Abstract
Background:
Benzodiazepine misuse is a growing public health problem, with increases in benzodiazepine-related overdose deaths and emergency room visits in recent years. However, relatively little attention has been paid to this emergent problem. We systematically reviewed epidemiological studies on benzodiazepine misuse to identify key findings, limitations, and future directions for research.
Methods:
PubMed and PsychINFO databases were searched through February 2019 for peer-reviewed publications on benzodiazepine misuse (e.g., use without a prescription; at a higher frequency or dose than prescribed). Eligibility criteria included human studies that focused on the prevalence, trends, correlates, motives, patterns, sources, and consequences of benzodiazepine misuse.
Results:
The search identified 1,970 publications, and 351 articles were eligible for data extraction and inclusion. In 2017, benzodiazepines and other tranquilizers were the third most commonly used illicit or prescription drug in the U.S. (approximately 2.2% of the population). Worldwide rates of misuse appear to be similar to those reported in the U.S. Factors associated with misuse include other substance use, receipt of a benzodiazepine prescription, and psychiatric symptoms and disorders. Benzodiazepine misuse encompasses heterogeneous presentations of motives, patterns, and sources. Moreover, misuse is associated with myriad poor outcomes, including mortality, HIV/HCV risk behaviors, poor self-reported quality of life, criminality, and continued substance use during treatment.
Conclusions:
Benzodiazepine misuse is a worldwide public health concern that is associated with a number of concerning consequences. Findings from the present review have implications for identifying subgroups who could benefit from prevention and treatment efforts, critical points for intervention, and treatment targets.
Keywords: Benzodiazepines, Sedatives, Tranquilizers, Prescription Drug Misuse, Nonmedical Prescription Drug Use
1. Introduction
Benzodiazepines are a class of prescription medication that bind to the GABAA receptor, resulting in anxiolytic (anti-anxiety), hypnotic (sleep-inducing), anticonvulsant, and muscle-relaxing effects (see Table 1 for a list of commonly prescribed benzodiazepines). They are among the most commonly prescribed psychiatric medications (Moore and Mattison, 2017), with more than 1 in 20 people in the U.S. filling a prescription each year (Bachhuber et al., 2016). They are also the third most commonly misused illicit or prescription substance among adults and adolescents in the U.S. (Center for Behavioral Health Statistics and Quality [CBHSQ], 2018b; Johnston et al., 2018).
Table 1.
Common Types of Benzodiazepines
| Generic Name | Brand Name | Onset of Effect | Dose Equivalents (mg) |
|---|---|---|---|
| alprazolam | Xanax | fast/intermediate | 0.5 |
| chlordiazepoxide | Librium | intermediate | 25 |
| clonazepam | Klonopin | intermediate | 0.5 |
| clorazepate | Tranxene | intermediate | 15 |
| diazepam | Valium | fast | 10 |
| estazolam | ProSom | slow | 2 |
| flunitrazepam | Rohypnol | fast | 1 |
| flurazepam | Dalmane | fast | 20 |
| lorazepam | Ativan | fast | 1 |
| midazolam | Versed | fast | 15 (IV) |
| oxazepam | Serax | slow | 20 |
| quazepam | Doral | slow | 20 |
| temazepam | Restoril | intermediate | 20 |
| triazolam | Halcion | fast | 0.5 |
Note: Dose equivalents are estimates. Onset definitions: slow = 15–30 minutes, intermediate = 30–60 minutes, slow = 60–120 minutes. Sources: (Ashton, 2005; Bisaga and Mariani, 2015)
Several trends indicate a growing public health problem related to benzodiazepines. Most notably, benzodiazepine-related overdose deaths increased by more than 400% from 1996–2013 (Bachhuber et al., 2016) and emergency department visits for benzodiazepines increased by more than 300% from 2004 to 2011 (Jones and McAninch, 2015). These increases have occurred concurrently with rising rates of benzodiazepine prescribing. The number of benzodiazepine prescriptions not only increased 67% from the mid-1990s to 2013, but the quantity (i.e., dose equivalents) increased more than 3-fold over this time period (Bachhuber et al., 2016). The proportion of people with an opioid analgesic prescription who were also prescribed a benzodiazepine increased 41% from 2002 to 2014 (Hwang et al., 2016), despite evidence that concomitant opioid and benzodiazepine prescriptions increase risk of overdose (Sun et al., 2017). Indeed, the use and misuse of benzodiazepines has contributed substantially to the current opioid overdose epidemic, with benzodiazepines involved in nearly 30% of opioid overdose deaths in 2015 (National Institute on Drug Abuse, 2018). New concerns continue to emerge, such as the increasing availability of highly lethal benzodiazepines on the illicit market (e.g., illicitly produced pills that combine benzodiazepines with fentanyl and potent “designer” benzodiazepines) (Hoiseth et al., 2016; Huppertz et al., 2018).
Despite the worsening public health indicators associated with benzodiazepine use, this issue remains overlooked by policymakers and the scientific community (Lembke et al., 2018). This may be partly attributable to the low perceived risk associated with benzodiazepines (Assanangkornchai et al., 2010; Quintero, 2012). In the U.S., benzodiazepines are classified as a Schedule IV controlled substance, which indicates relatively low risk for misuse, consistent with its regulation in most Western countries, East Asia, and Southeast Asia. Although benzodiazepines were initially believed to have minimal risk for misuse, evidence indicates that benzodiazepines have misuse potential, particularly in certain vulnerable subgroups, such as people with a history of substance use disorders (SUDs) (Griffiths and Weerts, 1997; Licata and Rowlett, 2008).
A better understanding of benzodiazepine misuse is needed to inform research on its prevention and treatment, and to mitigate the growing harms of this problem. The aim of this manuscript is to: (1) provide a comprehensive review and synthesis of the literature on the epidemiology of benzodiazepine misuse, and (2) to identify key next steps in the study of benzodiazepine misuse.
2. Methods
2.1. Search Strategy and Scope of the Review
We searched the PubMed and PsycINFO databases through February 2019 to identify peer-reviewed publications on the epidemiology of benzodiazepine misuse. Peer-reviewed publications were included if they examined issues relevant to the epidemiology of benzodiazepine misuse, including: Prevalence, trends, correlates, sources, patterns, motives, and consequences. International research was included in the present review; however, prevalence estimates primarily reflect data collected in the U.S. due to the limited availability of epidemiological data outside of the U.S. Accordingly, recent government publications using data from population-based surveys (e.g., National Survey on Drug Use and Health [NSDUH], Monitoring the Future [MTF]) and treatment settings (e.g., Treatment Episode Data Set [TEDS]) in the U.S. were included in the present review.
All methods were carried out in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA; Moher et al., 2015). See Supplementary Materials for additional details on methods, including search terms, inclusion criteria, and data extraction methods.
2.2. Definitions
The field has not reached a consensus about how to define the problematic use of prescription medications (e.g., use without a prescription, use in ways other than prescribed, use to get high, etc.), or the appropriate term to characterize problematic prescription medication use (e.g., nonmedical prescription drug use, prescription drug misuse, prescription drug abuse). In this review, we use the term misuse to broadly encompass any use of a prescription medication without a prescription, at a higher frequency or dose than prescribed, or for the feelings of the drug rather than its medical indication. The terms sedative, hypnotic or anxiolytic abuse, dependence, or use disorder (referred to as SHA abuse, dependence, or use disorder throughout the manuscript) refer to Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association, 2000) or International Statistical Classification of Diseases and Related Health Problems (ICD; World Health Organization, 1992) diagnoses.
Many studies reviewed utilize surveys combining benzodiazepines with other sedatives, tranquilizers, anxiolytics, and hypnotics. See Table 2 for characteristics of U.S. general population surveys included in the present review, including specific medications included in broader prescription drug categories, such as sedatives and tranquilizers. We will use the terms sedatives and tranquilizers when reporting prevalence data extracted from these general population surveys. Elsewhere, to balance accuracy with ease of interpretation, we use the term “benzodiazepines” to refer both to studies of benzodiazepines exclusively and in combination with other sedatives/tranquilizers.
Table 2.
Characteristics of U.S. Nationally-Representative Surveys Utilized in the Present Review
| Survey | Years Administe red |
Overview of Sample | Definition of Misuse/Nonmedi cal Use | Tranquili zers Specified |
Sedatives Specified |
|
|---|---|---|---|---|---|---|
| Monitori ng the Future (MTF) | 12th graders: 1975- present (annually) 8th & 10th graders: 1991- present (annually) |
|
“Use on your own—that is, without a doctor telling you to take them.” | Librium, Valium, Xanax |
Prior to 2004 (barbiturat es): barbiturates, downs/dow ners, goofballs, yellows, reds, blues, rainbows 2004 to present (sedatives/ barbiturate s): barbiturates, downs/dow ners, phenobarbit al, Ambien, Lunesta, Sonata, Tuinal, Nembutal, Seconal |
|
| National Comorbi dity Survey (NCS) |
Baseline interview: 1990–1992 |
|
“Use on your own; that is, either: One, without a doctor’s prescription, or Two, in greater amounts than prescribed, or Three, more often than prescribed, or Four, for any reasons other than a doctor said you should take them--such as for kicks, to get high, to feel good, or curiosity about the pill’s effect.” | Librium, Valium, Ativan, Meproba mate, “Nerve Pills” |
Barbiturates , Sleeping Pills, Seconal, “Downers” | |
| National Epidemi ologic Survey on Alcohol and Related Conditio ns (NESA RC) |
Wave 1: 2000–2001 Wave 2 (follow-up survey of Wave 1 respondent s): 20042005 |
|
“Use without a doctor’s prescription; in greater amounts, more often, or longer than prescribed; or for a reason other than a doctor said you should use them.” | Librium, Muscle relaxants, Valium, Xanax |
Barbiturates , Chloral Hydrate, Quaaludes, Seconal, Sleeping pills |
|
| National Epidemi ologic Survey on Alcohol and Related Conditio ns-III (NESA RC-III) |
2012–2013 |
|
“Use without a doctor’s prescription; in greater amounts, more often, or longer than prescribed; or for a reason other than a doctor said you should use them.” |
NESARC-III assessed sedatives and tranquilizers in combination: Alprazolam, Alurate, Amobarbital, Amytal, Aprobarbital, Aqualude, Atarax, Ativan, Barbital, Barbiturates, Benzodiazepines, Bromides, Butalbital, Butisol, Buticaps (Butisol Caps), Carbrital, Carbromal, Carisoprodol, Centrax, Chloral Hydrate, Chlordiazepoxide, Chlordiaz/clid, Chlordiazep, Cibas, Clonazepam, Clorazepate, Dalmane, Deprol, Desbutal, Diazepam, Dilantin, Doriden, Durrax, Equanil, Eskabarb, Estazolam, Ethchlorvynol, Flurazepam, Glutethimide, Halcion, Hydroxyzine, Lenetran, Libritabs, Librium, Lorazepam, Ludes, Luminal, Mebaral, Melzone, Meprobamate, Meprospan, Methaqualone, Methyprylon, Miltown, Mysoline, Nembutal, Nitrazepam, Noctec, Noludar, Octinox, Oxazepam, Paraldehyde, Parest, Paxipam, Pentobarbital, Pentothal, Phenergan, Phenobarbital, Placidyl, Prazepam, Primidone, Promethazine, Quaalude, Restoril, Secobarbital, Seconal, Seldane, Serax, SK- Lygen, Soma, Sopor, Taractan, Temazepam, Transpoise, Tranxene, Trepidome, Triazolam, Tuinal, Valium, Valmid, Vanadom, Veronal, Vistaril, Xanax |
||
| National Survey on Drug Use and Health (NSDU H) |
1971- present (annually) |
|
Prior to 2015: “Your use of a drug if the drug was not prescribed for you, or if you took the drug only for the experience or feeling it caused.” 2015-present: “Use in any way not directed by a doctor, including use without a prescription of one’s own; use in greater amounts, more often, or longer than told to take a drug; or use in any other way not directed by a doctor.” |
Alprazola m, Ativan, Buspirone, Clonazepa m, Cyclobenz aprine (also known as Flexeril), Diazepam, Hydroxyzi ne, Klonopin, Lorazepa m, Meprobam ate, Soma, Valium, Xanax |
Ambien, Butisol, Zolpidem, Flurazepa m (also known as Dalmane), Halcion, Lunesta or eszopiclon e, Phenobarbi tal, Restoril, Sonata or zaleplon, Seconal, Temazepa m, Triazolam |
|
3. Results
3.1. Search Results
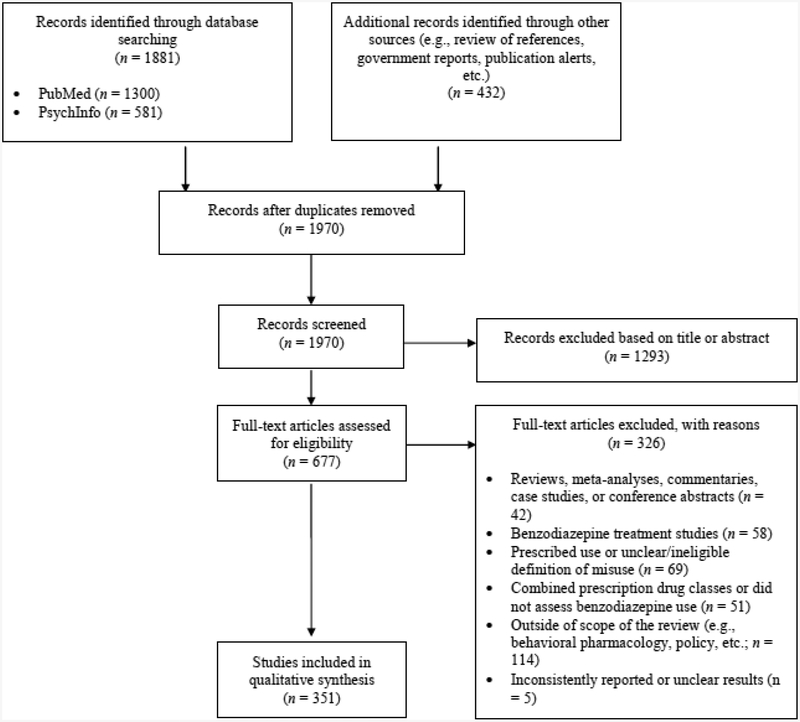
Results of the search are presented in Figure 1. Our search strategy yielded 1,970 unique records, of which 351 were included in the present review. Of the 677 full-text manuscripts that were assessed for eligibility, 326 were excluded. Reasons for exclusion include the following: topic outside of the scope of the review (n=114); focus on use as prescribed or unclear/ineligible definition of misuse (n=69); treatment outcome study (n=58); combined prescription drug classes or did not assess benzodiazepine misuse (n=51); review, meta-analysis, commentary, case study, or conference abstract (n=42); and inconsistently reported or unclear results (n=5). Of the studies included in the present review, 14 were published prior to 1990 (the oldest study being published in 1975), 57 were published between 1990–1999, 95 were published between 2000–2009, and 185 were published between 2010–2018. Data from 179 studies were collected in the U.S., 77 from Western Europe, 35 from Australia, 23 from Canada, 17 from East Asia, 9 from Israel, 6 from other regions (e.g., Brazil, India, Nepal, and Poland), and 5 studies did not specify location.
Figure 1.
Flow diagram of records identified, screened, and included.
Note: Records could be excluded for multiple reasons.
3.2. Prevalence and Trends
3.2.1. U.S. Statistics.
Data from the 2017 NSDUH indicate that approximately 6 million U.S. citizens ages 12 and older (approximately 2.2% of the population) misused tranquilizers in the previous year, making tranquilizers the third most commonly misused illicit substance following marijuana (15%) and prescription opioids (4.1%). Prevalence rates for past-year tranquilizer misuse were nearly identical to those reported for cocaine use. Additionally, approximately 1.4 million people (0.5%) misused sedatives in the previous year.
Although tranquilizers are among the most commonly misused drug types, tranquilizer use disorder was only the fifth most common illicit drug use disorder. An estimated 739,000 people met criteria for a tranquilizer use disorder (0.3% of U.S. population). Notably, this estimate is slightly higher than the estimate for heroin use disorder. Approximately 198,000 individuals met criteria for a sedative use disorder (0.1%), making sedative use disorder the second least common SUD (the least common being inhalant use disorder). This discrepancy between a relatively high prevalence of misuse but low prevalence of use disorders is consistent with an analysis of National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data indicating that few individuals with sedative/tranquilizer misuse meet criteria for a sedative/tranquilizer use disorder at a 3-year follow-up, with most discontinuing misuse over that time (Boyd et al., 2018). Among individuals with opioid use disorder (OUD), conditional dependence, or the percentage of people with misuse who meet criteria for dependence, for benzodiazepines is lower than for other substances (Wu et al., 2012).
Despite increases in benzodiazepine prescribing over the past decade (Bachhuber et al., 2016), prevalence estimates for sedative/tranquilizer misuse and use disorder have remained relatively stable among both adolescents and adults in the U.S. (CBHSQ, 2015a, 2018b; Johnston et al., 2018; Palamar et al., 2019), including among those with opioid misuse (Boggis et al., 2019) (see Supplementary Materials for data on trends prior to the previous decade). Yet, overdose deaths and emergency room visits involving benzodiazepines have increased (Cai et al., 2010; Day, 2013; Jones and McAninch, 2015). SUD treatment admissions for benzodiazepines as a primary substance more than doubled from 2005 to 2011, but have decreased somewhat through 2015 (8,163 in 2004, 18,855 in 2011, 14,000 in 2015; CBHSQ, 2017). This pattern may reflect increasing polysubstance use, with benzodiazepines being combined with other substances. Indeed, 82.1% of all SUD treatment admissions related to benzodiazepines are for benzodiazepines as a secondary substance of use (CBHSQ, 2011), and treatment admissions involving both benzodiazepines and opioid analgesics increased 570% from 2000 to 2010 (CBHSQ, 2012).
3.2.2. International Statistics.
As previously noted, limited population-based data on the prevalence of benzodiazepine misuse is available for countries outside of the U.S. Available data from countries outside of the U.S. suggest that rates of misuse are similar to those reported in the U.S. For example, a 2008–2009 general population survey of over 20,000 individuals ages 15 to 64 in Sweden found that 2.2% of participants misused benzodiazepines and other sedatives in the previous year (Abrahamsson and Hakansson, 2015). The same rate of current benzodiazepine misuse was found in a 2008–2009 household survey of 2,280 individuals ages 15 and older residing in the Ubon Ratchathani Province region of Thailand (Puangkot et al., 2010). Yet, a nationwide survey of 26,633 general population respondents across Thailand (ages 12–65) found a slightly lower prevalence of misuse, with approximately 1% reporting the misuse of anxiolytic and hypnotics in the previous year (Assanangkornchai et al., 2010). Similar rates of past-year misuse (approximately 1–2%) have been reported in general population samples in Brazil (Galduróz et al., 2005) and Australia (Hall et al., 1999). Although few studies outside of the U.S. have examined trends in misuse, a nationwide study of 179,114 school-age respondents (14 to 18 years old) in Spain found that the prevalence of tranquilizer, sedative, and sleeping pill misuse increased from 2.4% in 2004 to 3.0% in 2014 (Carrasco-Garrido et al., 2018).
