Abstract
Background:
Hypertension is a risk factor for renal disease. Therefore, this study was aimed at estimating the prevalence of hypertension in renal patients in Iran through meta-analysis.
Methods:
The search was carried out using authentic Persian and English keywords in national and international databases including IranMedex, SID, Magiran, IranDoc, Medlib, ScienceDirect, Pubmed, Scopus, Cochrane, Embase, Web of Science, Medline, and Google Scholar search engine without any time limitation until 2017. Heterogeneity of studies was assessed using the I2 index. Data were analyzed using STATA ver 11.
Results:
In 35 reviewed studies with a sample of 39,621 subjects, the prevalence of hypertension in renal patients was 35% (95% CI: 29%–41%) (25% in women and 18% in men). The prevalence of systolic hypertension in renal patients was 5%, diastolic hypertension 26%, and diabetes 23%. The prevalence of hypertension in hemodialysis patients was 34%, 27% in peritoneal dialysis, 43% in kidney transplantation, and 26% in chronic renal failure. In addition, meta-regression showed that the prevalence of hypertension in renal patients did not significantly decrease during the years 1988–2017.
Conclusions:
More than a third of kidney patients in Iran suffer from high blood pressure. The diastolic blood pressure of these patients is about five times higher than their systolic blood pressure. Moreover, the age group under 30 is a high-risk group. The prevalence of hypertension in women with kidney disease is higher than in men. In addition, patients who have kidney transplants are more likely to have high blood pressure than other kidney patients.
Keywords: Hypertension, Iran, kidney disease, meta-analysis, renal disease
Introduction
Among the selected articles from 1999 to 2012, the prevalence of hypertension was 17%. The prevalence of hypertension among the people above 20 years was 24% and that among the people below 20 years was 5%.[1] In 32 studies with a sample of 34,714 subjects, the prevalence of hypertension in Iranian diabetic patients was 51% (95% CI: 43%–60%). The prevalence of hypertension was 55% in type I diabetics and 53% in type II diabetic patients.[2] In Haghdoust study, in 2006, the prevalence of hypertension in 29 studies was 21.9%.[3]
Today, chronic disease is one of the most important health problems affecting different dimensions of physical, psychological, economic, social, and quality of life of patients.[4,5,6,7,8,9] Hypertension is a common chronic disease that underlies several diseases such as heart attack, brain attack, and advanced kidney disease,[10,11,12,13,14,15,16,17] which is defined as systolic blood pressure above 140 mmHg and diastolic blood pressure above 90 mmHg.[12] As a global problem, it is a common asymptomatic disease, often called a silent killer.[18] According to the World Health Organization, high blood pressure after smoking has been introduced as the second leading cause of death in developing countries and is the third most common cause of noncommunicable diseases. This disease has different prevalence in different societies and the prevalence ranges from 10% to more than 60% in different countries.[19,20] It has also been estimated that blood pressure has been responsible for 4.5% of the global burden of diseases.[21,22,23,24]
End-stage renal disease (ESRD) is the severe type of chronic kidney disease, which is the final stage of an irreversible progressive renal disorder. In this disease, the body's ability to maintain the balance between fluid and electrolyte disappears and leads to uremia or asthenia.[25,26,27,28,29,30,31] In fact, when more than 95% of the kidney tissue is destroyed for various reasons, the accumulation of toxins in the body increases considerably and life-threatening complications force the person to undergo Renal replacement therapies forever.[32,33] The population of patients with kidney failure in Iran is 320,000; 49% of them use renal transplantation therapy, 48% of them use the hemodialysis method, and 3% of them use the peritoneal dialysis method.[34] This disease can lead to death if the patient does not undergo dialysis or kidney transplantation.[25,26,27,35,36,37]
In 1990, renal failure was considered as the 27th mortality factor in the world, and reached the 18th rank in 2010.[38] According to the Centers for Disease Control and Prevention, in 2014, more than 20% of people with serious hypertension suffered from chronic kidney disease and were at risk for ESRD.[39] On the other hand, about 75%–80% of patients with ESRD have high blood pressure.[40] In all developed countries and in many developing countries, diabetes and hypertension are considered as the main cause of chronic kidney disease.[23,36,41,42,43,44,45,46,47,48]
Considering that published articles about the prevalence of hypertension in renal patients in Iran reported varied incidence of 9%–86% for the prevalence of high blood pressure, the need for a meta-analysis seemed necessary.
Materials and Methods
Study protocol
This study is a systematic review and meta-analysis study that the prevalence of hypertension in Iranian renal patients. This study was conducted on the basis of the PRISMA1 statement that is concerned with systematic review and meta-analysis studies.[49] Based on this protocol, all stages of the research methodology such as search, selection of studies and qualitative assessment of studies, and data extraction from the studies were conducted by two researchers independently. If there was a difference in the report of the researchers, the third researcher investigated and resolved the dispute.
Search strategy
This study is a meta-analysis that investigates the prevalence of hypertension in renal patients. The findings of this study were based on studies conducted in Iran. We searched national databases including IranMedex, SID, Magiran, IranDoc and Medlib, and international databases including ScienceDirect, PubMed, Scopus, Cochrane, Embase, Web of Science, and Medline. The mechanism for searching articles mainly based on the systematic search of related Persian keywords and their English equivalents (“Iran,” “Meta-analysis,” “Kidney disease,” “Renal disease,” “Hypertension”) was carried out independently by two researchers. For the final analysis, keywords were also searched in the Google Scholar search engine without time limit until 2017. It should be noted that the keywords were also searched together using (OR/AND) operators.
Study selection
First, all articles related to this subject in Iran were collected and a list of abstracts was prepared after the search was completed. This task was done independently by two researchers. Then, the articles with duplicate titles were excluded. Subsequently, the abstracts of articles were reviewed to find appropriate studies. Regarding international databases, the process was similar to that of national databases.
In the first stage of the search, 732 articles were found, and after reviewing the titles of articles, 285 overlapping articles were removed. Among the remaining 447 papers, 229 articles were excluded from the exit criteria. The following is a list of the exclusion reasons: (1) the study was performed on other patients, except for renal patients; (2) the study was conducted in a country other than Iran; (3) the articles looked at risk factors or blood pressure complications. The full text of 218 articles was reviewed. Among them, 182 articles were excluded, because they were incomplete or their full text was not available. In the remaining 36 articles, 1 article was removed because of low quality. Finally, 35 appropriate articles were selected to enter the meta-analysis stage [Figure 1].
