Abstract
Purpose
Multiphase computed tomography angiography (MP-CTA) is an innovative imaging tool that can give those managing acute ischemic stroke temporal information on degree and extent of pial collateral arterial filling in the affected brain. We sought to estimate the incidence of false-positive or -negative evaluation of the carotid bifurcation or intracranial thrombus on single-phase CTA (SP-CTA) compared with MP-CTA.
Material and methods
A single-center, retrospective consecutive review was conducted of imaging and clinical records of 150 patients in two months who presented with neurological symptoms with a National Institutes of Health Stroke Scale score ≥ 2 and who received an MP-CTA as part of their investigative work-up. The cohort consisted of 52.3% male and 47.7% female patients. Median individual age was 68 years (interquartile range 60–79). Extracranial and intracranial vessel images of the initial early arterial phase were evaluated and compared with late arterial and early venous phase images.
Results
In the cohort of 150 patients, in three patients (2%) SP-CTA would have led to an incorrect diagnosis and management without MP-CTA–acquired source imaging. The three scenarios represented differentiating a carotid string sign from internal carotid artery occlusion, determining the appearance and extent of thrombus in carotid T-occlusion, and differentiating slow flow and contrast mixing-related artifacts from intraluminal thrombus.
Conclusions
In addition to improving assessment of collateral circulation in acute stroke patients, MP-CTA is also useful in assessing specific flow-related scenarios for which SP-CTA may give spurious results.
Keywords: Multiphase CTA, pseudo-occlusion, pseudo-thrombosis, single-phase CTA, slow flow, stroke
Introduction
Ischemic stroke is a devastating disease with a high burden of neurologic disability and death.1 Hyperacute recanalization with mechanical thrombectomy has proven to be paramount for clinical outcome.2 The Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) trial was designed to assess whether patients with acute ischemic stroke, who were selected on the basis of results of computed tomography (CT) and CT angiography (CTA), would benefit from rapid endovascular treatment involving contemporary endovascular techniques.3 Demchuk et al. demonstrated that use of multiphase CTA, fast and efficient workflow, and effective thrombectomy devices provided evidence of benefit of endovascular treatment in patients with moderate-to-severe ischemic stroke.4 Multiphase CTA (MP-CTA) is an innovative imaging tool that is quick to perform and yields images that are easy to acquire and interpret. It gives those managing acute ischemic stroke information about the degree and extent of pial collateral arterial filling in the affected brain in a time-resolved manner that can influence clinical decision making.5,6 The MP-CTA data set also contains very thin-sliced 0.6 mm source images. We believe these images can be used in addition to the standard maximal intensity projection (MIP) images in acute stroke imaging to better recognize pseudo-occlusion and pseudo-thrombosis, as well as defining clot length.
The purpose of our study is to estimate the incidence of a false-positive or false-negative evaluation of the carotid bifurcation or intracranial thrombus on single-phase CTA (SP-CTA) compared with MP-CTA.
Material and methods
This is a retrospective, single-center cohort study performed between February and April 2017. A total of 150 patients who presented at the emergency department of our center with neurological symptoms with a National Institutes of Health Stroke Scale (NIHSS) score of ≥2 received an MP-CTA as part of their investigative work-up. The cohort consisted of 52.3% male and 47.7% female patients. Median individual age was 68 years (interquartile range (IQR) 60–79). Median time between symptom onset and MP-CTA imaging was 215 minutes (IQR 145–945). Median time between admission and MP-CTA imaging was 25 minutes (IQR 15–41).
In each patient, extracranial and intracranial vessel images of the initial early arterial phase were evaluated and compared with late arterial and early venous phase images. The question was asked whether these two additional phases yielded, aside from the collateral score, additional important information of the carotid bifurcation and intracranial thrombus evaluation, which would have led to a false-positive or false-negative evaluation. NIHSS was evaluated for each patient. All patients were scanned with a Somatom Force Siemens scanner (Siemens Healthcare GmbH, Erlangen, Germany).
The initial phase of the scan was performed as per local protocol for a CT angiogram “arch to vertex” examination, imaging from the level of the aortic arch to the vertex of the skull. As described in the ESCAPE trial3 and outlined in the paper by Menon and colleagues,5 two further CTA phases were then acquired in the clinical setting of a “hot stroke”: “Late arterial” and “early venous” CTA phases were acquired at eight and 16 seconds, respectively, after the start of the initial acquisition (Table 1). Originally, only the MIP series of these phases were sent to our picture archiving and communication system (PACS) to allow for assessment of the intracranial collateral circulation as described in the ESCAPE trial. Given the possible utility of the source imaging in providing additional spatial and temporal resolution of the distal extracranial and circle of Willis arteries, 1 mm contiguous axial series for the eight- and 16-second MP-CTAs were also sent to PACS.
