Abstract
Objective
To investigate the impact of premature extraction of primary teeth (PEPT) on orthodontic treatment need in a cohort of children participating in the Born in Bradford (BiB) longitudinal birth cohort.
Design
Observational, cross sectional cohort.
Participants
We aim to recruit 1000 children, aged 7 to 11 years, 500 with a history of PEPT, and 500 matched non-PEPT controls.
Methods
Following informed consent/assent orthodontic records will be collected, including extra and intra-oral photographs and alginate impressions for study models. Participants will also complete a measure of oral health-related quality of life (COHIP-SF 19). The records will be used to quantify space loss, identify other occlusal anomalies and assess orthodontic treatment need using the Index of Orthodontic Treatment Need. For each outcome, summary statistics will be calculated and the data for children with and without PEPT compared. The records of the children identified to be in need of orthodontic treatment will be examined by an expert orthodontic panel to judge if this treatment should be undertaken at the time of the records or delayed until the early permanent dentition.
Collecting robust records in the mixed dentition provides the clinical basis to link each stage of the causal chain and enable the impact of PEPT on orthodontic need to be characterised. This study is the first to provide the foundations for future longitudinal data collection allowing the long-term impact of PEPT to be studied.
Introduction
Background and Rationale
Extraction of carious primary teeth is the most common reason for young children to have a general anaesthetic in England. In 2015/ 2016 over 45,000 children (NHS Digital 2015-2016) underwent this procedure at an estimated cost of £50.5 million to the NHS (Public Health England 2017). In addition to the financial cost, these have a significant impact for children and their families with associated anxiety, reduced school attendance and post-operative morbidity (Rodd et al. 2014; Wong et al. 2015; Knapp et al. 2016).
Professional bodies (Fayle et al. 2001; American Academy Of Paediatric Dentistry 2014; American Academy of Pediatric Dentistry 2014; Faculty of Dental Surgery 2015) urge clinicians to restore primary teeth where feasible, to maintain the space for the permanent dentition and thereby reduce malocclusion and the potential future need for orthodontic treatment. A systematic review by Bhujel et al (2016) examined the impact of premature extraction of primary teeth with orthodontic treatment need in the permanent dentition. Bhujel et al (2016) found six short-term studies, (Clinch and Healy 1959; Ronnerman 1965, 1977; Leighton 1981; Kau et al. 2004; Sayın and Türkkahraman 2006) which examined the impact of premature extraction of primary teeth (PEPT) in the mixed dentition, with each study identifying space loss as a sequela. One longitudinal case-control study was identified, (Hoffding and Kisling 1978) which reported a 10% increase in the frequency of at least one feature of malocclusion in children with a history of PEPT, compared to children with no history of PEPT (non-PEPT). None of the previous studies used a validated index to measure orthodontic treatment need and thus quantify the impact of PEPT.
Tooth loss has been shown to have a negative impact on Oral Health Related Quality of Life (OHRQoL) in the permanent dentition (Gerritsen et al. 2010). However the impact of PEPT on the quality of life of children has received very little attention. Monte-Santo et al. (2018) recently published their study, which used the child OHRQoL to investigate the impact of untreated caries and PEPT on a Brazilian cohort of 667 children aged 8-9 years old. Children with PEPT presented with significantly greater OHRQoL scores especially in the domains of oral symptoms, functional limitation and emotional well being.
The aetiology of malocclusion is complex involving both genetic and environmental factors. To date, the literature to support and characterise the contribution of PEPT to malocclusion is very limited. Robust longitudinal studies are required, which include data collection in both the mixed and permanent dentitions.
In Bradford, approximately 800 children a year undergo extraction of primary teeth under general anaesthetic with each child having an average of eight primary teeth extracted (Bradford District Care NHS Foundation Trust 2015). There is substantial heterogeneity in the number of teeth extracted, thereby providing a natural experiment in which to explore the impact of PEPT, as well as the contribution of the number and the type of primary teeth extracted. An earlier retrospective study in Bradford showed association between the number of teeth extracted and orthodontic need; however, the study design and small numbers (116 children with 66 having a history of PEPT) limited the external validity of the findings (Bhujel et al. 2014).
The Born in Bradford birth cohort (BiB) offers a unique chance to examine the impact of PEPT on the development of malocclusion and subsequent orthodontic treatment need. BiB is a population-based, longitudinal, prospective study (Wright et al. 2012) developed to provide evidence about the causes of health and disease, by following the lives of 13,858 children born between 2007 and 2011.
