Abstract
Background
Older adults aged 65 and over will make up more than 20% of U.S. residents by 2030, and in 2050, this population will reach 83.7 million. Depression among older adults is a major public health concern projected to be the second leading cause of disease burden. Despite having Medicare, and other employer supplements, the burden of out of pocket healthcare expenses may be an important predictor of depression. The current study aims to investigate whether delay in seeing a doctor when needed but could not because of medical cost is significantly associated with symptoms of current depression in older adults.
Methods
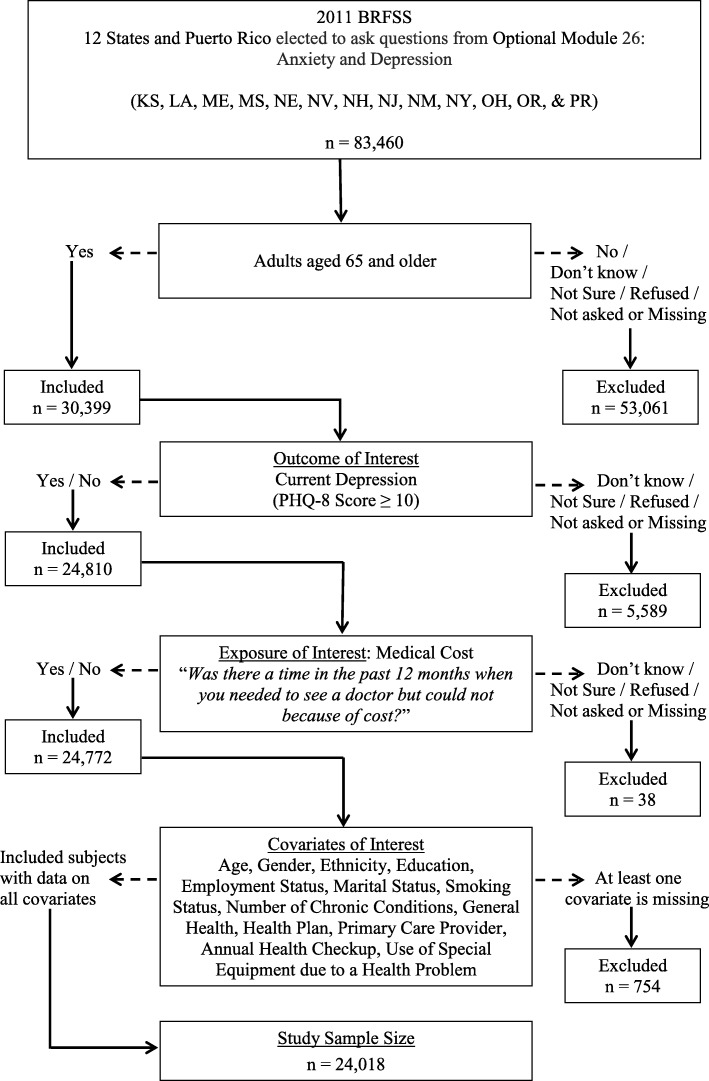
Cross-sectional data from the 2011 Behavioral Risk Factor Surveillance System (BFRSS) from 12 states and Puerto Rico were used for this study (n = 24,018).
Results
The prevalence of symptoms of current depression among older adults who reported medical cost as a barrier to seeking health care was significantly higher (17.8%) when compared to older adults who reported medical cost not being a barrier to seeking health care (5.5%). Older adults who reported medical cost as a barrier to seeking health care were more likely to report current depressive symptoms compared to their counterparts [Adjusted Odds Ratio (AOR): 2.2 [95% CI: 1.5–3.3]).
Conclusions
Older adults (≥ 65 years of age) who experience the burden of medical cost for health care are significantly more likely to report symptoms of depression. Health care professionals and policymakers should consider effective interventions to improve access to health care among older adults.
Electronic supplementary material
The online version of this article (10.1186/s12877-019-1203-2) contains supplementary material, which is available to authorized users.
Keywords: Medical cost, Out-of-pocket expenses, Depression, Current depressive symptoms, BRFSS
Background
The rapid aging of the United States population is due, in part; to the increase in life expectancy and the aging of the post-World War II baby boom generation [1]. By 2030, older adults aged 65 and over will make up more than 20% of U.S. residents, and by 2050, this population will reach 83.7 million, almost double the 2012 estimated population of 43.1 million [1, 2]. Older adults are disproportionately affected by chronic conditions with approximately 60% living with at least one chronic condition and 42% with at least two chronic conditions [3]. Access to health services is essential for prevention and management of chronic illnesses to minimize the disease burden and associated health care costs. The overarching goal of Healthy People 2020 is to improve the health, function, and quality of life of older adults, which includes an objective to increase the proportion of older adults who are up to date on a core set of clinical preventive health services for maintaining quality of life and overall wellness [4].
Depression is a serious problem and a major public health concern among older adults [5, 6]. The prevalence of depression among community dwelling adults aged 65 and older is estimated to be between 5 and 10% and is projected to be the second leading cause of disease burden in this population by the year 2020 [7, 8]. Risk factors for depression such as chronic diseases [9], disability [10, 11], lack of social support, and socio-economic status [12–14], have been well documented. Given that aging is associated with multiple chronic health conditions and limited financial resources for disease management, and despite the availability of Medicare, Medicaid and employer supplements [15–19], the burden of out of pocket healthcare expenses may be an important predictor of depression.
