Abstract
The abuse of alcohol during adolescence is widespread and represents a particular concern given that earlier age of drinking onset is associated with increased risk for the development of alcohol use disorders (AUDs). Despite this risk, it remains unclear whether binge-like adolescent alcohol exposure facilitates drinking despite aversive consequences, a characteristic common among individuals with AUDs. The present study examined voluntary alcohol consumption and aversion-resistant drinking in adult male Long-Evans rats that had undergone adolescent intermittent ethanol (AIE) exposure by vapor inhalation between post-natal days (PD) 28-44. Ethanol consumption during adulthood was examined using a two-bottle choice (2BC) intermittent access procedure. Rats were tested for aversion-resistant drinking using ethanol adulterated with quinine (10, 30, 100 mg/L) after two 7-week periods of 2BC drinking. After completion of the second test of aversion-resistant drinking, rats were trained to operantly self-administer ethanol. The results revealed that both air control (AIR) and AIE exposed rats exhibited similar ethanol intake and preference in the 2BC paradigm. After seven weeks of 2BC drinking, quinine adulteration significantly suppressed ethanol intake, but only at the highest concentration examined (100 mg/L). However, upon retesting after a total of 17 weeks of 2BC drinking, 30 mg/L quinine suppressed ethanol intake. Notably, AIR and AIE exposed rats were equally sensitive to quinine adulterated ethanol at both time-points. In addition, AIR and AIE exposed rats responded similarly during operant ethanol self-administration on both fixed and progressive ratio schedules of reinforcement. Finally, both AIR and AIE exposed rats exhibited similar preference for sucrose. The results of this study show that binge-like ethanol vapor exposure during adolescence does not alter voluntary ethanol consumption, motivation to operantly respond for ethanol, or promote aversion-resistant ethanol consumption in adulthood. These data, together with previous work reporting conflicting results across various rodent models of adolescent alcohol exposure, underscore the need to further explore the role that exposure to alcohol during adolescence has on the development of heavy and compulsive drinking phenotypes in adulthood.
Keywords: Alcohol, Avoidance, Binge, Compulsive, Development, Quinine
Introduction
Consumption of alcohol during adolescence is widespread and represents a major health problem. Worldwide, an estimated 34% of individuals 15 to 19 years of age are current alcohol drinkers (World Health Organization, 2014). In the United States, alcohol is the most widely abused substance by adolescents, with the majority of 12th graders reporting lifetime alcohol use (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2017). Adolescents typically consume alcohol in intermittent binge-like patterns that often result in high levels of intoxication and “blackouts” (White, Jamieson-Drake, & Swartzwelder, 2002). A survey on adolescent binge drinking revealed that 10.5% of high school seniors in the U.S. reported consuming 10+ drinks in a row, and 5.6% reported consuming 15+ drinks in a row (Patrick et al., 2013). These instances of excessive alcohol intake are particularly alarming because they pose immense health risks in this age group. For example, the Global Burden of Disease Study 2013 reported that alcohol misuse is the leading cause of death for young people 15-24 years old (Mokdad et al., 2016).
In addition to overall health risks, adolescent alcohol use produces long-term changes in brain structure and function that can extend into adulthood (Spear, 2018). Adolescent alcohol use is frequently accompanied by accelerated reductions in cortical gray matter, attenuated development of white matter, and altered white matter integrity (Feldstein Ewing, Sakhardande, & Blakemore, 2014; Luciana, Collins, Muetzel, & Lim, 2013). Excessive drinking during adolescence is also correlated with functional impairments in learning and memory (Nguyen-Louie et al., 2016), attention (Tapert, Granholm, Leedy, & Brown, 2002), and visuospatial processing (Hanson, Medina, Padula, Tapert, & Brown, 2011), with preclinical observations in good consilience with these findings in humans. For example, rodent models have demonstrated that adolescent ethanol exposure similarly results in deficits in adulthood, including reduced regional brain volume, diminished white matter integrity, and impairments on cognitive tasks (Coleman Jr, He, Lee, Styner, & Crews, 2011; Gass et al., 2014; Vetreno, Yaxley, Paniagua, Johnson, & Crews, 2017).
Along with neural deficits, adolescent alcohol use is associated with a heightened risk for developing an alcohol use disorder (AUD) later in life. Specifically, earlier age of first alcohol use is associated with increased risk for the development of AUD symptoms (Dawson, Goldstein, Patricia Chou, June Ruan, & Grant, 2008; Hingson, Heeren, & Winter, 2006). One hallmark of AUD is seeking and taking of alcohol despite aversive consequences such as health risks, loss of job or family, and legal repercussions (Hasin et al., 2013). Aversion-resistant alcohol use is often accompanied by greater relapse vulnerability and proves difficult to treat using available methods (Hopf & Lesscher, 2014; Koob & Volkow, 2010).
In an effort to understand the neurobiological mechanisms underlying aversion-resistant alcohol consumption, this phenotype has been successfully recapitulated in animal models of alcohol dependence by adulterating ethanol with the bitter tastant quinine or pairing delivery of ethanol reinforcers with mild footshock (Hopf & Lesscher, 2014). Using these models, several groups have demonstrated the development of aversion-resistant ethanol intake following prolonged ethanol exposure and/or dependence (Hopf, Chang, Sparta, Bowers, & Bonci, 2010; Kimbrough, Kim, Cole, Brennan, & George, 2017; Seif et al., 2013, 2015; Vendruscolo et al., 2012) as well as the presence of this phenotype in selectively bred alcohol-preferring rats (Giuliano et al., 2018). Because adolescent alcohol use is associated with a heightened risk for developing AUD, an important question is whether adolescent alcohol exposure influences the development of AUD-related phenotypes, including aversion-resistant intake. Toward that end, the present study investigated whether binge-like exposure to ethanol during adolescence facilitated aversion-resistant ethanol intake in adulthood.
Materials & Methods
Animals
Two Long-Evans rat dams (Envigo, Indianapolis, IN), shipped with 10 pups each (two female, eight male) that were postnatal day (PD) 22 upon arrival. At PD 24, female pups were culled from the litter and remaining male pups were weaned and pair housed in standard polycarbonate cages. The vivarium was maintained on a reverse 12:12 light-dark cycle with lights off at 09:00. All rats had ad libitum access to food and water unless otherwise indicated. All experimental procedures were conducted with the approval of the Institutional Animal Care and Use Committee at the Medical University of South Carolina and adhered to the guidelines set forth by the National Research Council’s Guide for the Care and Use of Laboratory Animals (National Research Council, 2011).
Adolescent Intermittent Ethanol Exposure
Adolescent intermittent ethanol (AIE) exposure was carried out in a binge-like manner via vapor inhalation as described previously (Barker, Bryant, Osborne, & Chandler, 2017; Gass et al., 2014) in order to mimic high levels of alcohol exposure associated with typical adolescent drinking patterns. Half of the rats from each litter were randomly assigned to AIE or AIR groups (n=8/group). Vapor exposure was carried out between PD 28-44 and involved five repeating exposure cycles. Each cycle consisted of two consecutive days of intermittent exposure to ethanol vapor or air followed by two ethanol-free days (Figure 1). Each vapor exposure day began at 18:00 and lasted for 14 hrs. AIE exposed rats were scored for behavioral signs of intoxication daily immediately upon removal from the vapor chambers using a subjective 5-point scale (Gass et al., 2014; Nixon & Crews, 2002) where 1 = no signs of intoxication; 2 = slight motor impairment; 3 = obvious motor impairment but able to walk; 4 = dragging abdomen, loss of righting reflex; 5 = loss of righting and eyeblink reflexes. For the present study, we targeted a moderately high level of behavioral impairment, which corresponds to an intoxication score of 2-3 on the rating scale. The average intoxication score for all AIE exposed rats was 2.81 ± 0.18. As a complement to the intoxication score, tail-vein blood samples were collected after the second exposure day of each of the five cycles for determination of blood ethanol concentrations (BECs) using an Analox alcohol analyzer (Analox Instruments, Atlanta, GA). AIE exposed rats achieved an average BEC (mg/dL) of 428.3 ± 22.9 across all five exposure cycles. Following completion of the last exposure cycle, rats were left undisturbed in their home cages for 15 days until individually housed at PD 59 in preparation for initiation of home cage drinking.
