Abstract
Increasing evidence indicates that immunoglobulins are important for the regulation of various cancers including prostate cancer (PCa). However, the underlying mechanisms of IgG regulated PCa development remain to be further explored. Here, we demonstrated that IgG1 heavy chain (IGHG1) was increased in tissues from PCa patients. Inhibition of IGHG1 by antibody blocking or genetic knockdown suppressed cell growth and induced cell cycle arrest and ultimate apoptosis. Expression levels of c-Myc were positively correlated with the levels of IGHG1. Furthermore, MEK/ERK/c-Myc pathway lied downstream of IGHG1 in cultured prostate cancer cells. Inhibition of IGHG1 restrained the tumor growth in nude mice and inactivated MEK/ERK/c-Myc pathway both in vitro and in vivo. These findings suggest that IGHG1 play a crucial role during the development of prostate cancer and inhibition of IGHG1 may be a potential therapy in the treatment of PCa.
1. Introduction
Prostate cancer (PCa), the second leading cause of cancer-related death of man, is one of the most common cancers of urinary system [1]. Same as other cancers, metastasis induces the morbidity and mortality of PCa patients [2, 3]. Hormone therapy is one the most common treatments of PCa. Restricted androgen level shrinks cancer volume and delays the development of tumors. However, hormone therapy only results in a medium survival time of around 12 months in patients with metastatic PCa [4]. Thus, further elucidation of PCa development of molecular mechanisms and exploration of new therapeutic targets and reliable biomarkers for detection of metastatic potential are of specific importance.
It is commonly known that immunoglobulins (IgG) are produced only by B lymphocytes and plasma cells; however, many nonlymphoid cells are reported to produce IgG, especially in cancer cells, such as breast cancer cells [5–7], colorectal cancer cells [8, 9], papillary thyroid cancer cells [10], and prostate cancer cells [11, 12]. IgG secreted by human cancers is reported to promote cancer cell proliferation in vitro [5]. IgG expressed in a variety of neoplasms shows correlation with proliferation markers and tumor grades [5]. Moreover, genetic knockdown of IgG by siRNA approaches inhibits cancer cell proliferation in vitro and in vivo [13]. The role of IgG in prostate cancer remains obscure. Our previous reports showed that IgG1 heavy chain (IGHG1) was expressed in LNCaP and PC3 prostate cancer cell lines, and inhibition of IGHG1 suppressed cell viability of PCa cells. However, the regulatory mechanisms of IGHG1 regulated PCa development remain to be further explored.
In this study, we further determined the effect of IGHG1 and investigated the cellular mechanism of IGHG1 in prostate cancer. We found that IGHG1 was upregulated in clinical prostate cancer tissue from PCa patients and downregulation of IGHG1 reduced the growth and proliferation of PCa cells. Further, the expressions of IGHG1 and c-Myc were positively correlated in PCa samples. Inhibition of IGHG1 suppressed the activation of MEK/ERK/c-Myc pathway in vitro and in vivo.
2. Methods and Materials
2.1. Ethics Statement
All human experiments were approved by the Jinan University and in accordance with the Declaration of Helsinki. Informed consent was received from all participating subjects prior to the study. 164 cases of human tissue samples of prostate cancer and 55 cases of benign prostatic hyperplasia were obtained from patients in the First Affiliated Hospital of Jinan University, from June 2010 to June 2014. All animal procedures followed the humane care guidelines of the Chinese National Institute of Health, and the protocols were approved by the Committee on Animal Research of Jinan University.
2.2. Cell Culture
Cell lines human prostate cancer DU145 and PC3 were from the First Affiliated Hospital of Jinan University. Cells were maintained in medium RPMI 1640 (HyClone, Logan, UT, USA) supplemented with 10% fetal bovine serum (FBS, Sigma-Aldrich-Chemie, Steinheim, Germany), penicillin (Sigma, 100 U/ml), and streptomycin (Sigma, 100 μg/ml) at 37°C in a humidified atmosphere with 5% CO2, as previously reported [12].
2.3. siRNA and Transfection
siRNA experiments were performed as previously reported [12]. Briefly, when cells reached 40% confluence, the siRNA fragments were transfected by Lipofectamine RNAiMax (Invitrogen, Grand Island, NY, USA) accordingly. The transfection efficiency was determined by western blot. Scrambled siRNA sequence was used as control (si-Ctrl), comparing with experiment group (si-IGHG1).
2.4. Western Blot
Cells were lysed in sample buffer and subjected to SDS-polyacrylamide gel electrophoresis as described previously [14]. Primary antibodies against IGHG1, MEK, phosphorylated-MEK (p-MEK), ERK, phosphorylated-ERK (p-ERK), c-Myc, p21, and Cyclin D1 were obtained from Santa Cruz Biotechnology, Santa Cruz, CA, USA. GAPDH (Santa Cruz) was used as the loading control. Polyvinylidene fluoride (PVDF) membranes (Millipore, Boston, MA, USA) transferred with proteins were washed and incubated with the appropriate horseradish peroxidase-conjugated secondary antibodies (Amersham Biosciences, Uppsala, Sweden) for 1 h, and bands were detected by enhanced chemiluminescence (Amersham, Bucks, UK). Densitometric values were normalized to GAPDH levels. Values (protein/GAPDH) in control group were set to 100%.
