEST [86] | 1902 | 52 | Moderate-to-severe | Placebo | 180–210ƒ | 0.87–0.97 | 0.065 | 0 |
| Dupilumab | 320–340ƒ | 0.46–0.52 | 0.035 | 0 | ||||
Ranges indicate results with different doses/routes of administration. ED: emergency department; ICS: inhaled corticosteroid; LABA: long-acting β2-agonist. #: asthma severity based on treatment requirements and prior asthma exacerbation rates; ¶: events are expressed as episodes per patient per year, unless otherwise specified; +: rounded to 0 decimal places; §: data are for the subgroup with severe asthma and eosinophils ≥300 cells·µL−1 (n=728 in CALIMA and n=809 in SCIROCCO); ƒ: change from baseline at week 12 (all other FEV1 data presented as change from baseline at the final study visit).
Less is known about changes in lung function over time, and analyses are complicated by the inherent variability of lung function in asthma, large placebo effects in many studies and limited follow-up duration. As a result, definitive conclusions about the rate of decline in lung function in severe asthma and the impact of treatment are not possible. Nevertheless, the very large populations studied and the use of novel methods to assess airway structure allow some tentative conclusions. Haldar et al. [88] reported a reduction in bronchial wall thickening assessed by computed tomography after 1 year of treatment with mepolizumab, suggesting some effect on airway remodelling. In keeping with this, Castro et al. [86] found a statistically significant difference in the rate of decline in post-bronchodilator FEV1 in patients with moderate-to-severe asthma after 1 year of treatment with dupilumab.
Exacerbations requiring oral corticosteroid (OCS) treatment, or resulting in emergency department visits and/or hospitalisation, occur more frequently in severe asthma and are generally much more responsive to treatment with biological agents than other outcome measures (table 1). Risk factors for these events include poor treatment adherence, low lung function and, in particular, a prior history of exacerbations [72]. In addition, clinical trials have shown a consistent relationship between an increased risk of exacerbations and a raised blood eosinophil count or FENO [89]. These biomarkers are also predictive of efficacy of biological treatment, with blood eosinophils relating most closely to the response to anti-IL-5 [90] and FENO to the response to anti-IL-4/13 [86] and omalizumab [77].
The morbidity associated with regular [91] or frequent rescue OCS use, such as weight gain, diabetes mellitus, hypertension, osteoporosis and cataract formation [92], is considerable and impacts most on patients with severe asthma. Biological agents have marked OCS sparing effects [93–95], so it is likely that this is another aspect of the longer-term natural history of severe asthma that will be improved in future.
Effects of current medications on mortality
As discussed earlier, the decreases in asthma mortality in the last 30 years are a result of improvements in socioeconomic conditions and of pharmacological treatment [6, 96]. The latter can be briefly summarised as the identification of the overuse of rescue SABA and no controller medications (ICS) as a risk factor for asthma death [61], the increasing use of ICS [17], the superiority of ICS/bronchodilator combinations in controlling moderate and severe asthma [76, 97], the introduction of combined ICS and fast-acting β2-agonists (i.e. formoterol) as both reliever and controller medication [68, 98], the additional effect of tiotropium [99], and the introduction of monoclonal antibodies in severe asthma [100].
The optimisation of care that takes place when patients are enrolled in controlled clinical trials must be taken into account when evaluating evidence provided by RCTs, including severe adverse events and hospitalisations and death. Clearly, adherence to care in these settings is profoundly different from that in real life.
A report on asthma deaths published by the UK College of Physicians underlines that the strongest risk factors for asthma death are overuse of β2-agonists, absence of maintenance anti-inflammatory treatment, previous hospitalisation and poor adherence to guideline recommendations [101]. The suggestions provided for preventing asthma deaths can be summarised in the concept that every hospital and primary care practice should have designated specifically labelled clinical services responsible for formal training in the identification of the patients at risk of asthma death and proper management of acute asthma [101]. This is particularly relevant considering that >95% of asthma deaths occur in adults with identifiable risk factors and that >85% of asthma deaths occur not acutely, but as progressive worsening. Data from the Finnish Asthma Programme confirm that the introduction of anti-inflammatory treatment (principally ICS) was associated with a decline in asthma morbidity, thereby reducing the utilisation of emergency services, hospitalisations and deaths [102]. Given this background, it is difficult to explore the mechanisms of action of currently available medications in terms of prevention of asthma mortality. Furthermore, it is impossible to conduct RCTs to test treatment efficacy or mechanisms on such an outcome due to the extremely small number of events.
Currently available biological treatments are effective in reducing exacerbations, hospitalisations and near-fatal adverse events, and it is possible that they may prevent acute fatal events. Real-life observations will provide this information in the future. However, all presently available agents, including approved biologicals and new chemical entities in development, are believed to work predominantly in patients with type 2 high disease [100]. Unfortunately, nothing new appears to be available for patients with severe type 2 low asthma [71, 96, 100].
Impact of ICS on long-term changes in lung function
In the majority of individuals with asthma, treatment with ICS improves symptoms and lung function, reduces the frequency of exacerbations, and reduces airway inflammation [6]. In addition, the very earliest studies of the efficacy of ICSs in asthma demonstrated their ability to reduce or eliminate the need for OCSs as a maintenance treatment [103, 104]. Furthermore, registry studies have shown that even low doses of ICS reduce the risk of severe asthma exacerbations and death from asthma [17, 105]. The ability of ICS to reduce the risk of severe exacerbations can even be seen when ICSs and rapid-onset inhaled β2-agonists, delivered from the same inhaler, are only used as a reliever treatment [66, 106].