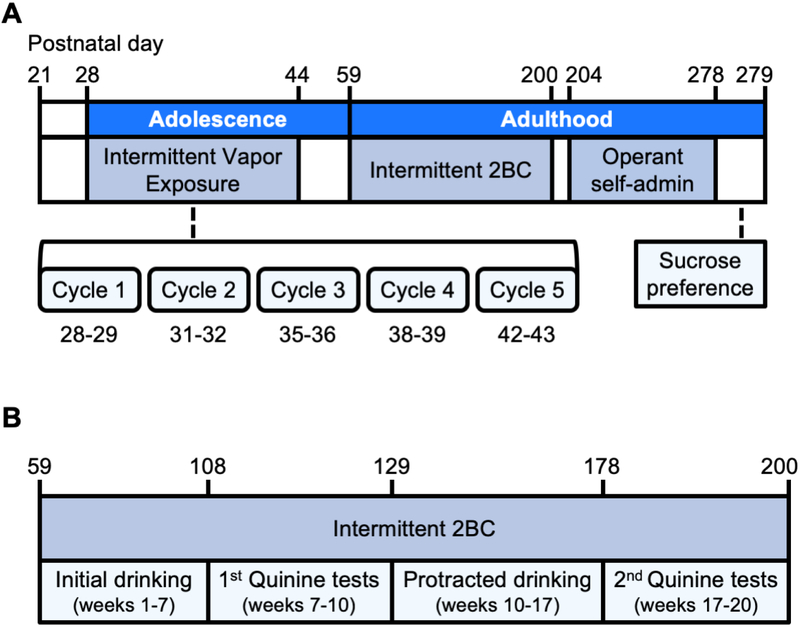
Figure 1. Schema of experimental timeline.
(A) Pair-housed Long-Evans rats were exposed to five cycles of intermittent ethanol vapor inhalation between PD 28-44 and tested in adulthood for two-bottle choice (2BC) and quinine adulterated ethanol drinking, operant ethanol self-administration, and sucrose preference. Litter mate control rats were exposed to plain air during the ethanol exposure period. (B) Intermittent 2BC drinking consisted of 20 cumulative weeks of home cage ethanol drinking. To examine aversion resistant drinking, the effects of quinine adulteration of the ethanol solution was examined after two 7-week periods of intermittent 2BC drinking separated by the first quinine test. Both quinine test sessions involved adulteration of the ethanol bottle with increasing concentrations of quinine. Each concentration of quinine was tested on Wednesdays of each of the three weeks, with unadulterated ethanol provided on the Monday and Friday of each week of quinine testing.
Two-bottle choice intermittent alcohol access and aversion-resistant drinking
Home cage drinking was assessed using a standard 2BC intermittent alcohol access procedure as previously described (Simms et al., 2008). On Monday, Wednesday, and Friday of each week, rats were provided access to two bottles, with one bottle containing water and the other containing ethanol (20% v/v). On all other days, the rats were provided access to two bottles containing water only. Fluid intake was measured 30 min and 24 hrs after the start of each drinking session by calculating the difference in bottle weights prior to bottle insertion and following bottle removal. The position of the ethanol bottle was alternated for each session to control for side preferences. An empty cage with both water and ethanol containing bottles was used to correct for spillage associated with inserting and removing bottles. Unadulterated ethanol intake was examined across two 7-week periods with the first (PD 59-106) and second (PD 131-176) 2BC periods separated by the first test of aversion-resistant ethanol intake. A second test of aversion-resistant ethanol intake was performed following the second 2BC period which thus represented a total of 17 weeks of 2BC drinking (Figure 1). Therefore, the end of the first period of 2BC drinking, when the first quinine test session was initiated, represented seven weeks of intermittent 2BC drinking (21 drinking days), and the end of the second period of 2BC drinking, when the second quinine test session was initiated, represented a cumulative period of 17 weeks of drinking (51 drinking days). Aversion-resistant ethanol consumption was evaluated using a standard quinine-adulteration procedure (Hopf et al., 2010). Ethanol drinking bottles were adulterated with increasing concentrations of quinine (10, 30, 100 mg/L) once a week on Wednesdays. Thus, testing occurred over a period of three weeks (a total of nine drinking days), with unadulterated ethanol being provided on Mondays and Fridays during this period.
Operant Ethanol Self-administration and response motivation
Following completion of 2BC drinking, rats were trained to operantly self-administer ethanol (Figure 1) using standard operant boxes (Med Associates, St. Albans, VT, United States) fitted with a house light and two cue lights located above two retractable levers. Levers were separated by a receptacle connected to a syringe pump that enabled delivery of liquid reinforcer. To facilitate acquisition of operant responding, rats were food restricted to 85% of their free-feeding weight. They were then trained to lever press on a fixed ratio (FR) 1 schedule of reinforcement where one response on the active lever resulted in the delivery of 100 uL of ethanol (20% v/v). Ethanol delivery was accompanied by retraction of both levers, illumination of cue light above the active lever, and illumination of liquid receptacle. Responses on the inactive lever were recorded but had no programed consequences. Upon stable responding, rats transitioned to an FR3 schedule and the concentration of the ethanol reinforcer was reduced to 10% (v/v). Responding during the last seven FR3 sessions was used to assess operant self-administration rates between groups. The liquid receptacle was inspected following each operant session and used to confirm that all rats had consumed all ethanol reinforcers during these operant sessions. Two AIR and three AIE rats were excluded from analysis due to failure to acquire ethanol self-administration.
Progressive Ratio and Sucrose Preference Test
To assess potential group differences in the motivation to respond for ethanol, rats underwent two sessions using a progressive ratio (PR) schedule of reinforcement based on methods adapted from Hopf et al (2010). Following the first PR session, the rats returned to an FR3 schedule for a minimum of three days before the second PR session. In the PR procedure, the number of lever presses required to obtain ethanol reinforcer was calculated as follows using previously published methods (Bowers et al., 2008; Hopf et al., 2010): responses per reinforcer = 5e(0.1 x reinforcer(s)previously earned) – 5. PR sessions terminated after five hours or if 20 min elapsed without any responses on the active lever. Breakpoint was defined as the final response ratio completed.
Following completion of PR responding for ethanol, rats were tested for sucrose preference in their home cage. Water bottles were removed and three hours later rats were presented with two bottles, one containing 10% sucrose (w/v) and the other containing water. Sucrose and water consumption were measured following one hour of access to both bottles.
Statistical Analysis
Repeated measures analysis of variance (RM ANOVA) with adolescent exposure and drinking day as factors were used to analyze water intake, ethanol intake, and ethanol preference during intermittent 2BC. RM ANOVAs with exposure and quinine concentration as factors were used to analyze ethanol consumption and preference during quinine testing. Similarly, RM ANOVAs with exposure and session as factors were used to analyze the number of ethanol reinforcers obtained and ethanol breakpoint. Unpaired two-tailed t-tests were used to analyze mean fluid intake, sucrose preference, and sucrose intake. Bonferroni corrections were applied to all pairwise comparisons to correct for multiple comparisons following significant main effects or interactions. All data were analyzed using GraphPad Prism 7.0 software. Data are presented as means ± SEM, and effects were considered statistically significant at p ≤ 0.05.
Results
Effect of AIE on aversion-resistant ethanol drinking using two-bottle choice intermittent access
To investigate the hypothesis that binge-like adolescent alcohol exposure promotes aversion-resistant drinking, rats first voluntarily consumed ethanol using a standard 2BC intermittent access procedure. Quinine adulterated ethanol was then used to examine the development of aversion-resistant drinking after two periods of access to unadulterated ethanol (Figure 1). In the first set of studies, we examined the time course of changes in ethanol consumption in AIR and AIE exposed rats during the first 7-week period of 2BC drinking. Similar to previous work (Carnicella, Amamoto, & Ron, 2009; Simms et al., 2008), both groups exhibited a progressive increase in ethanol consumption over the first 3-4 weeks of 2BC drinking that subsequently stabilized over the course of the remaining 2-3 weeks (Figure 2A, 2B). Analysis by RM ANOVA of consumption at the 30 min time-point revealed a main effect of day (F(20, 260) = 6.661, p < 0.001), but no main effect of exposure (F(1, 13) = 0.670, p = 0.428) or day by exposure interaction (F(20, 260) = 0.805, p = 0.705). Analysis of consumption at the 24 hr time-point also revealed a main effect of day (F(20, 260) = 8.918, p < 0.001), but no main effect of exposure (F(1, 13) = 0.334, p = 0.572) or day by exposure interaction (F(20, 260) = 0.556, p = 0.938). Taken together, these data show that rats escalated their consumption of ethanol during the first 7-week period of 2BC drinking as expected, but AIE exposure did not alter either the rate of escalation or total ethanol intake after reaching a stable baseline.
