Abstract
Injection drug use and heterosexual transmission from male key populations to their female partners have been the dominant modes of HIV transmission in Vietnam. A demonstration project was conducted to offer immediate antiretroviral therapy (ART) (regardless of CD4 cell count) to HIV-seropositive partners in serodiscordant couples. During March–December 2013, couples HIV testing and counselling (HTC) and immediate ART were offered in two drug use-affected provinces. Of 256 couples receiving couples HTC, 146 (57%) were serodiscordant; 134 (92%) seropositive partners initiated ART irrespective of CD4 cell count. Of these, 86% were male; 57% reported ever using illicit drugs; median CD4 cell count before ART initiation was 374 cells/mm3. Consistent condom use was reported by 58, 70 and 71% among HIV-positive partners at months 0, 3 and 12. At 12 months after ART initiation, 119 (89%) HIV-positive partners were retained in care; 96 (95% of those tested) achieved viral suppression (<1000 copies/ml). Uptake of immediate ART and viral suppression among those initiating ART were high, paving the way for ART regardless of CD4 cell count as national policy in Vietnam.
Keywords: Antiretroviral therapy, HIV, Asia, prevention
Introduction
In Vietnam’s concentrated HIV epidemic, injection drug use has been the dominant mode of HIV transmission. Sexual transmission from people who inject drugs (PWID) – who are predominantly male – to their partners through unprotected sex plays an increasingly important role.1–3 Modelling analysis estimated that the second largest number of new HIV infections in 2015, approximately 25% of new infections, occurred in women who did not themselves engage in injection drug use or sex work and are presumed to be sex partners of men who inject drugs.1 In a serosurvey of female partners of PWID in Dien Bien province in 2012, HIV seroprevalence was 14%.4 Moreover, more than half of new HIV infections among women are estimated to be attributable to the male partner’s risk behaviour.5 Additionally, condom use, particularly with regular partners, among male key populations has not been high.6
A randomized clinical trial (HPTN052) among 1763 HIV serodiscordant couples (97% heterosexual couples) in nine countries reported that initiation of antiretroviral therapy (ART) among HIV-infected persons with CD4 cell count between 350 and 550 cells/mm3 was associated with 93% lower risk of linked partner transmission within serodiscordant couples than delayed ART started among those with CD4 cell count less than 250 cells/mm3.7,8 After the interim results of the HPTN052 trial were reported in 2011,8 the Vietnam Ministry of Health (MOH) started planning how to translate the trial findings into its programme. The national HIV treatment guidelines in Vietnam at the time recommended ART initiation in individuals with CD4 cell count less than 350 cells/mm3 or with clinical stage 3 or 4 disease. Various programmatic questions were raised regarding provision of ART among HIV-infected persons with higher CD4 cell counts, including (1) feasibility and acceptability of couples HIV testing and counselling (HTC) and immediate ART initiation; (2) adherence, retention and viral suppression when ART is started irrespective of CD4 cell count among populations where drug use is prevalent; (3) possible behavioural disinhibition after ART initiation and (4) whether adverse effects of ART might affect adherence among patients with high CD4 cell counts.
Therefore, an implementation research study was designed to answer these programmatic questions, in order to inform potential adoption of earlier initiation of ART as Vietnamese national policy and further optimization of ART programme in Vietnam.
Methods
Study population and sites
The study was conducted in two high-burden provinces: Dien Bien, a mountainous province in northwest Vietnam, and Can Tho, located in the Mekong Delta region in southern Vietnam. HIV prevalence among PWID was 40% in Dien Bien and was 18% in Can Tho; according to national HIV sentinel surveillance, the average HIV prevalence among PWID nationally was approximately 12%.9,10 Couples HTC was offered at 13 HIV HTC service sites (six in Can Tho and seven in Dien Bien) and immediate ART and follow-up of couples was provided at ten HIV outpatient clinics (OPCs) (four in Can Tho and six in Dien Bien); these public HTC sites and OPCs were managed by the MOH with financial support from external donors.