This paper describes the protocol for a study that will explore the effect that PEPT has on malocclusion and subsequent orthodontic need. This study will improve on previous study designs by collecting robust records of space loss and occlusal anomalies in the mixed dentition and providing the clinical basis to link each stage of the causal chain and enable the impact of PEPT on orthodontic need to be characterised. It will also provide the base for further longitudinal data collection to examine the effects of PEPT in the permanent dentition.
Aim
To investigate the impact of premature extraction of primary teeth (PEPT) on orthodontic treatment need.
Objectives
To compare a group of children aged 7 to 11 years, who have undergone premature extraction of primary teeth (PEPT) with a similar cohort of children who have not undergone premature extraction of primary teeth (non-PEPT) in regard to:
-
-
The effect on space loss and other occlusal anomalies;
-
-
The proportion of children judged to need orthodontic treatment;
-
-
The timing of future orthodontic treatment. Children deemed to need orthodontic treatment will be categorised into those who require treatment in either the mixed dentition or in the early permanent dentition. This will be judged by a panel of specialist orthodontists.
-
-
To explore the impact of PEPT on children’s Oral Health Related Quality of Life.
Design
This stage of the study is an observational, cross sectional design involving a sample from the Born in Bradford (BiB) longitudinal birth cohort. The study will provide baseline data for a prospective, longitudinal cohort study. During development of the project representatives from BiB parents group met the research team to discuss the project design, child and parent information sheets and recruitment strategy. This feedback was extremely valuable and informed adaptions to the project methodology.
Methods: Participants, interventions, and outcomes
Study Population
The Born in Bradford birth cohort (BiB): A total of 13,858 children were recruited to the BiB cohort over a five-year period, 11,711 of whom are known currently to be attending primary schools in Bradford. The cohort is predominantly from a multi-ethnic origin with 45% Pakistani, 39% White British and 15% from other ethnic groups. Following ethics and appropriate research permissions, we will recruit at least 500 BiB children aged 7-11 years old who have undergone dental extractions. An on-going dental data linkage feasibility study, funded by the Wellcome Institutional Strategic Support fund, has identified BiB children who have received extraction of primary teeth under general anaesthesia. To date, this study has recruited 1,139 BiB children and identified information such as age at the time of the operation, number and type of teeth extracted.
An equal number of BiB children (at least 500) with no history of dental extractions will be recruited for a non-PEPT control group. To ensure control group children have not undergone PEPT with local anaesthetic, parents and children will be asked about any previous extractions. The control group will be matched for academic year group and where possible by the school they attend.
Eligibility criteria
Children will be eligible to be included in the study if;
They are an active participant in the BiB cohort, with ongoing family consent;
Aged 6 to 11 years.
Participants will have either a;
History or clinical evidence of premature extraction of one or more primary (baby or deciduous) tooth under either local or general anaesthetic (PEPT group)
Or
No history or clinical evidence of premature extraction of primary (baby or deciduous) molars (non-PEPT group).
Children will be ineligible if the fit any of the following;
Not an active participant in the BiB cohort;
History or clinical evidence of extraction of any secondary (adult or permanent) teeth;
Unable to manage or do not give consent to having dental records, including a dental exam, dental impressions and intra & extra oral photographs. Reasons may include medical history, learning impairments, gag reflex or anxiety regarding the procedure;
History of orthodontic (brace) treatment;
Currently undergoing orthodontic (brace) treatment;
Cleft of the lip or palate
Study Setting
Data collection will be undertaken in primary schools in Bradford. A designated private area away from the normal classroom will be used for the dental assessment. Requests to visit schools will be made in advance and the number of visits will be kept as low as possible to minimise disruption.
Outcomes
Primary outcome:
-
-
To quantify the proportion of children who are assessed as having a need for orthodontic treatment
Secondary outcomes:
-
-
Space loss and occlusal anomalies in the mixed dentition
-
-
To assess the proportions who would be treated in the mixed dentition or in the early permanent dentition
-
-
To explore the impact of PEPT on children’s Oral Health Related Quality of Life.
