Abstract
Objective
The AllplexTM Respiratory Panel 1 (ARP) is a new assay based on a real-time polymerase chain reaction (RT-PCR) for the detection of influenza A (Flu A), influenza B virus (Flu B), and respiratory syncytial virus (RSV), including subtyping by multiple detection temperature (MuDT) technology. We evaluated the performance of the Allplex Respiratory Panel compared to the SimplexaTM Flu A/B & RSV assay (SP) and other diagnostic tools.
Materials and Methods
A total of 372 samples were collected from patients at the Korea University Guro Hospital in Seoul, Korea. All samples were tested for influenza virus and RSV by ARP, SP, and an in-house RT-PCR.
Results
The sensitivity of ARP was 95.56, 100, and 95.24% for Flu A, Flu B, and RSV, respectively. The specificity of ARP was 100, 100, and 100% for Flu A, Flu B, and RSV, respectively. SP had sensitivities and specificities of 98.89 and 100% for Flu A, 100 and 100% for Flu B, and 100 and 100% for RSV.
Conclusion
The Allplex panel showed high sensitivity, specificity, positive predictive, and negative predictive values for the detection of Flu A, Flu B, and RSV. This assay is fast and easy to perform because it takes only about 150 min and there is no need for post-PCR electrophoresis. The ARP can be used as a reliable and convenient assay in clinical laboratories.
Keywords: AllplexTMRespiratory Panel 1, Respiratory virus, Real-time polymerase chain reaction, Influenza, Respiratory syncytial virus
Significance of the Study
The performance of the AllplexTM Respiratory Panel was evaluated and compared to that of the SimplexaTM Flu A/B & RSV assay and other diagnostic tools for the detection of respiratory viruses. This panel can be used as a reliable and convenient assay for the detection of respiratory viruses because of its high sensitivity and specificity.
Introduction
Influenza virus is a major cause of morbidity and mortality in old and young patients and especially in immunocompromised individuals [1]. Influenza occurs globally with an estimated annual attack rate of 5–10% in adults and 20–30% in children [2]. In 2009, pandemic influenza A (H1N1) caused 29,669 cases of infection, including 145 deaths, in 74 countries [3]. Respiratory syncytial virus (RSV) is the most common cause of bronchiolitis and pneumonia in infants and young children and it is the leading cause of respiratory infections that require hospitalization in infants [4]. Unfortunately, prior exposure to RSV does not protect against subsequent reinfection [5]. RSV reinfection also causes substantial morbidity in the elderly and in high-risk patients [6]. Although influenza virus and RSV are of considerable clinical importance, most research has focused on bacteria as the principal agent of community-acquired pneumonia in the past [7]. Influenza virus and RSV are important pathogens among children suffering from acute lower respiratory infections [8]. In particular, the pandemic H1N1 influenza A infection has steered public concern towards the causative virus in patients with respiratory symptoms, such as cough, rhinorrhea, sore throat, and fever.
To date, numerous diagnostic tools, such as viral culture, direct immunofluorescence assay, a rapid antigen test, and real-time polymerase chain reaction (RT-PCR) have been developed for the detection of respiratory viruses [9]. Viral culture has been the primary technique used to detect respiratory viruses, but it is time consuming and labor intensive [10]. Many rapid antigen tests still show an inferior sensitivity compared to RT-PCR, though they have several advantages, such as their rapid result times, ease of use and interpretation, and lower costs [11]. Various commercial multiplex RT-PCR assays have enabled clinical laboratories to detect the causative virus in patients with respiratory symptoms [1]. The SimplexaTM Flu A/B & RSV assay (SP) (Focus Diagnostics, Cypress, CA, USA) is an RT-PCR-based assay for in vitro detection of Flu A, Flu B, and RSV, but it cannot discriminate their subtyping.