It has been much more difficult to prove whether long-term ICS treatment leads to a better outcome with regard to preservation of lung function. As mentioned earlier, a substantial minority of patients with asthma experience accelerated decline in FEV1 and FEV1/FVC ratio, potentially leading to irreversible airflow limitation [107]. This is likely to be caused by airway wall thickening, so-called airway remodelling, rather than development of emphysema as in COPD [108]. Studies suggest that some components of airway remodelling may be reduced by ICS [109, 110]. Since ICS, particularly in combination with a LABA, can reduce the risk of severe asthma exacerbations that may accelerate FEV1 decline, early initiation of long-term treatment may alter the natural history of FEV1 decline in the subgroup of patients who are prone to rapid loss of lung function [111].
Observational, nonrandomised studies of both children and adults followed in asthma clinics [112, 113], and studies of adults with asthma from the general population [114], have suggested that ICS treatment may have beneficial effects on the course of lung function. However, this has been very difficult to prove in an RCT, since in excess of 3 years of observation are needed to draw conclusions about long-term changes in FEV1, due to the combination of considerable measurement error and a very modest age-related annual FEV1 decline [115]. In addition, randomisation of individuals with even mild asthma to placebo maintenance therapy may result in substantial withdrawal during such a study due to inadequately controlled symptoms and the occurrence of exacerbations.
However, two RCTs with sufficiently long observation periods have evaluated the effect of ICS on longitudinal lung function changes. The CAMP (Childhood Asthma Management Program) study randomised children aged 5–12 years with mild-to-moderate asthma to budesonide, nedocromil or placebo and followed them for up to 6 years [116]. The study found no benefit of ICS over either nedocromil or placebo regarding the growth velocity in post-bronchodilator FEV1. The START (Inhaled Steroid Treatment as Regular Therapy in Early Asthma) study randomised children and adults with mild persistent asthma of <2 years duration to either budesonide or placebo as maintenance medication [117]. There was a reduced mean decline from baseline in post-bronchodilator FEV1 at 1 and 3 years in the budesonide group compared with placebo, both in adult smokers and nonsmokers [118]. After 3 years, all patients were given budesonide; those switched from placebo to budesonide caught up to those who received budesonide throughout the study in terms of several clinical variables, including FEV1 [119]. This result on lung function is similar to that seen in the CAMP study.
Another study of early intervention with ICS showed clear benefits in the group who initiated ICS early compared with those initially treated with SABA as needed, including a better improvement of lung function [120]. After the initial 2 years, the participants who initially started on SABA were switched to ICS. On conclusion of the study, participants had their ICS dose adjusted in a real-life setting. After 13 years of follow-up, the investigators could no longer observe differences with regard to lung function in those initiating the ICS therapy early versus those who started ICS after 2 years [121].
Role of ICS, alone or in combination, in different asthma phenotypes
The understanding of the biology and pathophysiology of asthma has progressed, with the identification of a number of distinct phenotypes [87, 122, 123]. However, current international guidelines recommend initiating ICS treatment to almost all patients [6]. ICSs work through both positive gene regulation and gene repression, with the result of this dual action being potent anti-inflammatory action in the airways [124].
The improvement with ICS in some clinical parameters, such as spirometry, is variable [125]. As a result, different biomarkers, alone or in combination, are being used to increase the predictability of ICS response [126]. For example, sputum eosinophil levels have been shown to predict response to ICS [127, 128] and to predict exacerbation risk on ICS withdrawal [129]. In a separate study, titration of ICS treatment according to sputum eosinophil counts resulted in significantly fewer severe exacerbations compared with guideline-driven treatment [130]. However, the analysis of induced sputum is still not widely available for routine use. Furthermore, by using multiple markers of inflammation (FENO, serum eosinophilic cationic protein concentration and blood eosinophil count), incremental ICS dosing in persistent asthma is associated with a plateau in symptoms and lung function, but with progressive improvement in inflammatory outcomes and AHR [131]. Unfortunately, the use of either biomarker-based or symptom-based adjustment of ICS is not superior to physician assessment-based adjustment of ICS in terms of time to treatment failure [132].
The variable response to ICS is attributed to different mechanisms underlying airway inflammation [133]. A study using a panel of biomarkers that aimed to identify the presence of atopic inflammation and oxidative stress for prediction of clinical response to steroids showed that the combination of high FENO values and high urinary bromotyrosine levels (an indicator of oxidative stress) predicted a favourable clinical response to ICS therapy (in terms of Asthma Control Questionnaire score, FEV1 and AHR), although the lack of a placebo control limited the validity of the study [126]. A randomised pragmatic trial of ICS optimisation in severe asthma using a composite biomarker algorithm (FENO, blood eosinophils and serum periostin) to adjust ICS dose versus standard care has been recently proposed [134]. The U-BIOPRED (Unbiased BIOmarkers in PREDiction of respiratory disease outcomes) project is a 5-year European-wide project that aims to identify biomarkers for severe asthma [135]. Several biomarkers are currently available and U-BIOPRED will help clarify further the potential use of these and other biomarkers in routine practice, and provide evidence for the clinical utility of new potential biomarkers.
