In 2016, children and adolescents (1 to 19 years of age) represented a quarter of the total estimated U.S. population1; reflecting relatively good health, they accounted for less than 2% of all U.S. deaths.2 By 2016, death among children and adolescents had become a rare event. Declines in deaths from infectious disease or cancer, which had resulted from early diagnosis, vaccinations, antibiotics, and medical and surgical treatment, had given way to increases in deaths from injuryrelated causes, including motor vehicle crashes, firearm injuries, and the emerging problem of opioid overdoses. Although injury deaths have traditionally been viewed as “accidents,” injuryprevention science that evolved during the latter half of the 20th century increasingly shows that such deaths are preventable with evidence-based approaches.
In this report, we summarize the leading causes of death in children and adolescents (1 to 19 years of age) in the United States. Unless otherwise indicated, data on deaths were obtained from the Wide-ranging Online Data for Epidemiologic Research (WONDER) system of the Centers for Disease Control and Prevention (CDC), known as CDC WONDER,2 in which data are derived from U.S. death certificates compiled from 57 vital-statistics jurisdictions.2 Data are presented for 2016, the most recent year with national data available.2 Where appropriate, rates are expressed per 100,000 children and adolescents and include the 95% confidence interval.
LEADING CAUSES OF CHILD AND ADOLESCENT DEATH
BURDEN OF DISEASE
In 2016, there were 20,360 deaths among children and adolescents in the United States. More than 60% resulted from injury-related causes, which included 6 of the 10 leading causes of death (Table 1, and Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Injuries were classified according to underlying mechanism (e.g., motor vehicle crash or firearm-related injury) and intent (e.g., suicide, homicide, unintentional, or undetermined), both of which are critical to understanding risk and protective factors and to developing effective prevention strategies. When we examined all deaths among children and adolescents according to intent, unintentional injuries were the most common cause of injury-related death (57%; 7047 of 12,336 deaths), and among intentional injuries, suicide was slightly more common (21%; 2560 of 12,336) than homicide (20%; 2469 of 12,336).
Table 1.
The 10 Leading Causes of Child and Adolescent Death in the United States in 2016, in Order of Frequency.*
| Cause of Death | No. of Deaths | Rate per 100,000 (95% CI) | Percent of Deaths |
|---|---|---|---|
| All causes | 20,360 | 26.06 (25.70–26.42) | |
| All injury-related causes | 12,336 | 15.79 (15.51–16.07) | 60.6 |
| Motor vehicle crash | 4,074 | 5.21 (5.06–5.38) | 20.0 |
| Firearm-related injury | 3,143 | 4.02 (3.88–4.16) | 15.4 |
| Homicide | 1,865 | 2.39 (2.28–2.50) | |
| Suicide | 1,102 | 1.41 (1.33–1.50) | |
| Unintentional | 126 | 0.16 (0.13–0.19) | |
| Undetermined intent | 50 | 0.06 (0.05–0.09) | |
| Malignant neoplasm | 1,853 | 2.37 (2.27–2.48) | 9.1 |
| Suffocation† | 1,430 | 1.83 (1.74–1.93) | 7.0 |
| Suicide | 1,110 | 1.42 (1.34–1.51) | |
| Unintentional | 235 | 0.30 (0.26–0.34) | |
| Drowning | 995 | 1.27 (1.20–1.36) | 4.9 |
| Drug overdose or poisoning | 982 | 1.26 (1.18–1.34) | 4.8 |
| Suicide | 123 | 0.16 (0.13–0.19) | |
| Unintentional | 761 | 0.97 (0.91–1.05) | |
| Congenital anomalies | 979 | 1.25 (1.18–1.33) | 4.8 |
| Heart disease | 599 | 0.77 (0.71–0.83) | 2.9 |
| Fire or burns | 340 | 0.44 (0.39–0.48) | 1.7 |
| Unintentional | 272 | 0.35 (0.31–0.39) | |
| Chronic lower respiratory disease | 274 | 0.35 (0.31–0.40) | 1.3 |
Data were obtained from the Wide-ranging Online Data for Epidemiologic Research system of the Centers for Disease Control and Prevention,2 according to the codes of the International Classification of Diseases, 10th Revision (ICD-10),3 for the leading causes of death among children and adolescents. Age was restricted to children and adolescents 1 to 19 years of age. Cruderates (deaths per 100,000) were calculated with a population denominator of 78,134,923, with 95% confidence intervals (CIs) presented. All data are calculated for 2016, the most recent year with available data. See Table S1 in the Supplementary Appendix for more data regarding intent (homicide, suicide, unintentional, or undetermined).