Although several studies have documented the risk factors for depression in the elderly [9, 10, 12–14], and while others have examined the impact of depression on healthcare costs [20–22], to the best of our knowledge, out of pocket healthcare expenses (e.g., delay in seeing a doctor when needed but could not because of medical cost) as a predictor of current depressive symptomatology in a nationally representative sample of community-dwelling older adults in the U.S. has not been documented yet. Previous reported research on the association between financial strain and depressive symptoms among older adults focused on financial strain measured by a 4-item scale and was not specific to financial strain due to the burden of out of pocket healthcare expenses [23, 24]. As such, the purpose of this study is to:
estimate the prevalence of current depressive symptoms in a sample of community dwelling older adults (≥ 65 years of age) who reported a delay in seeing a doctor when needed but could not because of medical cost,
investigate whether delay in seeing a doctor when needed but could not because of medical cost is significantly associated with symptoms of current depression in the elderly after accounting for possible potential confounders, and.
describe the socio-demographic characteristics of older adults who are more likely to report delay in seeing a doctor when needed but could not because of medical cost.
This current study is motivated by “The theory of cost-sharing” framework. Cost-sharing is any kind of out-of-pocket expenses made by individuals for health care services. It may result in individuals’ delaying a follow-up health care visit or completely wait out a health problem [25, 26]. Therefore, we sought to understand the relationship between cost-sharing, as defined by medical cost as a barrier to seeking health care, on symptoms of current depression which is an important health outcome.
Methods
General study design
The Behavioral Risk Factor and Surveillance System (BRFSS) is a federally funded telephone survey designed and conducted annually by the Centers for Disease Control and Prevention (CDC) in collaboration with state health departments in all 50 states, Washington, DC; Puerto Rico; the U.S. Virgin Islands; and Guam. The survey collects data on health conditions, preventive health practices, and risk behaviors of the adults selected [27]. All BRFSS questionnaires, data, and reports are available at http://www.cdc.gov/brfss/. Data for this study were obtained from 12 states (Kansas, Louisiana, Maine, Mississippi, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, Ohio, and Oregon) and Puerto Rico that administered the ‘Anxiety and Depression’ optional module in the 2011 BRFSS data. The weighted response rates ranged from 33.4 to 61.7%.
Delay in seeing a doctor due to cost: primary exposure of interest
To determine if cost is a barrier to seeking health care among older adults, responses to the following question: “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost? ” were used to create a binary exposure variable (Yes / No).
Current depressive symptoms: primary outcome of interest
Current depressive symptomatology is defined based on the responses to the eight-item Patient Health Questionnaire (PHQ-8) depression scale [28]. The scores for each item, which range from 0 to 3, are summed to produce a total score between 0 and 24 points. Symptoms of current depression is defined as PHQ-8 score ≥ 10 [25]. The PHQ-8 consists of eight of the nine DSM-IV criteria for depressive disorders [29, 30].
Covariates of interest
Socio-demographic variables: age, gender (male, female), race/ethnicity (White non-Hispanic, African American non-Hispanic, Hispanic, Others), marital status (married, unmarried), education (less than college, college graduate), and employment (employed, unemployed); Health indicators: general health (“Excellent / Very good / Good” or “Fair / Poor”), use of special equipment due to a health problem (Yes / No), smoking (Yes / No), and number of chronic conditions other than current depression; and Health care indicators: having a health plan (Yes / No), having a primary care provider (Yes / No), and having an annual checkup (Yes / No), were considered as covariates of interest in this study.
Statistical analyses
Sampling weights provided in the 2011 BRFSS public-use data that adjust for unequal selection probabilities, survey non-response, and oversampling were used to account for the complex sampling design and to obtain population-based estimates that reflect U.S. non-institutionalized individuals. In order to describe the characteristics of the study population, weighted prevalence estimates, and corresponding 95% confidence intervals (CI) were computed based on the sample of individuals (n = 24,018) with complete data on all variables considered in this study (Fig. 1). Logistic regression models were used to examine if delay in seeing a doctor when needed but could not because of medical cost is significantly associated with symptoms of current depression in the elderly, adjusting for potential confounders and other covariates.
Fig. 1.
Flowchart of Study Population and Sample Size
All analyses were conducted in SAS 9.3 (SAS Institute, Cary, NC, USA) using SAS survey procedures (PROC SURVEYFREQ, PROC SURVEYMEANS, PROC SURVEYLOGISTIC) to account for the complex sampling design.