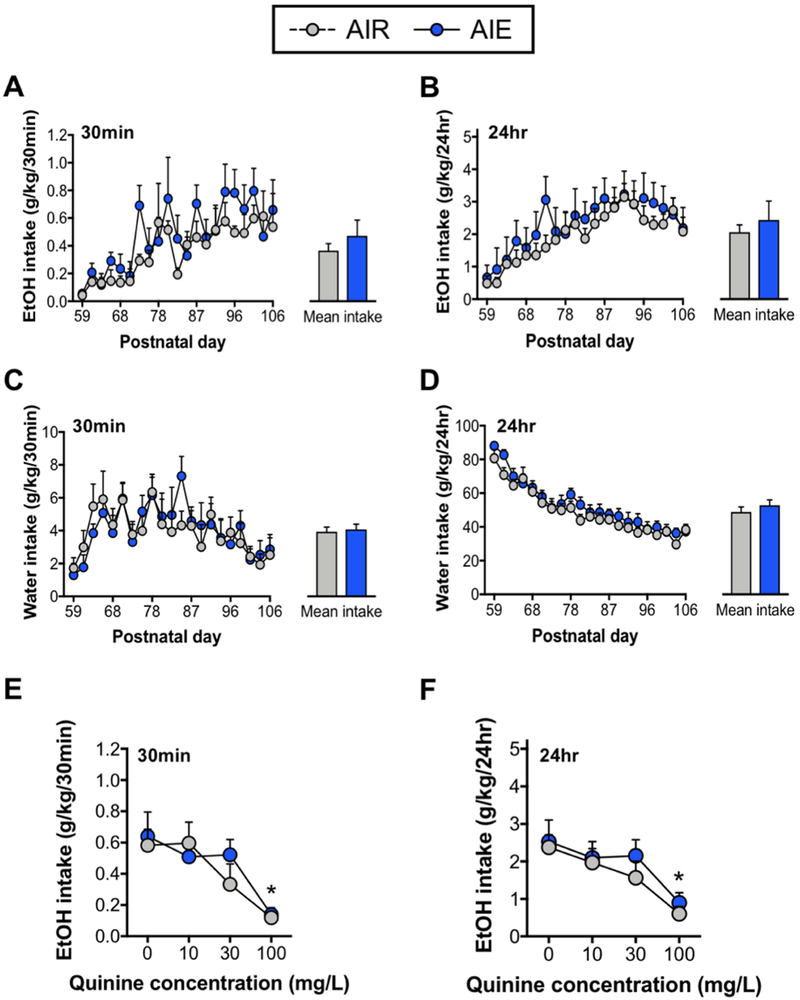
Figure 2. Ethanol consumption, water consumption, and quinine resistant drinking after the first 7-week period of two-bottle choice drinking.
Measurement of ethanol consumption at the 30 min (A) and 24 hr (B) time points during the first 7-week period of intermittent 2BC drinking. Both AIR control and AIE exposed rats significantly escalated consumption over drinking days. There was no significant difference between AIR and AIE exposed rats in the average daily consumption of ethanol across the entire drinking period (bar graph insets). The volume of water consumed by AIR and AIE exposed rats at 30 min (C) and 24 hr (D) time points also did not differ significantly. Both AIR and AIE groups elevated their 30 min water intake across days, whereas 24 hr water intake progressively decreased over time and showed little variability. Average intake was not significantly different between AIR and AIE exposed rats at either time-point (bar graph insets). Following the first 7-week period of 2BC drinking, assessment of quinine suppression of ethanol intake revealed a significant decrease in consumption relative to baseline that was only observed at the highest concentration (100 mg/L) of quinine tested at both the 30 min (E) and 24 hr (F) time-points. There were no significant differences in intake between AIR and AIE at any concentration of quinine adulterated ethanol. Baseline drinking represented consumption during the week preceding initiation of quinine testing. Asterisks indicate significantly different from 0 mg/L. *p < 0.05; n = 7-8/group.
In addition to assessment of ethanol consumption, changes in water consumption were examined. Analysis by RM ANOVA of water intake during the 30 min time-point (Figure 2C) revealed a main effect of day (F(20, 260) = 4.592, p < 0.001), but no main effect of exposure (F(1,13) = 0.020, p = 0.885) or day by exposure interaction (F(20, 260) = 0.719, p = 0.804). For the 24 hr time-point (Figure 2D), RM ANOVA revealed a main effect of day (F(20, 260) = 43.29, p < 0.001), but no main effect of exposure (F(1, 13) = 0.878, p = 0.365) or a day by exposure interaction (F(20, 260) = 0.719, p = 0.805). These data suggest that, as expected, overall water intake steadily decreased over time as ethanol intake increased.
The next set of studies used quinine adulteration of the ethanol solution to determine whether AIE exposure altered the development of aversion-resistant drinking following the first 7-week period of 2BC drinking (Figure 2E, 2F). For this experiment, the average level of ethanol consumed during the week prior to initiation of quinine testing was taken as the baseline level of consumption. Analysis by RM ANOVA of consumption at the 30 min time-point revealed a main effect of quinine concentration (F(3, 39) = 10.86, p < 0.001), but no main effect of exposure (F(1, 13) = 0.196, p = 0.664) or concentration by exposure interaction (F(3, 39) = 0.772, p = 0.516). Pairwise comparisons indicated that while 10 and 30 mg/L quinine adulteration had no impact on ethanol consumption, 100 mg/L quinine significantly suppressed ethanol intake (p values < 0.01). Analysis of ethanol consumption at the 24 hr time-point also revealed a main effect of concentration (F(3, 39) = 17.08, p < 0.001), but no main effect of exposure (F(1, 13) = 0.359, p = 0.559) or concentration by exposure interaction (F(3, 39) = 0.361, p =0.780). Similar to results at the 30 min time-point, pairwise comparisons indicated that 100 mg/L, but not 10 or 30 mg/L, significantly suppressed ethanol intake (p values < 0.01). These results indicate that AIE exposure did not accelerate the onset of aversion-resistant drinking following the first seven weeks of intermittent 2BC drinking.
After completion of the first test of aversion-resistant drinking, rats returned to drinking unadulterated ethanol (Figure 1), and consumption was again monitored for an additional seven weeks of 2BC drinking. As before, consumption was assessed at both 30 min and 24 hr time-points (Figure 3A, 3B) on each drinking day. Analysis by RM ANOVA of consumption at the 30 min time-point revealed a main effect of day (F(18, 234) = 2.663, p < 0.001), but no main effect of exposure (F(1, 13) < 0.001, p > 0.99) or day by exposure interaction (F(18, 234) = 1.217, p = 0.248). For the 24 hr time-point, analysis by RM ANOVA revealed no main effect of day (F(18, 243) = 1.512, p = 0.086) or exposure (F(1, 13) = 0.164, p = 0.692), and no day by exposure interaction (F(18, 243) = 0.1.455, p = 0.107). These observations indicate that, in contrast to the escalation of baseline drinking during the first 7-week period of 2BC drinking, ethanol consumption during the second 7-week 2BC drinking period remained stable. In addition, similar to our observation during the first drinking period, AIE exposure did not alter total ethanol consumption during the second 7-week 2BC drinking period.
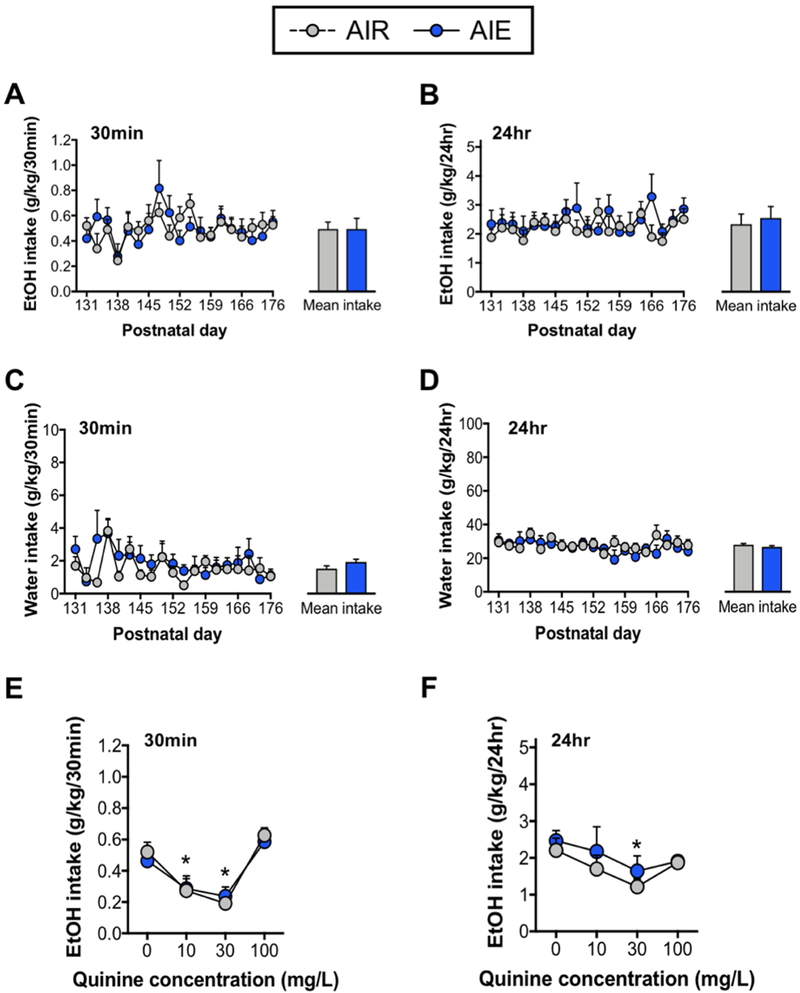
Figure 3. Ethanol consumption, water consumption, and quinine resistant consumption after 17 weeks of two-bottle choice drinking.
