Abstract
Background
Untreated mental health disorders among people living with HIV (PLHIV) may prevent low- and middle-income countries (LMICs) from achieving the UNAIDS 90–90-90 targets. Anxiety disorders may be associated with decreased adherence to antiretroviral therapy (ART). We sought to review and meta-analyze studies estimating associations between anxiety and ART adherence in LMICs.
Methods
We performed a systematic review and meta-analysis of studies assessing reported anxiety and ART adherence among PLHIV receiving ART in LMICs. We searched PubMed, PsychINFO, CINAHL and EMBASE for relevant studies published before July 18, 2018. We defined anxiety as reported anxiety scores from screening questionnaires or having a clinical diagnosis of an anxiety disorder, and poor ART adherence as missed doses, poor visit attendance, or scores from structured adherence questionnaires. We used a random effects model to conduct a meta-analysis for calculating a pooled odds ratio, and conducted sensitivity analyses by time on ART, anxiety evaluation method, and study region.
Results
From 472 screened manuscripts, thirteen studies met our inclusion criteria. Eleven studies were included in the meta-analysis. PLHIV who reported anxiety had 59% higher odds of poor ART adherence compared with those who did not report anxiety disorder (pooled odds ratio [pOR]: 1.59, 95% confidence interval [CI]: 1.29–1.96, p<.001). When excluding PLHIV who initiated ART within 6 months, reported anxiety remained strongly associated with poor ART adherence (pOR: 1.61, 95% CI: 1.18–2.20, p=.003).
Conclusions
Among PLHIV in LMICs, reported anxiety was associated with poor ART adherence. This association persisted after the ART initiation period. Increased resources for mental health may be important for achieving virologic suppression in LMICs.
Keywords: HIV, antiretroviral therapy, anxiety, adherence, low-income countries
Introduction
While many high-income countries have achieved significant progress towards the UNAIDS 90–90-90 goals[1,2], four years after their inception, many low- and middle-income countries (LMICs) are not on target to reach these goals[2]. Closing this gap will require interventions tailored to vulnerable populations, including people living with co-morbid HIV and mental health disorders [2]. Most LMIC’s health systems do not provide adequate mental health services; an estimated 74% of people living with mental illness in LMICs still receive no treatment [3]. In 2014, the World Health Organization (WHO) set a goal for 80% of countries to have at least two national programs to better address mental health by 2020. Currently, however, only 32% of countries meet this criteria [4].
The majority of existing literature on mental health and HIV in LMICs focuses on depression. Depression is associated with poor ART adherence[5], risky sexual behavior[6], lower CD4 counts[7], and treatment failure[8,9]. While not as well studied, anxiety disorders may also interrupt the cascade of HIV care by making individuals less likely to present for HIV testing, remain engaged in HIV care, and adhere to antiretroviral therapy (ART) [10–15]. Anxiety has also been associated with risky sexual behavior, increasing the risk for further transmission [10,16,17]. Although estimates suggest there is a substantial burden of anxiety among people living with HIV (PLHIV) in LMICs, research and interventions targeting anxiety in these settings have been limited [4,18]. Thus, little is known about the effects of untreated anxiety on HIV viral load suppression and mortality.
Previous reviews have focused on the epidemiology of all mental health conditions and their prevalence among PLHIV, but have not assessed associations between mental health and HIV-related clinical outcomes [19]. Moreover, previous reviews on anxiety and HIV predate the change to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) removing post-traumatic stress disorder (PTSD) from the “anxiety disorder” category [18–21]. We sought to describe associations between anxiety and poor ART adherence among PLHIV in LMICs, with the aim of addressing these gaps in the literature and motivating further research.
Methods
Search Strategy
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22], we searched PubMed, CINAHL, PsycINFO, and Embase for articles published from database inception until July 16th, 2018. Our search included keywords relating to HIV, antiretroviral therapy, adherence, mental health, anxiety disorders, screening for anxiety disorders, and a list of low and middle-income countries (Appendix 1). We also manually searched the reference lists of all studies included in the final sample for eligible studies not captured by our database search.
Study Selection and Extraction
Results from each database search were uploaded to Covidence.org [23]. Duplicate articles were removed, and two authors (JW and CK) independently reviewed titles and abstracts and discussed any disagreement prior to making a final decision. The same two authors then performed full-text review on the included articles, alternating primary and secondary extraction with a standardized form. When data clarifications were needed, we contacted corresponding authors to request or clarify additional data.
Eligibility Criteria
Study Design and Population
We included cross-sectional studies, case-control studies, retrospective and prospective cohort studies, and randomized controlled trials. We excluded qualitative studies, systematic reviews, and non-peer reviewed abstracts. When multiple time points were reported from randomized controlled trials and cohort studies, we used the initial enrollment data to better correspond with the data reported in the other cross-sectional studies. Using World Bank Classifications [24], we included any paper reporting data from a low-income, lower middle-income, or upper middle-income country. We did not exclude articles based on the duration of ART use. We excluded studies recruiting participants under age 15, or participants not on ART, unless eligible subgroup analyses were available.
Exposure
Our primary exposure of interest was reported anxiety. We included papers that included either the diagnosis of an anxiety disorder or self-reported anxiety symptoms as an exposure variable. We defined anxiety by positive responses on a structured screening questionnaire, or a clinical diagnosis made during a diagnostic interview. When anxiety scores were reported in multiple groups (e.g., “mild,” “moderate,” and “severe” anxiety) we categorized the data into “no anxiety” and “some anxiety” for the analysis. We excluded papers that focused exclusively on PTSD. In addition, we extracted data on the prevalence of anxiety and methods used to measure anxiety.
Outcomes
Our primary outcome of interest was poor ART adherence. When multiple measures were used to evaluate adherence in the same population, we used whichever measure was more consistent with a “gold standard” method (previously used in a similar population and validated in prior research). However, when it was not possible to ascertain a “gold standard” measure, or the results were equivocal, we utilized the measure that evaluated adherence over a longer course of time. We attempted to include HIV-1 RNA levels (viral load) and CD4 count as secondary outcomes. However, as none of the included studies reported data related to these outcomes, we were unable to complete this analysis.