Sample Size: Power calculation
The primary outcome is a binary outcome of Need/No Need for orthodontic treatment using the current NHS threshold Index of Orthodontic Treatment Needs (IOTN) score of 4 or 5 in the Dental Health Component (DHC) or 3 (DHC with a score of 6-10 in the Aesthetic Component (AC) (Brook P 1989). Based on this we have used the raw data from the 2008 Dental Epidemiology Survey for Bradford to evaluate statistical power. A sample size of 1000 subjects (of which 50% are PEPT cases) could achieve at least 81% of power at a 5% significance level to detect a difference of 10% in the orthodontic treatment need (see Table 1).
Table 1. Power calculation for a combination of parameters.
| Power | PEPT cases | Total sample size | Allocation ratio | Clinically relevant difference in orthodontic need | Multiple correlation between the exposure and the other independent variables | Alpha |
|---|---|---|---|---|---|---|
| 85% | 500 | 1000 | 1 | 10% | 0.1 | 0.05 |
| 81% | 500 | 1000 | 1 | 10% | 0.2 | 0.05 |
| 91% | 500 | 1000 | 1 | 11% | 0.1 | 0.05 |
| 88% | 500 | 1000 | 1 | 11% | 0.2 | 0.05 |
| 95% | 500 | 1000 | 1 | 12% | 0.1 | 0.05 |
| 93% | 500 | 1000 | 1 | 12% | 0.2 | 0.05 |
| 91% | 600 | 1200 | 1 | 10% | 0.1 | 0.05 |
| 87% | 600 | 1200 | 1 | 10% | 0.2 | 0.05 |
| 95% | 600 | 1200 | 1 | 11% | 0.1 | 0.05 |
| 93% | 600 | 1200 | 1 | 11% | 0.2 | 0.05 |
| 91% | 500 | 1250 | 1.5 | 10% | 0.1 | 0.05 |
| 87% | 500 | 1250 | 1.5 | 10% | 0.2 | 0.05 |
| 95% | 500 | 1250 | 1.5 | 11% | 0.1 | 0.05 |
| 93% | 500 | 1250 | 1.5 | 11% | 0.2 | 0.05 |
| 93% | 500 | 1500 | 2 | 10% | 0.1 | 0.05 |
| 90% | 500 | 1500 | 2 | 10% | 0.2 | 0.05 |
Recruitment
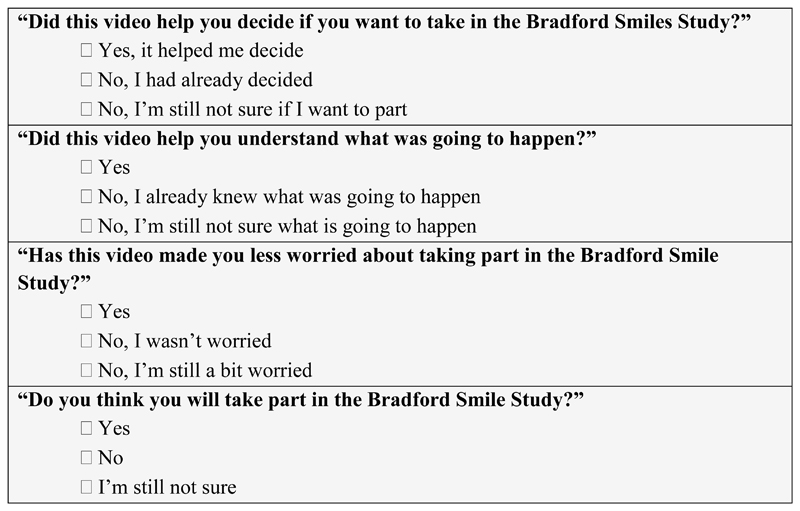
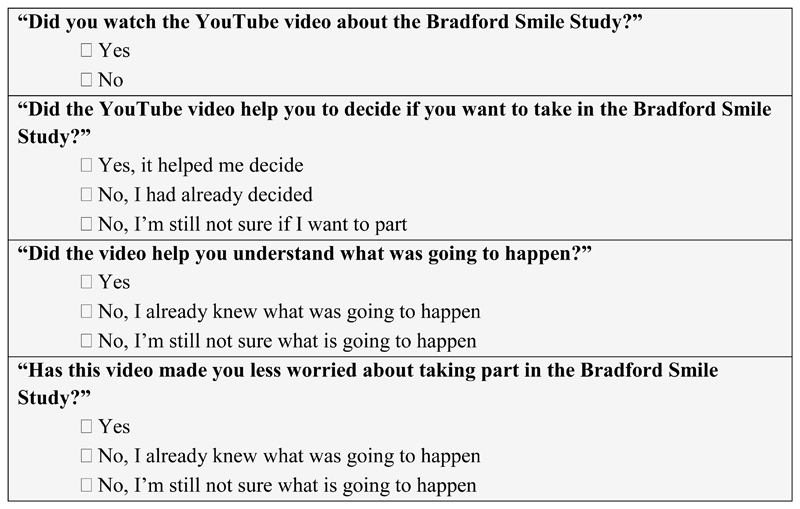
Identification of potential participants in both groups will be undertaken by the BiB research team. Lists of children taking part in the BiB cohort, the school they attend and their contact details will be collated. These details will only be available to the BiB research team and the Clinical Research Network (CRN) team who will initially send out recruitment letters. Invitation letters will be sent to family addresses alongside information sheets. To enhance the understanding of the data collection process for children and their families, and to reduce anxiety about unfamiliar procedures, an information video has been produced (https://www.youtube.com/watch?v=eY9LAwunaBY). This explains the purpose of the research and shows how the examination, impressions and photographs will be collected. The video aims to provide an alternative format of information for those with low literacy or English as a second language and enhance the consent process. The use of an information video is relatively novel in dental research recruitment and the research team plan to evaluate the efficacy of this tool. Evaluation will be undertaken through questions embedded into the YouTube video and a questionnaire (Figure 1 & 2) during the recruitment process. The questionnaire aims to evaluate the number of potential participants watching the video, whether it encouraged their participation and whether it alleviated any anxieties about taking part.