Results
Sample characteristics
In 2011, the prevalence of current depressive symptoms among U.S. older adults from the 12 states and Puerto Rico was 6.1% (95% CI: 5.3–7.0%). About 6 % (5.7, 95% CI: 4.9–6.6%) reported medical cost as a barrier to seeking health care when needed in the past 12 months. Table 1 describes the overall characteristics of older adults, the weighted prevalence of reporting medical cost as a barrier to seeking health care and the weighted prevalence of current depressive symptoms along with the corresponding 95% confidence intervals. The average age of older adults at the time of survey was 74.1 years [95% CI: 73.9–74.4]. The majority of these adults were females (56.3%), White Non-Hispanic (77.5%), and more than three-fourth of them were either retired or unable to work. A little less than half of the older adults were unmarried (48.3%), and had more than high school education (44.6%). A little over one-fourth of the older adults reported “fair/poor” general health (28.8%), almost 80% of them had at least one chronic condition other than current depression, were predominantly non-smokers (91.2%), and did not use any special equipment due to a health problem (81.0%). The majority of older adults in the 12 states and Puerto Rico reported having a health plan (97.9%), having a primary care provider (94.7%), and having an annual health checkup (87.1%).
Table 1.
Characteristics of Adults Aged 65 and Older (n = 24,018)
| Unweighted n | Overall Mean or Proportion (95% CI) |
Yes, Medical Cost a Barrier to Health Carea Mean or Proportion (95% CI) |
Current Depressive Symptoms (PHQ-8 Score ≥ 10) Mean or Proportion (95% CI) |
||||
|---|---|---|---|---|---|---|---|
| Socio-demographics | |||||||
| Age in years | 24018 | 74.1 | (73.9–74.4) | 73.0 | (72.1–74.0) | 73.8 | (72.2–75.4) |
| Gender | |||||||
| Male | 8457 | 43.7 | (42.0–45.4) | 4.7 | (3.5–5.8) | 4.6 | (3.6–5.6) |
| Female | 15561 | 56.3 | (54.6–57.9) | 6.5 | (5.3–7.7) | 7.4 | (6.1–8.6) |
| Ethnicity | |||||||
| White Non-Hispanic | 20135 | 77.5 | (76.0–79.0) | 4.3 | (3.5–5.2) | 5.6 | (4.7–6.4) |
| Black Non-Hispanic | 1479 | 7.7 | (6.7–8.7) | 10.1 | (6.6–13.6) | 5.1 | (2.9–7.3) |
| Hispanic | 1785 | 11.9 | (10.8–13.1) | 11.7 | (8.0–15.3) | 11.0 | (7.4–14.6) |
| Othersb | 619 | 2.9 | (2.2–3.5) | 6.3 | (3.7–8.9) | 4.8 | (1.8–7.9) |
| Marital Status | |||||||
| Married | 11330 | 51.7 | (50.1–53.4) | 4.7 | (3.6–5.8) | 5.0 | (4.0–6.0) |
| Unmarriedc | 12688 | 48.3 | (46.6–49.9) | 6.8 | (5.5–8.1) | 7.4 | (6.0–8.8) |
| Education | |||||||
| Elementary/Some High School/High School Graduate | 11359 | 55.4 | (53.8–57.0) | 7.2 | (5.9–8.5) | 7.0 | (5.7–8.3) |
| Some College or Technical School/College graduate | 12659 | 44.6 | (43.0–46.2) | 3.9 | (2.9–4.8) | 5.1 | (4.1–6.1) |
| Employment | |||||||
| Employed | 3520 | 13.6 | (12.4–14.7) | 4.9 | (2.9–6.8) | 5.4 | (2.3–8.5) |
| Unemployedd | 20498 | 86.4 | (85.3–87.6) | 5.9 | (4.9–6.8) | 6.3 | (5.4–7.1) |
| Health Indicators | |||||||
| General Health | |||||||
| Excellent/Very Good/Good | 17903 | 71.2 | (69.6–72.7) | 3.8 | (3.0–4.7) | 2.8 | (2.1–3.6) |
| Fair/Poor | 6115 | 28.8 | (27.3–30.4) | 10.4 | (8.4–12.4) | 14.3 | (12.1–16.6) |
| Number of Chronic Conditions | |||||||
| 0 | 5123 | 20.9 | (19.6–22.2) | 3.8 | (2.4–5.2) | 2.8 | (1.6–3.9) |
| 1 | 7673 | 30.7 | (29.2–32.2) | 5.1 | (3.8–6.4) | 4.1 | (2.6–5.6) |
| 2 | 5719 | 24.4 | (23.0–25.9) | 5.7 | (3.9–7.5) | 6.4 | (4.7–8.1) |
| ≥ 3 | 5503 | 23.9 | (22.4–25.4) | 8.2 | (6.0–10.4) | 11.5 | (9.4–13.7) |
| Smoking | |||||||
| Yes | 2103 | 8.8 | (7.8–9.7) | 11.3 | (6.1–16.4) | 10.8 | (6.5–15.0) |
| No | 21915 | 91.2 | (90.3–92.2) | 5.2 | (4.4–5.9) | 5.7 | (5.0–6.5) |
| Use of Special Equipment due to a Health Problem | |||||||
| Yes | 4531 | 19.0 | (17.7–20.2) | 10.0 | (7.4–12.4) | 15.5 | (12.8–18.1) |
| No | 19487 | 81.0 | (79.8–82.3) | 4.7 | (3.9–5.6) | 4.0 | (3.2–4.8) |
| Health Care Indicators | |||||||
| Have a Health Plan | |||||||
| Yes | 23626 | 97.9 | (97.2–98.5) | 5.2 | (4.4–6.0) | 6.2 | (5.4–7.1) |
| No | 382 | 2.1 | (1.5–2.8) | 27.3 | (13.1–41.5) | 3.3 | (1.5–5.1) |
| Have a Primary Care Provider | |||||||
| Yes | 22726 | 94.7 | (93.9–95.5) | 5.4 | (4.5–6.2) | 6.2 | (5.3–7.0) |
| No | 1292 | 5.3 | (4.5–6.1) | 11.8 | (6.9–16.6) | 6.0 | (3.1–8.7) |
| Annual Health Checkup | |||||||
| Yes | 20255 | 87.1 | (86.0–88.1) | 4.9 | (4.1–5.7) | 6.1 | (5.2–6.9) |
| No | 3763 | 12.9 | (11.8–14.0) | 11.4 | (7.8–15.1) | 6.6 | (3.8–9.5) |
a Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?