Worldwide rates of SHA use disorder are also similar to those reported in the U.S. In the same study referenced above conducted in the Ubon Ratchathani Province region of Thailand, 0.6% of respondents met criteria for DSM-IV benzodiazepine abuse and 0.2% of respondents met criteria for dependence (Puangkot et al., 2010). An older survey of 10,641 adult respondents in Australia conducted in 1997 found that 0.4% of respondents met criteria for benzodiazepine and other sedative dependence (Hall et al., 1999). Although international rates of benzodiazepine misuse and SHA use disorder are similar to those reported in U.S. general population surveys, there is significant variability in methods across these surveys (e.g., definitions of misuse, categorization of prescription drug classes). Consistent definitions of benzodiazepine misuse are needed to determine cross-national differences in the prevalence of misuse, as well as the impact of benzodiazepine availability and regulations on misuse.
3.3. Correlates and Risk Factors for Benzodiazepine Misuse
An overview of findings on sociodemographic correlates of benzodiazepine misuse is presented in Table 3. The findings on substance use and psychiatric correlates of benzodiazepine misuse presented below have been replicated in numerous samples; details and further citations in support of these findings are included in Supplementary Materials.
Table 3.
Findings on Sociodemographic Correlates of Benzodiazepine Misuse
| Population | Finding | References |
|---|---|---|
| Age | ||
| General population samples in the U.S. | Younger age (e.g., < 25) was associated with benzodiazepine misuse | (Arterberry et al., 2016; Blanco et al., 2018; Fenton et al., 2010; Ford et al., 2018; Goodwin and Hasin, 2002; Huang et al., 2006; Maust et al., 2018; McCabe et al., 2006a) |
| General population samples outside of the U.S. | Older age was associated with benzodiazepine misuse | (Assanangkornchai et al., 2010; Schneider et al., 2015) |
| Adolescents/young adults in the U.S. | ||
| No association between age and benzodiazepine misuse | (Boyd et al., 2015) | |
| Adults with opioid misuse/SUDs/injection drug use | ||
| No association between age and benzodiazepine misuse | (Apantaku-Olajide et al., 2012; Bleich et al., 1999; Bleich et al., 2002; de Wet et al., 2004; Dobbin et al., 2003; Eiroa-Orosa et al., 2010; Lavie et al., 2009; Malcolm et al., 1993; McHugh et al., 2018; McHugh et al., 2017; Moses et al., 2018; Schuman-Olivier et al., 2013; Stein et al., 2017b) | |
| Gender | ||
| General population samples in the U.S. | ||
| No association between gender and benzodiazepine misuse | (Blanco et al., 2013; Ford et al., 2018; Huang et al., 2006) | |
| General population samples outside of the U.S. | ||
| No association between gender and benzodiazepine misuse | (Hall et al., 1999) | |
| Adolescents/young adults in the U.S. | ||
| No association between gender and benzodiazepine misuse | (Boyd et al., 2015; Boyd et al., 2006; Ford, 2008b, 2009; McCabe et al., 2007a; McCabe et al., 2017a; Pickover et al., 2016; Shadick et al., 2016) | |
| Adolescents/young adults outside of the U.S. | Women were at greater risk of benzodiazepine misuse | (Carrasco-Garrido et al., 2018; Currie and Wild, 2012; Kokkevi et al., 2008) |
| Adults with opioid misuse/SUDs/injection drug use | ||
| No association between gender and benzodiazepine misuse | (Bawor et al., 2015; Bleich et al., 1999; Boggis et al., in press; Darke et al., 1994a; Davies et al., 1996; Eiroa-Orosa et al., 2010; Ghitza et al., 2008; Hearon et al., 2011; Ickowicz et al., 2015; McHugh et al., 2018; McHugh et al., 2017; Moitra et al., 2013; Mulvaney et al., 1999; Ng et al., 2007; Peles and Adelson, 2006; Peles et al., 2009; Perera et al., 1987; Schiff et al., 2007; Schuman-Olivier et al., 2013; Shand et al., 2011) | |
| Race/Ethnicity1 | ||
| General population samples in the U.S. | ||
| No association between race/ethnicity and benzodiazepine misuse | (Maust et al., 2018) | |
| Adolescents/young adults in the U.S. | ||
| “Other” racial/ethnic identity was associated with benzodiazepine misuse, as compared to Black and Hispanic identities | (McCabe et al., 2017b) | |
| Adolescents/young adults outside of the U.S. | Aboriginal racial/ethnic identity was associated with benzodiazepine misuse, as compared to non-Aboriginal identities | (Currie and Wild, 2012) |
| Adults with opioid misuse/SUDs/injection drug use | ||
| No association between race/ethnicity and benzodiazepine misuse | (Bleich et al., 2002; Ickowicz et al., 2015; Moitra et al., 2013) | |
| Other subgroups (e.g., men who have sex with men, adults with HIV, adults in the club drug scene) | ||
| No association between race/ethnicity and benzodiazepine misuse | (Kelly et al., 2015a) | |
| Sexual Identity | ||
| General population samples in the U.S. | Sexual minority groups were more likely to misuse benzodiazepines, as compared to those with heterosexual identities | (Cochran et al., 2004) |
| Adolescents/young adults in the U.S. | Sexual minority groups were more likely to misuse benzodiazepines, as compared to those with heterosexual identities | (Dagirmanjian et al., 2017; McCabe, 2005; Shadick et al., 2016) |
| Adolescents/young adults outside of the U.S. | Sexual minority groups were more likely to misuse benzodiazepines, as compared to those with heterosexual identities | (Li et al., 2018) |
| Other subgroups (e.g., men who have sex with men, adults in the club drug scene) | ||
| Gay sexual identity was associated with lower risk of benzodiazepine misuse, as compared to hetero- or bi-sexual identities | (Kecojevic et al., 2015c) | |
| Other Sociodemographic Factors | ||
| General population samples in the U.S. (adults and young adults/adolescents) | Lower levels of education, lower income, unemployment, and being unmarried were associated with benzodiazepine misuse | (Arterberry et al., 2016; Becker et al., 2007; Blanco et al., 2018; Goodwin and Hasin, 2002; Huang et al., 2006; McCabe et al., 2018; Schepis et al., 2018a) |
| Adults with opioid misuse/SUDs/injection drug use | ||
| No association between homelessness, marital status, employment status, level of education, income, and benzodiazepine misuse | (Bouvier et al., 2018; Brands et al., 2008; Fry and Bruno, 2002; Ghitza et al., 2008; Mateu-Gelabert et al., 2017; McHugh et al., 2018; McHugh et al., 2017; Rooney et al., 1999; Williams et al., 1996) | |
Note: References included in the table do not represent an exhaustive list of studies examining sociodemographic correlates of benzodiazepine misuse. Instead, this table provides an overview of the main findings.
The vast majority of studies examining racial/ethnic identity as a correlate of benzodiazepine misuse have been conducted in the U.S., and therefore racial/ethnic minority status refers to U.S. demographics.
3.3.1. Age.
Benzodiazepine misuse is most common in young adults. According to data from the 2015–2016 NSDUH, the highest past-year rates of combined sedative/tranquilizer misuse were observed among 18 to 25-year-olds (5.8%), followed by 26 to 34-year-olds (4%) (Schepis et al., 2018b). In the U.S., the typical age of onset of benzodiazepine misuse is during early adulthood (i.e., 18–25 years) (Boyd et al., 2018; McCabe et al., 2007b), and the average age of onset for SHA use disorder is the early-to-late 20s (Conrod et al., 2000; Huang et al., 2006). In this section, we provide a brief overview of benzodiazepine misuse across the developmental spectrum.
Estimates of benzodiazepine misuse are highly variable between general population samples in the U.S. and student-based samples, making it difficult to ascertain the impact of benzodiazepine misuse in this age group. According to 2016 NSDUH data, <2% of adolescents ages 12 to 17 reported past-year combined sedative/tranquilizer misuse and 2.3% reported lifetime misuse (Schepis et al., 2018b). However, estimates from the MTF survey are more than twice as high, and indicate that more than 5.5% of 8th, 10th, and 12th graders reported lifetime tranquilizer misuse in 2017 (Johnston et al., 2018). These prevalence rates are comparable to those reported among a sample of approximately 85,000 secondary school students in European countries (Kokkevi et al., 2008). Similarly, in a national sample of 10,904 college students in the U.S., 7.8% reported lifetime benzodiazepine misuse, 4.5% reported past-year misuse, and 1.6% reported past-month misuse (McCabe, 2005).
High rates of benzodiazepine misuse among adolescents and young adults are particularly concerning given that younger age of benzodiazepine misuse onset is associated with greater risk for and more rapid development of SHA disorder (Chen et al., 2009; McCabe et al., 2007b). The transition to college may be a particularly risky time; a study of college sophomores found a 102.9% increase in the prevalence of misuse from pre-college – one of the greatest rates of increase among all substances during this time period (Arria et al., 2008).
Little is known about benzodiazepine misuse in older adults, despite high rates of prescribing in this group (Maust et al., 2018; Schepis et al., 2018b). Rates of tranquilizer and sedative misuse are lower in adults over the age of 50, as compared to younger age groups (Maust et al., 2018; Schepis et al., 2018b), and are lower than rates of prescription opioid misuse in this age group (Blazer and Wu, 2009). Yet, the prevalence of lifetime and past-year tranquilizer misuse increased among this age group from 2002–2003 to 2012–2013 (from 4.5% to 6.6% and 0.6% and 0.9%, respectively; Schepis and McCabe, 2016). In addition, the proportion of individuals with past-year tranquilizer misuse who are over the age of 50 doubled from 2005–2006 to 2013–2014 (from 7.9% to 16.5%; Palamar et al., 2019). Benzodiazepine misuse and dependence appears to be more common among older adults with a prescription or who are treated in psychiatric settings (Landreat et al., 2010; Voyer et al., 2009; Yen et al., 2015).
3.3.2. Gender.
In 2017, women and men over the age of 12 in the U.S. reported similar rates of tranquilizer misuse (2.1% vs. 2.3%, respectively) (CBHSQ, 2018b). Indeed, studies among adults and adolescents in the U.S. have not demonstrated consistent gender differences in the prevalence of benzodiazepine misuse (Table 3). In contrast, research in countries outside of the U.S. has generally demonstrated a greater likelihood of benzodiazepine misuse and SHA use disorder amongst female adolescents and adults (Table 3).
Analyses of gender differences in benzodiazepine prevalence from the same datasets (e.g., NSDUH) have, at times, yielded different results, suggesting that gender differences are likely modest and may be impacted substantially by factors such as sample size, covariates, and methodological variations across studies. For example, several studies controlling for history of a benzodiazepine prescription have identified higher misuse rates (Fenton et al., 2010; Maust et al., 2018) and higher likelihood of developing a use disorder among men (Lev-Ran et al., 2013). This is consistent with data from approximate 85,000 high school students across Europe, in which gender moderated the association between having a prescription and misuse, such that exposure via prescription increased the likelihood of misuse more in boys than girls (Kokkevi et al., 2008). Furthermore, a recent analysis of NSDUH data found that males between the ages of 18–49 had lower odds of benzodiazepine misuse than females, whereas there was no association between gender and benzodiazepine misuse at younger (12–17 years) and older age ranges (50 years and older) (Schepis et al., 2018b). These findings illustrate that gender differences in misuse might vary according to prescription status and age. Nevertheless, the comparable prevalence between men and women in the U.S. and higher rates of misuse among women outside of the U.S. is in contrast to many other substances (e.g., heroin, marijuana), for which prevalence is generally higher in men (CBHSQ, 2018b).
3.3.3. Race/Ethnicity.
Nearly all studies examining the associations between race/ethnicity and benzodiazepine misuse indicate that misuse is more common among people who identify their race/ethnicity as Non-Hispanic White (Table 3). Nonetheless, in the 2017 NSDUH, rates of misuse for those with multiple racial/ethnic identities were nearly identical to those reported by Non-Hispanic Whites for both tranquilizers and sedatives (2.6% and 0.5%, respectively, for those with multiple racial/ethnic identities vs. 2.6% and 0.6% for Non-Hispanic Whites) (CBHSQ, 2018b). Furthermore, the proportion of individuals with past-year tranquilizer misuse who reported a racial/ethnic minority identity increased from 2005–2006 to 2013–2014 (Palamar et al., 2019).
Many studies on this topic combine heterogeneous racial/ethnic minority groups (e.g., Non-Hispanic Asian, Native American, multiple racial ethnic identities) into one “other” racial/ethnic category, which is a significant limitation of this literature. In addition, few studies control for access to benzodiazepines via legitimate prescription, despite findings that people identifying as Non-Hispanic White are more likely to be prescribed benzodiazepines (Cook et al., 2018; Olfson et al., 2015). In one U.S. general population study of individuals who had ever received an anxiety medication prescription, odds of lifetime benzodiazepine misuse were higher for Non-Hispanic White adults, as compared to Black adults (Fenton et al., 2010). Looking at this question in a different way, a recent general population study comparing people who reported only using benzodiazepine as prescribed to people who reported misuse did not find an effect of racial/ethnic identity (Maust et al., 2018).
3.3.4. Other Sociodemographic Correlates.
Large-scale studies across several subgroups indicate that sexual minority groups are more likely to misuse benzodiazepines (Table 3). However, this has not been replicated in some smaller studies among specific populations (e.g., young adults using club drugs). Studies examining other sociodemographic correlates of benzodiazepine misuse (e.g., employment status, housing status, etc.) are less consistent and appear to diverge between general population studies and samples of people with SUDs (Table 3). In population-based studies, lower levels of education, lower income, unemployment, and being unmarried are generally associated with benzodiazepine misuse. Yet, findings in samples of people with SUDs are equivocal.
3.3.5. Substance Use.
People with SUDs, particularly OUD, have much higher rates of benzodiazepine misuse than the general population. Analyses of 2008–2014 NSDUH data found that adults with OUD had a rate of combined sedative/tranquilizer misuse that was approximately 20 times greater than the U.S. general population, with 43% reporting past-year sedative/tranquilizer misuse (Votaw et al., 2019). Benzodiazepine misuse is often even more prevalent among people in treatment for OUD; past-month estimates range from 7–73%, with a majority (67%) of studies reviewed reporting rates greater than 40% (Apantaku-Olajide et al., 2012; Bleich et al., 2002; Darke et al., 1993, 1994b; Eiroa-Orosa et al., 2010; Franklyn et al., 2017; Gelkopf et al., 1999; Ghitza et al., 2008; Gilchrist et al., 2006; Lavie et al., 2009; McHugh et al., 2017; Metzger et al., 1991; Millson et al., 2006; Moitra et al., 2013; Naji et al., 2016; Peles et al., 2009, 2010; Stein et al., 2017b; Stein et al., 2016; Vogel et al., 2013; Wu et al., 2010).
The prevalence of benzodiazepine misuse has been understudied among individuals with alcohol use disorder (AUD), despite evidence that alcohol use and AUD increase risk of benzodiazepine misuse (Becker et al., 2007; Goodwin and Hasin, 2002; Huang et al., 2006; McCabe et al., 2006a), and that alcohol contributes to benzodiazepine-related overdoses (Jones et al., 2014). An analysis of 2008–2014 NSDUH data found that approximately 7.6% of those with AUD, including those with DSM-IV alcohol abuse or dependence, reported past-year sedative/tranquilizer misuse, a rate 3–4 times greater than among the U.S. general population (Votaw et al., 2019). Rates of misuse might be higher among those with greater AUD severity, as evidenced by an analysis of NSDUH data wherein approximately 12% of those with DSM-IV alcohol dependence reported past-year sedative/tranquilizer misuse (Hedden et al., 2010). Indeed, studies of people with AUD in treatment demonstrate even higher rates, with estimates of recent benzodiazepine misuse (self-reported past-month use or urine drug screen results) ranging from 19–40% (McHugh et al., 2018; Morel et al., 2016; Ogborne and Kapur, 1987; Ross, 1993).
Benzodiazepine misuse is also common (i.e., >50% over study periods ranging from the past month to participants’ lifetimes) among those with illicit drug use (e.g., cocaine, amphetamines) and/or prescription drug misuse (Darke et al., 1994a; Havens et al., 2010; Kecojevic et al., 2015c; Kelly and Parsons, 2007; Kurtz et al., 2011; Lankenau et al., 2007; Lankenau et al., 2012b; Roy et al., 2018) and those in SUD treatment settings (Beary et al., 1987; Murphy et al., 2014; Pattanayak et al., 2010; Wolf et al., 1989). This is consistent with data that other substance use is consistently associated with benzodiazepine misuse in numerous populations, and that benzodiazepine misuse is associated with greater substance use severity cross-sectionally and prospectively (see Supplementary Materials). In fact, benzodiazepine misuse increases with the overall level of polysubstance use (McHugh et al., 2018; Schuman-Olivier et al., 2013; Votaw et al., 2019). Benzodiazepine misuse is strongly associated with risk for other prescription drug misuse and use disorders, particularly prescription opioid misuse and OUD (Blanco et al., 2018; Boggis et al., 2019; Han et al., 2017; Han et al., 2015; Huang et al., 2006; Jones and McCance-Katz, 2019; Jones, 2017; Maust et al., 2018). This co-occurrence is so common that a factor analysis indicated that prescription drug use disorders reflect a single latent factor (Blanco et al., 2013).
3.3.6. Psychiatric Comorbidity and Affective Vulnerabilities.
Greater psychiatric symptoms and psychiatric disorders, particularly anxiety and mood disorders, are associated with both benzodiazepine misuse and SHA use disorder in large epidemiological studies among adults (Abrahamsson and Hakansson, 2015; Goodwin and Hasin, 2002; Huang et al., 2006; Martins and Gorelick, 2011; Rigg and Ford, 2014) and adolescents (Boyd et al., 2015; Schepis and Krishnan-Sarin, 2008; Zullig and Divin, 2012). This finding has been replicated across heterogeneous populations (see Supplementary Materials). The few studies that have examined personality disorders have also demonstrated a strong association with benzodiazepine misuse (see Supplementary Materials)9.
There are few longitudinal studies addressing this topic; thus, causality and temporality remain largely unknown. In a study across the two waves of the NESARC, lifetime history of benzodiazepine misuse was associated with risk for onset of psychiatric disorders three years later (Schepis and Hakes, 2011), with evidence that higher frequency of misuse was associated with increased risk of incident mood or anxiety disorders (Schepis and Hakes, 2013). Earlier age of onset of major depressive disorder has been associated with higher likelihood of a SHA use disorder (Schepis and McCabe, 2012).
