1. Background
Cervical cancer is the fourth leading type of cancer in women worldwide (Joshi and Sankaranarayana, 2015; World Health Organization, 2015). According to Bigoni et al. (2015) cervical cancer is a major public health problem with new diagnosed cases at 530,232, and 275,008 deaths annually. It is estimated that around 270,000 women died from cervical cancer in 2012; more than 85% of these deaths occurring in low- and middle-income countries which includes Botswana (McFarland, 2009). According to McFarland (2009) cervical cancer is the most common cancer leading to mortality and mobility among women in Botswana. Ministry of Health in Botswana (2009) noted that cervical cancer incidents continue to rise each year. World Health Organization (WHO) as cited by Ramogola-Masire (2014) “predicted that morbidity and mortality due to cervical cancer will increase by more than 20 per cent by 2025 in women under the age of 65, if no change occurs in the current trends (p. 81)”. It is therefore crucial for developing countries like Botswana to take action just like the developed countries. The United Nations (2018) places Botswana as a developing country. A developing country is a low or a middle income country. Furthermore, Lim and Ojo (2017) noted that all countries in the sub Saharan African region of which Botswana is part are classified as developing countries.
The developed countries have less mortality rate of cervical cancer amongst women. This is because they have established and well organized screening programs that allow the early detection of the virus. This allows for the women to get the appropriate treatment hence preventing the development of cervical cancer. The opposite is true for Botswana where screening is opportunistic. About 90% of women presenting with cervical cancer have been observed to have never been screened for cervical cancer in their lifetime (Ramogola-Masire et al., 2012). According to Bano et al. (2007) cervical cancer screening has been observed to be an important diagnostic tool to detect pre-cancerous and cancerous lesions of the uterine cervix. It is well documented that the evolution of cervical intraepithelial lesion and the implication of persistent infection with the human papillomavirus (HPV), a common sexually transmitted infection (Pitts and Clarke, 2002; Sigurdsson and Sigvaldason, 2007) are closely related. Even though there are over 100 sub-types of HPV, only a few do cause cervical cancer. HPV sub-types 16 and 18 have been observed to account for about 70% of cervical cancers (Dodd et al., 2014; Schiffman & Solomon, 2013).
In spite of the fact that cervical cancer is the leading cause of women deaths in Botswana (McFarland, 2009; Ramogola-Masire et al., 2012) and the reported benefits of cancer screening uncertainties surrounding cervical cancer screening, very few women go for screening. Inadequate knowledge about the importance of cervical cancer screening and the negative attitude towards cervical cancer amongst women in Botswana has been identified as one of the reasons for low cervical cancer screening rates (McFarland, 2003). Similarly (71%) of women surveyed in Kenya, were not aware of what cervical cancer is. For those who had been screened 6% cited barriers for cervical cancer screening such as fear, lack of time and lack of knowledge about cervical cancer (Sudenga, Rositch, Otieno, & Smith, 2013).
Successful cervical cancer screening programs are dependent on informed target populations (Ibekwe, Hoqe & Ntuli-Ngcobo, 2010). In addition, women who had misconceptions about cervical cancer do not feel the need to go for screening (Rosser, Njoroge & Huchko, 2015). Therefore, this study is conducted to find out the norms and beliefs regarding cervical cancer screening among women in Botswana.
2. Statement of the problem
Since health care services in Botswana are offered at no cost, one would expect that all these services are fully utilized. This can only be true if all factors that can impact negatively on utilization of services are explored. This situation therefore called for the exploration of beliefs and norms of women about going for cervical cancer screening. It has been documented that norms and beliefs are important components on people’s lives and have huge implications on the overall health of human beings. It was therefore critical to explore the norms and beliefs associated with going for cervical cancer screening so as to better develop a cultural-relevant and population specific intervention that will promote going for cervical cancer screening amongst Botswana women.