b Includes non-Hispanic Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaskan Native only, Multiracial and other race only
c Includes Divorced, Widowed, Separated, Never Married, and Member of an unmarried couple
d Includes Homemaker, Student, Retired, Unable to Work, and Out of work
Significant sub-groups of older adults with medical cost as a barrier to seeking health care
Among the different covariates examined for significant differences in the proportion of older adults who reported medical cost as a barrier to seeking health care when needed in the past 12 months, the following sub-groups of individuals were significantly higher in proportion to report medical cost as a barrier to seeking health care compared to some of the older adults who reported medical cost not being a barrier to seeking health care: i) Hispanics vs. White non-Hispanics (11.7% vs. 4.3%); ii) Black non-Hispanics vs. White non-Hispanics (10.1% vs. 4.3%); iii) older adults with no college education vs. those with some college education (7.2% vs. 3.9%); iv) those who reported “Fair/Poor” general health vs. those with “Excellent/Very Good/Good” general health (10.4% vs. 3.8%); v) those with 3 or more chronic conditions other than current depression vs. those with no chronic conditions (8.2% vs. 3.8%); vi) smokers vs non-smokers (11.3% vs. 5.2%); vii) those who reported use of special equipment due to a health condition vs. those who did not use (10.0% vs. 4.7%); viii) those with no health plan vs. those with a health plan (27.3% vs. 5.2%); ix) those with no primary care provider vs. those with a primary care provider (11.8% vs. 5.4%); and x) those who reported not having an annual health checkup vs. those who did (11.4% vs. 4.9%). There was no significant difference in the average age of older adults who reported medical cost as a barrier to seeking health care when compared to those who did not report medical cost as a barrier (73.0 years vs. 74.2 years).
Significant sub-groups of older adults with current depressive symptoms
Females were significantly higher in proportion to report symptoms of current depression compared to males (7.4% vs. 4.6%). Among the sub-groups of individuals who reported medical cost as a barrier to seeking health care, the following also reported symptoms of current depression: i) Hispanics vs. White non-Hispanics (11.0% vs. 5.6%); ii) those who reported “Fair/Poor” general health vs. those with “Excellent/Very Good/Good” general health (14.3% vs. 2.8%); iii) those with 3 or more chronic conditions other than current depression vs. those with no chronic conditions (11.5% vs. 2.8%); iv) smokers vs non-smokers (10.8% vs. 5.7%); and v) those who reported use of special equipment due to a health condition vs. those who did not use (15.5% vs. 4.0%). Interestingly, older adults with a health plan were significantly higher in proportion for symptoms of current depression compared to those without a health plan (6.2% vs. 3.3%). Average age between individuals with and without symptoms of current depression was not significant (73.8 years vs. 74.1 years).
Model based odds ratios for symptoms of current depression
The prevalence of symptoms of current depression among older adults who reported medical cost as a barrier to seeking health care was significantly higher [17.8, 95% CI: (11.4–21.1%)] when compared to older adults who reported medical cost not being a barrier to seeking health care [5.5, 95% CI: (4.7–6.2%)]. After adjusting for all covariates of interest, older adults who reported medical cost as a barrier to seeking health care were more than twice likely to report current depressive symptoms compared to older adults who reported medical cost not being a barrier to seeking health care (Adjusted Odds Ratio (AOR): 2.2 [95% CI: 1.5–3.3]) (Table 2). Additional file 1: Table S1 provides additional details on possible potential confounders we adjusted for in determining the association between medical cost as a barrier to seeking health care and current depressive symptoms in older adults.
Table 2.
