Abstract
Objectives
HIV/AIDS has become the leading cause of death by infectious disease in China since 2009. However, the trend of gender disparities in HIV/AIDS has not been reported in China since 1990. Our study aimed to explore the secular trend of HIV/AIDS mortality in China from 1990 to 2016 and to identify its gender disparities over the past 27 years.
Method
The mortality data of HIV/AIDS were obtained from the Global Burden of Disease Study 2016 (GBD 2016). Logistic regression was used to estimate the prevalence odds ratio (POR) of gender for HIV/AIDS mortality in different surveys.
Results
The standardized mortality of HIV/AIDS in China rose dramatically from 0.33 per 100,000 people in 1990 to 2.50 per 100,000 people in 2016. The rate of HIV/AIDS mortality increased more quickly in men than in women, and the sex gap of mortality of HIV/AIDS widened. By 2016, the HIV/AIDS mortality in men was 3 times that in women and was 5.74 times that in women within the 75- to 79-year-old age group.
Conclusions
The mortality of HIV/AIDS in China is increasing, with a widening gender disparity. It is critical for policymakers to develop policies to eliminate these disparities and to ensure that everyone can live a long life in full health.
Introduction
Human immunodeficiency virus (HIV) and the consequent acquired immunodeficiency syndrome (AIDS) have caused a globally devastating pandemic, which led to major distortions in population age-sex distributions in the most affected areas[1, 2]. Worldwide, 77.3 million people have become infected with HIV, and 35.4 million people died from AIDS-related illnesses by 2018. The number of global deaths caused by HIV/AIDS reached a peak of nearly 1.9 million in 2006 and declined afterwards. In 2017, the number of AIDS-related deaths was nearly 1 million, which had dropped 51% compared with 2006[3]. In the northeast of South Africa, more than 60% of the deaths that occurred between 1992 and 2013 could be attributed to HIV. Although there was a 30% decrease in adult HIV-related mortality between 2007 and 2008, most South African villages still experienced a small increase in mortality from 2007 to 2013[4]. In some Eastern Mediterranean Regions (EMRs), the male mortality rate of HIV/AIDS increased from 0.38 per 100,000 to 2.15 per 100,000, with an increase of 6.7% annually since 1990, which was double that among females[5].
In China, the HIV epidemic has continued to expand, and the mortality attributable to HIV/AIDS has become a major public health concern[6]. In July 2017, approximately 728,270 persons were living with HIV/AIDS in China, and 223,798 died from AIDS-related illnesses[7]. Since HIV/AIDS has become the leading infectious cause of death in 2009[8], the number of reported HIV cases has increased over time, and the number of deaths related to HIV/AIDS has also increased from 5,544 in 2007 to 15,251 in 2017[9].
Although HIV/AIDS mortality in both males and females has rapidly increased in different areas of the world, gender differences are apparent. In most countries, men have higher mortality than women. The results of studies from South Africa and Zimbabwe have shown higher mortality among males than among females[10, 11]. In other countries, such as Malawi and Tanzania, females have had a significantly higher survival rate than similarly situated males[12, 13]. A 2-year follow-up study in China also suggested that women had an overall lower mortality[14]. However, there are no reports on how gender disparities in HIV/AIDS have changed over time in Chinese individuals. Therefore, a better understanding of these gender differences in HIV/AIDS is critical for AIDS prevention and control in China.
In this study, we used data from the Global Burden of Disease Study 2016 (GBD 2016) to identify the trend in gender differences over the past 27 years in China. Furthermore, since no study [15–19] has used the GBD 2016 dataset to conduct studies related to HIV/AIDS, we also hope to fill this research gap by using these data.
Data sources and methods
Data sources
Data were extracted from the GBD 2016, a large international cooperation project that globally, regionally, and nationally provides age-sex mortality for 264 causes of death from 1980 to 2016, including HIV/AIDS[20]. Original data, which the GBD adapted to estimate the HIV/AIDS mortality, were mainly from the Disease Surveillance Point (DSP) and the Notifiable Infectious Disease Reporting (NIDR) system. Both systems were administered by the Chinese Centers for Disease Control and Prevention[21].
In this study, we extracted and used 2 indicators to analyze HIV/AIDS mortality trends for 14 age groups (10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, and 75–79) from 1990 to 2016 in China: the age- and sex-specific number of deaths, mortality and their UI (uncertainty interval). The UI was the yield with 95% uncertainty intervals for the estimated data that included all age-specific mortality rates by the Estimation and Projection Package (EPP)-Spectrum model[21]. By using the number of deaths in each age group divided by the mortality rate in each age group, we estimated the population of each age group in China from 1990 to 2016 (see S1 Table).