2.5. MTS Assay
MTS assay was applied to reveal cell growth as previously reported [15], by the CellTiter 96® AQueous One Solution Cell Proliferation Assay Kit (Promega, Madison, WI, USA) accordingly. In each group, cells were cultured for 12, 24, and 48 h. At harvesting, 20 μl of CellTiter 96 AQueous One Solution reagent was added to each well in a total volume of 100 μl of medium for 3 h. Absorbance was measured at 450 nm using an ELISA plate reader. The growth rate was calculated from the absorbance, and the readings at 0 h time points in each group were set to 100%.
2.6. Flow Cytometry Assay
Annexin-V-FITC Apoptosis Detection Kit (BIPEC, USA) was used to determine apoptotic cells and PI staining was used to reveal cell cycle stage [15]. Briefly, cells were resuspended with 400 μl binding buffer, labeled with annexin-V-FITC for 15 min and with PI for another 5 min; then cells were analyzed by flow cytometry by a FACScan flow cytometer (BD Biosciences, Mountain View, CA, USA).
2.7. Xenograft Mouse Model
Six- to eight-week-old male nude mice were kept on a 12 h light-dark cycle with access to food and water ad libitum. DU145 cells transfected with siRNA fragments (si-IGHG1 or si-Ctrl) for two days were collected and nude mice were subcutaneously injected with these DU145 prostate cancer cell xenografts (1 × 106 DU145 cells). IGHG1 antibody was daily subcutaneously injected at the right axillary region of nude mice for four weeks. 30 days later, the mice were sacrificed by ketamin injection (50 mg/kg) and the xenografts were dissected out. After the measurement of tumor volume, xenografts were frozen in liquid nitrogen and stored at −80°C until further processing.
2.8. Immunohistochemistry
To analyze clinically collected samples, immunohistochemistry was performed as previously reported [15]. Briefly, paraffin sections were treated with hydrogen peroxide and later antigen retrieval was applied in a microwave in 10 mM citrate buffer. Then sections were fixed with paraformaldehyde and then permeabilized, blocked, and incubated with anti-IGHG1 and c-Myc antibodies. Immunostaining was analyzed with Super Sensitive Non-Biotin Polymer HRP Detection System according to the manufacturer's instructions (BioGenex, San Ramon, Canada).
2.9. Statistical Analysis
All experiments were repeated at least three times, and the results are presented as the mean ± SEM. Analyses of significance were performed using Student's t-tests or one-way ANOVAs, followed by Bonferroni corrections. P < 0.05 was considered statistically significant.
3. Results
3.1. Inhibition of IGHG1 Suppresses Cell Growth of Prostate Cancer
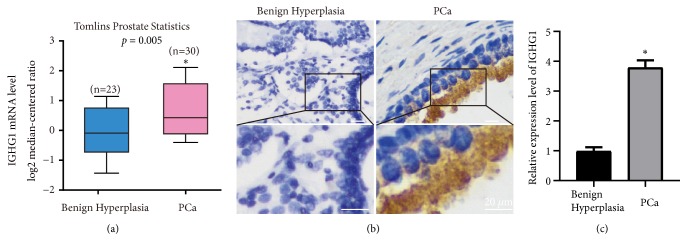
In order to further determine the role of IGHG1, we firstly searched the Oncomine database for gene expressions in prostate cancer. As shown in Figure 1(a), the mRNA levels of IGHG1 were found significantly upregulated in prostate cancer samples compared to that in benign hyperplasia samples. Furthermore, we also collected prostate cancer and benign hyperplasia tissues clinically. And by immunohistochemical approach, we found that the protein expression of IGHG1 was also upregulated (Figures 1(b) and 1(c)).
Figure 1.
The expression of IGHG1 in prostate cancer tissues. (a) Database of Oncomine reveals the upregulation of IGHG1 in prostate cancers. (b) By immunohistochemistry detection, comparing to benign prostatic hyperplasia samples, IGHG1 is highly expressed in prostate cancer tissues. Scale bar, 20 μm. (c) The statistical data of (b) were shown. ∗ donates p < 0.05.