Couples HTC
Since March 2013, couples HTC has been promoted in the two study provinces, after HTC service providers were trained to deliver couples HTC and to address special issues related to partner testing. At HTC sites and OPCs, if one partner was known to be HIV infected or tested HIV-seropositive, he or she was counselled to refer his/her partner for HTC, and mutual disclosure was supported through couples counselling sessions. Persons with HIV infection newly diagnosed at HTC sites that were not offering couples HTC or through provider-initiated HTC services were referred to the study-designated couples HTC sites with their partner. HIV status was established by using the nationally-approved HIV testing algorithm, consisting of one rapid test and two types of enzyme immunoassay. All identified serodiscordant couples were provided with counselling on risk reduction and information about therapeutic and preventive benefits of ART. Couples were then referred to the study OPCs.
Study enrolment and eligibility criteria
Eligible serodiscordant couples were enrolled in the study during March–December 2013. The serodiscordant couples who were either linked from couples HTC services, or found among pre-ART clients at study OPCs (i.e. those not receiving ART and whose partners tested HIV-seronegative), were evaluated for study eligibility. To be eligible, couples had to meet the following criteria: (i) two persons self-reporting ongoing sexual relationship; (ii) residence in Dien Bien or Can Tho province at the time of enrolment; (iii) both partners aged ≥ 18 years; (iv) one partner tested HIV seropositive, and the other tested seronegative and (v) both partners provided written informed consent, which included agreement for couples on mutual disclosure of HIV status, and for seropositive partners to start ART immediately regardless of CD4 cell count.
Behavioural assessment and counselling for the couples
Upon enrolment, couples were asked individually about demographic characteristics and behaviours relevant to HIV transmission, such as condom use, the number of sexual partners, drug use and injection behaviours. Through counselling, concomitant use of other methods to prevent HIV transmission was promoted (e.g. condoms, clean needles and methadone maintenance therapy were made available free of charge for key populations). Couples were asked to return for behavioural assessment and counselling at 3, 6 and 12 months after the HIV-positive partner initiated ART. Couples were followed for 12 months after the date the HIV-positive partner initiated ART.
ART, routine care and follow-up of the index partners
ART was provided to HIV-positive partners irrespective of CD4 cell count. As per national guidelines, a fixed-dose combination of tenofovir, lamivudine and efavirenz was prescribed as the preferred first-line regimen, unless contraindicated. Upon ART initiation, HIV-positive partners received the standard of care in line with national guidelines, including monthly clinic visits, opportunistic infection prophylaxis and treatment, TB screening, routine CD4 monitoring (every six months), adherence support, monitoring for adverse effects of ART, and possible ARV drug substitution or switch when necessary. At the time of this study, routine viral load monitoring had not been implemented in Vietnam. As part of this study, viral load was measured at three time points: before initiating ART (baseline), at three months after ART initiation (month 3) as an early indication of response to ART and at 12 months after ART initiation (month 12). Specimens for viral load measurement from Dien Bien province were tested at Bach Mai Hospital Laboratory in Hanoi and those from Can Tho province were tested at Pasteur Institute in Ho Chi Minh City. The study also used targeted spontaneous reporting11 of specific adverse effects; specifically, OPC staff members were asked to assess and report nephrotoxicity associated with tenofovir (abnormal creatinine test results) and central nervous system (CNS) side effects potentially associated with EFV. Estimated glomerular filtration rate (eGFR) was calculated based on reported serum creatinine, age and gender.12
HIV testing of originally seronegative partners during the follow-up
HIV testing was offered to the originally seronegative partners when the couples were invited for behavioural assessment and counselling at months 3, 6 and 12. Follow-up of couples was terminated if the originally negative partner seroconverted, in which case the seroconverted individual was offered HIV treatment and care, following the national guidelines.
Statistical analysis
Data were managed using EpiInfo version 7.0 (Centers for Disease Control and Prevention, Georgia, USA) and analysis was conducted using SPSS version 20.0 (IBM SPSS Statistic, New York, USA). The proportion of HIV-seropositive partners with viral suppression (VL < 1000 copies/ml) was analysed using three different subsets of participants: (1) among all participants who initiated ART, regardless of whether cases were retained in care or had VL measured (intention to treat analysis); (2) among only the subset of participants who had VL measured at each given time point (e.g. viral suppression at 12 months after ART initiation was measured among all participants with an available viral load measurement 12 months after ART initiation); (3) among only the subset of participants who had VL measurements available from all three time points, i.e. baseline, month 3 and month 12. Cox proportional hazards analysis was conducted to analyse retention on treatment, and Chi square analysis was used to compare viral suppression between those with CD4 cell count ≤ 350 cells/mm3 and those with CD4 cell count > 350 cells/mm3 at baseline. Logistic regression analysis was conducted to identify potential correlates for non-retention and non-viral suppression.