Statistical analysis
We calculated the crude death rate of HIV/AIDS (per 100,000 people) among people aged 10–79 in China from 1990 to 2016 by using the numbers of deaths from individuals 10 to 79 years old divided by the estimated total population of individuals 10 to 79 years old; we also used the 2010 national census to determine the standardized mortality. By calculating the ratio of HIV/AIDS mortality of males to females (M/F) for different years for each age subgroup, we were able to calculate the Relative Risk (RR) to assess the gender and age differences at different time points. Data extraction was conducted using SPSS (SPSS 22.0 for Windows, IBM Inc, Chicago, IL, USA), and other analyses were conducted using Excel software, version 2016 (Microsoft, Redmond, Washington).
Results
Gender differences in HIV/AIDS mortality trends in China
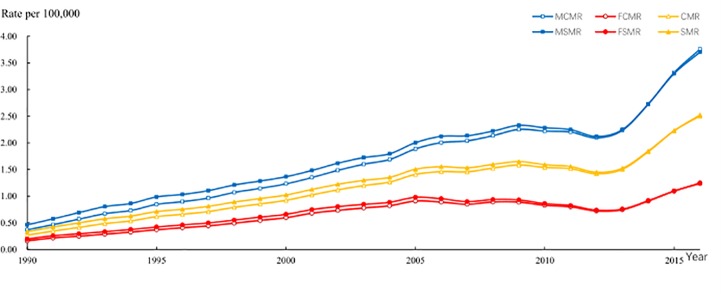
HIV/AIDS mortality was increasing continuously over the past 27 years. Fig 1 shows the crude death rate (CDR) and the standardized mortality rate (SMR) of HIV/AIDS in the 10- to 79-year-old age group from 1990 to 2016, and HIV/AIDS mortality increased rapidly in both males and females. The male HIV/AIDS standardized mortality increased from 0.46 per 100,000 people in 1990 to 3.70 per 100,000 people in 2016, and the standardized mortality of females increased from 0.20 per 100,000 people in 1990 to 1.24 per 100,000 people in 2016.
Fig 1. CDR and SMR trends in HIV/AIDS in the 10- to 79-year-old age group from 1990 to 2016.
The standardized mortality rate (SMR) of the 10- to 79-year-old age group was based on the distribution of males and females in the 2010 census data.
Gender differences in the HIV/AIDS mortality trends by age group
Fig 2 shows the trends in HIV/AIDS mortality by age and gender. As shown in Fig 2, the HIV/AIDS mortality for males remained very low in the 10- to 14-year-old age group and in the 15- to 19-year-old age group and then rose significantly until age 49, reaching its highest point of 5.55 per 100,000 in the 40- to 44-year-old age group in 2016; after that, it experienced a slight drop and soon climbed to its second peak again in the 75- to 79-year-old age group of 6.21 per 100,000 deaths in 2016. Compared with males, female mortality trends changed relatively steadily. After a relatively stable increase from age 10 to age 34, when the female HIV/AIDS mortality reached 1.53 per 100,000 in the 30- to 34-year-old age group in 2016, the female HIV/AIDS mortality rate maintained a small fluctuation. During the past 27 years, the mortality of HIV/AIDS in all age subgroups showed an increasing trend for both males and females. However, the increasing trends among females were lower than those among males.
Fig 2.
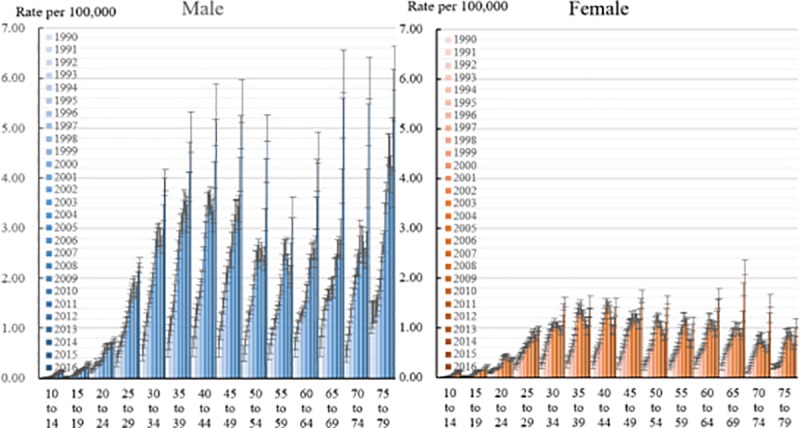
Age-specific mortality of HIV/AIDS and 95% uncertainty interval (UI) among males (left figure) and females (right figure) aged 10 to 79 years old from 1990 to 2016. Increasing trends were observed in both males and females, but the increase among females was less than that among males.