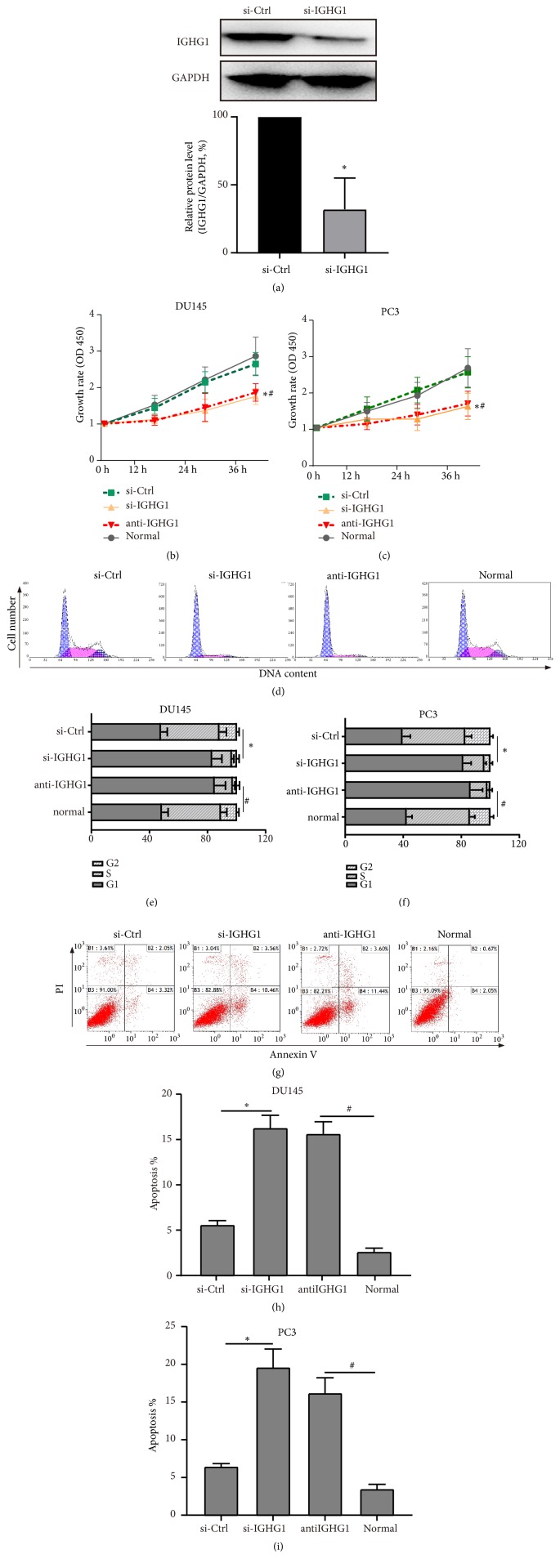
We previously designed siRNA fragments against IGHG1 and determined that genetic knockdown of IGHG1 suppressed prostate cancer cell growth [12]. Here, besides siRNA approach, we also applied IGHG1 antibody blocking to further identify the effect of IGHG1 on prostate cancer development. As shown in Figure 2(a), we determined the siRNA efficiency by western blot and found the working genetic knockdown affected the expression level of IGHG1 (si-IGHG1) in DU145 cells. By MTS assay, the cell growth rate of DU145 (Figure 3(b)) and PC3 (Figure 3(c)) cells was significantly inhibited by the transfection of siRNA fragments and by the addition of IGHG1 antibody (anti-IGHG1 group), comparing to control/normal culture groups. Furthermore, by flow cytometry with PI and Annexin-V staining, the cell cycle was arrested in si-IGHG1 and anti-IGHG1 groups (Figure 2(d)). The percentage of G1 phase was significantly upregulated under the inhibition of IGHG1 (Figures 2(e) and 2(f)). Inhibition of IGHG1 also induced cell apoptosis of prostate cancer cells (Figures 2(g)-2(h)). These data suggest that IGHG1 is important for the cell growth of prostate cancer, which is consistent with our previous results [12].
Figure 2.
Inhibition of IGHG1 suppresses the growth of PCa cells. (a) Cultured DU145 cells were transfected with IGHG1 siRNA fragment, and the siRNA efficiency was confirmed by western blot. Then the DU145 (b) and PC3 (c) cells were subjected to MTS assay to evaluate the cell growth. The data of 0 h, 12 h, 24 h, and 48 h after transfection was shown as the growth rate. And the cells were stained with PI and Annexin-V to reveal cell cycle (d) and apoptosis (g) by flow cytometry technique. The statistical data were shown in (e), (h) in DU145 cells and (f), (i) in PC3 cells. All experiments were performed in triplicate, and results are expressed as the mean ± SD. ∗ denotes p < 0.05 versus si-Ctrl group; # denotes p < 0.05 versus normal control group.
Figure 3.