Data Analysis
We conducted a random effects meta-analysis to assess the pooled association between any reported anxiety and poor ART adherence. Our model included odds ratios as the common measure of association across eleven studies; we excluded data from studies reporting hazard ratio, risk differences, or correlation coefficient estimates which were not comparable to odds ratios. Of the included studies, six reported adjusted odds ratios that accounted for the influence of potential confounding variables in their study populations, and five reported unadjusted odds ratios or proportions only.
We used a random effects model to adjust for within-study and between-study variance, given the different study locations and data collection measures [25]. We assessed between-study heterogeneity using the Cochrane Q statistic, I2 proportion, and tau2 statistic. We conducted analyses examining the influence of publication bias on our pooled odds ratio. All analyses were conducted using the metan package in Stata version 14 (StataCorp, College Station, TX).
We conducted four sensitivity analyses. The first focused only on studies where all participants had been on ART for at least six months to determine whether an association between reported anxiety and ART adherence might persist after an ART initiation phase. The second analysis included studies that used the Hospital Anxiety and Depression Scale to evaluate for reported anxiety, as this was the most commonly used measure to assess anxiety among the included studies. The final two sensitivity analyses were regional, with the first including studies located in Asia, and the second including studies located in Africa.
Results
Our search returned 664 titles for review. After removing 192 duplicate studies, 472 titles were included for abstract review (Figure 1). 302 abstracts were excluded at the title/abstract level, leaving 170 articles for full-text review. Full-text review initially yielded 16 articles for inclusion. Three studies appeared to collect data that would have been compatible with our analysis, however, they did not report poor adherence outcomes in the manuscript. The authors were contacted and asked to provide this data, but none of these authors responded to multiple queries [26–28]. Consequently, these three articles were excluded, leaving 13 articles for inclusion. Two titles met criteria for inclusion in the review but did not report data that could not be summarized for the planned meta-analysis [29,30]. Of these two studies, one reported the association between anxiety and poor adherence as a hazard ratio [29], and the other reported it as a Pearson’s correlation coefficient [30].
Figure 1.
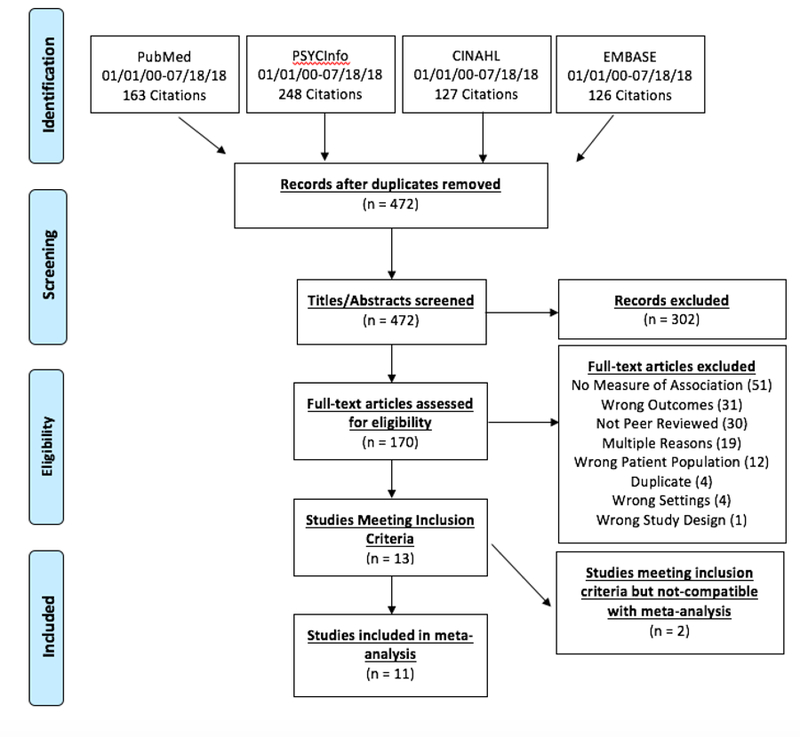
PRISMA flow diagram of study identification, screening, and inclusion
Characteristics of Included Sample
In total, the 13 studies included in the review (Table I) ranged in sample size from 101–2924 participants [29–39]. One study included only male participants [39]. Among the other twelve studies, proportion of female to male participants varied from 11% [40] to 82% female [33]. Not all included studies reported participants’ ages, however, among those that did the mean age ranged from 34.2 [27] to 42.1 years [26]. These papers were from eight unique countries, distributed across Africa, Asia, and South America. In ten studies, all participants had been taking ART for greater than six months, while two studies focused only on newly initiating patients, and one study did not distinguish between newly initiating and previously established patients. One paper focused exclusively on men who have sex with men (MSM) [39], while the remaining papers did not specify if any portion of the study population identified as MSM. None reported data relating to CD4 count and HIV viral load.
Table I.