Although not consistently studied, several studies examining gender as a moderator of the association between symptoms of anxiety and/or depression and benzodiazepine misuse have found a stronger association among women than men (Hearon et al., 2011; McHugh et al., 2018; McHugh et al., 2017; Zullig and Divin, 2012). Analysis of a large general population sample in the U.S. found that the association between anxiety disorders and SHA use disorder was stronger among women relative to men; however, the association between panic disorder without agoraphobia and sedative dependence was higher among men (Conway et al., 2006). Findings that gender moderates the association between psychiatric disorders/vulnerabilities and benzodiazepine misuse are consistent with data suggesting that women are more likely than men to misuse benzodiazepines to cope with negative affect (Boyd et al., 2015; Kokkevi et al., 2008; McCabe et al., 2009; McCabe and Cranford, 2012; McLarnon et al., 2014; Terry-McElrath et al., 2009).
3.3.7. Receipt of a Benzodiazepine Prescription.
One of the most consistent correlates of benzodiazepine misuse is the receipt of a benzodiazepine prescription. Population-based data in the U.S. indicate that those with any prescription anxiety medication have 1.9 times greater odds of past-year benzodiazepine misuse and 2.6 times greater odds of SHA use disorder (Fenton et al., 2010), a finding that has been replicated in numerous populations (see Supplementary Materials)). There is some evidence that people diagnosed with a condition for which benzodiazepines are commonly prescribed (e.g., anxiety, insomnia) are more sensitive to the reinforcing effects of benzodiazepines (Helmus et al., 2005). Nonetheless, previous studies indicate that benzodiazepine prescriptions are independently associated with greater odds of misuse, even after controlling for psychiatric disorders and anxiety/depression symptoms (Boyd et al., 2015; Fenton et al., 2010). Earlier age of prescription initiation (Austic et al., 2015; McLarnon et al., 2011), longer duration of prescription use (Boyd et al., 2015), and greater frequency of prescription use (McCabe et al., 2011a) are associated with greater odds of benzodiazepine misuse.
Misuse of one’s own prescription might occur without knowledge that such behavior comprises misuse, as evidenced by findings that using a greater dose than prescribed for therapeutic purposes is the most common form of misuse (as opposed to taking a greater dose to get high or to modify other drug effects) among those with benzodiazepine prescriptions (Ladewig and Grossenbacher, 1988; McCabe et al., 2011a; McLarnon et al., 2011). There are also studies suggesting that some individuals, particularly those with illicit drug use, intentionally seek out benzodiazepine prescriptions for the purpose of misusing (Ibanez et al., 2013; Mateu-Gelabert et al., 2017; Ross et al., 1996).
3.4. The How and Why of Benzodiazepine Misuse: Sources, Patterns, and Motives
Many findings reported below have been replicated in numerous populations; further support for these findings is included in Supplementary Materials).
3.4.1. Sources.
Benzodiazepines that are misused are obtained from a variety of sources, such as diversion from friends and family members with a prescription, prescriptions from a doctor (or multiple doctors), and purchase through an illicit source (CBHSQ, 2018b). Receiving diverted medications from friends and family members is the most common source of benzodiazepines (CBHSQ, 2018b; Inciardi et al., 2010; McCabe and Boyd, 2005; McCabe and West, 2014); 64.4% of NSDUH respondents with past-year tranquilizer misuse most recently received tranquilizers from friends or family members. Over 80% of these participants reported that their friend or family member had obtained the medication via a prescription from a doctor (CBHSQ, 2018b). Although limited, data indicate that over 20% of adolescents and adults with a benzodiazepine prescription have diverted their medications (Boyd et al., 2007; McCabe et al., 2011b; McLarnon et al., 2011).
Misuse of one’s own benzodiazepine prescription is common across heterogenous populations, including both substance-using and general population samples of adults and adolescents (see Supplementary Materials). Notably, individuals misusing their own prescription are more likely to report frequent misuse and greater benzodiazepine use severity, as compared to those who receive benzodiazepines from friends or family (Ford and Lacerenza, 2011; McCabe et al., 2018; Stein et al., 2016). Adults with more severe substance use presentations also commonly report obtaining benzodiazepines from illicit sources, such as drug dealers (Ruben and Morrison, 1992; Stein et al., 2016), multiple doctors (Allgulander et al., 1984; Ruben and Morrison, 1992), and a combination of illicit and licit sources (Liebrenz et al., 2015; Nielsen et al., 2013; Ross et al., 1996; Ruben and Morrison, 1992). A recent analysis of young adult NSDUH respondents found that obtaining benzodiazepines from multiple sources is associated with greater risk of SUDs (McCabe et al., 2018).
3.4.2. Benzodiazepine Formulations.
Certain benzodiazepine formulations are more commonly misused than others, and availability (vis-à-vis prescribing rates) robustly affects the misuse of different benzodiazepine products. Among the U.S. general population, 73% of those with past-year benzodiazepine misuse reported misuse of alprazolam products (Hughes et al., 2016), a finding that has been replicated in numerous subgroups in the U.S. (see Supplementary Materials)12. This is consistent with data indicating that alprazolam is the most commonly prescribed benzodiazepine in the U.S. (Lindsley, 2012). In the reviewed studies, participants also reported misusing clonazepam, diazepam, and lorazepam (also among the most commonly prescribed psychiatric medications in the U.S.; Moore and Mattison, 2017). Commonly misused benzodiazepine products appear to vary internationally, likely reflecting variability in prescribing rates for certain benzodiazepines. For example, misuse of oxazepam (Fleischhacker et al., 1986; Frauger et al., 2011; Kan et al., 2001; Morel et al., 2016) and lormetazepam (Lugoboni et al., 2014; Quaglio et al., 2012) has been reported in European samples, but is not common in U.S.-based samples.
Although prevalence estimates for misuse of specific benzodiazepine formulations appear to coincide with prescribing rates, certain benzodiazepines are more preferred than others, potentially reflecting higher abuse liability. In several substance-using samples, participants reported preferring diazepam and flunitrazepam (as indicated by ratings of drug liking, high, and preferred drug), as compared to other benzodiazepine products (Barnas et al., 1992; Iguchi et al., 1993; Malcolm et al., 1993; Stitzer et al., 1981). However, these studies were published over two decades ago, and therefore preference might—at least in part—reflect availability during this period. Route of administration might also determine one’s preference, given that temazepam (particularly the gel-filled capsule formulation) and flunitrazepam appear to be the most commonly injected benzodiazepines (Forsyth et al., 1993; Fountain et al., 1999; Fry and Miller, 2001; Fry et al., 2007; Fry and Bruno, 2002; Lavelle et al., 1991; Oyefeso et al., 1996; Strang et al., 1994; Sunjic and Howard, 1996; Williams et al., 1996). Recent studies from East Asia also report midazolam injection (Hayashi et al., 2013; Kerr et al., 2010; Ti et al., 2014; Van Griensven et al., 2005).
3.4.3. Frequency of Misuse.
For NSDUH respondents who misused tranquilizers in the past month, the average frequency of misuse was 5 days, with over 50% of respondents reporting 1–2 days of misuse (CBHSQ, 2018b). However, the frequency of benzodiazepine misuse varies widely with study sample and time frame assessed. Most college students with past-year benzodiazepine misuse report misuse on fewer than five occasions in the previous year (Messina et al., 2016; Pickover et al., 2016). Among those with OUD and/or injection drug use who misused benzodiazepines in the previous month, 27–60% report daily benzodiazepine misuse (Darke et al., 1993; Fatseas et al., 2009; Gilchrist et al., 2006), with misuse occurring on an average of 13 days (Eiroa-Orosa et al., 2010; Stein et al., 2016).
3.4.4. Route of Administration.
Oral route of administration, or swallowing a pill, is by far the most common route of administration (Brandt et al., 2014a; McLarnon et al., 2014; Pauly et al., 2012). Intranasal benzodiazepine misuse is the second most common route of administration, with approximately 10% of college students (Brandt et al., 2014a) and 45% of young adults with recent prescription drug misuse (Lankenau et al., 2012a) reporting lifetime intranasal use. Smoking and injecting benzodiazepines are both relatively uncommon and have primarily been documented in samples with SUDs or severe patterns of substance use (e.g., injection heroin use). Even in these populations, the prevalence of smoking benzodiazepines is low (i.e., 3–7%) (Lankenau et al., 2012a; Navaratnam and Foong, 1990; Vogel et al., 2013).
The prevalence of benzodiazepine injection varies widely, from <2–37% over periods ranging from past-month to past-year (Bennett and Higgins, 1999; Darke et al., 2002; Darke et al., 1995; Davies et al., 1996; Dobbin et al., 2003; Fry and Bruno, 2002; Gelkopf et al., 1999; Horyniak et al., 2012; Ickowicz et al., 2015; Nielsen et al., 2013; Nielsen et al., 2007; Van Griensven et al., 2005). The studies in which injection use is common (>20%) have typically included samples of injection opioid users (Ross and Darke, 2000) or have specifically recruited benzodiazepine injectors (Strang et al., 1994) or injection drug users (Hayashi et al., 2013; Kerr et al., 2010; Smyth et al., 2001) (see Supplementary Materials for additional information on benzodiazepine injection in these populations). Benzodiazepine injection is associated with greater substance use severity (Hayashi et al., 2013; Kerr et al., 2010; Smyth et al., 2001; Van Griensven et al., 2005), accidental overdose (Bennett and Higgins, 1999; Darke et al., 2002), scarring/bruising/abscesses around injection sites (Breen et al., 2004; Darke et al., 2002; Hayashi et al., 2013), vascular disease (Hayashi et al., 2013), and increased risk of infectious disease (Zhang et al., 2015).
3.4.5. Co-Ingestion.
Benzodiazepines are often co-ingested, or used simultaneously, with other substances in a range of heterogenous samples (see Supplementary Materials)13. Qualitative and descriptive results indicate that coingesting benzodiazepines with alcohol increases the intoxicating effects of both substances (Calhoun et al., 1996; Dåderman and Lidberg, 1999; Perera et al., 1987). Mixing benzodiazepines with opioids (Dwyer, 2008; Gelkopf et al., 1999; Hayashi et al., 2013; Lankenau et al., 2012a; Navaratnam and Foong, 1990; Ng et al., 2007; Ross et al., 1996; Ruben and Morrison, 1992; Vogel et al., 2013) and opioid agonist medication (i.e., methadone, buprenorphine) (Gelkopf et al., 1999; Nielsen et al., 2007; Stitzer et al., 1981; Vogel et al., 2013) to enhance the effects of opioids (Dwyer, 2008; Hayashi et al., 2013; Lankenau et al., 2007; Lankenau et al., 2012b; Mateu-Gelabert et al., 2017; Motta-Ochoa et al., 2017; Navaratnam and Foong, 1990; Ng et al., 2007; Ruben and Morrison, 1992) is widespread among those with opioid use and/or injection drug use. Interestingly, one study among individuals in OUD treatment found that nearly 90% of participants who mixed benzodiazepines with other drugs did so to “improve emotional states” (Gelkopf et al., 1999).
Beyond increasing the effects of opioids and alcohol, benzodiazepines are combined with stimulants (e.g., amphetamines, cocaine) and ecstasy to “come down from” or decrease the effects of these substances (e.g., anxiety, irritation, insomnia) (Calhoun et al., 1996; Fountain et al., 1999; Gelkopf et al., 1999; Kelly et al., 2015b; Lankenau et al., 2012a; Motta-Ochoa et al., 2017; Rigg and Ibanez, 2010). Benzodiazepines are also commonly co-ingested with marijuana (Brandt et al., 2014a; Calhoun et al., 1996; McLarnon et al., 2011; Schepis et al., 2016; Vogel et al., 2013), sometimes by smoking both substances (Calhoun et al., 1996; Kelly et al., 2015b; Lankenau et al., 2007), but little is known about motives for this combination. The widespread use of benzodiazepines is particularly concerning given that co-ingesting benzodiazepines with other substances, particularly opioids and alcohol, is associated with increased risk of overdose (Jones et al., 2012).
3.4.6. Motives.
Common motives for benzodiazepine misuse and correlates of motives are reviewed below. It is important to note that currently available quantitative measures of motives for benzodiazepine misuse focus on a limited range of motives and the factor structure for these measures is unclear (Messina et al., 2016; Vogel et al., 2013). Nonetheless, several qualitative studies provide a broader picture of the motives for benzodiazepine misuse.
Much like other prescription drugs (e.g., opioids, stimulants) (McHugh et al., 2015), benzodiazepines are most commonly misused for reasons aligned with the drug’s indication (e.g., sleep, anxiety). Over 75% of NSDUH respondents with past-year tranquilizer misuse reported that they misused prescription tranquilizers to help with conditions for which benzodiazepines are indicated, such as sleep, tension, or emotions (CBHSQ, 2018b). The finding that self-treatment or coping motives are the most common reasons for benzodiazepine misuse has been replicated across heterogenous samples (see Supplementary Materials). However, benzodiazepines are also misused out of curiosity (Chen et al., 2011; Kapil et al., 2014; Kokkevi et al., 2008; Liebrenz et al., 2015) and for recreational motives, such as to get high (Boyd et al., 2006; Brandt et al., 2014b; Calhoun et al., 1996; Johnston and O’Malley, 1986; Kecojevic et al., 2015a; Kelly et al., 2015b; McCabe et al., 2009; McLarnon et al., 2014; Nattala et al., 2011; Nattala et al., 2012; Quintero et al., 2006; Rigg and Ibanez, 2010; Silva et al., 2013a; Terry-McElrath et al., 2009) and to modify the effects of other substances (Section 3.4.5.). Notably, those who report recreational motives also display more problematic use, such as combining benzodiazepines with other substances, reporting greater substance use severity, taking higher doses, taking benzodiazepines by non-oral routes of administration, and illicitly purchasing benzodiazepines (Fatseas et al., 2009; McCabe et al., 2009; McCabe and Cranford, 2012; McLarnon et al., 2014; Schepis et al., 2016; Stein et al., 2016).
Many individuals with benzodiazepine misuse report multiple motives for misuse (McCabe et al., 2009). Misusing benzodiazepines for multiple reasons is particularly common among those with opioid use and/or injection drug use (Fatseas et al., 2009; Vogel et al., 2013), which is consistent with findings that reporting multiple motives is associated with greater substance use severity (e.g., greater benzodiazepine use frequency [McCabe et al., 2009; Nattala et al., 2011]; co-ingesting benzodiazepines and alcohol [Nattala et al., 2012]). Among those with opioid use and/or injection drug use, benzodiazepines are commonly misused to enhance the effects of opioids or opioid agonist medications (see Section 3.4.5.). Studies in these populations have also found that benzodiazepines are misused to decrease opioid withdrawal symptoms (Gelkopf et al., 1999; Hayashi et al., 2013; Lankenau et al., 2007; Lankenau et al., 2012b; Motta-Ochoa et al., 2017; Nielsen et al., 2013; Perera et al., 1987; Ross et al., 1996; Ruben and Morrison, 1992; Stein et al., 2016; Vogel et al., 2013) and to substitute for opioids, either as a strategy to help decrease opioid use (Lankenau et al., 2012b; Mateu-Gelabert et al., 2017; Perera et al., 1987) or during times of decreased opioid availability (Fry et al., 2007; Lankenau et al., 2012b; Ruben and Morrison, 1992).
3.5. Functional Consequences Associated with Benzodiazepine Misuse.
A number of studies have examined the association between benzodiazepine misuse and an array of clinical and functional consequences (e.g., suicide, physical health, etc.). In many of these studies, it is difficult to ascertain whether the association is attributable to a benzodiazepine-specific effect or more generally to a worse substance use profile (e.g., more polysubstance use). Consistent with this weakness, several findings have not been consistently replicated, likely due to significant variability in methods across studies. Throughout this section, we provide potential explanations for the association between benzodiazepine misuse and functional consequences. Yet, results should be interpreted with caution. An overview of findings on consequences associated with benzodiazepine misuse is presented in Table 4.
Table 4.
Findings on Functional Consequences Associated with Benzodiazepine Misuse
| Population | Finding | References |
|---|---|---|
| Overdose | ||
| Individuals with opioid use, prescription drug misuse, or injection drug use | ||
| Benzodiazepine misuse was associated with overdose in unadjusted but not adjusted analyses | (Calvo et al., 2017; Jenkins et al., 2011; Mcgregor et al., 1998; Ochoa et al., 2005) | |
| Suicidal Behaviors | ||
| Individuals with opioid use, prescription drug misuse, or injection drug use | ||
| Benzodiazepine misuse was not associated with suicidal ideation or attempt, or associations were only significant in unadjusted but not adjusted analyses | (Backmund et al., 2011; Maloney et al., 2009; Wines et al., 2004) | |
| Individuals with alcohol dependence | Benzodiazepine misuse was associated with suicidal ideation or attempt | (Preuss et al., 2003) |
| General population samples in the U.S. | Benzodiazepine misuse was associated with suicidal ideation or attempt | (Blanco et al., 2018; Borges et al., 2000; Schepis et al., 2019; Schepis et al., 2018b) |
| Adolescent samples outside of the U.S. | Benzodiazepine misuse was associated with suicidal ideation or attempt | (Guo et al., 2016; Juan et al., 2015; Kokkevi et al., 2012) |
| Infectious Disease and Associated Behaviors | ||
| Individuals with opioid use, prescription drug misuse, or injection drug use | ||
| Benzodiazepine misuse was not associated with HCV infection or sexual risk behaviors | (Havens et al., 2013; Kecojevic et al., 2015b) | |
| College students in the U.S. | Benzodiazepine misuse was associated with regretted sexual experiences and sexual victimization | (Parks et al., 2017; Young et al., 2011) |
| Criminality | ||
| Individuals with opioid use, prescription drug misuse, or injection drug use | ||
| Benzodiazepine misuse was not associated with criminality | (Darke et al., 2002; Hall et al., 1993) | |
| Adolescents in the U.S. | Benzodiazepine misuse was associated with criminal involvement | (Ford, 2008a) |
| Treatment Outcomes (Substance Use) | ||
| Individuals receiving SUD treatment (most commonly for OUD) | ||
| No association between baseline benzodiazepine misuse and substance use during and after treatment | (Darke et al., 2010; Eiroa-Orosa et al., 2010) | |
| Treatment Outcomes (Retention) | ||
| Individuals receiving SUD treatment (most commonly for OUD) | ||
| Benzodiazepine misuse was not associated with treatment retention | (Davstad et al., 2007; Kellogg et al., 2006; Proctor et al., 2015; Schuman-Olivier et al., 2013; Specka et al., 2011) | |
| Quality of Life and Physical Health | ||
| General population samples in the U.S. | Benzodiazepine misuse was associated with poorer self-reported physical health and disability | (Ford et al., 2018; Schepis et al., 2018b) |
| General population samples outside of the U.S. | Benzodiazepine misuse was associated with poorer self-reported quality of life | (Abrahamsson et al., 2015) |
| Individuals with opioid use, illicit/prescription drug misuse, or injection drug use | ||
| Benzodiazepine misuse was associated with greater sleep dysfunction | (Blanco et al., 2013; Manconi et al., 2017; Mazza et al., 2014; Peles et al., 2009) | |
| Other subgroups (e.g., healthcare workers, adolescents in the emergency department) | ||
| Benzodiazepine misuse was associated with more emergency department visits | (Whiteside et al., 2013) | |
3.5.1. Overdose.
Benzodiazepines increase the risk of heart rate and respiratory depression when co-ingested with opioids and/or alcohol, increasing the risk for overdose (Jones et al., 2012). In three prospective studies of individuals with SUDs (primarily OUD) and/or injection drug use, benzodiazepine misuse was associated with greater odds of mortality (Pavarin, 2015), particularly related to overdose deaths (Gossop et al., 2002; Riley et al., 2016). Likewise, benzodiazepine misuse and dependence have been associated with non-fatal overdose in retrospective studies (Table 4). Benzodiazepines are also involved in methadoneand buprenorphine-related (both prescribed and non-prescribed) overdoses (Lee et al., 2014; Nielsen et al., 2007), which is particularly concerning given the association between receiving a greater methadone dose and benzodiazepine misuse (Bleich et al., 1999; Bleich et al., 2002; Darke et al., 1993; Rooney et al., 1999; Swensen et al., 1993). Notably, samples of people with OUD vary in their awareness of the heightened risk for overdose when opioids and benzodiazepines are combined (Motta-Ochoa et al., 2017; Neira-Leon et al., 2006; Rowe et al., 2016; Stein et al., 2017b; Strang et al., 1999).