Measurement of ethanol intake at the 30 min (A) and 24 hr (B) time points over the second 7-week period of intermittent 2BC drinking. Both AIR and AIE exposed rats exhibited stable ethanol intake across days. The average daily consumption of ethanol over the drinking period was not significantly different between groups (bar graph insets). The volume of water consumed by AIR and AIE exposed rats at 30 min (C) and 24 hr (D) time points during the second 7-week 2BC drinking period. Day to day consumption of water at both the 30 min and 24 hr time points was stable, and again there were no differences between AIR and AIE exposed rats in average intake (bar graph insets). Following a total of 17 weeks of 2BC drinking, assessment of quinine suppression of consumption revealed significant decreases in ethanol intake relative to baseline at the 30 min time-point (E) for the 10 and 30 mg/L concentrations of quinine, but not for the 100 mg/L concentration. Similarly, 30 mg/L quinine reduced consumption at the 24 hr time-point (F) indicating partial expression of aversion resistant drinking. No significant differences between AIR and AIE exposed rats were observed at any quinine concentrations tested. Asterisks indicate significantly different from 0 and 100 mg/L (E) or only 0 mg/L (F). *p < 0.05; n = 7-8/group.
Water consumption was also assessed during the second 7-week period of 2BC drinking. Analysis by RM ANOVA of water intake at the 30 min time-point (Figure 3C) revealed a main effect of day (F(18, 234) = 2.271, p < 0.001), but no main effect of exposure (F(1, 13) = 0.438, p = 0.519) or day by exposure interaction (F(18, 234) = 1.042, p = 0.413). Analysis of consumption at the 24 hr time-point (Figure 3D) revealed a main effect of day (F(18, 234) = 1.994, p = 0.109), but no main effect of exposure (F(1, 13) = 0.143, p = 0.711) or day by exposure interaction (F(18, 234) = 1.621, p = 0.055). Lastly, unpaired t-tests indicated that total fluid intake (i.e., the sum of the volume of water and ethanol consumed) was similar for both exposure groups during both the first (AIR: 24.81±0.275, AIE: 25.1±0.302; t(13) = 0.702, p = 0.495) and second (AIR: 24.8±0.378, AIE: 23.92±0.391; t(13) = 1.607, p = 0.132) 7-week period of 2BC drinking. Taken together, these results are consistent with previous observations (Simms et al., 2008) involving the 2BC intermittent access procedure in which rats display a corresponding decrease in the amount of water consumed as ethanol intake progressively increases, with both becoming stable after an extended period of drinking (e.g. compare Figure 2D with Figure 3D).
Assessment of aversion-resistant intake was re-examined at the end of the second 7-week 2BC period after a total of 17 weeks of 2BC drinking. (Figure 3E, 3F). As before, the average daily amount of alcohol consumed during the week prior to initiation of aversion-resistant drinking was used as baseline consumption. Analysis of consumption at the 30 min time-point by RM ANOVA revealed a main effect of quinine concentration (F(3, 39) = 21.28, p < 0.001), but no main effect of exposure (F(1, 13) = 0.024, p = 0.877) or concentration by exposure interaction (F(3, 39) = 0.367, p = 0.776). Pairwise comparisons indicated that 10 and 30 mg/L quinine significantly suppressed ethanol intake relative to baseline and the 100 mg/L concentration (p values < 0.05). However, adulteration of ethanol with 100 mg/L quinine did not significantly alter intake relative to baseline (p > 0.05). Analysis of intake at the 24 hr time-point revealed a main effect of quinine concentration (F(3, 39) = 4.326, p = 0.011), but no main effect of exposure (F(1, 13) = 0.490, p = 0.496) or concentration by exposure interaction (F(3, 39) = 0.301, p = 0.824). In contrast to intake at the 30 min time-point, pairwise comparisons indicated that only 30 mg/L quinine significantly suppressed 24 hr ethanol intake relative to baseline (p = 0.006). Taken together, these data support the idea that AIR and AIE exposed rats become sensitized to bitter taste following repeated exposure to quinine such that lower quinine concentrations serve to limit binge (30 min) alcohol intake. However, this sensitization was not great enough to significantly limit levels of intake spanning 24 hrs.
To complement the analysis of ethanol consumption, ethanol preference was also examined during the first and second 7-week periods of 2BC drinking, and during the two tests of aversion-resistant drinking. As expected, the results for ethanol preference mirror our findings with respect to ethanol intake across the study. Specifically, for the first 7-week drinking period (Figure 4A, 4B), RM ANOVA analysis of ethanol preference at the 30 min time-point revealed a main effect of day (F(20, 260) = 5.511, p < 0.001), but no main effect of exposure (F(1, 13) = 0.175, p = 0.682) or day by exposure interaction (F(20, 260) = 0.754, p = 0.767). For the 24 hr time-point, analysis of preference revealed a main effect of day (F(20, 260) = 12.16, p < 0.001), but no main effect of exposure (F(1, 13) = 0.047, p = 0.830) or day by exposure interaction (F(20, 260) = 0.490, p = 0.968). For preference at the 30 min time-point during the first quinine test period (Figure 4C and 4D), analysis of the data by RM ANOVA revealed a main effect of concentration (F(3, 39) = 14.08, p < 0.001), but no main effect of exposure (F(1, 13) = 0.009, p = 0.925) or concentration by exposure interaction (F(3, 39) = 0.546, p 0.653). Pairwise comparisons indicated that 100 mg/L quinine significantly suppressed ethanol preference relative to baseline and to the two other concentrations of quinine (p values < 0.05). Analysis of ethanol preference at the 24 hr time-point indicated a main effect of concentration (F(3, 39) = 15.95, p < 0.001), but no main effect of exposure (F(1, 13) = 0.152, p = 0.702) or concentration by exposure interaction (F(3, 39) = 0.509, p = 0.678). Pairwise comparisons also indicated that 100 mg/L quinine significantly suppressed ethanol preference relative baseline and to the two other concentrations of quinine (p values < 0.01). Taken together, these data indicate that, similar to the escalation and stabilization of ethanol consumption during the first 7-week period of 2BC drinking, ethanol preference during this time exhibited a similar pattern of escalation followed by stabilization. In addition, AIE exposure did not alter ethanol preference during either the first period of 2BC drinking or during the first quinine test.
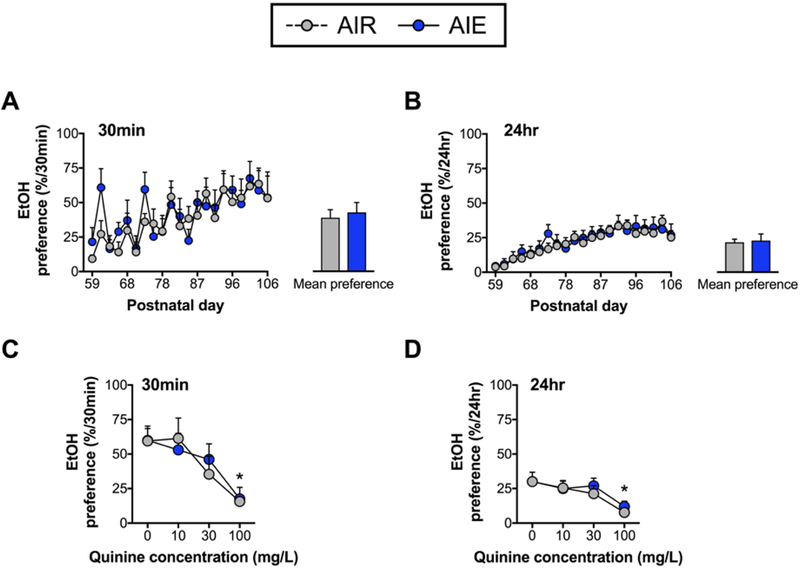
Figure 4. Ethanol preference during the first 7-week period of two-bottle choice drinking and quinine testing.