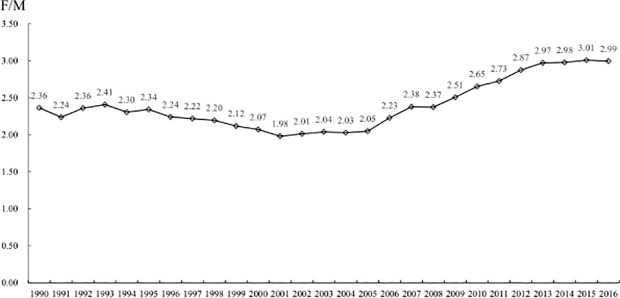
Fig 3 shows the changes in the ratio of HIV/AIDS mortality between males and females. In 1990, the male HIV/AIDS standardized mortality was 2.36 times that of the female rate. However, since 2001, the gap between male and female standardized mortality increased significantly, from 1.98 times in 2001 to 2.99 times in 2016.
Fig 3. Changes in the ratio of HIV/AIDS mortality of males to females.
From 2001 to 2016, the gap between male and female standardized mortality increased significantly.
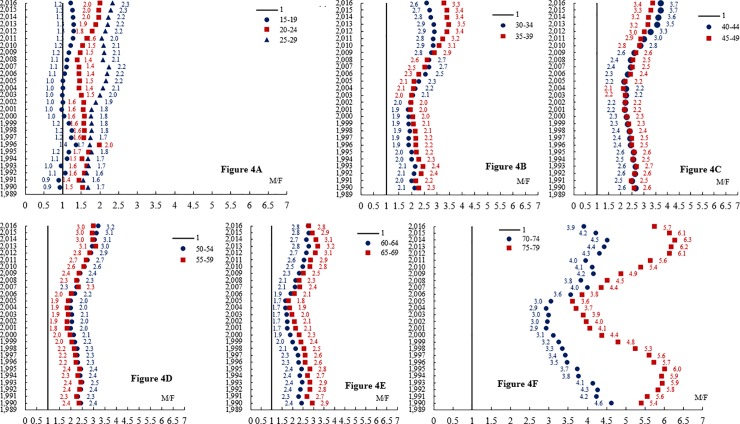
Age-specific HIV/AIDS mortality risk ratios of males versus females
As shown in Fig 3, from 1990 to 2016, a significant increasing trend in HIV/AIDS mortality was more obvious in males than in females. We calculated the risk ratio (RR) of male HIV/AIDS mortality versus that of female HIV/AIDS mortality for different years for each age subgroup (Fig 4). In Fig 4A, in the 15- to 19-year-old subgroup, few differences in gender disparities were evident in the past 27 years. For the 20- to 24-year-old subgroup, the gender difference reached its peak in 2016 (RR = 2.0). Similarly, the difference in HIV/AIDS mortality between males and females in the 25- to 29-year-old subgroup also peaked in 2016 (RR = 2.3).
Fig 4. Age-specific HIV/AIDS mortality risk ratios (RRs) of males compared with females in different years in China.
The gender difference in HIV/AIDS mortality was readily apparent and increased gradually with age.
In Fig 4B, the gender disparities in the 30- to 34-year-old and 35- to 39-year-old subgroups were apparent. From 1990 to 2009, the difference between HIV/AIDS mortality among males and females in the two groups was roughly the same (with similar RRs). However, since 2009, the difference in the 35- to 39-year-old subgroup gradually became higher than that of the 30- to 34-year-old subgroup and reached its peak in 2013 (RR = 3.5).