3.5.2. Suicidal Behaviors.
Benzodiazepine misuse is also associated with suicidal ideation and attempt in numerous populations (Table 4). Notably, a recent analysis of older adult NSDUH respondents found that misuse of benzodiazepines was associated with suicidal ideation, whereas use as prescribed was not, after adjusting for mental health variables (Schepis et al., 2019). To our knowledge, only one longitudinal study has attempted to explain mechanisms underlying the association between benzodiazepine misuse and suicidal behaviors. This study found that depressive symptoms partially mediated associations between benzodiazepine misuse and suicidal ideation and attempt (Guo et al., 2016), whereas others have identified an association between benzodiazepine misuse and suicidal behaviors after controlling for psychiatric symptoms or disorders (Artenie et al., 2015a; Artenie et al., 2015b; Borges et al., 2000; Juan et al., 2015).
Another potential explanation is that benzodiazepines are used as a means to attempt suicide by intentional overdose, a method that is common among those with SUDs (Darke and Ross, 2001; Neale, 2000). Furthermore, two recent analyses of NSDUH data found that those with concurrent benzodiazepine and opioid misuse had a higher rate of suicidal ideation, as compared to those with benzodiazepine or opioid misuse alone (Schepis et al., 2019; Schepis et al., 2018b). These findings underscore the need to further understand the relationship between benzodiazepine misuse, polysubstance use, and suicidal behaviors.
3.5.3. Infectious Disease and Associated Behaviors.
The association between benzodiazepine misuse and overall mortality among those with opioid use and/or injection drug use might also be explained, in part, by higher rates of HIV and HCV infection in this population (Table 4). These findings are consistent with evidence that benzodiazepine misuse is associated with HIV/HCV risk-taking behaviors, such as injection drug use, unsafe injection practices (e.g., sharing needles, not cleaning needles, etc.), and risky sexual behaviors (e.g., unprotected sex, multiple partners, prostitution) (Table 4). It is possible that the disinhibiting effects of benzodiazepines might increase the likelihood of risky behaviors. In studies of individuals with cocaine and/or opioid use, participants reported engaging in risky sexual behaviors during benzodiazepine intoxication (Johnson et al., 2013), and that benzodiazepines “slowed their thinking” and made them “not too conscious about risk” (Motta-Ochoa et al., 2017). Elevated rates of benzodiazepine prescriptions among those with HIV/HCV (Wixson and Brouwer, 2014) might also increase risk of misuse in this population through increased availability and exposure.
3.5.4. Criminality.
Benzodiazepine misuse has been retrospectively associated with criminal involvement among those with opioid use and/or injection drug use, as well as in a population-based study of adolescents in the U.S. (Table 4). Participants in several qualitative studies have reported intentionally misusing benzodiazepines prior to criminal behavior to become disinhibited or to gain the “confidence” to commit a crime (Calhoun et al., 1996; Dåderman and Lidberg, 1999; Forsyth et al., 2011; Fountain et al., 1999; Payne and Gaffney, 2012; Ruben and Morrison, 1992). In particular, criminal involvement has been reported by those misusing flunitrazepam—a particularly potent benzodiazepine—which might be due to subjective effects that include “loss of control,” feelings of violence, and blackouts (Barnas et al., 1992; Calhoun et al., 1996; Dåderman and Lidberg, 1999). Qualitative findings also suggest that drinking alcohol in combination with benzodiazepines increases disinhibiting and violence-producing effects of these substances (Dåderman and Lidberg, 1999; Forsyth et al., 2011). However, these studies have recruited small samples from specific high-risk subgroups (e.g., male juvenile offenders reporting flunitrazepam misuse). Thus, the prevalence of benzodiazepine misuse to facilitate criminal behavior in the broader population remains unclear.
3.5.5. Treatment Outcomes.
The studies that have examined the impact of benzodiazepine misuse on SUD treatment outcomes (i.e., treatment retention, opioid relapse) have yielded different results depending on the time frame assessed. Specifically, ongoing benzodiazepine misuse during treatment is associated with substance use during and after treatment, whereas baseline benzodiazepine misuse has not consistently predicted substance use treatment outcomes (Table 4).
Studies examining the impact of benzodiazepine misuse on treatment retention have also yielded mixed results, regardless of time frame (Table 4). Nevertheless, previous studies indicate that benzodiazepine dependence is associated with more severe opioid withdrawal symptoms (de Wet et al., 2004) and poorer sleep during OUD treatment (Peles et al., 2009), which might influence reinitiation or continued opioid use. This association may also be dependent on broader substance use patterns. In two previous studies, benzodiazepine misuse in combination with stimulant misuse was associated with poor treatment outcomes (e.g., methadone non-adherence, early dropout), but benzodiazepine misuse alone was not (DeMaria et al., 2000; Raffa et al., 2007). These findings underscore the need to consider overall polysubstance use in future studies determining the impact of benzodiazepine misuse on treatment outcomes.
3.5.6. Quality of Life and Physical Health.
Benzodiazepine misuse and dependence have been associated with poorer self-reported quality of life, greater pain severity, sleep dysfunction, and repeated emergency department visits in a range of populations (Table 4). Yet, these associations have not been consistently studied and, to our knowledge, no longitudinal studies have attempted to test the directions of and mechanisms underlying these associations. In addition, few studies examining these associations have controlled for receipt of a benzodiazepine prescription, despite findings from two recent analyses of NSDUH data that poorer self-reported general health was associated with lower odds of misuse, as compared to use as prescribed (Blanco et al., 2018; Maust et al., 2018).
4. Discussion
4.1. Overview of Findings and Implications
The aim of this comprehensive review was to characterize the current state of the science on the epidemiology of benzodiazepine misuse. Below, we summarize several key findings.
People with SUDs in the U.S. have rates of benzodiazepine misuse 3.5 to 24 times higher than the general population (Votaw et al., 2019), and the misuse of other substances is the most consistent and robust correlate of benzodiazepine misuse. In fact, it is unclear how frequently benzodiazepine misuse occurs in isolation, rather than as part of a pattern of polysubstance use. Answering this question will help identify factors influencing the development of benzodiazepine misuse and populations who might benefit from interventions to reduce benzodiazepine misuse. Based on the present review, it is likely that the misuse of benzodiazepines for multiple reasons partially explains the high prevalence of misuse among those with SUDs. Future studies evaluating motives for benzodiazepine misuse among other vulnerable populations, including those with psychiatric disorders and benzodiazepine prescriptions, are needed to understand the relationship between motives and benzodiazepine misuse incidence and severity.
People with psychiatric symptoms and disorders also appear to be more vulnerable to benzodiazepine misuse. This is consistent with findings that regulating negative affective and somatic states is the most common motive for benzodiazepine misuse. Yet, it is unclear if psychiatric distress is an antecedent or consequence of benzodiazepine misuse (or both), and findings from the reviewed studies provide partial support for both explanations. It is likely that greater psychiatric distress motivates misuse to relieve symptoms, and symptoms of psychiatric distress are also a consequence of acute or protracted benzodiazepine withdrawal. The association between psychiatric distress and benzodiazepine misuse underscores the importance of first considering non-benzodiazepine treatments (e.g., cognitive-behavioral therapy, antidepressants) for psychiatric symptoms among those who are most likely to misuse benzodiazepines. Women are more likely to report misusing benzodiazepines to cope with negative affect, and associations between psychiatric distress and benzodiazepine misuse appear to be stronger in women than in men. Accordingly, women might particularly benefit from efforts to reduce benzodiazepine misuse and related harms that target negative affect.
Unsurprisingly, exposure to a benzodiazepine prescription is associated with likelihood of misuse. This link between a prescription and misuse may reflect greater access/exposure to benzodiazepines, greater abuse liability among those for whom these medications are likely to be prescribed, or purposeful seeking of prescriptions with the intention of misuse; likely all of these factors contribute to this association. This highlights the need to carefully assess for misuse risk when prescribing benzodiazepines. There are currently no validated screening measures for likelihood of benzodiazepine misuse; however, results from this review suggest that factors such as history of substance use disorders and greater psychiatric severity are markers of concern. It is important to note that benzodiazepine diversion was common among people with a benzodiazepine prescription. Safe medication storage and disposal education should also be standard practice for those prescribing benzodiazepines to help mitigate diversion and accidental exposure.
Benzodiazepine misuse encompasses heterogeneous presentations of motives, patterns, and sources. Most of the participants in the reviewed studies received benzodiazepines from a friend/family member with a prescription and misused benzodiazepines infrequently and for the purposes aligned with their indication (e.g., anxiety, insomnia). Yet, high-risk profiles were also documented, and included: frequent misuse, co-ingestion with other substances, obtaining from illicit sources, non-oral routes of administration, multiple motives for use, and significant health and functional consequences. High-risk profiles were mostly observed among those with SUDs, but not all individuals with SUDs exhibited these risky patterns, with many misusing benzodiazepines infrequently and for the purpose of coping, rather than to feel high.
Benzodiazepine misuse is associated with a range of consequences, including overdose, suicidal and risk-taking behaviors, infectious disease, criminality, poor SUD treatment outcomes, and low quality of life. Overall, little is known about mechanisms underlying these associations. Overdoses related to benzodiazepines are more likely during co-ingestion with opioids and/or alcohol, a common pattern of benzodiazepine misuse. Improving education about the increased risk of overdose when benzodiazepines are combined with opioids and/or alcohol is important in the context of continued increases in drug overdoses in the U.S. Benzodiazepine injection has also been associated with a number of these consequences, including overdose, infectious disease, and physical health issues. Benzodiazepine misuse and greater substance use severity (particularly polysubstance use) are consistently associated; substance use severity might be an overlooked factor confounding the association between benzodiazepine misuse and poor outcomes.
4.2. Limitations of the Current Literature
Although our review identified a large number of studies on the epidemiology of benzodiazepine misuse (N=351), this literature has a number of limitations and gaps that present important areas of future study.
Inconsistency in the definition of misuse is perhaps the biggest limitation in the extant literature (Table 2). In the reviewed studies, the term misuse (also referred to as nonmedical use, abuse, recreational use, etc.) was used broadly and inconsistently, resulting in highly heterogeneous groups and hampering the ability to compare studies. Inconsistencies among studies in the use of terminology (e.g., misuse, nonmedical use, abuse) might also explain different findings on prevalence estimates, patterns of prescription drug misuse, and factors associated with prescription drug misuse. For example, the NSDUH survey modified its definition in 2015; the original definition (non-prescribed use or use that occurred only for the feelings/experiences the prescription drugs caused) was expanded to include use in any way a doctor did not direct, such as using without a prescription or in greater amounts/more often/longer than prescribed. Following the implementation of this expanded definition, the percentage of people reporting their own prescription as their most recent source of tranquilizers increased from 14.1% to 21.8% (CBHSQ, 2015a, 2016). Such findings underscore the importance of carefully defining misuse.
Two papers published a decade ago highlight the challenges in defining prescription drug misuse (Barrett et al., 2008; Boyd and McCabe, 2008). Yet, based on the present review, few steps have since been taken to improve upon the classification of benzodiazepine misuse. Several changes to current research practices may help to improve this ongoing issue. Most importantly, definitions should clearly convey what behaviors constitute misuse and clearly distinguish among these behaviors, including medication overuse (e.g., using one’s legitimate prescription at greater doses or more often than prescribed), nonmedical use (e.g., without one’s own prescription or a prescription obtained for a reason other than its intended indication), and other illicit use (e.g., buying or trading for medication on the streets). Future studies separating these different forms of misuse are also needed to determine their relative clinical significance. In addition, studies enrolling individuals with SUDs should not rely exclusively on benzodiazepine-positive urine drug screens (e.g., in studies examining medical records), given high rates of benzodiazepine prescriptions among those with SUDs (Abrahamsson et al., 2017; Stein et al., 2017a; Tjagvad et al., 2016). Urine-confirmed self-report and assessment for current prescriptions is needed in these populations.
A related limitation of the literature includes inconsistent definitions of prescription drug classes (Table 2). Surveys evaluating benzodiazepine misuse commonly combined benzodiazepines with other sedatives and tranquilizers (e.g., muscle relaxants, barbiturates, z-drugs) or included benzodiazepine products in separate categories (e.g., sedatives, tranquilizers, sleeping medications, anxiolytic medications). This presents a significant barrier to identifying trends that may be informative for public health interventions, such as educating prescribers on potential risks associated with benzodiazepine prescribing. This is a common challenge for population-based surveys, which aim to evaluate a wide range of substances while minimizing participant burden. However, the increasing public health burden of benzodiazepines highlights the necessity of specifically evaluating benzodiazepine products.
Finally, our understanding of benzodiazepine misuse is limited by the reliance on samples of people with opioid use and/or injection drug use or general population samples. This both introduces potential confounds (e.g., limits the ability to isolate the impact of benzodiazepine misuse relative to a broader pattern of polydrug use) and may leave vulnerable populations understudied. Most notably, little is known about the co-use of alcohol and benzodiazepines, despite elevated rates of benzodiazepine misuse among those with problematic drinking and increased risk of overdose when alcohol and benzodiazepines are combined. Future research is needed to identify individuals who are most vulnerable to alcohol and benzodiazepine co-use and motives for this combination. Other notable populations in need of additional research include those with psychiatric disorders and individuals with benzodiazepine prescriptions.
4.3. Future Research Directions
Little is known about benzodiazepine misuse trajectories over time. Longitudinal studies should examine risks for the development of misuse, factors influencing the transition from prescribed use to misuse and from oral routes of administration to non-oral routes of administration (including injection use), and factors influencing the escalation to SHA use disorder. In addition, longitudinal studies will help to determine the temporal associations between benzodiazepine misuse and potential consequences (e.g., suicidality, poor physical health). Such studies would inform the development of screening tools to identify people at the highest risk for benzodiazepine misuse and the identification of factors that may be important targets for the prevention and treatment of benzodiazepine misuse.
There is also a dearth of research on the prevention and treatment of benzodiazepine misuse and use disorder. Most treatment studies have focused on benzodiazepine tapers in people with long-term benzodiazepine prescriptions for anxiety or insomnia, and do not specifically focus on misuse (Morin et al., 2004; Otto et al., 2010). The development of effective interventions to mitigate benzodiazepine misuse is particularly important to reduce overdose risk. Of note, adding cognitive-behavioral therapy (particularly, interoceptive exposure-based treatment) to a slow benzodiazepine taper enhances success among people seeking to discontinue benzodiazepine prescriptions (Otto et al., 2010; Otto et al., 1993). Accordingly, such approaches may also have promise for the treatment of benzodiazepine misuse, particularly given the strong link between anxiety and benzodiazepine misuse (McHugh et al., 2018; McHugh et al., 2017).
4.4. Limitations of the Present Review
The results of the present review are qualified by several methodological limitations. First, our search strategy was limited to the search terms used, and therefore we might have missed relevant studies that did not include these key words. Second, we chose to use the term “benzodiazepine misuse” throughout the present review, although many studies combined benzodiazepines with other sedative and tranquilizer medications. We described study findings in this manner to balance accuracy with interpretability; however, it is unknown how the inclusion of other sedatives and tranquilizers in the reviewed literature impacted results. We also chose to include studies among those with SUDs that defined benzodiazepine misuse based on urine drug screen results, as opposed to clear definitions of misuse. Although these studies suggest, or imply, that this constitutes problematic use, these studies may have included participants who were using benzodiazepines as prescribed. The extant literature on some topics examined in the present review is outdated. In particular, the majority of the literature on preferences for specific benzodiazepine formulations was published over two decades ago, thus limiting strong conclusions about reasons for preferring specific benzodiazepine formulations. Lastly, prevalence estimates primarily reflect data collected in the U.S., though 49% of studies included in the present review were conducted in countries outside of the U.S. Given that benzodiazepine misuse is an international issue, future studies should continue to characterize the epidemiology of benzodiazepine misuse worldwide.
5. Conclusions
Research has identified numerous risk factors, motives, consequences, and common patterns of benzodiazepine misuse. These findings have important implications for identifying subgroups who could benefit from prevention and treatment efforts (e.g., people with substance use and/or psychiatric distress), critical points for intervention (e.g., in adolescence/young adulthood, during benzodiazepine prescribing, in SUD treatment), and appropriate content for such interventions (e.g., targeting negative affect, psychoeducation on overdose risk). Nonetheless, much remains unknown about the epidemiology of benzodiazepine misuse. With the continued escalation of treatment admissions and overdose deaths related to benzodiazepine misuse, studies designed to better understand this growing public health problem should be a research priority for the field of substance use disorder research.
Supplementary Material
Highlights.
We reviewed epidemiological studies on benzodiazepine misuse
Polysubstance use and psychiatric distress increase risk of misuse
Benzodiazepines are commonly co-ingested with other substances
Coping with negative affect and sleep are the most common motives for misuse
Misuse is associated with poor outcomes, including morbidity and mortality
Role of Funding Source
Effort on this manuscript was supported by NIDA grant K23 DA035297 and the Sarles Young Investigator Award (Dr. McHugh). These funding sources had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared.