Measurement of ethanol preference at the 30 min (A) and 24 hr (B) time-points during the first 2BC drinking period. Both AIR and AIE exposed rats exhibited escalated preference over drinking days. The mean preference across all drinking days was not significantly different between AIR and AIE exposed rats (bar graph insets). Following the first 2BC drinking period, AIR and AIE exposed rats exhibited comparable preference for quinine adulterated ethanol across increasing concentrations at both the 30 min (C) and 24 hr (D) time points. As indicated by the asterisks, significant suppression of ethanol preference was observed in both AIR and AIE exposed groups at the highest concentration of quinine (100 mg/L) relative to baseline (0 mg/L). *p < 0.05; n = 7-8/group.
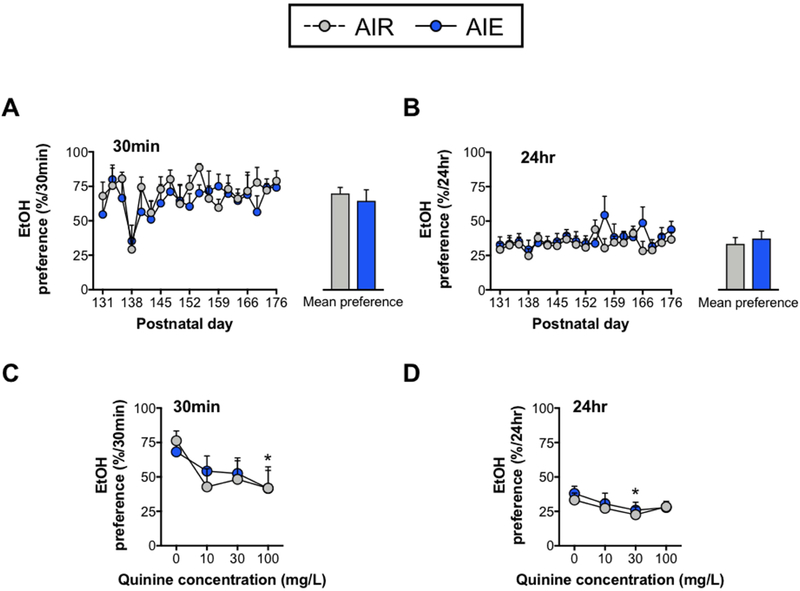
With respect to ethanol preference during the second 7-week 2BC drinking period (Figure 5A, 5B), analysis by RM ANOVA at the 30 min time-point revealed a main effect of day (F(18, 234) = 3.604, p < 0.001), but no main effect of exposure (F(1, 13) = 0.308, p = 0.588) or day by exposure interaction (F(18, 234) = 0.808, p = 0.689). Analysis of ethanol preference at the 24 hr time-point showed a main effect of day (F(18, 234) = 1.745, p = 0.033) and day by exposure interaction (F(18, 234) = 1.648, p = 0.049), but no main effect of exposure (F(1, 13) = 0.281, p = 0.604). These data indicate that ethanol preference was stable and was not altered by AIE exposure. Analysis by RM ANOVA of ethanol preference at the 30 min time-point during the second quinine test (Figure 5C, 5D) showed a main effect of quinine concentration (F(3, 39) = 3.901, p = 0.015), but no main effect of exposure (F(1, 13) = 0.024, p = 0.878) or concentration by exposure interaction (F(3, 39) = 0.372, p = 0.773). Pairwise comparisons indicated that 100 mg/L quinine significantly reduced ethanol preference relative to baseline (p < 0.05). Analysis of ethanol preference at the 24 hr time-point also revealed a main effect of quinine concentration (F(3, 39) = 3.746, p = 0.018), but no main effect of exposure (F(1, 13) = 0.169, p = 0.687) or concentration by exposure interaction (F(3, 39) = 0.217, p = 0.884). Pairwise comparisons indicated that 30 mg/L quinine significantly reduced ethanol preference relative to baseline preference (p < 0.05). Therefore, as with ethanol preference observed during the second 7-week period of unadulterated ethanol 2BC drinking, AIE exposure did not significantly alter preference for quinine adulterated ethanol during the second test of aversion-resistant drinking.
Figure 5. Ethanol preference during the second 7-week period of two-bottle choice drinking and second quinine test.
Measurement of ethanol preference at the 30 min (A) and 24 hr (B) time points over the second 7-week 2BC drinking period. Both AIR and AIE exposed rats exhibited stable preference across days, and the mean preference for all drinking days was not significantly different between groups (bar graph insets). Following protracted 2BC drinking, no significant differences in preference were observed between groups during quinine adulterated drinking sessions at either 30 min (C) or 24 hr (D) time points. As indicated by the asterisks, preference in both groups was significantly reduced, relative to baseline, by 30 mg/L quinine at the 30 min time point, and by 100 mg/L quinine at the 24 hr time point. *p < 0.05; n = 7-8/group.
Effect of AIE on operant ethanol self-administration and response motivation
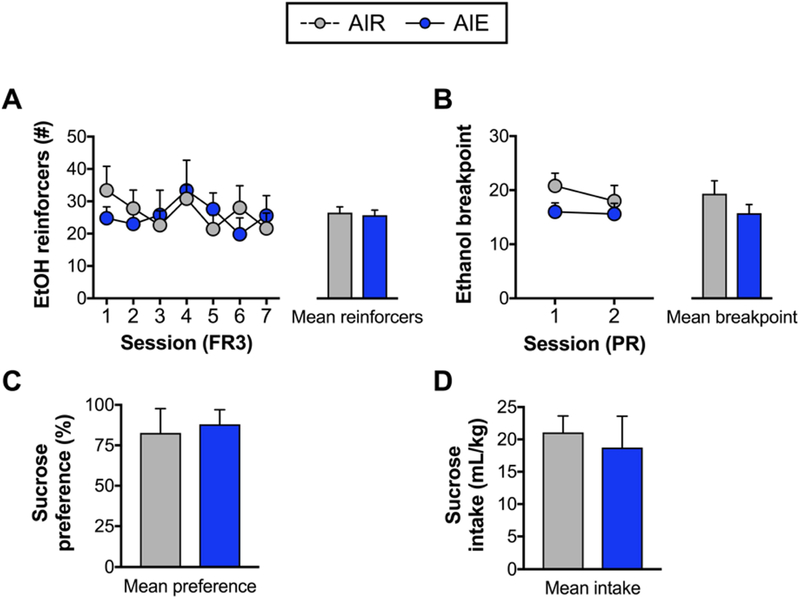
Following completion of 2BC and quinine-adulterated home cage drinking, the effects of AIE exposure on the willingness to work for ethanol was examined using operant self-administration. Responding for ethanol was compared between groups following acquisition of stable lever pressing behavior. As shown in Figure 6A, analysis by RM ANOVA indicated no main effect of session (F(6, 48) = 1.711, p = 0.138) or exposure (F(1, 8) = 0.013, p = 0.909), and no session by exposure interaction (F(6, 48) = 1.576, p = 0.174). Therefore, both AIR and AIE exposed rats exhibited similar levels of responding for ethanol. In the next set of studies, responding on a PR schedule of reinforcement was used to assess whether AIE exposure impacted the motivation for ethanol. Figure 6B shows the breakpoint for ethanol responding across two separate PR sessions and breakpoint as an average for both sessions (bar graph inset). Analysis by RM ANOVA of the two PR sessions revealed no main effect of session (F(1, 8) = 1.403, p = 0.270) or exposure (F(1, 8) = 1.557, p = 0.247), and no session by exposure interaction (F(1, 8) = 0.789, p = 0.400). Therefore, these data indicate that both AIR and AIE exposed groups exhibited a similar motivation to obtain ethanol.
Figure 6. Operant ethanol self-administration and sucrose preference test following protracted two-bottle choice drinking.
(A) Number of ethanol reinforcers obtained across seven operant sessions under an FR3 schedule of reinforcement. Both groups exhibited similar levels of responding for ethanol. (B) When tested on a progressive ratio schedule of reinforcement, AIR and AIE exposed groups exhibited similar breakpoints for ethanol across sessions. There was no difference between AIR and AIE exposed rats in their preference (C) or intake (D) during the sucrose preference test. n = 5/group.
The final set of studies examined sucrose preference and intake to assess whether AIE exposure altered anhedonia-like behavior or consumption of a non-drug reinforcer. Analysis of the results presented in Figure 6C and 6D indicated that neither consumption (mL/kg; t(8) = 0.429, p = 0.678) nor preference for sucrose (t(8) = 0.304, p = 0.768) were significantly different between AIR and AIE exposed rats (unpaired t-test), indicating that AIE exposure did not alter the hedonic set point of the rats.