Prevalence of and Estimated Odds Ratio (95% CI) for Current Depressive Symptoms (PHQ-8 Score ≥ 10)
| Unweighted n | % (95% CI) | UOR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Was there a time in the past 12 months when you needed to see a doctor but could not because of cost? | ||||
| Yes | 1062 | 17.8 (11.4–24.1) | 3.7 (2.4–5.9) | 2.2 (1.5–3.3) |
| No | 22956 | 5.5 (4.7–6.2) | Reference | Reference |
%: Prevalence, UOR Unadjusted Odds Ratio
AOR Adjusted Odds Ratio. Adjusted for age, gender, ethnicity, marital status, education, employment, number of chronic conditions, smoking, general health status, having a health plan, having a primary care provider, annual health checkup, and use of special equipment due to a health problem
Predictors of reporting medical cost as a barrier to seeking health care
According to the adjusted logistic regression model results, gender (females: AOR: 1.52 [95% CI: 1.07–2.17]), ethnicity (Black non-Hispanics: AOR: 1.79 [95% CI: 1.09–2.96]; Hispanics: AOR: 2.48 [95% CI: 1.53–4.02]), education (less than college education: AOR: 1.49 [95% CI: 1.05–2.10]), general health (“Fair / Poor”: AOR: 2.12 [95% CI: 1.42–3.17]), smoking status (smokers: AOR: 1.72 [95% CI: 1.07–2.76]), having a health plan (No: AOR: 5.44 [95% CI: 2.67–11.09]), getting an annual checkup (No: AOR: 2.82 [95% CI: 1.91–4.17]), and use of special equipment due to a health problem (Yes: AOR: 1.64 [95% CI: 1.13–2.39]) were significant predictors of reporting medical cost as a barrier to seeking health care (Table 3).
Table 3.
Predictors of Reporting Medical Cost as a Barrier to Seeking Health Care among Adults Aged 65 and Older (n = 24,018)
| Unadjusted Odds Ratio (UOR) and 95% CI for Medical Cost as a Barrier to Seeking Health Care | Adjusted Odds Ratio (AOR) and 95% CI for Medical Cost as a Barrier to Seeking Health Care | |||
|---|---|---|---|---|
| Socio-demographics | ||||
| Age in years | 0.98 | (0.96–1.00) | 0.97 | (0.95–1.00) |
| Gender | ||||
| Male | Reference | Reference | ||
| Female | 1.43 | (1.04–1.97) | 1.52 | (1.07–2.17) |
| Ethnicity | ||||
| White Non-Hispanic | Reference | Reference | ||
| Black Non-Hispanic | 2.48 | (1.60–3.83) | 1.79 | (1.09–2.96) |
| Hispanic | 2.91 | (1.94–4.36) | 2.48 | (1.54–4.02) |
| Othersa | 1.48 | (0.89–2.47) | 1.37 | (0.82–2.30) |
| Marital Status | ||||
| Married | Reference | Reference | ||
| Unmarriedb | 1.46 | (1.07–2.01) | 1.10 | (0.77–1.56) |
| Education | ||||
| Some College or Technical School/College Graduate | Reference | Reference | ||
| Elementary/Some High School/High School Graduate | 1.92 | (1.39–2.65) | 1.49 | (1.05–2.10) |
| Employment | ||||
| Employed | Reference | Reference | ||
| Unemployedc | 1.21 | (0.77–1.92) | 0.92 | (0.60–1.41) |
| Health Indicators | ||||
| General Health | ||||
| Excellent / Very Good / Good | Reference | Reference | ||
| Fair / Poor | 2.92 | (2.12–4.01) | 2.12 | (1.42–3.17) |
| Number of Chronic Conditions | ||||
| 0 | Reference | Reference | ||
| 1 | 1.35 | (0.85–2.16) | 1.36 | (0.81–2.28) |
| 2 | 1.52 | (0.92–2.54) | 1.35 | (0.70–2.61) |
| ≥ 3 | 2.24 | (1.38–3.64) | 1.68 | (0.92–3.07) |
| Smoking | ||||
| No | Reference | Reference | ||
| Yes | 2.33 | (1.36–3.99) | 1.72 | (1.07–2.76) |
| Use of Special Equipment due to a Health Problem | ||||
| No | Reference | Reference | ||
| Yes | 2.21 | (1.58–3.09) | 1.64 | (1.13–2.39) |
| Health Care Indicators | ||||
| Have a Health Plan | ||||
| Yes | Reference | Reference | ||
| No | 6.79 | (3.34–13.82) | 5.44 | (2.67–11.09) |
| Have a Primary Care Provider | ||||
| Yes | Reference | Reference | ||
| No | 2.34 | (1.44–3.83)) | 1.17 | (0.72–1.88) |
| Annual Health Checkup | ||||
| Yes | Reference | Reference | ||
| No | 2.53 | (1.70–3.76) | 2.83 | (1.91–4.18) |
aIncludes non-Hispanic Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaskan Native only, Multiracial and other race only
bIncludes Divorced, Widowed, Separated, Never Married, and Member of an unmarried couple
cIncludes Homemaker, Student, Retired, Unable to Work, and Out of work
Statistical signifiance at 5% alpha is indicated by odds ratios in bold
Discussion
Study overview
Broadly speaking, studies on depression in the elderly have focused either on its risk factors or associated increases in health care costs and utilization. The current study is unique as it represents the first study of its kind to report the prevalence of symptoms of current depression in a sample of community dwelling older adults (≥ 65 years of age) in the U.S. who self-reported medical cost as a barrier to seeking health care. In addition, this study examined the association between self-reported medical cost as a barrier to seeking health care and current depressive symptomatology and identified the socio-demographic characteristics of older adults who had a significantly higher likelihood to report medical cost as a barrier to seeking health care. The findings from this study highlight the need for effective interventions to address the barriers to seeking health care due to the burden of out-of-pocket medical cost on the individual, particularly for those with multiple chronic conditions. This may help minimize the risk for current depression in older adults.