References
- Abrahamsson T, Berge J, Öjehagen A, Håkansson A, 2017. Benzodiazepine, z-drug and pregabalin prescriptions and mortality among patients in opioid maintenance treatment—A nation-wide register-based open cohort study. Drug Alcohol Depend. 174, 58–64. [DOI] [PubMed] [Google Scholar]
- Abrahamsson T, Berglund M, Hakansson A, 2015. Non-medical prescription drug use (NMPDU) and poor quality of life in the Swedish general population. Am. J. Addict 24, 271–277. [DOI] [PubMed] [Google Scholar]
- Abrahamsson T, Hakansson A, 2015. Nonmedical prescription drug use (NMPDU) in the Swedish general population--correlates of analgesic and sedative use. Subst. Use Misuse 50, 148–155. [DOI] [PubMed] [Google Scholar]
- Allgulander C, Borg S, Vikander B, 1984. A 4–6 year follow-up of 50 patients with primary dependence on sedative and hypnotic drugs. Am. J. Psychiatry 141, 1580–1582. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2000. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Association, Washington, DC. [Google Scholar]
- Anagnostopoulos A, Abraham AG, Genberg BL, Kirk GD, Mehta SH, 2018. Prescription drug use and misuse in a cohort of people who inject drugs (PWID) in Baltimore. Addict. Behav 81, 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apantaku-Olajide T, Ducray K, Byrne P, Smyth BP, 2012. Perception of unmet needs and association with benzodiazepine misuse among patients on a methadone maintenance treatment programme. Psychiatrist 36, 169–174. [Google Scholar]
- Arria AM, Caldeira KM, O’Grady KE, Vincent KB, Fitzelle DB, Johnson EP, Wish ED, 2008. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Subst. Abus 29, 19–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artenie AA, Bruneau J, Roy E, Zang G, Lesperance F, Renaud J, Tremblay J, Jutras-Aswad D, 2015a. Licit and illicit substance use among people who inject drugs and the association with subsequent suicidal attempt. Addiction 110, 1636–1643. [DOI] [PubMed] [Google Scholar]
- Artenie AA, Bruneau J, Zang G, Lespérance F, Renaud J, Tremblay J, Jutras-Aswad D, 2015b. Associations of substance use patterns with attempted suicide among persons who inject drugs: Can distinct use patterns play a role? Drug Alcohol Depend. 147, 208–214. [DOI] [PubMed] [Google Scholar]
- Arterberry BJ, Horbal SR, Buu A, Lin HC, 2016. The effects of alcohol, cannabis, and cigarette use on the initiation, reinitiation and persistence of non-medical use of opioids, sedatives, and tranquilizers in adults. Drug Alcohol Depend. 159, 86–92. [DOI] [PubMed] [Google Scholar]
- Ashton H, 2005. The diagnosis and management of benzodiazepine dependence. Curr. Opin. Psychiatry 18, 249–255. [DOI] [PubMed] [Google Scholar]
- Assanangkornchai S, Sam-Angsri N, Rerngpongpan S, Edwards JG, 2010. Anxiolytic and hypnotic drug misuse in Thailand: Findings from a national household survey. Drug Alcohol Rev. 29, 101–111. [DOI] [PubMed] [Google Scholar]
- Austic E, McCabe SE, Stoddard SA, Ngo QE, Boyd C, 2015. Age and cohort patterns of medical and nonmedical use of controlled medication among adolescents. J. Addict. Med 9, 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bach P, Walton G, Hayashi K, Milloy MJ, Dong H, Kerr T, Montaner J, Wood E, 2016. Benzodiazepine Use and Hepatitis C Seroconversion in a Cohort of Persons Who Inject Drugs. Am. J. Public Health 106, 1067–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL, 2016. Increasing Benzodiazepine Prescriptions and Overdose Mortality in the United States, 1996–2013. Am. J. Public Health 106, 686–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backmund M, Meyer K, Henkel C, Soyka M, Reimer J, Schütz CG, 2005. Co-consumption of benzodiazepines in heroin users, methadone-substituted and codeine-substituted patients. J. Addict. Dis 24, 17–29. [DOI] [PubMed] [Google Scholar]
- Backmund M, Meyer K, Schütz C, Reimer J, 2011. Factors associated with suicide attempts among injection drug users. Subst. Use Misuse 46, 1553–1559. [DOI] [PubMed] [Google Scholar]
- Barnas C, Rossmann M, Roessler H, Riemer Y, Fleischhacker WW, 1992. Benzodiazepines and other psychotropic drugs abused by patients in a methadone maintenance program: Familiarity and preference. J. Clin. Psychopharmacol 12, 397–402. [PubMed] [Google Scholar]
- Barrett SP, Meisner JR, Stewart SH, 2008. What constitutes prescription drug misuse? Problems and pitfalls of current conceptualizations. Curr. Drug Abuse Rev 1, 255–262. [DOI] [PubMed] [Google Scholar]
- Bawor M, Dennis BB, Varenbut M, Daiter J, Marsh DC, Plater C, Worster A, Steiner M, Anglin R, Pare G, Desai D, Thabane L, Samaan Z, 2015. Sex differences in substance use, health, and social functioning among opioid users receiving methadone treatment: A multicenter cohort study. Biol. Sex Differ 6, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beary M, Christofides J, Fry D, Ghodse A, Smith E, Smith V, 1987. The benzodiazepines as substances of abuse. Practitioner 231, 19. [PubMed] [Google Scholar]
- Becker WC, Fiellin DA, Desai RA, 2007. Non-medical use, abuse and dependence on sedatives and tranquilizers among U.S. adults: Psychiatric and socio-demographic correlates. Drug Alcohol Depend. 90, 280–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GA, Higgins DS, 1999. Accidental overdose among injecting drug users in Dorset, UK. Addiction 94, 1179–1189. [DOI] [PubMed] [Google Scholar]
- Bisaga A, Mariani JJ, 2015. Benzodiazepines and other sedatives and hypnotics, in: Galanter M, Klber DH, Brady KT (Eds.), Textbook of Substance Abuse Treatment 5th Edition American Psychiatric Publishing, Washington, DC. [Google Scholar]
- Blanco C, Han B, Jones CM, Johnson K, Compton WM, 2018. Prevalence and correlates of benzodiazepine use, misuse, and use disorders among adults in the United States. J. Clin. Psychiatry 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Rafful C, Wall MM, Jin CJ, Kerridge B, Schwartz RP, 2013. The latent structure and predictors of non-medical prescription drug use and prescription drug use disorders: A national study. Drug Alcohol Depend. 133, 473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer DG, Wu LT, 2009. Nonprescription use of pain relievers by middle-aged and elderly community-living adults: National Survey on Drug Use and Health. J. Am. Geriatr. Soc 57, 1252–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich A, Gelkopf M, Schmidt V, Hayward R, Bodner G, Adelson M, 1999. Correlates of benzodiazepine abuse in methadone maintenance treatment. A 1 year prospective study in an Israeli clinic. Addiction 94, 1533–1540. [DOI] [PubMed] [Google Scholar]
- Bleich A, Gelkopf M, Weizman T, Adelson M, 2002. Benzodiazepine abuse in a methadone maintenance treatment clinic in Israel: Characteristics and a pharmacotherapeutic approach. Isr. J. Psychiatry Relat. Sci 39, 104–112. [PubMed] [Google Scholar]
- Boggis JS, Feder K,2019. Trends in and correlates of tranquilizer Misuse among adults who misuse opioids in the United States, 2002–2014. Drug Alcohol Depend. 198, 158–161. [DOI] [PubMed] [Google Scholar]
- Borges G, Walters EE, Kessler RC, 2000. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. Am. J. Epidemiol 151, 781–789. [DOI] [PubMed] [Google Scholar]
- Bouvier BA, Waye KM, Elston B, Hadland SE, Green TC, Marshall BDL, 2018. Prevalence and correlates of benzodiazepine use and misuse among young adults who use prescription opioids non-medically. Drug Alcohol Depend. 183, 73–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd C, West B, McCabe S, 2018. Does misuse lead to a disorder? The misuse of prescription tranquilizer and sedative medications and subsequent substance use disorders in a US longitudinal sample. Addict. Behav 79, 17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, Austic E, Epstein-Ngo Q, Veliz PT, McCabe SE, 2015. A prospective study of adolescents’ nonmedical use of anxiolytic and sleep medication. Psychol. Addict. Behav 29, 184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE, 2008. Coming to terms with the nonmedical use of prescription medications. Subst. Abuse Treat. Prev. Policy 3, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE, Cranford JA, Young A, 2006. Adolescents’ motivations to abuse prescription medications. Pediatrics 118, 2472–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE, Cranford JA, Young A, 2007. Prescription drug abuse and diversion among adolescents in a southeast Michigan school district. Arch. Pediatr. Adolesc. Med 161, 276–281. [DOI] [PubMed] [Google Scholar]
- Brady KT, Johnston AL, Cunningham M, Malcolm R, 1991. Profiles of hospitalized benzodiazepine abusers. J. Psychoactive Drugs 23, 71–72. [DOI] [PubMed] [Google Scholar]
- Brands B, Blake J, Marsh DC, Sproule B, Jeyapalan R, Li S, 2008. The impact of benzodiazepine use on methadone maintenance treatment outcomes. J. Addict. Dis 27, 37–48. [DOI] [PubMed] [Google Scholar]
- Brandt SA, Taverna EC, Hallock RM, 2014a. A survey of nonmedical use of tranquilizers, stimulants, and pain relievers among college students: Patterns of use among users and factors related to abstinence in non-users. Drug Alcohol Depend. 143, 272–276. [DOI] [PubMed] [Google Scholar]
- Breen CL, Degenhardt LJ, Bruno RB, Roxburgh AD, Jenkinson R, 2004. The effects of restricting publicly subsidised temazepam capsules on benzodiazepine use among injecting drug users in Australia. Med. J. Aust 181, 300–304. [DOI] [PubMed] [Google Scholar]
- Cai R, Crane E, Poneleit K, Paulozzi L, 2010. Emergency department visits involving nonmedical use of selected prescription drugs in the United States, 2004–2008. J. Pain Palliat. Care Pharmacother. 24, 293–297. [DOI] [PubMed] [Google Scholar]
- Calhoun SR, Wesson DR, Galloway GP, Smith DE, 1996. Abuse of flunitrazepam (Rohypnol) and other benzodiazepines in Austin and south Texas. J. Psychoactive Drugs 28, 183–189. [DOI] [PubMed] [Google Scholar]
- Calvo M, MacFarlane J, Zaccaro H, Curtis M, Caban M, Favaro J, Passannante MR, Frost T, 2017. Young people who use drugs engaged in harm reduction programs in New York City: Overdose and other risks. Drug Alcohol Depend. 178, 106–114. [DOI] [PubMed] [Google Scholar]
- Caplehorn JR, 1996. Risk factors for non-HIV-related death among methadone maintenance patients. Eur. Addict. Res 2, 49–52. [Google Scholar]
- Caplehorn JR, Saunders JB, 1993. Factors associated with heroin users’ AIDS risk-taking behaviours. Aust. J. Public Health 17, 13–17. [DOI] [PubMed] [Google Scholar]
- Carrasco-Garrido P, Jiménez-Trujillo I, Hernández-Barrera V, García-Gómez-Heras S, Alonso-Fernández N, Palacios-Ceña D, 2018. Trends in the misuse of tranquilizers, sedatives, and sleeping Pills by adolescents in Spain, 2004–2014. J. Adolesc. Health 63, 709–716. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2011. The TEDS Report: Substance Abuse Treatment Admissions for Abuse of Benzodiazepines. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.datafiles.samhsa.gov/study-publication/substance-abuse-treatment-admissions-abuse-benzodiazepines-nid14638 [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2012. The TEDS Report: Admissions Reporting Benzodiazepine and Narcotic Pain Reliever Abuse at Treatment Entry. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.datafiles.samhsa.gov/study-publication/admissions-reporting-benzodiazepine-and-narcotic-pain-reliever-abuse-treatment [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2015a. 2014 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/NSDUHDetTabs2014/NSDUH-DetTabs2014.pdf [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2015b. 2016 National Survey on Drug Use and Health (NSDUH): CAI Specifications for Programming (English Version). Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/NSDUHmrbCAIquex2016v2.pdf [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2016. 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/report/results-2015-national-survey-drug-useand-health-detailed-tables [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2017. Treatment Episode Data Set (TEDS): 2005–2015. National Admissions to Substance Abuse Treatment Services. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/report/treatment-episode-data-set-teds-2005-2015-state-admissions-substance-abuse-treatment-services [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2018a. 2016 National Survey on Drug Use and Health Public Use File Codebook. Substance Abuse and Mental Health Services Administration, Rockville, MD: http://samhda.s3-usgov-west-1.amazonaws.com/s3fs-public/field-uploads-protected/studies/NSDUH-2016/NSDUH-2016-datasets/NSDUH-2016-DS0001/NSDUH-2016-DS0001-info/NSDUH-2016-DS0001-infocodebook.pdf [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2018b. 2017 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf [Google Scholar]
- Chen C-Y, Storr CL, Anthony JC, 2009. Early-onset drug use and risk for drug dependence problems. Addict. Behav 34, 319–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen KW, Berger CC, Forde DP, D’Adamo C, Weintraub E, Gandhi D, 2011. Benzodiazepine use and misuse among patients in a methadone program. BMC Psychiatry 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Ackerman D, Mays VM, Ross MW, 2004. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction 99, 989–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comiskey CM, Snel A, 2016. Using client’s routine urinalysis records from multiple treatment systems to model five-year opioid substitution treatment outcomes. Subst. Use Misuse 51, 498–507. [DOI] [PubMed] [Google Scholar]
- Comiskey CM, Stapleton R, Kelly PA, 2012. Ongoing cocaine and benzodiazepine use: Effects on acquisitive crime committal rates amongst opiate users in treatment. Drugs (Abingdon Engl) 19, 406–414. [Google Scholar]
- Compton WM 3rd, Cottler LB, Ben Abdallah A, Phelps DL, Spitznagel EL, Horton JC, 2000. Substance dependence and other psychiatric disorders among drug dependent subjects: Race and gender correlates. Am. J. Addict 9, 113–125. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Pihl RO, Stewart SH, Dongier M, 2000. Validation of a system of classifying female substance abusers on the basis of personality and motivational risk factors for substance abuse. Psychol. Addict. Behav 14, 243–256. [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF, 2006. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry 67, 247–257. [DOI] [PubMed] [Google Scholar]
- Cook B, Creedon T, Wang Y, Lu C, Carson N, Jules P, Lee E, Alegría M, 2018. Examining racial/ethnic differences in patterns of benzodiazepine prescription and misuse. Drug Alcohol Depend. 187, 29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie CL, Wild TC, 2012. Adolescent use of prescription drugs to get high in Canada. Can. J. Psychiatry 57, 745–751. [DOI] [PubMed] [Google Scholar]
- Dåderman AM, Lidberg L, 1999. Flunitrazepam (Rohypnol) abuse in combination with alcohol causes premeditated grievous violence in male juvenile offenders. J. Am. Acad. Psychiatry Law 27, 83–99. [PubMed] [Google Scholar]
- Dagirmanjian FR, McDaniel AE, Shadick R, 2017. Sexual orientation and college students’ reasons for nonmedical use of prescription drugs. Subst. Use Misuse 52, 1011–1018. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Ross M, Wodak A, 1992. Benzodiazepine use and HIV risk-taking behaviour among injecting drug users. Drug Alcohol Depend. 31, 31–36. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, 2001. The relationship between suicide and heroin overdose among methadone maintenance patients in Sydney, Australia. Addiction 96, 1443–1453. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Cohen J, 1994a. The use of benzodiazepines among regular amphetamine users. Addiction 89, 1683–1690. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Hall W, 1996. Overdose among heroin users in Sydney, Australia: I. Prevalence and correlates of non‐fatal overdose. Addiction 91, 405–411. [PubMed] [Google Scholar]
- Darke S, Ross J, Lynskey M, Teesson M, 2004. Attempted suicide among entrants to three treatment modalities for heroin dependence in the Australian Treatment Outcome Study (ATOS): Prevalence and risk factors. Drug Alcohol Depend. 73, 1–10. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Mills K, Teesson M, Williamson A, Havard A, 2010. Benzodiazepine use among heroin users: Baseline use, current use and clinical outcome. Drug Alcohol Rev. 29, 250–255. [DOI] [PubMed] [Google Scholar]
- Darke S, Swift W, Hall W, Ross M, 1993. Drug use, HIV risk-taking and psychosocial correlates of benzodiazepine use among methadone maintenance clients. Drug Alcohol Depend. 34, 67–70. [DOI] [PubMed] [Google Scholar]
- Darke S, Swift W, Hall W, Ross M, 1994b. Predictors of injecting and injecting risk‐taking behaviour among methadone maintenance clients. Addiction 89, 311–316. [DOI] [PubMed] [Google Scholar]
- Darke S, Topp L, Ross J, 2002. The injection of methadone and benzodiazepines among Sydney injecting drug users 1996–2000: 5-year monitoring of trends from the Illicit Drug Reporting System. Drug Alcohol Rev. 21, 27–32. [DOI] [PubMed] [Google Scholar]
- Darke SG, Ross JE, Hall WD, 1995. Benzodiazepine use among injecting heroin users. Med. J. Aust 162, 645–647. [DOI] [PubMed] [Google Scholar]
- Davies A, Dominy N, Peters A, Richardson A, 1996. Gender differences in HIV risk behaviour of injecting drug users in Edinburgh. AIDS Care 8, 517–528. [DOI] [PubMed] [Google Scholar]
- Davstad I, Stenbacka M, Leifman A, Beck O, Korkmaz S, Romelsjo A, 2007. Patterns of illicit drug use and retention in a methadone program: A longitudinal study. J. Opioid Manag 3, 27–34. [DOI] [PubMed] [Google Scholar]
- Day C, 2013. Benzodiazepines in Combination with Opioid Pain Relievers or Alcohol: Greater Risk of More Serious ED Visit Outcomes The CBHSQ Report. Substance Abuse and Mental Health Services Administration (US), Rockville (MD) pp. 1–9. [PubMed] [Google Scholar]
- de Wet C, Reed L, Glasper A, Moran P, Bearn J, Gossop M, 2004. Benzodiazepine co-dependence exacerbates the opiate withdrawal syndrome. Drug Alcohol Depend. 76, 31–35. [DOI] [PubMed] [Google Scholar]
- Deacon RM, Nielsen S, Leung S, Rivas G, Cubitt T, Monds LA, Ezard N, Larance B, Lintzeris N, 2016. Alprazolam use and related harm among opioid substitution treatment clients—12 months follow up after regulatory rescheduling. Int. J. Drug Policy 36, 104–111. [DOI] [PubMed] [Google Scholar]
- DeMaria PA Jr., Sterling R, Weinstein SP, 2000. The effect of stimulant and sedative use on treatment outcome of patients admitted to methadone maintenance treatment. Am. J. Addict 9, 145–153. [DOI] [PubMed] [Google Scholar]
- Dietze P, Jolley D, Fry C, Bammer G, 2005. Transient changes in behaviour lead to heroin overdose: Results from a case‐crossover study of non‐fatal overdose. Addiction 100, 636–642. [DOI] [PubMed] [Google Scholar]
- Dinwiddie SH, Cottler L, Compton W, Abdallah AB, 1996. Psychopathology and HIV risk behaviors among injection drug users in and out of treatment. Drug Alcohol Depend. 43, 1–11. [DOI] [PubMed] [Google Scholar]
- Dobbin M, Martyres RF, Clode D, Champion De Crespigny FE, 2003. Association of benzodiazepine injection with the prescription of temazepam capsules. Drug Alcohol Rev. 22, 153–157. [DOI] [PubMed] [Google Scholar]
- Donoghoe MC, Dolan KA, Stimson GV, 1992. Life‐style factors and social circumstances of syringe sharing in injecting drug users. Addiction 87, 993–1003. [DOI] [PubMed] [Google Scholar]
- Dwyer R, 2008. Privileging pleasure: temazepam injection in a heroin marketplace. Int. J. Drug Policy 19, 367–374. [DOI] [PubMed] [Google Scholar]
- Eiroa-Orosa FJ, Haasen C, Verthein U, Dilg C, Schafer I, Reimer J, 2010. Benzodiazepine use among patients in heroin-assisted vs. methadone maintenance treatment: Findings of the German randomized controlled trial. Drug Alcohol Depend. 112, 226–233. [DOI] [PubMed] [Google Scholar]
- Evans JL, Hahn JA, Lum PJ, Stein ES, Page K, 2009. Predictors of injection drug use cessation and relapse in a prospective cohort of young injection drug users in San Francisco, CA (UFO Study). Drug Alcohol Depend. 101, 152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatseas M, Lavie E, Denis C, Auriacombe M, 2009. Self-perceived motivation for benzodiazepine use and behavior related to benzodiazepine use among opiate-dependent patients. J. Subst. Abuse Treat 37, 407–411. [DOI] [PubMed] [Google Scholar]
- Fenton MC, Keyes KM, Martins SS, Hasin DS, 2010. The role of a prescription in anxiety medication use, abuse, and dependence. Am. J. Psychiatry 167, 1247–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischhacker WW, Barnas C, Hackenberg B, 1986. Epidemiology of benzodiazepine dependence. Acta Psychiatr. Scand 74, 80–83. [DOI] [PubMed] [Google Scholar]
- Ford JA, 2008a. Nonmedical prescription drug use and delinquency: An analysis with a national sample. J. Drug Issues 38, 493–516. [Google Scholar]
- Ford JA, 2008b. Social learning theory and nonmedical prescription drug use among adolescents. Sociol. Spectr 28, 299–316. [Google Scholar]
- Ford JA, 2009. Nonmedical prescription drug use among adolescents the influence of bonds to family and school. Youth Soc. 40, 336–352. [Google Scholar]
- Ford JA, Hinojosa MS, Nicholson HL, 2018. Disability status and prescription drug misuse among US adults. Addict. Behav 85, 64–69. [DOI] [PubMed] [Google Scholar]
- Ford JA, Lacerenza C, 2011. The relationship between source of diversion and prescription drug misuse, abuse, and dependence. Subst. Use Misuse 46, 819–827. [DOI] [PubMed] [Google Scholar]
- Ford JA, Reckdenwald A, Marquardt B, 2014. Prescription drug misuse and gender. Subst. Use Misuse 49, 842–851. [DOI] [PubMed] [Google Scholar]
- Forsyth AJ, Farquhar D, Gemmell M, Shewan D, Davies JB, 1993. The dual use of opioids and temazepam by drug injectors in Glasgow (Scotland). Drug Alcohol Depend. 32, 277–280. [DOI] [PubMed] [Google Scholar]
- Forsyth AJM, Khan F, Mckinlay B, 2011. Diazepam, alcohol use and violence among male young offenders:’The devil’s mixture’. Drugs (Abingdon Engl) 18, 468–476. [Google Scholar]
- Fountain J, Griffiths P, Farrell M, Gossop M, Strang J, 1999. Benzodiazepinesin Polydrug-using Repertoires: the impact of the decreased availability of temazepam gel-filled capsules. Drugs (Abingdon Engl) 6, 61–69. [Google Scholar]
- Franklyn AM, Eibl JK, Gauthier G, Pellegrini D, Lightfoot NK, Marsh DC, 2017. The impact of benzodiazepine use in patients enrolled in opioid agonist therapy in Northern and rural Ontario. Harm. Reduct. J 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frauger E, Pauly V, Pradel V, Rouby F, Arditti J, Thirion X, Lapeyre Mestre M, Micallef J, 2011. Evidence of clonazepam abuse liability: Results of the tools developed by the French Centers for Evaluation and Information on Pharmacodependence (CEIP) network. Fundam. Clin. Pharmacol 25, 633–641. [DOI] [PubMed] [Google Scholar]
- Fry CL, Miller PG, 2001. Victorian Drug Trends 2000: Findings from the Melbourne arm of the Illicit Drug Reporting System (IDRS). National Drug and Alcohol Research Centre, University of NSW, Sydney NSW Australia: https://research.monash.edu/en/publications/victorian-drug-trends-2000-findings-from-the-melbourne-arm-of-the [Google Scholar]
- Fry C, Smith B, Bruno R, O’Keefe B, Miller P, 2007. Benzodiazepine and pharmaceutical opioid misuse and their relationship to crime: An examination of illicit prescription drug markets in Melbourne, Hobart and Darwin: Victorian report.