Figure 1.
Questions asked electronically immediately after the video via a pop-up question box.
Figure 2.
Questions on the consent form.
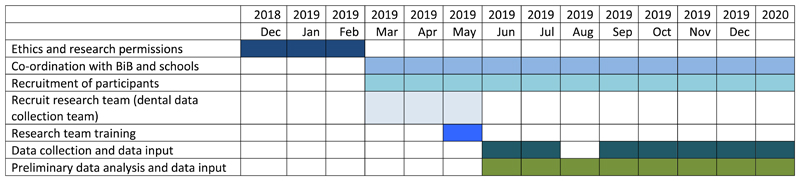
Figure 3, a Gant Chart shows the expected timing for recruitment, data collection analysis and dissemination.
Figure 3.
Gant chart showing expected timing for the study.
Methods: Data collection, management, and analysis
Data collection
Overarching protocols from the National Child Dental Health Survey, which is conducted in a school setting, will be followed (HSCIC 2015). The research team (1x dentist or dental therapist, 1x dental nurse) will complete a dental examination. This will allow intraoral photographs to be validated and correct inter-digitation of study models. The number of teeth present as well as obvious dental findings e.g. cavitated dental caries and molar incisor hypo-mineralisation will also be recorded.
The team will take standardised intra and extra-oral orthodontic photographs. Alginate impressions will be taken and scanned to facilitate the production of digital study models, with the articulation validated by intraoral photographs. Children will be asked to complete the Child Oral Health Impact Profile–Short Form 19 (COHIP-SF 19) questionnaire (Broder et al. 2012).
Training of examiners
The research team will undertake bespoke training in orthodontic photography and impression taking. During the early stages of data collection an orthodontist will accompany the research team to ensure consistency in record taking.
Data Management
Data will be hosted in the BiB data warehouse at Bradford Teaching Hospitals NHS Foundation Trust and managed in accordance with well-established BiB data access and security protocols. Consultation with the Health Research Authority ensured that patient information sheets complied with the new General Data Protection Regulation (GDPR) guidance (Local Government Association 2018) introduced in May 2018.
Analysis
Statistical Methods
The exposure, premature extraction of primary teeth (PEPT) or no premature extractions (non-PEPT) will be captured as a single event. Confounders in the two groups will be identified within a directed acyclic graph, and appropriate minimally sufficient adjustment sets of confounders will be accommodated in all subsequent analyses (Greenland et al. 1999), allowing appropriate causal inferences to be made.