A landmark study published over 20 years ago in 1997 showed that in patients with persistent symptoms of asthma despite treatment with ICS, the addition of formoterol to budesonide therapy was able to reduce the rate of mild and severe exacerbations, and improved symptoms and lung function without lessening asthma control [76]. Subsequently, a series of other ICS/LABA combinations have demonstrated beneficial effects as maintenance therapy in patients with asthma [6]. For example, the GOAL (Gaining Optimal Asthma ControL) study demonstrated that an ICS/LABA combination (fluticasone/salmeterol) was more effective than the ICS alone in achieving asthma control over 1 year [136] and the benefit persisted for at least 6 months, with little evidence of loss of control with stable dosing [137]. The concept of achieving better disease control with maintenance ICS/LABA combinations compared with doubling ICS monotherapy in moderate-to-severe asthma has been widened to the use of an ICS/LABA combination as both maintenance and reliever, since such use ensures a timely administration of anti-inflammatory agents in the event of disease worsening [68, 98, 138]. The benefit of giving ICS concomitantly to fast-acting bronchodilators in case of symptom worsening has been applied also in mild asthma with beclometasone–salbutamol combination [106] and, more recently, with budesonide–formoterol combination [66, 67].
Finally, ICS therapy is associated with changes in relative abundance in the lower airway microbiome, particularly with the combination of ICSs and OCSs impacting on the α- and β-diversity of different bacterial species [139]. Even in patients with mild steroid-naive asthma, differences in the bronchial microbiome are associated with different immunological and clinical features of the disease, and response to ICS [140].
Conclusions
There is compelling evidence of the value of ICS in improving asthma control, as measured by improved symptoms, pulmonary function and reduced exacerbations. There is, however, less convincing evidence that ICS prevents the decline in pulmonary function that occurs in some, although not all, patients with asthma. Severe exacerbations are associated with a more rapid decline in pulmonary function, and by reducing the risk of severe exacerbations, it is likely that ICS will, at least partially, prevent this decline. Studies using administrative databases also support an important role for ICS in reducing asthma mortality, but the fact that asthma mortality is, fortunately, an uncommon event makes it highly improbable that this will be demonstrated in prospective trials.
Acknowledgements
Editorial support (in the form of editing for grammar, consistency, formatting references and drawing figures) was provided by David Young (Young Medical Communications and Consulting Ltd, Horsham, UK). This support was funded by Chiesi Farmaceutici SpA.
Footnotes
Support statement: This work was supported by Chiesi Farmaceutici SpA. Funding information for this article has been deposited with the Crossref Funder Registry.
Conflict of interest: L.M. Fabbri reports grants, personal fees and nonfinancial support from Chiesi, personal fees and nonfinancial support from AstraZeneca, GSK, Novartis, Menarini, Boehringer Ingelheim, Zambon, Pearl Therapeutics, nonfinancial support from Dompe, outside the submitted work.
Conflict of interest: I.D. Pavord reports speaker's honoraria, travel expenses and honoraria for attending advisory boards from AstraZeneca, GSK, Boehringer Ingelheim and Teva, grants and speaker fees, fees for advisory boards and travel expenses for attending international meetings from Chiesi, personal fees for advisory board work from Sanofi/Regeneron, Merck, Novartis, Knopp and Roche/Genentech, personal fees for speaking from Circassia and Mundipharma, grants and personal fees for advisory board work from Afferent, outside the submitted work.
Conflict of interest: A. Papi reports board membership, consultancy, payment for lectures, grants for research and travel expenses reimbursement from Chiesi, AstraZeneca, GSK, Boehringer Ingelheim, Mundipharma and Teva, payment for lectures and travel expenses reimbursement from Menarini, Novartis and Zambon, grants from Sanofi, outside the submitted work.
Conflict of interest: S. Petruzzelli is employed by Chiesi Farmaceutici SpA, the sponsor of the studies.
Conflict of interest: P. Lange reports grants and personal fees for teaching and advisory board work from AstraZeneca, Boehringer Ingelheim and GSK, personal fees for teaching and advisory board work from Chiesi, outside the submitted work.
Conflict of interest: P. O'Byrne reports receiving speaker fees from AstraZeneca, Chiesi, GSK, Medimmune and Novartis; advisory board membership with AstraZeneca, Medimmune, Novartis, GSK and Chiesi; and grants-in-aid from AstraZeneca, Medimmune, Genentech and Novartis.
References
- 1.Siegel SC. History of asthma deaths from antiquity. J Allergy Clin Immunol 1987; 80: 458–462. [DOI] [PubMed] [Google Scholar]
- 2.Salter HH. On Asthma: Its Pathology and Treatment. London, Churchill, 1860. [Google Scholar]
- 3.Carter BD, Abnet CC, Feskanich D, et al. Smoking and mortality – beyond established causes. N Engl J Med 2015; 372: 631–640. [DOI] [PubMed] [Google Scholar]
- 4.Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease 2019. https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf Date last accessed: March 8, 2019.
- 5.Sears MR. Worldwide trends in asthma mortality. Bull Int Union Tuberc Lung Dis 1991; 66: 79–83. [PubMed] [Google Scholar]
- 6.Global Initiative for Asthma Global Strategy for Asthma Management and Prevention. 2018 https://ginasthma.org/wp-content/uploads/2018/04/wms-GINA-2018-report-V1.3-002.pdf Date last accessed: March 8, 2019.