- Fry CL, Bruno RB, 2002. Recent trends in benzodiazepine use by injecting drug users in Victoria and Tasmania. Drug Alcohol Rev. 21, 363–367. [DOI] [PubMed] [Google Scholar]
- Galduróz JCF, Noto AR, Nappo SA, Carlini E, 2005. Household survey on drug abuse in Brazil: Study involving the 107 major cities of the country—2001. Addict. Behav 30, 545–556. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Coffin PO, Tracy M, Piper TM, Ompad D, Vlahov D, 2006. Heroin and cocaine dependence and the risk of accidental non-fatal drug overdose. J. Addict. Dis 25, 79–87. [DOI] [PubMed] [Google Scholar]
- Gelkopf M, Bleich A, Hayward R, Bodner G, Adelson M, 1999. Characteristics of benzodiazepine abuse in methadone maintenance treatment patients: A 1 year prospective study in an Israeli clinic. Drug Alcohol Depend. 55, 63–68. [DOI] [PubMed] [Google Scholar]
- Ghitza UE, Epstein DH, Preston KL, 2008. Self-report of illicit benzodiazepine use on the Addiction Severity Index predicts treatment outcome. Drug Alcohol Depend. 97, 150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilchrist G, Atkinson J, Gruer L, 2006. Illicit tranquilliser use and dependence among female opiate users. Drug Alcohol Rev. 25, 459–461. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Hasin DS, 2002. Sedative use and misuse in the United States. Addiction 97, 555–562. [DOI] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Treacy S, Marsden J, 2002. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction 97, 39–47. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, Jiao R, Ren W, Goldstein R, n.d. National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III), Source and Accuracy Statement; National Institute on Alcohol Abuse and Alcoholism, Rockville, MD: https://www.niaaa.nih.gov/research/nesarc-iii [Google Scholar]
- Griffiths RR, Weerts EM, 1997. Benzodiazepine self-administration in humans and laboratory animals--implications for problems of long-term use and abuse. Psychopharmacology (Berl) 134, 1–37. [DOI] [PubMed] [Google Scholar]
- Guo L, Xu Y, Deng J, Huang J, Huang G, Gao X, Wu H, Pan S, Zhang WH, Lu C, 2016. Association between nonmedical use of prescription drugs and suicidal behavior among adolescents. JAMA Pediatr. 170, 971–978. [DOI] [PubMed] [Google Scholar]
- Hakansson A, Schlyter F, Berglund M, 2008. Factors associated with history of non-fatal overdose among opioid users in the Swedish criminal justice system. Drug Alcohol Depend. 94, 48–55. [DOI] [PubMed] [Google Scholar]
- Hall W, Bell J, Carless J, 1993. Crime and drug use among applicants for methadone maintenance. Drug Alcohol Depend. 31, 123–129. [DOI] [PubMed] [Google Scholar]
- Hall W, Teesson M, Lynskey M, Degenhardt L, 1999. The 12-month prevalence of substance use and ICD-10 substance use disorders in Australian adults: Findings from the National Survey of Mental Health and Well-Being. Addiction 94, 1541–1550. [PubMed] [Google Scholar]
- Hammersley R, Lavelle T, Forsyth A, 1992. Predicting initiation to and cessation of buprenorphine and temazepam use amongst adolescents. Br. J. Addict 87, 1303–1311. [DOI] [PubMed] [Google Scholar]
- Hammersley R, Morrison V, 1987. Effects of Polydrug Use on the Criminal Activities of Heroin‐users. Addiction 82, 899–906. [DOI] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM, 2017. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann. Intern. Med 167, 293–301. [DOI] [PubMed] [Google Scholar]
- Han B, Compton WM, Jones CM, Cai R, 2015. Nonmedical Prescription Opioid Use and Use Disorders Among Adults Aged 18 Through 64 Years in the United States, 2003–2013. JAMA 314, 1468–1478. [DOI] [PubMed] [Google Scholar]
- Havens JR, Lofwall MR, Frost SD, Oser CB, Leukefeld CG, Crosby RA, 2013. Individual and network factors associated with prevalent hepatitis C infection among rural Appalachian injection drug users. Am. J. Public Health 103, e44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens JR, Oser CB, Knudsen HK, Lofwall M, Stoops WW, Walsh SL, Leukefeld CG, Kral AH, 2011. Individual and network factors associated with non-fatal overdose among rural Appalachian drug users. Drug Alcohol Depend. 115, 107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens JR, Walker R, Leukefeld CG, 2010. Benzodiazepine use among rural prescription opioids users in a community-based study. J. Addict. Med 4, 137–139. [DOI] [PubMed] [Google Scholar]
- Hayashi K, Suwannawong P, Ti L, Kaplan K, Wood E, Kerr T, 2013. High rates of midazolam injection and associated harms in Bangkok, Thailand. Addiction 108, 944–952. [DOI] [PubMed] [Google Scholar]
- Hearon BA, Calkins AW, Halperin DM, McHugh RK, Murray HW, Otto MW, 2011. Anxiety sensitivity and illicit sedative use among opiate-dependent women and men. Am. J. Drug Alcohol Abuse 37, 43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Martins SS, Malcolm RJ, Floyd L, Cavanaugh CE, Latimer WW, 2010. Patterns of illegal drug use among an adult alcohol dependent population: Results from the National Survey on Drug Use and Health. Drug Alcohol Depend. 106, 119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmus TC, Tancer M, Johanson CE, 2005. Reinforcing effects of diazepam under anxiogenic conditions in individuals with social anxiety. Exp. Clin. Psychopharmacol 13, 348–356. [DOI] [PubMed] [Google Scholar]
- Hoiseth G, Tuv SS, Karinen R, 2016. Blood concentrations of new designer benzodiazepines in forensic cases. Forensic Sci. Int 268, 35–38. [DOI] [PubMed] [Google Scholar]
- Horyniak D, Dietze P, Degenhardt L, Agius P, Higgs P, Bruno R, Alati R, Burns L, 2016. Age-related differences in patterns of criminal activity among a large sample of polydrug injectors in Australia. J. Subst. Use 21, 48–56. [Google Scholar]
- Horyniak D, Reddel S, Quinn B, Dietze P, 2012. The use of alprazolam by people who inject drugs in Melbourne, Australia. Drug Alcohol Rev. 31, 585–590. [DOI] [PubMed] [Google Scholar]
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, Saha TD, Smith SM, Goldstein RB, Grant BF, 2006. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry 67, 1062–1073. [DOI] [PubMed] [Google Scholar]
- Hughes A, Williams MR, Lipari RN, Bose J, Copello EAP, Kroutil LA, 2016. Prescription drug use and misuse in the United States: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR2-2015/NSDUH-FFR2-2015.htm
- Huppertz LM, Moosmann B, Auwarter V, 2018. Flubromazolam - Basic pharmacokinetic evaluation of a highly potent designer benzodiazepine. Drug Test Anal. 10, 206–211. [DOI] [PubMed] [Google Scholar]
- Hwang CS, Kang EM, Kornegay CJ, Staffa JA, Jones CM, McAninch JK, 2016. Trends in the Concomitant Prescribing of Opioids and Benzodiazepines, 2002–2014. Am. J. Prev. Med 51, 151–160. [DOI] [PubMed] [Google Scholar]
- Ibanez GE, Levi-Minzi MA, Rigg KK, Mooss AD, 2013. Diversion of benzodiazepines through healthcare sources. J. Psychoactive Drugs 45, 48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickowicz S, Hayashi K, Dong H, Milloy MJ, Kerr T, Montaner JS, Wood E, 2015. Benzodiazepine use as an independent risk factor for HIV infection in a Canadian setting. Drug Alcohol Depend. 155, 190–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iguchi MY, Handelsman L, Bickel WK, Griffiths RR, 1993. Benzodiazepine and sedative use/abuse by methadone maintenance clients. Drug Alcohol Depend. 32, 257–266. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Cicero TJ, Rosenblum A, Ahwah C, Bailey JE, Dart RC, Burke JJ, 2010. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 110, 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins LM, Banta-Green CJ, Maynard C, Kingston S, Hanrahan M, Merrill JO, Coffin PO, 2011. Risk factors for nonfatal overdose at Seattle-area syringe exchanges. J. Urban Health 88, 118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiraporncharoen W, Likhitsathian S, Lerssrimongkol C, Jiraniramai S, Siriluck L, Angkurawaranon C, 2016. Sedative use: Its association with harmful alcohol use, harmful tobacco use and quality of life among health care workers in Thailand. J. Subst. Use 21, 414–422. [Google Scholar]
- Johnson KM, Fibbi M, Langer D, Silva K, Lankenau SE, 2013. Prescription drug misuse and risk behaviors among young injection drug users. J. Psychoactive Drugs 45, 112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Bachman JG, O’Malley PM, Schulenberg JE, 2015. Monitoring the Future: A Continuing Study of American Youth (8th- and 10th-Grade Surveys), 2013. Inter-university Consortium for Political and Social Research, Ann Arbor, MI: http://www.monitoringthefuture.org/ [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME, 2018. Monitoring the Future national survey results on drug use: 1975–2017: Overview, key findings on adolescent drug use. Institute for Social Research, The University of Michigan, Ann Arbor, MI: http://www.monitoringthefuture.org/ [Google Scholar]
- Johnston LD, O’Malley PM, 1986. Why do the nation’s students use drugs and alcohol? Self-reported reasons from nine national surveys. J. Drug Issues 16, 29–66. [Google Scholar]
- Jones CM, 2017. The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence - An assessment of demographic and substance use trends, United States, 2003–2014. Addict. Behav 65, 229–235. [DOI] [PubMed] [Google Scholar]
- Jones CM, McAninch JK, 2015. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am. J. Prev. Med 49, 493–501. [DOI] [PubMed] [Google Scholar]
- Jones CM, McCance-Katz EF, 2019. Co-Occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 197, 78–82. [DOI] [PubMed] [Google Scholar]
- Jones CM, Paulozzi LJ, Mack KA, 2014. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths - United States, 2010. MMWR Morb. Mortal. Wkly. Rep 63, 881–885. [PMC free article] [PubMed] [Google Scholar]
- Jones JD, Mogali S, Comer SD, 2012. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 125, 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan W, Jian-Xiong D, Lan G, Yuan H, Xue G, Jing-Hui H, Guo-Liang H, Ci-Yong L, 2015. Non-medical use of psychoactive drugs in relation to suicide tendencies among Chinese adolescents. Addict. Behav 51, 31–37. [DOI] [PubMed] [Google Scholar]
- Kamal F, Flavin S, Campbell F, Behan C, Fagan J, Smyth R, 2007. Factors affecting the outcome of methadone maintenance treatment in opiate dependence. Ir. Med. J 100, 393–397. [PubMed] [Google Scholar]
- Kan CC, Breteler MHM, van der Ven AHGS, Timmermans MAY, Zitman FG, 2001. Assessment of benzodiazepine dependence in alcohol and drug dependent outpatients: A research report. Subst. Use Misuse 36, 1085–1109. [DOI] [PubMed] [Google Scholar]
- Kapil V, Green JL, Le Lait C, Wood DM, Dargan PI, 2014. Misuse of benzodiazepines and Z-drugs in the UK. Br. J. Psychiatry 205, 407–408. [DOI] [PubMed] [Google Scholar]
- Kecojevic A, Corliss HL, Lankenau SE, 2015a. Motivations for prescription drug misuse among young men who have sex with men (YMSM) in Philadelphia. Int. J. Drug Policy 26, 764–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Silva K, Sell RL, Lankenau SE, 2015b. Prescription drug misuse and sexual risk behaviors among young men who have sex with men (YMSM) in Philadelphia. AIDS Behav. 19, 847–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Wong CF, Corliss HL, Lankenau SE, 2015c. Risk factors for high levels of prescription drug misuse and illicit drug use among substance-using young men who have sex with men (YMSM). Drug Alcohol Depend. 150, 156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellogg S, Melia D, Khuri E, Lin A, Ho A, Kreek MJ, 2006. Adolescent and young adult heroin patients: drug use and success in methadone maintenance treatment. J. Addict. Dis 25, 15–25. [DOI] [PubMed] [Google Scholar]
- Kelly BC, Parsons JT, 2007. Prescription drug misuse among club drug-using young adults. Am. J. Drug Alcohol Abuse 33, 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly BC, Parsons JT, 2010. Prevalence and predictors of non-medical prescription drug use among men who have sex with men. Addict. Behav 35, 312–317. [DOI] [PubMed] [Google Scholar]
- Kelly BC, Rendina HJ, Vuolo M, Wells BE, Parsons JT, 2015a. Influences of motivational contexts on prescription drug misuse and related drug problems. J. Subst. Abuse Treat 48, 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly BC, Vuolo M, Pawson M, Wells BE, Parsons JT, 2015b. Chasing the bean: Prescription drug smoking among socially active youth. J. Adolesc. Health 56, 632–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly BC, Wells BE, Leclair A, Tracy D, Parsons JT, Golub SA, 2013. Prevalence and correlates of prescription drug misuse among socially active young adults. Int. J. Drug Policy 24, 297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr T, Fairbairn N, Tyndall M, Marsh D, Li K, Montaner J, Wood E, 2007. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug Alcohol Depend. 87, 39–45. [DOI] [PubMed] [Google Scholar]
- Kerr T, Kiatying-Angsulee N, Fairbairn N, Hayashi K, Suwannawong P, Kaplan K, Lai C, Wood E, 2010. High rates of midazolam injection among drug users in Bangkok, Thailand. Harm. Reduct. J 7, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, 2008. National Comorbidity Survey: Baseline (NCS-1), 1990–1992. Inter-university Consortium for Political and Social Research, Ann Arbor, MI: https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/6693# [Google Scholar]
- Khosla N, Juon HS, Kirk GD, Astemborski J, Mehta SH, 2011. Correlates of non-medical prescription drug use among a cohort of injection drug users in Baltimore City. Addict. Behav 36, 1282–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinner SA, Milloy M, Wood E, Qi J, Zhang R, Kerr T, 2012. Incidence and risk factors for non-fatal overdose among a cohort of recently incarcerated illicit drug users. Addict. Behav 37, 691–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klee H, Faugier J, Hayes C, Boulton T, Morris J, 1990. AIDS-related risk behaviour, polydrug use and temazepam. Br. J. Addict 85, 1125–1132. [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Fotiou A, Arapaki A, Richardson C, 2008. Prevalence, patterns, and correlates of tranquilizer and sedative use among European adolescents. J. Adolesc. Health 43, 584–592. [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Richardson C, Olszewski D, Matias J, Monshouwer K, Bjarnason T, 2012. Multiple substance use and self-reported suicide attempts by adolescents in 16 European countries. Eur. Child Adolesc. Psychiatry 21, 443–450. [DOI] [PubMed] [Google Scholar]