The worldwide pandemic of influenza virus began with the Spanish influenza (type A/HIN1) in 1918, followed by the Asian flu (type A/H2N2) in 1957, the Hong Kong flu (type A/H3N2) in 1968, and the swine flu epidemic (type A/H1N1) in 2009 [12]. The subtyping of influenza viruses is important for predicting clinical characteristics to manage patients, and for estimating the prevalence rate epidemiologically. Therefore, it is important not only to detect whether an infection is caused by influenza virus but also to detect the subtype of influenza virus.
AllplexTM Respiratory Panel 1 (ARP) (Seegene, Seoul, Korea) is a new RT-PCR-based assay for detection of influenza virus and RSV infection including their subtyping. ARP employs multiple detection temperature (MuDT) technology, which provides multithreshold cycle (Ct) values in a single fluorescence channel without requiring melt curve analysis as in RT-PCR instruments [13]. In ARP, 7 analytes can be detected in a single sample, including influenza A virus (Flu A), influenza B virus (Flu B), influenza A virus subtype H1 (Flu A-H1), influenza A virus subtype H3 (Flu A-H3), influenza A virus subtype H1N1 (Flu A-H1pdm09), RSV A, and RSV B. Nasopharyngeal swabs, nasopharyngeal aspirates, and bronchoalveolar lavage (BAL) can be used as specimens for ARP.
We evaluated the performance of the Allplex Respiratory Panel compared to SP and other diagnostic tools for the detection of respiratory viruses.
Materials and Methods
Subjects
This study was approved by the Institutional Research Ethics Board of the Korea University Guro Hospital (approval No. MD16056). Three hundred seventy-two samples were collected from patients at the Korea University Guro Hospital in Seoul, Korea, between January 2015 and February 2017. A total of 312 samples were collected from patients with respiratory symptoms, such as high fever, cough, and rhinorrhea; 60 samples were collected from healthy individuals as negative controls; 199, 153, 15, and 5 samples were from nasopharyngeal swabs, nasopharyngeal aspirates, BAL, and sputum, respectively.
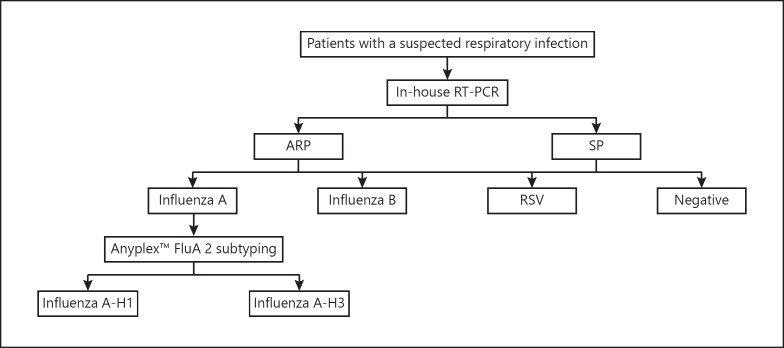
Each sample was transported in a vial containing 3 mL of viral transport medium and immediately used for RT-PCR-based testing of influenza virus and RSV. The remaining specimens were then cryopreserved at −80°C until influenza rapid antigen testing was conducted. All specimens were subjected to a single freeze-thaw cycle. All samples were tested for influenza virus and RSV by ARP, SP, and an in-house RT-PCR. Influenza A samples were additionally tested for their subtyping using the AnyplexTM FluA 2 Real-Time Subtyping Kit (Seegene) (Fig. 1). ARP, SP, and Anyplex FluA 2 Real-Time Subtyping tests were carried out according to the manufacturer's instructions.
Fig. 1.
Flow chart of tests for the detection of influenza virus and RSV.
Nucleic Acid Extraction and Internal Control
Nucleic acid was extracted from patient specimens and assay controls using the NucliSENS® easyMAGTM extraction method (Biomerieux, Durham, NC, USA).
Internal control was added to each specimen to monitor the entire process from nucleic acid extraction to PCR, according to the manufacturer's instructions.