Suffocation includes such incidents as suffocation or strangulation due to bed linen, the mother’s body, pillows, or plastic bags. It also includes aspiration or obstruction of the airway by a food bolus, a foreign body, or vomitus. The category also includes intentional self-harm by hanging and intentional violence by strangulation or suffocation. For a complete list of ICD codes and definitions, see Figure S3 in the Supplementary Appendix.
Motor vehicle crashes were the leading cause of death for children and adolescents, representing 20% of all deaths; firearm-related injuries were the second leading cause of death, responsible for 15% of deaths. Among firearm deaths, 59% were homicides, 35% were suicides, and 4% were unintentional injuries (e.g., accidental discharge). (The intent was undetermined in 2% of firearm deaths.) In contrast, among U.S. adults (≥20 years of age), 62% of firearm deaths were from suicide and 37% were from homicide. Furthermore, although unintentional firearm deaths were responsible for less than 2% of all U.S. firearm deaths, 26% occurred among children and adolescents.
Despite improvements in pediatric cancer care, malignant neoplasms were the third leading cause of death, representing 9% of overall deaths among children and adolescents. The fourth leading cause of death was suffocation, responsible for 7% of all deaths. Suffocation (e.g., due to bed linens, plastic bags, obstruction of the airway, hanging, or strangulation) varies with respect to intent (e.g., homicide, suicide, or unintentional). The remaining six leading causes of death represented less than 25% of the overall contribution to deaths in children and adolescents in 2016.
The leading causes of death varied between younger and older children. Among children 1 to 4 years of age, drowning was the most common cause of death, followed by congenital abnormalities and motor vehicle crashes. Children most commonly drown in swimming pools (1 to 4 years of age) and in pools, rivers, and lakes4 (≥5 years of age). Among older, school-aged children (5 to 9 years of age), death was relatively rare, representing only 12% of all deaths in children and adolescents. In this age group, malignant neoplasm was the leading cause of death, followed by motor vehicle crashes and congenital abnormalities. Unlike in children 1 to 4 years of age, drowning was only the fourth most common cause of death among those 5 to 9 years of age, which potentially reflects widespread swim training among school-aged children.5
The majority (68%) of youth who died did so during adolescence. Among these adolescent youth (10 to 19 years of age), injury deaths from motor vehicle crashes, firearms, and suffocation were the three leading causes of death; these findings reflect social and developmental factors that are associated with adolescence, including increased risk-taking behavior, differential peer and parental influence, and initiation of substance use.6
There were also differences in intent for injuryrelated causes of death between children and adolescents. Although unintentional injuries were the most common intent underlying injury deaths among children, intentional causes (i.e., homicide and suicide) were increasingly common with injury deaths during adolescence. For example, although unintentional causes comprised 26% of all firearm deaths among children (1 to 9 years of age), they represented 3% of firearm deaths among adolescents (10 to 19 years of age). Similarly, unintentional causes comprised 78% of all suffocation deaths among children, whereas they comprised 7% of suffocation deaths among adolescents.
Finally, although intentional causes of death were an increasingly important factor during adolescence, the underlying intent varied according to mechanism. For example, among adolescents, 61% of intentional firearm deaths (1733 of 2835) resulted from homicide and 98% of intentional suffocation deaths (1103 of 1128) resulted from suicide. Such variations highlight the need to implement public health strategies that are tailored according to age, underlying developmental factors, and injury-related intent.
TIME TRENDS
In 1900, the leading causes of death for the entire U.S. population were pneumonia, tuberculosis, and diarrhea or enteritis, with 40% of these deaths occurring among children younger than 5 years of age.7 In 2016, none of these diseases were among the 10 leading causes of child and adolescent death, with declines in mortality from infectious disease continuing to occur.
