Abstract
Introduction
One way to slow the spread of resistant bacteria is by improved stewardship of antibiotics: using them more carefully and reducing the number of prescriptions. With an estimated 7%–10% of antibiotic prescriptions globally originating from dental practices and up to 80% prescribed unnecessarily, dentistry has an important role to play. To support the design of new stewardship interventions through knowledge transfer between contexts, this study aimed to identify factors associated with the decision to prescribe antibiotics to adults presenting with acute conditions across primary care (including dentistry).
Methods
Two reviews were undertaken: an umbrella review across primary healthcare and a systematic review in dentistry. Two authors independently selected and quality assessed the included studies. Factors were identified using an inductive thematic approach and mapped to the Theoretical Domains Framework (TDF). Comparisons between dental and other settings were explored. Registration number: PROSPERO_CRD42016037174.
Results
Searches identified 689 publications across primary care and 432 across dental care. Included studies (nine and seven, respectively) were assessed as of variable quality. They covered 46 countries, of which 12 were low and middle-income countries (LMICs). Across the two reviews, 30 factors were identified, with ‘patient/condition characteristics’, ‘patient influence’ and ‘guidelines & information’ the most frequent. Two factors were unique to dental studies: ‘procedure possible’ and ‘treatment skills’. No factor related only to LMICs.
Conclusions
A comprehensive list of factors associated with antibiotic prescribing to adults with acute conditions in primary care settings around the world has been collated and should assist theory-informed design of new context-specific stewardship interventions.
Introduction
Use of antibiotics is contributing to the rise in drug-resistant infections.1,2 One way to slow the spread of resistant bacteria is by improved stewardship of antibiotics: using them more carefully and reducing the number of prescriptions. Globally, dentists are major prescribers of antibiotics, accounting for an estimated 7%–10% of all antibiotic prescriptions.3 Worryingly, some countries, including the USA and Canada, are currently seeing increases in dental antibiotic use.3–6 Across NHS England during 2017, 5.2% of antibiotic prescriptions were from primary dental care.7 Most of these were systemic drugs prescribed for adult patients presenting at urgent appointments with severe pain and/or acute infection.8,9 Antibiotics are not, however, appropriate for the treatment of pain and guidance states that a dental procedure is more usually indicated to remove the source of the problem; antibiotics are only required in the presence of a spreading or systemic infection.10–12 It has been estimated that antibiotics may be prescribed unnecessarily for as many as 80% of dental patients in the UK.13,14 Dental antibiotic stewardship interventions are therefore necessary.
The behavioural and social sciences are increasingly appreciated as fundamental to the development of interventions aimed at improving people’s health and modifying clinician/patient behaviours.15 Although interventions attempting to change antibiotic prescribing behaviour are regularly reported in the scientific literature, largely in hospital and primary medical care settings, few have been explicitly designed using behaviour change theory16,17 or tested in primary dental care.18 A more comprehensive understanding of the determinants of antibiotic prescribing behaviour should improve the effectiveness and sustainability of future interventions.19
With antibiotic resistance being a global problem that requires a global solution, the health research community has turned its focus towards understanding specific issues for its emergence and spread in hotspots such as South-East Asia.20,21 An increase in interest about antibiotic prescribing in these areas has become apparent, including from the WHO and a number of low- and middle-income countries (LMICs).20–22 Including international studies in the review enabled comparisons between factors in different parts of the world.
Prescribing of antibiotics for paediatric patients is particularly high in primary medical care.23 In contrast, NHS England prescribing statistics show 87% of dental antibiotics in 2015/16 were prescribed to adults, with most linked to urgent rather than routine dental care.8,9 This study aimed, therefore, to identify the factors associated with decisions about whether to prescribe systemic antibiotics for adult patients during urgent appointments/with acute conditions. In order to maximize the opportunity to translate existing knowledge between primary care settings, first the factors influencing antibiotic prescribing decisions for urgent consultations in all primary care settings were explored. Owing to the plethora of studies relating to antibiotic prescribing across primary medical care, an umbrella review (systematic review of systematic reviews) was chosen as an efficient way to identify factors and summarize the extensive evidence base. Next, a systematic review was undertaken to collate the sparse dental-specific evidence base. Finally, the factors were compared and contrasted between clinical settings and between countries (including LMICs) in order to inform the development of future antibiotic stewardship interventions.
