Abstract
Background
Higher circulating levels of tissue inhibitor of matrix metalloproteinases (TIMP)-1 early after ischemic stroke have been associated with lower survival. The objectives of this study were to determine serum TIMP-1 levels during the first week of a severe cerebral infarction in surviving and non-surviving patients, and whether those levels during the first week could be used as a mortality biomarker for these patients.
Methods
We included patients with severe malignant middle cerebral artery infarction (MMCAI) defined as computer tomography showing ischaemic changes in more than 50% of the middle cerebral artery territory and Glasgow Coma Scale (GCS) ≤ 8. We measured serum levels of matrix metalloproteinases (MMP)-9 and TIMP-1. End-point study was 30-day mortality.
Results
We found higher TIMP-1 concentrations at days 1 (p < 0.001), 4 (p = 0.001), and 8 (p = 0.03) of MMCAI in non- urviving (n = 34) than in surviving (n = 34) patients. We found lower serum MMP-9 concentrations at day 1 (p = 0.03) of MMCAI and no significant differences at days 4 and 8. ROC curve analysis of TIMP-1 concentrations performed at days 1, 4, and 8 of MMCAI showed an area under curve to predict 30-day mortality of 81% (p < 0.001), 80% (p < 0.001) and 72% (p = 0.07) respectively.
Conclusions
The new findings of our study were that non-surviving MMCAI patients showed higher serum TIMP-1 levels during the first week of MMCAI that surviving patients, and those levels during the first week of MMCAI could be used as mortality biomarkers.
Keywords: TIMP-1, Ischemic stroke, Patients, Mortality, Prognosis
Background
Ischemic stroke produces many disabilities, deaths and healthcare expenses [1]. Matrix metalloproteinases (MMPs) are a family of proteinases whose function is to remodel the extracellular matrix (ECM) and are regulated by tissue inhibitors of matrix metalloproteinases (TIMPs). MMPs play a role in different physiological processes such as morphogenesis, tissue remodelling, menstrual cycle, and angiogenesis, and in different pathological processes such as atherosclerosis, arthritis, tumour invasion [2, 3], and cerebral ischemia [4–6].
Higher circulating MMP-9 levels have been found in ischemic stroke patients with worst neurologic outcome [7–23]. In addition, higher circulating TIMP-1 levels at day 1 of ischemic stroke have been associated with poor neurological outcome [24, 25] and lower survival [26]. However, there is no data about circulating TIMP-1 levels in surviving and non-surviving patients with cerebral infarction during the first week of cerebral infarction. Thus, the objectives of this study were to compare serum TIMP-1 levels during the first week of a severe cerebral infarction between non-surviving and surviving patients and to determine whether those levels during the first week of a severe cerebral infarction could be used as a biomarker of early mortality.
Methods
Design and subjects
This was an observational, prospective study, carried out in Spain in 6 Critical Care Units. The period time for patient recruitment was 2009–2012. The Institutional Review Board of the 6 hospitals approved the protocol study. The hospitals that participated in the study were: H. Insular in Las Palmas de Gran Canaria, H. General de La Palma in La Palma, H. Universitario de Canarias in La Laguna, H. Clínico Universitario de Valencia in Valencia, H. Universitario Nuestra Señora de Candelaria in Santa Cruz de Tenerife, and H. Universitario Dr. Negrín in Las Palmas de Gran Canaria. We obtained the written informed consent from some family member of the patient to participate in the study.
We included in the study patients with severe malignant middle cerebral artery infarction (MMCAI). We diagnosed ischemic stroke based on clinical and computed tomography findings [1]. We considered that patients showed a severe MMCAI when the findings of computer tomography showed ischaemic changes in more than 50% of the middle cerebral artery territory and patients showed an acute neurological deterioration consisting of a Glasgow Coma Scale (GCS) [27]≤8. We excluded those patients with age less than 18 years, inflammatory or malignant disease, or pregnancy.
We had previously determined serum levels of TIMP-1 and MMP-9 at MMCAI diagnosis in some of those patients [26]. In our current work, we have determined those levels in 68 patients on days 1, 4 and 8 of MMCAI.
Variables recorded
We recorded the following variables from the patients: age, diabetes mellitus, sex, arterial hypertension, chronic renal failure, chronic obstructive pulmonary disease (COPD), heart failure, Acute Physiology and Chronic Health Evaluation II (APACHE II) score [28], GCS, body temperature, creatinine, sodium, bilirubin, glycaemia, lactic acid, pressure of arterial oxygen (PaO2), fraction inspired oxygen (FI02), PaO2/FIO2 ratio, international normalized ratio (INR), fibrinogen, activated partial thromboplastin time (aPTT), leukocytes, platelets, haemoglobin, haemorrhagic transformation, infarct volume, midline shift, thrombolysis, and decompressive craniectomy. End-point study was 30-day mortality.