3. Theoretical framework
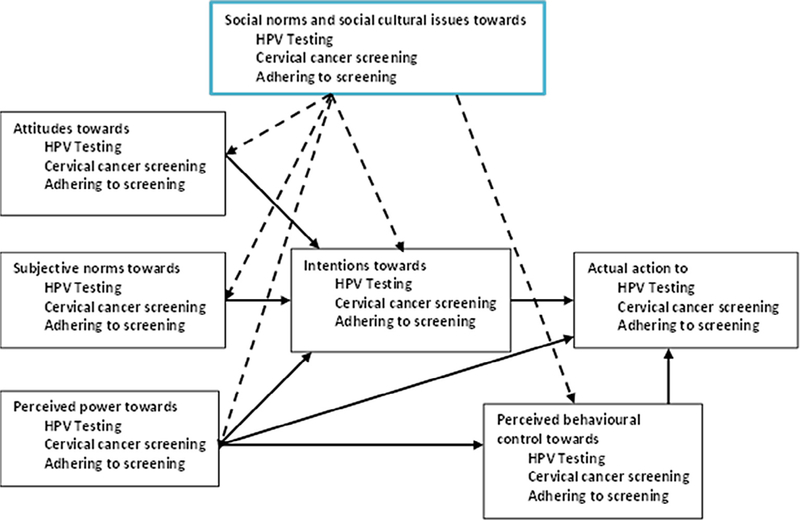
The study was guided by the theory of reasoned action (TRA) and its extension the theory of planned behavior (TPB) together with the social cognitive theory (SCT). These theories posit that human behavior can be influenced by personal attitudes, social pressure and a sense of control. According to TRA, intention is the immediate precursor of the behavior. In the TBP an individual’s perception over behavioral performance is specified as an additional predictor of behavior. The TPB, which comprises of the six construct, attitudes, behavioral intentions, subjective norms, social norms, perceived power, and perceived behavioral control provided the conceptual framework for the study which examined the norms and beliefs related to testing for HPV and cervical cancer screening amongst women aged 25–49 in Botswana. The theories guided the researchers’ in the development of the questions asked in the focus group discussion. The Social Cognitive Theory of Bandura (SCT) guided the study on the influence of socio-cultural issues and how the dynamics and the reciprocal interaction of the individual with the environment and behavior relate. The theory’s main feature was on social influence and its emphasis on external and internal social support and how it influences whether one will engage in a specific behavior and the reasons why a person engages in that behavior. These theories were appropriate to study norms and beliefs related to going for cervical cancer screening because they allowed for understanding of the cultural perspectives affecting the behavior (see Fig. 1).
Fig. 1.
Conceptual framework as drawn from the study theory.
4. Purpose
The major aim of this elicitation study was to identify saline beliefs and characteristic among Botswana women going for cervical cancer screening. The specific aims were:
to explore the norms and beliefs that influence cervical cancer screening amongst women in Botswana aged 25–49 years
to describe the attitudes, behavioral intentions, subjective norms, social norms, perceived power, and perceived behavioral control about cervical cancer screening amongst women aged 25–49 years in Botswana.
5. Significance of the study
The study was beneficial to the health care providers to review the norms and beliefs with a view of helping women overcome the barriers. Identifying norms and beliefs that could influence cervical cancer screening for women between 25 and 49 years would therefore, influence the development of interventions to encourage women to screen while they are only still at risk of developing pre cancer lesions, before the incidence of invasive cancer picks up. Furthermore, the study also provided recommendations of culturally sensitive initiatives to improve the uptake cancer screening rates
6. Research method/design
A qualitative, descriptive and context relevant design was used. Creswell (2003) noted the need to use a wide array of research methods. Creswell (2003) denotes that qualitative approach espouses meanings, concepts definitions, metaphors, description of things and contexts, hence more descriptive in nature. This concept is also noted by Saunders, Thornhill, and Lewis (2016) who state that in such studies people should carefully elicit people’s feelings, opinions and perceptions in an unbiased manner. The study employed qualitative context relevant case study approach to obtain in-depth first-hand information from the targeted women regarding going for cervical cancer screening. Mills, Durepos, and Wiebe (2010) affirm a case study research examines that person, place, event, phenomenon, or other type of subject of analysis in order to extrapolate key themes and results that help predict future trends, illuminate previously hidden issues that can be applied to practice, and/or provide a means for understanding an important research problem with greater clarity. This study was conducted at two different sites to sort and identify the norms and beliefs that influence cervical cancer screening amongst women in Botswana aged 25–49 years. The study design also enabled the researchers to establish perceptions of women regarding going for cervical cancer screening.
7. Study setting
Most studies in the area of cervical cancer screening have been done mainly in Gaborone whilst the same health service can be found in villages around the country. As a result one purports that Gaborone is over populated with these studies and at times is not fully representative of the national audience though cosmopolitan. Two locations Moshupa village in the Ngwaketse District and Mochudi village in the Kgatleng district were selected for this pilot study. These two villages are approximately 120 km apart and as such the issue of influence would be minimized. Mochudi is approximately 50 km east of Gaborone while Moshupa is approximately 70 km west of Gaborone city. The two villages share tribal population of predominantly Bakgatla ethnic groups and are considered peri-urban areas with village attributes. The villages are also run by district councils or municipalities but have different and separate administration. The selection of these two villages was premised on the fact that the Ministry of Health has rolled out cervical cancer screening services nation-wide, therefore, essentially for both to have access to the health care services.
8. Subject recruitment
Ethical clearance was sought from Institutional Review Boards (IRB) of the University of Botswana(Ref no: UBR/RES/IRB/1647) , Ministry of Health Botswana (Ref no: HPDME: 13/18/1 vol X (6 7 9), and from the University of Pennsylvania (Protocol No: 825673). Following approval of the IRB’s, a purposive sample selection procedure was used to identify the participants. First, the research team met with the gate-keepers to inform them of the aims and objectives of the study and then requested for their corporation and assistance in ensuring that the relevant targeted participants are reached. The research team contacted the headmen in different wards of identified research areas to assist in identifying participants to be enrolled. As village gatekeepers they had access to community activities such as drought relief programmes and self-reliance programmes (Ipelegeng), where researchers were able to access community women. The clinics through the District Management Health Team (DMHT) were consulted as some participants were sought from the health services (Clinics). Once the permission was sought from the relevant authorities and gatekeepers, the research team spoke to the leaders of the groups who further allowed them to access the women on site. A deliberate decision was made to select only women who were by originated from the research sites. Eligibility criteria as per the WHO (2013) included females between 25 and 49 years of age in Botswana. The WHO (2013) encourages persons between 25 and 49 years to screen as this is the cohort with a high level of cervical cancer. However, beyond the age of 49 years, women still have access to screening in Botswana. In the selection of the participants and the study sites, a deliberate choice was made to identify two research sites in peri-urban rural type villages not more than 75 km from the main capital city to ensure that follow-up if need be are not compromised.