Fig 4C had a trend similar to those shown in Fig 4D and 4E. As shown in Fig 4C, 4D and 4E, the gender differences in HIV/AIDS mortality remained significant but decreased with age. In 2016, the RRs of the 40- to 44-year-old, 45- to 49-year-old, 50- to 54-year-old, 55- to 59-year-old, 60- to 64-year -old, and 65- to 69-year-old age groups were 3.4, 3.7, 3.0, 3.2, 2.8, and 2.8, respectively. However, for the 70- to 74-year-old age group, the gender disparity began to increase with age and peaked in the 75- to 79-year-old age group (see Fig 4F).
In summary, the gender difference in HIV/AIDS mortality was readily apparent and increased gradually with age. For example, in 2016, with increasing age, the RR increased from 1.2 (15- to 19-year-old subgroup) to 5.7 (75- to 79-year-old subgroup), for a nearly five-fold total increase.
Discussion
We found that HIV/AIDS mortality was continuously increasing in China and that gender differences were becoming more evident over time. The data of this study also correspond to those of the two periods of the development of AIDS in China. First, from 1990 to 1993, the HIV-related mortality increased from 0.33 per 100,000 people to 0.58 per 100,000 people and expanded to 21 Chinese provinces; this time interval was termed the diffusion period. Second, after 1993, the mortality of HIV/AIDS has increased rapidly, from 0.63 per 100,000 people in 1994 to 2.50 per 100,000 people in 2016, nearly 4 times the mortality in 1994. In this period, 31 provinces and municipalities in China reported HIV-infected persons; this time interval was termed the rapid growth period. In theory, with the advent of antiretroviral treatment (ART), the mortality rate would decrease significantly, which was also reported by previous studies[14,22]. However, great numbers of people who do not meet the treatment criteria may have higher mortality rates; therefore, the HIV/AIDS mortality may continue to rise from 1990 to 2016. In terms of gender differences, the 27-year period can also be divided into two stages in China. First, from 1990 to 2008, the male HIV/AIDS mortality was double the female mortality. Second, after 2008, the gap between male and female mortality became wider. By 2016, male mortality was nearly three times that of females. This result could be attributed to the pattern of the HIV epidemic, which has changed over time, and men who have sex with men (MSM) now account for more new infections than before. The contribution of our study is the finding that gender disparities in HIV/AIDS mortality became larger over time, and this study is also one of the few reports on the long-term trends of gender differences in HIV/AIDS mortality in China.
One reason why HIV/AIDS mortality among males was higher than that among females is the significant gender gap in China. According to several censuses, the sex ratios (male vs female ratios) at birth (SRB) were 111.14 in 1990, 116.86 in 2000, 117.94 in 2010 and 115.88 in 2014[23]. This difference may cause a higher HIV prevalence among males, which could then cause higher mortality among males. In addition, another Chinese survey showed that between 1990 and 2000, the male mortality was higher than the female mortality, and this difference has widened[24].
The second reason is that MSM not only have the highest HIV incidence internationally but also bear a disproportionate burden of HIV infection in China[22, 25]. Moreover, some high-risk sexual behaviors, such as inconsistent condom use or having multiple sexual partners or alcohol/drug abuse, would put MSM at a higher risk for HIV infection than normal individuals[14,26,27]. The proportion of MSM increased from 1.5% in 2006 to 23.4% in 2018, an almost 15-fold increase; that mode of transmission was the fastest-growing method for HIV/AIDS spread in China[28,29]. Therefore, the number of infected men was higher than the number of infected women in China.
The third reason for these gender differences is the outcomes of treatment for HIV/AIDS. Many studies have shown that ART not only helps to reduce the global death rate of HIV/AIDS but also benefits women more than men[10, 11]. Since the Chinese government provided ART drugs for free in 2002, the free ART database, which was established to monitor and evaluate the treatment process, suggested a positive association between the female sex and positive treatment outcomes[30,31]. Another article drew a similar conclusion regarding gender differences in the 2-year mortality of the HIV-infected Chinese population[14]. Compared with men, women not only experience a better effect of ART but also have better adherence to treatment. Therefore, more effort should be made to encourage HIV-infected males to participate in ART—the earlier, the better.
Finally, the gender differences in HIV/AIDS mortality may also be attributed to genes. Previous studies indicated that HIV-infected women tend to have higher CD4+ levels, meaning they may experience a more favorable course of disease than men[32]. Women also have a better response to the drugs biologically[14]. In addition, prenatal HIV testing, family planning, and gynecological services provide women with wider access to HIV testing and timely treatment[33,34]. We strongly recommend that MSM participate in counseling and testing services to verify their HIV status.