Blood samples and serum level determination of MMP-9 and TIMP-1
Serum blood samples were obtained on days 1, 4 and 8 of MMCAI and frozen at − 80 °C until assay determinations in the Atherosclerosis Research Laboratory in CIMA-Navarra University (Pamplona, Spain). MMP-9 and TIMP-1 determinations were performed by ELISAs using the kits Quantikine® (R&D Systems, Abingdon, United Kingdom). The intra-assay coefficient of variation (CV) in both techniques was 5%, the inter-assay CV for each assay were 8 and 5% respectively, and detection limit were 0.16 ng/mL and 0.08 ng/mL respectively.
Statistical methods
We tested normality assumption. Continuous variables that showed a normal distribution were reported as mean (standard deviation) and compared between patient groups (surviving and non-surviving) with Student’s t test. Continuous variables that were not normally distributed were reported as median (interquartile ranges) and compared between patient groups with Wilcoxon-Mann-Whitney test. Categorical variables were reported as frequencies (percentages) and compared between patient groups with chi-square test. We used the technique of receiver operating characteristic (ROC) to determine the capacity for 30-day mortality prediction by serum TIMP-1 levels at days 1, 4 and 8 of MMCAI. We used the Spearman correlation coefficient to test the association between continuous variables. We carried out a multiple logistic regression analysis to determine the association between serum TIMP-1 levels and 30 day-mortality controlling for lactic acid, GCS, and platelet count. We used SPSS 17.0 (SPSS Inc., Chicago, IL, USA), NCSS 2000 (Kaysville, Utah) and LogXact 4.1 (Cytel Co., Cambridge, MA) to do statistical analyses. We accepted as statistically significant those p-values lower than 0.05.
Results
Table 1 shows clinical variables of surviving (n = 34) and non-surviving (n = 34) patients. We did not find significant differences between groups in age, diabetes mellitus, sex, arterial hypertension, chronic renal failure, COPD, heart failure, APACHE-II, body temperature, creatinine, sodium, bilirubin, glycaemia, lactic acid, PaO2, PaO2/FIO2 ratio, INR, fibrinogen, aPTT, leukocytes, haemoglobin, haemorrhagic transformation, infarct volume, midline shift, thrombolysis, or decompressive craniectomy. Non-surviving patients showed lower GCS and platelets than survivors.
Table 1.
Clinical and biochemical characteristics of surviving and non-surviving MMCAI patients
| Survivors (n = 34) | Non-survivors (n = 34) | P- value | |
|---|---|---|---|
| Age (years) - median (p 25–75) | 59 (47–68) | 63 (53–70) | 0.36 |
| Diabetes mellitus - n (%) | 4 (11.8) | 9 (26.5) | 0.22 |
| Gender female - n (%) | 14 (41.2) | 13 (38.2) | 0.99 |
| Arterial hypertension - n (%) | 19 (55.9) | 16 (47.1) | 0.63 |
| Chronic renal failure - n (%) | 2 (5.9) | 2 (5.9) | 0.99 |
| COPD - n (%) | 1 (2.9) | 1 (2.9) | 0.99 |
| Heart failure - n (%) | 1 (2.9) | 1 (2.9) | 0.99 |
| APACHE-II score - mean ± SD | 20.38 ± 6.89 | 22.85 ± 5.93 | 0.12 |
| GCS score - median (p 25–75) | 7 (6–8) | 6 (3–7) | 0.01 |
| Temperature (°C) - median (p 25–75) | 36.4 (36.0–37.0) | 36.9 (36.0–37.3) | 0.15 |