Analysis of Secondary Outcomes
To characterise space loss and occlusal anomalies in the mixed dentition
For each child, the following information will be recorded from the clinical photographs and digital study models: molar and incisor relationship, overjet, overbite, crossbites, skeletal pattern and the degree of crowding or spacing. From the study models further measurements will be calculated for each arch and will include: arch perimeter and hemi-perimeter, arch length, arch width and E and D space as defined by Northway (Northway and Wainright 1980).
This analysis will be required in order to allow the primary outcome to be evaluated. For each measurement, an appropriate summary statistic will be calculated for children in the PEPT and non-PEPT groups. The groups will be compared either descriptively or through appropriate statistical test to detect any differences.
Analysis of the Primary Outcome
To quantify the proportion of children who are assessed as having a need for orthodontic treatment
Using the study models and photographs (but with no access to radiographs) each child’s records will be assessed by the research team following appropriate training, using the IOTN Dental Health Component.
Orthodontic indices, including the Index of Orthodontic Treatment Need (IOTN), the Index of Complexity, Outcome and Need (ICON) and the Dental Aesthetic Index (DAI), have been used in the mixed dentition to measure prevalence of malocclusion and estimate orthodontic treatment need (Tausche et al. 2004; Mohamed et al. 2014; Rauten et al. 2016) and to assess changes in occlusal features and treatment need over time (Lagana et al. 2013; Boronat-Catala et al. 2016). The IOTN was more stable than other indices for estimating treatment need across different age groups (Tarvit and Freer 1998; Baubiniene et al. 2009; Costa et al. 2011; Boronat-Catala et al. 2016) and while not developed specifically to predict future treatment need, IOTN may be used as a guide to estimate this. To date, no studies have observed a single group of participants longitudinally to quantify the predictive ability of any index in the mixed dentition. After discussion within the research team IOTN was judged to be the most appropriate objective measure of orthodontic need that is currently available.
Analysis of Secondary Outcomes
To assess the proportions who would be treated in the mixed dentition or in the early permanent dentition
An expert panel of three specialist orthodontists will independently examine the clinical photographs and digital study models for those children who have an orthodontic treatment need according to IOTN DHC or are deemed by the expert panel to require interceptive orthodontic treatment. A decision will be made as to whether they would recommend orthodontic treatment to be undertaken at the time that the records were taken (e.g. in the mixed dentition) or to wait and treat in the early permanent dentition. A standardised data collection form will provide a systematic and objective format for evaluating records and determining the timing of any orthodontic need. Disagreements will be resolved through discussion.
To explore the impact of PEPT on children’s Oral Health Related Quality of Life
Several measures are available to assess Children’s Oral Health Related Quality of Life including Child Perceptions Questionnaire (CPQ), the Child Oral Impacts on Daily Performances (C-OIDP), and the Child Oral Health Impact Profile (COHIP (Broder et al. 2012; Gilchrist et al. 2014). Each self-reported measure has been validated and has been shown to discriminate between groups. Certain measures have been adapted for specific age groups (Humphris et al. 2005; Gilchrist et al. 2014).
The Child Oral Health Impact Profile-Reduced Questionnaire (COHIP-SF 19) (Broder et al. 2012) will be used to assess any impact PEPT has on children’s oral health related quality of life. Although CPQ 8-10 (Humphris et al. 2005) was used to measure children’s OHRQoL in previous PEPT studies (Monte-Santo et al. 2018), COHIP-SF 19 was felt to be most appropriate for this study for several reasons. This tool has been validated for use in children aged 7-15 years old (Broder et al. 2012; Gilchrist et al. 2014). This is crucial to allow the continuous use of this OHRQoL measurement tool in the planned longitudinal data collection of this cohort. The COHIP-SF 19 is also short to complete thus allowing ease of use and reducing the impact on participants during data collection.
The results of the COHIP-SF 19 will be computed by summing the values of each question. The total score will range from 0 to 76. The distribution of the total score will be assessed. If normally distributed, the total COHIP-SF 19 score will be compared between PEPT and non-PEPT groups using two-sided two-sample t-test; otherwise nonparametric Mann-Whitney U test will be used. Generalized linear model will be used to assess the difference in oral health related quality of life between PEPT and non-PEPT groups adjusting for other explanatory variables (e.g. presence of decayed teeth). If statistical significance is found for PEPT then the significance of different sub-domains will be explored.
Ethics and dissemination
Research ethics approval
Full ethical approval via the Health Research Authority and an NHS Research Ethics Committee was sought and granted (18/YH/04).