8.1. Trustworthiness, credibility and dependability of the study
According to Carlson (2010) trustworthiness refers to the extent of which the data reflect what the researcher endeavors to measure. Trustworthiness was achieved by paying attention to credibility, transferability, dependability and confirmability.
In this study, the interview guide was first moderated by the two mentors one from the University of Botswana and one from the University of Pennsylvania in the United States of America. The mentors checked for relevance, on behavioral beliefs, normative beliefs and control beliefs. These mentors have conducted a number of behavioral studies in South Africa, Botswana, and the United States of America.
After they have evaluated the questions, the researchers piloted the instruments in one of the villages in the Southern district of Botswana having similar features to the villages were the study was conducted. Responses and comments from the pilot study were then incorporated in the final interview guide. The use of multiple sources of data through individual interviews and focus group data were triangulated as a measure to assure credibility of the information collected. The designed interview guide which had standardized similar items for both the individual and focus group interviews was in both Setswana and English languages versions. Further to this the development of the instrument was informed by Theory of Reasoned Action, Theory of Planned Behaviour, and Social Cognitive Theory. The use of appropriate languages and based on a acceptable theoretical framework facilitated for dependability of the data collected as the participants were able to express themselves freely in the language that they were most familiar with within clear delineated study variables. The purposive sampling method approach also contributed to dependability of the data collected from the participants.
The study participants consented for the individual interviews and focus group discussion to be recorded using the tape recorder and note pads. This information was checked among the group where there was need for clarification. The use of this process and content analysis provided for the confirmability of the data collected.
The study eligibility criteria drew participants from two villages that shared tribal population of predominantly Bakgatla ethnic groups and are considered peri-urban areas with village attributes. These populations which are the central government administration receive public health services provided by the Ministry of Health and Wellness. The homogeneous characteristic ensures the transferability of the research methodology and lesson learnt to similar communities.
9. Participants
The target aged group for this project was women aged 25–49 as recommended by WHO (2013). The participants were supposed to be Bakgatla residing in Moshupa or Mochudi villages. Twenty-nine women participated in the study. The participants were not supposed to be on cancer treatment.
10. Data collection instrument and methods
Focus groups discussions and individual interviews were used to elicit the women’s beliefs.
By integrating population-specific beliefs about the behaviors of interest with behavior-change theory, it was possible to develop a theoretically grounded approach that was tailored to the population. Data was collected through focus groups discussions, and individual interviews using the same semi-structured interview guide items. The focus group discussion and the individual interviews were conducted in Setswana (local/mother) language of the participants. Using the mother language allowed participants to express themselves freely and they could tell stories, proverbs and myths that are related to cervical cancer. The use of indigenous research methodologies helped the researchers to develop relationships with the researched and to use methods of inquiry consistent with local expressions of culture (e.g. stories).
The individual and focus group interviews data collection instrument consisted of the same items and sections. The instrument was divided into 4 sections: Section A which had probe items to elicit on behavioral beliefs about going for cervical cancer screening. Section B covered limiting sexual partners, while section C looked at the use of condoms during sexual intercourse. The last section, section D focused was on the use of oral contraceptives. The interview tool was developed by the researchers guided by the Theory of Reasoned Action, Theory of Planned Behaviour, and Social Cognitive Theory. This instrument was piloted at Ramotswa village- an urban-rural village, to refine the procedures and interview tool. This was an important step in ensuring that the tool was appropriate for the target population.
Participants completed the consent forms and a 2-page, self-report pre-individual interview/focus-group tool to allow us to characterize the kinds of people who participated. The informed consent stated the purpose of the study and ensured participants confidentiality. The consent also stated that all data will be used for research purposes only and no names or identifying information of participants was to be included in the research reports. Permission to audio-tape was also sought from each participant.
A total of twenty-nine participants participated in the study. Two focus groups were conducted at Moshupa village, one group consisted of five participants who were recruited at the clinic, and the other group consisted of five ordinary village people who were working at the drought relief program. Five individual interviews were also conducted at Moshupa village. Both the individual interviews and the focus group interviews at Moshupa were conducted on the 11th of May 2017.
In Mochudi, one focus group discussion was conducted with seven participants and seven individual interviews were conducted on the 16th of May 2017. The participants of this study were purposively selected, Batswana women only and those not on cancer treatment and residing in peri-urban rural type village. Purposive sampling also known as judgment or selective sampling, as the literature evidence (Bernard, 2003; Creswell and Plano Clark, 2011; Palys, 2008) suggest uses non probability sample. Therefore, a non-probability sampling approach was used to select women. Those who volunteered and willingly wanted to take part were further given a choice to either participate in Focus Group Interviews or Individual Interviews.