Ethics
Study procedures were approved by institutional review boards or ethics review committees of the Hanoi University of Public Health (Hanoi, Vietnam), the World Health Organization Regional Office for the Western Pacific (Manila, Philippines) and the U.S. Centers for Disease Control and Prevention (Atlanta, Georgia, USA). Written informed consent for study enrolment was obtained from both HIV-seropositive and -seronegative partners.
Results
Couples HTC, linkage to care and study enrolment
Among 256 couples who underwent couples HTC and received their results at the designated HTC sites, 146 (57%) couples were serodiscordant, 22 (9%) were concordant positive and 88 (34%) were concordant negative. Of the 146 serodiscordant couples, 133 (91%) couples were linked to study OPCs where seropositive partners were enrolled in HIV care. One additional serodiscordant couple was identified among those already receiving care (without ART) at an OPC. All 134 couples met eligibility criteria and consented to study participation (Figure 1).
Figure 1.
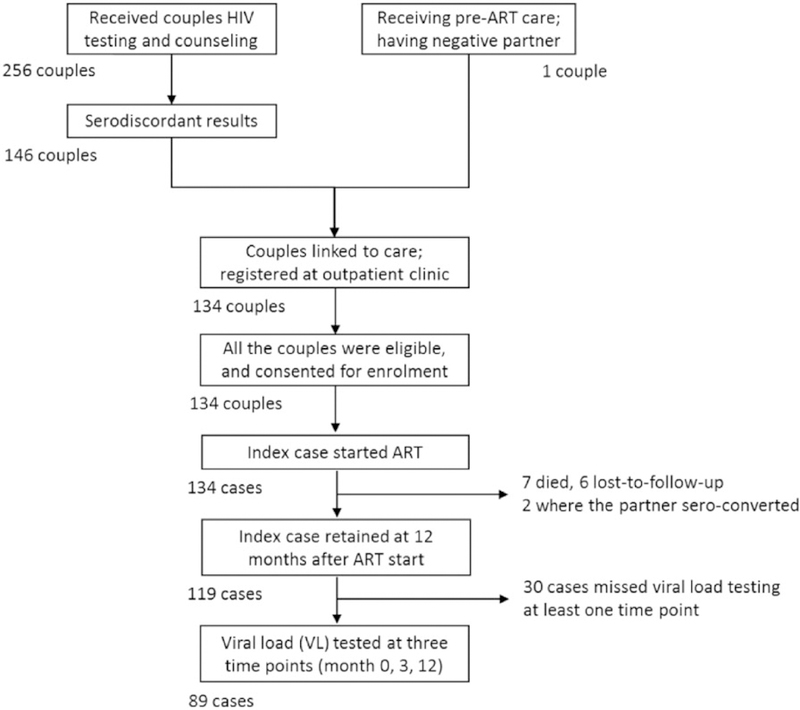
Flowchart summarizing the results of couples HTC, linkage to care and study enrolment. ART: antiretroviral therapy.
Sociodemographic of the couples and baseline clinical characteristics of HIV-positive partners
All 134 couples were heterosexual, and 116 (87%) were married (Table 1). Among the 134 HIV-positive partners, 115 (86%) were males, median age was 32 years, 76 (57%) were farmers, 79 (59%) had education at secondary school or higher, and median monthly income was 1.0 million Vietnamese Dong (approximately 48 US dollars). Seventy-six (57%) HIV-positive partners reported ever using drugs, among whom nine (12%) were receiving methadone maintenance therapy. Of the 134 negative partners, 19 (14%) were males, median age was 31 years, 85 (63%) were farmers, 61 (46%) had education at secondary school or higher, median monthly income was also 1.0 million Vietnamese Dong. Table 1 and 2 also show the characteristics of the 89 (66%) couples in which HIV-positive partners had VL measured at all three time points, which showed similar patterns as all the couples.
Table 1.