Methods
Protocol and research questions
The protocol for this two-part systematic review was registered in PROSPERO CRD42016037174. An umbrella review (also known as a systematic review of systematic reviews or overview of systematic reviews) was undertaken to answer the first research question: ‘What is known from published systematic reviews about the factors associated with the decision whether to prescribe systemic antibiotics to adult patients across urgent primary care?’. A systematic review was undertaken for the second: ‘What is known from the published literature about the factors associated with the decision to prescribe systemic antibiotics to adult patients in urgent primary dental care?’. Primary care was defined as ‘the first point of contact in the healthcare system …. including general practice, community pharmacy, dental and optometry services.’.24 Urgent primary dental care included out-of-hours (OOH)/emergency dental services provided in community settings.
Both reviews conformed to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.25 In addition, the umbrella review was guided by the Joanna Briggs Institute methodology for umbrella reviews.26
Search strategies
In July 2018, five databases were searched from their earliest dates: Ovid MEDLINE, Ovid EMBASE, Ovid PsychINFO, Web of Science and the British Library e-thesis on-line service (EThOS). Separate search strategies and inclusion/exclusion criteria were developed for each review in collaboration with an information specialist (Tables S1 and S2, available as Supplementary data at JAC Online). The search strategies used a ‘human’ search limit as animal studies were not eligible for the reviews and an ‘English language’ limit due to a lack of resources for translation. The reference lists of included studies were manually searched for additional potentially relevant studies; other papers were also identified through discussion among the authors. After performing the full search for each review, titles and abstracts retrieved from each database were combined in EndNote X7 and duplicates were removed. Separate EndNote libraries were used for the umbrella review across primary care and the systematic review in primary dental care.
Study selection
Studies published as original research articles in peer-reviewed journals were included if they contained factors associated with decisions about whether to prescribe systemic antibiotics for the treatment of adult patients with acute conditions in non-specialist primary care settings. Studies related to specialist care delivered in primary care settings and/or primary care services delivered in hospital settings were excluded.
For the umbrella review, a sensitive approach to the search was employed: systematic reviews were included if they reported, as a minimum, factors relating to the provision of care for adults with acute conditions in primary care settings. Two authors (W. T. and J. A. T. S.) screened all titles and abstracts independently for potential relevance. The full texts of all studies identified as potentially relevant were then assessed for inclusion eligibility independently by the same two authors. Discrepancies or disagreements were resolved through discussion.
For the systematic review, a more specific application of the eligibility criteria was employed: primary research studies (qualitative, quantitative and mixed methods) were included only if they reported on the provision of care for adults with acute dental conditions (pain and/or infection) in primary dental care settings. Studies that included additional types of care, such as prophylactic use of antibiotics for routine procedures or the provision of care in specialist as well as primary dental care settings, were excluded. Case studies were also excluded. Two authors (W. T. and G. V. A. D.) screened all titles and abstracts independently for potential relevance. The full texts of all studies identified as potentially relevant were then assessed for inclusion eligibility independently by the same two authors. Discrepancies or disagreements were resolved through discussion.
Quality assessment
Quality assessment of the systematic reviews included in the umbrella review used the Critical Appraisal Skills Programme (CASP) Checklist for Systematic Reviews (Table S3).27 Two authors (W. T. and J. A. T. S.) independently quality assessed the studies included in the umbrella review, with discrepancies or disagreements resolved through discussion.
Quality assessment of the primary research studies included in the systematic review of primary dental care used the 16 criteria of the Quality Assessment Tool for Studies with Diverse Design (QATSDD) (Table S4).28 One author (W. T.) quality assessed all of the studies included in the systematic review and another author (V. R. A.) independently assessed >50% (4/7), with discrepancies or disagreements resolved through discussion.
Analysis and synthesis
All included papers were imported into NVivo 11 as electronic pdf versions for thematic coding and synthesis. Thematic synthesis was an inductive, iterative process that broadly consisted of three stages: (i) free line-by-line coding of the Results and Discussion sections of the included papers; (ii) organization of these ‘free codes’ into related areas; and (iii) the identification, development and refinement of detailed descriptions of the factors associated with antibiotic prescribing.29 To assist the organization of the free codes into related areas, they were first grouped according to whether they related to clinician, patient, clinical context or wider social/political context, as this structure was presented in several of the systematic reviews included in the umbrella review across primary care.30–32 To assist the identification, development and refinement of the factors associated with antibiotic prescribing, the Theoretical Domains Framework (TDF) was used to ensure clarity of meaning for each influence on behaviour being characterized. The TDF is a theory-informed approach to identify determinants of behaviour and support behaviour change intervention design.33
Given the heterogeneous nature of the included studies, many of the findings in these studies were irrelevant to the research question; only findings of direct relevance to the aims of the umbrella and systematic review were coded.