| Creatinine (mg/dl) - median (p 25–75) | 0.80 (0.60–1.13) | 1.00 (0.70–1.25) | 0.19 |
| Sodium (mEq/L)- median (p 25–75) | 139 (136–145) | 140 (139–145) | 0.38 |
| Bilirubin (mg/dl) - median (p 25–75) | 0.60 (0.40–0.83) | 0.60 (0.33–1.10) | 0.95 |
| Glycemia (g/dL) - median (p 25–75) | 127 (100–170) | 136 (118–162) | 0.40 |
| Lactic acid (mmol/L)-median (p 25–75) | 1.20 (0.90–1.70) | 1.55 (1.00–2.70) | 0.05 |
| PaO2 (mmHg) - median (p 25–75) | 156 (105–293) | 115 (94–267) | 0.26 |
| PaO2/FI02 ratio - mean ± SD | 298 ± 116 | 262 ± 96 | 0.17 |
| INR - median (p 25–75) | 1.06 (1.00–1.20) | 1.20 (1.01–1.31) | 0.07 |
| Fibrinogen (mg/dl) - median (p 25–75) | 443 (416–489) | 419 (337–631) | 0.90 |
| aPTT (seconds) - median (p 25–75) | 28 (25–30) | 27 (26–32) | 0.91 |
| Leukocytes-median*103/mm3 (p 25–75) | 12.4 (9.6–16.9) | 13.9 (9.7–20.1) | 0.32 |
| Hemoglobin (g/dL) - mean ± SD | 12.60 ± 1.73 | 12.82 ± 1.96 | 0.67 |
| Platelets - mean ± SD | 225242 ± 84667 | 179382 ± 61975 | 0.01 |
| Haemorrhagic transformation - n (%) | 7 (20.6) | 6 (17.6) | 0.99 |
| Volumen infarction (ml) - mean ± SD | 162 ± 82 | 182 ± 110 | 0.61 |
| Midline shift (mm) - mean ± SD | 7.47 ± 6.14 | 9.09 ± 6.60 | 0.44 |
| Thrombolysis - n (%) | 11 (32.4) | 10 (29.4) | 0.99 |
| Decompressive craniectomy – n (%) | 9 (26.5) | 7 (20.6) | 0.78 |
| MMP-9 (ng/mL) - median (p 25–75) | 839 (719–1192) | 708 (396–949) | 0.03 |
| TIMP-1 (ng/mL) - median (p 25–75) | 206 (173–262) | 375 (248–468) | < 0.001 |
P 25–75 Percentile 25th–75th, SD Standard deviation, COPD Chronic obstructive pulmonary disease, APACHE II Acute Physiology and Chronic Health Evaluation, GCS Glasgow Coma Scale, PaO2 Pressure of arterial oxygen/fraction inspired oxygen, FIO2 Pressure of arterial oxygen/fraction inspired oxygen, INR International normalized ratio, aPTT Activated partial thromboplastin time, MMP Matrix metalloproteinase, TIMP Tissue inhibitor of matrix metalloproteinases
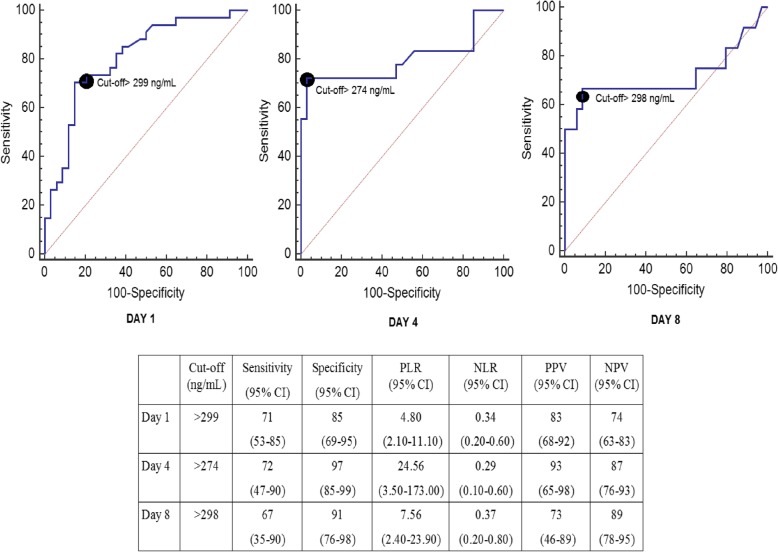
We found higher serum TIMP-1 concentrations at days 1 (p < 0.001), 4 (p = 0.001), and 8 (p = 0.03) of MMCAI in non-surviving than in the surviving patient group (Table 2 and Fig. 1). We found lower serum MMP-9 concentrations at day 1 (p = 0.03) of MMCAI in the non- surviving than in the surviving patient group; however, we did not find statistically significant differences in serum MMP-9 concentrations at days 4 and 8 (Table 2 and Fig. 1).
Table 2.
Serum TIMP-1 and MMP-9 levels at day 1, 4 and 8 of severe MMCAI in 30-day surviving and non-surviving patients
| Parameters Median and percentiles 25th -75th |
Survivors | Nonsurvivors | P |
|---|---|---|---|
| Day 1 | (n = 34) | (n = 34) | |
| TIMP-1 (ng/mL) - median (p 25–75) | 206 (173–262) | 375 (248–468) | < 0.001 |
| MMP-9 (ng/mL) - median (p 25–75) | 839 (719–1192) | 708 (396–949) | 0.03 |
| Day 4 | (n = 34) | (n = 18) | |
| TIMP-1 (ng/mL) - median (p 25–75) | 208 (193–247) | 350 (213–461) | < 0.001 |
| MMP-9 (ng/mL) - median (p 25–75) | 596 (408–792) | 414 (183–884) | 0.13 |
| Day 8 | (n = 34) | (n = 12) | |
| TIMP-1 (ng/mL) - median (p 25–75) | 234 (213–262) | 370 (211–451) | 0.03 |
| MMP-9 (ng/mL) - median (p 25–75) | 370 (295–721) | 361 (211–459) | 0.61 |
Fig. 1.