Discussion
A number of previous studies have observed that binge-like exposure to ethanol in adolescent rats is associated with long-term changes in behavior including cognitive impairments characterized by inflexibility and alterations in the processing of rewarding/aversive information (Spear, 2018). Based on these lasting effects of adolescent alcohol exposure, the goal of the present study was to test the hypothesis that binge-like adolescent alcohol exposure promotes aversion-resistant drinking in adulthood. We reasoned that this would be observed as a more rapid onset of aversion-resistant drinking and/or a change in the sensitivity to varying concentrations of quinine. In addition, we hypothesized that adolescent alcohol exposure would augment ethanol intake in adulthood, which would be represented by increased voluntary ethanol consumption in 2BC and/or increased responding for ethanol during operant self-administration. In contrast to our expectations, the results of the present study reveal that exposure of adolescent rats to intermittent binge-like ethanol by vapor inhalation does not alter voluntary ethanol consumption, aversion-resistant drinking, or motivation for ethanol in adulthood.
Specifically, examination of quinine adulterated ethanol consumption revealed that rats from both AIR and AIE groups exhibited aversion-resistant drinking with the 10 mg/L and 30 mg/L concentrations of quinine, while intake was equally suppressed at the 100 mg/L concentration. Thus, the results revealed that after the first 7-week 2BC drinking period, both AIR and AIE exposed rats were equally sensitive to quinine adulteration of the ethanol solution. Our observation of resistance to ethanol adulterated with relatively low quinine concentrations was surprising given that previous work has reported sensitivity to quinine adulterated ethanol at 10-30 mg/L concentrations following ethanol drinking of a similar time frame or longer (Kimbrough et al., 2017; Seif et al., 2015). For example, Seif and colleagues (2015) observed suppression of ethanol intake at 30 mg/L quinine following six and eight weeks of intermittent 2BC drinking despite similar methodological approaches to those used in the present study (e.g., the intermittent 2BC and quinine testing procedures). However, strain differences may help explain these discrepancies given that the present study was carried out in Long-Evans rats, whereas the study by Seif et al used Wistar rats. In support of this, Tordoff and colleagues (Tordoff, Alarcon, & Lawler, 2008) assessed quinine sensitivity across 14 different rat strains and found that Long-Evans rats exhibited greater preference for quinine over water relative to Wistar rats.
Similar to the results of the quinine testing performed after the first 7-week period of 2BC drinking, AIE had no significant effect on aversion-resistant ethanol intake when examined following protracted ethanol consumption after a total of 17 weeks of 2BC drinking. At this time period, both AIR and AIE exposed rats reduced their ethanol consumption in the presence of the two lower concentrations of quinine (10 and 30 mg/L) but did not reduce their intake of ethanol adulterated with the higher 100 mg/L quinine concentration. This latter observation was unexpected as this same concentration of quinine has been shown to reduce voluntary ethanol consumption following 12-16 weeks of intermittent 2BC drinking (Hopf et al., 2010; Spoelder et al., 2015) and 52 weeks of continuous 2BC drinking (Turyabahika-Thyen & Wolffgramm, 2006).
While strain differences may have contributed to differences in sensitivity to 100 mg/L quinine after protracted 2BC drinking, procedural differences may have also played a role. In the present study, each rat was presented with three concentrations of quinine in ascending order during each of the two test periods of aversion-resistant drinking. Exposure to successively increasing concentrations of quinine following the initial 2BC period may have increased sensitivity to lower concentrations of quinine during re-testing as suggested by previous work (Mook & Blass, 1968). It remains unclear, however, why insensitivity was observed to adulteration by the 100 mg/L concentration of quinine following 17 weeks of ethanol drinking. Additional studies in the absence of repeated quinine exposure will be necessary to determine whether prolonged ethanol exposure has selective effects on alcohol consumption with adulteration of high versus low quinine concentrations. Regardless of nuances in the differences in sensitivity to different concentrations of quinine, our results clearly show that AIE exposure did not alter either the development of aversion-resistant drinking after the first 7-week period of intermittent 2BC drinking, or alter the sensitivity to quinine when retested after protracted 2BC drinking.
Our results also revealed that AIE exposure did not facilitate escalated drinking or motivation to drink ethanol in adulthood when assessed after a protracted period of ethanol drinking. These results agree with previous work reporting a similar absence of escalated ethanol intake during adulthood using the vapor exposure paradigm (Jury et al., 2017; Slawecki & Betancourt, 2002). However, not all findings are in agreement. The majority of work demonstrating a faciliatory effect of adolescent ethanol exposure on ethanol intake in adulthood has been conducted using either experimenter administered intraperitoneal (i.p.) or intragastric (i.g.) ethanol (e.g., Alaux-Cantin et al., 2013; Maldonado-Devincci, Alipour, Michael, & Kirstein, 2010; Pandey, Sakharkar, Tang, & Zhang, 2015) or voluntary oral self-administration (Amodeo, Kneiber, Wills, & Ehlers, 2017; Broadwater, Varlinskaya, & Spear, 2013; Moore, Mariani, Linsenbardt, Melón, & Boehm, 2010). Thus, route of ethanol administration may be an important factor in driving positive results. It is possible that the nature of repeated, forced administration of ethanol via the i.p. or i.g. route of administration acts synergistically with voluntary ethanol consumption to facilitate increased ethanol intake in adulthood (relative to the effects produced using the more passive ethanol vapor exposure procedure). Whereas, increased ethanol intake in adulthood following oral self-administration during adolescence may be attributed, at least in part, to familiarity and learned experiences associated with consuming alcohol (e.g., Broadwater et al., 2013). Differences in BEC achieved using various routes of administration may also play a role. For example, while BECs are maintained relatively constant throughout the ethanol vapor exposure paradigm, i.p. and i.g. ethanol administration result in a comparatively faster increase in BEC after which it declines over a period of hours as ethanol is metabolized. Similar effects can be achieved during oral consumption of ethanol as experienced drinkers frequently binge drink large volumes of ethanol at the onset of a drinking session. This rapid spike in BEC compared to the slower ramping up of BEC over several hours during vapor exposure may play a role in rendering animals more vulnerable to increased ethanol consumption during adulthood. Finally, it is possible that first pass metabolism through the stomach and liver is required for robust effects of adolescent ethanol exposure on increased propensity to drink in adulthood. It should be noted, however, that routes of administration requiring first pass metabolism have not always produced consistent results. For example, studies have also reported no change (Broadwater et al., 2013; Tambour, Brown, & Crabbe, 2008; Varlinskaya, Kim, & Spear, 2017) or decreased ethanol consumption (Gilpin, Karanikas, & Richardson, 2012; Siegmund, Vengeliene, Singer, & Spanagel, 2005) during adulthood following either voluntary oral consumption or experimenter administered (i.p. or i.g.) ethanol during adolescence.
A number of studies using the ethanol vapor method to expose adolescents to ethanol have also reported an increase in ethanol intake during adulthood. Gass and colleagues (Gass et al., 2014) observed an increase in operant responding for ethanol in adults following AIE vapor exposure. However, this increase in responding was not accompanied by a significant increase in the BEC. Others have found that rats exposed to ethanol vapor during late adolescence through adulthood following 2BC drinking during early adolescence exhibited a small but significant increase in responding for ethanol relative to controls (Criado & Ehlers, 2013). A more recent study by this group (Amodeo et al., 2018) reported similar findings in adult rats that were allowed to drink between cycles of ethanol vapor exposure during adolescence. Thus, more prolonged ethanol exposure during adolescence and early adulthood may be required to observe lasting effects on ethanol intake when using the vapor exposure method. Alternatively, a combination of oral ethanol self-administration and non-contingent vapor exposure may be needed to elicit robust increases in adult ethanol consumption compared to adolescent ethanol vapor exposure alone.
Symptoms of depression, including reduced sensitivity to natural rewards, are frequently observed following chronic alcohol exposure (Heilig, Egli, Crabbe, & Becker, 2010). With this in mind, the sucrose preference test, a widely accepted model of anhedonia (Scheggi, De Montis, & Gambarana, 2018) was used to determine whether binge-like AIE vapor exposure altered reward sensitivity. We observed that both AIR and AIE exposed rats exhibited a similarly strong preference for sucrose over water. These observations are in contrast to previous work by Gilpin et al (2012) showing that involuntary, but not voluntary, ethanol exposure during adolescence significantly reduced preference for a solution sweetened with glucose and saccharin. Of note, however, rats in this study were exposed to the same sweetened solution during adolescence immediately preceding i.p. injection of a bolus dose of ethanol potentially facilitating a conditioned taste aversion and driving reduced preference during adulthood. On the other hand, our data are consistent with previous work reporting no effect of experimenter administered ethanol during adolescence on sucrose preference (Ribeiro-Carvalho et al., 2011), motivation to respond for sucrose (Alaux-Cantin et al., 2013; Gass et al., 2014), and brain stimulation threshold (Boutros, Semenova, & Markou, 2014) during adulthood suggesting that AIE exposure does not affect reward sensitivity. However, using a different model of depression, Ehlers et al (2011) showed that adolescent alcohol exposure increased time spent immobile during the forced swim test. Taken together, these data suggest that while AIE exposure may not have lasting effects on reward sensitivity, it may facilitate other depression-like symptoms including inadequate coping or maladaptive responding to stressful circumstances (Commons, Cholanians, Babb, & Ehlinger, 2017).