Figure 1.
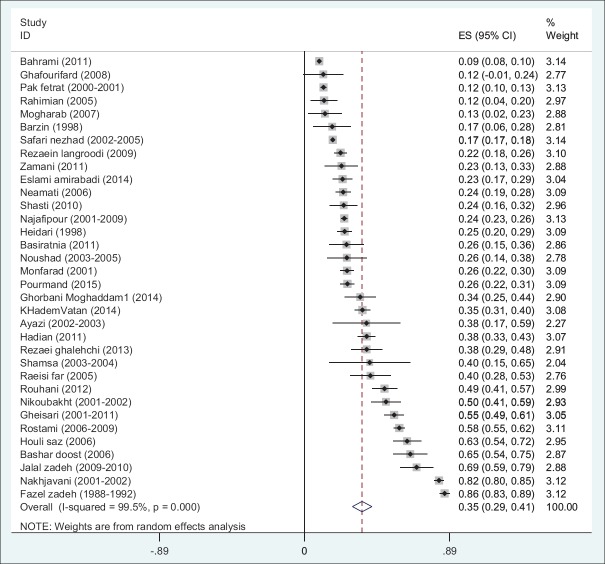
Prevalence of hypertension in renal patients in Iran with a 95% confidence interval based on the author's name and year of research according to the random effects model. The midpoint of each section shows the prevalence of hypertension in renal patients in each study. The lozenge shows the prevalence of hypertension in renal patients in Iran for all studies
Quality evaluation
All studies that reported the prevalence of osteoporosis in Iranian elderly people entered the study. To assess the quality of the studies, STROBE (3) was used as the standard checklist. This checklist contains 22 items that cover different parts of a report (sampling, measurement of variables, study objectives, and statistical analysis). One point was given to each item, and some other items that were more important to us had more points. The STROBE checklist contains 22 sections that cover different parts of a report, and the maximum score of a report equals 44, so that a score of 1–15 indicates poor quality, 16–30 shows average quality, and 31–44 is considered to be excellent. Articles with a total score of less than 16 were excluded from the meta-analysis.
Data extraction
To reduce reporting bias and error in data collection, two researchers independently extracted data from articles and entered the extracted data into a checklist containing the following items: first author's name, study title, sample size, year and place of study, prevalence of hypertension in renal patients based on sex, prevalence of systolic and diastolic hypertension, prevalence of diabetes, Type of disease, age, etc.
Statistical analysis
To analyze and combine the results of various studies, the prevalence of hypertension in renal patients in each study was considered as a binomial probability distribution and its variance was calculated by binomial distribution. The heterogeneity of studies was measured using the Q test and I square (I2) index. Due to the heterogeneity of the studies, the random effects model was used to combine the results of the studies. The data were analyzed using STATA Ver. 11, and the significance level of the test was considered as 0.05.
Meta-regression was used to investigate the relationship between the prevalence of hypertension in renal patients and the sample size and year of research. Sensitivity analysis was used to determine the effect of removing each study on the final meta-analysis.
Results
Summary of how to enter the articles into the meta-analysis process
In 35 articles with a sample size of 39,621 people, the prevalence of hypertension in Iranian renal patients was 35% (95% CI: 29%–41%). The lowest and highest prevalence of hypertension were 9% in Brahimi's study[50] and 86% in Fazelzadeh's study,[51] respectively. Considering the heterogeneity of studies, the confidence interval (CI) for each study based on the random effects model is presented in Diagram 1. The characteristics of the reviewed articles are presented in Table 1.
Diagram 1.
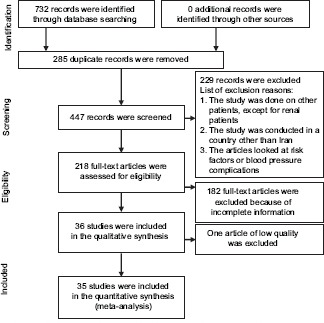
Flowchart of studies to the systematic review and meta-analysis
Table 1.
Characteristics of Studies Qualified for Systematic Review and Meta-Analysis
| Author | Age mean (SD) | Year of study | City of study | Type of disease | Sample size | Prevalence of hypertension (%) |
|---|---|---|---|---|---|---|
| [52]Bashardoost | 53 (16.7) | 2006 | Ardebil | Hemodialysis Patients | 80 | 64.9 |
| [53]Hasan Zamani | 48 (18.03) | 2011 | Mashhad | Hemodialysis Patients | 66 | 22.7 |
| [54]Pourmand | 39.3 | 2015 | Tehran | Kidney transplantation patients | 400 | 26.3 |
| [55]Basiratnia | 17.4 | 2011 | Shiraz | Kidney transplantation patients | 66 | 25.7 |
| [56]Shamsa | 35.26 | 2003-2004 | Mashhad | Kidney transplantation patients | 15 | 40 |
| [51]Fazel zadeh | 45 | 1988-1992 | Shiraz | Kidney transplantation patients | 500 | 86 |
| [57]Houli saz | 40.26 | 2006 | Tehran | Kidney transplantation patients | 119 | 63 |
| [58]Nikoubakht | 40.45 | 2001-2002 | Tehran | Kidney transplantation patients | 119 | 50 |
| [59]Noushad | 48 | 2003-2005 | Tabriz | Kidney transplantation patients | 50 | 26 |
| [60]Rostami | 40.7 | 2006-2009 | Tehran | Kidney transplantation patients | 804 | 58.2 |
| [61]Pak fetrat | 38.5 | 2000-2001 | Shiraz | Kidney transplantation patients | 1354 | 11.6 |
| [62]Rezaei ghalehchi | 25-70 | 2013 | Ardebil | Hemodialysis Patients | 100 | 38.2 |
| [63]Noubakht haghighi | 30.43 | 2005-2008 | Iran | Donor nephrectomies | 1549 | - |
| [64]Rouhani | 61.3 | 2012 | Tehran | Hemodialysis Patients | 163 | 49.1 |
