Abstract
Trichophyton erinacei is an emerging cause of dermatophyte infections, which are frequently isolated from hedgehogs. Nail infections from T. erinacei are rarely reported. We describe the case of a 23-year-old Thai female who had a history of systemic lupus erythematosus with lupus nephritis type III and who developed widespread skin and nail infections caused by T. erinacei that were most likely transmitted from a hedgehog. Although the patient did not demonstrate a clinical improvement or mycological cure following systemic itraconazole and fluconazole treatment, she achieved clinical and mycological cures after terbinafine therapy. A drug susceptibility test should be performed in patients with T. erinacei infections to facilitate decision-making about antifungal therapy. Here, we are the first to report a case of proximal subungual onychomycosis from a T. erinacei infection.
Keywords: Fingernail onychomycosis, Tinea unguium, T. erinacei, Trichophyton erinacei
Introduction
Nail infections from Trichophyton erinacei are rarely reported. We present a case of widespread skin and nail infections caused by T. erinacei that was likely transmitted from a hedgehog in Thailand.
Case Report
A 23-year-old Thai female had a history of systemic lupus erythematosus with lupus nephritis type III for 15 years. She took chloroquine (250 mg/day), prednisolone (15 mg/day), cyclosporine A (25 mg/day), and dapsone (200 mg/day) for the lupus. She presented with a 1-month history of multiple, itchy, scaly erythematous patches on her face and left 4th fingernail dystrophy. She had a history of contact with a hedgehog for 2 weeks. A physical examination revealed multiple, well-defined, scaly erythematous patches with some pustules on her face, forearms, hands, and feet. Proximal subungual white patches were observed on the left 2nd and 3rd fingernails, and onychodystrophy was found on her left 4th fingernail (Fig. 1). A potassium hydroxide examination of her right cheek, left palm, and the left 2nd, 3rd, 4th, and 5th fingernails showed branching septate hyphae with arthrospores. All of the fungal cultures were positive for T. erinacei (Fig. 2). The patient was diagnosed with tinea faciei, tinea manuum, tinea corporis, and tinea unguium caused by T. erinacei. Despite 4 months of systemic itraconazole and 6 months of fluconazole treatment, she did not exhibit any clinical improvement or mycological cure. However, clinical and mycological cures were achieved following a 4-month course of terbinafine.
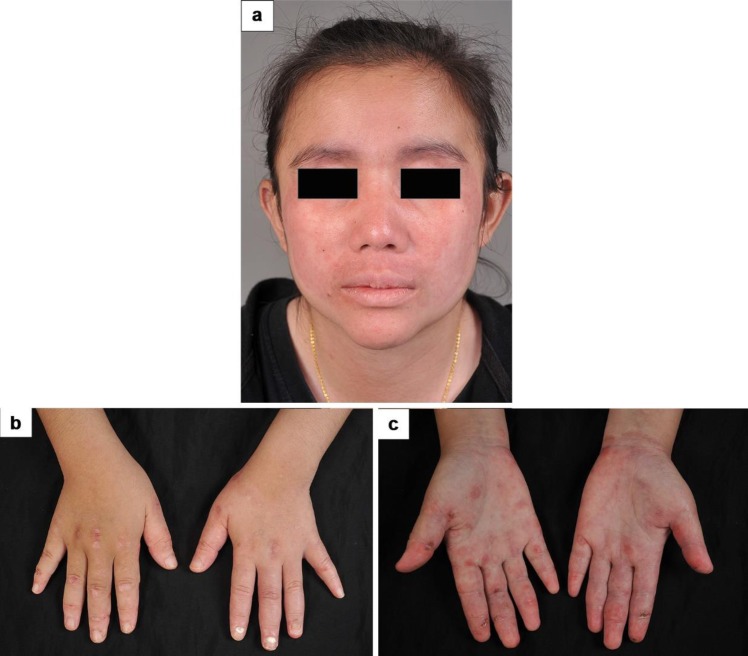
Fig. 1.
a Multiple, well-defined, scaly erythematous patches with some pustules on the face. b, c Multiple, well-defined, scaly erythematous patches and plaques on both hands; and proximal, subungual, white patches on the left 2nd and 3rd fingernails, with onychodystrophy on the left 4th fingernail.