In conclusion, the current study showed that binge-like AIE vapor exposure did not facilitate increased ethanol consumption or aversion-resistant ethanol drinking in adulthood. While adolescent exposure to ethanol has been shown to result in a number of lasting neurobiological and behavioral changes in adulthood, it does not appear to facilitate compulsive drinking. An important question moving forward is whether methodological differences in adolescent alcohol exposure, which engender different drinking profiles in adulthood, also produce differences in the development of an aversion-resistant phenotype.
Highlights.
Long-Evans rats exhibited quinine-resistant ethanol intake after seven weeks of 2BC
Adolescent intermittent ethanol (AIE) exposure did not alter ethanol intake in adulthood
AIE exposure did not facilitate the development of aversion-resistant drinking
AIE exposure did not alter motivation to respond for ethanol in adulthood
Acknowledgments
This work was supported by funding from the National Institutes on Alcohol Abuse and Alcoholism grants AA019967 (LJC), AA022701 (LJC), and AA022836 (EJG). The authors would like to thank Alyson Selchick and Amanda Nilsen for technical assistance with performing some of the procedures.
Footnotes
Declarations of interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alaux-Cantin S, Warnault V, Legastelois R, Botia B, Pierrefiche O, Vilpoux C, & Naassila M (2013). Alcohol intoxications during adolescence increase motivation for alcohol in adult rats and induce neuroadaptations in the nucleus accumbens. Neuropharmacology, 67, 521–531. 10.1016/j.neuropharm.2012.12.007 [DOI] [PubMed] [Google Scholar]
- Amodeo LR, Kneiber D, Wills DN, & Ehlers CL (2017). Alcohol drinking during adolescence increases consumptive responses to alcohol in adulthood in Wistar rats Alcohol (Fayetteville, N.Y.), 59, 43–51. 10.1016/j.alcohol.2016.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amodeo LR, Wills DN, Sanchez-Alavez M, Nguyen W, Conti B, & Ehlers CL (2018). Intermittent voluntary ethanol consumption combined with ethanol vapor exposure during adolescence increases drinking and alters other behaviors in adulthood in female and male rats. Alcohol. 10.1016/j.alcohol.2018.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker JM, Bryant KG, Osborne JI, & Chandler LJ (2017). Age and Sex Interact to Mediate the Effects of Intermittent, High-Dose Ethanol Exposure on Behavioral Flexibility. Frontiers in Pharmacology, 8, 450 10.3389/fphar.2017.00450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutros N, Semenova S, & Markou A (2014). Adolescent intermittent ethanol exposure diminishes anhedonia during ethanol withdrawal in adulthood. European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology, 24(6), 856–864. 10.1016/j.euroneuro.2014.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers MS, Hopf FW, Chou JK, Guillory AM, Chang S-J, Janak PH, … Diamond I (2008). Nucleus accumbens AGS3 expression drives ethanol seeking through G betagamma. Proceedings of the National Academy of Sciences of the United States of America, 105(34), 12533–12538. 10.1073/pnas.0706999105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadwater M, Varlinskaya EI, & Spear LP (2013). Effects of Voluntary Access to Sweetened Ethanol During Adolescence on Intake in Adulthood. Alcoholism: Clinical and Experimental Research, 37(6), 1048–1055. 10.1111/acer.12049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnicella S, Amamoto R, & Ron D (2009). Excessive alcohol consumption is blocked by glial cell line–derived neurotrophic factor. Alcohol, 43(1), 35–43. 10.1016/j.alcohol.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman LG Jr, He J, Lee J, Styner M, & Crews FT (2011). Adolescent Binge Drinking Alters Adult Brain Neurotransmitter Gene Expression, Behavior, Brain Regional Volumes, and Neurochemistry in Mice: ADULT BRAIN FOLLOWING ADOLESCENT BINGE. Alcoholism: Clinical and Experimental Research, 35(4), 671–688. 10.1111/j.1530-0277.2010.01385.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commons KG, Cholanians AB, Babb JA, & Ehlinger DG (2017). The Rodent Forced Swim Test Measures Stress-Coping Strategy, Not Depression-like Behavior. ACS Chemical Neuroscience, 8(5), 955–960. 10.1021/acschemneuro.7b00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criado JR, & Ehlers CL (2013). Effects of adolescent onset voluntary drinking followed by ethanol vapor exposure on subsequent ethanol consumption during protracted withdrawal in adult Wistar rats. Pharmacology Biochemistry and Behavior, 103(3), 622–630. 10.1016/j.pbb.2012.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Patricia Chou S, June Ruan W, & Grant BF (2008). Age at First Drink and the First Incidence of Adult-Onset DSM-IV Alcohol Use Disorders. Alcoholism: Clinical and Experimental Research, 32(12), 2149–2160.https://doi.Org/10.1111/j.1530-0277.2008.00806.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Criado JR, Wills DN, Liu W, & Crews FT (2011). Periadolescent ethanol exposure reduces adult forebrain ChAT+IR neurons: correlation with behavioral pathology. Neuroscience, 199, 333–345. 10.1016/j.neuroscience.2011.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Sakhardande A, & Blakemore S-J (2014). The effect of alcohol consumption on the adolescent brain: A systematic review of MRI and fMRI studies of alcohol-using youth. NeuroImage: Clinical, 5, 420–437. 10.1016/j.nicl.2014.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gass JT, Glen WBJ, McGonigal JT, Trantham-Davidson H, Lopez MF, Randall PK, … Chandler LJ (2014). Adolescent alcohol exposure reduces behavioral flexibility, promotes disinhibition, and increases resistance to extinction of ethanol self-administration in adulthood. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology, 39(11), 2570–2583. 10.1038/npp.2014.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin NW, Karanikas CA, & Richardson HN (2012). Adolescent binge drinking leads to changes in alcohol drinking, anxiety, and amygdalar corticotropin releasing factor cells in adulthood in male rats. PloS One, 7(2), e31466 10.1371/journal.pone.0031466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano C, Pena-Oliver Y, Goodlett CR, Cardinal RN, Robbins TW, Bullmore ET, … Everitt BJ (2018). Evidence for a Long-Lasting Compulsive Alcohol Seeking Phenotype in Rats. Neuropsychopharmacology, 43(4), 728–738. 10.1038/npp.2017.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson KL, Medina KL, Padula CB, Tapert SF, & Brown SA (2011). Impact of Adolescent Alcohol and Drug Use on Neuropsychological Functioning in Young Adulthood: 10-Year Outcomes. Journal of Child & Adolescent Substance Abuse, 20(2), 135–154. 10.1080/1067828X.2011.555272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, … Grant BF (2013). DSM-5 Criteria for Substance Use Disorders: Recommendations and Rationale. American Journal of Psychiatry, 170(8), 834–851. 10.1176/appi.ajp.2013.12060782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heilig M, Egli M, Crabbe JC, & Becker HC (2010). Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked? Addiction Biology, 15(2), 169–184. 10.1111/j.1369-1600.2009.00194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Heeren T, & Winter M (2006). Age at Drinking Onset and Alcohol DependenceAge at Onset, Duration, and Severity. ARCH PEDIATR ADOLESC MED, 160, 8. [DOI] [PubMed] [Google Scholar]
- Hopf F. Woodward, & Lesscher HMB (2014). Rodent models for compulsive alcohol intake. Alcohol, 48(3), 253–264. 10.1016/j.alcohol.2014.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopf F Woodward, Chang S-J, Sparta DR, Bowers MS, & Bonci A (2010). Motivation for Alcohol Becomes Resistant to Quinine Adulteration After 3 to 4 Months of Intermittent Alcohol Self-Administration: MOTIVATION FOR ALCOHOL BECOMES RESISTANT TO QUININE ADULTERATION. Alcoholism: Clinical and Experimental Research, 34(9), 1565–1573. 10.1111/j.1530-0277.2010.01241.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, & Schulenberg JE (2017).Monitoring the Future national survey results on drug use, 1975-2016: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research: The University of Michigan. [Google Scholar]