To elicit behavioral beliefs or outcome expectancies, we asked the participants to report the good things and bad things that would happen if they engaged in the behavior of interest (e.g., what are the good things that would happen if you were screened for cervical cancer?). To elicit normative beliefs, we will ask participants to list the referents who would approve or disapprove of their engaging in the behavior (e.g., which people or groups think you should always use condoms if you have sexual intercourse). To elicit control beliefs relevant to self-efficacy, we asked participants to report factors that would facilitate or inhibit their ability to perform the behavior (e.g., what would make it easy for you to limit the number of people with whom you have sexual intercourse). This helped us to identify barriers to safer sex that must be assessed.
11. Data analysis
The background and demographic data of all the participants was analysed using the descriptive statistics. Content analysis method was used to analyse qualitative data. The process involved interview transcription, data coding, identification of themes, and theme patterning. After conducting individual and focus group interviews with the participants, the researchers transcribed all of the audiotapes and created transcripts. Response to semi-structured individual interviews, memos and observational comments that were noted when interviewing the participants were typed. The interviews that were conducted in Setswana were translated into English by two of the researchers who were fluent in both English and Setswana. The researchers read the transcripts, over and over to familiarize themselves with the data. This has been supported by Ary, Jacobs, and Sorensen (2006) that the researcher has to reread the notes and transcripts, and listen repeatedly to the audio-tape in order to familiarize with the data. To ensure qualitative rigor, research team members agreed on the themes and coding.
12. Results/findings
Table 1 shows that the mean age of the women at the focus group interview and for individual interviews at both sites, Mochudi and Moshupa was above 30 years with an age range of between 25 and 48 years old. Most of these women reported to be single and had a primary or secondary level education. Most of them also reported that they lived with a partner and they had had sexual intercourse by the age of 18 years. The majority of the women reported that they had been pregnant (> 80%), had used a condom the last time of sexual encounter (> 75%) and used contraceptives (> 65%). More than 55% of the women reported not to have indulged in drinking and smoking behaviors. Though more than 50% had heard of cervical cancer and Pap smear or cervical screening, on the contrary less than 58% had had the Pap smear screening in the last twelve months. A small number of the participating women reported to have heard of the Human papilloma-virus (HPV) and HPV vaccine. The majority of the women were however willing to take up Pap smear screening.
Table 1.
Social-demography characteristics of the participants at the Mochudi and Moshupa focus group discussions and individual interviews.
| Mochudi (n = 12) | Moshupa (n = 17) | |||
|---|---|---|---|---|
| Characteristic | Count | % | Count | % |
| Educational Level | ||||
| 1. Never gone to school | 4 | 33.3 | 1 | 5.9 |
| 2. Primary | 0 | 0 | 4 | 23.5 |
| 3. Secondary | 7 | 58.3 | 10 | 58.8 |
| 4. University/College | 1 | 8.3 | 2 | 11.8 |
| 5. Non formal | 0 | 0 | 0 | 0 |
| Employment status | ||||
| 1. Student | 3 | 25 | 0 | 0 |
| 2. Employed | 7 | 58.3 | 10 | 58.8 |
| 3. Self employed | 2 | 16.7 | 4 | 23.5 |
| Lived with a partner | ||||
| 1. No | 3 | 25 | 7 | 41.2 |
| 2. Yes | 9 | 75 | 10 | 58.8 |
| Marital status | ||||
| 1. Single | 10 | 83.3 | 13 | 76.5 |
| 2. Married | 2 | 16.7 | 2 | 11.8 |
| 3. Divorced | 0 | 0 | 1 | 5.9 |
| 4. Widowed | 0 | 0 | 0 | 0 |
| Ever had sexual intercourse | ||||
| 1. No | 2 | 16.7 | 0 | 0 |
| 2. Yes | 10 | 83.3 | 17 | 100 |
| Useed a condom last time of sexual intercourse | ||||
| 1. I have never had sexual intercourse. | 1 | 8.3 | 0 | 0 |
| 2. No | 1 | 8.3 | 4 | 23.5 |
| 3. Yes | 10 | 83.3 | 13 | 76.5 |
| Have you ever been pregnant | ||||
| 1. No | 1 | 8.3 | 2 | 11.8 |
| 2. Yes | 10 | 83.3 | 15 | 88.2 |
| Do you use contraceptive | ||||
| 1. No | 2 | 16.7 | 5 | 29.4 |
| 2. Yes | 8 | 66.7 | 12 | 70.6 |
| Drunk alcohol in past 30 days | ||||
| 1. No | 7 | 58.3 | 13 | 76.5 |
| 2. Yes | 5 | 41.7 | 3 | 17.6 |
| Smoked in past 30 days | ||||
| 1. No | 12 | 100 | 13 | 76.5 |
| 2. Yes | 0 | 0 | 3 | 17.6 |
| Heard of Human papillomavirus (HPV) | ||||
| 1. No | 4 | 33.3 | 8 | 47.4 |