Serum TIMP-1 and MMP-9 levels at day 1, 4 and 8 of severe MMCAI in 30-day surviving and non-surviving
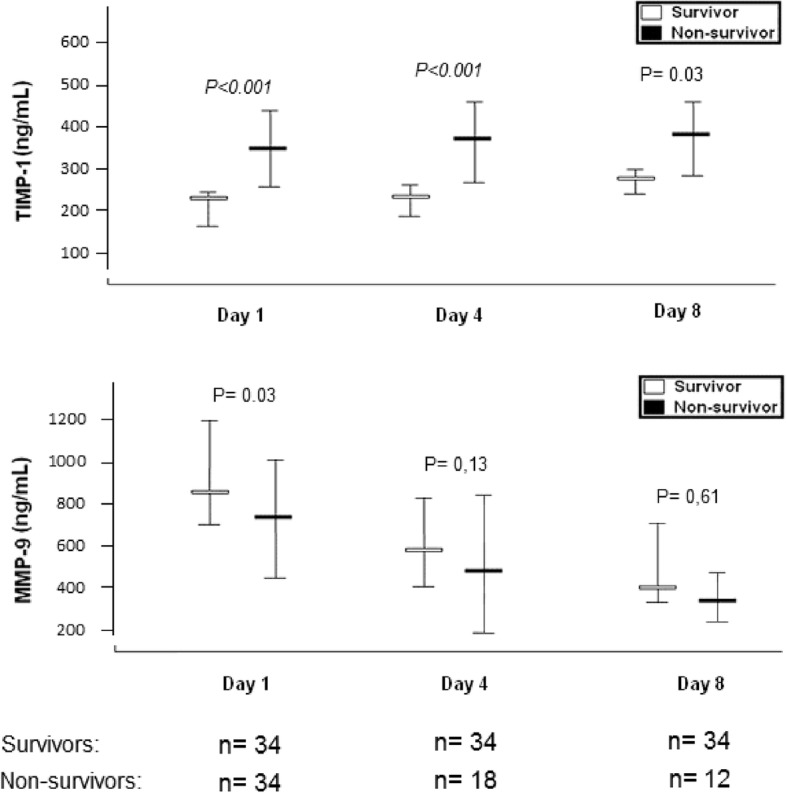
ROC curve analyses assessing serum TIMP-1 concentrations at days 1, 4, and 8 of MMCAI showed an area under curve (and 95% confidence interval) to predict 30-day mortality of 81% (69–89%; p < 0.001), 80% (66–90%; p < 0.001) and 72% (56–84%, p = 0.07) respectively (Fig. 2).
Fig. 2.
Receiver operation characteristic analysis using serum TIMP-1 levels at day 1, 4 and 8 of severe MMCAI as predictor of mortality at 30 days. CI: confidence intervals, PLR: positive likelihood ratio, NLR: negative likelihood ratio, PPV: positive predicted value, NPV: negative predicted value
In multiple logistic regression analysis we found that serum TIMP-1 levels were associated with 30-day mortality controlling for platelet count, GCS and lactic acid (OR = 1.011; 95% CI = 1.005–1.018; p = 0.001) (Table 3).
Table 3.
Multiple logistic regression analysis to predict 30-day mortality
| Variable | Odds Ratio | 95% Confidence Interval | P |
|---|---|---|---|
| TIMP-1 (ng/mL) | 1.011 | 1.005–1.018 | 0.001 |
| Lactic acid (mmol/L) | 1.131 | 0.626–2.046 | 0.68 |
| Platelet count (each 1,000/mm3) | 0.991 | 0.981–1.001 | 0.08 |
| Glasgow Coma Scale (points) | 0.707 | 0.497–1.005 | 0.054 |
No association between serum levels of TIMP-1 and MMP-9 at days 1 (rho = − 0.17; p = 0.16), 4 (rho = 0.02; p = 0.86) or 8 (rho = 0.11; p = 0.46) could be demonstrated.
Discussion
The new findings of our study were that non-surviving MMCAI patients showed higher serum TIMP-1 levels during the first week of MMCAI than surviving patients, and that those levels could be used as mortality biomarkers.
Previous studies found higher brain concentrations of TIMP-1 in infarcted than in healthy brain areas [29], higher monocytes expression of TIMP-1 in ischemic stroke patients than in healthy subjects [30], and higher circulating levels of TIMP-1 in ischemic stroke patients than in controls [31–35]. In addition, higher circulating TIMP-1 levels at day 1 of ischemic stroke have been previously associated with poor neurological outcome [24, 25] and lower survival [26]. Thus, the finding in our current study that serum TIMP-1 levels during the first week of a severe MMCAI were higher in surviving than in non-surviving patients is a novel finding. Previously, we also found that circulating TIMP-1 levels on the first day of MMCAI could be used as biomarkers of mortality [26]. Therefore, according to the results of the ROC analyses, serum TIMP-1 levels on days 1, 4 and 8 of MMCAI could be used for 30-day mortality prediction of those patients, being this is another novel finding of our study. Patients with serum TIMP-1 levels higher than 299 ng/mL on day 1 of MMCAI, higher than 274 ng/mL on day 4 or higher than 298 ng/mL on day 8 have higher risk of death during the first 30 days than patients with lower levels.