Synthesis of the studies in the umbrella review across primary care
Codes were produced initially for the umbrella review across primary care by two authors (W. T. and J. A. T. S.) working independently; discrepancies or disagreements were resolved through discussion. To ensure that the factors identified related to the population of interest, identified factors were cross-checked back to the underpinning references within the umbrella review’s constituent systematic reviews. Codes that were found not to relate to the specific criteria of this review (e.g. studies only about paediatric patients, hospital settings or prophylactic prescribing) were excluded from the synthesis.
Synthesis of studies in the systematic review of primary dental care
The dental care studies were analysed using the bank of codes produced from the umbrella review across primary care by two authors (W. T. and G. V. A. D.) working independently; discrepancies or disagreements were resolved through discussion. Where necessary, additional codes were included for new factors as they emerged from the dental studies.
Independent checks
Following completion of synthesis of the umbrella and systematic reviews, a group of authors (W. T., S. H. P., R. R. C. M., G. V. A. D. and J. A. T. S.) and the study’s patient and public involvement (PPI) representatives undertook a sense check of the full list of identified factors. An independent check of the factors/definitions and how they mapped to the TDF was then undertaken by S. T.-C. Discrepancies or disagreements were resolved through discussion.
Comparing the factors
The final stage was to compare and contrast the factors identified between the settings: across primary care versus primary dental care specific; and between countries (including UK versus other countries and high-income countries versus LMICs).34
Results
Study selection
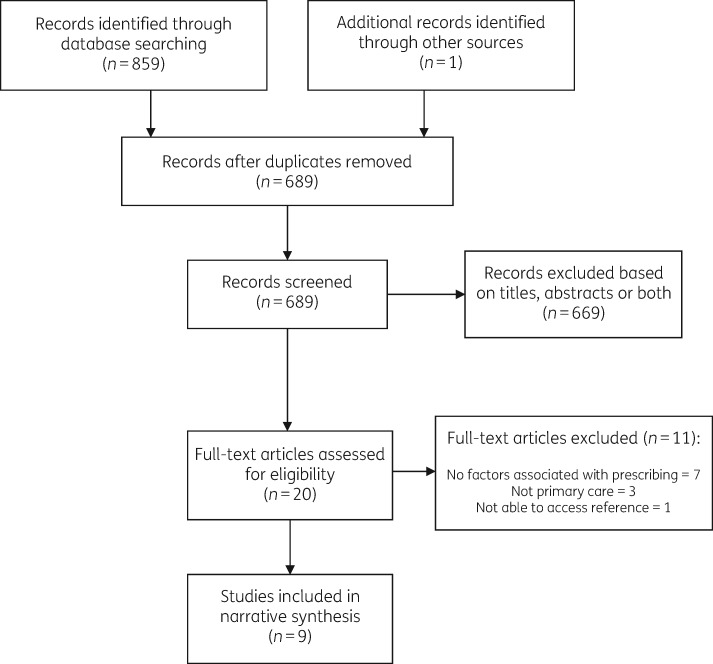
For the umbrella review across primary care, 689 studies were identified for possible inclusion in the review. Of these, nine studies met the inclusion criteria and were included in the final synthesis.30–32,35–40 Details of the study selection process are shown in Figure 1.
Figure 1.
PRISMA flow chart detailing selection of the systematic reviews included in the umbrella review of factors associated with the decision whether to prescribe systemic antibiotics for adult patients with acute conditions across primary care.
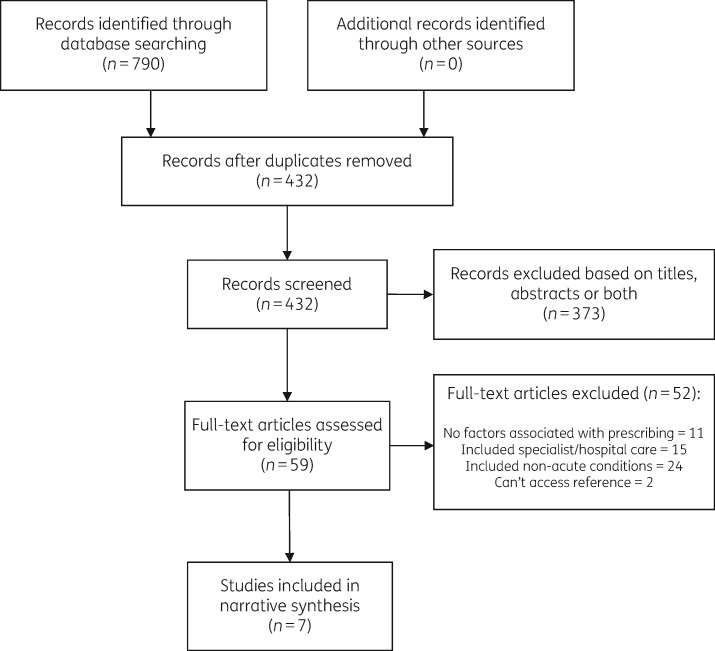
For the systematic review of primary research studies, 432 studies were identified for possible inclusion in the review. Of these, seven studies met the inclusion criteria and were included in the final synthesis.13,14,41–45 Details of the study selection process are shown in Figure 2.