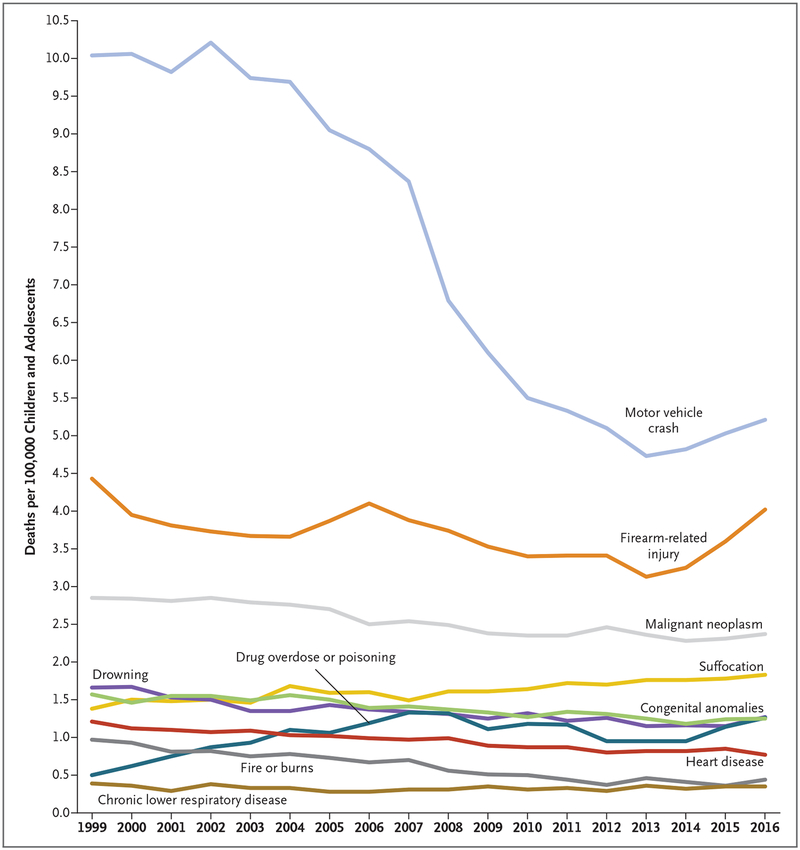
The rate of deaths from motor vehicle crashes among children and adolescents showed the most notable change over time (Fig. 1), with a relative decrease of 38% between 2007 and 2016. This has been attributed to the widespread adoption of seat belts and appropriate child safety seats, the production of cars with improved safety standards, better constructed roads, graduated driver-licensing programs,8,9 and a focus on reducing teen drinking and driving. Such reductions in mortality occurred despite increases in the overall number of U.S. vehicles and annual vehiclemiles traveled.10 Unfortunately, there was a reversal of this trend in mortality, with the rate increasing annually between 2013 and 2016. Although the cause of this reversal is not yet clear, it probably is multifactorial and includes such factors as an increase in distracted driving by teenagers11 (e.g., because of peer passengers or cell-phone use). Finally, although the effect of the changing landscape of marijuana legalization on adolescent crash risk is to date unknown, decreased risk perceptions among adolescents12 arouse concern about potential drugged driving and motor vehicle crashes, with future data needed.
Figure 1. Mortality Rates (Deaths per 100,000 Children and Adolescents) for the 10 Leading Causes of Death in the United States from 1999 to 2016.
Data were obtained from the Wide-ranging Online Data for Epidemiologic Research (WONDER) system of the Centers for Disease Control and Prevention (CDC), known as CDC WONDER,2 according to the codes of the International Classification of Diseases, 10th Revision (ICD-10),3 for the leading causes of death among children and adolescents. Age was restricted to children and adolescents 1 to 19 years of age.
Although firearm-related mortality among children and adolescents was lower in 2016 than the most recent peak mortality observed in 1993 (8.12 per 100,000; 95% confidence interval [CI], 7.91 to 8.23), rates remained stable between 2007 and 2016 without improvement, with an overall rate of 3.54 per 100,000 (95% CI, 3.50 to 3.58). Between 2013 and 2016, there was a 28% relative increase in the rate of firearm deaths. This upward trend in firearm mortality reflected increases in rates of firearm homicide (by 32%) and firearm suicide (by 26%), whereas rates of unintentional firearm deaths remained relatively stable. The nonfirearm suicide rate increased 15% while the nonfirearm homicide rate decreased 4% between 2013 and 2016. Although firearm violence in school settings makes up less than 1% of all suicides and homicides among schoolaged children and adolescents,13 a recent review noted increasing trends in school shooting incidents, with 154 between 2013 and 2015 (35, 55, and 64, respectively, per year).14
The rate of death from malignant neoplasm, the sole non–injury-related cause among the five leading causes of death, decreased 32% between 1990 and 2016, which reflects scientific advancements in cancer prevention, detection, and treatment.15 Drowning deaths declined by 46% during that time period because of public health efforts, including mandatory fencing around pools and a greater focus on pool safety (e.g., lifeguards, use of life jackets, and swimming lessons).16 Deaths due to residential fires fell nearly 73% between 1990 and 2016, in part owing to decreasing rates of smoking,17 increased installation of smoke detectors, and improved building fire codes.18,19
In contrast, drug overdoses or poisonings rose to the sixth leading cause of death among children and adolescents in 2016. This increase was largely due to an increase in opioid overdoses,20 which account for well over half of all drug overdoses among adolescents.