We believe that those high TIMP-1 levels during the first week of cerebral infarction that we found in non-surviving compared to surviving patients do not contribute to the death of patients. We think that those high TIMP-1 levels in non-surviving patients could be due to the attempt to maintain the balance between the activity of MMPs and TIMPs.
We recognized the limitations of our study such as that we did not report data about others MMPs and TIMPs. In addition, we have determined serum MMP-9 levels by ELISA that detects the active form and latent pro-form; however, we have not determined the active form by gelatin zymography [36]. Besides, we determined serum TIMP-1 levels at days 1, 4, and 8 of MMCAI; however, it could have been interesting the determination of those levels at other moments of evolution as well. In addition, we have not registered all treatment for each patient; however, we did not find significant differences between surviving and non-surviving patients in thrombolysis and decompressive craniectomy.
In rat models of ischemic stroke the administration of MMP activity modulators showed beneficial effects such as to reduce blood-brain barrier leakage, infarct volume, neurological impaired and death rate [37–45].
We think that the findings of our study about the potential use of serum TIMP-1 levels during the first week of cerebral infarction for 30-day mortality prediction of those patients, and the finding in animal studies about the potential benefits of MMP activity modulators could motivate the research about the role of serum TIMP-1 levels for the mortality prediction and the MMP modulation to reduce death risk of these patients.
Conclusions
The new findings of our study were that non-surviving MMCAI patients showed higher serum TIMP-1 levels during the first week of MMCAI that surviving patients, and that those levels during the first week of MMCAI could be used as mortality biomarkers.
Abbreviations
- APACHE II
Acute Physiology and Chronic Health Evaluation
- aPTT
Activated partial thromboplastin time
- FIO2
Pressure of arterial oxygen/fraction inspired oxygen
- GCS
Glasgow Coma Scale
- INR
International normalized ratio
- MMP
Matrix metalloproteinases
- PaO2
Pressure of arterial oxygen/fraction inspired oxygen
- TIMP
Tissue inhibitor of matrix metalloproteinases
Authors’ contributions
LL conceived, designed and coordinated the study, participated in acquisition and interpretation of data, and drafted the manuscript.MMM, LR, MA, JJC, JSV, JMBL, AFGR participated in acquisition of data. JO, JAR and JAP participated in blood determination levels. AJ participated in the interpretation of data. All authors revised the manuscript critically for important intellectual content, made the final approval of the version to be published, and were agree to be accountable for all aspects of the work.
Funding
This study was supported by a grant (OA18/011) from Fundación DISA a la Investigación Médica 2017 (Santa Cruz de Tenerife. Spain). Funding did not influence in the study design, the collection, analysis, and interpretation of data, the manuscript writing, and the decision to submit it for publication.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the local ethics committees of the 6 hospitals participating in the study: H. Insular in Las Palmas de Gran Canaria, H. General de La Palma in La Palma, H. Universitario de Canarias in La Laguna, H. Clínico Universitario de Valencia in Valencia, H. Universitario Nuestra Señora de Candelaria in Santa Cruz de Tenerife, and H. Universitario Dr. Negrín in Las Palmas de Gran Canaria. Legal guardians of the patients signed informed consent to participate in the study. The study adheres to the World Medical Association Declaration of Helsinki regarding ethical conduct of research involving human subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Leonardo Lorente, Email: lorentemartin@msn.com.
María M. Martín, Email: mar.martinvelasco@gmail.com
Luis Ramos, Email: lramosgomez@gmail.com.
Mónica Argueso, Email: moni_begasa@hotmail.com.
Juan J. Cáceres, Email: jcacagr@gobiernodecanarias.org
Jordi Solé-Violán, Email: jcacagr@gobiernodecanarias.org.
Alejandro Jiménez, Email: ajimenezsosa@gmail.com.
Juan M. Borreguero-León, Email: jmborreguero@hotmail.com
Agustín F. González-Rivero, Email: agonriv@hotmail.com
Josune Orbe, Email: Spainjosuneor@unav.es.