| 2. Yes | 8 | 66.7 | 8 | 47.4 |
| Heard of the vaccine for Human papillomavirus (HPV) | ||||
| 1. No | 1 | 8.3 | 0 | 0 |
| 2. Yes | 1 | 8.3 | 2 | 11.8 |
| Ever heard of cervical cancer | ||||
| 1. No | 2 | 16.7 | 1 | 5.9 |
| 2. Yes | 8 | 66.7 | 16 | 94.1 |
| Ever heard of Pap smear screening | ||||
| 1. No | 2 | 16.7 | 8 | 47.1 |
| 2. Yes | 8 | 66.7 | 9 | 52.9 |
| Ever had Pap smear screening | ||||
| 1. No | 7 | 58.3 | 12 | 70.6 |
| 2. Yes | 4 | 33.3 | 5 | 29.4 |
| Pap smear screening in the past 12 months | ||||
| 1. No | 5 | 41.7 | 3 | 17.6 |
| 2. Yes | 1 | 8.3 | 0 | 0 |
| Willing to have Pap smear screening | ||||
| 1. No | 1 | 8.3 | 4 | 23.5 |
| 2. Yes | 10 | 83.3 | 13 | 76.5 |
| Age Range | 25 Mean |
48 SD |
25 Mean |
41 SD |
| Mean Age | 35.33 | 7.679 | 32.35 | 5.291 |
| Mean age of first sexual intercourse | 18.50 | 6.375 | 19.35 | 2.120 |
| Mean age of first Pap smear screening for | 25.20 | 16.649 | 32.00 | 4.637 |
13. Behavioral beliefs
Some participants had the knowledge about cervical cancer screening and its importance from the health practitioners in the clinics they attended, whilst some had very limited knowledge as they asked the research to first elaborate what cervical cancer screening is. It seemed most of the elderly people had the knowledge as compared to the younger women. The majority of the participants believed that going for cervical cancer screening was a very good idea as one would get treated if found with the signs or have cervical cancer. One participant said: “Botlhokwa jwa teng ke gore o itlhatlhobela gore otle o fiwe kalafi e lebaneng e sa ntse ele ntšha” [“Its importance is that you should check yourself such that you get the appropriate medication and assistance early”]. Another added that: “Gore ke tle ke itse seemo same, ke bone kalafi ga nka tshwarwa ka kankere” [“So that I know my status and get treatment in time if I am diagnosed with cancer”].
Even though most believed that going for cervical cancer screening was a good idea, the participants expressed the fear and misconception for going for cervical cancer screening as they stated that if you are found to be having the signs of cancer or you have cancer, often people will think that you have been having sexual intercourse with many men. One participant noted that if the signs of cervical cancer are found “you will have to remove the uterus and this will leave a big opening and you won’t find a male partner. One participant alluded that: “fa popelo e ntshitswe o tla nyalwa ke mang? Ke mang yoo ka nyalang mosadi yo o sa tsholeng. O tla opelelwa dipina tsa tlhatswa lesire” [“If your uterus has been removed, who will marry you” Who will want to marry a barren woman? songs like wash the wedding gown will be sung to you”]. Similarly, another participant noted: “hei fa popelo e ntshitswe o tla nna wa ga mang ruri” [“if the cervix and uterus are removed who will want or marry you”].
Participant also stated that sometimes it is the fear of knowing your status as cancer is associated with dying. The stigma attached to cervical cancer and the cultural beliefs attached to the disease tend to be one of the many factors that hinder women to go for cervical cancer screening.
14. Normative beliefs
Participants noted that the health practitioners were the ones who encouraged them to go for cervical cancer screening. Some noted that sometimes at the clinic they are taught about cervical cancer but due to stigma attached to cervical cancer, most of them indicated that they were reluctant to go for screening. In contradiction, some participants indicated that there are certain Christian churches that do not approve women to go for cervical cancer screening. One participant noted that some of these churches do not believe in any screening for any disease. Another participant alluded that “these pastors tell you to throw away the treatment if you had gone to the medical doctors” One added that “they claim to have cured the disease so you do not need any medication”. In addition, one said: “Baruti ba dikereke tsa pholoso ka ba dumela gore pholo e tswa ko modimong”. [“These ‘born again churches’ often mislead people in the name of God”].
15. Control beliefs (what makes it easy or difficult)
Most participants noted that it is discouraging to go for cervical cancer screening because of the delaying results. One participant stated that: “mma ke nale ngwaga o tlhe ke tlhatlhobilwe, le jaana ke eme. Fa e le gore kena le mogare kana kena le kankere ke tla bo ke swe” [“madam, it’s almost a year since I went for screening till this day I have not received my results. If I have the cancer virus or have cancer I will just die”].