Table 1.
Multiphase CTA scan protocol hot stroke.
| Initial phase | Arterial + early venous phase | |
|---|---|---|
| Bolus tracking | Aortic arch | N/A |
| Contrast + normal saline (ml) | 80 (Omnipaque 350) + 20 | N/A |
| Injection rate (ml/second) | 3 | N/A |
| Collimation (mm) | 128 × 0.6 | 128 × 0.6 |
| Pitch | 0.7 | 0.8 |
| CARE Dose 4D (reference mAs) | 475 | 100 |
| Dose length product (mG-cm) | 800 | 70 |
| Reconstruction thickness (mm) | 1 mm ax arch to vertex | 24 mm ax MIP |
| 4 mm MIP ax/cor/sag/sag oblique neck | ||
| 4 mm MIP ax/cor/sag circle of Willis |
ax: axial; CTA: computed tomography angiography; cor: coronal; MIP: Maximum Intensity Projections; N/A: not applicable; sag: sagittal.
Results
In the cohort of 150 patients, three patients (2%) fulfilled our research criteria. They would have had a wrong evaluation of their carotid bifurcation or intracranial thrombus if the assessment had been based solely on the SP-CTA. With MP-CTA we were able to detect the following three different scenarios.
Pseudo-occlusion
A 72-year-old man was referred from an outside hospital with acute onset of right-sided hemiplegia. His symptoms had already almost completely spontaneously resolved before arrival at our institution with only mild dysarthria and neglect for the right remaining, resulting in an NIHSS score of 2 points. On the SP-CTA performed at the outside hospital, a long segment occlusion of the cervical segment of the left internal carotid artery (ICA) was described with recanalization at the junction of the cervical and petrous segment. An MP-CTA performed at our hospital 215 minutes after symptom onset and 12 minutes after admission demonstrated again the absence of opacification in the left ICA on the early arterial phase. However, on the subsequent additional late arterial and early venous phases of the MP-CTA, there was a thin column of contrast visible in the cervical segment of the ICA, extending into the horizontal segment and carotid siphon, representing a “string” sign (Figure 1).
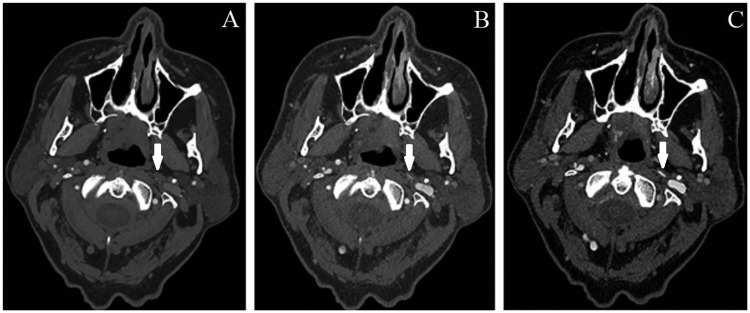
Figure 1.
Axial computed tomography angiography in the (a) early arterial, (b) late arterial and (c) early venous phase in a 72-year-old man with acute-onset, right-sided hemiplegia (National Institutes of Health Stroke Scale score of 2). (a) Absence of opacification in the left internal carotid artery (ICA) (white arrow). (b) Trickle opacification or “string” sign present within the left ICA segment (white arrow). (c) Trickle opacification or “string” sign present within the left ICA segment (white arrow).
Slow flow
An 82-year-old man presented to our institution with a right-sided hemiparesis and aphasia. His NIHSS score was 20 points. An MP-CTA was performed 151 minutes after symptom onset and eight minutes after admission. The first phase of the MP-CTA demonstrated an apparent extensive left-sided carotid “T”-occlusion with suggestion of thrombus in the supraclinoid ICA and no filling of the A1 and M1 segments. The late arterial and venous phases of the MP-CTA, however, demonstrated progressive antegrade contrast filling of the supraclinoid ICA beyond the point of initial suspected occlusion to the true point of carotid-T occlusion, with retrograde filling of the middle cerebral artery (MCA), confirming that the thrombus was completely occlusive (Figure 2).
Figure 2.
Axial computed tomography angiography in the (a) early arterial and (b) late venous phase in an 82-year-old man with a two-hour history of right-sided hemiparesis and aphasia (National Institutes of Health Stroke Scale score of 20). (a) No opacification of the supraclinoid left internal carotid artery (ICA) (white arrow). (b) Better characterization of the extent of the left ICA terminus thrombus (white arrow).