| [65]Najafi | 46.6 | 2001-2009 | Iran | peritoneal dialysis | 2302 | 24.4 |
| [50]Barahimi | >30 | 2011 | Shahreza | Chronic kidney disease | 11720 | 9 |
| [66]Gheisari | 11.01 | 2001-2011 | Esfahan | Chronic kidney disease | 268 | 55 |
| [67]Jalal zadeh | 56.6 | 2009-2010 | Zanjan | Hemodialysis Patients | 80 | 68.8 |
| [68]Neamati | 62 | 2006 | Tehran, Ahvaz, Kermanshah, Mashhad, shiraz | Hemodialysis Patients | 337 | 23.7 |
| [69]Safari nezhad | >14 | 2002-2005 | Iran | Chronic kidney disease | 16354 | 17.3 |
| [70]Ayazi | 51.2 | 2002-2003 | Tehran | peritoneal dialysis | 21 | 38 |
| [71]Nakhjavani | 32-89 | 2001-2002 | Tehran | Hemodialysis Patients | 620 | 82.5 |
| [72]Barzin | 49 | 1998 | Sari | Hemodialysis Patients | 41 | 17 |
| [73]Monfarad | 2001 | Gilan | Hemodialysis Patients | 414 | 17 | |
| [74]Shasti | 62.2 (13.7) | 2010 | Tehran | Hemodialysis Patients | 100 | 26.1 |
| [75]Raeisi far | 51.48 | 2005 | Abadan | Hemodialysis Patients | 59 | 40.4 |
| [76]Ghafourifard | 48.6 (19) | 2008 | Esfahan | Hemodialysis Patients | 26 | 11.5 |
| [77]Heidari | 47 | 1998 | Mazandaran | Hemodialysis Patients | 353 | 24.6 |
| [78]Mogharab | 56-65 | 2007 | Birjand | Hemodialysis Patients | 40 | 12.5 |
| [79]Eslami amirabadi | 50.4 (15.2) | 2014 | Tehran | Hemodialysis Patients | 189 | 23.3 |
| [80]Rahimian | 56.7 | 2005 | Yazd | Hemodialysis Patients | 60 | 12 |
| [81]Ghorbani Moghaddam1 | 55.7 (15.63) | 2014 | Bushehr | Hemodialysis Patients | 93 | 34.2 |
| [82]Hadian | 53.2 (16.4) | 2011 | Lorestan | Hemodialysis Patients | 318 | 38.1 |
| [83]Rezaein langroodi | 56-65 | 2009 | Hamedan | Hemodialysis Patients | 455 | 22.1 |
| [84]KhademVatan | 55 (17.7) | 2014 | Orumie | Hemodialysis Patients | 386 | 35.5 |
The prevalence of hypertension in women with renal disease was 25% (95% CI: 16%–35%) and in men was 18% (95% CI: 15%–22%). In addition, the prevalence of systolic hypertension in renal patients was 5% (95% CI: 0%–13%), the prevalence of diastolic hypertension was 26% (95% CI: 0%–77%), and the prevalence of diabetes was 23% (95% CI: 17%–29%). The prevalence of hypertension in women with renal disease is 7% higher than men [Table 2].
Table 2.
Prevalence of hypertension in renal patients in the studied subgroups
| Subgroups | Number of study | Prevalence (95% CI) | P | I2 (%) | |
|---|---|---|---|---|---|
| Sex | Total | 34 | 35 (29-41) | P<0.001 | 99.5 |
| Women | 3 | 25 (16-35) | P<0.001 | 91.7 | |
| Men | 3 | 18 (15-22) | 0.103 | 56.1 | |
| Type of hypertension | Systolic | 3 | 5 (0-13) | P<0.001 | 99.2 |
| Diastolic | 3 | 26 (0-77) | P<0.001 | 100 | |
| Type of disease | Hemodialysis Patients | 20 | 34 (23-45) | P<0.001 | 98.4 |
| Kidney transplantation patients | 9 | 43 (19-67) | P<0.001 | 99.6 | |
| Chronic kidney disease | 3 | 26 (17-34) | P<0.001 | 99.7 | |
| Peritoneal dialysis | 2 | 27 (16-38) | 0.201 | 38.9 | |
| Age (Year) | <30 | 2 | 41 (12-69) | P<0.001 | 95.6 |
| 30-39 | 3 | 22 (9-36) | P<0.001 | 95.3 | |
| 40-49 | 10 | 39 (20-57) | P<0.001 | 99.4 | |
| 50-59 | 11 | 35 (26-44) | P<0.001 | 94.0 | |
| 60-70 | 3 | 32 (16-48) | P<0.001 | 93.9 | |
| Region | North | 14 | 42 (28-55) | P<0.001 | 98.7 |
| South | 2 | 37 (29-44) | 0.442 | 0 | |
| Center | 7 | 30 (10-50) | P<0.001 | 99.8 | |
| West | 5 | 38 (25-50) | P<0.001 | 95.3 | |
| East | 3 | 21 (9-33) | 0.091 | 58.4 | |
In an analysis based on the type of renal disease, we found that the prevalence of hypertension in hemodialysis patients was 34% (95% CI: 23%–45%) in 20 reviewed studies. In nine other studies performed on renal transplant patients, the prevalence of hypertension was 43% (95% CI: 19%–67%). Two studies were also performed on peritoneal dialysis patients with a hypertension prevalence of 27% (95% CI: 16%–38%). The three last studies were conducted on chronic renal failure patients and we found that the prevalence of hypertension was 26% (95% CI: 17%–34%). The prevalence of hypertension in renal transplant patients is higher than that of hemodialysis, peritoneal, and chronic kidney dialysis patients [Table 2].
In an analysis performed based on the age group, the prevalence of hypertension was 41% (95% CI: 12%–69%) among 1–29-year-old renal patients, 22% (95% CI: 9%–36%) among 30–39-year-old patients, 39% (95% CI: 20%–57%) among 40–49-year-old renal patients, 35% (95% CI: 26%–44%) among 50–59-year-old renal patients, and 32% (95% CI: 16%–48%) among 60–70-year-old renal patients. Moreover, 1–29-year-old renal patients are more likely to have hypertension compared with other patients; however, given the varying number of studies in any age group, we cannot say with certainty [Table 2].