Characteristics of study participants at enrolment: Socio-demographic characteristics of HIV-positive partners and their seronegative partners.
| All enrolled couples with HIV-positive partner starting ART (N = 134) |
Couples with HIV-positive partners having VL measured at all three time points (N = 89) |
|||
|---|---|---|---|---|
| HIV-positive partners | Negative partners | HIV-positive partners | Negative partners | |
| Individuals | ||||
| Male, number (%) | 115 (85.8) | 19 (14.2) | 75 (84.3) | 14 (15.7) |
| Age, in years | ||||
| Median (IQR) | 32 (27–36) | 31 (27–37) | 33 (27–38) | 32 (28–38) |
| Categorized, number (%) 18–24 | 14 (10.4) | 20 (14.9) | 6 (6.7) | 11 (12.4) |
| 25–34 | 76 (56.7) | 69 (51.5) | 52 (58.4) | 47 (52.8) |
| 35–44 | 34 (25.4) | 39 (29.1) | 22 (24.7) | 26 (29.2) |
| ≥ 45 | 10 (7.5) | 6 (4.5) | 9 (10.1) | 5 (5.6) |
| Education, number (%) | ||||
| Illiterate | 20 (14.9) | 36 (26.9) | 16 (18.0) | 26 (29.2) |
| Primary school (1–5) | 35 (26.1) | 37 (27.6) | 22 (24.7) | 26 (29.2) |
| Secondary school (6–9) | 51 (38.1) | 34 (25.4) | 33 (37.1) | 20 (22.5) |
| High school (10–12) | 25 (18.7) | 21 (15.7) | 16 (18.0) | 12 (13.5) |
| College/University | 3 (2.2) | 6 (4.5) | 2 (2.2) | 5 (5.6) |
| Occupation, number (%) | ||||
| Farmer | 76 (56.7) | 85 (63.4) | 53 (59.6) | 57 (64.0) |
| Government official | 2 (1.5) | 7 (5.2) | 0 (0.0) | 6 (6.7) |
| Business | 10 (7.5) | 16 (11.9) | 5 (5.6) | 9 (10.1) |
| Unemployed | 8 (6.0) | 3 (2.2) | 2 (2.2) | 1 (1.1) |
| Others | 38 (28.4) | 23 (17.2) | 29 (32.6) | 16 (18.0) |
| Monthly income, in million Vietnam Dong | ||||
| Mean | 1.9 | 1.8 | 1.9 | 1.8 |
| Median | 1.0 | 1.0 | 1.2 | 1.1 |
| Self-reported risk behaviour and substance use, number (%) | ||||
| Ever using drugs | 76 (56.7) | 2 (1.5) | 50 (56.2) | 1 (1.1) |
| Heavy alcohol use in the past month | 90 (67.2) | 33 (24.6) | 61 (68.5) | 22 (24.7) |
| Unprotected sex within the couple in the past three months | 29 (26.4) | 29 (26.9) | 17 (23.3) | 17 (23.0) |
| Sex with external partner in the past three months | 2 (1.5) | 5 (4.0) | 2 (2.2) | 3 (3.3) |
| Service use, number (%) | ||||
| Methadone maintenance therapy | 9 (6.7) | 0 (0.0) | 7 (7.9) | 0 (0.0) |
| Needle syringe programme | 7 (5.2) | 0 (0.0) | 4 (4.5) | 0 (0.0) |
| Couples | ||||
| Median distance to the clinic, in km (IQR) | 7 (3–15) | 7 (2–14) | ||
| Marital status (% married) | 116 (86.6) | 78 (87.6) | ||
ART: antiretroviral therapy; IQR: interquartile range; VL: viral load.
Table 2.
Characteristics of study participants at enrolment: Clinical characteristics of the HIV-positive partners at baseline (before ART start).
| All enrolled couples with HIV-positive partner starting ART (N = 134) | Couples with HIV-positive partners having VL measured at all three time points (N=89) | |
|---|---|---|
| CD4 cell count tested, number (%) | 133 (99.3%) | 89 (100%) |
| Median CD4 cell count (cells/mm3) (IQR) | 374 (147–566.5) | 374 (155–570) |
| CD4 cell count (cells/mm3) | ||
| ≤100 | 28 (21.1%) | 18 (20.2%) |
| 101–350 | 35 (26.3%) | 23 (25.8%) |
| 351–500 | 24 (18.0%) | 15 (16.9%) |
| >500 | 46 (34.6%) | 33 (37.1%) |
| Median VL | ||
| Number of index partners tested for VL | 123 (91.8%) | 89 (100%) |
| Median VL log10 (IQR) | 4.81 (3.96–5.47) | 4.75 (3.91–5.34) |
ART: antiretroviral therapy; IQR: interquartile range; VL: viral load.