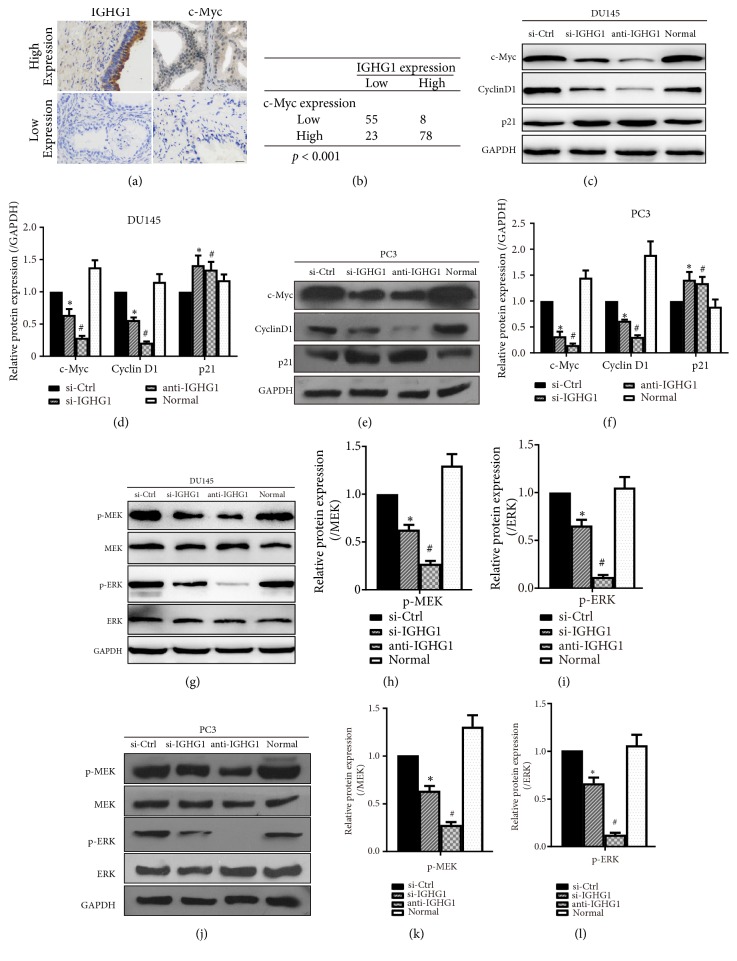
IGHG1 regulates PCa cell growth via MEK/ERK/c-Myc pathway. PCa tissue samples were subjected to immunohistochemistry; the representative images of IGHG1 and c-Myc expression were shown in (a) and the expression levels between the two proteins were shown in (b). DU145 cells (c, g) and PC3 cells (e, j) were transfected with IGHG1 siRNA fragment or si-Ctrl or with IGHG1 antibody and were subjected to western blot with c-Myc, Cyclin D1, p21, phosphor-MEK, total MEK, phosphor-ERK, and total ERK antibodies. GAPDH was used as loading control. The statistical data of expression of c-Myc, Cyclin D1, and p21 proteins (comparing to GAPDH) were shown in (d) and (f). The statistical data of p-MEK (comparing to total MEK, (h) and (k)) and p-ERK (comparing to total ERK, (i) and (l)) were shown as the mean ± SD. ∗ denotes p < 0.05 versus si-Ctrl group; # denotes p < 0.05 versus normal control group.
3.2. MEK/ERK/c-Myc Pathway Is Involved in IGHG1 Regulated PCa Cell Growth
Next, we explored the signaling pathway underlying IGHG1 regulated prostate cancer cell growth. By analyzing our immunohistochemical results from prostate cancer samples, we found that the expression of IGHG1 was positively correlated with c-Myc (Figure 3(a)). Among the 164 patients, 86 patients' samples were positive for IGHG1, whereas 78 patients' samples were negative for IGHG1. 101 patients' samples were positive for c-Myc, whereas 63 samples were negative for c-Myc (Figure 3(b)). These data suggested that IGHG1/c-Myc pathway was affected in patients with PCa. Thus, we determined whether the cell cycle proteins were involved in IGHG1 regulated PCa development. Levels of c-Myc, Cyclin D1, and p21 were evaluated by western blot, under the treatment of IGHG inhibition. The results showed that once IGHG1 was inhibited, the levels of c-Myc and Cyclin D1 were decreased, while the levels of p21 were upregulated (Figures 3(c) and 3(d) in DU145 cells; Figures 3(e) and 3(f) in PC3 cells).
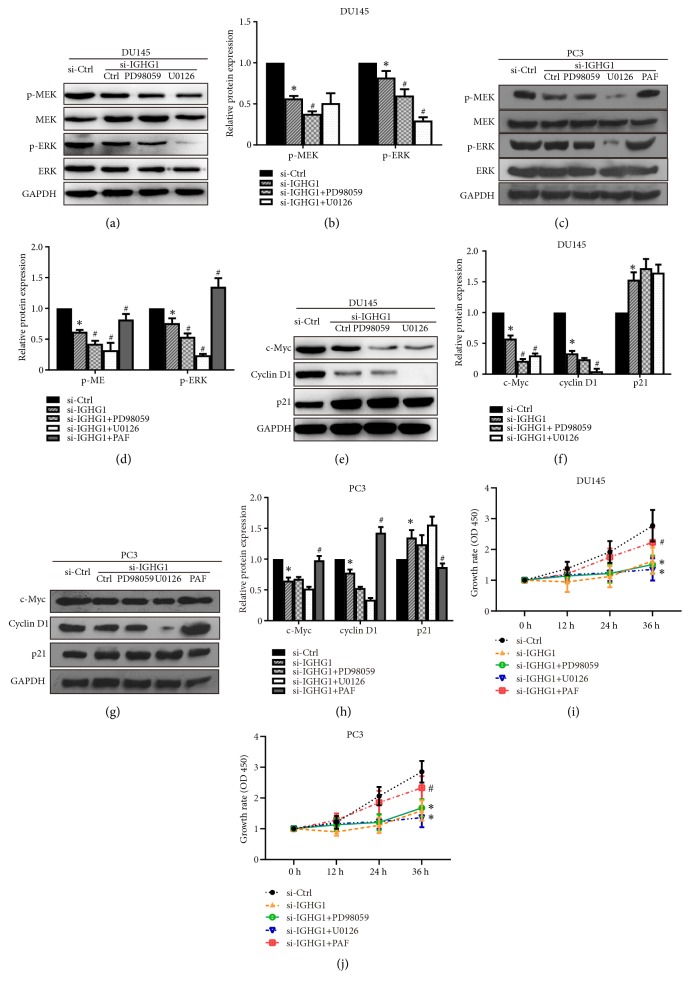
MAPKs/c-Myc axis has been reported in sustaining cancer development in many cancer types [16–18]. And the MEK/ERK/c-Myc pathway is involved in regulation of PCa cell growth [19]. Therefore, we determined the levels and activation of MEK/ERK under IGHG1 management. As shown in Figures 3(g)–3(l), the total levels of MEK and ERK remained unchanged upon the inhibition of IGHG1. However, the phosphorylation levels of MEK and ERK were significantly decreased when IGHG1 was inhibited, suggesting that the activation of MEK/ERK was inhibited. Statistical data were shown in Figures 3(h)–3(l) in both DU145 and PC3 cells. We further confirmed the data by pharmacological approaches, by using MEK/ERK inhibitors PD98059 and U0126. As shown in Figures 4(a)–4(d), inhibition of IGHG1 reduced the activation of MEK and ERK kinases and combination administration of PD98059 and U0126 further suppressed the levels of phosphorylated MEK and ERK levels. PAF(C-16) is an activator of MEK/ERK