- Jury NJ, Pollack GA, Ward MJ, Bezek JL, Ng AJ, Pinard CR, … Holmes A (2017). Chronic Ethanol During Adolescence Impacts Corticolimbic Dendritic Spines and Behavior. Alcoholism: Clinical and Experimental Research, 41(7), 1298–1308. 10.1111/acer.13422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrough A, Kim S, Cole M, Brennan M, & George O (2017). Intermittent Access to Ethanol Drinking Facilitates the Transition to Excessive Drinking After Chronic Intermittent Ethanol Vapor Exposure. Alcoholism: Clinical and Experimental Research, 41(8), 1502–1509. 10.1111/acer.13434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Volkow ND (2010). Neurocircuitry of Addiction. Neuropsychopharmacology, 35(1), 217–238. 10.1038/npp.2009.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciana M, Collins PF, Muetzel RL, & Lim KO (2013). Effects of alcohol use initiation on brain structure in typically developing adolescents. The American Journal of Drug and Alcohol Abuse, 39(6), 345–355. 10.3109/00952990.2013.837057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado-Devincci AM, Alipour KK, Michael LA, & Kirstein CL (2010). Repeated binge ethanol administration during adolescence enhances voluntary sweetened ethanol intake in young adulthood in male and female rats. Pharmacology Biochemistry and Behavior, 96(4), 476–487. 10.1016/j.pbb.2010.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Forouzanfar MH, Daoud F, Mokdad AA, El Bcheraoui C, Moradi-Lakeh M, … Murray CJL (2016). Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 387(10036), 2383–2401. 10.1016/S0140-6736(16)00648-6 [DOI] [PubMed] [Google Scholar]
- Mook DG, & Blass EM (1968). Quinine-aversion thresholds and “finickiness” in hyperphagic rats. Journal of Comparative and Physiological Psychology, 65(2), 202–207. [DOI] [PubMed] [Google Scholar]
- Moore EM, Mariani JN, Linsenbardt DN, Melón LC, & Boehm SL (2010). Adolescent C57BL/6J (but not DBA/2J) mice consume greater amounts of limited-access ethanol compared to adults and display continued elevated ethanol intake into adulthood. Alcoholism, Clinical and Experimental Research, 34(4), 734–742. 10.1111/j.1530-0277.2009.01143.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council. (2011). Guide for the Care and Use of Laboratory Animals: Eighth Edition (8th ed.). Washington DC: National Academies Press. [Google Scholar]
- Nguyen-Louie TT, Tracas A, Squeglia LM, Matt GE, Eberson-Shumate S, & Tapert SF (2016). Learning and Memory in Adolescent Moderate, Binge, and Extreme-Binge Drinkers. Alcoholism: Clinical and Experimental Research, 40(9), 1895–1904. 10.1111/acer.13160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon K, & Crews FT (2002). Binge ethanol exposure decreases neurogenesis in adult rat hippocampus. Journal of Neurochemistry, 83(5), 1087–1093. [DOI] [PubMed] [Google Scholar]
- Pandey SC, Sakharkar AJ, Tang L, & Zhang H (2015). Potential role of adolescent alcohol exposure-induced amygdaloid histone modifications in anxiety and alcohol intake during adulthood. Neurobiology of Disease, 82, 607–619. https://doi.Org/10.1016/j.nbd.2015.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Schulenberg JE, Martz ME, Maggs JL, O’Malley PM, & Johnston LD (2013). Extreme Binge Drinking Among 12th-Grade Students in the United States: Prevalence and Predictors. JAMA Pediatrics, 167(11), 1019 10.1001/jamapediatrics.2013.2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro-Carvalho A, Lima CS, Nunes-Freitas AL, Filgueiras CC, Manhaes AC, & Abreu-Villaça Y (2011). Exposure to nicotine and ethanol in adolescent mice: effects on depressive-like behavior during exposure and withdrawal. Behavioural Brain Research, 221(1), 282–289. 10.1016/j.bbr.2011.03.014 [DOI] [PubMed] [Google Scholar]
- Scheggi S, De Montis MG, & Gambarana C (2018). Making Sense of Rodent Models of Anhedonia. The International Journal of Neuropsychopharmacology, 21(11), 1049–1065. 10.1093/ijnp/pyy083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seif T, Chang S-J, Simms JA, Gibb SL, Dadgar J, Chen BT, … Hopf FW (2013). Cortical activation of accumbens hyperpolarization-active NMDARs mediates aversion-resistant alcohol intake. Nature Neuroscience, 16(8), 1094–1100. 10.1038/nn.3445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seif T, Simms JA, Lei K, Wegner S, Bonci A, Messing RO, & Hopf FW (2015). D-Serine and D-Cycloserine Reduce Compulsive Alcohol Intake in Rats. Neuropsychopharmacology, 40(10), 2357–2367. 10.1038/npp.2015.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegmund S, Vengeliene V, Singer MV, & Spanagel R (2005). Influence of age at drinking onset on long-term ethanol self-administration with deprivation and stress phases. Alcoholism, Clinical and Experimental Research, 29(7), 1139–1145. [DOI] [PubMed] [Google Scholar]
- Simms JA, Steensland P, Medina B, Abernathy KE, Chandler LJ, Wise R, & Bartlett SE (2008). Intermittent access to 20% ethanol induces high ethanol consumption in Long-Evans and Wistar rats. Alcoholism, Clinical and Experimental Research, 32(10), 1816–1823. 10.1111/j.1530-0277.2008.00753.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slawecki CJ, & Betancourt M (2002). Effects of adolescent ethanol exposure on ethanol consumption in adult rats. Alcohol, 26(1), 23–30. 10.1016/S0741-8329(01)00192-6 [DOI] [PubMed] [Google Scholar]
- Spear LP (2018). Effects of adolescent alcohol consumption on the brain and behaviour. Nature Reviews Neuroscience, 19(4), 197–214. 10.1038/nrn.2018.10 [DOI] [PubMed] [Google Scholar]
- Spoelder M, Hesseling P, Baars AM, Lozeman-van ‘t Klooster JG, Rotte MD, Vanderschuren LJMJ, & Lesscher HMB (2015). Individual Variation in Alcohol Intake Predicts Reinforcement, Motivation, and Compulsive Alcohol Use in Rats. Alcoholism: Clinical and Experimental Research, 39(12), 2427–2437. 10.1111/acer.12891 [DOI] [PubMed] [Google Scholar]
- Tambour S, Brown LL, & Crabbe JC (2008). Gender and age at drinking onset affect voluntary alcohol consumption but neither the alcohol deprivation effect nor the response to stress in mice. Alcoholism, Clinical and Experimental Research, 32(12), 2100–2106. 10.1111/j.1530-0277.2008.00798.x [DOI] [PubMed] [Google Scholar]
- Tapert SF, Granholm E, Leedy NG, & Brown SA (2002). Substance use and withdrawal: Neuropsychological functioning over 8 years in youth. Journal of the International Neuropsychological Society, 8(07). 10.1017/S1355617702870011 [DOI] [PubMed] [Google Scholar]
- Tordoff MG, Alarcon LK, & Lawler MP (2008). Preferences of 14 rat strains for 17 taste compounds. Physiology & Behavior, 95(3), 308–332. 10.1016/j.physbeh.2008.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turyabahika-Thyen K, & Wolffgramm J (2006). Loss of Flexibility in Alcohol-Taking Rats: Promoting Factors. European Addiction Research, 12(4), 210–221. 10.1159/000094423 [DOI] [PubMed] [Google Scholar]
- Varlinskaya EI, Kim EU, & Spear LP (2017). Chronic intermittent ethanol exposure during adolescence: Effects on stress-induced social alterations and social drinking in adulthood. Brain Research, 1654(Pt B), 145–156. 10.1016/j.brainres.2016.03.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vendruscolo LF, Barbier E, Schlosburg JE, Misra KK, Whitfield TW, Logrip ML, … Koob GF (2012). Corticosteroid-Dependent Plasticity Mediates Compulsive Alcohol Drinking in Rats. Journal of Neuroscience, 32(22), 7563–7571. 10.1523/JNEUROSCI.0069-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetreno RP, Yaxley R, Paniagua B, Johnson GA, & Crews FT (2017). Adult rat cortical thickness changes across age and following adolescent intermittent ethanol treatment: AIE alters cortical thickness in the adult brain. Addiction Biology, 22(3), 712–723. 10.1111/adb.12364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, Jamieson-Drake DW, & Swartzwelder HS (2002). Prevalence and Correlates of Alcohol-Induced Blackouts Among College Students: Results of an E-Mail Survey. Journal of American College Health, 51(3), 117–131. 10.1080/07448480209596339 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2014). Global status report on alcohol and health 2014. Genova: World Health Organization; Retrieved from http://www.who.int/substance_abuse/publications/global_alcohol_report/en/ [Google Scholar]