- 7.Silverstein MD, Reed CE, O'Connell EJ, et al. Long-term survival of a cohort of community residents with asthma. N Engl J Med 1994; 331: 1537–1541. [DOI] [PubMed] [Google Scholar]
- 8.Diaz-Guzman E, Khosravi M, Mannino DM. Asthma, chronic obstructive pulmonary disease, and mortality in the U.S. population. COPD 2011; 8: 400–407. [DOI] [PubMed] [Google Scholar]
- 9.Savage JH, Matsui EC, McCormack M, et al. The association between asthma and allergic disease and mortality: a 30-year follow-up study. J Allergy Clin Immunol 2014; 133: 1484–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang S, Vasquez MM, Halonen M, et al. Asthma, airflow limitation and mortality risk in the general population. Eur Respir J 2015; 45: 338–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kendzerska T, To TM, Aaron SD, et al. The impact of a history of asthma on long-term outcomes of people with newly diagnosed chronic obstructive pulmonary disease: a population study. J Allergy Clin Immunol 2017; 139: 835–843. [DOI] [PubMed] [Google Scholar]
- 12.Reed CE. The natural history of asthma. J Allergy Clin Immunol 2006; 118: 543–548. [DOI] [PubMed] [Google Scholar]
- 13.Lange P, Çolak Y, Ingebrigtsen TS, et al. Long-term prognosis of asthma, chronic obstructive pulmonary disease, and asthma-chronic obstructive pulmonary disease overlap in the Copenhagen City Heart study: a prospective population-based analysis. Lancet Respir Med 2016; 4: 454–462. [DOI] [PubMed] [Google Scholar]
- 14.Çolak Y, Afzal S, Nordestgaard BG, et al. Characteristics and prognosis of never-smokers and smokers with asthma in the Copenhagen General Population Study. A prospective cohort study. Am J Respir Crit Care Med 2015; 192: 172–181. [DOI] [PubMed] [Google Scholar]
- 15.Dantzer C, Tessier JF, Nejjari C, et al. Mortality of elderly subjects with self-reported asthma in a French cohort, 1991–1996. Eur J Epidemiol 2001; 17: 57–63. [DOI] [PubMed] [Google Scholar]
- 16.Campbell MJ, Cogman GR, Holgate ST, et al. Age specific trends in asthma mortality in England and Wales, 1983–95: results of an observational study. BMJ 1997; 314: 1439–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000; 343: 332–336. [DOI] [PubMed] [Google Scholar]
- 18.Suissa S, Ernst P. Inhaled corticosteroids: impact on asthma morbidity and mortality. J Allergy Clin Immunol 2001; 107: 937–944. [DOI] [PubMed] [Google Scholar]
- 19.Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases. Lancet 2018; 391: 350–400. [DOI] [PubMed] [Google Scholar]
- 20.Bloom CI, Nissen F, Douglas IJ, et al. Exacerbation risk and characterisation of the UK's asthma population from infants to old age. Thorax 2018; 73: 313–320. [DOI] [PubMed] [Google Scholar]
- 21.Fuchs O, Bahmer T, Rabe KF, et al. Asthma transition from childhood into adulthood. Lancet Respir Med 2017; 5: 224–234. [DOI] [PubMed] [Google Scholar]
- 22.McGeachie MJ, Yates KP, Zhou X, et al. Patterns of growth and decline in lung function in persistent childhood asthma. N Engl J Med 2016; 374: 1842–1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tai A, Tran H, Roberts M, et al. Outcomes of childhood asthma to the age of 50 years. J Allergy Clin Immunol 2014; 133: 1572–1578. [DOI] [PubMed] [Google Scholar]
- 24.Tagiyeva N, Devereux G, Fielding S, et al. Outcomes of childhood asthma and wheezy bronchitis. A 50-year cohort study. Am J Respir Crit Care Med 2016; 193: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez FD. Early-life origins of chronic obstructive pulmonary disease. N Engl J Med 2016; 375: 871–878. [DOI] [PubMed] [Google Scholar]
- 26.Lange P. Persistent airway obstruction in asthma. Am J Respir Crit Care Med 2013; 187: 1–2. [DOI] [PubMed] [Google Scholar]
- 27.Sears MR. Smoking, asthma, chronic airflow obstruction and COPD. Eur Respir J 2015; 45: 586–588. [DOI] [PubMed] [Google Scholar]
- 28.Thomson NC. Does age of onset of asthma influence the effect of cigarette smoking on lung function? Am J Respir Crit Care Med 2016; 194: 249–250. [DOI] [PubMed] [Google Scholar]
- 29.Hancox RJ, Gray AR, Poulton R, et al. The effect of cigarette smoking on lung function in young adults with asthma. Am J Respir Crit Care Med 2016; 194: 276–284. [DOI] [PubMed] [Google Scholar]
- 30.Aanerud M, Carsin A-E, Sunyer J, et al. Interaction between asthma and smoking increases the risk of adult airway obstruction. Eur Respir J 2015; 45: 635–643. [DOI] [PubMed] [Google Scholar]
- 31.Perret JL, Dharmage SC, Matheson MC, et al. The interplay between the effects of lifetime asthma, smoking, and atopy on fixed airflow obstruction in middle age. Am J Respir Crit Care Med 2013; 187: 42–48. [DOI] [PubMed] [Google Scholar]
- 32.Peat JK, Woolcock AJ, Cullen K. Rate of decline of lung function in subjects with asthma. Eur J Respir Dis 1987; 70: 171–179. [PubMed] [Google Scholar]
- 33.Lange P, Parner J, Vestbo J, et al. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med 1998; 339: 1194–1200. [DOI] [PubMed] [Google Scholar]
- 34.Bai TR, Vonk JM, Postma DS, et al. Severe exacerbations predict excess lung function decline in asthma. Eur Respir J 2007; 30: 452–456. [DOI] [PubMed] [Google Scholar]