The prevalence of hypertension in renal patients in the north of Iran was 42% (95% CI: 28%–55%), in the south was 37% (95% CI: 29%–44%), in the center was 30% (95% CI: 10%–50%), and in the west was 38% (95% CI: 25%–50%). Renal patients in the north of Iran suffer more from high blood pressure compared with other regions of Iran [Table 2].
In sensitivity analysis, we find that the prevalence of hypertension in renal patients in Iran was reduced to 33.65% (95% CI: 28.55%–38.75%) by removing the study of Fazelzadeh[20] and increased to 36.16% (95% CI: 28.58%–43.77%) after removing Brahimi's study,[19] and these two studies are the most effective studies in the final meta-analysis [Figure 2].
Figure 2.
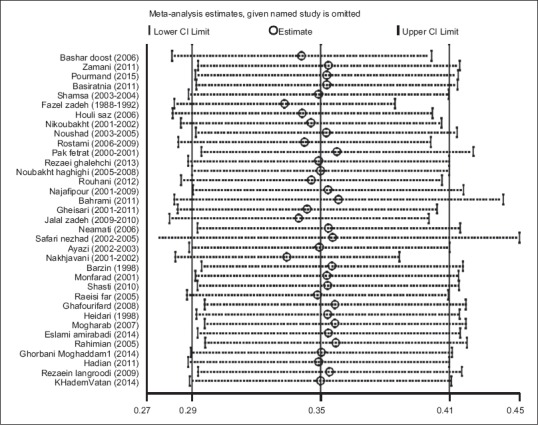
Sensitivity analysis
Discussion
In 35 reviewed studies with a sample of 39,621 subjects, the prevalence of hypertension in renal patients was 35% (95% CI: 29%–41%) (25% in women and 18% in men). The prevalence of systolic hypertension in renal patients was 5%, diastolic hypertension 26%, and diabetes 23%. The prevalence of hypertension in hemodialysis patients was 34%, 27% in peritoneal dialysis, 43% in kidney transplantation, and 26% in chronic renal failure. In addition, meta-regression showed that the prevalence of hypertension in renal patients did not significantly decrease during the years 1988–2017.
According to the initial care system surveys of noncommunicable disease risk factors in Iran in 2005, the prevalence of hypertension in individuals aged 15–64 was 17.1%.[19,20] In a general study, the prevalence of hypertension was 11% in Isfahan, 17% in Chaharmahal and Bakhtiari, 11.6% in Gilan, 17.5% in Zanjan, 6.25% in Kermanshah, and 18.9% in Arak.[85] In the study of Bashardost et al., 44.9% of hemodialysis patients had high blood pressure.[86] In a study on renal transplant patients, Rostami et al. found that the prevalence of hypertension was 58.2%.[60] In another study by Rezaei Ghalechi to analyze depression in hemodialysis patients, the prevalence of hypertension and diabetes was 38.2% and 34.2%, respectively.[62] The prevalence of hypertension was estimated to be 17.3% in a study conducted in Iran in 2002–2005 to investigate the risk factors associated with chronic kidney disease.[69] In the study of Malekmakan et al., the most common causes of chronic renal failure in hemodialysis patients in Fars province were hypertension and diabetes.[87] In a study entitled “A 17-year history of peritoneal dialysis in Iran,” which was conducted on 2302 people, the prevalence of high blood pressure in these patients was 24.4%.[65] Due to the differences in the results of studies on the prevalence of high blood pressure in renal patients, this study was conducted through systematic review and meta-analysis.
In 35 articles with a sample size of 39,621 individuals, performed from 1988 to 2017, 34 articles outlined the prevalence of high blood pressure in renal patients, and the prevalence of hypertension in renal patients was estimated to be 35% (95% CI: 29%–41%) (25% in women and 18% in men). The prevalence of systolic hypertension in renal patients was 5%, diastolic hypertension was 26%, and diabetes was 23%.
Meta-regression showed that there was no significant relationship between the prevalence of hypertension in renal patients and the number of research samples (P = 0.128), that is, with an increase in the number of samples, the prevalence of hypertension in renal patients decreased, but this was not statistically significant [Figure 3]. There was no significant relationship between the prevalence of hypertension in renal patients and the year of study (P = 0.102). During the years 1988–2017, the prevalence of hypertension in renal patients in Iran decreased but was not statistically significant [Figure 4]. In Figures 5 and 6, we see that the effect of publication bias is not statistically significant.
Figure 3.
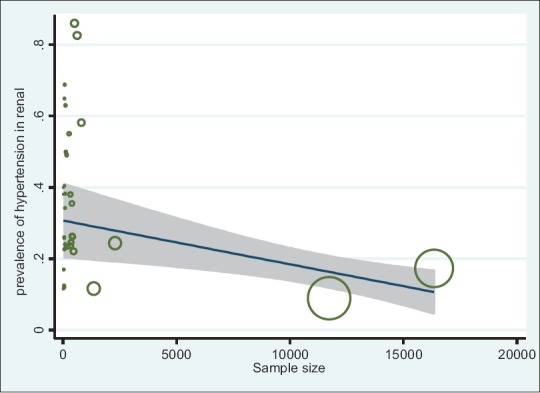
Relationship between high prevalence of hypertension in renal patients in Iran and the sample size using meta-regression
Figure 4.
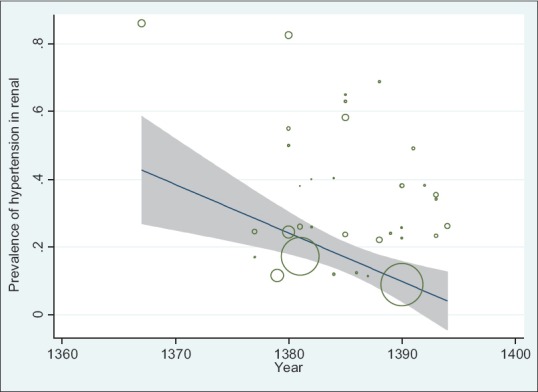
Relationship between the prevalence of hypertension in renal patients in Iran and the year of research using meta-regression
Figure 5.