Characteristics of Included Studies (n=13)
| Study | Location | Cohort Description | Anxiety Evaluation Method | Study Type | Anxiety Prevalence | Adherence Evaluation Method | Poor Adherence Prevalence |
|---|---|---|---|---|---|---|---|
| Nguyen et al. 2016[32] | Vietnam | 1050 HIV + adults, on ART >6 months | EQ-5D-5L | Cross-Sectional | 43.8% | 30 Day VAS Scale | 30.9% |
| Joshi et al. 2014[34] | India | 2924 HIV+ adults, mix of newly initiating ART and on ART for >6 months | Hospital Anxiety and Depression Scale (HADS) | Cross-Sectional | 69.8% | AACTG Questionnaire | 24.0% |
| Guimares et al. 2008[35] | Brazil | 350 HIV+ adults initiating ART | Hospital Anxiety and Depression Scale (HADS) | Prospective Cohort | 36.0% | Patient Interview | 51.4% |
| Nel et al 2013[33] | South Africa | 101 HIV + adults, on ART >6 months | Beck’s Anxiety Inventory | Cross-Sectional | 28.7% | Six Item Self-Reporting Questionnaire | 45.5% |
| Adejumo et al. 2016[36] | Nigeria | 453 HIV + adults, on ART >6 months | Composite International Diagnostic Instrument (CIDI) | Cross-Sectional | 2.5% | 1 week and 1 month self-reported missed doses | 9.7% |
| Yunusa et al. 2014[37] | Nigeria | 159 HIV + adults, on ART >6 months | Hospital Anxiety and Depression Scale | Cross-Sectional | 17.1% | Self-reported pattern of adherence | 5.7% |
| Pefura-Yone et al. 2013[38] | Cameroon | 889 HIV + adults, on ART >6 months | GAD-7, Self-Administered | Cross-Sectional | 11.1% | Antiretroviral Medication Self-Report 7-day recall | 22.5% |
| Tao et al. 2017[39] | China | 228 HIV+ MSM on ART >6 months | Hospital Anxiety and Depression Scale | Prospective Cohort | 49.0% | Self-reported missed doses over last 3 months | 8.0% |
| Prasithsirikul et al. 2017[31] | Thailand | 2023 HIV + adults, on ART >6 months | Hospital Anxiety and Depression Scale | Cross-Sectional | 4.5% | >90% Self-Reported Dose Adherence | 14.0% |
| Yu et al 2018[40] | China | 207 newly diagnosed HIV+ adults initiating ART | GAD-7 | Cross-Sectional | 29.5% | CPCRA Antiretroviral Medications Self-Report Questionnaire | 14.5% |
| Pokhrel et al 2018[41] | Nepal | 655 HIV+ adults, on ART >1 year | Comprehensive International Diagnostic Interview-Short Form (CIDI-SF) | Randomized Controlled Trial | 11.6% | AACTG Questionnaire | 19.0% |
| Campos et al. 2008[29]* | Brazil | 293 H HIV + adults, on ART >6 months | Hospital Anxiety and Depression Scale | Prospective Cohort | 12.6% | >95% Self-Reported 3 day dose adherence | 37.2% |
| Qiao et al. 2015[30]* | China | 1254 HIV + adults, on ART >6 months | Zung Self-Rating Anxiety Scale | Cross-Sectional | Not reported | AACTG Questionnaire | Not Reported |
Not included in the final meta-analysis
Measurement of Anxiety and Adherence
Six different tools were used to assess anxiety (Table II). Six studies used the Hospital Anxiety and Depression Scale (HADS) [29,31,34,35,37,39], two studies used the Generalized Anxiety Disorder 7-item scale (GAD-7) [38,40] and two studies used the Comprehensive International Diagnostic Instrument [36,41]. The remaining three studies used unique methods: Beck’s Anxiety Inventory[33], the EQ-5D-5L[42], and the Zung Self-Rating Anxiety Scale[30]. Eleven of thirteen studies used questionnaires developed as screening tools for anxiety, while two [36,41] used a structured interview and questionnaire. The total prevalence of reported anxiety ranged from 2.5–69.8%. Three studies used the same tool to assess adherence, [30,34,41], the AACTG questionnaire. The other ten studies each used a unique method. Of these, two [33,40] used standardized, validated questionnaire tools, while the other used non-standardized self-report measures.
Table II.
Tools for Assessing Anxiety
| Measure of Anxiety | Number of Studies Using this Method | Number of Studies Using this Method Included in Analysis | Description | Validated in Study Population? |
|---|---|---|---|---|
| Beck’s Anxiety Inventory | 1 | 1 | 21 item survey of anxiety signs/symptoms scored using a 3 point Likert scale[44] | Yes, in same country[58] |
| Composite International Diagnostic Instrument | 2† | 2 | Structured comprehensive interview with standard questions assessing for mood, anxiety, and substance use disorders including 59 questions relating to anxiety signs/symptoms[59] | Yes, in same country[60–62] |
| EQ-5D-5L | 1 | 1 | 5 questions regarding daily functioning and depression/anxiety; participants’ anxiety is measured specifically by asking to answer the single question “I am ___anxious or depressed (not, slightly, moderately, severely, extremely)[48] | Yes, in same country[63] |
| GAD-7 | 2 | 2 | 7 item survey of anxiety signs/symptoms scored using a 4 point Likert scale[45] | Yes‡ |
| Hospital Anxiety and Depression Scale | 6 | 5 | 7 item survey of anxiety signs/symptoms scored using a 7 point Likert scale[46] | Yes[64–70] in all countries |
| Zung Self-Rating Anxiety Scale | 1 | 0 | 20 item survey of anxiety signs/symptoms using a 4 point Likert scale[47] | Yes[14], in the same country |
Outcomes
Among the eleven studies included in the final meta-analysis, reported anxiety was positively and strongly associated with poor ART adherence (pooled odds ratio [pOR]: 1.59, 95% confidence interval [CI]: 1.29–1.96, p<.001) (Figure 2). Separate subgroup analysis excluding patients newly initiating ART also showed that anxiety was positively associated with poor ART adherence in participants previously established on ART (pOR: 1.61, 95% CI: 1.18–2.20, p=.003) (Figure 3A). Reported anxiety was also positively associated with poor ART adherence in a pooled analysis of the five studies that used the Hospital Anxiety and Depression Scale to assess anxiety (pOR: 1.78, 95% CI: 1.18–2.68, p=0.006) (Figure 3B).
Figure 2.