Pseudo-thrombosis
An 83-year-old man presented with a four-month history of gait instability, with acute worsening in the interim leading up to his imaging work-up. An SP-CTA performed at an outside hospital demonstrated poor opacification of the left V3 segment, with an apparent occlusion of the distal left V4 segment, and suspected thrombus extending into the basilar artery. Because of this diagnosis of intraluminal thrombus, the patient was treated with low-molecular weight-heparin (LMWH). However, an MP-CTA was performed in our hospital 15 hours after acute worsening and 36 minutes after admission because of the suspicion that the findings may have been artifactual given the minimal clinical deficits exhibited by the patient in the setting of the extensive thrombus described on his previous CTA. MP-CTA demonstrated similar appearances on the arterial phase as the previous SP-CTA. However, late arterial and venous phase source images demonstrated progressive antegrade contrast filling in the V3 and V4 segments through the high-grade stenosis in the distal V4 segment and no evidence of thrombus in the distal vertebral or basilar artery, with reversal of the degree of contrast opacification in the normally flowing blood from the normal side and the slow-flowing blood from the stenotic vertebral artery (Figure 3).
Figure 3.
(a) Coronal and (b) axial computed tomography (CT) angiography in the early arterial phase and (c) oblique sagittal and (d) axial CT angiography in the early venous phase in an 84-year-old man with a four-month history of gait instability. (a and b) Central poor opacification in the basilar artery (white arrows), concerning for intraluminal thrombus. (c) Focal severe left vertebral artery stenosis (white arrow). (d) No evidence of thrombus in the basilar artery (white arrow).
Discussion
In this single-center, retrospective cohort study of 150 patients, we found three patients (2%) who would have had an incorrect evaluation of their carotid bifurcation or intracranial thrombus if the assessment had been based solely on the SP-CTA.
We believe that MP-CTA has a distinct and clinically important value over SP-CTA, in addition to its described use for the evaluation of collaterals. The additional phases of MP-CTA provide potentially valuable temporal information, thereby allowing enhanced ability to assess the distal extracranial and circle of Willis arteries, and avoid the classic pitfalls of SP-CTA. As the incorrect diagnosis of an occlusion or thrombosis can have far-reaching clinical implications for patient care, our series highlights this value of MP-CTA.
In the patient with the pseudo-occlusion, the differentiation between true carotid occlusion and a “string” sign was made with MP-CTA, allowing accurate assessment of the severely impaired flow beyond the critical proximal ICA stenosis/near occlusion.7,8 This distinction has important clinical implications, as those patients with preocclusive lesions may still benefit from surgical treatment, whereas patients with occlusive lesions are typically treated medically.9,10 Although postulated by others, the specifics of delayed-phase imaging for this purpose have not been described previously.11
In the patient with the slow flow, the precise location and extent of the carotid T-occlusion is much better delineated on the late venous source images of the MP-CTA because of the profoundly limited antegrade flow (and resultant contrast opacification) in the entire ICA, with additional appropriate collateral scoring possible for the MCA territory perfused in a retrograde manner. Proper delineation of the extent of the thrombus has important clinical consequences for considering thrombolytic therapy, as well as for determining need for adjuvant endovascular therapy strategies. First, there is a strong association between occult residual anterograde flow and successful thrombolysis, even in patients with apparently long thrombi.12 Second, there is very limited potential to recanalize occluded arteries with intravenous thrombolytic therapy if the thrombus length exceeds 8 mm.13 MP-CTA has been suggested to be a reliable and valid measure of clot length in acute stroke.14
Finally, MP-CTA imaging of the patient with pseudo-thrombosis highlights that accurate identification of pseudo-thrombosis will lead to avoiding unnecessary medical treatment (such as in our case, in which LMWH had been initiated on the basis of the interpretation of the SP-CTA findings). As medical (and potentially surgical or endovascular) treatment is not without risk, with potential for side effects and complications such as systemic and intracranial bleeding, accurate diagnosis is of the utmost importance.15 We were able to demonstrate that the posterior circulation pseudo-thrombus was due to the delayed arrival of contrast as a result of slow flow beyond a critical stenosis in the V4 segment of the affected vertebral artery. Helical flow in the basilar artery has been earlier described as due to the confluence of asymmetric flow from the vertebral arteries.16 This is demonstrated in our case by contrast opacification of the left vertebral artery on the early venous phase being higher than on the right. The pseudo-thrombus appearance on the SP-CTA is thought to be due to abnormal mixing of contrast-opacified blood from the normal right vertebral artery and nonopacified blood from the left vertebral artery.