GLOBAL COMPARISONS
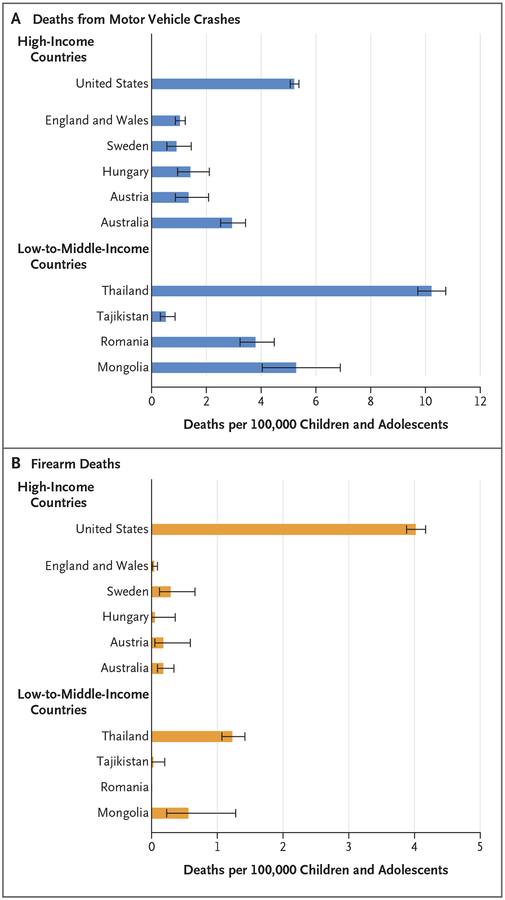
Figure 2 shows the rates of the two leading causes of child and adolescent death in the United States, as compared with rates in other high-income countries and in low-to-middle-income countries with available World Health Organization (WHO) data for 2016 (see Fig. S1 in the Supplementary Appendix for data on all countries with WHO data for 2016).21 The rate of death from motor vehicle crashes among U.S. children and adolescents was the highest observed among high-income countries; the U.S. rate was more than triple the overall rate observed in 12 other developed countries (5.21 per 100,000 [95% CI, 5.06 to 5.38] vs. 1.63 per 100,000 [95% CI, 1.49 to 1.77]). Although the U.S. rate of death from motor vehicle crashes was higher than the rates in other, similar English-speaking countries, such as Australia (2.94 per 100,000; 95% CI, 2.52 to 3.43) and England and Wales (1.04 per 100,000; 95% CI, 0.87 to 1.23), the disproportionate rate among U.S. children and adolescents was most pronounced relative to the rate in Sweden (0.91 per 100,000; 95% CI, 0.56 to 1.45), where government investment in road-traffic safety through a Vision Zero policy22 probably contributed to a rate that was approximately one sixth that in the United States.
Figure 2. Global Comparison of Mortality for the Two Leading Causes of Child and Adolescent Death in the United States in 2016.
Rates of death in countries other than the United States are from the World Health Organization (WHO) Mortality Database,21 according to ICD-10 codes3 for leading causes of death (www.who.int/healthinfo/statistics/mortality_rawdata/en/). Death counts were tabulated with the use of the same ICD-10 codes that were specified in the CDC WONDER query (Fig. S3 in the Supplementary Appendix). Population denominators that were used to calculate rates were obtained from files available on the WHO Mortality Database website for population according to country and age group, and data on the five largest high-income countries (besides the United States) and the four largest low-to-middle-income countries are presented here. In the case of Australia, 2016 population data were not available and 2015 data are presented. The error bars indicate 95% confidence intervals. See Figure S1 in the Supplementary Appendix for all countries with available 2016 data.
In contrast, rates of death from motor vehicle crashes among children and adolescents in lowto-middle-income countries were more variable, probably owing to differential levels of economic development.23 Rates of death from motor vehicle crashes are rising in developing countries despite global initiatives such as the United Nations Sustainable Development Goals,24 owing in large part to underinvestment in road infrastructure, underdeveloped public health infrastructure, limited access to emergency health care services, and a lack of widespread safety measures.25 Thus, although the rate of death from motor vehicle crashes among children and adolescents was lower in the United States than in some low-to-middle-income countries, there remains room for improvement in comparison with similar high-income countries.26