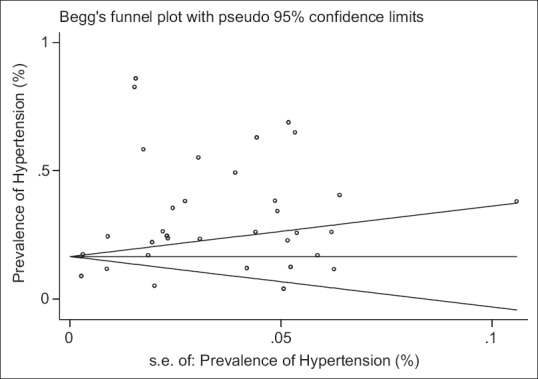
Meta-bias
Figure 6.
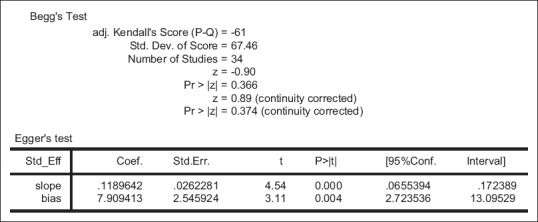
Beggs test and Eggers test to examine the significance of bias
In the study of Familoni et al., 53.2% of the subjects referred to hypertension as one of the causes of brain attack, renal failure, and cardiac failure.[88] In a study on patients in developed countries, 11.1% of the cause of chronic kidney disease was diabetes and 10.6% was high blood pressure.[89] According to studies in the United States, the most common causes of kidney failure are diabetes (50%), and both diabetes and high blood pressure (50–80%).[90] In a study in Pakistan in 1998–2001, high blood pressure (19.45%) and diabetes (19.67%) were identified as the most important causes of kidney failure.[91] In a study in Australia in 1997, hypertension (12%) was the most common cause of chronic renal failure.[92] In another study in Japan, this was reported as 6.2%.[93] In a Saudi study on renal patients, the prevalence of hypertension was reported to be 22.1%.[94]
Limitations of the study
Lack of uniform distribution of studies in different regions of Iran, different age groups, and different genders. Failure to report hypertension accurately in some studies.
Conclusions
The prevalence of hypertension in women with kidney disease is higher than men, and patients with kidney transplantation are at higher risk of hypertension than other renal patients. The prevalence of diastolic hypertension in renal patients is about five times higher than systolic blood pressure.
Ethical considerations
Ethical issues (including plagiarism, data fabrication, double publication) have been completely observed by the authors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mohsenzadeh Y, Motedayen M, Hemmati F, Sayehmiri K, Sarokhani M, Sarokhani D. Investigating the prevalence rate of hypertension in Iranian men and women: A study of systematic review and meta-analysis. J Bas Res Med Sci. 2017;4:53–62. [Google Scholar]
- 2.Motedayen M, Sarokhani D, Meysami A, Jouybari L, Sanagoo A, Hasanpour Dehkordi A. The prevalence of hypertension in diabetic patients in Iran; a systematic review and meta-analysis. J Nephropathol. 2018;7:137–44. [Google Scholar]
- 3.Von Elm E, Altman D, Egger M, Pocock S, Gotzsche P, Vandenbroucke J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 4.Ahmadi SM, Jalali A, Jalali R. Factors associated with the choice of peritoneal dialysis in Iran: Qualitative study. Open Access Macedonian J Medical Sciences. 2018;6:1253. doi: 10.3889/oamjms.2018.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rezaei Z, Jalali A, Jalali R, Khaledi-Paveh B. Psychological problems as the major cause of fatigue in clients undergoing hemodialysis: A qualitative study. International J Nursing Sciences. 2018;5:262–7. doi: 10.1016/j.ijnss.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalender B, Ozdemir A, Dervisoglu E, Ozdemir O. Quality of life in chronic kidney disease: Effects of treatment modality, depression, malnutrition and inflammation. International J Clinical Practice. 2007;61:569–76. doi: 10.1111/j.1742-1241.2006.01251.x. [DOI] [PubMed] [Google Scholar]
- 7.Noghabi AA, Zandi M, Mehran A, Alavian SM, Dehkordi AH. The effect of education on quality of life in patients under interferon therapy. Hepatitis Monthly. 2010;10:218. [PMC free article] [PubMed] [Google Scholar]
- 8.Cruz MC, Andrade C, Urrutia M, Draibe S, Nogueira-Martins LA, Sesso RdCC. Quality of life in patients with chronic kidney disease. Clinics. 2011;66:991–5. doi: 10.1590/S1807-59322011000600012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hasanpour AD. Influence of yoga and aerobics exercise on fatigue, pain and psychosocial status in patients with multiple sclerosis: A randomized trial. The J Sports Medicine and Physical Fitness. 2016;56:1417–22. [PubMed] [Google Scholar]
- 10.Series WTR. Hypertension control. Report of a WHO Expert Committee. 1996 [PubMed] [Google Scholar]
- 11.Burt V. Prevalence of hypertension in the US adult population: Results from the third National health and nutrition examination survey, 1988-1991. Hypertension. 1995;25:305–13. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 12.Damir Chi A, Mehrbani J. Prevalence of obesity, overweight and hypertension and their associated risk factors in adult males. Olympic J. 2009;17:87–103. [Google Scholar]
- 13.Dalvand S, Salehi Z, Asl MT, Zahednezhad H, Ebrahimi N, Nazari M, et al. An examination of factors effecting systolic blood pressure, diastolic blood pressure, and total cholesterol simultaneously using mixed responses model. Iranian Red Crescent Med J. 2017;19:e42309. [Google Scholar]
- 14.Akbari R, Bahadoram M, Ghorbani A, Zarghami A. Campaigning for kidney health; an experience from kidney day in Iran. Ann Res Dial. 2016;1:e02. [Google Scholar]
- 15.Gadhavi BP, Makwana AH, Mehta HB, Shah CJ, Gokhale PA. Early screening of hypertension and cardiac dysautonomia in each hypertensive is needed-inference from a study of QTc interval in Gujarat, India. Int J Prev Med. 2018;9:62. doi: 10.4103/ijpvm.IJPVM_423_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tamadon M. On the occasion of world kidney day 2018 with the theme of kidney disease in women; vitamin D deficiency and kidney diseases in women. J Renal Inj Prev. 2018;7:33–4. [Google Scholar]