Consent
Informed consent will be collected from BiB children’s parents or legal guardians. The CRN staff or member of the BiB team who collect the consent are all trained in Good Clinical Practice and highly skilled in collecting informed consent. Verbal assent will be gained from the children prior to data collection. Children will be informed that they can stop at any point if they wish.
Ethical considerations
Dental staff collecting records will receive tailored training. Safeguarding principles will be followed and children with extensive untreated caries or signs of dental infection will be highlighted with a letter sent to their parents.
Dissemination Policy
Dissemination of the study findings will aim to engage all important stakeholders including 1) Participants, their families and the wider BiB community; 2) Dental professionals; 3) Commissioners and policy-makers involved in children’s dental services. BiB representatives will inform the approach for public-facing dissemination and innovative methods to share research findings will be explored in collaboration with University of Leeds School of Dentistry public engagement champions. Professional dissemination will include publication in peer-reviewed journals, presentation at relevant international conferences and sharing of the key findings through appropriate social media channels.
Discussion
Multiple factors affect the development of malocclusions and subsequent orthodontic need. There is also no accepted single measure of malocclusion. As such, designing a study to evaluate the effect that PEPT has on the developing occlusion is challenging. A multi-disciplinary approach has been required to overcome these challenges to develop a robust research methodology to answer the research questions.
Embedding a dental study within an existing longitudinal birth cohort provides both exciting opportunities and logistical challenges. A strong relationship with the BiB research team has been crucial in developing the protocol, which is considerate of wider research projects, participant burden and goodwill of local primary schools. Ultimately the study is only possible as a result of the research funding and infrastructure established for other studies involving the cohort.
The research team aim to utilise the opportunities of working within a longitudinal birth cohort. An additional aim to the study is to provide the foundation for future longitudinal data collection, when children are in the permanent dentition. Future data collection will allow the accuracy of the IOTN prediction analysis to be examined and enable the effects of PEPT to be studied. The impact of PEPT on current and future orthodontic need will also be characterised. A decision tree, based on the predicted care pathways, will be constructed and this will allow the costs associated with different clinical outcomes (need or no need for orthodontic treatment) to be estimated.
Acknowledgments
This research is supported by a grant from the British Orthodontic Society Foundation. The initial dental data linkage was supported by grants from the Oral Dental Research Trust and the Wellcome Institutional Strategic Support Fund. Two of the authors of this paper (PD, RM) were supported by the NIHR CLAHRC Yorkshire and Humber. www.clahrc-yh.nihr.ac.uk. The views and opinions expressed are those of the author(s), and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Born in Bradford is only possible because of the enthusiasm and commitment of the Children and Parents in BiB. We are grateful to all the participants, health professionals and researchers who have made Born in Bradford happen. The BiB New Wave project is supported by a number of grants including:
A joint grant from the UK Medical Research Council (MRC) and UK Economic and Social Science Research Council (ESRC): MR/N024391/1
The British Heart Foundation (BHF) (CS/16/4/32482)
A Wellcome Trust infrastructure grant (WT101597MA)
The National Institute for Health Research under its Collaboration for Applied Health Research and Care (CLAHRC) (IS-CLA-0113-10020)
The NIHR Clinical Research Network which provided research delivery support for this study
Many thanks to Adam Jones, Joshua Thornton, Colin O’Sullivan and Tim Zoltie for their help in producing the patient information video.
Footnotes
Lucy Brown: ORCHiD: 0000 0002 6793 9990
Declaration of interest statement: The authors declare no conflict of interests.
References
- American Academy Of Paediatric Dentistry. Guideline on Management of the Developing Dentition and Occlusion in Paediatric Dentistry. [accessed 23/10/18];2014 http://www.aapd.org/media/Policies_Guidelines/G_DevelopDentition.pdf.