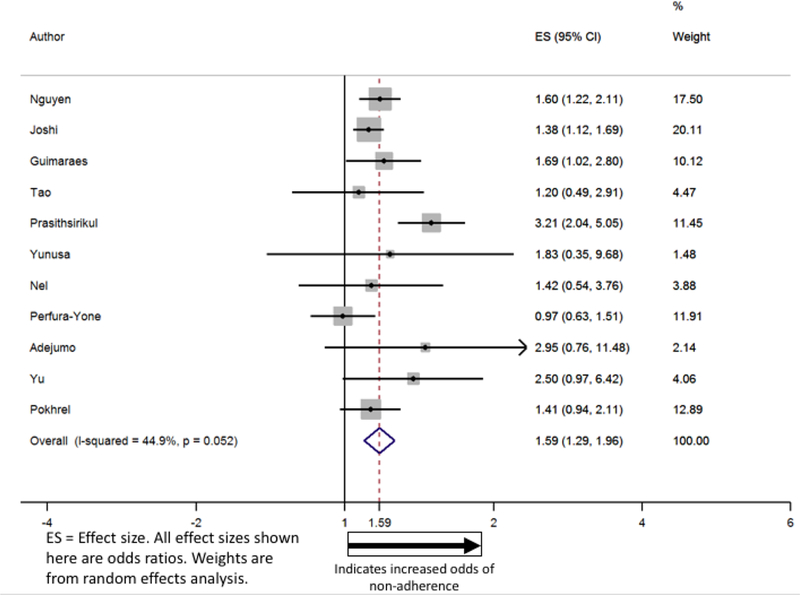
Forest plot of odds ratios between anxiety and poor adherence.
Figure 3A-D.
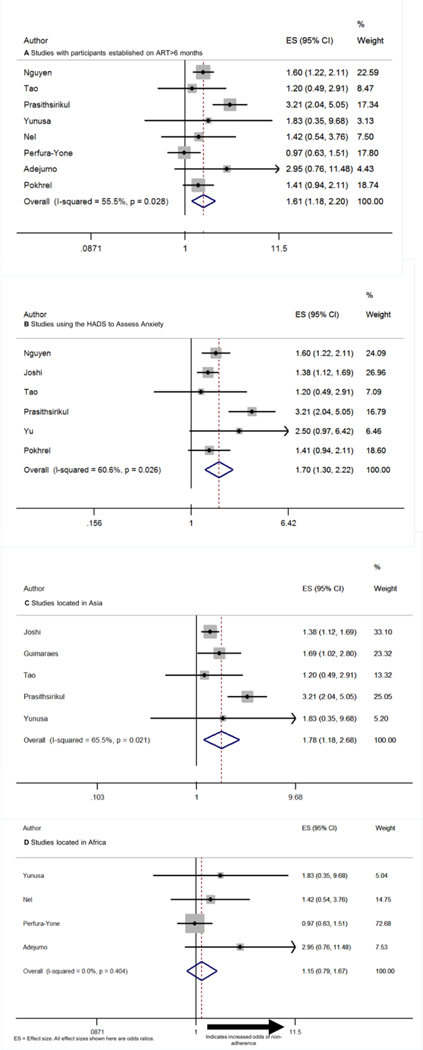
Forest plots of odds ratios between anxiety and poor adherence in four sensitivity analyses
In the six studies located in Asia, anxiety was positively associated with poor adherence (pOR: 1.70, 95% CI: 1.30–2.23, p<.001) (Figure 3C). This included studies located in China, Nepal, Vietnam, Thailand, and India[31,34,39–42]. Among the four studies located in Africa, anxiety was not statistically significantly associated with poor ART adherence, (pOR: 1.15, 95% CI; .79–1.67, p=.455) (Figure 3D). These four studies were located in Cameroon, Nigeria, and South Africa[33,36–38]. We did not pursue subgroup analysis for Latin American countries due to our search only returning one study, located in Brazil, that was compatible with our analysis [35].
Assessments of Heterogeneity and Publication Bias
For the eleven included studies, the Cochrane Q statistic was 18.15 (p=0.052) and the I2 proportion was 44.9%, representing moderate heterogeneity. The estimate of between-study variance (tau2) was 0.045. Egger’s test failed to demonstrate a statistically significant difference in effect size between smaller and larger studies (p=0.898). A funnel plot of the eleven studies was asymmetric, however, subsequent trim and fill analysis which included three new hypothetical studies only slightly moved the random effects estimate closer to the null value (pOR: 1.39, 95% CI: 1.00–1.78 ), and the pooled estimate remained statistically significant when these two hypothetical studies were included (p=0.01).
Discussion
In this meta-analysis of 11 studies, reported anxiety was strongly associated with poor ART adherence among PLHIV in LMICs. This strong association persisted among those PLHIV received ART for at least six months. There was a wide range in reported anxiety prevalence. Anxiety was also associated with poor adherence among the five studies that used the Hospital Anxiety and Depression Scale (HADS) to assess adherence. Regional subgroup analysis demonstrated that reported anxiety was positively associated with poor ART adherence in Asia but failed to demonstrate a statistically significant association in among studies in Africa.
While the reported prevalence of anxiety varied among included studies, the reported prevalence of anxiety in studies using the HADS alone ranged from 4.5–69.8%, suggesting that the variation in overall prevalence found in our study is unlikely to be explained solely by the use of different diagnostic anxiety scales. In the study that reported the highest anxiety prevalence [43], conducted in India, the authors used the median HADS score to derive a categorical cut-off for anxiety, rather than a predetermined value. In comparison, the study with the lowest reported anxiety among those using the HADS [31], conducted in Thailand, used a pre-determined cutoff of anxiety scores greater than or equal to eleven out of fifteen possible points to diagnose anxiety. Despite using the same screening tool, this difference in diagnostic criteria may account for the large difference in anxiety prevalence across the included studies. Notably, the two studies with the lowest reported anxiety prevalence also reported two of the strongest associations between anxiety and poor adherence, and two of the lowest rates of poor ART adherence. [31,36]. However, the reported prevalence of anxiety and poor adherence also falls below prior estimates for people living with HIV in low and middle-income countries, and so it is likely that these discrepancies are related to challenges in accurately measuring anxiety and adherence in low-resource settings.