Another participant said: “Ditlamelo di bokoa, mo gongwe ba latlha maduo a gago, kana di diriswa ga di yo, kana ene o o tlhatlhobang ga a yo”. [“Services at the clinics are poor, sometimes they lose your results, sometimes equipment for the screening are not there or even someone who do the screening is not even there”]. To add on that one noted: “Fa o ka reetsa dipuo tsa Batswana wa seka wa ya go ikutlwela o tla tsha-bela ruri”. [“If you listen to what is being said and don’t go, you will never come back”]. Some participants just indicated the fear of knowing as the major issue that makes them not to go for screening.
The participants believed that the knowledge about the disease would make it easy for them to go for screening. They indicated that they lacked knowledge of cervical cancer. They stated that cervical cancer has not been publicized like HIV and AIDS. They said with HIV, there were pamphlets everywhere and the radio and the television broad casted about the dangers of the disease. They recommended that cervical cancer screening should also be given the same publicity in terms of knowledge just like HIV to help people especially in the remote areas to know about the diseases.
16. Socio-Cultural barriers to cervical cancer screening
Participants expressed being fearful about diagnosis of the disease and associated the disease with death. Other source of fear included the procedure, having to be done vaginal exam and having a speculum inserted in the private parts. There was the belief that when the spec-ulum is inserted in the vagina, the cervix and uterus will be left gaping. Culturally, being done vaginal examination is embarrassing alluded one participant. Some believed that others shy away because they heard that it affects the uterus. Sexual organs are private and not supposed to be touched or to be a topic of discussion. One participant said:
“Fa gongwe ka gore ga re itse e dirwa jang, o mongwe o tla bo a dumela gore ga o simolla o tsengwa lebogo ka fa tlase he..! Go a go affecta popelo, go a go reng, koore re ipha ditlamorago dilo tse eseng re di dire, re utlwa magatwe ka motho ba ba senang boitsaanape ..ka gone go tlhatlhoba kankere ya popelo ..Ke dumela gore ba bangwe ba go raa ba re nyaa,wa go tsenngwa tshipi fela e tona ..Hey popelo e bile ga entse jalo ya go sala e atlhame ba bua dio fela tse eleng gore dia go go kgoba marapo”. [As we don’t know how it comes about, another person might believe that if you start getting fingered in the genitalia it affects the cervix due to giving ourselves consequences to things we have not done before, we listen to hearsay from people with no expertise about cervical cancer screening. I believe that say they are going to insert a large spec-ulum; and hey your cervix will be left gaping, saying that will end up discouraging you].
Other factors included stigma that is associated with cervical cancer. There is a belief that if one has cervical cancer it is because of having sexual relationship with many men. This leads to many women being shy of going for cervical cancer screening for fear of being la-belled a promiscuous person. One said: “…go tla bo nna gore bogolo jang thata ngwao ya Setswana go dumelwe mo go reng motho ga o bona a nna le botlhoko ko popelong ke gore ke motho yo o dirisetsweng….” [“.. it will mean in Setswana culture that if someone has cervical pain that they have slept with a lot of”].
Some cultures are against any use of health services. They do not use health facilities, and such people do not go for cervical cancer screening.
17. Discussion
The findings of this study revealed that knowledge, norms and beliefs affected women’s going for cervical cancer screening. The study looked at beliefs for; a) going for cervical cancer screening, b) limiting male sexual partners, c) consistent use of condoms during sexual intercourse and d) the implications of the use of oral contraceptives among the women. These were socio-cultural issues that presented themselves as deterrents for women to go for screening. Research has shown that the impact of social cultural norms and beliefs regarding cervical cancer screening is un-denied and needs attention (Wong, Wong, Low, Khoo, & Shuib, 2008). Basing the study on the theories above enabled the researcher to describe the norms and beliefs about cervical cancer screening.
It is evident from the study that most women (59.5% or 17/29 had heard about cervical cancer screening, and yet only 8.3% or 1/29 reported having undergone cervical cancer screening. This shows that knowledge does not necessarily translate to practice. Findings of the study are similar to a study done in Yemen where cervical cancer screening was low with only 7% of all knowledgeable about cancer screening reporting to have undergone screening (Abdul-Aziz, 2012). From the focus group discussions, it was eminent that most participants lacked proper knowledge on cervical cancer, hence had myths about it. This suggests that there is lack of information dissemination across the country and/or lack of suitable training for all service providers within the health facilities as in clinics. This may be purported by diversified nature of the country and skills acquisition by the relevant offcers. Accordingly, most participants lacked proper knowledge of cervical cancer screening, and this ignorance and lack of knowledge is not only putting the participants at risk but suggest that most people of the same age range in Botswana are susceptible and prone to cervical cancer.
Other aspects which are culturally based were fear of the unknown, fear of victimization and people’s misconception about someone undertaking cervical cancer screening. Fear and misconception regarding cancer screening was also evidenced by Williams (2014) in a study carried out at Kumasi in Ghana. Women in this study indicated that “fear and panic generated by the cancer diagnosis” prevented the women to go for screening. The findings are consisted with Williams (2014) results were one of the participants in this study noted:
There is a saying that if you don’t go and do the test, how would you know that you have it. So for the fear of the unknown, many would not do the test to find out if they have it or not. It is just like the HIV/AIDS test. The perception is that once you know that you have the cancerous cells, you would die early. So some do prefer the unknown in order to live a bit longer. (p. 559)
So the participants have a belief that having cervical cancer is a death sentence and knowing that you have been diagnosed with cancer can cause much stress, and can lead to early death. The women believe that cancer is incurable like AIDS.