In this study, males and females in the 35- to 49-year-old age group had a higher HIV/AIDS mortality rate. The results were similar to those reported in other provinces and cities in China[35,36,37]. Most of the causes of death were AIDS-related diseases, and the survival period (from diagnosis to death) was 5 to 15 years. In addition, the elderly males (age group 65–79) had the highest mortality rate, which may be because the average life expectancy of men in China in 2015 is 73.64[38]. Most men approximately 70 years old, even if they are not HIV-infected or AIDS patients, will die of natural death or other diseases. The mortality of the 20- to 24-year-old subgroup was higher than that of the 15- to 19-year-old subgroup, and few gender differences in HIV/AIDS mortality emerged in the 15- to 19-year-old subgroup. However, for the 20- to 24-year-old subgroup, HIV/AIDS mortality among males was almost 1.5–2 times that among females. Despite the fact that some Chinese adolescents have sex at the age of 10, the average age of the onset of their sexual behavior is 18–20 years. In addition, given the long duration between initial infection with HIV/AIDS to death, some 15- to 19-year-old teenagers who contract sexually transmitted infections die at 20–24 years of age. To date, there have been few studies on HIV/AIDS among adolescents[39–42], but the impact of this epidemic on this age group cannot be underestimated, especially for young males. Considering the characteristics of the age group, adolescent (15–24 year old) males are more likely influenced by homosexuality-related discrimination and exhibit high-risk behaviors, thus leading to infection. Policymakers should focus on taking measures to prevent the spread of this epidemic among young teenagers.
The gender difference of HIV/AIDS mortality increased with age and reached the maximum in the 75- to 79-year-old age group. This phenomenon can be explained by the following four points: First, the gender gap in China is high, and the number of infected women is lower than the number of infected men in China[30]. Second, women experience a more favorable course of disease[33]. Third, women have better adherence to the ART and have better response to the drugs[14]. Last, the average life expectancy of women in China is older than that of men[38].
From this study, we also discovered a frustrating phenomenon: HIV/AIDS mortality worldwide is decreasing, while HIV/AIDS mortality in China is still steadily increasing. Because of the widespread use of ART, there was a 48% decline in the number of deaths from AIDS-related causes in the world. In eastern and southern Africa, the number of deaths from AIDS-related illnesses showed the sharpest decrease, from 1.1 million in 2004 to 420,000 in 2016[43]. Although the introduction of ART has also helped many people infected with HIV/AIDS in China, the mortality of HIV/AIDS is still on the rise[44, 45]. Previous studies have shown that highly active antiretroviral therapy (HAART), late diagnosis, poverty, lower education, and being older than 40 years of age were strongly related to AIDS-associated death[22,46]. Therefore, Chinese policymakers should expand testing to increase early HIV diagnosis and recommend ART to all diagnosed individuals as early as possible to reduce the number of AIDS-related deaths[47].
The limitations of our study are as follows. First, the data we analyzed are only speculative data of the GBD; it is possible that unintentional errors occurred when estimating the mortality rates and comparing the trends. However, the GBD 2016 collected a large sample of globally representative data, and the estimated mortality was standardized according to the 2010 age-sex distribution in China. Therefore, the conclusions drawn from the data are accurate and representative. The second limitation of our study is the age scale. The population of interest in this survey was not the whole population, as the data lack representation from the populations aged 0–10 years and over 79 years. Very few surveys have been conducted to examine HIV/AIDS mortality in these two age groups. Considering the fact that these age groups comprise only a small proportion of the population, the absence of these data in our surveys is unlikely to change the findings of this study.
Our research reveals the gender disparities in HIV/AIDS mortality. Given that this difference has increased over time, policymakers should make use of gender-specific approaches in the development of intervention strategies to reduce the mortality of HIV/AIDS in China. We propose several methods to slow the growth of HIV/AIDS mortality. First, we have promoted public HIV/AIDS education beginning in primary school to reduce the HIV/AIDS infection. Second, the groups at high risk for HIV should be regularly tested for HIV, and once these individuals become infected, they should receive ART immediately to prolong life. We also found very few studies on the complex causes of gender disparities in HIV/AIDS mortality in China; therefore, it is necessary to design cohort studies to better understand the effects of age, ART and other factors on HIV/AIDS mortality in men and women.
In conclusion, the mortality of HIV/AIDS in China is increasing, and the difference between males and females is gradually widening. Our study on this gender difference in mortality provides a basis for policymakers to formulate policies to eliminate these disparities and to ensure that everyone can live a long life in full health.