Allplex Respiratory Panel 1
The ARP assay can analyze samples to detect Flu A, Flu B, Flu A-H1, Flu A-H3, Flu A-H1pdm09, RSV A, and RSV B with each Ct value, and it was performed on a CFX96TM (Bio-Rad, Hercules, CA, USA) according to the manufacturer's instructions.
The test results were interpreted automatically, and the analyzed data were presented using Seegene Viewer. If the Ct value was below 42 cycles, the sample was considered positive for presence of the pathogen. A negative specimen was defined by the absence of amplification for any pathogen with the presence of amplification of the internal control.
Simplexa Flu A/B & RSV Assay
The SP assay can analyze samples to detect Flu A, Flu B, and RSV. SP for in vitro diagnostic use was approved by the US Food and Drug Administration (FDA) and Conformité Européenne (CE). This assay was performed on a 3M Integrated CyclerTM (Focus Diagnostics, CA, USA) according to the manufacturer's instructions.
A well-defined curve was considered a positive test result when it crossed the threshold cycle within 40 cycles of Flu A, Flu B, and RSV. In addition, multiple detections of 3 viruses were possible with this assay.
Anyplex FluA 2 Real-Time Subtyping
In parallel with the ARP assay, all the influenza A specimens were tested using an Anyplex FluA 2 Real-Time Subtyping Kit (Seegene), which is a commercial RT-, mPCR assay for the detection of influenza A and influenza B. This assay was performed on a CFX96TM according to the manufacturer's instructions. Viral RNA was extracted using the NucliSENS easyMAG apparatus, and the Anyplex FluA 2 Real-Time Subtyping Kit was used to detect influenza A and influenza B, according to the manufacturer's instructions. Results were visualized using Seegene Viewer.
In-House Real-Time PCR for the Detection of Respiratory Viruses
For the in-house method, viral RNA was extracted with a QIAamp® Viral RNA Mini Kit (Qiagen, Hilden, Germany) from 140 μL of the respiratory specimen by the in-house PCR protocol. A single-step real-time RT-PCR was performed as described previously with minor modifications [14]. The real-time PCR primers and probes are listed in Table 1. TaqMan amplification and detection were performed on a real-time thermocycler CFX96 (Bio-Rad). Thermocycling conditions were as follows: reverse transcription at 50°C for 20 min and initial denaturation at 95°C for 10 min, followed by 45 cycles at 95°C for 15 s and at 60°C for 60 s. Each result was considered positive if the threshold cycle value (Ct) was less than 40.0. For quality control of in-house PCR, standard curves were produced with these 6 standard points of 10-fold dilution series of the virus culture stock samples (influenza A H1N1pdm/ H3N2 ATCC VR-544, influenza B ATCC VR-10-1, and RSV KBPV-VR-41, 42).
Table 1.
In-house RT-PCR primer and probe sequences
| Virus target | Primer or probe | Sequence |
|---|---|---|
| Influenza A virus | FluA-F FluA-R FluA-probe |
AGAT GAGTCTTCTAACC GAGGTCG TGACA GRAT YGGTCTT GTCTTTA GCCA YTCCA [5FAM]TCA GGCCCCCTCAAA GCC GAG[3BHQ1] |
| Influenza B virus | FluB-F FluB-R FluB-probe |
TACACA GCAAAAA GACCC TCCACTCCCTTTCTCCCC [5HEX]ACACCCCCA GACCA GAT GA[3BHQ1] |
| Respiratory syncytial virus A | RSA-1 RSA-2 RSA probe |
AGATCAACTTCTGTCATCCAGCAA ATTGATACTCCTAATTATGATGTGC CACCATCCAACGGAGCACAGGAGAT |
| Respiratory syncytial virus B | RSB-1 RSB-2 RSB probe |
AAGATGCAAATCATAAATTCACAGGA CACTATAAAGATACTTAAAGATGCTGGATATCA AGGTATGTTATATGCTATGTCCAGGTTAGGAAGGGAA |
Data Analysis
Results of ARP and SP were analyzed and compared. Statistical analysis was performed with SPSS Statistics version 18 software (IBM Corporation, New York, NY, USA). The McNemar test for 2-by-2 contingency table analysis was performed between ARP and SP. Ct values of Flu A and Flu A subtyping, defined as an analysis of Flu A subtypes such as Flu A-H1, Flu A-H3, and Flu A-H1pdm09, were analyzed using a paired t test and the Pearson correlation coefficient. p < 0.05 was considered statistically significant.