José A. Rodríguez, Email: josean@unav.es
José A. Páramo, Email: japaramo@unav.es
References
- 1.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL, American Heart Association Stroke Council 2018 guidelines for the early Management of Patients with Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–e110. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 2.Brinckerhoff CE, Matrisian LM. Matrix metalloproteinases: a tail of a frog that became a prince. Nat Rev Mol Cell Biol. 2002;3:207–214. doi: 10.1038/nrm763. [DOI] [PubMed] [Google Scholar]
- 3.Birkedal-Hansen H, Moore WG, Bodden MK, Windsor LJ, Birkedal-Hansen B, DeCarlo A, Engler JA. Matrix metalloproteinases: a review. Crit Rev Oral Biol Med. 1993;4:197–250. doi: 10.1177/10454411930040020401. [DOI] [PubMed] [Google Scholar]
- 4.Candelario-Jalil E, Yang Y, Rosenberg GA. Diverse roles of matrix metalloproteinases and tissue inhibitors of metalloproteinases in neuroinflammation and cerebral ischemia. Neuroscience. 2009;158:983–994. doi: 10.1016/j.neuroscience.2008.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morancho A, Rosell A, García-Bonilla L, Montaner J. Metalloproteinase and stroke infarct size: role for anti-inflammatory treatment? Ann N Y Acad Sci. 2010;1207:123–133. doi: 10.1111/j.1749-6632.2010.05734.x. [DOI] [PubMed] [Google Scholar]
- 6.Ramos-Fernandez M, Bellolio MF, Stead LG. Matrix metalloproteinase-9 as a marker for acute ischemic stroke: a systematic review. J Stroke Cerebrovasc Dis. 2011;20:47–54. doi: 10.1016/j.jstrokecerebrovasdis.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Horstmann S, Kalb P, Koziol J, Gardner H, Wagner S. Profiles of matrix metalloproteinases, their inhibitors, and laminin in stroke patients: influence of different therapies. Stroke. 2003;34:2165–2170. doi: 10.1161/01.STR.0000088062.86084.F2. [DOI] [PubMed] [Google Scholar]
- 8.Lucivero V, Prontera M, Mezzapesa DM, Petruzzellis M, Sancilio M, Tinelli A, Di Noia D, Ruggieri M, Federico F. Different roles of matrix metalloproteinases-2 and -9 after human ischaemic stroke. Neurol Sci. 2007;28:165–170. doi: 10.1007/s10072-007-0814-0. [DOI] [PubMed] [Google Scholar]
- 9.Heo JH, Kim YS, Lee KY, Kim EH, Chu CK, Nam JM. Increase in plasma matrix metalloproteinase-9 in acute stroke patients with thrombolysis failure. Stroke. 2003;34:e48–e50. doi: 10.1161/01.STR.0000073788.81170.1C. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds MA, Kirchik HJ, Dahlen JR, Anderberg JM, McPherson PH, Nakamura KK, Laskowitz DT, Valkirs GE, Buechler KF. Early biomarkers of stroke. Clin Chem. 2003;49:1733–1739. doi: 10.1373/49.10.1733. [DOI] [PubMed] [Google Scholar]
- 11.Lynch JR, Blessing R, White WD, Grocott HP, Newman MF, Laskowitz DT. Novel diagnostic test for acute stroke. Stroke. 2004;35:57–63. doi: 10.1161/01.STR.0000105927.62344.4C. [DOI] [PubMed] [Google Scholar]
- 12.Kim YS, Lee KY, Koh SH, Park CY, Kim HY, Lee YJ, Kim HT, Kim J, Kim MH, Kim KS, Chang DI, Kim SH. The role of matrix metalloproteinase 9 in early neurological worsening of acute lacunar infarction. Eur Neurol. 2006;55:11–15. doi: 10.1159/000091137. [DOI] [PubMed] [Google Scholar]
- 13.Montaner J, Alvarez-Sabín J, Molina C, Anglés A, Abilleira S, Arenillas J, González MA, Monasterio J. Matrix metalloproteinase expression after human cardioembolic stroke: temporal profile and relation to neurological impairment. Stroke. 2001;32:1759–1766. doi: 10.1161/01.STR.32.8.1759. [DOI] [PubMed] [Google Scholar]
- 14.Koh SH, Park CY, Kim MK, Lee KY, Kim J, Chang DI, Kim HT, Kim SH. Microbleeds and free active MMP-9 are independent risk factors for neurological deterioration in acute lacunar stroke. Eur J Neurol. 2011;18:158–164. doi: 10.1111/j.1468-1331.2010.03100.x. [DOI] [PubMed] [Google Scholar]
- 15.Barr TL, Latour LL, Lee KY, Schaewe TJ, Luby M, Chang GS, El-Zammar Z, Alam S, Hallenbeck JM, Kidwell CS, Warach S. Blood-brain barrier disruption in humans is independently associated with increased matrix metalloproteinase-9. Stroke. 2010;41:e123–e128. doi: 10.1161/STROKEAHA.109.570515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodríguez JA, Sobrino T, Orbe J, Purroy A, Martínez-Vila E, Castillo J, Páramo JA. proMetalloproteinase-10 is associated with brain damage and clinical outcome in acute ischemic stroke. J Thromb Haemost. 2013;11:1464–1473. doi: 10.1111/jth.12312. [DOI] [PubMed] [Google Scholar]