Many of the anxiety scales used in the included studies were meant primarily for screening rather than diagnosis, which could also have contributed to the variation in reported prevalence [44–48]. Screening tools are often used for diagnosis due to the lack of availability of trained clinicians, however the data presented here demonstrate the potential lack of reliability when they are used. While the WHO advocates for and outlines a general framework for screening for anxiety and other mental health conditions, they do not recommend the use of one screening tool over another [49]. A universal screening tool that has been validated for use in resource-limited settings, such as the GAD-7 [50,51], would allow for uniformity across study data and make training and scaling up of mental health programs easier. Regardless of the screening tool used, each instrument should be validated in the local language and culture, and adapted as needed, before widespread implementation [52,53].
Given the limited mental health resources available in many LMICs, identifying patients that will most likely benefit from mental health-related interventions will be vital in moving towards the UNAIDS 90–90-90 treatment goals. The subgroup analysis of studies from Asia, coupled with the ongoing gap in viral suppression among people living with HIV in Asian countries [2] illustrates a clear need to scale up mental health resources in Asian countries. Though the analysis of studies located in Africa failed to demonstrate a statistically significant association, it was limited by a small sample size. For 90% of HIV-infected adults on treatment to be virally suppressed, health systems need to be able to identify those most at risk for poor adherence [54]. Though resources may be limited in many of the countries included in this review, effective, affordable mental health interventions have been validated in these settings; moving forward it is possible to increase access to these resources in a cost-effective manner [18].
This paper focuses on poor ART adherence as an outcome of anxiety disorders, however, virologic failure may be a better measure of HIV-related outcomes. While adherence can be used as a surrogate for viral suppression, it remains an imperfect marker, in part because many of the tools traditionally used to assess adherence are not completely sensitive or specific [55]. Accurately validating these tools is challenging, in part due to the lack of an inexpensive gold-standard against which to measure accuracy. As quantitative point-of-care viral load testing was recently approved by the WHO for use in resource-limited settings [56], viral load could be an effective surrogate for assessing adherence [57].
While a prior review assessed the association between symptoms of depression, alcohol use disorders, and ART adherence in sub-Saharan Africa [5], to our knowledge this is the first review specific to LMICs focused on anxiety and ART adherence. Our review is limited by the heterogeneity of the studies included, and a relatively small number of studies included in the meta-analysis. Additionally, because most of the included studies did not include outcomes stratified by age and gender, we were unable to perform further subgroup analysis. Two papers met inclusion criteria for our analysis but reported outcomes in a way that were not compatible with the meta-analysis [29,39]. Both studies also demonstrated a positive association between anxiety and poor adherence. While our analysis demonstrated an association between anxiety and poor adherence, this does not prove a causal relationship. Additionally, due to the overall paucity of data on this topic, our analysis is limited by the inclusion of multiple study types. The majority of studies were cross-sectional, however, we also included three retrospective cohort studies, and one randomized controlled trial. Previous studies suggested that the association between anxiety disorder and ART adherence may be non-linear, with more severe anxiety disorder associated with increased ART adherence relative to no anxiety disorder. We were unable to confirm or dispute this characterization given the limited data available from LMICs.
Our analysis adds to the existing body of research regarding mental health and HIV in LMICs. Depression, alcohol use, and now anxiety have all been demonstrated to be associated with poor ART adherence. We recommend that future research on this topic focus on the role of an integrated, transdiagnostic mental health approach to screening and treatment of these related, but distinct conditions. Furthermore, we recommend further research to better characterize the association between anxiety severity and poor adherence, as this may help to better identify high-risk patients.
In conclusion, reported anxiety appears to be strongly associated with poor ART adherence among PLHIV in LMICs. The use of standardized, validated, and culturally adapted tools to measure anxiety and adherence would allow for more accurate analysis. Effective, evidence-based services for the treatment of anxiety disorder and other common mental disorders are warranted across LMICs. Once such services are available, PLHIV should be routinely screened for mental health issues, including anxiety.
Supplementary Material
Acknowledgement:
The authors would like to thank Adrienne Shapiro MD, PhD, Rachel Kubiak, Haylea Hannah, and the other members of the Drain TB/HIV Research Lab for their mentorship and editing support.
Funding Sources: Infectious Disease Society of America Medical Scholars Program. Research reported in this publication was supported by the Infectious Disease Society of America Education & Research Foundation (IDSA ERF) and National Foundation for Infectious Diseases (NFID), the National Institute of Allergy and Infectious Disease of the National Institutes of Health (K23 AI108293), the National Institute for Mental Health (F31 MH112397), the Harvard University Center for AIDS Research (P30 AI060354), the Massachusetts General Hospital Executive Committee on Research, and the University of Washington / Fred Hutch Center for AIDS Research, an NIH-funded program under award number AI027757 which is supported by the following NIH Institutes and Centers: NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, NIDDK.. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or other funding agencies.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: Authors Wykowski, Kemp, Velloza, Rao and Drain all declare they have no conflicts of interest to report.
Ethical approval: This article does not contain any studies with human participants performed by any of the authors.