Figure 2.
PRISMA flow chart detailing selection of the primary research studies included in the systematic review of factors associated with the decision whether to prescribe systemic antibiotics for adult patients with acute dental conditions/during urgent primary dental care appointments.
Study characteristics
Umbrella review: characteristics of the included systematic reviews
The characteristics of the nine systematic reviews included in the umbrella review across primary care are described in Table 1. Within these systematic reviews, a total of 98 qualitative and quantitative primary research studies contributed factors relating to adult patients with acute conditions in primary care settings. Across these 98 studies, the participants were primary care professionals (including doctors, nurses and pharmacists) working in 45 countries. Eleven of the countries were LMICs and 26 studies were undertaken in the UK (Table S5). The studies had a date range of 1990–2017.
Table 1.
Characteristics of studies included in the umbrella review of factors associated with prescribing of systemic antibiotics to adult patients with acute conditions across primary care
| Author (lead), year | Objectives | Participant characteristics | Setting/context | No. of databases searched | Relevant constituent studies* |
||
|---|---|---|---|---|---|---|---|
| date range | countries included | number, type | |||||
| Germeni, 201835 | Primary care practitioner experiences of antibiotic prescribing for acute respiratory tract infections. | primary care professionals (including GPs, nurses and pharmacists) | primary care | 6 | 1998–2014 | Australia, Belgium, Finland, Germany Hungary, Iceland, India, Italy, Lithuania, Netherlands, Norway, Poland, Portugal, Russia, Spain, UK, USA | 22 qualitative studies |
| Keller, 201836 | What is known about effective ambulatory AS interventions and identify barriers to and facilitators of successful implementation of ambulatory AS interventions? | unclear | ambulatory care | 6 | 1999–2017 | Belgium, China, Denmark, France, Germany, Hungary, Ireland, Italy, Netherlands, Norway, Poland, Spain, Sweden, Switzerland, UK, USA | 24 qualitative & quantitative studies |
| Lopez-Vazquez, 201230 | To identify the factors, attitudes and knowledge linked to mis-prescription of antibiotics. | doctors | primary care | 2 | 1990–2007 | Australia, Belgium, Canada, Denmark, Germany, Hong Kong, Korea, Malaysia, Ireland, Netherlands, Spain, Taiwan, UK, USA | 24 quantitative studies |
| McKay, 201631 | Assessment of the factors associated with antibiotic prescribing for respiratory tract infections (RTIs). | prescribers for patients with respiratory tract infection | all healthcare | 3 | 1997–2013 | Belgium, Canada, Finland, Germany, Hungary, Italy, Netherlands, Norway, Poland, Slovakia, Spain, Sweden, UK, USA | 18 quantitative studies |
| Ness, 201637 | To explore the influences on the antimicrobial prescribing behaviour of independent nurse prescribers. | nurse prescribers | all healthcare | 7 | 2005–12 | UK, USA | 2 qualitative & quantitative studies |
| Rezal, 201538 | To review knowledge, perceptions and behaviour of physicians in relation to antibiotic prescribing. | physicians of patients with respiratory tract infection | all healthcare | 6 | 2010–14 | Bangladesh, Belgium, Hungary, India, Spain, UK, Poland, Italy, Norway, Netherlands | 4 qualitative & quantitative studies |
| Rodrigues, 201332 | To explore physicians’ perceptions of factors influencing antibiotic prescribing. | physicians | all healthcare | 1 | 2001–11 | Germany, Iceland, India, Netherlands, Spain, Sweden, UK, USA | 13 qualitative studies |
| Tonkin-Crine, 201139 | To understand how GPs perceive antibiotic prescribing. | GPs of patients with acute conditions | primary care | 5 | 2002–10 | Belgium, France, Iceland, Netherlands, Norway, Poland, Spain, UK, USA | 7 qualitative studies |
| Touboul-Lundgren, 201540 | To describe the influence of culture on antibiotic use, using a framework of cultural dimensions. | unclear | primary care | 10 | 1997–2013 | Austria, Belgium, Bulgaria, Czech Republic, Denmark, East Germany, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, Malta, Morocco, Nepal, Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Thailand, Turkey, UK, Yugoslavia (former) | 6 qualitative & quantitative studies |
Relevant studies are the 98 primary research papers included within the systematic reviews that relate to adult patients in non-specialist primary care settings. Further details of those 98 papers are provided in Table S5.