There is an assumption that someone who undergoes cervical cancer screening has had multiple sexual partners. Mutyaba, Faxelid, Mirembe, & Weiderpass, (2007) as cited by Lim and Ojo (2017) noted that most households are headed by men, and if a woman had to be screened and diagnosed with cervical cancer, the spouse will conclude that the woman has been unfaithful. This by itself is detrimental and injurious to the government and attempts to advocating and encouraging of women within the specified age range to undergo cervical cancer screening. The research evidence of this study indicating lack of participation by women in cervical cancer screening endorse the findings by WHO (2002) that approximately 80% of the deaths that occurred in 2000 and related to cervical cancer was in developing countries. The findings further suggested that this was due to lack of accesses to effective screening programmes. Botswana has got one of the better screening facilities in its health stations which are satisfactorily well distributed across the country. The Ministry of Health and Wellness is one of the Ministries that always have a larger share of the country’s annual budget. The question that arises would be how can Botswana improve on its efficacy and effectiveness of ensuring that cervical cancer screening programmes reach most of the people in the country? Are the technological facilities affordable to most Botswana and are facilities accessible to many people? As observed by McFarland (2003) Botswana had a low level cervical screening rate by then and should the status quo be maintained. To have many women going for cervical cancer screening the targeted population should be informed (Ibekwe et al., 2010). The WHO (2002) also asserts that cervical cancer screening is an important area of action for any cancer control program because of the burden of disease, and the potential for effective prevention via screening. Implication for knowledge empowerment efforts and public health awareness needs to be put in place.
18. Conclusion
Consistent with TRA and TBP theories, helped understand the norms and beliefs for going for cervical cancer screening. The women in the study revealed the norms and beliefs that influenced their behavior to go for cervical cancer screening. More education about cervical cancer screening is required to further increase awareness and willingness to undergo cervical cancer screening. This could help improve appropriate culturally sensitive cervical cancer screening health programs for Botswana women.
Furthermore, the findings for this study, contribute towards U54 program long term strategy of lowering the burden associated with morbidity and mortality associated with cervical cancer. It is therefore imperative to have two follow-up studies country wide, one being the quantitative study informed by the attributes of this qualitative study and lastly an intervention strategy generated and implemented to establish if there would be any change to these initial findings. Such intervention study should be cultural and relevant and be population specific.
19. Limitations
Those women who did not volunteer could have provided extra information during the focus group or individual interviews. However, the assistant of the village chiefs and health personnel at the clinics in recruiting the participants ensured that the identified participants had relevant information.
Social desirability bias could not be avoided amongst the women as some might have responded to impress the researchers. This was addressed by administering confidentiality and honest pledge form which ensured that the participants signed to indicate that they will be honest in their responses.
Acknowledgement
UPenn for funding this pilot study.
Funding sources
NIH/UPenn.
Footnotes
Ethical approval details
Reference No: HPDME: 13/18/1 vol X (6 7 9); UPenn Protocol No: 825673; University of Botswana IRB: UBR/RES/IRB/1647.
Conflict of interest
None.
References
- Abdul-Aziz M (2012). Knowledge, attitude and practice towards cervical cancer among reproductive health clients at the University of Science & Technology Hospital-Sana’a in Yemen. Yemeni Journal for Medical Sciences, 6, 21–27. [Google Scholar]
- Ary D, Jacobs LC, & Sorensen C (2006). Introduction to research in education.Wadsworth: Cengage Learning. [Google Scholar]
- Bano F, Kolhe S, Zamblera D, Jolaoso A, Folayan O, Page L, et al. (2007). Cervical screening in under 25s: A high-risk young population. European Journal of Obstetric Gynecology Reproduction, 1389, 86–89. [DOI] [PubMed] [Google Scholar]
- Bernard HR (2003). Research methods in anthropology: Qualitative and quantitative approaches (3rd ed.). Walnut Creek, CA: Alta Mira Press. [Google Scholar]
- Bigoni J, Gundar M, Tebeu PM, Bongoe A, Schäfer S, Fokom-Domgue J, et al. (2015). Cervical cancer screening in sub-Saharan Africa: A randomized trial of VIA versus cytology for triage of HPV-positive women. International Journal of cancer, 137(1), 127–134. 10.1002/ijc.29353. [DOI] [PubMed] [Google Scholar]
- Carlson JA (2010). Avoiding traps in member checking. The Qualitative Research Report,15(5), 1102–1113. [Google Scholar]