pathway, and in PC3 cells, the application of PAF(C-16) markedly reversed the inhibition effect of IGHG1 knockdown (Figures 4(c) and 4(d)). The statistical data were shown in Figures 4(b) and 4(d). Meanwhile, additional treatment with MEK/ERK inhibitors resulted in further decreased expression of c-Myc and Cyclin D1 and upregulated level of p21 (Figures 4(e)–4(h)). And activation of MEK/ERK pathway restored the levels of c-Myc and Cyclin D1 and suppressed p21 expressions (Figures 4(g) and 4(h)). Furthermore, inhibition of MER/ERK pathway was significantly suppressed while activation of that rescued the cell growth in both DU145 and PC3 cells upon IGHG1 genetic knockdown (Figures 4(i) and 4(j)). These data indicate that MEK/ERK/c-Myc pathway lies downstream of IGHG1 regulated prostate cancer cell growth.
Figure 4.
Inhibition of MEK/ERK pathway by inhibitors confers the inhibition effect of IGHG1. Cells transfected with or without IGHG1 siRNA fragments with added MEK/ERK inhibitors PD98059 and U0126 and MEK/ERK activator PAF(C-16). The cell lysates were subjected to western blot. The representative images were shown in (a), (e) in DU145 cells and (c), (g) in PC3 cells of activation of MEK and ERK and the statistical data were shown in (b), (f) in DU145 cells and (d), (h) in PC3 cells with the expression of c-Myc, Cyclin D1, and p21. The DU145 (i) and PC3 (j) cells with indicated administrations were subjected to MTS assay to evaluate the cell growth. The data of 0 h, 12 h, 24 h, and 48 h after transfection was shown as the growth rate. Data are expressed as the mean ± SD. ∗ denotes p < 0.05, compared with si-Ctrl group; # denotes p < 0.05, compared with si-IGHG1 group.
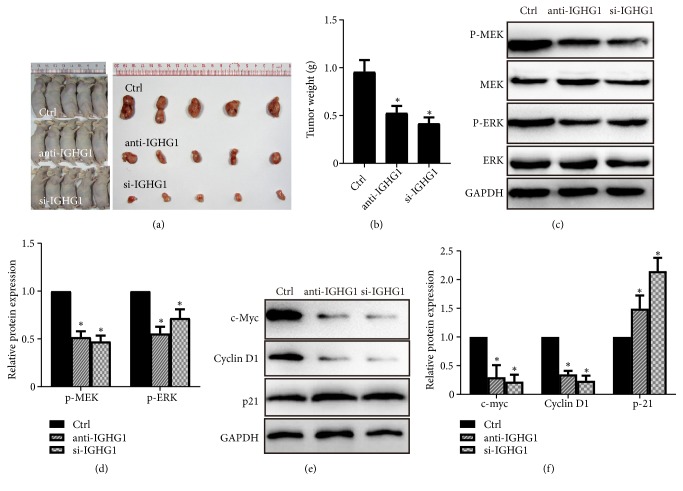
3.3. Inhibition of IGHG1 Suppresses MEK/ERK/c-Myc Pathway In Vivo
To confirm the effect of IGHG1 on prostate cancer cell growth in vivo, we performed a xenograft assay of DU145 cell in athymic nude mice. Human prostate cancer DU145 cells were inoculated into nude mice subcutaneously, and IGHG1 antibody was simultaneously injected into the mice. Afterwards, the same amount of antibody was also injected every five days. DU145 cells with IGHG1 genetically silenced were injected as another group. One month later, mice bearing tumors were sacrificed and the tumors were isolated for further analysis. As shown in Figure 5(a), tumors in IGHG1 blocked group (anti-IGHG1 group) and IGHG1 silenced group (si-IGHG1) were much smaller than those in control mice. The tumor weight was decreased as shown in Figure 5(b). By western blot analysis, the expression levels of total MEK and ERK remained unchanged. However, the phosphorylated levels of MEK and ERK were significantly reduced by IGHG1 inhibition (Figures 5(c) and 5(d)). The expression levels of c-Myc and Cyclin D1 were decreased, while that of p21 was increased (Figures 5(e) and 5(f)). These data are consistent with the scenario in vitro, indicating that inhibition of IGHG1 inhibits the tumor growth of PCa via the MEK/ERK/c-Myc pathway in vivo.
