Abstract
Calciphylaxis is a rare cutaneous disease that may cause fatal complications in patients on long-term dialysis. Early diagnosis and proper management decrease complications. However, it can mimic cutaneous infections, especially ecthyma gangrenosum and cutaneous vasculitis. The authors report on a patient with chronic kidney disease (CKD) on dialysis for 10 years who developed painful skin necrosis on his right thigh. The tissue culture was positive for Enterobacter cloacae, Citrobacter freundii, and Pseudomonas aeruginosa, but the histopathology was compatible with calciphylaxis. This report aims to further the knowledge of physicians in order to help them recognize calciphylaxis in CKD patients with painful necrotic ulcers.
Keywords: Calciphylaxis, Chronic kidney disease, Ecthyma gangrenosum, End-Stage renal disease
Introduction
Calciphylaxis is a rare, life-threatening vascular calcification with cutaneous necrosis that occurs most frequently in patients with chronic kidney disease on long-term dialysis [1]. It is also known as calcific uremic arteriopathy and may cause fatal complications. The common presenting symptoms are painful eschars and non-healing ulceration with skin necrosis, so the differential diagnoses include skin infections, particularly ecthyma gangrenosum, cutaneous vasculitis, and other vasculitis mimicking conditions. We report on an Asian man with chronic kidney disease on regularly dialysis developed painful skin necrosis on the right thigh, compatible with calciphylaxis.
Case report
A 43-year-old Asian man with end-stage renal disease (ESRD) for 10 years on peritoneal dialysis with osteoporosis, secondary hyperparathyroidism status post subtotal parathyroidectomy, hypertension, and dyslipidemia. He smoked cigarettes for 10 years but stopped 10 years before and cannabis. The patient presented with thigh pain that progressed to necrotic skin lesions on the right thigh (Fig. 1) about 2 weeks prior to admission, then developed into large skin necrosis on the right thigh with a violaceous patch on the left thigh on admission (Fig. 2) without fever.
Fig. 1.
The clinical photograph shows a localized, painful, necrotic skin on the right inner thigh.
Fig. 2.
Clinical photographs show progressive large painful necrotic skin on both thighs. (A, the right inner thigh; B, the left lateral thigh).
Laboratory investigations were consistent chronic renal injury with blood urea nitrogen 60.2 (6–20) mg/dL, creatinine 16.84 (0.67–1.17) mg/dL, serum calcium 8 (8.6–10.2) mg/dL, phosphate 7.7 (2.7–4.5) mg/dL, and parathyroid hormone 78.69 (11–16) pg/mL. The complete blood count showed white blood cells count 15,200 /uL (neutrophils 88%, lymphocytes 3%, eosinophils 3%, monocytes 5%, myelocyte 1%), hemoglobin 8.6 g/dL, and platelet count 311,000 /uL.
A skin biopsy was performed. The sections of skin on the right thigh showed non-specific inflammation and necrosis with calcification involving small arteries without findings suggestive of vasculitis (Fig. 3). The tissue culture was positive for Enterobacter cloacae, Citrobacter freundii, and Pseudomonas aeruginosa. A blood culture showed no growth. He was diagnosed with calciphylaxis with a secondary skin infection. His scheduled continuous ambulatory peritoneal dialysis (CAPD) duration was not changed from eight hours per day.
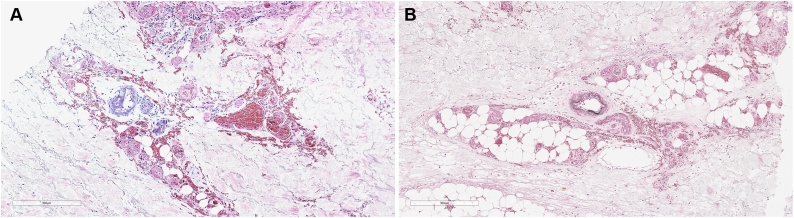
Fig. 3.
The skin biopsy specimen from the right thigh shows (A) calcific vessel walls on the deep dermis and (B) the calcification is positive of von Kossa stain.
The patient was received intravenous ciprofloxacin. Skin lesions were managed with twice daily wound care. The patient was given systemic sodium thiosulfate therapy of 12.5 mg three times a week with discontinuing the calcium-containing phosphate. His severe pain had to be controlled with oral opioids, gabapentin, and intravenous fentanyl. After 2 months of treatment, the patient skin condition was still progressive. The patient refused to surgical debridement and died from sepsis 3 months after presenting cutaneous lesions.
Discussion
The term “calciphylaxis” was first used by Hans Selye in 1961 [2]. Calciphylaxis was considered a rare diagnosis that typically manifests as painful cutaneous lesions and results in poor outcomes. However, it is increasingly being reported in an increasing number of patients with chronic kidney disease [1]. Risk factors for calciphylaxis are kidney failure, obesity, female sex, white race, liver disease, elevated calcium-phosphorus products, medications (warfarin, systemic steroids, calcium binders, and vitamin D analogs), a hypercoagulable state, and hypoalbuminemia [1]. Warfarin is most frequently associated with the disease [3]. Moreover, calciphylaxis is associated with high morbidity and mortality, especially in patients with ulcerated lesions and multiple comorbidities, with a reported 1-year mortality of 30–80% [4]. Cause of death relates to the progression of the necrotic wound, promoting the infection and sepsis [5].