- 17.Bogoslovsky T, Spatz M, Chaudhry A, Maric D, Luby M, Frank J, Warach S. Circulating CD133+CD34+ progenitor cells inversely correlate with soluble ICAM-1 in early ischemic stroke patients. J Transl Med. 2011;9:145. doi: 10.1186/1479-5876-9-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sapojnikova N, Kartvelishvili T, Asatiani N, Zinkevich V, Kalandadze I, Gugutsidze D, Shakarishvili R, Tsiskaridze A. Correlation between MMP-9 and extracellular cytokine HMGB1 in prediction of human ischemic stroke outcome. Biochim Biophys Acta. 1842;2014:1379–1384. doi: 10.1016/j.bbadis.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 19.Abdelnaseer MM, Elfauomy NM, Esmail EH, Kamal MM, Elsawy EH. Matrix Metalloproteinase-9 and recovery of acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26:733–740. doi: 10.1016/j.jstrokecerebrovasdis.2016.09.043. [DOI] [PubMed] [Google Scholar]
- 20.Kicherova OA, Reikhert LI, Skorikova VG, Semeshko SA. Prognostic biochemical markers of thrombolytic therapy in ischemic stroke. Zh Nevrol Psikhiatr Im S S Korsakova. 2016;116(8 Pt 2):48–51. doi: 10.17116/jnevro20161168248-51. [DOI] [PubMed] [Google Scholar]
- 21.Ning M, Furie KL, Koroshetz WJ, Lee H, Barron M, Lederer M, Wang X, Zhu M, Sorensen AG, Lo EH, Kelly PJ. Association between tPA therapy and raised early matrix metalloproteinase-9 in acute stroke. Neurology. 2006;66:1550–1555. doi: 10.1212/01.wnl.0000216133.98416.b4. [DOI] [PubMed] [Google Scholar]
- 22.Inzitari D, Giusti B, Nencini P, Gori AM, Nesi M, Palumbo V, Piccardi B, Armillis A, Pracucci G, Bono G, Bovi P, Consoli D, Guidotti M, Nucera A, Massaro F, Micieli G, Orlandi G, Perini F, Tassi R, Tola MR, Sessa M, Toni D, Abbate R, MAGIC Study Group MMP9 variation after thrombolysis is associated with hemorrhagic transformation of lesion and death. Stroke. 2013;44:2901–2903. doi: 10.1161/STROKEAHA.113.002274. [DOI] [PubMed] [Google Scholar]
- 23.Castellanos M, Leira R, Serena J, Pumar JM, Lizasoin I, Castillo J, Davalos A. Plasma metalloproteinase-9 concentration predicts hemorrhagic transformation in acute ischemic stroke. Stroke. 2003;34:40–46. doi: 10.1161/01.STR.0000046764.57344.31. [DOI] [PubMed] [Google Scholar]
- 24.Worthmann H, Tryc AB, Goldbecker A, Ma YT, Tountopoulou A, Hahn A, Dengler R, Lichtinghagen R, Weissenborn K. The temporal profile of inflammatory markers and mediators in blood after acute ischemic stroke differs depending on stroke outcome. Cerebrovasc Dis. 2010;30:85–92. doi: 10.1159/000314624. [DOI] [PubMed] [Google Scholar]
- 25.Rosell A, Alvarez-Sabín J, Arenillas JF, Rovira A, Delgado P, Fernández-Cadenas I, Penalba A, Molina CA, Montaner J. A matrix metalloproteinase protein array reveals a strong relation between MMP-9 and MMP-13 with diffusion-weighted image lesion increase in human stroke. Stroke. 2005;36(7):1415–1420. doi: 10.1161/01.STR.0000170641.01047.cc. [DOI] [PubMed] [Google Scholar]
- 26.Lorente L, Martín MM, Ramos L, Cáceres JJ, Solé-Violán J, Argueso M, Jiménez A, Borreguero-León JM, Orbe J, Rodríguez JA, Páramo JA. Serum tissue inhibitor of matrix metalloproteinase-1 levels are associated with mortality in patients with malignant middle cerebral artery infarction. BMC Neurol. 2015;15:111. doi: 10.1186/s12883-015-0364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teasdale G, Jennett B. Assessement of coma and impaired conciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 28.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Cuadrado E, Rosell A, Penalba A, Slevin M, Alvarez-Sabín J, Ortega-Aznar A, Montaner J. Vascular MMP-9/TIMP-2 and neuronal MMP-10 up-regulation in human brain after stroke: a combined laser microdissection and protein array study. J Proteome Res. 2009;8:3191–3197. doi: 10.1021/pr801012x. [DOI] [PubMed] [Google Scholar]
- 30.Kouwenhoven M, Carlström C, Ozenci V, Link H. Matrix metalloproteinase and cytokine profiles in monocytes over the course of stroke. J Clin Immunol. 2001;21:365–375. doi: 10.1023/A:1012244820709. [DOI] [PubMed] [Google Scholar]