Figure 5.
IGHG1 functions via the MEK/ERK/c-Myc axis to regulate PCa tumor growth in vivo. (a) DU145 cells were injected to nude mice, together with or without IGHG1 genetic silenced or IGHG1 antibody injection. One month later, mice were sacrificed, and the tumors were isolated. (b) The tumor weight was evaluated, and the samples lysates were subjected to western blot to detect the activation of MEK/ERK pathway ((c) and (d)) and the expression of c-Myc protein ((e) and (f)). Data are expressed as the mean ± SD. ∗ denotes p < 0.05.
4. Discussion
Prostate cancer is the third leading cause of cancer-related deaths of men in China. Endocrine therapy is an advanced treatment of prostate cancer; however, this approach would result in hormonal resistance [20, 21]. Moreover, once patients develop metastasis, the mortality rate of prostate cancer is extremely high. Thus, revealing the underlying mechanisms and identifying novel targets for treatment of prostate cancer have important significance. Here, in the current study, we found that IGHG1 was significantly upregulated in prostate cancer tissues. Inhibition of IGHG1 by genetic knockdown or antibody blocking markedly reduced the growth of prostate cancer cells and induced cell cycle arrest and cell apoptosis. Furthermore, MEK/ERK pathway was inactivated when IGHG1 was suppressed. Cell cycle related proteins, such as c-Myc, Cyclin D1, and p21, lied downstream of MEK/ERK pathway to mediate IGHG1 regulated prostate cancer.
The relationship between IGHG1 and many cancers has been identified during recent years. However, the role of IGHG1 in prostate cancer and the regulatory mechanisms remain largely unknown. We have revealed the presence of cytoplasmic and membranous IGHG1 in prostate cancer cell lines (LNCaP, PC3) previously and found that inhibition of IGHG1 by siRNA approach suppressed cell proliferation and induced apoptosis [12]. Here, we further supplemented our previous work and we showed that IGHG1 was upregulated in human prostate cancer tissues, comparing with benign hyperplasia samples (Figure 1). Administration of anti-IgG antibodies had been demonstrated to inhibit the growth of tumor cells in vitro and in mouse [5, 22]. Similar results were obtained by blocking of cancer-derived IgG to inhibit cancer cell growth [23]. Thus, using antibodies to block IGHG1 is an effective way besides siRNA approach, and we found that both of these methods resulted in similar effect in vitro and in vivo.
C-Myc plays critical role in PCa onset and progression; c-Myc overexpression induces neoplastic phenotype on human prostate normal epithelial cells [24], promotes PCa carcinogenesis during early stage [25, 26], confers androgen-independent growth [27], and induces tumor relapse after radiation therapy [28]. Furthermore, MAPK signaling, which is frequently deregulated in PCa [29], has been shown to promote the c-Myc gene expression [30]. Thus, dysregulated c-Myc oncoprotein expression is critical for PCa carcinogenesis [25, 31], leading to c-Myc being identified as a strategic therapeutic target for PCa treatment [32]. Inhibition of c-Myc transcription or reducing c-Myc stability and function has consequently used to counteract c-Myc protein accumulation in many cancers including PCa. Here, in our study, we found that c-Myc was overexpressed in PCa tissue samples, and c-Myc expression was positively correlated with IGHG1. Inhibition of IGHG1 by siRNA approach or by antibody blocking induced the downregulation of c-Myc, indicating that c-Myc lies downstream of IGHG1.
A variety of signaling pathways have been reported in the development of PCa and MAPKs have been reported to be closely related with PCa [29]. Here, the role played by MEK/ERK signaling in c-Myc protein was confirmed by means of selective and specific MEK/ERK inhibitor U0126 and PD98059. Firstly, increased activation of MEK and ERK was found with increased phosphorylation in cultured PCa cell line, and inhibition of IGHG1 reduced this activation, indicating that IGHG1 functioned via MEK/ERK/c-Myc axis to regulate PCa cancer growth. Moreover, MEK/ERK inhibitors significantly reduced phosphor-active MEK and ERK and downregulated c-Myc protein in DU145 cells. The inhibitors further enhanced the inhibition effect of IGHG1 suppression. Finally, by xenograft assay in nude mice, we confirmed that the inhibition of IGHG1 induced the downregulation of phosphor-activated MEK/ERK and expression of c-Myc, leading to the suppressed PCa growth in vivo. MEK/ERK/c-Myc axis may play a role in mediating response to radiation, in vitro and in vivo [19]. And radiation therapy induces the selection of aggressive PCa cells in an ERK-dependent manner [33]. We suspect that this may be due to the upregulated c-Myc expression via MEK/ERK activation.