Supporting information
The number of deaths in each age group divided by the mortality rate in each age group.
(DOCX)
Data Availability
Data were extracted from the GBD 2016 (http://ghdx.healthdata.org/gbd-2016).
Funding Statement
This work was supported by the National Natural Science Foundation of China (No. 81673245 to YM, No 81773454 to ZZ) and China Scholarship Council (No 201806015008 to ZZ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Streatfield PK, Khan WA, Bhuiya A, Hanifi SMA, Alam N, Diboulo E, et al. HIV/AIDS-related mortality in Africa and Asia: evidence from INDEPTH health and demographic surveillance system sites. Glob Health Action. 2014; 7: 25370 10.3402/gha.v7.25370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cock KMKD, Jaffe HWH, Curran JWJ. Reflections on 30 years of AIDS. Emerg Infect Dis. 2011; 17(6): 1044–1048. 10.3201/eid/1706.100184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNAIDS. Trend of AIDS-related deaths. 18 March 2019. Available from: http://aidsinfo.unaids.org/ Cited 18 March 2019. [Google Scholar]
- 4.Mee P, Kahn K, Kabudula CW, Wagner RG, Gomez-Olive FX, Madhavan S, et al. The development of a localised HIV epidemic and the associated excess mortality burden in a rural area of South Africa. Glob Health Epidemiol Genom. 2016; 1: e7 10.1017/gheg.2016.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mokdad AH. Trends in HIV/AIDS morbidity and mortality in Eastern Mediterranean countries, 1990–2015: findings from the Global Burden of Disease 2015 study. Int J Public Health. 2018; 63(Suppl 1): 123–136. 10.1007/s00038-017-1023-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li M, Tang W, Bu K, Mahapatra T, Zhang XY, Feng YB, et al. Mortality among People Living with HIV and AIDS in China: Implications for Enhancing Linkage. Sci Rep. 2016; 6: 28005 10.1038/srep28005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NCAIDS, NCSTD, China CDC. Update on the AIDS/STD epidemic in China in July,2017. Chin J AIDS STD. 2017; 09:775 [Google Scholar]
- 8.Jiang ZS, Jiang JN. Research progress in death risk factors of HIV infector and AIDS patients. Inter J Epidemiol Infect Dis. 2012, 39 (1): 63–67. [Google Scholar]
- 9.Ministry of Health of the People’s Republic of China, China 2010 UNGASSCountry Progress Report (2008–2009). 2nd April 2010. Available from: http://data.unaids.org/pub/Report/2010/China_2010_country_progress_report_en.pdf. Cited 29 December 2018
- 10.Cornell M, Myer L, Kaplan R, Bekker LG, Wood R. The impact of gender and income on survival and retention in a South African antiretroviral therapy programme. Trop Med Int Health. 2009;14(7): 722–731. 10.1111/j.1365-3156.2009.02290.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takarinda KC, Harries AD, Shiraishi RW, Mutasa-Apollo T, Abdul-Quader A, Mugurungi O. Gender-related differences in outcomes and attrition on antiretroviral treatment among an HIV-infected patient cohort in Zimbabwe: 2007–2010. Int J Infect Dis. 2015; 30: 98–105. 10.1016/j.ijid.2014.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen SC, Yu JK, Harries AD, Bong CN, Kolola-Dzimadzi R, Tok TS, et al. Increased mortality of male adults with AIDS related to poor compliance to antiretroviral therapy in Malawi. Trop Med Int Health. 2008; 13(4): 513–519. 10.1111/j.1365-3156.2008.02029.x [DOI] [PubMed] [Google Scholar]
- 13.Hawkins C, Chalamilla G, Okuma J, Spiegelman D, Hertzmark E, Aris E, et al. Sex differences in antiretroviral treatment outcomes among HIV-infected adults in an urban Tanzanian setting. Aids. 2011; 25(9): 1189–1197. 10.1097/QAD.0b013e3283471deb [DOI] [PubMed] [Google Scholar]
- 14.Dou Z, Xu J, Jiao JH, Ma Y, Durako S, Yu L, et al. Gender difference in 2-year mortality and immunological response to ART in an HIV-infected Chinese population, 2006–2008. PLoS One. 2011; 6(8): e22707 10.1371/journal.pone.0022707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu WZ, Su LY, Xie XD, Xiang XR, Huang J, Hi P. Prevalence and Years Lived with Disability for Dental Caries among Children Aged 0–14 Years in China, 1990–2016. Biomed Environ Sci. 2018; 31(5): 376–381. 10.3967/bes2018.048 [DOI] [PubMed] [Google Scholar]