- 17.Sadeghi M, Roohafza H, Kelishadi R. High blood pressure and associated cardiovascular risk factors in Iran: Isfahan Healthy Heart Programme. Med J Malaysia. 2004;59:460–7. [PubMed] [Google Scholar]
- 18.Rafiei M, Sayfi A. Distribution of blood pressure values in menopousal women in Arak population in 2007. Arak Univ Med Sci. 2006;12:47–56. [Google Scholar]
- 19.Delavari A, Horri N, Alikhani S, Guya M, Mahdavi A, Hoseini M, et al. Prevalence of hypertension in Iranian urban and rural populations aged over 20 years in 2004. J Mazandaran Univ Med Sci. 2007;17:79–86. [Google Scholar]
- 20.Refahi S, Shamsi A, Ebadi A, Saeeid Y, Moradi A. Comparison of military and civilian life style of people with hypertension. J Health Promot Manag. 2012;1:43–50. [Google Scholar]
- 21.Whitworth J. World Health Organization (WHO), International Society of Hypertension Writing Group (ISH). Statement on Management of Hypertension. J Hypertens. 2003;21:1983–92. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 23.Mahmoodnia L, Beigrezaei S. Chronic kidney disease and obesity; a mini-review to the current knowledge. J Nephropharmacol. 2017;6:30–2. [Google Scholar]
- 24.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. Jama. 2017;317:165–82. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 25.Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R. The effectiveness and cost -effectiveness of methods of storing donated kidneys from deceased donors: A systematic review and economic model. Health Technol Assess. 2009;13:1–156. doi: 10.3310/hta13380. [DOI] [PubMed] [Google Scholar]
- 26.Raiiesifar A, Torabpour M, Mohsenizad P. Causes of chronic renal failure in hemodialysis patients of Abadan. IJCCN. 2010;2:157–60. [Google Scholar]
- 27.Tayebi A, Raiesifar A, Ebadi A, Eynollahi B, Rafiyan Z, Keyvanloo F. Review the renal transplantation patients' quality of life by using kidney transplantation questionnaire (KTQ-25) J Crit Care Nurs. 2010;3:13–4. [Google Scholar]
- 28.Hasanpour- Dehkordi A. Kidneys and women's health, the theme of world kidney day 2018. J Negat Results Clin Exp Stud. 2018;1:e02. [Google Scholar]
- 29.Freedman BI, Langefeld CD, Andringa KK, Croker JA, Williams AH, Garner NE, et al. End-stage renal disease in African Americans with lupus nephritis is associated with APOL1. Arthritis and Rheumatology. 2014;66:390–6. doi: 10.1002/art.38220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wheeler DC, Winkelmayer WC. Improving, and G.Work, KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Kidney Int Suppl. 2017;7:1. doi: 10.1016/j.kisu.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wanner C, Lachin JM, Inzucchi SE, Fitchett D, Mattheus M, George J, et al. Empagliflozin and clinical outcomes in patients with type 2 diabetes mellitus, established cardiovascular disease, and chronic kidney disease. Circulation. 2018;137:119–29. doi: 10.1161/CIRCULATIONAHA.117.028268. [DOI] [PubMed] [Google Scholar]
- 32.Sayin A, Mutluay R, Sindel S. Quality of life in hemodialysis, peritoneal dialysis, and transplantation patients. Transplant Proc. 2007;39:3047–53. doi: 10.1016/j.transproceed.2007.09.030. [DOI] [PubMed] [Google Scholar]
- 33.Eryilmaz M, Ozdemir C, Yurtman F, Cilli A, Karaman T. Quality of sleep and quality of life in renal transplantation patients. Transplant Proc. 2005;37:2072–6. doi: 10.1016/j.transproceed.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 34.Ghaffari A. Seminar of kidney transplantation report. Biomed Eng. 2008;6:73. [Google Scholar]
- 35.Nasri H. Trends toward amelioration of renal inflammation and fibrosis in various kidney diseases. J Inj Inflamm. 2016;1:e02. [Google Scholar]
- 36.Jay CL, Dean PG, Helmick RA, Stegall MD. Reassessing preemptive kidney transplantation in the United States: Are we making progress? Transplantation. 2016;100:1120. doi: 10.1097/TP.0000000000000944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith JM, Martz K, Blydt-Hansen TD. Pediatric kidney transplant practice patterns and outcome benchmarks, 1987–2010: A report of the North American Pediatric Renal Trials and Collaborative Studies. Pediatric Transplantation. 2013;17:149–57. doi: 10.1111/petr.12034. [DOI] [PubMed] [Google Scholar]
- 38.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prevention CfDCa. National Chronic Kidney Disease Fact Sheet. 2014 [Google Scholar]
- 40.Vendemia F, Amico G. Antihypertensive therapy in dialysed patients. Contrib Nephrol. 1988;61:161–70. doi: 10.1159/000415247. [DOI] [PubMed] [Google Scholar]
- 41.Jha V, Garcia Garcia G, Iseki K, Li Z, Naicker S, Plattner B, et al. Chronic kidney disease: Global dimension and perspectives. Lancet. 2013;382:260–72. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 42.Ezeonwu B, Nwafor I, Nnodim I, Ayodeji A, Ajaegbu O, Maduemem E, et al. Risk factors for chronic kidney disease in children attending pediatric outpatient clinic in federal medical center Asaba. J Prev Epidemiol. 2016;1:e10. [Google Scholar]
- 43.Lala M, Nazar C, Lala H, Singh J. Interrelation between blood pressure and diabetes. J Ren Endocrinol. 2015;1:e05. [Google Scholar]