In conclusion, the data in the current study further confirmed the role of IGHG1 in prostate cancer development. Inhibition of IGHG1 suppresses cancer cell growth in vitro and in vivo. Furthermore, IGHG1 functions via the MEK/ERK/c-Myc pathway and regulates the downstream cell cycle related proteins. These data elucidate the mechanisms of IGHG1 regulated prostate cancer cell proliferation, providing theoretical foundation and potential target for the clinical treatment of prostate cancer.
Acknowledgments
This work was supported by the Natural Science Foundation of Guangdong Province (2017A030307037 and 2018A0303070016), Medical Scientific Research Foundation of Guangdong Province, China (B2016138), the Youth Fund Project of Research Development, and Research Fund of Zhuhai People's Hospital (201604).
Contributor Information
Weifeng Zhong, Email: zhongweifengzwf@126.com.
Bin Pan, Email: panbin@jnu.edu.cn.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
Authors' Contributions
Jing Chu, Yutong Li, and Zhihai Deng contributed equally to this study.
References
- 1.Grönberg H. Prostate cancer epidemiology. The Lancet. 2003;361(9360):859–864. doi: 10.1016/s0140-6736(03)12713-4. [DOI] [PubMed] [Google Scholar]
- 2.Foley R., Hollywood D., Lawler M. Molecular pathology of prostate cancer: The key to identifying new biomarkers of disease. Endocrine-Related Cancer. 2004;11(3):477–488. doi: 10.1677/erc.1.00699. [DOI] [PubMed] [Google Scholar]
- 3.Glinsky G. V., Glinskii A. B., Stephenson A. J., Hoffman R. M., Gerald W. L. Gene expression profiling predicts clinical outcome of prostate cancer. The Journal of Clinical Investigation. 2004;113(6):913–923. doi: 10.1172/JCI20032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Bono J. S., Oudard S., Ozguroglu M. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. The Lancet. 2010;376(9747):1147–1154. doi: 10.1016/S0140-6736(10)61389-X. [DOI] [PubMed] [Google Scholar]
- 5.Qiu X. Y., Zhu X. H., Zhang L., et al. Human epithelial cancers secrete immunoglobulin G with unidentified specificity to promote growth and survival of tumor cells. Cancer Research. 2003;63(19):6488–6495. [PubMed] [Google Scholar]
- 6.Zhang S., Mao Y., Huang J., et al. Immunoglobulin gene locus events in epithelial cells of lactating mouse mammary glands. Cellular and Molecular Life Sciences. 2010;67(6):985–994. doi: 10.1007/s00018-009-0231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donato R., Cannon B. R., Sorci G., et al. Functions of S100 proteins. Current Molecular Medicine. 2013;13(1):24–57. doi: 10.2174/156652413804486214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Z., Qiu X., Gu J. Immunoglobulin expression in non-lymphoid lineage and neoplastic cells. American Journal of Pathology. 2009;174(4):1139–1148. doi: 10.2353/ajpath.2009.080879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niu N., et al. IgG expression in human colorectal cancer and its relationship to cancer cell behaviors. PLoS One. 2012;7(11):p. e47362. doi: 10.1371/journal.pone.0047362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qiu Y., Korteweg C., Chen Z., et al. Immunoglobulin G expression and its colocalization with complement proteins in papillary thyroid cancer. Modern Pathology. 2012;25(1):36–45. doi: 10.1038/modpathol.2011.139. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y., Chen Z., Niu N., et al. IgG gene expression and its possible significance in prostate cancers. The Prostate. 2012;72(6):690–701. doi: 10.1002/pros.21476. [DOI] [PubMed] [Google Scholar]
- 12.Pan B., Zheng S., Liu C., Xu Y. Suppression of IGHG1 gene expression by siRNA leads to growth inhibition and apoptosis induction in human prostate cancer cell. Molecular Biology Reports. 2013;40(1):27–33. doi: 10.1007/s11033-012-1944-x. [DOI] [PubMed] [Google Scholar]
- 13.Li M., Zheng H., Duan Z., et al. Promotion of cell proliferation and inhibition of ADCC by cancerous immunoglobulin expressed in cancer cell lines. Cellular & Molecular Immunology. 2012;9(1):54–61. doi: 10.1038/cmi.2011.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pan B., Zhong W., Deng Z., et al. Inhibition of prostate cancer growth by solanine requires the suppression of cell cycle proteins and the activation of ROS/P38 signaling pathway. Cancer Medicine. 2016;5(11):3214–3222. doi: 10.1002/cam4.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan B., Ye Y., Liu H., et al. URG11 Regulates prostate cancer cell proliferation, migration, and invasion. BioMed Research International. 2018;2018:10. doi: 10.1155/2018/4060728.4060728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gravina G. L., Festuccia C., Popov V. M., et al. c-Myc sustains transformed phenotype and promotes radioresistance of embryonal rhabdomyosarcoma cell lines. Journal of Radiation Research. 2016;185(4):411–422. doi: 10.1667/RR14237.1. [DOI] [PubMed] [Google Scholar]