- 35.O'Byrne PM, Pedersen S, Lamm CJ, et al. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med 2009; 179: 19–24. [DOI] [PubMed] [Google Scholar]
- 36.van Veen IH, Ten Brinke A, Sterk PJ, et al. Exhaled nitric oxide predicts lung function decline in difficult-to-treat asthma. Eur Respir J 2008; 32: 344–349. [DOI] [PubMed] [Google Scholar]
- 37.Coumou H, Westerhof GA, de Nijs SB, et al. Predictors of accelerated decline in lung function in adult-onset asthma. Eur Respir J 2018; 51: 1701785. [DOI] [PubMed] [Google Scholar]
- 38.Contoli M, Baraldo S, Marku B, et al. Fixed airflow obstruction due to asthma or chronic obstructive pulmonary disease: 5-year follow-up. J Allergy Clin Immunol 2010; 125: 830–837. [DOI] [PubMed] [Google Scholar]
- 39.de Nijs SB, Venekamp LN, Bel EH. Adult-onset asthma: is it really different? Eur Respir Rev 2013; 22: 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ulrik CS, Lange P. Decline of lung function in adults with bronchial asthma. Am J Respir Crit Care Med 1994; 150: 629–634. [DOI] [PubMed] [Google Scholar]
- 41.Amelink M, de Nijs SB, Berger M, et al. Non-atopic males with adult onset asthma are at risk of persistent airflow limitation. Clin Exp Allergy 2012; 42: 769–774. [DOI] [PubMed] [Google Scholar]
- 42.Porsbjerg C, Lange P, Ulrik CS. Lung function impairment increases with age of diagnosis in adult onset asthma. Respir Med 2015; 109: 821–827. [DOI] [PubMed] [Google Scholar]
- 43.Gupta RP, Mukherjee M, Sheikh A, et al. Persistent variations in national asthma mortality, hospital admissions and prevalence by socioeconomic status and region in England. Thorax 2018; 73: 706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marmot M. Inequalities in asthma mortality: a specific case of a general issue of health inequalities. Thorax 2018; 73: 704–705. [DOI] [PubMed] [Google Scholar]
- 45.Ulrik CS, Frederiksen J. Mortality and markers of risk of asthma death among 1,075 outpatients with asthma. Chest 1995; 108: 10–15. [DOI] [PubMed] [Google Scholar]
- 46.Lange P, Ulrik CS, Vestbo J. Mortality in adults with self-reported asthma. Copenhagen City Heart Study Group. Lancet 1996; 347: 1285–1289. [DOI] [PubMed] [Google Scholar]
- 47.Eftekhari P, Forder PM, Majeed T, et al. Impact of asthma on mortality in older women: an Australian cohort study of 10,413 women. Respir Med 2016; 119: 102–108. [DOI] [PubMed] [Google Scholar]
- 48.Backman H, Hedman L, Stridsman C, et al. A population-based cohort of adults with asthma: mortality and participation in a long-term follow-up. Eur Clin Respir J 2017; 4: 1334508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baarnes CB, Andersen ZJ, Tjønneland A, et al. Incidence and long-term outcome of severe asthma–COPD overlap compared to asthma and COPD alone: a 35-year prospective study of 57,053 middle-aged adults. Int J Chron Obstruct Pulmon Dis 2017; 12: 571–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Markowe HL, Bulpitt CJ, Shipley MJ, et al. Prognosis in adult asthma: a national study. Br Med J (Clin Res Ed) 1987; 295: 949–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garcia-Aymerich J. The role of smoking in the association between asthma and cardiovascular disease. An example of poorly controlled confounding. Am J Respir Crit Care Med 2015; 192: 123. [DOI] [PubMed] [Google Scholar]
- 52.Woolcock A, Rubinfeld AR, Seale JP, et al. Thoracic society of Australia and New Zealand. Asthma management plan, 1989. Med J Aust 1989; 151: 650–653. [PubMed] [Google Scholar]
- 53.Hargreave FE, Dolovich J, Newhouse MT. The assessment and treatment of asthma: a conference report. J Allergy Clin Immunol 1990; 85: 1098–1111. [DOI] [PubMed] [Google Scholar]
- 54.Guidelines on the Management of Asthma. Statement by the British Thoracic Society, the Brit. Paediatric Association, the Research Unit of the Royal College of Physicians of London, the King's Fund Centre, the National Asthma Campaign, the Royal College of General Practitioners, the General Practitioners in Asthma Group, the Brit. Assoc. of Accident and Emergency Medicine, and the Brit. Paediatric Respiratory Group. Thorax 1993; 48: S1–S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute. National Asthma Education Program. Expert Panel Report. J Allergy Clin Immunol 1991; 88: 425–534. [PubMed] [Google Scholar]
- 56.Asher MI, Pattemore PK, Harrison AC, et al. International comparison of the prevalence of asthma symptoms and bronchial hyperresponsiveness. Am Rev Respir Dis 1988; 138: 524–529. [DOI] [PubMed] [Google Scholar]
- 57.O'Byrne PM. Airway inflammation and airway hyperresponsiveness. Chest 1986; 90: 575–577. [DOI] [PubMed] [Google Scholar]
- 58.O'Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? Eur Respir J 2017; 50: 1701103. [DOI] [PubMed] [Google Scholar]
- 59.Gauvreau GM, Jordana M, Watson RM, et al. Effect of regular inhaled albuterol on allergen-induced late responses and sputum eosinophils in asthmatic subjects. Am J Respir Crit Care Med 1997; 156: 1738–1745. [DOI] [PubMed] [Google Scholar]