- Kurtz SP, Surratt HL, Levi-Minzi MA, Mooss A, 2011. Benzodiazepine dependence among multidrug users in the club scene. Drug Alcohol Depend. 119, 99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladewig D, Grossenbacher H, 1988. Benzodiazepine abuse in patients of doctors in domiciliary practice in the Basle area. Pharmacopsychiatry 21, 104–108. [DOI] [PubMed] [Google Scholar]
- Landreat MG, Vigneau CV, Hardouin JB, Bronnec MG, Marais M, Venisse JL, Jolliet P, 2010. Can we say that seniors are addicted to benzodiazepines? Subst. Use Misuse 45, 1988–1999. [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Sanders B, Bloom JJ, Hathazi DS, Alarcon E, Tortu S, Clatts M, 2007. Prevalence and patterns of prescription drug misuse among young ketamine injectors. J. Drug Issues 37, 717–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankenau SE, Schrager SM, Silva K, Kecojevic A, Bloom JJ, Wong C, Iverson E, 2012a. Misuse of prescription and illicit drugs among high-risk young adults in Los Angeles and New York. J. Public Health Res 1, 22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankenau SE, Teti M, Silva K, Bloom JJ, Harocopos A, Treese M, 2012b. Patterns of prescription drug misuse among young injection drug users. J. Urban Health 89, 1004–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavelle TL, Hammersley R, Forsyth A, 1991. The use of buprenorphine and temazepam by drug injectors. J. Addict. Dis 10, 5–14. [DOI] [PubMed] [Google Scholar]
- Lavie E, Fatseas M, Denis C, Auriacombe M, 2009. Benzodiazepine use among opiate-dependent subjects in buprenorphine maintenance treatment: correlates of use, abuse and dependence. Drug Alcohol Depend. 99, 338–344. [DOI] [PubMed] [Google Scholar]
- Lee SC, Klein-Schwartz W, Doyon S, Welsh C, 2014. Comparison of toxicity associated with nonmedical use of benzodiazepines with buprenorphine or methadone. Drug Alcohol Depend. 138, 118–123. [DOI] [PubMed] [Google Scholar]
- Lembke A, Papac J, Humphreys K, 2018. Our other prescription drug problem. N. Engl. J. Med 378, 693–695. [DOI] [PubMed] [Google Scholar]
- Lev-Ran S, Le Strat Y, Imtiaz S, Rehm J, Le Foll B, 2013. Gender differences in prevalence of substance use disorders among individuals with lifetime exposure to substances: Results from a large representative sample. Am. J. Addict 22, 7–13. [DOI] [PubMed] [Google Scholar]
- Li P, Huang Y, Guo L, Wang W, Xi C, Lei Y, Luo M, Pan S, Deng X, Zhang W-H, Lu C, 2018. Sexual attraction and the nonmedical use of opioids and sedative drugs among Chinese adolescents. Drug Alcohol Depend. 183, 169–175. [DOI] [PubMed] [Google Scholar]
- Licata SC, Rowlett JK, 2008. Abuse and dependence liability of benzodiazepine-type drugs: GABA(A) receptor modulation and beyond. Pharmacol. Biochem. Behav 90, 74–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebrenz M, Schneider M, Buadze A, Gehring MT, Dube A, Caflisch C, 2015. High-dose benzodiazepine dependence: A qualitative study of patients’ perceptions on initiation, reasons for use, and obtainment. PLoS One 10, e0142057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsley CW, 2012. The top prescription drugs of 2011 in the United States: Antipsychotics and antidepressants once again lead CNS therapeutics. ACS Chem. Neurosci 3, 630–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugoboni F, Mirijello A, Faccini M, Casari R, Cossari A, Musi G, Bissoli G, Quaglio G, Addolorato G, 2014. Quality of life in a cohort of high-dose benzodiazepine dependent patients. Drug Alcohol Depend. 142, 105–109. [DOI] [PubMed] [Google Scholar]
- Malcolm R, Brady KT, Johnston AL, Cunningham M, 1993. Types of benzodiazepines abused by chemically dependent inpatients. J. Psychoactive Drugs 25, 315–319. [DOI] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Nelson EC, 2009. Are non-fatal opioid overdoses misclassified suicide attempts? Comparing the associated correlates. Addict. Behav 34, 723–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manconi M, Ferri R, Miano S, Maestri M, Bottasini V, Zucconi M, Ferini-Strambi L, 2017. Sleep architecture in insomniacs with severe benzodiazepine abuse. Clin. Neurophysiol 128, 875–881. [DOI] [PubMed] [Google Scholar]
- Martins SS, Gorelick DA, 2011. Conditional substance abuse and dependence by diagnosis of mood or anxiety disorder or schizophrenia in the U.S. population. Drug Alcohol Depend. 119, 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateu-Gelabert P, Jessell L, Goodbody E, Kim D, Gile K, Teubl J, Syckes C, Ruggles K, Lazar J, Friedman S, 2017. High enhancer, downer, withdrawal helper: Multifunctional nonmedical benzodiazepine use among young adult opioid users in New York City. Int. J. Drug Policy 46, 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maust DT, Lin LA Blow FC, 2018. Benzodiazepine use and misuse among adults in the United States. Psychiatr. Serv 70, 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza M, Losurdo A, Testani E, Marano G, Di Nicola M, Dittoni S, Gnoni V, Di Blasi C, Giannantoni NM, Lapenta L, Brunetti V, Bria P, Janiri L, Mazza S, Della Marca G, 2014. Polysomnographic findings in a cohort of chronic insomnia patients with benzodiazepine abuse. J. Clin. Sleep Med 10, 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, 2005. Correlates of nonmedical use of prescription benzodiazepine anxiolytics: Results from a national survey of U.S. college students. Drug Alcohol Depend. 79, 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, 2005. Sources of prescription drugs for illicit use. Addict. Behav 30, 1342–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ, 2006a. The relationship between past-year drinking behaviors and nonmedical use of prescription drugs: Prevalence of co-occurrence in a national sample. Drug Alcohol Depend. 84, 281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ, 2006b. Medical use, illicit use, and diversion of abusable prescription drugs. J. Am. Coll. Health 54, 269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Young A, 2007a. Medical and nonmedical use of prescription drugs among secondary school students. J. Adolesc. Health 40, 76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Morales M, Cranford JA, Boyd CJ, 2007b. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction 102, 1920–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Teter CJ, 2009. Subtypes of nonmedical prescription drug misuse. Drug Alcohol Depend. 102, 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Cranford JA, Ross-Durow P, Young A, Teter CJ, Boyd CJ, 2011a. Medical misuse of controlled medications among adolescents. Arch. Pediatr. Adolesc. Med 165, 729–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Ross-Durow P, Young A, Boyd CJ, 2011b. Characteristics associated with the diversion of controlled medications among adolescents. Drug Alcohol Depend. 118, 452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, 2012. Motivational subtypes of nonmedical use of prescription medications: Results from a national study. J. Adolesc. Health 51, 445–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, 2014. Medical and nonmedical use of prescription benzodiazepine anxiolytics among U.S. high school seniors. Addict. Behav 39, 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Boyd CJ, 2014. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addict. Behav 39, 1176–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, Boyd CJ, Schulenberg JE, 2017a. Medical and nonmedical use of prescription sedatives and anxiolytics: Adolescents’ use and substance use disorder symptoms in adulthood. Addict. Behav 65, 296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, Patrick ME, 2017b. High-intensity drinking and nonmedical use of prescription drugs: Results from a national survey of 12th grade students. Drug Alcohol Depend. 178, 372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ, Wilens TE, Schepis TS, 2018. Sources of prescription medication misuse among young adults in the United States: The role of educational status. J. Clin. Psychiatry 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor C, Darke S, Ali R, Christie P, 1998. Experience of non‐fatal overdose among heroin users in Adelaide, Australia: circumstances and risk perceptions. Addiction 93, 701–711. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Nielsen S, Weiss RD, 2015. Prescription drug abuse: From epidemiology to public policy. J. Subst. Abuse Treat 48, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Geyer R, Karakula S, Griffin ML, Weiss RD, 2018. Nonmedical benzodiazepine use in adults with alcohol use disorder: The role of anxiety sensitivity and polysubstance use. Am. J. Addict. 27, 485–490. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Votaw VR, Bogunovic O, Karakula SL, Griffin ML, Weiss RD, 2017. Anxiety sensitivity and nonmedical benzodiazepine use among adults with opioid use disorder. Addict. Behav 65, 283–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLarnon ME, Monaghan TL, Stewart SH, Barrett SP, 2011. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy 31, 262. [DOI] [PubMed] [Google Scholar]
- McLarnon ME, Darredeau C, Chan J, Barrett SP, 2014. Motives for the non-prescribed use of psychiatric medications: Relationships with psychopathology, other substance use and patterns of use. J. Subst. Use 19, 421–428. [Google Scholar]
- Messina BG, Dutta NM, Silvestri MM, Diulio AR, Garza KB, Murphy JG, Correia CJ, 2016. Modeling motivations for non-medical use of prescription drugs. Addict. Behav 52, 46–51. [DOI] [PubMed] [Google Scholar]
- Metzger D, Woody GE, De Philippis D, McLellan AT, O’Brien CP, Platt J, 1991. Risk factors for needle sharing among methadone-treated patients. Am. J. Psychiatry 148, 636–640. [DOI] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, Bachman JG, O’Malley PM, Schulenberg JE, 2018a. Monitoring the Future: A Continuing Study of American Youth (8thand 10th-Grade Surveys), 2017. Inter-university Consortium for Political and Social Research, Ann Arbor, MI: https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/37183 [Google Scholar]
- Miech RA, Johnston LD, Bachman JG, O’Malley PM, Schulenberg JE, 2018b. Monitoring the Future: A Continuing Study of American Youth (12th-Grade Survey), 2017. Inter-university Consortium for Political and Social Research, Ann Arbor, MI: https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/37182# [Google Scholar]
- Millson P, Challacombe L, Villeneuve PJ, Strike CJ, Fischer B, Myers T, Shore R, Hopkins S, 2006. Determinants of health-related quality of life of opiate users at entry to low-threshold methadone programs. Eur. Addict. Res 12, 74–82. [DOI] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, 2015. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev 4, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitra E, Anderson BJ, Stein MD, 2013. Perceived stress and substance use in methadone-maintained smokers. Drug Alcohol Depend. 133, 785–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TJ, Mattison DR, 2017. Adult Utilization of psychiatric drugs and differences by sex, age, and race. JAMA Intern. Med 177, 274–275. [DOI] [PubMed] [Google Scholar]
- Morel A, Grall-Bronnec M, Bulteau S, Chauvin-Grelier P, Gailledrat L, Pinot ML, Jolliet P, Victorri-Vigneau C, 2016. Benzodiazepine dependence in subjects with alcohol use disorders: what prevalence? Expert Opin. Drug Saf 15, 1313–1319. [DOI] [PubMed] [Google Scholar]
- Morin CM, Bastien C, Guay B, Radouco-Thomas M, Leblanc J, Vallieres A, 2004. Randomized clinical trial of supervised tapering and cognitive behavior therapy to facilitate benzodiazepine discontinuation in older adults with chronic insomnia. Am. J. Psychiatry 161, 332–342. [DOI] [PubMed] [Google Scholar]
- Moses TEH, Lundahl LH, Greenwald MK, 2018. Factors associated with sedative use and misuse among heroin users. Drug Alcohol Depend. 185, 10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta-Ochoa R, Bertrand K, Arruda N, Jutras-Aswad D, Roy E, 2017. “I love having benzos after my coke shot”: The use of psychotropic medication among cocaine users in downtown Montreal. Int. J. Drug Policy 49, 15–23. [DOI] [PubMed] [Google Scholar]
- Mulvaney FD, Brown LS Jr., Alterman AI, Sage RE, Cnaan A, Cacciola J, Rutherford M, 1999. Methadone-maintenance outcomes for Hispanic and African-American men and women. Drug Alcohol Depend. 54, 11–18. [DOI] [PubMed] [Google Scholar]
- Murphy KD, Byrne S, McCarthy S, Lambert S, Sahm LJ, 2014. Benzodiazepine use among young attendees of an Irish substance treatment center. J. Addict. Med 8, 199–204. [DOI] [PubMed] [Google Scholar]
- Naji L, Dennis BB, Bawor M, Plater C, Pare G, Worster A, Varenbut M, Daiter J, Marsh DC, Desai D, Thabane L, Samaan Z, 2016. A prospective study to investigate predictors of relapse among patients with opioid use disorder treated with methadone. Subst. Abuse 10, 9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, n.d. National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III), Alcohol, Drug, and Medicine Guide. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, 2010. Alcohol use and alcohol use disorders in the United States, a 3-year follow-up: Main findings from the 2004–2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). US Alcohol Epidemiologic Data Reference Manual, Bethesda, MD: https://pubs.niaaa.nih.gov/publications/manual.htm [Google Scholar]
- National Institute on Drug Abuse, 2018. Benzodiazepines and opioids. https://www.drugabuse.gov/drugs-abuse/opioids/benzodiazepinesopioids#Reference.accessed on January 1, 2019.