Of 133 HIV-positive partners who had their CD4 cell count tested before ART start, median CD4 cell count was 374 (IQR 147–567) cells/mm3, 46 (35%) had CD4 cell count over 500 cells/mm3, 24 (18%) between 350 and 500 cells/mm3, 35 (26%) between 100 and 350 cells/mm3, and 28 (21%) below 100 cells/mm3 (Table 2). All 134 HIV-positive partners started ART. Of 134 HIV-positive partners, seven had no VL tested before ART start, and four had delayed VL testing (more than five days after ART start); among the remaining 123, median log10 VL was 4.81 (IQR 3.96–5.47) copies/ml (Table 2). Among the 64 HIV-positive partners who had CD4 cell count over 350 cells/mm3, a large proportion had high VL (92% having over 1000 copies/ml and 67% over 10,000 copies/ml).
Retention and viral suppression among HIV-positive partners
Among the 134 HIV-positive partners, 124 (93%) and 119 (89%) persons were retained at 3 and 12 months after ART initiation, respectively. By 12 months after ART initiation, seven had died, six were lost to follow-up, and follow-up had been terminated for two HIV-positive partners whose originally seronegative partners had seroconverted. Excluding the two cases with partners’ seroconversion and one case without baseline CD4 cell count, retention on ART at 12 months was 94% among those who started ART with CD4 cell count at or greater than 350 cells/mm3 compared with 85.5% among those starting ART with CD4 cell count less than 350 cells/mm3 although the difference was not statistically significant (p 0.061) (Figure 2).
Figure 2.
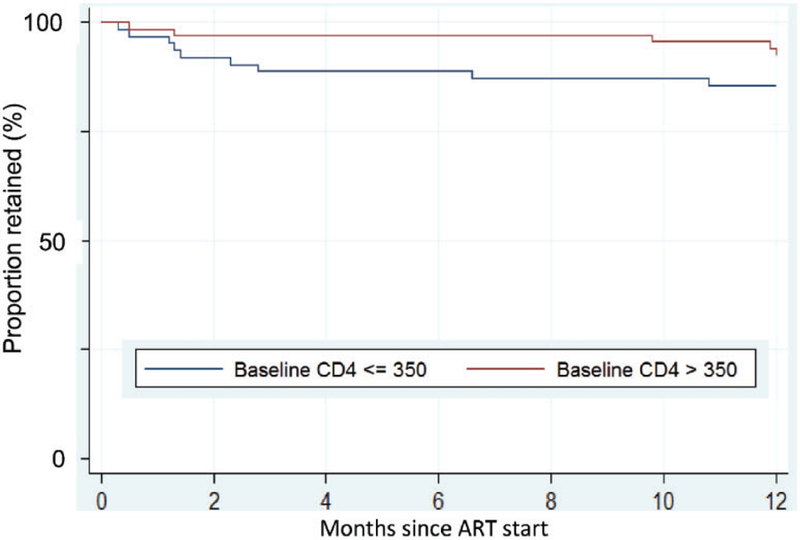
Kaplan–Meier curve showing the retention of the HIV-positive partners (N = 134) disaggregated by the baseline CD4 cell count. N = 70 had CD4 cell count over 350 cells/mm3 and N = 63 had CD4 cell count equal to or less than 350 cells/mm3. ART: antiretroviral therapy.
As per intention to treat analysis, among HIV-positive partners starting ART with CD4 cell count > 350 cells/mm3, 81% were virally suppressed at 12 months compared with 75% of those with CD4 cell count ≤ 350 cells/mm3 at baseline (p > 0.05) (Figure 3(a)). Among the subset of participants who had VL measured at that time point, those with baseline CD4 cell count > 350 cells/mm3 and CD4 cell count ≤ 350 cells/mm3 had equivalent level of viral suppression (95% versus 94%, respectively, at month 12) (Figure 3(b)). Even when only the subset of participants who had VL measured at all three time points (months 0, 3 and 12) are included in the analysis, the result was similar, showing high and similar levels of viral suppression in those with baseline CD4 cell count > 350 cells/mm3 and with CD4 cell count ≤350 cells/mm3 (90% in both groups). Gender, age, education, occupation, income, drug use and alcohol use were not associated with viral suppression at 12 months after ART initiation, regardless of which denominators were used.
Figure 3.