- 60.Sears MR, Taylor DR, Print CG, et al. Regular inhaled beta-agonist treatment in bronchial asthma. Lancet 1990; 336: 1391–1396. [DOI] [PubMed] [Google Scholar]
- 61.Spitzer WO, Suissa S, Ernst P, et al. The use of beta-agonists and the risk of death and near death from asthma. N Engl J Med 1992; 326: 501–506. [DOI] [PubMed] [Google Scholar]
- 62.Salpeter SR, Buckley NS, Ormiston TM, et al. Meta-analysis: effect of long-acting beta-agonists on severe asthma exacerbations and asthma-related deaths. Ann Intern Med 2006; 144: 904–912. [DOI] [PubMed] [Google Scholar]
- 63.Reddel HK, Bateman ED, Becker A, et al. A summary of the new GINA strategy: a roadmap to asthma control. Eur Respir J 2015; 46: 622–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reddel HK, Busse WW, Pedersen S, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: a post-hoc efficacy analysis of the START study. Lancet 2017; 389: 157–166. [DOI] [PubMed] [Google Scholar]
- 65.Global Initiative for Asthma Pocket Guide for Asthma Management and Prevention 2019. https://ginasthma.org/wp-content/uploads/2019/04/GINA-2019-main-Pocket-Guide-wms.pdf Date last accessed April 15, 2019.
- 66.O'Byrne PM, FitzGerald JM, Bateman ED, et al. Inhaled combined budesonide–formoterol as needed in mild asthma. N Engl J Med 2018; 378: 1865–1876. [DOI] [PubMed] [Google Scholar]
- 67.Bateman ED, Reddel HK, O'Byrne PM, et al. As-needed budesonide–formoterol versus maintenance budesonide in mild asthma. N Engl J Med 2018; 378: 1877–1887. [DOI] [PubMed] [Google Scholar]
- 68.O'Byrne PM, Bisgaard H, Godard PP, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med 2005; 171: 129–136. [DOI] [PubMed] [Google Scholar]
- 69.Larsen K, Zhu J, Feldman LY, et al. The annual September peak in asthma exacerbation rates. Still a reality? Ann Am Thorac Soc 2016; 13: 231–239. [DOI] [PubMed] [Google Scholar]
- 70.Pelkonen MK, Notkola I-LK, Laatikainen TK, et al. 30-year trends in asthma and the trends in relation to hospitalization and mortality. Respir Med 2018; 142: 29–35. [DOI] [PubMed] [Google Scholar]
- 71.Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014; 43: 343–373. [DOI] [PubMed] [Google Scholar]
- 72.Israel E, Reddel HK. Severe and difficult-to-treat asthma in adults. N Engl J Med 2017; 377: 965–976. [DOI] [PubMed] [Google Scholar]
- 73.Ivanova JI, Bergman R, Birnbaum HG, et al. Effect of asthma exacerbations on health care costs among asthmatic patients with moderate and severe persistent asthma. J Allergy Clin Immunol 2012; 129: 1229–1235. [DOI] [PubMed] [Google Scholar]
- 74.Pavord ID. Complex airway disease: an approach to assessment and management. Lancet Respir Med 2013; 1: 84–90. [DOI] [PubMed] [Google Scholar]
- 75.Shaw DE, Berry MA, Hargadon B, et al. Association between neutrophilic airway inflammation and airflow limitation in adults with asthma. Chest 2007; 132: 1871–1875. [DOI] [PubMed] [Google Scholar]
- 76.Pauwels RA, Löfdahl CG, Postma DS, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med 1997; 337: 1405–1411. [DOI] [PubMed] [Google Scholar]
- 77.Hanania NA, Wenzel S, Roseń K, et al. Exploring the effects of omalizumab in allergic asthma: an analysis of biomarkers in the EXTRA study. Am J Respir Crit Care Med 2013; 187: 804–811. [DOI] [PubMed] [Google Scholar]
- 78.Chen W, Marra CA, Lynd LD, et al. The natural history of severe asthma and influences of early risk factors: a population-based cohort study. Thorax 2016; 71: 267–275. [DOI] [PubMed] [Google Scholar]
- 79.Busse WW, Bateman ED, Caplan AL, et al. Combined analysis of asthma safety trials of long-acting β2-agonists. N Engl J Med 2018; 378: 2497–2505. [DOI] [PubMed] [Google Scholar]
- 80.Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet 2012; 380: 651–659. [DOI] [PubMed] [Google Scholar]
- 81.Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med 2014; 371: 1198–1207. [DOI] [PubMed] [Google Scholar]
- 82.Chupp GL, Bradford ES, Albers FC, et al. Efficacy of mepolizumab add-on therapy on health-related quality of life and markers of asthma control in severe eosinophilic asthma (MUSCA): a randomised, double-blind, placebo-controlled, parallel-group, multicentre, phase 3b trial. Lancet Respir Med 2017; 5: 390–400. [DOI] [PubMed] [Google Scholar]
- 83.FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2016; 388: 2128–2141. [DOI] [PubMed] [Google Scholar]
- 84.Bleecker ER, FitzGerald JM, Chanez P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting beta2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet 2016; 388: 2115–2127. [DOI] [PubMed] [Google Scholar]
- 85.Castro M, Zangrilli J, Wechsler ME, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med 2015; 3: 355–366. [DOI] [PubMed] [Google Scholar]
- 86.Castro M, Corren J, Pavord ID, et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N Engl J Med 2018; 378: 2486–2496. [DOI] [PubMed] [Google Scholar]