- 31.Chen S, Martens-Lobenhoffer J, Weissenborn K, Kielstein JT, Lichtinghagen R, Deb M, Li N, Tryc AB, Goldbecker A, Dong Q, Bode-Böger SM, Worthmann H. Association of dimethylarginines and mediators of inflammation after acute ischemic stroke. J Neuroinflammation. 2012;9:251. doi: 10.1186/1742-2094-9-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jaroslav P, Christian R, Stefan O, Alexander Z, Zepper P, Holger P, Hans-Henning E. Evaluation of serum biomarkers for patients at increased risk of stroke. Int J Vasc Med. 2012;2012:906954. doi: 10.1155/2012/906954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pelisek J, Rudelius M, Zepper P, Poppert H, Reeps C, Schuster T, Eckstein HH. Multiple biological predictors for vulnerable carotid lesions. Cerebrovasc Dis. 2009;28:601–610. doi: 10.1159/000247605. [DOI] [PubMed] [Google Scholar]
- 34.Park SY, Kim MH, Kang SY, Suh JT, Lee WI. Inflammatory marker expression and its implication in Korean ischemic stroke patients. Korean J Lab Med. 2007;27:197–204. doi: 10.3343/kjlm.2007.27.3.197. [DOI] [PubMed] [Google Scholar]
- 35.Lorenzl S, De Pasquale G, Segal AZ, Beal MF. Dysregulation of the levels of matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases in the early phase of cerebral ischemia. Stroke. 2003;34:e37–e38. doi: 10.1161/01.STR.0000075563.45920.24. [DOI] [PubMed] [Google Scholar]
- 36.Remacle AG, Noël A, Duggan C, McDermott E, O'Higgins N, et al. Assay of matrix metalloproteinases types 1, 2, 3 and 9 in breast cancer. Br J Cancer. 1998;77:926–931. doi: 10.1038/bjc.1998.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Z, Xue Y, Jiao H, Liu Y, Wang P. Doxycycline-mediated protective effect against focal cerebral ischemia-reperfusion injury through the modulation of tight junctions and PKCδ signaling in rats. J Mol Neurosci. 2012;47:89–100. doi: 10.1007/s12031-011-9689-x. [DOI] [PubMed] [Google Scholar]
- 38.Leonardo CC, Eakin AK, Ajmo JM, Collier LA, Pennypacker KR, Strongin AY, Gottschall PE. Delayed administration of a matrix metalloproteinase inhibitor limits progressive brain injury after hypoxia-ischemia in the neonatal rat. J Neuroinflammation. 2008;5:34. doi: 10.1186/1742-2094-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yrjänheikki J, Keinänen R, Pellikka M, Hökfelt T, Koistinaho J. Tetracyclines inhibit microglial activation and are neuroprotective in global brain ischemia. Proc Natl Acad Sci U S A. 1998;95:15769–15774. doi: 10.1073/pnas.95.26.15769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cai Z, Lin S, Fan LW, Pang Y, Rhodes PG. Minocycline alleviates hypoxic-ischemic injury to developing oligodendrocytes in the neonatal rat brain. Neuroscience. 2006;137:425–435. doi: 10.1016/j.neuroscience.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 41.Fan LW, Lin S, Pang Y, Rhodes PG, Cai Z. Minocycline attenuates hypoxia-ischemia-induced neurological dysfunction and brain injury in the juvenile rat. Eur J Neurosci. 2006;24:341–350. doi: 10.1111/j.1460-9568.2006.04918.x. [DOI] [PubMed] [Google Scholar]
- 42.Machado LS, Kozak A, Ergul A, Hess DC, Borlongan CV, Fagan SC. Delayed minocycline inhibits ischemia-activated matrix metalloproteinases 2 and 9 after experimental stroke. BMC Neurosci. 2006;7:56. doi: 10.1186/1471-2202-7-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Asahi M, Asahi K, Jung JC, del Zoppo GJ, Fini ME, Lo EH. Role for matrix metalloproteinase 9 after focal cerebral ischemia: effects of gene knockout andenzyme inhibition with BB-94. J Cereb Blood Flow Metab. 2000;20:1681–1689. doi: 10.1097/00004647-200012000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Jiang X, Namura S, Nagata I. Matrix metalloproteinase inhibitor KB-R7785 attenuates brain damage resulting from permanent focal cerebral ischemia in mice. Neurosci Lett. 2001;305:41–44. doi: 10.1016/S0304-3940(01)01800-6. [DOI] [PubMed] [Google Scholar]
- 45.Rosenberg GA, Estrada EY, Dencoff JE. Matrix metalloproteinases and TIMPs are associated with blood-brain barrier opening after reperfusion in rat brain. Stroke. 1998;29:2189–2195. doi: 10.1161/01.STR.29.10.2189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.