- Nattala P, Leung KS, Abdallah AB, Cottler LB, 2011. Heavy use versus less heavy use of sedatives among non-medical sedative users: Characteristics and correlates. Addict. Behav 36, 103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nattala P, Leung KS, Abdallah AB, Murthy P, Cottler LB, 2012. Motives and simultaneous sedative-alcohol use among past 12-month alcohol and nonmedical sedative users. Am. J. Drug Alcohol Abuse 38, 359–364. [DOI] [PubMed] [Google Scholar]
- Navaratnam V, Foong K, 1990. Opiate dependence–the role of benzodiazepines. Curr. Med. Res. Opin 11, 620–630. [DOI] [PubMed] [Google Scholar]
- Neale J, 2000. Suicidal intent in non-fatal illicit drug overdose. Addiction 95, 85–93. [DOI] [PubMed] [Google Scholar]
- Neale J, Robertson M, 2005. Recent life problems and non‐fatal overdose among heroin users entering treatment. Addiction 100, 168–175. [DOI] [PubMed] [Google Scholar]
- Neira-Leon M, Barrio G, Brugal MT, de la Fuente L, Ballesta R, Bravo MJ, Silva TC, Rodriguez-Martos A, 2006. Do young heroin users in Madrid, Barcelona and Seville have sufficient knowledge of the risk factors for unintentional opioid overdose? J. Urban Health 83, 477–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng W, Mythily S, Song G, Chan Y, Winslow M, 2007. Concomitant use of midazolam and buprenorphine and its implications among drug users in Singapore. Ann. Acad. Med. Singap 36, 774. [PubMed] [Google Scholar]
- Nielsen S, Dietze P, Lee N, Dunlop A, Taylor D, 2007. Concurrent buprenorphine and benzodiazepines use and self-reported opioid toxicity in opioid substitution treatment. Addiction 102, 616–622. [DOI] [PubMed] [Google Scholar]
- Nielsen S, Bruno R, Degenhardt L, Stoove MA, Fischer JA, Carruthers SJ, Lintzeris N, 2013. The sources of pharmaceuticals for problematic users of benzodiazepines and prescription opioids. Med. J. Aust 199, 696–699. [DOI] [PubMed] [Google Scholar]
- Nirenberg TD, Cellucci T, Liepman MR, Swift RM, Sirota AD, 1996. Cannabis versus other illicit drug use among methadone maintenance patients. Psychol. Addict. Behav 10, 222. [Google Scholar]
- Ochoa KC, Davidson PJ, Evans JL, Hahn JA, Page-Shafer K, Moss AR, 2005. Heroin overdose among young injection drug users in San Francisco. Drug Alcohol Depend. 80, 297–302. [DOI] [PubMed] [Google Scholar]
- Ogborne AC, Kapur BM, 1987. Drug use among a sample of males admitted to an alcohol detoxication center. Alcohol. Clin. Exp. Res 11, 183–185. [DOI] [PubMed] [Google Scholar]
- Olfson M, King M, Schoenbaum M, 2015. Benzodiazepine use in the United States. JAMA Psychiatry 72, 136–142. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Sachs GS, Reiter SR, Meltzer-Brody S, Rosenbaum JF, 1993. Discontinuation of benzodiazepine treatment: Efficacy of cognitive-behavioral therapy for patients with panic disorder. Am. J. Psychiatry 150, 1485–1490. [DOI] [PubMed] [Google Scholar]
- Otto MW, McHugh RK, Simon NM, Farach FJ, Worthington JJ, Pollack MH, 2010. Efficacy of CBT for benzodiazepine discontinuation in patients with panic disorder: Further evaluation. Behav. Res. Ther 48, 720–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyefeso A, Ghodse H, Williams H, 1996. Prevalence and pattern of benzodiazepine abuse and dependence among patients in a methadone detoxification programme: A repeated cross-sectional analysis (benzodiazepine abuse among opiate addicts). Addict. Res 4, 57–64. [Google Scholar]
- Palamar JJ, Han BH, Martins SS, 2019. Shifting characteristics of nonmedical prescription tranquilizer users in the United States, 2005–2014. Drug Alcohol Depend. 195, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks KA, Frone MR, Muraven M, Boyd C, 2017. Nonmedical use of prescription drugs and related negative sexual events: Prevalence estimates and correlates in college students. Addict. Behav 65, 258–263. [DOI] [PubMed] [Google Scholar]
- Pattanayak RD, Jain R, Ray R, 2010. Comparison of self-reported benzodiazepine use and urinalysis among consecutive treatment seekers at a tertiary care drug dependence treatment centre. Indian J. Physiol. Pharmacol 54, 337–343. [PubMed] [Google Scholar]
- Pauly V, Pradel V, Pourcel L, Nordmann S, Frauger E, Lapeyre-Mestre M, Micallef J, Thirion X, 2012. Estimated magnitude of diversion and abuse of opioids relative to benzodiazepines in France. Drug Alcohol Depend. 126, 13–20. [DOI] [PubMed] [Google Scholar]
- Pavarin RM, 2015. Mortality risk among heroin abusers: Clients and non-clients of public treatment centers for drug addiction. Subst. Use Misuse 50, 1690–1696. [DOI] [PubMed] [Google Scholar]
- Payne J, Gaffney A, 2012. How much crime is drug or alcohol related? Self-reported attributions of police detainees. Trends and Issues in Crime and Criminal Justice 439, 1. [Google Scholar]
- Peles E, Adelson M, 2006. Gender differences and pregnant women in a methadone maintenance treatment (MMT) clinic. J. Addict. Dis 25, 39–45. [DOI] [PubMed] [Google Scholar]
- Peles E, Schreiber S, Adelson M, 2006. Factors predicting retention in treatment: 10-year experience of a methadone maintenance treatment (MMT) clinic in Israel. Drug Alcohol Depend. 82, 211–217. [DOI] [PubMed] [Google Scholar]
- Peles E, Schreiber S, Adelson M, 2009. Documented poor sleep among methadone-maintained patients is associated with chronic pain and benzodiazepine abuse, but not with methadone dose. Eur. Neuropsychopharmacol 19, 581–588. [DOI] [PubMed] [Google Scholar]
- Peles E, Schreiber S, Adelson M, 2010. 15-Year survival and retention of patients in a general hospital-affiliated methadone maintenance treatment (MMT) center in Israel. Drug Alcohol Depend. 107, 141–148. [DOI] [PubMed] [Google Scholar]
- Perera KM, Tulley M, Jenner FA, 1987. The use of benzodiazepines among drug addicts. Br. J. Addict 82, 511–515. [DOI] [PubMed] [Google Scholar]
- Pickover AM, Messina BG, Correia CJ, Garza KB, Murphy JG, 2016. A behavioral economic analysis of the nonmedical use of prescription drugs among young adults. Exp. Clin. Psychopharmacol 24, 38–47. [DOI] [PubMed] [Google Scholar]
- Preuss UW, Schuckit MA, Smith TL, Danko GP, Bucholz KK, Hesselbrock MN, Hesselbrock V, Kramer JR, 2003. Predictors and correlates of suicide attempts over 5 years in 1,237 alcohol-dependent men and women. Am. J. Psychiatry 160, 56–63. [DOI] [PubMed] [Google Scholar]
- Proctor SL, Copeland AL, Kopak AM, Hoffmann NG, Herschman PL, Polukhina N, 2015. Predictors of patient retention in methadone maintenance treatment. Psychol. Addict. Behav 29, 906. [DOI] [PubMed] [Google Scholar]
- Puangkot S, Laohasiriwong W, Saengsuwan J, Chiawiriyabunya I, 2010. Benzodiazepines misuse: The study community level Thailand. Indian J. Psychol. Med 32, 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quaglio G, Pattaro C, Gerra G, Mathewson S, Verbanck P, Des Jarlais DC, Lugoboni F, 2012. High dose benzodiazepine dependence: Description of 29 patients treated with flumazenil infusion and stabilised with clonazepam. Psychiatry Res. 198, 457–462. [DOI] [PubMed] [Google Scholar]
- Quintero G, Peterson J, Young B, 2006. An exploratory study of socio-cultural factors contributing to prescription drug misuse among college students. J. Drug Issues 36, 903–931. [Google Scholar]
- Quintero G, 2012. Problematizing “drugs”: A cultural assessment of recreational pharmaceutical use among young adults in the United States. Contemp. Drug Probl 39, 493–535. [PMC free article] [PubMed] [Google Scholar]
- Raffa JD, Grebely J, Tossonian H, Wong T, Viljoen M, Khara M, Mead A, McLean M, Duncan F, Petkau AJ, DeVlaming S, Conway B, 2007. The impact of ongoing illicit drug use on methadone adherence in illicit drug users receiving treatment for HIV in a directly observed therapy program. Drug Alcohol Depend. 89, 306–309. [DOI] [PubMed] [Google Scholar]
- Rigg KK, Ibanez GE, 2010. Motivations for non-medical prescription drug use: A mixed methods analysis. J. Subst. Abuse Treat 39, 236–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigg KK, Ford JA, 2014. The misuse of benzodiazepines among adolescents: Psychosocial risk factors in a national sample. Drug Alcohol Depend. 137, 137–142. [DOI] [PubMed] [Google Scholar]
- Riley ED, Evans JL, Hahn JA, Briceno A, Davidson PJ, Lum PJ, Page K, 2016. A longitudinal study of multiple drug use and overdose among young people who inject drugs. Am. J. Public Health 106, 915–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooney S, Kelly G, Bamford L, Sloan D, O’Connor JJ, 1999. Co-abuse of opiates and benzodiazepines. Ir. J. Med. Sci 168, 36–41. [DOI] [PubMed] [Google Scholar]
- Ross HE, 1993. Benzodiazepine use and anxiolytic abuse and dependence in treated alcoholics. Addiction 88, 209–218. [DOI] [PubMed] [Google Scholar]
- Ross J, Darke S, Hall W, 1996. Benzodiazepine use among heroin users in Sydney: Patterns of use, availability and procurement. Drug Alcohol Rev. 15, 237–243. [DOI] [PubMed] [Google Scholar]
- Ross J, Darke S, 2000. The nature of benzodiazepine dependence among heroin users in Sydney, Australia. Addiction 95, 1785–1793. [DOI] [PubMed] [Google Scholar]
- Rossow I, Lauritzen G, 1999. Balancing on the edge of death: Suicide attempts and life‐threatening overdoses among drug addicts. Addiction 94, 209–219. [DOI] [PubMed] [Google Scholar]
- Rowe C, Santos GM, Behar E, Coffin PO, 2016. Correlates of overdose risk perception among illicit opioid users. Drug Alcohol Depend. 159, 234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy E, Arruda N, Jutras-Aswad D, Berbiche D, Motta-Ochoa R, Bruneau J, 2018. Tranquilizer misuse among active cocaine users: Predictors of initiation. Drug Alcohol Rev. 37, 520–526. [DOI] [PubMed] [Google Scholar]
- Ruben SM, Morrison CL, 1992. Temazepam misuse in a group of injecting drug users. Br. J. Addict 87, 1387–1392. [DOI] [PubMed] [Google Scholar]
- Schepis TS, Krishnan-Sarin S, 2008. Characterizing adolescent prescription misusers: A population-based study. J. Am. Acad. Child Adolesc. Psychiatry 47, 745–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Hakes JK, 2011. Non‐medical prescription use increases the risk for the onset and recurrence of psychopathology: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction 106, 2146–2155. [DOI] [PubMed] [Google Scholar]
- Schepis TS, McCabe SE, 2012. Exploring age of onset as a causal link between major depression and nonmedical use of prescription medications. Drug Alcohol Depend. 120, 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Hakes JK, 2013. Dose-related effects for the precipitation of psychopathology by opioid or tranquilizer/sedative nonmedical prescription use: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Addict. Med 7, 39–44. [DOI] [PubMed] [Google Scholar]
- Schepis TS, McCabe SE, 2016. Trends in older adult nonmedical prescription drug use prevalence: Results from the 2002–2003 and 2012–2013 National Survey on Drug Use and Health. Addict. Behav 60, 219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, West BT, Teter CJ, McCabe SE, 2016. Prevalence and correlates of co-ingestion of prescription tranquilizers and other psychoactive substances by U.S. high school seniors: Results from a national survey. Addict. Behav 52, 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Teter CJ, McCabe SE, 2018a. Prescription drug use, misuse and related substance use disorder symptoms vary by educational status and attainment in US adolescents and young adults. Drug Alcohol Depend. 189, 172–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Teter CJ, Simoni-Wastila L, McCabe SE, 2018b. Prescription tranquilizer/sedative misuse prevalence and correlates across age cohorts in the US. Addict. Behav 87, 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Simoni-Wastila L, McCabe SE, 2019. Prescription opioid and benzodiazepine misuse is associated with suicidal ideation in older adults. Int. J. Geriatr. Psychiatry 34, 122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff M, Levit S, Moreno RC, 2007. Retention and illicit drug use among methadone patients in Israel: A gender comparison. Addict. Behav 32, 2108–2119. [DOI] [PubMed] [Google Scholar]
- Schneider R Jr., Ottoni GL, de Carvalho HW, Elisabetsky E, Lara DR, 2015. Temperament and character traits associated with the use of alcohol, cannabis, cocaine, benzodiazepines, and hallucinogens: Evidence from a large Brazilian web survey. Braz. J. Psychiatry 37, 31–39. [DOI] [PubMed] [Google Scholar]
- Schuman-Olivier Z, Hoeppner BB, Weiss RD, Borodovsky J, Shaffer HJ, Albanese MJ, 2013. Benzodiazepine use during buprenorphine treatment for opioid dependence: Clinical and safety outcomes. Drug Alcohol Depend. 132, 580–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadick R, Dagirmanjian FB, Trub L, Dawson H, 2016. Sexual orientation and first-year college students’ nonmedical use of prescription drugs. J. Am. Coll. Health 64, 292–299. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, LaSalvia TA, 1992. Patterns of substance use among methadone maintenance patients. Indicators of outcome. J. Subst. Abuse Treat 9, 143–147. [DOI] [PubMed] [Google Scholar]
- Shand FL, Degenhardt L, Slade T, Nelson EC, 2011. Sex differences amongst dependent heroin users: Histories, clinical characteristics and predictors of other substance dependence. Addict. Behav 36, 27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Cheng Y, Kral AH, 2007. Prevalence and correlates of opiate overdose among young injection drug users in a large US city. Drug Alcohol Depend. 88, 182–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva K, Kecojevic A, Lankenau SE, 2013a. Perceived drug use functions and risk reduction practices among high-risk nonmedical users of prescription drugs. J. Drug Issues 43, 483–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva K, Schrager SM, Kecojevic A, Lankenau SE, 2013b. Factors associated with history of non-fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Depend. 128, 104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni-Wastila L, Ritter G, Strickler G, 2004. Gender and other factors associated with the nonmedical use of abusable prescription drugs. Subst. Use Misuse 39, 1–23. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L, Strickler G, 2004. Risk factors associated with problem use of prescription drugs. Am. J. Public Health 94, 266–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth BP, Barry J, Keenan E, 2001. Syringe borrowing persists in Dublin despite harm reduction interventions. Addiction 96, 717–727. [DOI] [PubMed] [Google Scholar]
- Specka M, Bonnet U, Heilmann M, Schifano F, Scherbaum N, 2011. Longitudinal patterns of benzodiazepine consumption in a German cohort of methadone maintenance treatment patients. Hum. Psychopharmacol 26, 404–411. [DOI] [PubMed] [Google Scholar]
- Stein MD, Kanabar M, Anderson BJ, Lembke A, Bailey GL, 2016. Reasons for benzodiazepine use among persons seeking opioid detoxification. J. Subst. Abuse Treat 68, 57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Mendelsohn J, Gordon AJ, Dick AW, Burns RM, Sorbero M, Shih RA, Liccardo Pacula R, 2017a. Opioid analgesic and benzodiazepine prescribing among Medicaid-enrollees with opioid use disorders: The influence of provider communities. J. Addict. Dis 36, 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Anderson BJ, Kenney SR, Bailey GL, 2017b. Beliefs about the consequences of using benzodiazepines among persons with opioid use disorder. J. Subst. Abuse Treat 77, 67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer ML, Griffiths RR, McLellan AT, Grabowski J, Hawthorne JW, 1981. Diazepam use among methadone maintenance patients: Patterns and dosages. Drug Alcohol Depend. 8, 189–199. [DOI] [PubMed] [Google Scholar]
- Strang J, Griffiths P, Abbey J, Gossop M, 1994. Survey of use of injected benzodiazepines among drug users in Britain. BMJ 308, 1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, Griffiths P, Powis B, Fountain J, Williamson S, Gossop M, 1999. Which drugs cause overdose among opiate misusers? Study of personal and witnessed overdoses. Drug Alcohol Rev. 18, 253–261. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2012. Comparing and evaluating youth substance use estimates from the National Survey on Drug Use and Health and other surveys. HHS Publication, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/NSDUH-M9-Youth-2012/NSDUH-M9-Youth-2012.pdf [PubMed] [Google Scholar]
- Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S, 2017. Association between concurrent use of prescription opioids and benzodiazepines and overdose: Retrospective analysis. BMJ 356, j760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunjic S, Howard J, 1996. “Non injectables”: Methadone syrup and benzodiazepine injection by methadone-maintained clients. Drug Alcohol Rev. 15, 245–250. [DOI] [PubMed] [Google Scholar]
- Sutherland R, Sindicich N, Barrett E, Whittaker E, Peacock A, Hickey S, Burns L, 2015. Motivations, substance use and other correlates amongst property and violent offenders who regularly inject drugs. Addict. Behav 45, 207–213. [DOI] [PubMed] [Google Scholar]
- Swensen G, Ilett KF, Dusci LJ, Hackett LP, Ong RT, Quigley AJ, Lenton S, Saker R, Caporn J, 1993. Patterns of drug use by participants in the Western Australian methadone program, 1984–1991. Med. J. Aust 159, 373–376. [DOI] [PubMed] [Google Scholar]
- Terry-McElrath YM, O’Malley PM, Johnston LD, 2009. Reasons for drug use among american youth by consumption level, gender, and race/ethnicity: 1976–2005. J. Drug Issues 39, 677–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ti L, Hayashi K, Kaplan K, Suwannawong P, Wood E, Kerr T, 2014. Groin injecting among a community-recruited sample of people who inject drugsin Thailand. Subst. Abuse Treat. Prev. Policy 9, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjagvad C, Clausen T, Handal M, Skurtveit S, 2016. Benzodiazepine prescription for patients in treatment for drug use disorders: A nationwide cohort study in Denmark, 2000–2010. BMC Psychiatry 16, 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker D, Hayashi K, Milloy MJ, Nolan S, Dong H, Kerr T, Wood E, 2016. Risk factors associated with benzodiazepine use among people who inject drugs in an urban Canadian setting. Addict. Behav 52, 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Griensven F, Pitisuttithum P, Vanichseni S, Wichienkuer P, Tappero JW, Sangkum U, Kitayaporn D, Phasithiphol B, Orelind K, Choopanya K, 2005. Trends in the injection of midazolam and other drugs and needle sharing among injection drug users enrolled in the AIDSVAX B/E HIV-1 vaccine trial in Bangkok, Thailand. Int. J. Drug Policy 16, 171–175. [Google Scholar]
- Vigna-Taglianti FD, Burroni P, Mathis F, Versino E, Beccaria F, Rotelli M, Garneri M, Picciolini A, Bargagli AM, 2016. Gender Differences in Heroin Addiction and Treatment: Results from the VEdeTTE Cohort. Subst. Use Misuse 51, 295–309. [DOI] [PubMed] [Google Scholar]
- Vijayaraghavan M, Freitas D, Bangsberg DR, Miaskowski C, Kushel MB, 2014. Non-medical use of non-opioid psychotherapeutic medications in a community-based cohort of HIV-infected indigent adults. Drug Alcohol Depend. 143, 263–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel M, Knopfli B, Schmid O, Prica M, Strasser J, Prieto L, Wiesbeck GA, Dursteler-Macfarland KM, 2013. Treatment or “high”: Benzodiazepine use in patients on injectable heroin or oral opioids. Addict. Behav 38, 2477–2484. [DOI] [PubMed] [Google Scholar]
- Votaw VR, Witkiewitz K, Valeri L, Bogunovic O, McHugh RK, 2019. Nonmedical prescription sedative/tranquilizer use in alcohol and opioid use disorders. Addict. Behav 88, 48–55. [DOI] [PubMed] [Google Scholar]
- Voyer P, Préville M, Roussel M-E, Berbiche D, Béland S-G, 2009. Factors associated with benzodiazepine dependence among community-dwelling seniors. J. Community Health Nurs 26, 101–113. [DOI] [PubMed] [Google Scholar]
- White WL, Campbell MD, Spencer RD, Hoffman HA, Crissman B, DuPont RL, 2014. Patterns of abstinence or continued drug use among methadone maintenance patients and their relation to treatment retention. J. Psychoactive Drugs 46, 114–122. [DOI] [PubMed] [Google Scholar]
- Whiteside LK, Walton MA, Bohnert AS, Blow FC, Bonar EE, Ehrlich P, Cunningham RM, 2013. Nonmedical prescription opioid and sedative use among adolescents in the emergency department. Pediatrics 132, 825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams H, Oyefeso A, Ghodse AH, 1996. Benzodiazepine misuse and dependence among opiate addicts in treatment. Ir. J. Psychol. Med 13, 62–64. [Google Scholar]
- Wines JD Jr., Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH, 2004. Suicidal behavior, drug use and depressive symptoms after detoxification:A 2-year prospective study. Drug Alcohol Depend. 76, S21–29. [DOI] [PubMed] [Google Scholar]
- Wines JD, Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH, 2007. Overdose after detoxification: A prospective study. Drug Alcohol Depend. 89, 161–169. [DOI] [PubMed] [Google Scholar]
- Wixson SE, Brouwer ES, 2014. Sex differences in benzodiazepine use in the HIV-infected population. AIDS Care 26, 1218–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf B, Grohmann R, Biber D, Brenner PM, Rüther E, 1989. Benzodiazepine abuse and dependence in psychiatric inpatients. Pharmacopsychiatry 22, 54–60. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 1992. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. World Health Organization, Geneva: https://www.who.int/substance_abuse/terminology/icd_10/en/ [Google Scholar]
- Wu L-T, Ling W, Burchett B, Blazer DG, Shostak J, Woody GE, 2010. Gender and racial/ethnic differences in addiction severity, HIV risk, and quality of life among adults in opioid detoxification: Results from the National Drug Abuse Treatment Clinical Trials Network. Subst. Abuse Rehabil 1, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, Woody GE, Burchett B, Yang C, Pan JJ, Ling W, 2012. Alcohol and drug dependence symptom items as brief screeners for substance use disorders: Results from the Clinical Trials Network. J. Psychiatr. Res 46, 360–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen CF, Ko CH, Chang YP, Yu CY, Huang MF, Yeh YC, Lin JJ, Chen CS, 2015. Dependence, misuse, and beliefs regarding use of hypnotics by elderly psychiatric patients taking zolpidem, estazolam, or flunitrazepam. Asia Pac. Psychiatry 7, 298–305. [DOI] [PubMed] [Google Scholar]
- Young A, Grey M, Boyd CJ, McCabe SE, 2011. Adolescent sexual assault and the medical and nonmedical use of prescription medication. J. Addict. Nurs 11, 25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AM, Havens JR, 2012. Transition from first illicit drug use to first injection drug use among rural Appalachian drug users: A cross-sectional comparison and retrospective survival analysis. Addiction 107, 587–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Celentano DD, Le Minh N, Latkin CA, Mehta SH, Frangakis C, Ha TV, Mo TT, Sripaipan T, Davis WW, Quan VM, Go VF, 2015. Prevalence and correlates of HCV monoinfection and HIV and HCV coinfection among persons who inject drugs in Vietnam. Eur. J. Gastroenterol. Hepatol 27, 550–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zullig KJ, Divin AL, 2012. The association between non-medical prescription drug use, depressive symptoms, and suicidality among college students. Addict. Behav 37, 890–899. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.