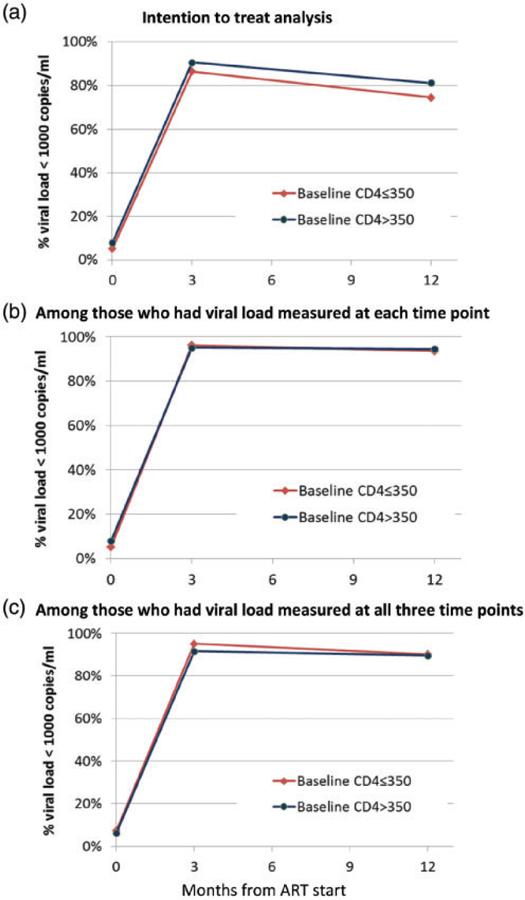
Proportion of the HIV-positive partners who had viral load less than 1000 copies/ml before and 3 and 12 months after ART start. (a) Intention to treat analysis, (b) among those who had viral load measured at each time point and (c) among those who had viral load measured at all three time points. Denominators are: a, N = 59 (CD4 cell count ≤350 cells/mm3) and 64 (CD4 cell count >350 cells/mm3); b, N = 59 (CD4 cell count ≤350 cells/mm3) and 64 (CD4 cell count >350 cells/mm3) at month 0, N = 53 (CD4 cell count ≤350 cells/mm3) and 61 (CD4 cell count >350 cells/mm3) at month 3 and N = 47 (CD4 cell count ≤350 cells/mm3) and 55 (CD4 cell count >350 cells/mm3) at month 12; c, N = 41 (CD4 cell count ≤350 cells/mm3) and 48 (CD4 cell count >350 cells/mm3). ART: antiretroviral therapy
Self-reported risk behaviours of the HIV-positive partners
HIV-positive partners’ report of consistent condom use with their partners showed increasing trend during follow-up (71% at baseline, 93% at month 3, 95% at month 6 and 99% at month 12 among the respondents). Their partners also reported a similar trend: 69% at baseline, 94% at month 3, 94% at month 6 and 100% at month 12.
Adverse events during treatment in the HIV-positive partners
Of the 134 HIV-positive partners, 21 (15%), 5 (4%) and 1 (1%) experienced Grade 1 (minor), Grade 2 (moderate) and Grade 3 (major) CNS adverse effects potentially associated with EFV. Of 91 individuals with measured eGFR, 17 (19%) had eGFR reduction in a range of 25–50% and 3 (4%) had eGFR reduction in a range of 50–75% compared to the baseline, during 12 months of follow-up. The three patients with renal injury were closely monitored without substitution of TDF. There were no significant differences in the pattern of adverse events between those with baseline CD4 cell count greater or less than 350 cells/mm3.
Seroconversion among originally seronegative partners
Among the 134 originally seronegative partners, 121 (90%), 113 (84%) and 109 (81%) persons visited clinics for couples counselling and behavioural assessment at month 3, 6 and 12, respectively. Nearly all (120, 113 and 108 persons at month 3, 6 and 12) received HIV testing. Among those tested, two persons had HIV-positive results at month 3. Their seropositive partners had CD4 cell counts of 136 and 843 cells/mm3 and VLs of 179,000 and 51,700 copies/ml at baseline, respectively. No additional seroconversions were detected at months 6 or 12.