Results
A total of 372 respiratory specimens were included in this study; 90 samples were positive for Flu A (including 24 Flu A-H1 and 66 Flu A-H3 samples), 67 samples were positive for Flu B, and 21 samples were positive for RSV. A total of 194 samples were negative for both influenza virus and RSV. Among the 372 samples, 173 (46.51%) were positive for 1 or more of the viruses tested by ARP while 177 (47.58%) samples were positive in the SP assay. Only 1 sample was positive for both Flu A and RSV. A total of 77 samples were taken from patients in the convalescent stage: 71 samples were negative and 4, 1, and 1 samples were positive for Flu A, Flu B, and RSV, respectively. In addition, 60 samples were taken from healthy individuals, and the results were all negative. There was no significant difference in the positive rate of the samples between 199 nasopharyngeal swabs, 153 nasopharyngeal aspirates, 15 BAL, and 5 sputum samples. All runs of ARP and SP were valid according to the specifications for internal control. The time required to perform the ARP assay was about 150 min, whereas the total assay time of SP was about 120 min.
A comparative analysis of viral detection by ARP and SP is shown in Table 2. In the detection of Flu A, the sensitivity and specificity of ARP were 95.56 and 100.00%, respectively, whereas these parameters in the case of Flu B were 100 and 100%, respectively. Similarly, the sensitivity and specificity of ARP in detecting RSV were 95.24 and 100.00%, respectively. The concordance rate between ARP and SP for detecting Flu A, Flu B, and RSV was 99.19, 100.00, and 99.71%, respectively. In the detection of Flu A, Flu B, and RSV, McNemar tests did not show any significant difference between ARP and SP (p = 0.25, 1.00, and 1.00).
Table 2.
Comparison of ARP and SP
| Virus | ARP |
SP |
Concordance,κ value % | McNemar'sp value | |||
|---|---|---|---|---|---|---|---|
| positive | negative | positive | negative | ||||
| Influenza A | 86 | 286 | 9 | 283 | 99.19 | 0.99 | 0.25 |
| Influenza B | 67 | 278 | 67 | 78 | 100.00 | 1.00 | 1.00 |
| RSV | 20 | 325 | 21 | 324 | 99.71 | 0.99 | 1.00 |
The influenza subtype of 90 samples, which were positive for influenza A, was tested using both the ARP and the Anyplex FluA 2 Real-Time Subtyping assay. A total of 24 samples were positive for Flu A-H1pdm09 by ARP and Anyplex FluA 2 Real-Time Subtyping assay and 66 samples were positive for Flu A-H3 by ARP and Anyplex FluA 2 Real-Time Subtyping assay. There were no discrepant results between ARP and Anyplex FluA 2 Real-Time Subtyping assay.
We observed discrepancies in 4 cases of viral detection by ARP and SP (Table 3). Three cases were positive for Flu A-H3 and negative for Flu A on investigation by ARP; however, they were positive for Flu A when tested by SP. Only a single case was negative for all of the respiratory viruses when tested by ARP, but RSV was found to be present in the sample when tested by SP.
Table 3.