- Creswell JW (2003, 2014). Educational research in education: Planning, conducting, and evaluating quantitative and qualitative research. Columbus, Ohio: Upper Saddle River. [Google Scholar]
- Creswell JW, & Plano Clark VL (2011). Designing and conducting mixed method research (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Dodd RH, McCaffery J, Marlow LAV, Ostini R, Zimet GD, & Waller J (2014). Knowledge of human papillomavirus (HPV) in the USA, the UK and Australia: An international survey. Sex Transm Infect, 90, 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibekwe CM, Houqe ME, & Ntuli-Ngcobo B (2010). Perceived benefits of cervical cancer screening among women attending Mahalapye District Hospital, Botswana. Asian Pacific Journal of Cancer Prevention, 11(4), 1021–1027. [PubMed] [Google Scholar]
- Joshi S, & Sankaranarayana R (2015). Opportunities for cervical cancer prevention inIndia. Journal of Krishna Institute of Medical Sciences University, 4(1), 8–17. [Google Scholar]
- Lim JNW, & Ojo AA (2017). Barriers to utilization of cervical cancer screening in Sub Sahara Africa: A systematic review. European Journal of Cancer and Care, 26, e12444 10.1111/ecc.12444. [DOI] [PubMed] [Google Scholar]
- McFarland DM (2003). Cervical cancer and Pap smear screening in Botswana: Knowledge and Perceptions. International Nursing Review, 50(3), 167–175. [DOI] [PubMed] [Google Scholar]
- McFarland DM (2009). Beliefs about the causes of cervical cancer in Botswana: Implications for nursing. International Nursing Review, 56, 426–432. [DOI] [PubMed] [Google Scholar]
- Mills AJ, Durepos G, & Wiebe E (2010). Encyclopedia of case study research. London: Sage. [Google Scholar]
- Ministry of Health (2009). Health statistics report. Gaborone: Government of Botswana. [Google Scholar]
- Mutyaba T, Faxelid E, Mirembe F, & Weiderpass E (2007). Influences on uptake of reproductive health services in Nsangi community of Uganda and their implications for cervical cancer screening. Reproductive Health, 4, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palys T (2008). Purposive sampling In Given LM (Ed.). The Sage Encyclopedia of Qualitative Research Methods (pp. 697–698). Los Angeles: Sage. [Google Scholar]
- Pitts M, & Clarke T (2002). Human papillomavirus infections and risks of cervical cancer: What do women know? Health Education Research, 17(6), 706–714. [DOI] [PubMed] [Google Scholar]
- Ramogola-Masire D, de Klerk R, Monare B, Ratshaa B, Freidman H, & Zetola N (2012). Cervical cancer screening in HIV-infected women using the “See and Treat” approach in Botswana. Journal of Acquired Immune Deficiency Syndrome, 59(3), 10.1097/QAI.0b013e3182426227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramogola-Masire D (2014). HPV vaccine for cervical cancer prevention in Botswana.Commonwealth Health Partnerships. [Google Scholar]
- Rosser JI, Njoroge B, & Huchko MJ (2015). Changing knowledge, attitudes, and behaviors regarding cervical cancer screening: The effects of an educational intervention in rural Kenya. Patient Education and Counseling, 98(7), 884–889. 10.1016/j.pec.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders MNK, Thornhill A, & Lewis P (2016). Research methods for business students (7th ed.). Essex: Pearson. [Google Scholar]
- Schiffman M, & Solomon D (2013). Cervical-cancer screening with human papillomavirus and cytologic co-testing. The New England Journal of Medicine, 369, 2324–2331. [DOI] [PubMed] [Google Scholar]
- Sigurdsson K, & Sigvaldason H (2007). Is it rational to start population-based cervical cancer screening at or soon after age 20? Analysis of time trends in preinvasive and invasive diseases. European Journal of Cancer, 43(4), 769–774. [DOI] [PubMed] [Google Scholar]
- Sudenga SL, Rositch AF, Otieno WA, & Smith JS (2013). Brief Report: Knowledge, attitudes, practices and perceived risk of cervical cancer among Kenyan women. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society, 23(5), 895–899. 10.1097/IGC.0b013e31828e425c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations (2018). World Economic Situation and Prospects (WESP). Retrieved from http://www.un.org/en/development/desa/policy/wesp/wesp_current/2014wesp_country_classification.pdf on the 26 July 2018. [Google Scholar]
- Williams MS (2014). A qualitative assessment of the social cultural factors that influence cervical cancer screening behaviors and the health communication preferences of women in Kumasi, Ghana. Journal of Cancer Education, 29(3), 555–562. 10.1007/s13187-014-0611-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong P, Wong YL, Low Y, Khoo EM, & Shuib R (2008). International Journal of Behavioral Medicine, 15, 289 10.1080/10705500802365490. [DOI] [PubMed] [Google Scholar]
- World Health Organisation (2002). Cervical cancer screening in developing countries report. Geneva: World Health Organisation. [Google Scholar]
- World Health Organisation. (2013). WHO Guidelines for screening and Treatment of precancerous lesions for cervical cancer prevention. http://apps.who.int/iris/bitstream/handle/10665/94830/9789241548694. [PubMed] [Google Scholar]
- World Health Organization. (2015). Human papillomavirus (HPV) and cervical cancer. Retrieved 30 October, 2015, from http://www.who.int/mediacentre/factsheets/fs380/en/30. [Google Scholar]