Discussion
Following the release of interim results of the HPTN 052 trial in 2011,8 our study was designed to assess the feasibility of applying immediate ART (providing ART regardless of CD4 cell count) to HIV-infected persons in serodiscordant partnerships in Vietnam. At that time, there were concerns among stakeholders that providing early ART to asymptomatic persons might lead to suboptimal ART adherence, lower retention in care, increases in risk behaviour or higher occurrence of adverse effects of ART in the programme setting in Vietnam. The concerns were partly due to the fact that injection drug use was the dominant mode of HIV transmission in Vietnam, whereas the HPTN052 trial enrolled very few PWID.8
Our study nevertheless demonstrated that HIV-positive partners in our cohort were willing to start ART irrespective of CD4 cell count. Neither retention in care nor achievement of viral suppression differed significantly among those starting ART with CD4 cell count >350 cells/mm3 (the recommended CD4 threshold by the Vietnam national guidelines at that time) compared with those starting with CD4 cell count less than 350 cells/mm3. Moreover, neither an increase in self-reported risk behaviours nor an increase in adverse events was observed in the cohort.
Our study also provided local data showing that many HIV-positive partners with CD4 cell counts over 350 cells/mm3 had high VLs (67% having over 10,000 copies/ml) and that consistent condom use among the couples was not high (71% at baseline). These data suggest that without additional intervention, continued sexual transmission will likely occur from people living with HIV (PLHIV) to their uninfected partners. Those data contributed to the decision of MOH to recommend provision of ART irrespective of CD4 cell count for the HIV-positive partners in serodiscordant relationships.
Two initially seronegative partners tested HIV-seropositive three months after the HIV-positive partners started ART. Approximately 90% of HIV-positive partners were virally suppressed at months 3 and 12, and no seroconversions were detected at months 6 or 12. Thus, these two cases of seroconversion are probably because either the originally seronegative partner was HIV tested during the window period or the transmission occurred during the early phase of ART before their HIV-infected partner achieved viral suppression.
In the HPTN052 trial, among the eight linked partner infections diagnosed, HIV infection was diagnosed among four initially uninfected partners less than 90 days after their seropositive partners initiated ART; the investigators suggested that these transmissions occurred before the virus was suppressed in the HIV-positive participants.7 In the other four cases, transmission occurred after ART treatment failure among the HIV-seropositive participants.7 These data highlight the importance of concomitant use of other prevention measures, especially if the HIV-infected partner is not known to be virally suppressed.
Our study suggested that couples HTC has the potential to facilitate mutual disclosure and earlier HIV diagnosis and to improve identification of serodiscordant couples. Behavioural counselling for serodiscordant couples is known to reduce risk behaviours (sexual and drug injection) and to improve adherence to ART among the seropositive partners.13 However, health staff faced challenges recruiting couples to test together. Raising awareness of the availability of couples HTC and the benefits of early diagnosis through community peer outreach, HIV OPCs and methadone maintenance services may improve recruitment for couples HTC. Further study in Vietnam may help to elucidate barriers to and opportunities for couples HTC and partner notification.14
Prior to the study, some programme stakeholders had been concerned about the possibility of risk compensation, that is of increases in sexual or injecting risk behaviours if key populations were provided with ART earlier in the course of HIV infection, when CD4 cell count were high. In our study, however, no decline in consistent condom use was observed during the follow-up. Other studies have also reported that ART initiation is not generally associated with increase in risky sexual behaviours. For example, a longitudinal analysis of HIV-infected persons found a decrease in condomless vaginal intercourse with primary partners but not with non-primary partners.15 We had hoped to also assess changes in injection behaviour among participants in our study, but likely under-reporting of current injecting behaviours due to stigma and fear of arrest precluded such analysis.
Our study had various limitations. First, our small sample size (N = 134) limited statistical power in particular for understanding potential risk factors for attrition or lack of viral suppression. Second, we believe that current injection drug use during the study was under-reported. A previous analysis reported that self-report of ever using drugs can be considered a proxy for current and ongoing heroin injection in Vietnam16; if true, an estimated 57% of HIV-infected partners were injecting drugs. Third, our study followed the couples only for the first 12 months. It is critical to have longitudinal follow-up to better understand durability of early ART. Fourth, some VL values were missing because no national system had been established for timely management of specimen shipment for VL testing and returning of test results.