References
- 1.UNAIDS. 90–90-90 An ambitious treatment target to help end the AIDS epidemic United Nations; 2014. [Google Scholar]
- 2.UNAIDS. Ending Aids Progress Towards the 90–90-90 Targets. Glob Aids Updat [Internet] 2017;198 Available from: http://www.unaids.org/sites/default/files/media_asset/Global_AIDS_update_2017_en.pdf
- 3.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004. June;291(21):2581–90. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Mental Health Atlas Vol. 93, Bulletin of the World Health Organization; 2015. [Google Scholar]
- 5.Nakimuli-Mpungu E, Bass JK, Alexandre P, Mills EJ, Musisi S, Ram M, et al. Depression, alcohol use and adherence to antiretroviral therapy in sub-Saharan Africa: A systematic review. AIDS Behav 2012;16(8):2101–8. [DOI] [PubMed] [Google Scholar]
- 6.Wagner GJ, Ghosh-Dastidar B, Holloway IW, Kityo C, Mugyenyi P. Depression in the pathway of HIV antiretroviral effects on sexual risk behavior among patients in Uganda. AIDS Behav 2012. October;16(7):1862–9. [DOI] [PubMed] [Google Scholar]
- 7.Alemu H, Mariam DH, Tsui A, Ahmed S, Shewamare A. Effect of depressive symptoms and social support on weight and CD4 count increase at HIV clinic in Ethiopia. AIDS Care [Internet] 2012. [cited 2016 Jun 24];24(7):866–76. Available from: http://www.tandfonline.com.offcampus.lib.washington.edu/doi/pdf/10.1080/09540121.2011.648160 [DOI] [PubMed] [Google Scholar]
- 8.Krumme AA, Kaigamba F, Binagwaho A, Murray MB, Rich ML, Franke MF. Depression, adherence and attrition from care in HIV-infected adults receiving antiretroviral therapy. J Epidemiol Community Health 2015. March;69(3):284–9. [DOI] [PubMed] [Google Scholar]
- 9.Marconi VC, Wu B, Hampton J, Ordonez CE, Johnson BA, Singh D, et al. Early warning indicators for first-line virologic failure independent of adherence measures in a South African urban clinic. AIDS Patient Care STDS 2013. December;27(12):657–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brandt C, Zvolensky MJ, Woods SP, Gonzalez A, Safren SA, O’Cleirigh CM. Anxiety symptoms and disorders among adults living with HIV and AIDS: A critical review and integrative synthesis of the empirical literature. Clin Psychol Rev [Internet] 2017. February 17;51:164–84. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5195877/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonzalez A, Solomon SE, Zvolensky MJ, Miller CT. The interaction of mindful-based attention and awareness and disengagement coping with HIV/AIDS-related stigma in regard to concurrent anxiety and depressive symptoms among adults with HIV/AIDS. J Health Psychol 2009. April;14(3):403–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nilsson Schonnesson L, Diamond PM, Ross MW, Williams M, Bratt G. Baseline predictors of three types of antiretroviral therapy (ART) adherence: A 2-year follow-up. AIDS Care 2006. May;18(4):407–14. [DOI] [PubMed] [Google Scholar]
- 13.van Servellen G, Chang B, Garcia L, Lombardi E. Individual and system level factors associated with treatment nonadherence in human immunodeficiency virus-infected men and women. AIDS Patient Care STDS 2002. June;16(6):269–81. [DOI] [PubMed] [Google Scholar]
- 14.Wang Z Chinese version of Zung’s self-rating anxiety scale. J Shanghai Psychiatry 1984;(2):73–4. [Google Scholar]
- 15.Rooks-Peck CR, Adegbite AH, Wichser ME, Ramshaw R, Mullins MM, Higa D, et al. Mental health and retention in HIV care: A systematic review and meta-analysis. Health Psychol 2018. June;37(6):574–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comulada WS, Rotheram-Borus MJ, Pequegnat W, Weiss RE, Desmond KA, Arnold EM, et al. Relationships over time between mental health symptoms and transmission risk among persons living with HIV. Psychol Addict Behav 2010. March;24(1):109–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mimiaga MJ, Biello K, Reisner SL, Crane HM, Wilson J, Grasso C, et al. Latent class profiles of internalizing and externalizing psychosocial health indicators are differentially associated with sexual transmission risk: Findings from the CFAR network of integrated clinical systems (CNICS) cohort study of HIV-infected men eng. Health Psychol 2015. September;34(9):951–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sikkema KJ, Dennis AC, Watt MH, Choi KW, Yemeke TT, Joska JA. Improving mental health among people living with HIV: a review of intervention trials in low- and middle-income countries. Glob Ment Heal [Internet] 2015. September 9;2:e19 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4589870/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rabkin JG. Prevalence of psychiatric disorders in HIV illness. Int Rev Psychiatry [Internet] 1996. January 1;8(2–3):157–66. Available from: 10.3109/09540269609046300 [DOI] [Google Scholar]
- 20.APA. Diagnostic and Statistical Manual of Mental Disorders 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 21.Radzniwan R, Alyani M, Aida J, Khairani O, Nik Jaafar N, Tohid H. Psychological status and its clinical determinants among people living with HIV/AIDS (PLWHA) in Northern Peninsular Malaysia. HIV AIDS Rev [Internet] 2016;15(4 PG-141–146):141–6. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L613805034NS - [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009. July;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Veritas Health Innovation. Covidence Systematic Review Software [Internet] Melborne, Australia: 2018. Available from: www.covidence.org. [Google Scholar]
- 24.The World Bank. The World Bank In Middle Income Countries [Internet] Available from: http://www.worldbank.org/en/country/mic/overview
- 25.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010. April;1(2):97–111. [DOI] [PubMed] [Google Scholar]
- 26.Calvetti P, Giovelli P, Gauer G, de Moraes J. Psychosocial factors associated with adherence to treatment and quality of life in people living with HIV/AIDS in Brazil. J Bras Psiquiatr [Internet] 2014;63(1 PG-8–15):8–15. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L373126011 NS - [Google Scholar]