- 44.Oluyombo R, Olamoyegun M, Ayodele O, Akinwusi P, Akinsola A. Clustering of chronic kidney disease and cardiovascular risk factors in South-West Nigeria. J Nephropathol. 2017;6:196–203. doi: 10.15171/jnp.2017.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Navaneethan SD, Schold JD, Jolly SE, Arrigain S, Winkelmayer WC, Nally JV., Jr Diabetes control and the risks of ESRD and mortality in patients with CKD. American J Kidney Diseases. 2017;70:191–8. doi: 10.1053/j.ajkd.2016.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: A systematic review. The Lancet. 2015;385:1975–82. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 47.Bah A, Lamine C, Balde M, Bah M, Rostaing L. Epidemiology of chronic kidney diseases in the Republic of Guinea; future dialysis needs. J Nephropathol. 2015;4:127–33. doi: 10.12860/jnp.2015.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Targher G, Bertolini L, Chonchol M, Rodella S, Zoppini G, Lippi G, et al. Non-alcoholic fatty liver disease is independently associatedwith an increased prevalence of chronic kidney diseaseand retinopathy in type 1 diabetic patients. Diabetologia. 2010;53:1341–8. doi: 10.1007/s00125-010-1720-1. [DOI] [PubMed] [Google Scholar]
- 49.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev J. 2015;4:1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barahimi H, Aghighi M, Aghayani K, Rahimi Foroushani A. Chronic kidney disease management program in Shahreza. Iran J Kidney Dis. 2014;8:450–6. [PubMed] [Google Scholar]
- 51.Fazelzadeh A, Mehdizadeh A, Ostovan M, Raiss Jalali G. Incidence of cardiovascular risk factors and complications before and after kidney transplantation. Transplant Proc. 2006;38:506–8. doi: 10.1016/j.transproceed.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 52.Bashardoost B, Adib A, Faaalpoor Z, Gavami Nashr M. The study of hypertension relationship with weight gain in patients hemodialysis intervals. J Ardabil Univ Med Sci. 2007;7:22–6. [Google Scholar]
- 53.Hasanzamani B, Zeraati A, Sharifpour F, Paeizi R. Prevalence of hypertension in hemodialisis versus peritoneal patients. Iran J Kidney Dis. 2011;5:53. [Google Scholar]
- 54.Pourmand G, Dehghani S, Rahmati M, Mehrsai A, Gooran S, Alizadeh F, et al. Does hypertension remain after kidney transplantation? Acta Med Iran. 2015;53:297–300. [PubMed] [Google Scholar]
- 55.Basiratnia M, Esteghamati M, Ajami G, Amoozgar H, Cheriki C, Soltani M, et al. Blood pressure profile in renal transplant recipients and its relation to diastolic function: Tissue Doppler echocardiographic study. Pediatr Nephrol. 2011;26:449–57. doi: 10.1007/s00467-010-1724-6. [DOI] [PubMed] [Google Scholar]
- 56.Shamsa A, Motavalli M, Aghdam B. Erectile function in end-stage renal disease before and after renal transplantation. Transplant Proc. 2005;37:3087–9. doi: 10.1016/j.transproceed.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 57.Hollisaaz M, Aghanassir M, Lorgard Dezfuli Nezad M, Assari S, Hafezie R, Ebrahiminia M. Medical comorbidities after renal transplantation. Transplant Proc. 2007;39:1048–50. doi: 10.1016/j.transproceed.2007.03.061. [DOI] [PubMed] [Google Scholar]
- 58.Nikoobakht M, Mahboobi A, Saraji A, Mehrsai A, Emamzadeh A, Mahmoudi M. Pelvic nerve neuropathy after kidney transplantation. Transplant Proc. 2007;39:1108–10. doi: 10.1016/j.transproceed.2007.03.085. [DOI] [PubMed] [Google Scholar]
- 59.Noshad H, Ardalan M, Mortazavi M, Tayebi H, Safa J, Nezami N. Kidney transplantation candidates and cardiovascular risk factors. Transplant Proc. 2007;39:871–4. doi: 10.1016/j.transproceed.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 60.Rostami Z, Shafighi N, Baghersad M, Einollahi B. Risk factors for immediate anemia in renal transplant recipients: A single-center experience. Transplant Proc. 2011;43:581–3. doi: 10.1016/j.transproceed.2011.01.072. [DOI] [PubMed] [Google Scholar]
- 61.Pakfetrata M, Roozbeha J, Nikooc M, Asemb Z, Malekmakanb L, Nikood M. Common echocardiography findings in pretransplant dialysis patients and their associations. Hong Kong J Nephrol. 2013;15:68–74. [Google Scholar]
- 62.Rezaei Ghalechi E, Kazemi R, Hagh Kerdar M. The evaluation of prevalence of depression in hemodialysis patients in north west of Iran. Eur Psychiatry. 2013;28:1–4. [Google Scholar]
- 63.Nobakht Haghighi A, Malakoutian T, Radfar M, Abdi E, Kamgar M, Broumand B, et al. A4-year follow-up of living unrelated donors of kidney allograft in Iran. Iran J Kidney Dis. 2015;9:273–8. [PubMed] [Google Scholar]
- 64.Rohani M, AghaeI M, Jenabi A, Yazdanfar S, Mousavi D, Miri S. Restless legs syndrome in hemodialysis patients in Iran. Neurol Sci. 2015;36:723–7. doi: 10.1007/s10072-014-2026-8. [DOI] [PubMed] [Google Scholar]
- 65.Najafi I, Alatab S, Atabak S, Nouri Majelan N, Sanadgol H, Makhdoomi K, et al. Seventeen years' experience of peritoneal dialysis in Iran: First official report of the Iranian peritoneal dialysis registry. Perit Dial Int. 2014;34:636–42. doi: 10.3747/pdi.2012.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gheissari A, Hemmatzadeh S, Merrikhi A, Fadaei Tehrani S, Madihi Y. Chronic kidney disease in children: A report from a tertiary care center over 11 years. J Nephropathol. 2012;1:177–82. doi: 10.5812/nephropathol.8119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jalalzadeh M, Mohammadi R, Mirzamohammadi F, Ghadiani M. Prevalence of metabolic syndrome in a hemodialysis population. Iran J Kidney Dis. 2011;5:248–54. [PubMed] [Google Scholar]
- 68.Nemati E, Ghanbrpour F, Taheri S, Einollahi B. Prevalence of hypertension among Iranian hemodialysis patients and risk factors: A nationwide multicenter study. J Biol Sci. 2008;11:910–4. doi: 10.3923/pjbs.2008.910.914. [DOI] [PubMed] [Google Scholar]