The rate of firearm deaths among children and adolescents was higher in the United States than in all other high-income countries and low to-middle-income countries with available 2016 data. The rate in the United States was 36.5 times as high as the overall rate observed in 12 other high-income countries (4.02 per 100,000 [95% CI, 3.88 to 4.16] vs. 0.11 per 100,000 [95% CI, 0.08 to 0.15]). Only 3 high-income countries (Croatia, Lithuania, and Sweden) had rates exceeding 0.20 per 100,000. Similarly, the U.S. rate was 5 times as high as the overall rate in 7 lowto-middle-income countries (0.80 per 100,000; 95% CI, 0.69 to 0.92). Although these comparisons use only 2016 data, the findings are similar to those of previous analyses that used multiple years of data.27,28
One in three U.S. homes with youth under 18 years of age has a firearm, with 43% of homes reporting that the firearm is kept unlocked and loaded, which increases the risk of firearm injuries.29 In addition to differences in availability between the United States and other countries, there is wide variability across countries in laws relating to the purchase of firearms, access to them, and safe storage.30
In contrast with rates of death from motor vehicle crashes or firearms, the rate of death from malignant neoplasm among children and adolescents in the United States (2.37 per 100,000; 95% CI, 2.27 to 2.48) was similar to the overall rate in other high-income countries (2.32 per 100,000; 95% CI, 2.16 to 2.49) (see Fig. S1 in the Supplementary Appendix for information on all countries with available 2016 data). The U.S. rate was 36% lower than the combined rate in low-to-middle-income countries (3.64 per 100,000; 95% CI, 3.41 to 3.89), which probably reflects differential environmental and genetic exposures combined with early detection and treatment from advanced diagnostics and a more developed health infrastructure in the United States.31
HEALTH DISPARITIES — RURALITY, RACE, ETHNIC GROUP, POVERTY, AND SEX
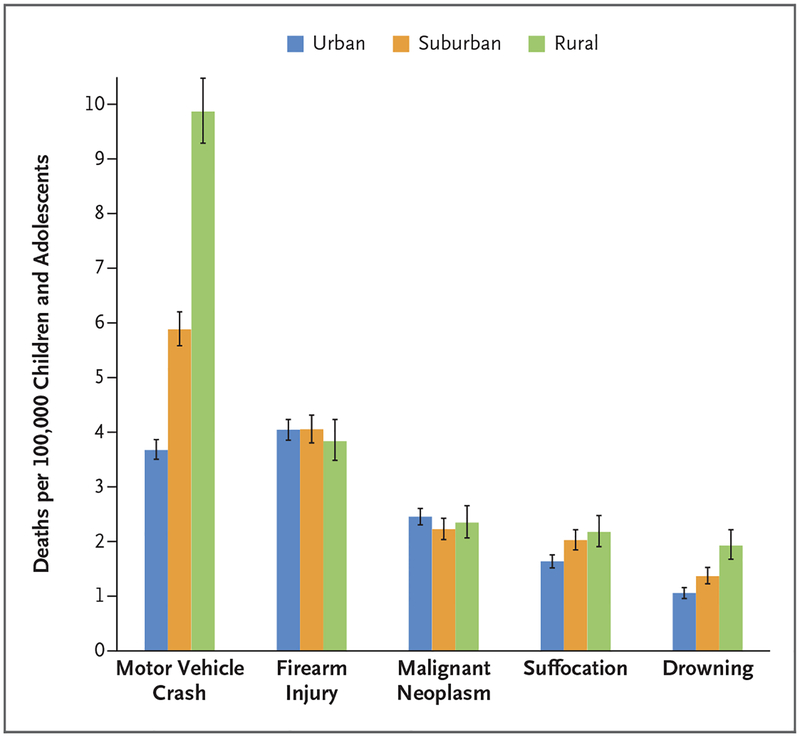
There were disparities in patterns of mortality according to rurality, race or ethnic group, and sex. Rural children and adolescents had higher mortality (33.4 per 100,000; 95% CI, 32.4 to 34.5) than those living in either suburban settings (27.5 per 100,000; 95% CI, 26.8 to 28.0) or urban settings (23.5 per 100,000; 95% CI, 23.0 to 23.9). These differences were primarily due to higher injury-related mortality in rural settings (Fig. 3, and Fig. S2 in the Supplementary Appendix), particularly with respect to motor vehicle crashes (the rate in rural settings was 2.7 times the rate in urban settings), fire or burn injuries (3.3 times), drowning (1.8 times), and suffocation (1.3 times).
Figure 3. Mortality for the Five Leading Causes of Child and Adolescent Death in 2016, According to Rurality.
Data were obtained from the CDC WONDER database,2 according to ICD-10 codes3 for the leading causes of death among children and adolescents. The 2013 National Center for Health Statistics Urban–Rural Classification Scheme for Counties was used to assign one of six categories to each county in the United States. Counties were classified as urban (Large Central Metro or Large Fringe Metro), suburban (Medium Metro or Small Metro), or rural (Micropolitan or Noncore). The I bars indicate 95% confidence intervals. See Figure S2 in the Supplementary Appendix for data on all 10 leading causes of death.