Main findings
Based on data from the 2011 BRFSS, the prevalence of symptoms of current depression in a sample of community dwelling older adults (≥ 65 years of age) in the U.S. was 6.1%. This prevalence is higher than previously reported based on data from 2006 BRFSS using similar criteria (score ≥ 10 on PHQ-8) for current depressive symptoms [28]. The prevalence of current depressive symptomatology was significantly higher (17.8%) among older adults who reported medical cost as a barrier to seeking health care when compared to older adults who did not report medical cost as a barrier (5.5%). After adjusting for all covariates, we found that older adults who reported medical cost as a barrier to seeking health care were twice more likely to report current depressive symptoms compared to those who did not report medical cost as a barrier to seeking health care. In addition, we also found that older adults with the following socio-demographics: females, Black non-Hispanics, Hispanics, and high school or less education; health indicators: “Fair/Poor” general health, smokers, and use of special equipment due to a health problem; and health care indicators: not having a health plan, and no annual checkup, were significantly more likely to report medical cost as a barrier to seeking health care. This finding is consistent with prior studies that have identified socio-demographic characteristics associated with out-of-pocket medical cost [15, 31, 32].
Association between medical cost as a barrier to seeking health care and symptoms of current depression
One of the most common barriers to seeking health care is out-of-pocket medical cost [33]. In particular, among older adults with chronic conditions, the burden of out-of-pocket medical cost is a major concern [34–36]. In this current study, though out-of-pocket health care expenses was not measured, consistent with previous studies [19, 37–39], we found that the proportion of older adults who reported medical cost as a barrier to seeking health care increased with the number of chronic conditions (Table 1). A plausible explanation could be that a significant proportion of medical cost may have to do with out-of-pocket expenses for medications and prescription drugs often required to manage chronic conditions [34–36, 39].
Empirical evidence presented in the current study suggests that the burden of out-of-pocket medical cost is significantly associated with symptoms of current depression, thus, taking a step further in our understanding of the consequences of out-of-pocket medical cost (cost-sharing) burden among older adults. This finding is consistent with previous studies which reported the association between financial strain in general and symptoms of depression among older adults [23, 24].
Several studies have reported that lack of health care coverage or type of coverage (e.g., Medicare only) would lead to high financial burden [19, 36, 40]. This finding was consistent in our study with 27.3% reporting medical cost as a barrier for seeking health care among those without a health plan compared to 5.2% reporting the same among those with a health plan. However, despite having a health plan, the unadjusted prevalence of symptoms of current depression among older adults who reported medical cost as a barrier for seeking health care was 18.8% [95% CI: 11.8–25.7%]. Whereas among older adults without a health plan, the unadjusted prevalence of symptoms of current depression among those who reported medical cost as a barrier for seeking health care was 8.6% [95% CI: 2.2–15.0%]. This could be because older adults with a health plan are more likely to utilize health care and as a result might have to sustain more out-of-pocket expenses compared to those without a health plan.
While we don’t have specific information about the type of health plan, to understand the extent to which having a health plan mitigates the association between the burden of out-of-pocket medical cost and the likelihood to report current depression after controlling for all socio-demographic and health related factors, we examined the magnitude of this association stratified by health plan status. Among older adults who reported having a health plan, after adjusting for possible potential confounders, older adults who reported medical cost as a barrier for seeking health care were more than twice as likely to report current depression compared to those who reported medical cost not being a barrier for seeking health care [AOR: 2.2 [95% CI: 1.5–3.4]); whereas among those who reported not having a health plan, the magnitude of this association was much augmented [AOR: 7.3 [95% CI: 2.2–22.4]). This finding suggests that the burden of out-of-pocket medical cost is significantly associated with symptoms of current depression though the magnitude of this association could be mitigated due to having a health plan. As the prevalence of individuals with persistently high medical cost burden is likely to surge in the future [34], policies to reduce the burden of out-of-pocket medical cost among older adults may help address depression to some extent among the elderly and thereby reduce health care costs associated with depression.
Strengths and limitations
Although this study documents, using a nationally representative sample, a significant association between the individuals’ burden of medical cost for health care and symptoms of depression among older adults, these findings are subject to limitations:
The cross-sectional nature of the BRFSS data precludes us from drawing any causal relationship between the burden of medical cost and symptoms of current depression.
BRFSS data are based on self-report and therefore may be subject to recall-bias for certain types of responses.
Analysis of data in this study did not consider social and emotional support system among older adults. It is likely that social isolation in older adults might be a contributing factor to individual’s mental health [41, 42]. In addition, the analysis did not account for annual income; approximately 1 out of 7 older adults reported as employed during the time of the survey.
Information about having a health plan was binary (Yes / No). Information about the type of health plan (e.g., types of insurance coverage) would have shed more light into the relationship between the burden of medical cost for health care and symptoms of current depression.
Finally, since the data used in the current study are from 12 states in the 2011 BRFSS survey and is limited to non-institutionalized older adults, the findings may not be generalizable to all older adults in the U.S.
Despite these limitations, this study documents an important finding that has policy implications. To the best of our knowledge, this is the first study to report a significant association between individuals’ burden of medical cost for health care and symptoms of depression.