- 27.Amirkhanian Y, Kelly J, DiFranceisco W, Kuznetsova A, Tarima S, Yakovlev A, et al. Predictors of HIV Care Engagement, Antiretroviral Medication Adherence, and Viral Suppression Among People Living with HIV Infection in St. Petersburg, Russia. AIDS Behav [Internet] 2016;(PG-). Available from: NS - [DOI] [PMC free article] [PubMed]
- 28.Panigrahi M, Swain T, Mohanty S. Nonadherence to anti-HIV medication is associated with higher level of anxiety: Experience from a tertiary care hospital of Odisha. Indian J Pharmacol [Internet] 47(6 PG-672–5):672–5. Available from: NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campos LN, Guimarães M, Remien R. Anxiety and Depression Symptoms as Risk Factors for Non-adherence to Antiretroviral Therapy in Brazil. AIDS Behav [Internet] 2008;((Campos L.N., lorenza@medicina.ufmg.br; Guimarães M.D.C.; Remien R.H.) HIV Center for Clinical and Behavioral Studies, New York State Psychiatric Institute and Columbia University, New York City, United States: PG-1–11):1–11. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L50216332 NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qiao S, Li X, Zhou Y, Shen Z, Tang Z, Stanton B. The role of enacted stigma in parental HIV disclosure among HIV-infected parents in China. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV [Internet] 2015;27((Zhou Y.; Shen Z.; Tang Z.) Guangxi Center of Disease Control and Prevention, Nanning, China PG-28–35):28–35. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L607108520 NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prasithsirikul W, Chongthawonsatid S, Ohata P, Keadpudsa S, Klinbuayaem V, Rerksirikul P, et al. Depression and anxiety were low amongst virally suppressed, long-term treated HIV-infected individuals enrolled in a public sector antiretroviral program in Thailand. AIDS Care [Internet] 2017;29(3 PG-299–305):299–305. Available from: NS - [DOI] [PubMed] [Google Scholar]
- 32.Nguyen N, Tran B, Hwang L, Markham C, Swartz M, Vidrine J, et al. Effects of cigarette smoking and nicotine dependence on adherence to antiretroviral therapy among HIV-positive patients in Vietnam. AIDS Care [Internet] 2016;28(3 PG-359–64):359–64. Available from: NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nel A, Kagee A. The relationship between depression, anxiety and medication adherence among patients receiving antiretroviral treatment in South Africa. AIDS Care [Internet] 2013;25(8 PG-948–55):948–55. Available from: NS - [DOI] [PubMed] [Google Scholar]
- 34.Joshi B, Chauhan S, Pasi A, Kulkarni R, Sunil N, Bachani D, et al. Level of suboptimal adherence to first line antiretroviral treatment & its determinants among HIV positive people in India. Indian J Med Res [Internet] 2014;140(1 PG-84–95):84–95. Available from: NS - [PMC free article] [PubMed] [Google Scholar]
- 35.Guimarães M, Rocha G, Camos L, de Freitas F, Gualberto F, Teixeira R, et al. Difficulties reported by HIV-infected patients using antiretroviral therapy in Brazil. Clinics (Sao Paulo) [Internet] 2008;63(2 PG-165–72):165–72. Available from: NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adejumo O, Oladeji B, Akpa O, Malee K, Baiyewu O, Ogunniyi A, et al. Psychiatric disorders and adherence to antiretroviral therapy among a population of HIV-infected adults in Nigeria. Int J STD AIDS [Internet] 2016;27(11 PG-938–49):938–49. Available from: NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yunusa MA, Njoku CH, Obembe A. Self-reported adherence to treatment: a study of socioeconomic factors and psychiatric morbidity among male and female patients with HIV infection in Sokoto, Nigeria. Running title: Treatment adherence, socioeconomic factors and psychiatric morbidity in H. Niger J Med [Internet] 2014;23(1 PG-33–39):33–9. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L373495804 NS - [PubMed] [Google Scholar]
- 38.Pefura-Yone E, Soh E, Kengne A., Balkissou AD, Kuaban C. Non-adherence to antiretroviral therapy in Yaounde: Prevalence, determinants and the concordance of two screening criteria. J Infect Public Health [Internet] 2013;6(4 PG-307–315):307–15. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L52549011 NS - [DOI] [PubMed] [Google Scholar]
- 39.Tao J, Qian H, Kipp A, Ruan Y, Shepherd B, Amico K, et al. Effects of depression and anxiety on antiretroviral therapy adherence among newly diagnosed HIV-infected Chinese MSM. AIDS [Internet] 2017;31(3 PG-401–406):401–6. Available from: NS - [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yu Y, Luo D, Chen X, Huang Z, Wang M, Xiao S. Medication adherence to antiretroviral therapy among newly treated people living with HIV. BMC Public Health 2018;18(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pokhrel KN, Sharma VD, Pokhrel KG, Neupane SR, Mlunde LB, Poudel KC, et al. Investigating the impact of a community home-based care on mental health and anti-retroviral therapy adherence in people living with HIV in Nepal : a community intervention study. BMC Infec 2018;18:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nguyen NTP, Tran BX, Hwang LY, Markham CM, Swartz MD, Vidrine JI, et al. Effects of cigarette smoking and nicotine dependence on adherence to antiretroviral therapy among HIV-positive patients in Vietnam. AIDS Care [Internet] 2015. [cited 2016 Nov 26];1–6. Available from: http://www.tandfonline.com/action/journalInformation?journalCode=caic20 [DOI] [PMC free article] [PubMed]
- 43.Joshi B, Chauhan S, Pasi A, Kulkarni R, Sunil N, Bachani D, et al. Level of suboptimal adherence to first line antiretroviral treatment & its determinants among HIV positive people in India. Indian J Med Res [Internet] 2014. July [cited 2016 Nov 26];140(1):84–95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25222782 [PMC free article] [PubMed] [Google Scholar]
- 44.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988. December;56(6):893–7. [DOI] [PubMed] [Google Scholar]
- 45.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006. May;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 46.Stern AF. The hospital anxiety and depression scale. Occup Med (Lond) 2014. July;64(5):393–4. [DOI] [PubMed] [Google Scholar]