Several factors contribute to this disparity. First, sparsely populated rural settings are associated with longer emergency medical service response times, which can delay available trauma services.32,33 Second, the markedly higher rates of death from motor vehicle crashes in rural settings persist after adjustment for the differences in vehicle-miles traveled. These higher rates of death are probably due to environmental factors (e.g., long stretches of uninterrupted roads, which may lead to higher speeds, and a lack of divided roads),32,34,35 behavioral factors (e.g., less use of seat belts and child safety seats and more alcohol-impaired driving), and policy factors (e.g., lower enforcement of traffic laws).32
Deaths from residential fires were more common in rural settings than in nonrural settings, owing to older homes, the use of more dangerous heating sources, and lower rates of smoke-detector and fire-alarm availability.32,36–38 Children and adolescents died from firearm injuries at a similar rate in urban settings (4.05 per 100,000) and rural settings (3.84 per 100,000); however, the firearm homicide rate was 2.3 times as high among urban youth as among rural youth, and the firearm suicide rate was 2.1 times as high among rural youth as among urban youth. Finally, the rate of overdose death was slightly higher (1.4 times as high) among urban youth than among rural youth. This probably reflects the mixed nature of the opioid epidemic, with a greater availability of heroin in urban settings39 and the disproportionate effect of prescription opioids in rural settings.40,41
For all leading causes of death, male children and adolescents died at higher rates than their female counterparts, with the disparity widening from a ratio of 1.2 times as high among children 1 year of age to 2.8 times as high by 19 years of age. This higher rate among male children and adolescents was most pronounced for firearm deaths (5.1 times the rate among female children and adolescents), drowning deaths (2.5 times), and suffocation deaths (1.8 times). Although less pronounced, disparities between boys and girls in injury-related mortality persisted even among children 1 to 4 years of age. Such disparities probably reflect differential socialization and normative constraints that lead to higher levels of risk-taking behavior among boys.42
With regard to race or ethnic group, mortality was higher among blacks (38.2 per 100,000; 95% CI, 37.1 to 39.3) and American Indians or Alaska Natives (28.0 per 100,000; 95% CI, 25.4 to 30.9) than among whites (24.2 per 100,000; 95% CI, 23.8 to 24.6) and Asians or Pacific Islanders (15.9 per 100,000; 95% CI, 14.8 to 17.0). Disparities for black youth resulted from higher mortality for both injury-related causes (i.e., firearms, drowning, and fire or burns) and medical causes (i.e., heart disease and respiratory disease). The disparities were most pronounced for deaths related to firearms, which were the lead ing cause of death among black youth and occurred at a rate 3.7 times as high as the rate among white youth. Black youth also had higher rates of drowning deaths (1.6 times as high) and fire-related deaths (2.3 times as high) than white youth. For medical illnesses, blacks had rates of death from heart disease and chronic lower respiratory diseases (e.g., asthma) that were 2.1 and 6.3 times as high, respectively, as the rates among white youth. Such disparities probably reflect underlying socioeconomic issues, including poverty, environmental exposures, and differential access to health care services.43–45
American Indian and Alaska Native youth had the highest rates of death from motor vehicle crashes or suffocation in comparison with other races or ethnic groups; this group also had a higher rate of firearm deaths than white youth. These disparities probably reflect both the rural nature of many reservation communities and higher rates of risky driving behaviors, including drunk driving and nonuse of seat belts.46 Disproportionate rates of suicide (by suffocation and firearm) may reflect risk factors such as alcohol misuse and untreated mental health issues, in concert with poor access to medical and mental health care.46 In contrast, white youth had a rate of death due to drug overdose or poisoning that was nearly twice as high as the rates observed in other races or ethnic groups, a finding that mirrors the overdose trends among adults, which may reflect factors related to setting (e.g., a high proportion of whites in rural settings) as well as differential prescribing practices according to race.40,47
Non-Hispanic children had higher mortality across all 10 leading causes of death than Hispanic children, with the exception of malignant neoplasm, for which the rates were similar. However, CDC WONDER data may underestimate rates of death among Hispanics.2
Finally, one limitation of CDC WONDER data is the lack of inclusion of poverty variables. However, a broad literature indicates that poverty is an important risk factor for injury across ages,48 including contributing to increased risks of motor vehicle crashes49 and firearm injuries.50
REDUCING DEATHS IN CHILDHOOD AND ADOLESCENCE
Childhood and adolescent mortality remains overwhelmingly related to preventable injury-related causes of death. Progress toward further reducing deaths among children and adolescents will require a shift in public perceptions so that injury deaths are viewed not as “accidents,” but rather as social ecologic phenomena that are amenable to prevention. The sound application of rigorous scientific public health methods has resulted in considerable success in some areas of injury, notably childhood deaths due to motor vehicle crashes, drowning, and residential fires. Expanding public health approaches to encompass all the leading causes of death could substantially reduce childhood and adolescent mortality, as well as the disparities observed.
Supplementary Material
Acknowledgments
We thank Dr. Jason Goldstick for his assistance with World Health Organization and Web-based Injury Statistics Query and Reporting System data abstraction related to this manuscript, and Jessica Roche and Wendi Mohl for their assistance in the preparation of an earlier version of the manuscript.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.U.S. Census Bureau, Population Division. Estimates of the U.S. population by age and sex: April 1, 2010, to July 1, 2016 (https://www.census.gov/newsroom/press-releases/2017/cb17-tps38-population-estimates-single-year-age.html).