Conclusions
In conclusion, findings from this study suggest that older adults (≥ 65 years of age) who experience the burden of medical cost for health care are significantly more likely to report symptoms of depression. Having a health plan might help mitigate the association between burden of medical cost for health care and symptoms of depression. Health care professionals and policymakers should consider effective interventions to improve access to health care among older adults. Such efforts may help address the mental health concerns such as depression among the elderly and thereby reduce the cost burden associated with it and improve health outcomes. Further research is necessary to confirm the findings from this study and to understand how older adults manage their comorbid conditions which puts on them a huge burden of out-of-pocket medical cost to deal with.
Additional file
Table S1. Estimated Odds Ratio (95% CI) for Current Depressive Symptoms (PHQ-8 Score ≥ 10) among Adults Aged 65 and Older (n = 24,018). (DOCX 20 kb)
Acknowledgements
The authors would like to acknowledge the participants in the 2011 BRFSS survey.
Abbreviations
- AOR
Adjusted Odds Ratio
- BRFSS
Behavioral Risk Factors Surveillance System
- CDC
Centers for Disease Control and Prevention
- U.S
United States
- UOR
Unadjusted Odds Ratio
Author’s contributions
VKC conceptualized and designed the study, designed the analytic plan, conducted the analyses, drafted, reviewed and revised the manuscript, and approved the final manuscript as submitted. ETC conducted the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Funding
No external funding was secured for this study.
Availability of data and materials
Datasets can be obtained from the corresponding author on reasonable request.
Ethics approval and consent to participate
No administrative permissions were required to access the raw data. This study was exempt from review by Kent State University’s IRB because BRFSS data are publicly available and deidentified.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Vinay K. Cheruvu, Phone: 330-672-6518, Email: vcheruvu@kent.edu
Edward T. Chiyaka, Email: echiyaka@kent.edu
References
- 1.Gill J, Moore MJ. The State of aging & health in America. Atlanta: Centers for Disease Control and Prevention; 2013.
- 2.Ortman JM, Velkoff VA, Hogan H. US Census Bureau. An aging nation: the older population in the United States. Available at: https://www.census.gov/prod/2014pubs/p25-1140.pdf. Accessed 9 Oct 2017.
- 3.Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. Santa Monica: RAND Corporation; 2017. [Google Scholar]
- 4.Office of Disease Prevention and Health Promotion [ODPHP] Healthy People 2020. Older adults. 2016. [Google Scholar]
- 5.Allan C, Valkanova V, Ebmeier K. Depression in older people is underdiagnosed. Practitioner. 2014;258(1771):19–22. [PubMed] [Google Scholar]
- 6.Manthorpe J, Iliffe S. Depression in Later Life. London; Jessica Kingsley Publishers; 2005.
- 7.Blazer DG. Depression in late life: review and commentary. J Gerontol Ser A Biol Med Sci. 2003;58(3):M249–M265. doi: 10.1093/gerona/58.3.M249. [DOI] [PubMed] [Google Scholar]
- 8.Lopez AD, Murray CC. The global burden of disease, 1990–2020. Nat Med. 1998;4(11):1241. doi: 10.1038/3218. [DOI] [PubMed] [Google Scholar]
- 9.Chang-Quan H, et al. Health status and risk for depression among the elderly: a meta-analysis of published literature. Age Ageing. 2009;39(1):23–30. doi: 10.1093/ageing/afp187. [DOI] [PubMed] [Google Scholar]
- 10.Lenze EJ, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9(2):113–135. doi: 10.1097/00019442-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Prince MJ, et al. Social support deficits, loneliness and life events as risk factors for depression in old age. The gospel oak project VI. Psychol Med. 1997;27(2):323–332. doi: 10.1017/S0033291796004485. [DOI] [PubMed] [Google Scholar]
- 12.Blazer D, et al. The association of age and depression among the elderly: an epidemiologic exploration. J Gerontol. 1991;46(6):M210–M215. doi: 10.1093/geronj/46.6.M210. [DOI] [PubMed] [Google Scholar]
- 13.Harris T, et al. Predictors of depressive symptoms in older people—a survey of two general practice populations. Age Ageing. 2003;32(5):510–518. doi: 10.1093/ageing/afg087. [DOI] [PubMed] [Google Scholar]
- 14.Vink D, Aartsen MJ, Schoevers RA. Risk factors for anxiety and depression in the elderly: a review. J Affect Disord. 2008;106(1–2):29–44. doi: 10.1016/j.jad.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Crystal S, et al. Out-of-pocket health care costs among older Americans. J Gerontol Soc Sci. 2000;55(1):S5I–S62. doi: 10.1093/gerona/55.1.B5. [DOI] [PubMed] [Google Scholar]
- 16.Goins RT, et al. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 17.Goldman DP, Zissimopoulos JM. High out-of-pocket health care spending by the elderly. Health Aff. 2003;22(3):194–202. doi: 10.1377/hlthaff.22.3.194. [DOI] [PubMed] [Google Scholar]
- 18.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27(2):384–391. doi: 10.2337/diacare.27.2.384. [DOI] [PubMed] [Google Scholar]