- American Academy of Pediatric Dentistry. Guideline on Management of the Developing Dentition and Occlusion in Pediatric Dentistry. 2014 http://www.aapd.org/media/policies_guidelines/g_developdentition.pdf. [PubMed]
- Baubiniene D, Sidlauskas A, Miseviciene I. The need for orthodontic treatment among 10-11- and 14-15-year-old Lithuanian schoolchildren. Medicina (Kaunas) 2009;45(10):814–821. [PubMed] [Google Scholar]
- Bhujel N, Duggal M, Munyombwe T, Godson J, Day P. The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment. European archives of paediatric dentistry : official journal of the European Academy of Paediatric Dentistry. 2014;15:393–400. doi: 10.1007/s40368-014-0128-x. [DOI] [PubMed] [Google Scholar]
- Bhujel N, Duggal MS, Saini P, Day PF. The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment. Eur Arch Paediatr Dent. 2016;17(6):423–434. doi: 10.1007/s40368-016-0247-7. eng. [DOI] [PubMed] [Google Scholar]
- Boronat-Catala M, Bellot-Arcis C, Montiel-Company JM, Catala-Pizarro M, Almerich-Silla JM. Orthodontic treatment need of 9, 12 and 15 year-old children according to the Index of Orthodontic Treatment Need and the Dental Aesthetic Index. J Orthod. 2016;43(2):130–136. doi: 10.1080/14653125.2016.1155815. [DOI] [PubMed] [Google Scholar]
- Bradford District Care NHS Foundation Trust. Service evaluation of dental extractions under general anaesthetic. Bradford: 2015. [Google Scholar]
- Broder HL, Wilson-Genderson M, Sischo L. Reliability and validity testing for the Child Oral Health Impact Profile-Reduced (COHIP-SF 19) Journal of public health dentistry. 2012;72(4):302–312. doi: 10.1111/j.1752-7325.2012.00338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook P, S W. The development of an index of orthodontic treatment priority. European Journal of Orthodontics. 1989;11:309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- Clinch L, Healy M. A longitudinal study of the results of premature extraction of deciduous teeth between 3–4 and 13–14 years of age. Dent Pract. 1959;9:109–27. [Google Scholar]
- Costa RN, Abreu MH, Magalhaes CS, Moreira AN. Validity of two occlusal indices for determining orthodontic treatment needs of patients treated in a public university in Belo Horizonte, Minas Gerais State, Brazil. Cadernos de saude publica / Ministerio da Saude, Fundacao Oswaldo Cruz, Escola Nacional de Saude Publica. 2011;27(3):581–590. doi: 10.1590/s0102-311x2011000300018. [DOI] [PubMed] [Google Scholar]
- mFaculty of Dental Surgery. The state of children's oral health in England. London: Royal College of Surgeons of England; 2015. [Google Scholar]
- Fayle SA, Welbury RR, Roberts JF, British Society of Paediatric Dentistry B British Society of Paediatric Dentistry: a policy document on management of caries in the primary dentition. International journal of paediatric dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children. 2001;11(2):153–157. doi: 10.1046/j.1365-263x.2001.011002153.x. [DOI] [PubMed] [Google Scholar]
- Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NHJ. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health and quality of life outcomes. 2010;8:126–126. doi: 10.1186/1477-7525-8-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilchrist F, Rodd H, Deery C, Marshman Z. Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health. 2014;14(1):40. doi: 10.1186/1472-6831-14-40. [journal article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology (Cambridge, Mass) 1999;10(1):37–48. eng. [PubMed] [Google Scholar]
- Hoffding J, Kisling E. Premature loss of primary teeth: part I, its overall effect on occlusion and space in the permanent dentition. ASDC journal of dentistry for children. 1978;45(4):279–283. [PubMed] [Google Scholar]
- HSCIC. Children’s Dental Health Survey 2013. 2015. [accessed 23/10/18]. Summary. http://digital.nhs.uk/catalogue/PUB17137; [Google Scholar]
- Humphris G, Freeman R, Gibson B, Simpson K, Whelton H. Oral health-related quality of life for 8-10-year-old children: an assessment of a new measure. Community Dent Oral Epidemiol. 2005;33(5):326–332. doi: 10.1111/j.1600-0528.2005.00220.x. eng. [DOI] [PubMed] [Google Scholar]
- Kau CH, Durning P, Richmond S, Miotti FA, Harzer W. Extractions as a form of interception in the developing dentition: a randomized controlled trial. Journal of Orthodontics. 2004;31(2):107–114. doi: 10.1179/146531204225020391. [DOI] [PubMed] [Google Scholar]
- Knapp R, Gilchrist F, Rodd HD, Marshman Z. Change in children's oral health-related quality of life following dental treatment under general anaesthesia for the management of dental caries: a systematic review. International Journal of Paediatric Dentistry. 2016 doi: 10.1111/ipd.12259. [DOI] [PubMed] [Google Scholar]
- Lagana G, Masucci C, Fabi F, Bollero P, Cozza P. Prevalence of malocclusions, oral habits and orthodontic treatment need in a 7- to 15-year-old schoolchildren population in Tirana. Prog Orthod. 2013;14:12. doi: 10.1186/2196-1042-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leighton B. Longitudinal study of features which might influence space loss after early extraction of lower deciduous molars. Proc Finn Dent Soc. 1981;77:95–103. [PubMed] [Google Scholar]
- Local Government Association. General Data Protection Regulation (GDPR) [accessed 23/10/18];2018 https://local.gov.uk/our-support/general-data-protection-regulation-gdpr.