Discrepancy between ARP and SP results
| Case No.ARP | Ct | ARP subtyping | Ct | SP | Ct | |
|---|---|---|---|---|---|---|
| 1 | negative | none | influenza A-H3 | 37.09 | influenza A | 35.74 |
| 2 | negative | none | influenza A-H3 | 34.32 | influenza A | 34.39 |
| 3 | negative | none | influenza A-H3 | 39.56 | influenza A | 33.66 |
| 4 | negative | none | negative | none | RSV | 33.07 |
All positive samples were analyzed for Ct values of ARP and SP (Table 4). The mean Ct values (±SD) of ARP and SP were 26.17 ± 3.93 and 24.98 ± 4.25, respectively, in the detection of Flu A. In the case of Flu B, the mean Ct values (±SD) of ARP and SP were 26.45 ± 3.77 and 31.94 ± 3.46, respectively. The Ct values determined by ARP and SP were 21.87 ± 5.90 and 24.16 ± 5.26, respectively, for RSV detection.
Table 4.
Comparison of Ct between ARP and SP
| Virus | ARP |
SP |
||
|---|---|---|---|---|
| mean | SD | mean | SD | |
| Influenza A | 26.17 | 3.93 | 24.98 | 4.25 |
| Influenza B | 26.45 | 3.77 | 31.94 | 3.46 |
| RSV | 21.87 | 5.90 | 24.16 | 5.26 |
Among 90 positive samples of Flu A, 86 positive samples were statistically analyzed for Ct values of Flu A and Flu A subtyping by correlation coefficients and paired t tests (Table 5). The other 4 positive samples were excluded because of discrepant results between Flu A and Flu A subtyping. The mean Ct values (±SD) of Flu A and Flu A subtyping were 26.17 ± 3.93 and 23.91 ± 3.87 for Flu A-positive samples, respectively. Ct values of Flu A were significantly different from those of Flu A subtyping as evaluated by a paired t test (p = 0.000). Between Flu A and Flu A subtyping, the correlation coefficient for the Ct values was 0.934 by Pearson's correlation analysis.
Table 5.
Comparison of Ct between influenza A virus and influenza A subtyping by ARP
| Influenza A |
Influenza A subtypinga |
Pairedt test |
Correlation coefficientb |
|||||
|---|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | t | p value | r | p value | |
| 26.17 | 3.93 | 23.91 | 3.87 | 15.31 | 0.000 | 0.934 | 0.000 | |
All Ct values used in this analysis were results of ARP test in samples of influenza A virus with all subtypes.
Tested using the ARP.
Pearson's correlation coefficient.
Discussion
Early diagnosis and treatment of the flu and RSV are very important because of the strong and rapid infectivity of the viruses. Mean serial intervals of Flu A-H3, Flu A-H1pdm09, and RSV and the duration between the onset of symptoms in a primary case and in its secondary cases are significantly shorter than in other contagious diseases, such as measles, varicella, smallpox, mumps, rubella, and pertussis [15]. Rapid diagnosis of a respiratory viral infection could reduce the rate of antibiotics use and unnecessary tests [16].
Because of the importance of early diagnosis for flu and RSV infections, numerous RT-PCR-based assays have been developed for the detection of respiratory pathogens. However, conventional RT-PCR assays have limitations, as they provide only a single Ct value in a single fluorescence channel. To overcome this limitation, conventional multiplex PCR assays were developed that have multiple fluorescence channels to acquire multiple Ct values for a faster analysis. FTD Respiratory pathogens 21 (Fast-track Diagnostics, Esch-sur-Alzette, Luxembourg) consists of 5 separate primer/probe mixes covering 16 human respiratory viruses, and each mix has 4 fluorescence channels [17]. The TaqMan array card (Life Technologies, Carlsbad, CA, USA) is comprised of 21 uniplex PCR assays that are conducted simultaneously in duplicate on a single 384-well microfluidic card with 8 ports [18]. Another alternative to overcome the limitations of conventional PCR assays is to use RT-PCR in combination with other technologies. The PLEX-ID Flu DetectionTM Kit (Abbott Molecular, Des Plaines, IL, USA) detects influenza viruses using the PCR-coupled electrospray ionization mass spectrometry technology [19]. The Verigene Respiratory Virus Plus test (Nanosphere, Northbrook, IL, USA) is an automated, multiplex nucleic acid test based on nanoparticle technology that does not require preextraction of specimens [20].