- 17.Ciccarelli C., Vulcano F., Milazzo L., et al. Key role of MEK/ERK pathway in sustaining tumorigenicity and in vitro radioresistance of embryonal rhabdomyosarcoma stem-like cell population. Molecular Cancer. 2016;15, article no. 16 doi: 10.1186/s12943-016-0501-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caforio M., Sorino C., Iacovelli S., Fanciulli M., Locatelli F., Folgiero V. Recent advances in searching c-Myc transcriptional cofactors during tumorigenesis. Journal of Experimental & Clinical Cancer Research. 2018;37(1):p. 239. doi: 10.1186/s13046-018-0912-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ciccarelli C., Di Rocco A., Gravina G. L., et al. Disruption of MEK/ERK/c-Myc signaling radiosensitizes prostate cancer cells in vitro and in vivo. Journal of Cancer Research and Clinical Oncology. 2018;144(9):1685–1699. doi: 10.1007/s00432-018-2696-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang H., Cui J., Zhang Y., Wang Z., Chong T., Wang Z. Isoflavones and Prostate Cancer. Chinese Medical Journal. 2016;129(3):341–347. doi: 10.4103/0366-6999.174488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lei J., Liu L., Wei Q., et al. Androgen-deprivation therapy alone versus combined with radiation therapy or chemotherapy for nonlocalized prostate cancer: a systematic review and meta-analysis. Asian Journal of Andrology. 2016;18(1):p. 102. doi: 10.4103/1008-682X.150840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee G., Chu R., Ting H. H. Preclinical assessment of anti-cancer drugs by using RP215 monoclonal antibody. Cancer Biology & Therapy. 2014;8(2):161–166. doi: 10.4161/cbt.8.2.7117. [DOI] [PubMed] [Google Scholar]
- 23.Zheng H., Li M., Liu H., et al. Immunoglobulin alpha heavy chain derived from human epithelial cancer cells promotes the access of S phase and growth of cancer cells. Cell Biology International. 2007;31(1):82–87. doi: 10.1016/j.cellbi.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 24.Gil J., Kerai P., Lleonart M., et al. Immortalization of primary human prostate epithelial cells by c-Myc. Cancer Research. 2005;65(6):2179–2185. doi: 10.1158/0008-5472.CAN-03-4030. [DOI] [PubMed] [Google Scholar]
- 25.Gurel B., Iwata T., Koh C. M., et al. Nuclear MYC protein overexpression is an early alteration in human prostate carcinogenesis. Modern Pathology. 2008;21(9):1156–1167. doi: 10.1038/modpathol.2008.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fleming W. H., Hamel A., Dodd J. G., et al. Expression of the c-myc protooncogene in human prostatic carcinoma and benign prostatic hyperplasia. Cancer Research. 1986;46(3):1535–1538. [PubMed] [Google Scholar]
- 27.Bernard D., Pourtier-Manzanedo A., Gil J., Beach D. H. Myc confers androgen-independent prostate cancer cell growth. The Journal of Clinical Investigation. 2003;112(11):1724–1731. doi: 10.1172/JCI19035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zafarana G., Ishkanian A. S., Malloff C. A., et al. Copy number alterations of c-MYC and PTEN are prognostic factors for relapse after prostate cancer radiotherapy. Cancer. 2012;118(16):4053–4062. doi: 10.1002/cncr.26729. [DOI] [PubMed] [Google Scholar]
- 29.Rodríguez-Berriguete G., Fraile B., Martínez-Onsurbe P., Olmedilla G., Paniagua R., Royuela M. MAP kinases and prostate cancer. Journal of signal transduction. 2012 doi: 10.1155/2012/169170.169170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murphy L. O., MacKeigan J. P., Blenis J. A network of immediate early gene products propagates subtle differences in mitogen-activated protein kinase signal amplitude and duration. Molecular and Cellular Biology. 2004;24(1):144–153. doi: 10.1128/MCB.24.1.144-153.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sears R. C. The life cycle of C-Myc: from synthesis to degradation. Cell Cycle. 2014;3(9):1133–1137. doi: 10.4161/cc.3.9.1145. [DOI] [PubMed] [Google Scholar]
- 32.Rebello R. J., et al. Therapeutic approaches targeting MYC-driven prostate cancer. Genes (Basel) 2017;8(2) doi: 10.3390/genes8020071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kyjacova L., Hubackova S., Krejcikova K., et al. Radiotherapy-induced plasticity of prostate cancer mobilizes stem-like non-adherent, Erk signaling-dependent cells. Cell Death & Differentiation. 2015;22(6):898–911. doi: 10.1038/cdd.2014.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.