A recent study described a potential role for perfusion-derived four-dimensional CTA (4D-CTA) in acute stroke imaging.17 However, MP-CTA has numerous benefits over 4D-CTA: It does not require any advanced mathematical postprocessing at an independent workstation; it has lower radiation exposure; there is no need for additional contrast material administration; and MP-CTA can be performed on virtually all modern CT scanners, whereas access to CT scanners with 4D-CTA scanning capability is extremely limited.5
The key limitation of MP-CTA is an increased radiation dose compared with SP-CTA. However, this incremental increase in dose is quite small (approximately 10% of the first phase of the CTA for each additional phase acquired). As SP-CTA is often adequate for providing the desired neurovascular information in most nonemergent settings, MP-CTA does not need to be performed in most patients, thereby avoiding this increased radiation dose exposure. The decision to perform MP-CTA must be made a priori, balancing the potential for diagnostic information gained against the increase in radiation dose. Another cost, such as the additional image processing time at the CT console, also has to be considered. Although MP-CTA will most commonly be performed in patients presenting with features of acute ischemic stroke, it may be of additional benefit in selected nonemergent cases, such as evaluation for a carotid “string” sign, or other situations in which there is potential for flow-related artifacts. Finally, as some institutions do not send these source images to PACS immediately after completion of the examination (given that they are used to generate the intracranial large-volume MIP images used for collateral scoring), we advocate that when MP-CTA is performed, this routinely includes generation and archiving of the 1 mm axial MPR series from the latter phases of the MP-CTA.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Latchaw RE, Alberts MJ, Lev MH, et al. Recommendations for imaging of acute ischemic stroke: A scientific statement from the American Heart Association. Stroke 2009; 40: 3646–3678. [DOI] [PubMed] [Google Scholar]
- 2.Kaschka IN, Kloska SP, Struffert T, et al. Clinical and radiological outcome after mechanical thrombectomy in acute ischemic stroke: What matters? Neuroradiol J 2016; 29: 99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demchuk AM, Goyal M, Menon BK, et al. Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) trial: Methodology. Int J Stroke 2015; 10: 429–438. [DOI] [PubMed] [Google Scholar]
- 4.Demchuk, Goyal M, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 5.Menon BK, d’Esterre CD, Qazi EM, et al. Multiphase CT angiography: A new tool for the imaging triage of patients with acute ischemic stroke. Radiology 2015; 275: 510–520. [DOI] [PubMed] [Google Scholar]
- 6.Maas MB, Lev MH, Ay H, et al. Collateral vessels on CT angiography predict outcome in acute ischemic stroke. Stroke 2009; 40: 3001–3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marquering HA, Nederkoorn PJ, Beenen LF, et al. Carotid pseudo-occlusion on CTA in patients with acute ischemic stroke: A concerning observation. Clin Neurol Neurosurg 2013; 115: 1591–1594. [DOI] [PubMed] [Google Scholar]
- 8.Grossberg JA, Haussen DC, Cardoso FB, et al. Cervical carotid pseudo-occlusions and false dissections: Intracranial occlusions masquerading as extracranial occlusions. Stroke 2017; 48: 774–777. [DOI] [PubMed] [Google Scholar]
- 9.Winslow CM, Solomon DH, Chassin MR, et al. The appropriateness of carotid endarterectomy. N Engl J Med 1988; 318: 721–727. [DOI] [PubMed] [Google Scholar]
- 10.Barnett HJM, Taylor DW, et al. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991; 325: 445–453. [DOI] [PubMed] [Google Scholar]
- 11.Delgado Almandoz JE, Romero JM, Pomerantz SR, et al. Computed tomography angiography of the carotid and cerebral circulation. Radiol Clin North Am 2010; 48: 265–281. [DOI] [PubMed] [Google Scholar]
- 12.Ahn SH, d’Esterre CD, Qazi EM, et al. Occult anterograde flow is an under-recognized but crucial predictor of early recanalization with intravenous tissue-type plasminogen activator. Stroke 2015; 46: 968–975. [DOI] [PubMed] [Google Scholar]
- 13.Riedel CH, Zimmermann P, Jensen-Kondering U, et al. The importance of size: Successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke 2011; 42: 1775–1777. [DOI] [PubMed] [Google Scholar]
- 14.Polito V, La Piana R, Del Pilar Cortes M, et al. Assessment of clot length with multiphase CT angiography in patients with acute ischemic stroke. Neuroradiol J 2017; 30: 593–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martel N, Lee J, Wells PS. Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: A meta-analysis. Blood 2005; 106: 2710–2715. [DOI] [PubMed] [Google Scholar]
- 16.Chong BW, Kerber CW, Buxton RB, et al. Blood flow dynamics in the vertebrobasilar system: Correlation of a transparent elastic model and MR angiography. Am J Neuroradiol 2014; 15: 733–745. [PMC free article] [PubMed] [Google Scholar]
- 17.Ng FC, Choi PM, Datta M, et al. Perfusion-derived dynamic 4D CT angiography identifies carotid pseudo-occlusion in hyperacute stroke. J Neuroimaging 2016; 26: 588–591. [DOI] [PubMed] [Google Scholar]