On a single fluorescence channel, SP provides a single Ct value, while ARP provides multiple Ct values via MuDT technology. This technology shows that the intensity of the fluorescence signals of 2 discrete Tm targets is different at certain temperatures called detection temperatures. Consequently, a high-Tm target can be detected regardless of the presence of a low-Tm target. MuDT technology enables identification of the low-Tm target by utilizing a change in the fluorescence signals between 2 different detection temperatures [13]. MuDT also facilitates a shorter turnaround time because melt curve analysis after amplification is not necessary. It allows quantification of multiple targets in a single channel. In this context, ARP provides multi-Ct values of 3 respiratory viruses with their subtyping by MuDT.
The ARP assay has 2 additional panels that allow the detection of 16 different types of respiratory viruses besides the influenza virus subtype and RSV [21, 22]. The ARP assay is highly useful as a routine examination in the hospital setting because the test time is the same even when other respiratory panels are added. In a recent study, ARP showed an overall sensitivity of 93.7% and a specificity of 100% for the detection of Flu A, Flu B, and RSV [23]. The ARP assay takes about 150 min, does not require electrophoresis after PCR, and can reduce the hands-on time by using automatic nucleic acid extraction equipment, such as MICROLAB STARlet IVD (Hamilton, Reno, NV, USA).
In this study, ARP demonstrated high sensitivity, specificity, positive predictive, and negative predictive values in patients with respiratory symptoms for causative viral detection. While SP was unable to identify the Flu A subtype, ARP could identify the Flu A subtype. The accuracy of the ARP assay for Flu A subtyping was 100%, compared to the Anyplex FluA 2 Real-Time Subtyping assay. In addition, the concordance rate between ARP and SP was very high. Ct values of positive samples where virus was detected were positively correlated between ARP and SP.
For the detection of Flu A, ARP showed no significant differences in sensitivity and specificity. Ct values of Flu A subtyping had a very strong correlation with Ct values of Flu A (r = 0.934). The mean Ct values for Flu A subtyping were significantly lower than those for Flu A. Flu A subtyping is more sensitive than detection of Flu A because of the strong correlation and significantly lower Ct values. For the detection of Flu B, ARP showed perfect agreement with SP assays. For detection of RSV, ARP showed no significant differences in sensitivity or specificity compared to SP.
Discrepancies between ARP and SP were observed in the detection of 3 cases of Flu A and in 1 case of RSV. In the detection of Flu A, 3 discrepant cases were detected only in Flu A subtyping but not in Flu A by ARP. We believe that Flu A subtyping is more sensitive than Flu A detection as the results of these samples would be interpreted as Flu A only by detection in Flu A subtyping. We suggest that if only the Flu A subtype is detected the sample indicates a very low viral load of influenza virus. However, if only Flu A is detected (and not the Flu A subtype), the subtype would be reported as unidentifiable and sequencing is recommended. For RSV detection, only 1 discrepant case was observed, having been detected by SP but not by ARP. In-house RT-PCR was used to verify the 4 discrepant results between ARP and SP, and it was confirmed that ARP missed 4 positive samples. This can be explained by a possible lack of sensitivity using the ARP test, because ARP is a multiplexing assay for the detection of Flu A, Flu B, and RSV with their subtyping in a single tube. However, confirmative tests such as culture or sequencing were not performed for discrepant results between ARP and SP.
Among the 372 samples collected from the patients suspected of having respiratory infections, 24 samples were positive for Flu A-H1pdm09. We suggest the possibility of an epidemic Flu A-H1pdm09 because all of the Flu A-H1 positive samples were positive for Flu A-H1pdm09. This possibility may be verified in the future by epidemiologic surveys in multicenter studies.