- 19.Schoenberg NE, et al. Burden of common multiple-morbidity constellations on out-of-pocket medical expenditures among older adults. Gerontologist. 2007;47(4):423–437. doi: 10.1093/geront/47.4.423. [DOI] [PubMed] [Google Scholar]
- 20.Bock J-O, et al. Impact of depression on health care utilization and costs among multimorbid patients–results from the multicare cohort study. PLoS One. 2014;9(3):e91973. doi: 10.1371/journal.pone.0091973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalsekar I, et al. The effect of depression on health care utilization and costs in patients with type 2 diabetes. Manag Care Interface. 2006;19(3):39–46. [PubMed] [Google Scholar]
- 22.Welch CA, et al. Depression and costs of health care. Psychosomatics. 2009;50(4):392–401. doi: 10.1176/appi.psy.50.4.392. [DOI] [PubMed] [Google Scholar]
- 23.Krause N. Chronic financial strain, social support, and depressive symptoms among older adults. Psychol Aging. 1987;2(2):185. doi: 10.1037/0882-7974.2.2.185. [DOI] [PubMed] [Google Scholar]
- 24.Mendes De Leon CF, Rapp SS, Kasl SV. Financial strain and symptoms of depression in a community sample of elderly men and women: a longitudinal study. J Aging Health. 1994;6(4):448–468. doi: 10.1177/089826439400600402. [DOI] [Google Scholar]
- 25.Remler DK, Greene J. Cost-sharing: a blunt instrument. Annu Rev Public Health. 2009;30:293–311. doi: 10.1146/annurev.publhealth.29.020907.090804. [DOI] [PubMed] [Google Scholar]
- 26.Baird KE. The financial burden of out-of-pocket expenses in the United States and Canada: How different is the United States? SAGE Open Med. 2016;4:2050312115623792. doi: 10.1177/2050312115623792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Behavioral Risk FactorSurveillanceSystem operational and user’s guide. Version 3.0. Available at: https://www.cdc.gov/brfss/pdf/userguide.pdf. Published March 4, 2005. Accessed 19 Nov 2017.
- 28.McGuire LC, et al. The patient health questionnaire 8: current depressive symptoms among US older adults, 2006 behavioral risk factor surveillance system. Am J Geriatr Psychiatry. 2009;17(4):324–334. doi: 10.1097/JGP.0b013e3181953bae. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, et al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 30.Frances A, Pincus HA, First M. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 31.Davidoff AJ, et al. Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 2013;119(6):1257–1265. doi: 10.1002/cncr.27848. [DOI] [PubMed] [Google Scholar]
- 32.Desmond K, Rice T, Cubanski J, Neuman P. The burden of out-of-pocket health spending among older versus younger adults: Analysis from the consumer expenditure survey, 1998–2003. Medicare Issue Brief. No. 7686. Menlo Park, C.A.: Kaiser Family Foundation; 2007.
- 33.Fitzpatrick AL, et al. Barriers to health care access among the elderly and who perceives them. Am J Public Health. 2004;94(10):1788–1794. doi: 10.2105/AJPH.94.10.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cunningham PJ. Chronic burdens: the persistently high out-of-pocket health care expenses faced by many Americans with chronic conditions. New York: Commonwealth Fund; 2009. [PubMed] [Google Scholar]
- 35.Hwang W, et al. Out-of-pocket medical spending for care of chronic conditions. Health Aff. 2001;20(6):267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 36.Sambamoorthi U, Shea D, Crystal S. Total and out-of-pocket expenditures for prescription drugs among older persons. Gerontologist. 2003;43(3):345–359. doi: 10.1093/geront/43.3.345. [DOI] [PubMed] [Google Scholar]
- 37.Soni A. Out-of-Pocket Expenditures for Adults with Health Care Expenses for Multiple Chronic Conditions, US Civilian Noninstitutionalized Population, 2014. Statistical brief #498. Rockville: Agency for Healthcare Research and Quality; 2017. [PubMed] [Google Scholar]
- 38.Paez KA, Zhao L, Hwang W. Rising out-of-pocket spending for chronic conditions: a ten-year trend. Health Aff. 2009;28(1):15–25. doi: 10.1377/hlthaff.28.1.15. [DOI] [PubMed] [Google Scholar]
- 39.Fahlman C, et al. Prescription drug spending for beneficiaries in the last Medicare plus choice year of life. J Palliat Med. 2006;9(4):884–893. doi: 10.1089/jpm.2006.9.884. [DOI] [PubMed] [Google Scholar]
- 40.Johnson RW, Mommaerts C. Are health care costs a burden for older Americans? 2009. [Google Scholar]
- 41.Oxman TE, et al. Social support and depressive symptoms in the elderly. Am J Epidemiol. 1992;135(4):356–368. doi: 10.1093/oxfordjournals.aje.a116297. [DOI] [PubMed] [Google Scholar]
- 42.Santini ZI, et al. The association between social relationships and depression: a systematic review. J Affect Disord. 2015;175:53–65. doi: 10.1016/j.jad.2014.12.049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Estimated Odds Ratio (95% CI) for Current Depressive Symptoms (PHQ-8 Score ≥ 10) among Adults Aged 65 and Older (n = 24,018). (DOCX 20 kb)
Data Availability Statement
Datasets can be obtained from the corresponding author on reasonable request.