- 69.Safarinejad M. The epidemiology of adult chronic kidney disease in a population-based study in Iran: Prevalence and associated risk factors. J Nephrol. 2009;22:99–108. [PubMed] [Google Scholar]
- 70.Ayazi K, Atabak S, Saghebi R, Ayazi S, Aryasepehr S. Evaluation of efficacy, survival rate and comlications of pert] itoneal catheter placement of patients with end – Stage renal disease. Saudi Med J. 2005;26:1391–3. [PubMed] [Google Scholar]
- 71.Nakhjavani M, Esfahanian F, Safavi M, Kalbasi Anaraki M, Zohrevand P. Prevalence of diabetic patients among under-Hemodialysis patients In ten hemodialysis centers of Tehran. Iran J Diabetes Metab (ijdld) 2004;4:39–46. [Google Scholar]
- 72.Barzin M, Tazikie O, Pezeshki M. Incidence of renal osteodytrophy in hemodialysis patients of fateme-Zahra hospital in Sari in 1998. J Mazandaran Univ Med Sci. 2001;11:31–7. [Google Scholar]
- 73.Monfared A, Khosravi M, Orang poor R, Moosavian Roshan Zamir S, Aghajani Nargesi D. Reasons of chronic renal failure in hemodialysis patients in Guilan Province. J Guilan Univ Med Sci. 2003;12:76–83. [Google Scholar]
- 74.Shasti S, Babahaji M. The assessment of dialysis adequacy among hemodialysis patients in Tehran City. EBNESINA- Journal of Medical. 2011;14:23–7. [Google Scholar]
- 75.Raiisifar A, Tayyebi A, Ebadi A, Najafi S, Hashemi S, Asiyabi M. An investigation of quality of life in kidney transplant patients. Iran J Crit Care Nurs. 2011;4:149–52. [Google Scholar]
- 76.Ghafourifard M, Rafieian M, Shahgholian N, Mortazavi M. Effect of sodium dialysate variation in combining with ultra filtration on intradialytic hypotension and intradialytic weight gain for patients on hemodialysis. J Mazandaran Univ Med Sci. 2009;19:19–26. [Google Scholar]
- 77.Heidari B. The etiology of kidney failure in hemodialysis patient in Mazandaran Mazandaran. Univ Med Sci J. 2001;11:43–71. [Google Scholar]
- 78.Mogharab M, Rezaee N, Tahouri F, Taheri P, Jani H. Complications during hemodialysis in chronic hemodialysis patients using dialysis buffer solution with sodium acetate and sodium bicarbonate. Mod Care J. 2007;4:21–8. [Google Scholar]
- 79.Eslami Amirabadi M, Hosein D, Nasrollahi A, Norouzian M, Bozorg B, Amjadi Kivi SM, et al. Cognitive dysfunction in hemodialysis patients and its related factors. Res Med. 2014;38:53–9. [Google Scholar]
- 80.Rahimian M, Hasan Zadeh A, Sami R. The effects of erythropoietin in the management of anemia of chronic renal failure in patients on hemodialysis. JSSU. 2005;13:12–5. [Google Scholar]
- 81.Ghorbani Moghadam Z, Sharifi S. The frequency of underlying conditions for chronic renal failure in patients undergoing dialysis in Shohada Hospital in Bushehr. Nurs J Vulnerable. 2015;2:46–54. [Google Scholar]
- 82.Hadian B, Anbari K, Heidari R. Epidemiologic study of end stage renal disease and related risk factors in patients under hemodialysis in Lorestan province. Yafte. 2014;16:44–53. [Google Scholar]
- 83.Rezaeian Langroodi R. Evaluation of risk factors for chronic renal failure in hemodialysis patients referring to hospitals affiliated to Hamedan University of Medical Sciences. Aflak Q J. 2008;7:13–9. [Google Scholar]
- 84.KhademVatan K, Rahmani A, Ghasemi S, Ahangary H, Mehrpooya M. Evaluation of the efective risk faktors for peripheral vascular disease in hemodialysis patients. J Urmia Nurs Midwifery Fac. 2014;12:585–90. [Google Scholar]
- 85.Ebadi P, Shamsi A, Refahi A, Saied Y. Comparison of the Quality of Life in Men with and Without Hypertension. Sci J Hamadan Nurs Midwifery. 2010;20:5–15. [Google Scholar]
- 86.Rocco M, Yan G, Heyka R, Benz R, Cheung A. Risk factors for hypertension in chronic hemodialysis patients: Baseline data from the HEMO study. Am J Nephrol. 2001;21:280–8. doi: 10.1159/000046262. [DOI] [PubMed] [Google Scholar]
- 87.Malekmakan L, Haghpanah S, Pakfetrat M, Malekmakan A, Khajehdehi P. Causes of chronic renal failure among Iranian hemodialysis patients. Saudi J Kidney Dis Transpl. 2009;20:501–4. [PubMed] [Google Scholar]
- 88.Familoni B, Ogun S, Aina A. Knowledge and awareness of hypertension among patients with hypertension. J Natl Med Assoc. 2004;96:620–4. [PMC free article] [PubMed] [Google Scholar]
- 89.Snouber S, Khader M, Alkhatib A, Nazzal Z, Dudin A. Prevalence of patients with end-stage renal disease on dialysis in the West Bank. Saudi J Kidney Dis Transpl. 2013;24:832–7. doi: 10.4103/1319-2442.113913. [DOI] [PubMed] [Google Scholar]
- 90.Goretti M, Janeza T, Croatia R, et al. Special problems in Hemodialysis patients. 2011:123–6. [Google Scholar]
- 91.Adibul A, Rizvi K. Causes of chronic renal failure in Pakistan: A single large center experience. Saudi Kidney Dis Transplant Proc. 2002;13:376–9. [PubMed] [Google Scholar]
- 92.Disney A, Russ G, Walker R, al e. Australia and New Zealand Dialysis and Transplant Registry. Kidney Int. 1998;62:2281–7. [Google Scholar]
- 93.Shinzato T, Nakai S, Akiba T, Yamazaki C, Sasaki R, Kitaoka T, et al. Current status of renal replacement therapy in Japan: Results of the annual survey of the Japanese Society for Dialysis Therapy in 1996. Kidney Int. 1999;55:700–12. doi: 10.1093/oxfordjournals.ndt.a027128. [DOI] [PubMed] [Google Scholar]
- 94.Faissal A, Shaheen N. Pre end stage renal failure: The Jeddah kidney center experience. Saudi Kidney Dis Transplant. 2002;13:371–5. [PubMed] [Google Scholar]