Further studies are needed to compare the limits of detection by ARP, SP, and in-house PCR. However, confirmative tests such as culture or sequencing were not performed for discrepant results between ARP and SP. In addition, the relatively small numbers of positive RSV samples were a limitation in this study.
Conclusion
In this study, the Allplex Respiratory Panel Test showed high sensitivity, specificity, positive predictive, and negative predictive values for the detection of Flu A, Flu B, and RSV with multi-Ct values. The concordance rate between ARP and SP was also very high. ARP allows identification of the viral subtype in a single tube, unlike other RT-PCR methods, such as SP. The ARP assay is fast and easy to perform because it takes only about 150 min and there is no need for post-PCR electrophoresis. ARP can be used as a reliable and convenient assay in clinical laboratories.
Disclosure Statement
The authors declare that they have no competing interests.
Acknowledgement
This study was supported by the National Research Foundation of Korea (NRF) (grant NRF-2016R1A5A1010148).
References
- 1.Vallières E, Renaud C. Clinical and economical impact of multiplex respiratory virus assays. Diagn Microbiol Infect Dis. 2013 Jul;76((3)):255–61. doi: 10.1016/j.diagmicrobio.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee AJ, Das SR, Wang W, Fitzgerald T, Pickett BE, Aevermann BD, et al. Diversifying selection analysis predicts antigenic evolution of 2009 pandemic H1N1 influenza A virus in humans. J Virol. 2015 May;89((10)):5427–40. doi: 10.1128/JVI.03636-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Influenza A (H1N1)—update 48. http://www.who.int/csr/don/2009_06_12/en/index.html (accessed 20 July 2017) [Google Scholar]
- 4.Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010 May;375((9725)):1545–55. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henderson FW, Collier AM, Clyde WA, Jr, Denny FW. Respiratory-syncytial-virus infections, reinfections and immunity. A prospective, longitudinal study in young children. N Engl J Med. 1979 Mar;300((10)):530–4. doi: 10.1056/NEJM197903083001004. [DOI] [PubMed] [Google Scholar]
- 6.Prendergast C, Papenburg J. Rapid antigen-based testing for respiratory syncytial virus: moving diagnostics from bench to bedside? Future Microbiol. 2013 Apr;8((4)):435–44. doi: 10.2217/fmb.13.9. [DOI] [PubMed] [Google Scholar]
- 7.McIntosh K. Community-acquired pneumonia in children. N Engl J Med. 2002 Feb;346((6)):429–37. doi: 10.1056/NEJMra011994. [DOI] [PubMed] [Google Scholar]
- 8.Berkley JA, Munywoki P, Ngama M, Kazungu S, Abwao J, Bett A, et al. Viral etiology of severe pneumonia among Kenyan infants and children. JAMA. 2010 May;303((20)):2051–7. doi: 10.1001/jama.2010.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck ET, Henrickson KJ. Molecular diagnosis of respiratory viruses. Future Microbiol. 2010 Jun;5((6)):901–16. doi: 10.2217/fmb.10.48. [DOI] [PubMed] [Google Scholar]
- 10.Kim DK, Poudel B. Tools to detect influenza virus. Yonsei Med J. 2013 May;54((3)):560–6. doi: 10.3349/ymj.2013.54.3.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miernyk K, Bulkow L, DeByle C, Chikoyak L, Hummel KB, Hennessy T, et al. Performance of a rapid antigen test (Binax NOW® RSV) for diagnosis of respiratory syncytial virus compared with real-time polymerase chain reaction in a pediatric population. J Clin Virol. 2011 Mar;50((3)):240–3. doi: 10.1016/j.jcv.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Vallières E, Renaud C. Clinical and economical impact of multiplex respiratory virus assays. Diagn Microbiol Infect Dis. 2013 Jul;76((3)):255–61. doi: 10.1016/j.diagmicrobio.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwon SH, Lee S, Jang J, Seo Y, Lim HY. A point-of-care diagnostic system to influenza viruses using chip-based ultra-fast PCR. J Med Virol. 2018 Jun;90((6)):1019–26. doi: 10.1002/jmv.25046. [DOI] [PubMed] [Google Scholar]