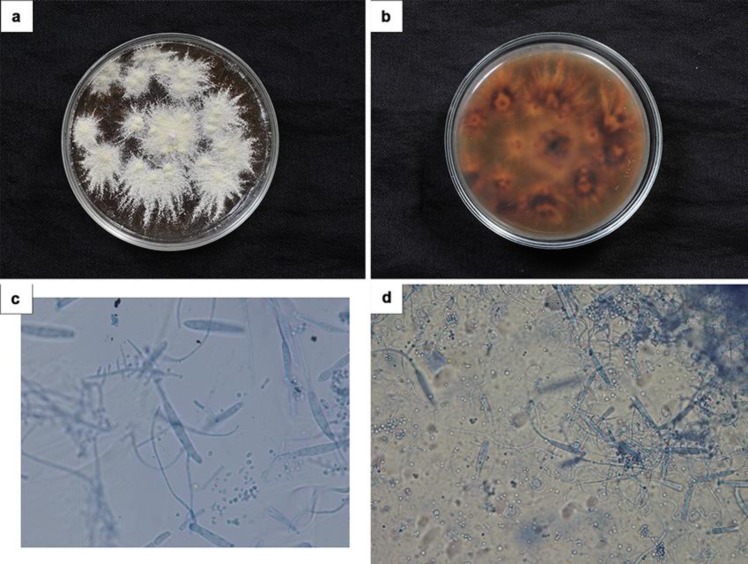
Fig. 2.
a, b Colonies are white, flat, powdery, and downy to fluffy, with a brilliant lemon-yellow reverse. c, d Numerous, large, clavate microconidia are borne on the sides of hyphae. The macroconidia are smooth-walled, two- to six-celled, clavate, variable in size, with terminal appendages.
Discussion
T. erinacei is a member of the T. mentagrophytes complex, a zoonotic dermatophyte which is a very rarely isolated human pathogen [1, 2, 3, 4, 5, 6]. It is the most common dermatophyte isolated in hedgehogs, with infection rates of 20–47% [7]. The most usual clinical manifestation is inflamed, pruritic eruptions in the form of pustules on an erythematous base, as seen in our patient [8]. This condition can easily be misdiagnosed as eczema, in which case receiving a corticosteroid may worsen the lesions. The lesions are typically located at the extremities, especially on the hands and wrists [9, 10], but skin infections at other locations (tinea corporis [9], tinea capitis [11], and tinea barbae [12]) have also been reported. However, tinea unguium caused by T. erinacei has rarely been reported; indeed, our literature review found only one report, involving 2 patients, from 1962. Both were diagnosed with fingernail onychomycosis from T. erinacei (unknown type) [13]. No involvement of the toenails has ever been described in the literature. Finger nail involvement appears to be an important source for the spread of an infection to other skin sites and the cause of multiple-site infections, as was the case with our patient's presentation. Here, we are the first to report a case of proximal subungual onychomycosis from a T. erinacei infection.
For the diagnosis, a potassium hydroxide examination from skin scrapings should be performed to detect hyphae. A fungal culture on Sabouraud dextrose agar typically reveals the growth of ivory-colored colonies with a gray, powdery surface; an elevated, cottony center; a brilliant yellow to lemon-colored reverse side; pear-shaped microconidia; and the rare production of spiral hyphae. Urease testing is usually negative, in contrast to T. mentagrophytes [14]. Sequencing of the internal transcribed spacer regions of the ribosomal fungal DNA provides explicit confirmation. However, as the sequencing procedure is costly, it is only performed at relatively few university hospitals, especially in resource-limited countries [1, 2, 3, 4].
A dramatic response with the use of systemic griseofulvin, itraconazole, or terbinafine, or with only topical antifungals (inadequate), or in a combination of those drugs, has been reported for T. erinacei infections [3]. There has only been one report, from 1962, of tinea unguium being caused by T. erinacei and being successfully treated with systemic griseofulvin [13]. In contrast, our patient failed to achieve clinical and mycologic cures with both fluconazole and itraconazole therapy. She was subsequently successfully treated, however, with a 4-month course of terbinafine. These results may be explained by the fungistatic effects of fluconazole and itraconazole on T. erinacei, whereas systemic terbinafine is a fungicidal agent. A previous study also reported that terbinafine was more effective in eliminating the fungus from infected hedgehogs than itraconazole [15]. The drug susceptibility test should be conducted on patients with T. erinacei infections to aid in the planning of an antifungal therapy regimen. If possible, the animals involved should also be treated to eliminate the source of the infections.
T. erinacei infection is an emerging disease. Previous studies have revealed an increasing prevalence of infections in household hedgehogs [5]. It was first described in New Zealand, but in recent years, the large majority of reports have been from Korea [8], Japan [9], and Taiwan [2] in Asia. One study reported the case of a Caucasian woman who had been exposed to an elephant in Thailand and developed a T. erinacei skin infection on the contact area [6]. However, our study reported the first case of T. erinacei skin and nail infections in Thailand that were most likely transmitted from a hedgehog. The prevalence and spread of T. erinacei infections in each country should be closely observed. Dermatologists must consider this zoophilic dermatophytosis if patients have a history of contact with exotic animals, especially hedgehogs.
Statement of Ethics
Informed consent has been obtained and the study has been done according to the Declaration of Helsinki.