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed mortality file, 1999–2016, on CDC WONDER online database. 2017. (https://wonder.cdc.gov/cmf-icd10.html).
- 3.ICD10Data.com home page (http://www.icd10data.com/).
- 4.Brenner RA, Trumble AC, Smith GS, Kessler EP, Overpeck MD. Where children drown, United States, 1995. Pediatrics 2001; 108: 85–9. [DOI] [PubMed] [Google Scholar]
- 5.Brenner RA. Prevention of drowning in infants, children, and adolescents. Pediatrics 2003; 112: 440–5. [DOI] [PubMed] [Google Scholar]
- 6.Arnett JJ. Adolescent storm and stress, reconsidered. Am Psychol 1999; 54: 317–26. [DOI] [PubMed] [Google Scholar]
- 7.Control of infectious diseases. MMWR Morb Mortal Wkly Rep 1999; 48: 621–9. [PubMed] [Google Scholar]
- 8.Zakrajsek JS, Shope JT, Greenspan AI, Wang J, Bingham CR, Simons-Morton BG. Effectiveness of a brief parent-directed teen driver safety intervention (Checkpoints) delivered by driver education instructors. J Adolesc Health 2013; 53: 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simons-Morton BG, Hartos JL, Leaf WA, Preusser DF. The effect on teen driving outcomes of the Checkpoints Program in a state-wide trial. Accid Anal Prev 2006; 38: 907–12. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Transportation, Federal Highway Administration, Office of Highway Policy Information. Travel monitoring: traffic volume trends. 2018. (https://www.fhwa.dot.gov/policyinformation/travel_monitoring/tvt.cfm).
- 11.U.S. Department of Transportation, National Highway Traf fic Safety Administration. Traffic safety facts: distracted driving 2015. March 2017. (https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/documents/812_381_distracteddriving2015.pdf).
- 12.Department of Health and Human Services, Substance Abuse and Mental Health Service Administration, Center for Behavioral Health Statistics and Quality. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. Rockville, MD: Office of Applied Studies, 2014. [Google Scholar]
- 13.Musu-Gillette L, Zhang A, Wang K, et al. Indicators of school crime and safety: 2017. Washington, DC: National Center for Education Statistics, Department of Education, Department of Justice Office of Justice Programs, 2018. [Google Scholar]
- 14.Kalesan B, Lagast K, Villarreal M, Pino E, Fagan J, Galea S. School shootings during 2013–2015 in the USA. Inj Prev 2017; 23: 321–7. [DOI] [PubMed] [Google Scholar]
- 15.Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin 2014; 64: 83–103. [DOI] [PubMed] [Google Scholar]
- 16.Quan L, Liller KD, Bennett E. Water-related injuries of children and adolescents In: DeSafey Liller K, ed. Injury prevention for children and adolescents. Washington, DC: Alpha Press, 2012: 295–302. [Google Scholar]
- 17.Leistikow BN, Martin DC, Milano CE. Fire injuries, disasters, and costs from cigarettes and cigarette lights: a global overview. Prev Med 2000; 31:91–9. [DOI] [PubMed] [Google Scholar]
- 18.Warda LJ, Ballesteros MF. Interventions to prevent residential fire injury In: Doll LS, Bonzo SE, Mercy JA, Sleet DA, Haas EN, eds. Handbook of injury and violence prevention. New York: Springer, 2008: 97–115. [Google Scholar]
- 19.Miller TR, Finkelstein AE, Zaloshnja E, Hendrie D. The cost of child and adolescent injuries and the savings from prevention In: DeSafey Liller K, ed. Injury prevention for children and adolescents. Washington, DC: Alpha Press, 2012: 50. [Google Scholar]
- 20.Department Of Health and Human Services, Office of Adolescent Health. Opioids and adolescents. 2017. (https://www.hhs.gov/ash/oah/adolescent-development/substance-use/drugs/opioids/index.html).
- 21.WHO mortality database. Geneva: World Health Organization; (http://www.who.int/healthinfo/mortality_data/en/). [Google Scholar]
- 22.Johansson R Vision Zero — implementing a policy for traffic safety. Saf Sci 2009; 47: 826–31. [Google Scholar]
- 23.Kopits E, Cropper M. Traffic fatalities and economic growth. Accid Anal Prev 2005; 37: 169–78. [DOI] [PubMed] [Google Scholar]
- 24.United Nations. Transforming our world: the 2030 agenda for sustainable development — resolution adopted by the General Assembly, 2015. (https://sustainabledevelopment.un.org/post2015/transformingourworld).