- 47.Zung WW. A rating instrument for anxiety disorders. Psychosomatics 1971;12(6):371–9. [DOI] [PubMed] [Google Scholar]
- 48.Rabin R, Oemar M, Oppe M, Janssen B, Herdman M. EQ-5D-5L user guide [Internet]. Basic information on how to use the EQ-5D-5L instrument 2015. Available from: http://www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/EQ-5D-5L_UserGuide_2015.pdf
- 49.World Health Organization. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP). mhGAP Interv Guid Ment Neurol Subst Use Disord Non-Specialized Heal Settings Ment Heal Gap Action Program [Internet] 2010;1–121. Available from: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:mhGAP+Intervention+Guide#1%5Cnhttp://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:mhGAP+intervention+guide#1%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/23741783
- 50.Barthel D, Barkmann C, Ehrhardt S, Bindt C. Psychometric properties of the 7-item Generalized Anxiety Disorder scale in antepartum women from Ghana and Cote d’Ivoire. J Affect Disord 2014. December;169:203–11. [DOI] [PubMed] [Google Scholar]
- 51.Chibanda D, Verhey R, Gibson LJ, Munetsi E, Machando D, Rusakaniko S, et al. Validation of screening tools for depression and anxiety disorders in a primary care population with high HIV prevalence in Zimbabwe. J Affect Disord 2016. July;198:50–5. [DOI] [PubMed] [Google Scholar]
- 52.Sweetland AC, Belkin GS, Verdeli H. MEASURING DEPRESSION AND ANXIETY IN SUB-SAHARAN AFRICA. Depress Anxiety [Internet] 2014. March 18;31(3):223–32. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4109689/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tennyson RL, Kemp CG, Rao D. Challenges and strategies for implementing mental health measurement for research in low-resource settings. Int Health 2016. November;8(6):374–80. [DOI] [PubMed] [Google Scholar]
- 54.Jiamsakul A, Kerr SJ, Kiertiburanakul S, Azwa I, Zhang F, Chaiwarith R, et al. Early suboptimal ART adherence was associated with missed clinical visits in HIV-infected patients in Asia. AIDS Care 2018. July;1–7. [DOI] [PMC free article] [PubMed]
- 55.Berg KM, Arnsten JH. Practical and Conceptual Challenges in Measuring Antiretroviral Adherence. J Acquir Immune Defic Syndr [Internet] 2006. December 1;43(Suppl 1):S79–87. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866146/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.WHO. WHO Prequalification of In Vitro Diagnostics PUBLIC REPORT Product : Xpert ® HIV-1 Viral Load with GeneXpert ® Dx, GeneXpert ® Infinity- 48, GeneXpert ® Infinity-48s and GeneXpert ® Infinity-80 WHO reference numbers : PQDx 0192–070-00, PQDx 0193–070-00 World Health Organization; 2017. [Google Scholar]
- 57.Dorward J, Drain PK, Garrett N. Point-of-care viral load testing and differentiated HIV care. lancet HIV 2018. January;5(1):e8–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Steele GI. Development and validation of the Xhosa translations of the Beck inventories: 2. Item analysis, internal consistency, and factor analysis. Vol. 18, Journal of psychology in Africa (south of the Sahara, the Caribbean, and Afro-Latin America) Enugu, Nigeria: :; 2008. p. 217. [Google Scholar]
- 59.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988. December;45(12):1069–77. [DOI] [PubMed] [Google Scholar]
- 60.Gureje O, Lasebikan VO, Kola L, Makanjuola VA. Lifetime and 12-month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well-Being. Br J Psychiatry [Internet] 2018/01/02. 2006;188(5):465–71. Available from: https://www.cambridge.org/core/article/lifetime-and-12month-prevalence-of-mental-disorders-in-the-nigerian-survey-of-mental-health-and-wellbeing/399785FE6103511ADBA2C3276E406CD3 [DOI] [PubMed] [Google Scholar]
- 61.Gureje O, Obikoya B. The GHQ-12 as a screening tool in a primary care setting. Soc Psychiatry Psychiatr Epidemiol 1990. September;25(5):276–80. [DOI] [PubMed] [Google Scholar]
- 62.Gureje O, Ogunniyi A, Kola L, Afolabi E. Functional disability among elderly Nigerians: results from the Ibadan Study of Ageing. J Am Geriatr Soc [Internet] 2006. November;54(11):1784–9. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2820715/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tran BX, Ohinmaa A, Nguyen LT. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual Life Outcomes 2012. November;10:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J Psychosom Res [Internet] 2002;52(2):69–77. Available from: http://www.sciencedirect.com/science/article/pii/S0022399901002963 [DOI] [PubMed] [Google Scholar]
- 65.Botega NJ, Bio MR, Zomignani MA, Garcia C Jr., Pereira WA. Mood disorders among inpatients in ambulatory and validation of the anxiety and depression scale HAD. Rev Saude Publica [Internet] 1995;29(5):355–63. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-0029384269&partnerID=40&md5=9a7981e7ea4306bacf73ca9722b6568f [DOI] [PubMed] [Google Scholar]
- 66.Lam CLK, Pan P-C, Chan AWT, Chan S-Y, Munro C. Can the Hospital Anxiety and Depression (HAD) Scale be used on Chinese elderly in general practice? Fam Pract [Internet] 1995. June 1;12(2):149–54. Available from: 10.1093/fampra/12.2.149 [DOI] [PubMed] [Google Scholar]
- 67.Abiodun OA. A validity study of the Hospital Anxiety and Depression Scale in general hospital units and a community sample in Nigeria. Br J Psychiatry 1994. November;165(5):669–72. [DOI] [PubMed] [Google Scholar]
- 68.Nilchaikovit T, Lotrakul M, Phisansuthideth U. Development of Thai version of Hospital Anxiety and Depression Scale in cancer patients. J Psychiatr Assoc Thail 1996;(41):18–30. [Google Scholar]
- 69.Lane DA, Jajoo J, Taylor RS, Lip GY, Jolly K. Cross-cultural adaptation into Punjabi of the English version of the Hospital Anxiety and Depression Scale. BMC Psychiatry 2007. January;7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thomas BC, Devi N, Sarita GP, Rita K, Ramdas K, Hussain BM, et al. Reliability and validity of the Malayalam hospital anxiety and depression scale (HADS) in cancer patients. Indian J Med Res 2005. November;122(5):395–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