Disclosure Statement
The authors have no conflict of interest to declare.
Funding Sources
This was an unfunded study.
Author Contributions
All authors are responsible for and significantly participated in writing the manuscript.
References
- 1.Choi E, Huang J, Chew KL, Jaffar H, Tan C. Pustular tinea manuum from Trichophyton erinacei infection. JAAD Case Rep. 2018 Jun;4((6)):518–20. doi: 10.1016/j.jdcr.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsieh CW, Sun PL, Wu YH. Trichophyton erinacei infection from a hedgehog: a case report from Taiwan. Mycopathologia. 2010 Dec;170((6)):417–21. doi: 10.1007/s11046-010-9333-2. [DOI] [PubMed] [Google Scholar]
- 3.Concha M, Nicklas C, Balcells E, Guzmán AM, Poggi H, León E, et al. The first case of tinea faciei caused by Trichophyton mentagrophytes var. erinacei isolated in Chile. Int J Dermatol. 2012 Mar;51((3)):283–5. doi: 10.1111/j.1365-4632.2011.04995.x. [DOI] [PubMed] [Google Scholar]
- 4.Kromer C, Nenoff P, Uhrlaß S, Apel A, Schön MP, Lippert U. Trichophyton erinacei Transmitted to a Pregnant Woman From Her Pet Hedgehogs. JAMA Dermatol. 2018 Aug;154((8)):967–8. doi: 10.1001/jamadermatol.2018.1124. [DOI] [PubMed] [Google Scholar]
- 5.Abarca ML, Castellá G, Martorell J, Cabañes FJ. Trichophyton erinacei in pet hedgehogs in Spain: occurrence and revision of its taxonomic status. Med Mycol. 2017 Feb;55((2)):164–72. doi: 10.1093/mmy/myw057. [DOI] [PubMed] [Google Scholar]
- 6.Borges-Costa J, Martins ML. Trichophyton erinacei skin infection after recreational exposure to an elephant in Southeast Asia. Pathog Glob Health. 2014 Jan;108((1)):58–9. doi: 10.1179/2047773213Y.0000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philpot CM, Bowen RG. Hazards from hedgehogs: two case reports with a survey of the epidemiology of hedgehog ringworm. Clin Exp Dermatol. 1992 May;17((3)):156–8. doi: 10.1111/j.1365-2230.1992.tb00193.x. [DOI] [PubMed] [Google Scholar]
- 8.Rhee DY, Kim MS, Chang SE, Lee MW, Choi JH, Moon KC, et al. A case of tinea manuum caused by Trichophyton mentagrophytes var. erinacei: the first isolation in Korea. Mycoses. 2009 May;52((3)):287–90. doi: 10.1111/j.1439-0507.2008.01556.x. [DOI] [PubMed] [Google Scholar]
- 9.Mochizuki T, Takeda K, Nakagawa M, Kawasaki M, Tanabe H, Ishizaki H. The first isolation in Japan of Trichophyton mentagrophytes var. erinacei causing tinea manuum. Int J Dermatol. 2005 Sep;44((9)):765–8. doi: 10.1111/j.1365-4632.2004.02180.x. [DOI] [PubMed] [Google Scholar]
- 10.Rosen T, Jablon J. Infectious threats from exotic pets: dermatological implications. Dermatol Clin. 2003 Apr;21((2)):229–36. doi: 10.1016/s0733-8635(02)00090-6. [DOI] [PubMed] [Google Scholar]
- 11.Jury CS, Lucke TW, Bilsland D. Trichophyton erinacei: an unusual cause of kerion. Br J Dermatol. 1999 Sep;141((3)):606–7. doi: 10.1046/j.1365-2133.1999.03092.x. [DOI] [PubMed] [Google Scholar]
- 12.Simpson JR. Tinea barbae caused by Trichophyton erinacei. Br J Dermatol. 1974 Jun;90((6)):697–8. doi: 10.1111/j.1365-2133.1974.tb06701.x. [DOI] [PubMed] [Google Scholar]
- 13.English MP, Evans CD, Hewit M, Warin RP. “Hed-gehog ringworm”. BMJ. 1962 Jan;1((5272)):149–51. doi: 10.1136/bmj.1.5272.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rush-Munro FM, Smith JM. Further observations on Trichophyton erinacei and T. proliferans. Sabouraudia. 1971 Mar;9((1)):61–4. [PubMed] [Google Scholar]
- 15.Bexton S, Nelson H. Comparison of two systemic antifungal agents, itraconazole and terbinafine, for the treatment of dermatophytosis in European hedgehogs (Erinaceus europaeus) Vet Dermatol. 2016 Dec;27((6)):500–e133. doi: 10.1111/vde.12378. [DOI] [PubMed] [Google Scholar]