Conclusion
Our study demonstrated that couples HTC and immediate ART among serodiscordant couples can be feasible in Vietnam. Our results showed that patients initiating ART with CD4 cell count >350 cells/mm3 were retained well on ART (>90%) and achieved high levels of viral suppression, without decline in self-reported consistent condom use. The study also generated local data showing that PLHIV have high VLs even with CD4 cell counts over 350 cells/mm3, suggesting that HIV-uninfected partners are exposed to ongoing transmission risk. Data from this study contributed to the decision of the MOH to recommend provision of ART irrespective of CD4 cell count for HIV-positive partners in serodiscordant relationships; since that time, immediate ART, regardless of CD4 cell count has been further expanded in Vietnam. At the same time, continued efforts are needed to promote earlier diagnosis through innovations in HIV testing and partner notification, and combination prevention integrating ART towards the Government’s vision to achieve ending AIDS by 2030.
Acknowledgements
Authors would like to thank all the participants in this demonstration project for their participation, and health staff at OPCs in Dien Bien and Can Tho provinces for their dedication for this project. We are also grateful to other members of the study team for collaboration and Ms Tham Le for her assistance in extensive literature search.
Funding
This work was supported by MAC AIDS Foundation, President’s Emergency Fund for AIDS Relief, and Global Fund to fight AIDS, tuberculosis and malaria.
Footnotes
Publisher's Disclaimer: Disclaimer
The views expressed in this paper are those of the authors and do not necessarily represent the official position of the authors’ institutions, Ministry of Health Vietnam, Centers for Disease Control and Prevention and World Health Organization.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.MOH. Optimizing Viet Nam’s HIV response: an investment case Hanoi: Viet Nam Ministry of Health, http://www.aidsdatahub.org/sites/default/files/publication/Vietnam_investment_case_2014.pdf (2014, accessed 10 March 2018). [Google Scholar]
- 2.AIDSInfo. UNAIDS, http://aidsinfo.unaids.org/ (2017, accessed 13 October 2017).
- 3.WPRO. Joint review of the health sector response to HIV in Viet Nam 2014 Manila: World Health Organization, Regional Office for the Western Pacific, http://iris.wpro.who.int/handle/10665.1/12787 (2016, accessed 10 March 2018). [Google Scholar]
- 4.PHR. Baseline surveys in female sexual partners of male IDUs in Dien Bien and Ho Chi Minh City Hanoi: Partners in Health Research, 2012. [Google Scholar]
- 5.Travis L, Tran TD and Tran HM. Triangulation exercise on intimate partner transmission of HIV in Viet Nam Hanoi: UNAIDS and UN Women, 2012. [Google Scholar]
- 6.NIHE. HIV/STI integrated biological and behavioral surveillance (IBBS) in Vietnam: results from round III 2013 and trends across three rounds (2005–2009–2013) of surveys Hanoi: Ministry of Health – Viet Nam, 2014. [Google Scholar]
- 7.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med 2016; 375: 830–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365: 493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.VAAC. Viet Nam HIV/AIDS estimates and projections 2011–2015 Hanoi: Viet Nam Authority of HIV/AIDS Control, Ministry of Health, 2012. [Google Scholar]
- 10.VAAC. HIV/STI Integrated biological and behavioral surveillance (IBBS) in Viet Nam 2009, Viet Nam Authority of HIV/AIDS Control, Hanoi, Vietnam, 2012. [Google Scholar]
- 11.WHO. Surveillance of antiretroviral drug toxicity within antiretroviral treatment programmes: technical brief, http://www.who.int/hiv/pub/arv_toxicity/technical-brief-surveillance/en/ (2013, accessed 10 March 2018).
- 12.WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach – first edition Geneva: World Health Organization, 2013. [PubMed] [Google Scholar]
- 13.Jiwatram-Negron T and El-Bassel N. Systematic review of couple-based HIV intervention and prevention studies: advantages, gaps, and future directions. AIDS Behav 2014; 18: 1864–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Guidelines on HIV self-testing and partner notification. Supplement to consolidated guidelines on HIV testing services Geneva: World Health Organization, 2016. [PubMed] [Google Scholar]
- 15.Mujugira A, Celum C, Ngure K, et al. Antiretroviral therapy initiation is not associated with risky sexual behavior among heterosexual human immunodeficiency virus-infected persons in serodiscordant partnerships. Sex Transm Dis 2017; 44: 57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linh-Vi L, Hoang TV and Sabin K (eds). Comparing drug-use responses with urinalysis in HIV behavioral surveys among female sex workers (FSW) and men who have sex with men (MSM). In: Australasian HIV/AIDS conference, Melbourne, Australia, 2012. [Google Scholar]