- 16.Ji N, Liu SW, Zeng XY, Dong WL, Jiang YY, Zhou MG. Disease burden for gynecological disease in China, 2016. Zhonghua Fu Chan Ke Za Zhi. 2018;53(5): 313–318. 10.3760/cma.j.issn.0529-567x.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 17.Roth GA, Johnson CO, Abate KH, Abd-Allah F, Ahmed M, Alam K, et al. The Burden of Cardiovascular Diseases Among US States, 1990–2016. JAMA Cardiol. 2018; 3(5): 375–389. 10.1001/jamacardio.2018.0385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martins-melo FR, Carneiro M, Ramos AN, Heukelbach J, Ribeiro ALP, Werneck GL. The burden of Neglected Tropical Diseases in Brazil, 1990–2016: A subnational analysis from the Global Burden of Disease Study 2016. PLoS Negl Trop Dis. 2018; 12(6): e0006559 10.1371/journal.pntd.0006559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cowan AJ, Allen C, Barac A, Basaleem H, Bensenor I, Curado MP, et al. Global Burden of Multiple Myeloma: A Systematic Analysis for the Global Burden of Disease Study 2016. JAMA Oncol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100): 1151–1210. 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.GBD 2016 Mortality Collaborators. Global, regional, and national under5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017; 390(10100): 1084–1150. 10.1016/S0140-6736(17)31833-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang F, Dou Z, Ma Y, Zhang Y, Zhao Y, Zhao D, et al. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: a national observational cohort study. Lancet Infectious Diseases. 2011; 11(7): 516–524. 10.1016/S1473-3099(11)70097-4 [DOI] [PubMed] [Google Scholar]
- 23.Liang MY, Ni C. Recognition of the imbalance of sex ratio at birth in China. Zhong Guo Ren Li Zi Yuan Kai Fa. 2018; 35(01): 112–121. [Google Scholar]
- 24.Ren Q, Zheng XY, Cao GY. A Study on Gender Differences in Death of Chinese Population in Recent 20 Years. Zhong Guo Ren Kou Ke Xue. 2005; 2005(1): 2–13. [Google Scholar]
- 25.Shang H, Xu J, Han X, Spero LJ, Arledge KC, Zhang L. HIV prevention:Bring safe sex to China. Nature. 2012; 485(7400): 576–577. 10.1038/485576a [DOI] [PubMed] [Google Scholar]
- 26.Wang X, Wang Z, Jiang X, Li R, Wang Y, Xu G, et al. A cross-sectional study of the relationship between sexual compulsivity and unprotected anal intercourse among men who have sex with men in shanghai, China. BMC Infect Dis. 2018; 18(1): 465 10.1186/s12879-018-3360-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhong F, Lin P, Xu H, Wang Y, Wang M, He Q, et al. Possible increase in HIV and syphilis prevalence among men who have sex with men in Guangzhou, China: results from a respondent-driven sampling survey. AIDS Behav. 2011; 15(5): 1058–66. 10.1007/s10461-009-9619-x [DOI] [PubMed] [Google Scholar]
- 28.Hei FX, Wang L, Qin QQ, Wang L, Guo W, Li DM, et al. Epidemic characteristics of HIV/AIDS among men who have sex with men from 2006 to 2010 in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2012; 33(1): 67–70. [PubMed] [Google Scholar]
- 29.NCAIDS, NCSTD, China CDC. Update on the AIDS/STD epidemic in China the second quarter of 2018. Chin J AIDS STD. 2018; 24(08): 755. [Google Scholar]
- 30.Wu Z, Sulkivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China's response to HIV/AIDS. Lancet. 2007; 369(9562): 679–690. 10.1016/S0140-6736(07)60315-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang F, Dou Z, Ma Y, Zhao Y, Liu Z, Bulterys M, et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Ann Intern Med. 2009; 151(4): 241–251, w-252. 10.7326/0003-4819-151-4-200908180-00006 [DOI] [PubMed] [Google Scholar]
- 32.Camara M, Dieye T, Seydi M, Diallo AA, Fall M, Diaw PA, et al. Low‐Level CD4\r, +\r, T Cell Activation in HIV‐Exposed Seronegative Subjects: Influence of Gender and Condom Use. The Journal of Infectious Diseases. 2010; 201(6): 835–842. 10.1086/651000 [DOI] [PubMed] [Google Scholar]