- 25.Staton C, Vissoci J, Gong E, et al. Road traffic injury prevention initiatives: a systematic review and metasummary of effectiveness in low and middle income countries. PLoS One 2016; 11(1): e0144971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evans L Traffic fatality reductions: United States compared with 25 other countries. Am J Public Health 2014; 104: 1501–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med 2016; 129: 266–73. [DOI] [PubMed] [Google Scholar]
- 28.Hemenway D, Miller M. Firearm availability and homicide rates across 26 high-income countries. J Trauma 2000; 49: 985–8. [DOI] [PubMed] [Google Scholar]
- 29.Schuster MA, Franke TM, Bastian AM, Sor S, Halfon N. Firearm storage patterns in US homes with children. Am J Public Health 2000; 90: 588–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carlsen A, Chinoy S. How to buy a gun in 15 countries. New York Times. March 2, 2018. (https://www.nytimes.com/interactive/2018/03/02/world/international-gun-laws.html).
- 31.Howard SC, Metzger ML, Wilimas JA, et al. Childhood cancer epidemiology in low-income countries. Cancer 2008; 112: 461–72. [DOI] [PubMed] [Google Scholar]
- 32.Peek-Asa C, Zwerling C, Stallones L. Acute traumatic injuries in rural populations. Am J Public Health 2004; 94: 1689–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maio RF, Green PE, Becker MP, Burney RE, Compton C. Rural motor vehicle crash mortality: the role of crash severity and medical resources. Accid Anal Prev 1992; 24: 631–42. [DOI] [PubMed] [Google Scholar]
- 34.Karlaftis MG, Golias I. Effects of road geometry and traffic volumes on rural roadway accident rates. Accid Anal Prev 2002; 34: 357–65. [DOI] [PubMed] [Google Scholar]
- 35.Baker DR, Clarke SR, Brandt EN Jr. An analysis of factors associated with seat belt use: prevention opportunities for the medical community. J Okla State Med Assoc 2000; 93: 496–500. [PubMed] [Google Scholar]
- 36.The rural fire problem in the United States. Washington, DC: United States Fire Administration, Federal Emergency Management Agency, August 1997. (https://www.usfa.fema.gov/downloads/pdf/statistics/rural.pdf). [Google Scholar]
- 37.Hall JR Jr. The U.S. experience with smoke detectors: who has them? How well do they work? When don’t they work? NFPA J 1994; 88: 36–46. [PubMed] [Google Scholar]
- 38.Harvey PA, Sacks JJ, Ryan GW, Bender PF. Residential smoke alarms and fire escape plans. Public Health Rep 1998; 113: 459–64. [PMC free article] [PubMed] [Google Scholar]
- 39.Curtin SC, Tejada-Vera B, Warner M. Drug overdose deaths among adolescents aged 15–19 in the United States: 1999–2015 NCHS data brief no. 282. Atlanta: National Center for Health Statistics, 2017. [PubMed] [Google Scholar]
- 40.Havens JR, Young AM, Havens CE. Nonmedical prescription drug use in a nationally representative sample of adolescents: evidence of greater use among rural adolescents. Arch Pediatr Adolesc Med 2011; 165: 250–5. [DOI] [PubMed] [Google Scholar]
- 41.Monnat SM, Rigg KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health 2016; 32: 204–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Byrnes JP, Miller DC, Schafer WD. Gender differences in risk taking: a meta-analysis. Psychol Bull 1999; 125: 367–83. [Google Scholar]
- 43.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood determinants. J Epidemiol Community Health 2000; 54: 517–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and the occurrence of fatal and nonfatal injury in the United States. Am J Public Health 2000; 90: 70–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams DR, Wyatt R. Racial bias in health care and health: challenges and opportunities. JAMA 2015; 314: 555–6. [DOI] [PubMed] [Google Scholar]
- 46.Sarche M, Spicer P. Poverty and health disparities for American Indian and Alaska Native children: current knowledge and future prospects. Ann N Y Acad Sci 2008; 1136: 126–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ. Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015. Pediatrics 2017; 139(4): e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karb RA, Subramanian SV, Fleegler EW. County poverty concentration and disparities in unintentional injury deaths: a fourteen-year analysis of 1.6 million US fatalities. PLoS One 2016; 11(5): e0153516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mannocci A, Saulle R, Villari P, La Torre G. Male gender, age and low income are risk factors for road traffic injuries among adolescents: an umbrella review of systematic reviews and metaanalyses. J Public Health 2018. June 1 (Epub ahead of print). [Google Scholar]
- 50.Lee J, Moriarty KP, Tashjian DB, Patterson LA. Guns and states: pediatric firearm injury. J Trauma Acute Care Surg 2013; 75: 50–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.