- 87.Haldar P, Pavord ID, Shaw DE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med 2008; 178: 218–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Haldar P, Brightling CE, Hargadon B, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med 2009; 360: 973–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Heaney LG, Djukanovic R, Woodcock A, et al. Research in progress: Medical Research Council United Kingdom Refractory Asthma Stratification Programme (RASP-UK). Thorax 2016; 71: 187–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ortega HG, Yancey SW, Mayer B, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir Med 2016; 4: 549–556. [DOI] [PubMed] [Google Scholar]
- 91.Sweeney J, Patterson CC, Menzies-Gow A, et al. Comorbidity in severe asthma requiring systemic corticosteroid therapy: cross-sectional data from the Optimum Patient Care Research Database and the British Thoracic Difficult Asthma Registry. Thorax 2016; 71: 339–346. [DOI] [PubMed] [Google Scholar]
- 92.Waljee AK, Rogers MAM, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ 2017; 357: j1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bel EH, Wenzel SE, Thompson PJ, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med 2014; 371: 1189–1197. [DOI] [PubMed] [Google Scholar]
- 94.Rabe KF, Nair P, Brusselle G, et al. Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. N Engl J Med 2018; 378: 2475–2485. [DOI] [PubMed] [Google Scholar]
- 95.Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med 2017; 376: 2448–2458. [DOI] [PubMed] [Google Scholar]
- 96.Papi A, Brightling C, Pedersen SE, et al. Asthma. Lancet 2018; 391: 783–800. [DOI] [PubMed] [Google Scholar]
- 97.Greening AP, Ind PW, Northfield M, et al. Added salmeterol versus higher-dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Allen & Hanburys Limited UK Study Group. Lancet 1994; 344: 219–224. [DOI] [PubMed] [Google Scholar]
- 98.Rabe KF, Atienza T, Magyar P, et al. Effect of budesonide in combination with formoterol for reliever therapy in asthma exacerbations: a randomised controlled, double-blind study. Lancet 2006; 368: 744–753. [DOI] [PubMed] [Google Scholar]
- 99.Kerstjens HAM, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med 2012; 367: 1198–1207. [DOI] [PubMed] [Google Scholar]
- 100.McGregor MC, Krings JG, Nair P, et al. Role of biologics in asthma. Am J Respir Crit Care Med 2019; 199: 433–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Royal College of Physicians Why Asthma Still Kills: The National Review of Asthma Deaths. London, RCP, 2014. [Google Scholar]
- 102.Haahtela T, Tuomisto LE, Pietinalho A, et al. A 10 year asthma programme in Finland: major change for the better. Thorax 2006; 61: 663–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cameron SJ, Cooper EJ, Crompton GK, et al. Substitution of beclomethasone aerosol for oral prednisolone in the treatment of chronic asthma. Br Med J 1973; 4: 205–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Brown HM, Storey G, George WH. Beclomethasone dipropionate: a new steroid aerosol for the treatment of allergic asthma. Br Med J 1972; 1: 585–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ernst P, Spitzer WO, Suissa S, et al. Risk of fatal and near-fatal asthma in relation to inhaled corticosteroid use. JAMA 1992; 268: 3462–3464. [PubMed] [Google Scholar]
- 106.Papi A, Canonica GW, Maestrelli P, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. N Engl J Med 2007; 356: 2040–2052. [DOI] [PubMed] [Google Scholar]
- 107.Ernst P. Inhaled corticosteroids moderate lung function decline in adults with asthma. Thorax 2006; 61: 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hudon C, Turcotte H, Laviolette M, et al. Characteristics of bronchial asthma with incomplete reversibility of airflow obstruction. Ann Allergy Asthma Immunol 1997; 78: 195–202. [DOI] [PubMed] [Google Scholar]
- 109.Chetta A, Marangio E, Olivieri D. Inhaled steroids and airway remodelling in asthma. Acta Biomed 2003; 74: 121–125. [PubMed] [Google Scholar]
- 110.Kurashima K, Kanauchi T, Hoshi T, et al. Effect of early versus late intervention with inhaled corticosteroids on airway wall thickness in patients with asthma. Respirology 2008; 13: 1008–1013. [DOI] [PubMed] [Google Scholar]
- 111.Haahtela T. Lung function decline in asthma and early intervention with inhaled corticosteroids. Chest 2006; 129: 1405–1406. [DOI] [PubMed] [Google Scholar]
- 112.Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994; 88: 373–381. [DOI] [PubMed] [Google Scholar]
- 113.Dijkstra A, Vonk JM, Jongepier H, et al. Lung function decline in asthma: association with inhaled corticosteroids, smoking and sex. Thorax 2006; 61: 105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lange P, Scharling H, Ulrik CS, et al. Inhaled corticosteroids and decline of lung function in community residents with asthma. Thorax 2006; 61: 100–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Burrows B, Lebowitz MD, Camilli AE, et al. Longitudinal changes in forced expiratory volume in one second in adults. Methodologic considerations and findings in healthy nonsmokers. Am Rev Respir Dis 1986; 133: 974–980. [DOI] [PubMed] [Google Scholar]
- 116.Childhood Asthma Management Program Research Group Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000; 343: 1054–1063. [DOI] [PubMed] [Google Scholar]