- 33.Delpierre C, Dray-Spira R, Cuzin L, et al. Correlates of late HIV diagnosis: implications for testing policy. International Journal of STD and AIDS. 2007; 18(5):3 12–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trepka MJ, Fennie KP, Sheehan DM, Lutfi K, Maddox L, Lieb S. Late HIV Diagnosis: Differences by Rural/Urban Residence, Florida, 2007–2011. AIDS patient care and STDs, 2014; 28(4): 188–97. 10.1089/apc.2013.0362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ailixiati N. Death Causes of AIDS and Its Impact on Life Expectancy in Yining City. Xinjiang Medical University; 2016. [Google Scholar]
- 36.Zhao HY, Wang L, Wu HJ, Zhu Q, Yang XY. Analysis of death data of HIV-infected and AIDS patients in Chuxiong Prefecture, Yunnan Province, 1996–2013. Pi Fu Bing Yu Xing Bing. 2016; 38(02): 118–121. [Google Scholar]
- 37.Jiang DD, Huang TR, Li RJ, Deng W, Huang ZB, Yu JH, et al. Retrospective analysis of AIDS deaths in Guangxi from 2004 to 2005. Ying Yong Yu Fang Yi Xue. 2014; 19(06): 340–343. [Google Scholar]
- 38.National Bureau of Statistics of China. The average life expectancy of men in China. 29 March 2019. Available from: http://data.stats.gov.cn/easyquery.htm?cn=C01&zb=A0304&sj=2018 Cited 29 March 2019.
- 39.Wang B, Li X, Barnett D, Zhao G, Zhao J, Stanton B. Risk and protective factors for depression symptoms among children affected by HIV/AIDS in rural China: a structural equation modeling analysis. Soc Sci Med. 2012; 74(9): 1435–1443. 10.1016/j.socscimed.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim MH, Mazenga AC, Yu X, Devandra A, Nguyen C, Ahmed S, et al. Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry. 2015; 15: 264 10.1186/s12888-015-0649-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim MH, Mazenga A C, Devandra A, Ahmed S, Kazembe PN, Yu X, et al. Prevalence of depression and validation of the Beck Depression Inventory-II and the Children's Depression Inventory-Short among HIV-positive adolescents in Malawi. J Int AIDS Soc. 2014; 17: 18965 10.7448/IAS.17.1.18965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Betancourt, Scorza P, Kanyanganzi F, Fawzi MC, Sezibera V, Cyamatare F, et al. HIV and Child Mental Health: A Case-Control Study in Rwanda. Pediatrics. 2014;134(2):e464–e472. Pediatrics. 2015; 135(5): 945–946. 10.1542/peds.2013-2734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.UNAIDS. UNAIDS DATA 2017. 20 July 2017. Available from:http://www.unaids.org/en/resources/documents/2017/2017_data_book Cited 29 December 2019.
- 44.Smith MK, Westreich D, Liu H, Zhu L, Wang L, He W, et al. Treatment to Prevent HIV Transmission in Serodiscordant Couples in Henan, China, 2006 to 2012. Clin Infect Dis. 2015; 61(1): 111–119. 10.1093/cid/civ200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jia Z, Mao Y, Zhang F, Ruan Y, Ma Y, Li J, et al. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003–11): a national observational cohort study. Lancet. 2013; 382(9899): 1195–1203. 10.1016/S0140-6736(12)61898-4 [DOI] [PubMed] [Google Scholar]
- 46.Chen L, Pan X, Ma Q, Yang J, Xu Y, Zheng J, et al. HIV cause-specific deaths, mortality, risk factors, and the combined influence of HAART and late diagnosis in Zhejiang, China, 2006–2013. Sci Rep. 2017; 7: 42366 10.1038/srep42366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang H, Mao Y, Tang W, Han J, Xu J, Li J. "Late for testing, early for antiretroviral therapy, less likely to die": results from a large HIV cohort study in China, 2006–2014. BMC Infect Dis. 2018; 18(1): 272 10.1186/s12879-018-3158-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The number of deaths in each age group divided by the mortality rate in each age group.
(DOCX)
Data Availability Statement
Data were extracted from the GBD 2016 (http://ghdx.healthdata.org/gbd-2016).