- 14.Lee YJ, Kim D, Lee K, Chun JY. Single-channel multiplexing without melting curve analysis in real-time PCR. Sci Rep. 2014 Dec;4((1)):7439. doi: 10.1038/srep07439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Elden LJ, Nijhuis M, Schipper P, Schuurman R, van Loon AM. Simultaneous detection of influenza viruses A and B using real-time quantitative PCR. J Clin Microbiol. 2001 Jan;39((1)):196–200. doi: 10.1128/JCM.39.1.196-200.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vink MA, Bootsma MC, Wallinga J. Serial intervals of respiratory infectious diseases: a systematic review and analysis. Am J Epidemiol. 2014 Nov;180((9)):865–75. doi: 10.1093/aje/kwu209. [DOI] [PubMed] [Google Scholar]
- 17.Doan Q, Enarson P, Kissoon N, Klassen TP, Johnson DW. Rapid viral diagnosis for acute febrile respiratory illness in children in the Emergency Department. Cochrane Database Syst Rev. 2012 May;5((5)):CD006452. doi: 10.1002/14651858.CD006452.pub3. [DOI] [PubMed] [Google Scholar]
- 18.Sakthivel SK, Whitaker B, Lu X, Oliveira DB, Stockman LJ, Kamili S, et al. Comparison of fast-track diagnostics respiratory pathogens multiplex real-time RT-PCR assay with in-house singleplex assays for comprehensive detection of human respiratory viruses. J Virol Methods. 2012 Nov;185((2)):259–66. doi: 10.1016/j.jviromet.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Driscoll AJ, Karron RA, Bhat N, Thumar B, Kodani M, Fields BS, et al. Evaluation of fast-track diagnostics and TaqMan array card real-time PCR assays for the detection of respiratory pathogens. J Microbiol Methods. 2014 Dec;107:222–6. doi: 10.1016/j.mimet.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mengelle C, Mansuy JM, Da Silva I, Guerin JL, Izopet J. Evaluation of a polymerase chain reaction-electrospray ionization time-of-flight mass spectrometry for the detection and subtyping of influenza viruses in respiratory specimens. J Clin Virol. 2013 Jul;57((3)):222–6. doi: 10.1016/j.jcv.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alby K, Popowitch EB, Miller MB. Comparative evaluation of the Nanosphere Verigene RV+ assay and the Simplexa Flu A/B & RSV kit for detection of influenza and respiratory syncytial viruses. J Clin Microbiol. 2013 Jan;51((1)):352–3. doi: 10.1128/JCM.02504-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vandendriessche S, Padalko E, Wollants E, Verfaillie C, Verhasselt B, Coorevits L. Evaluation of the Seegene Allplexâ„¢ Respiratory Panel for diagnosis of acute respiratory tract infections. Acta Clin Belg. 2018 Oct;11:1–7. doi: 10.1080/17843286.2018.1531605. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Lee J, Lee HS, Cho YG, Choi SI, Kim DS. Evaluation of Allplex Respiratory Panel 1/2/3 Multiplex real-time PCR assays for the detection of respiratory viruses with influenza A virus subtyping. Ann Lab Med. 2018 Jan;38((1)):46–50. doi: 10.3343/alm.2018.38.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gimferrer L, Andrés C, Rando A, Piñana M, Codina MG, Martin MD, et al. Evaluation of Seegene Allplex Respiratory Panel 1 kit for the detection of influenza virus and human respiratory syncytial virus. J Clin Virol. 2018 Aug;105:31–4. doi: 10.1016/j.jcv.2018.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]