- 117.Pauwels RA, Pedersen S, Busse WW, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003; 361: 1071–1076. [DOI] [PubMed] [Google Scholar]
- 118.O'Byrne PM, Lamm CJ, Busse WW, et al. The effects of inhaled budesonide on lung function in smokers and nonsmokers with mild persistent asthma. Chest 2009; 136: 1514–1520. [DOI] [PubMed] [Google Scholar]
- 119.Busse WW, Pedersen S, Pauwels RA, et al. The Inhaled Steroid Treatment As Regular Therapy in Early Asthma (START) study 5-year follow-up: effectiveness of early intervention with budesonide in mild persistent asthma. J Allergy Clin Immunol 2008; 121: 1167–1174. [DOI] [PubMed] [Google Scholar]
- 120.Haahtela T, Järvinen M, Kava T, et al. Comparison of a β2-agonist, terbutaline, with an inhaled corticosteroid, budesonide, in newly detected asthma. N Engl J Med 1991; 325: 388–392. [DOI] [PubMed] [Google Scholar]
- 121.Haahtela T, Tamminen K, Kava T, et al. Thirteen-year follow-up of early intervention with an inhaled corticosteroid in patients with asthma. J Allergy Clin Immunol 2009; 124: 1180–1185. [DOI] [PubMed] [Google Scholar]
- 122.Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med 2010; 181: 315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med 2012; 18: 716–725. [DOI] [PubMed] [Google Scholar]
- 124.Djukanović R, Wilson JW, Britten KM, et al. Effect of an inhaled corticosteroid on airway inflammation and symptoms in asthma. Am Rev Respir Dis 1992; 145: 669–674. [DOI] [PubMed] [Google Scholar]
- 125.Adams NP, Jones PW. The dose–response characteristics of inhaled corticosteroids when used to treat asthma: an overview of Cochrane systematic reviews. Respir Med 2006; 100: 1297–1306. [DOI] [PubMed] [Google Scholar]
- 126.Cowan DC, Taylor DR, Peterson LE, et al. Biomarker-based asthma phenotypes of corticosteroid response. J Allergy Clin Immunol 2015; 135: 877–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Brightling CE, Green RH, Pavord ID. Biomarkers predicting response to corticosteroid therapy in asthma. Treat Respir Med 2005; 4: 309–316. [DOI] [PubMed] [Google Scholar]
- 128.Demarche SF, Schleich FN, Henket MA, et al. Effectiveness of inhaled corticosteroids in real life on clinical outcomes, sputum cells and systemic inflammation in asthmatics: a retrospective cohort study in a secondary care centre. BMJ Open 2017; 7: e018186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Deykin A, Lazarus SC, Fahy JV, et al. Sputum eosinophil counts predict asthma control after discontinuation of inhaled corticosteroids. J Allergy Clin Immunol 2005; 115: 720–727. [DOI] [PubMed] [Google Scholar]
- 130.Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet 2002; 360: 1715–1721. [DOI] [PubMed] [Google Scholar]
- 131.Anderson WJ, Short PM, Jabbal S, et al. Inhaled corticosteroid dose response in asthma: should we measure inflammation? Ann Allergy Asthma Immunol 2017; 118: 179–185. [DOI] [PubMed] [Google Scholar]
- 132.Calhoun WJ, Ameredes BT, King TS, et al. Comparison of physician-, biomarker-, and symptom-based strategies for adjustment of inhaled corticosteroid therapy in adults with asthma: the BASALT randomized controlled trial. JAMA 2012; 308: 987–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Reddel HK, Taylor DR, Bateman ED, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009; 180: 59–99. [DOI] [PubMed] [Google Scholar]
- 134.Hanratty CE, Matthews JG, Arron JR, et al. A randomised pragmatic trial of corticosteroid optimization in severe asthma using a composite biomarker algorithm to adjust corticosteroid dose versus standard care: study protocol for a randomised trial. Trials 2018; 19: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.European Lung Foundation Unbiased BIOmarkers in PREDiction of respiratory disease outcomes 2019.. www.europeanlung.org/en/projects-and-research/projects/u-biopred/home Date last accessed March 8, 2019.
- 136.Bateman ED, Boushey HA, Bousquet J, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med 2004; 170: 836–844. [DOI] [PubMed] [Google Scholar]
- 137.Bateman ED, Bousquet J, Busse WW, et al. Stability of asthma control with regular treatment: an analysis of the Gaining Optimal Asthma controL (GOAL) study. Allergy 2008; 63: 932–938. [DOI] [PubMed] [Google Scholar]
- 138.Papi A, Corradi M, Pigeon-Francisco C, et al. Beclometasone–formoterol as maintenance and reliever treatment in patients with asthma: a double-blind, randomised controlled trial. Lancet Respir Med 2013; 1: 23–31. [DOI] [PubMed] [Google Scholar]
- 139.Denner DR, Sangwan N, Becker JB, et al. Corticosteroid therapy and airflow obstruction influence the bronchial microbiome, which is distinct from that of bronchoalveolar lavage in asthmatic airways. J Allergy Clin Immunol 2016; 137: 1398–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Durack J, Lynch SV, Nariya S, et al. Features of the bronchial bacterial microbiome associated with atopy, asthma, and responsiveness to inhaled corticosteroid treatment. J Allergy Clin Immunol 2017; 140: 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]