The pathogenesis of calciphylaxis is unclear. Histologic analysis suggests that calcified, narrowed microvessels lead to chronic, low-grade ischemia and further occlusion of the vessels induced by endothelial injury and microthrombosis resulting in infarction [1]. Calciphylaxis can clinically manifest in two phases. In the first phase, it presents with pruritus and cutaneous laminar erythema as a violaceous rash, which is nonspecific and may resemble livedo reticularis. Therefore, in this stage, misinterpretation can easily be made. During the second phase, it presents with a rash that progresses to painful eschars and later develops into painful non-healing ulceration and necrosis [6]. The most common involvement is of the lower extremities and skin regions with dense adipose tissue [7].
In patients with calciphylaxis, clinical suspicion is important for early diagnosis. Many disorders mimic calciphylaxis, including ecthyma gangrenosum, warfarin-induced skin necrosis, atherosclerotic vascular disease, and venous stasis ulcer. Skin biopsy is the standard method for confirmation of clinically suspected calciphylaxis; however, its role in practice is debated, given the risk of provoking new, nonhealing ulcers and infection [8].
After the diagnosis, proper management and treatment play vital roles in decreasing the suffering of the patient, avoiding further complications, and lowering the mortality rate to some degree [3]. Treatment should utilize a multi-disciplinary approach and include nephrologists, dermatologists, wound care specialists, and nutritionists. Pain management typically includes analgesics, wound care, proper nutrition, elimination of iatrogenic factors (e.g., warfarin), and the aggressive treatment of predisposing conditions. Other treatments to consider: sodium thiosulfate, bisphosphonate, and hyperbaric oxygen [1]. Management is mainly directed toward local wound care and the prevention of local and systemic infections, in addition to optimizing medical therapy for associated co-morbid conditions [9].
Conclusion
Calciphylaxis remains rare, but it can be the cause of major morbidity and mortality in patients with chronic kidney disease regardless of etiology. If the condition is detected early, there is a better chance of managing the symptoms and improving the quality of life for the patient. Clinicians need to have increased clinical suspicion for calciphylaxis in patients with CKD who develop painful, ischemic skin lesions.
CRediT authorship contribution statement
Ranchana Tangkham: Conceptualization, Data curation, Writing - original draft. Siripan Sangmala: Conceptualization, Data curation, Writing - original draft. Kumpol Aiempanakit: Conceptualization, Data curation, Writing - review & editing. Kanokphorn Chiratikarnwong: Conceptualization, Supervision, Writing - review & editing. Sauvarat Auepemkiate: Conceptualization, Supervision, Writing - review & editing.
Acknowledgments
This case report was approved by the Research Ethics Committee, Faculty of Medicine, Prince of Songkla University (REC 62-195-14-1). We would especially like to thank the International Affairs Office, Faculty of Medicine, Prince of Songkla University for language editing services.
References
- 1.Nigwekar S.U., Thadhani R., Brandenburg V.M. Calciphylaxis. N Engl J Med. 2018;378:1704–1714. doi: 10.1056/NEJMra1505292. [DOI] [PubMed] [Google Scholar]
- 2.Selye H., Gentile G., Jean P. An experimental model of “dermatomyositis” induced by calciphylaxis. Can Med Assoc J. 1961;85:770–776. [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed M.M., Zakir A., Ahsraf M.F., Ejaz A., Ashraf A., Namburu L. Chronic kidney disease and calciphylaxis: a literature review. Cureus. 2018;10:e3334. doi: 10.7759/cureus.3334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weenig R.H., Sewell L.D., Davis M.D., McCarthy J.T., Pittelkow M.R. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569–795. doi: 10.1016/j.jaad.2006.08.065. [DOI] [PubMed] [Google Scholar]
- 5.Santos P.W., He J., Tuffaha A., Wetmore J.B. Clinical characteristics and risk factors associated with mortality in calcific uremic arteriolopathy. Int Urol Nephrol. 2017;49:2247–2256. doi: 10.1007/s11255-017-1721-9. [DOI] [PubMed] [Google Scholar]
- 6.Fine A., Fleming S., Leslie W. Calciphylaxis presenting with calf pain and plaques in four continuous ambulatory peritoneal dialysis patients and in one predialysis patient. Am J Kidney Dis. 1995;25:498–502. doi: 10.1016/0272-6386(95)90116-7. [DOI] [PubMed] [Google Scholar]
- 7.Brewster U.C. Dermatological disease in patients with CKD. Am J Kidney Dis. 2008;51:331–344. doi: 10.1053/j.ajkd.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Brandenburg V.M., Evenepoel P., Floege J., Goldsmith D., Kramann R., Massy Z. Lack of evidence does not justify neglect: how can we address unmet medical needs in calciphylaxis? Nephrol Dial Transplant. 2016;31:1211–1219. doi: 10.1093/ndt/gfw025. [DOI] [PubMed] [Google Scholar]
- 9.Vedvyas C., Winterfield L.S., Vleugels R.A. Calciphylaxis: a systematic review of existing and emerging therapies. J Am Acad Dermatol. 2012;67 doi: 10.1016/j.jaad.2011.06.009. [DOI] [PubMed] [Google Scholar]