- Mohamed AM, Ariffin WFM, Rosli TI, Mahyuddin A. The feasibility of Index of Orthodontic Treatment Need (IOTN) in labial segment malocclusion among 8-10 years old. Arch Orofac Sci. 2014;9:76–84. [Google Scholar]
- Monte-Santo AS, Viana SVC, Moreira KMS, Imparato JCP, Mendes FM, Bonini G. Prevalence of early loss of primary molar and its impact in schoolchildren's quality of life. Int J Paediatr Dent. 2018;28(6):595–601. doi: 10.1111/ipd.12416. eng. [DOI] [PubMed] [Google Scholar]
- mNHS Digital. Hospital Admitted Patient Care. 2015–2016.
- Northway WM, Wainright RW. D E space--a realistic measure of changes in arch morphology: space loss due to unattended caries. Journal of dental research. 1980;59(10):1577–1580. doi: 10.1177/00220345800590100401. [DOI] [PubMed] [Google Scholar]
- Public Health England. Health Matters: Child Dental Health. [accessed 23/10/2018];2017 www.gov.uk/government/publications/health-matters-child-dental-health/health-matters-child-dental-health.
- Rauten AM, Georgescu C, Popescu MR, Maglaviceanu CF, Popescu D, Gheorghe D, Camen A, Munteanu C, Olteanu M. Orthodontic Treatment Needs in Mixed Dentition - For Children of 6 and 9 years old. Rom J Oral Rehab. 2016;8:28–39. [Google Scholar]
- Rodd H, Hall M, Deery C, Gilchrist F, Gibson BJ, Marshman Z. ‘I felt weird and wobbly.’ Child-reported impacts associated with a dental general anaesthetic. British Dental Journal. 2014;216(8):E17. doi: 10.1038/sj.bdj.2014.333. eng. [DOI] [PubMed] [Google Scholar]
- Ronnerman A. Early extraction of deciduous molars and canines--its incidence and influence on spacing. Report of the congress European Orthodontic Society. 1965;41:153–168. eng. [PubMed] [Google Scholar]
- Ronnerman A. The effect of early loss of primary molars on tooth eruption and space conditions. A longitudinal study. Acta odontologica Scandinavica. 1977;35(5):229–239. doi: 10.3109/00016357709019797. eng. [DOI] [PubMed] [Google Scholar]
- Sayin M, Türkkahraman H. Effects of Lower Primary Canine Extraction on the Mandibular Dentition. The Angle Orthodontist. 2006;76(1):31–35. doi: 10.1043/0003-3219(2006)076[0031:EOLPCE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Tarvit DJ, Freer TJ. Assessing malocclusion--the time factor. Br J Orthod. 1998;25(1):31–34. doi: 10.1093/ortho/25.1.31. [DOI] [PubMed] [Google Scholar]
- Tausche E, Luck O, Harzer W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. Eur J Orthod. 2004;26(3):237–244. doi: 10.1093/ejo/26.3.237. [DOI] [PubMed] [Google Scholar]
- Wong M, Copp PE, Haas DA. Postoperative Pain in Children After Dentistry Under General Anesthesia. Anesthesia Progress. 2015;62(4):140–152. doi: 10.2344/14-27.1. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright J, Small N, Raynor P, Tuffnell D, Bhopal R, Cameron N, Fairley L, Lawlor DA, Parslow R, Petherick ES, et al. Cohort profile: The Born in Bradford multi-ethnic family cohort study. International journal of epidemiology. 2012 doi: 10.1093/ije/dys112. Eng. [DOI] [PubMed] [Google Scholar]