Systematic review: characteristics of the included primary research studies
The characteristics of the seven studies included in the systematic review of primary dental care are described in Table 2. The study participants were all dentists working in primary dental care (including OOH dental clinics). Two of the studies took place in LMICs (Turkey and Iran) and the other five were UK studies. The studies had a date range of 2000–16.
Table 2.
Characteristics of studies included in the systematic review of factors associated with prescribing of systemic antibiotics to adult patients with acute dental conditions/during urgent primary dental care
| Author (lead), year | Objectives | Country | Dental care setting | Clinician characteristics | Patient characteristics (if applicable) | Study type/design | Size of population | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Cope, 201613 | To describe factors associated with antibiotic prescription in the absence of spreading infection or systemic involvement. | UK | general dental practice | NHS or private general dental practitioners | adults with pulpal, apical or periodontal pathology | quantitative/cross-sectional prospective | 42 general dental practitioners/568 cases | Features of the healthcare environment, such as clinical time pressures, and patient-related characteristics, such as expectations for antibiotics and refusal of operative treatment, are associated with antibiotic prescribing in the absence of infection. |
| Dailey, 200141 | To investigate the therapeutic prescribng of antibiotics to patients presenting for emergency dental treatment. | UK | OOH dental | NHS dentists | walk-in emergency dental patients | quantitative/cross-sectional prospective | 55 dentists/1011 cases | The majority of patients attending the emergency dental clinics had pain, with a large proportion having localized infections either as pulpitis or localized dental abscess. |
| Kaptan, 201342 | To gather information about Turkish general dental practitioners’ treatment approaches towards endodontic emergencies, antibiotic-prescribing habits, and participation in lifelong learning programmes. | Turkey | general dental practice | general dental practitioners | NA | quantitative/survey | 589 analysed/1400 distributed | There have been discrepancies between taught and observed practice. Educational initiatives are needed to prevent inappropriate prescription of antibiotics. |
| Newlands, 201643 | To understand the barriers to and facilitators of using local measures instead of prescribing antibiotics to manage bacterial infections. | UK | not clear | general dental practitioners | NA | qualitative/semi-structured interviews | 30 interviews | Results suggest a number of intervention functions through which future interventions could change general dental practitioners’ antibiotic prescribing for bacterial infections, including through training, modelling or incentivization. |
| Palmer, 200044 | To study the therapeutic prescribing of antibiotics by general dental practitioners. | UK | general dental practice | general dental practitioners | patients with an acute dental infection | quantitative/survey | 891 analysed/1546 distributed | Therapeutic prescribing of antibiotics in general dental practice varies widely and is suboptimal. Practitioners were generally not influenced by patient’s expectations of receiving antibiotics, but would prescribe when under pressure of time, if they were unable to make a definitive diagnosis, or if treatment had to be delayed. |
| Tulip, 200814 | To investigate the clinical management of patients attending for emergency dental treatment. | UK | OOH dental | general dental practitioners | patients with an acute dental condition | quantitative/retrospective data analysis | 1167 patient records | General dental practitioners working within the OOH services are not adhering to current clinical and best practice guidelines with respect to patient examination, diagnosis, management, and in particular the correct prescribing of antibiotics for dental infections. |
| Vessal, 201145 | To evaluate the knowledge and practices of dentists in Shiraz, Iran regarding their use of antibiotics for patients with dentoalveolar infections. | Iran | not clear | dental practitioners | NA | quantitative/ survey | 219 analysed/450 distributed | Guidelines on rational antibiotic use are needed for dental practitioners in the Islamic Republic of Iran. |
Overlap between the reviews
None of the seven dental studies of the systematic review was included in any of the nine systematic reviews within the umbrella review.
Overlap within the systematic reviews of the umbrella review
Analysis of the overlap between primary research studies within the umbrella review’s systematic reviews found that 12/98 studies appeared in two of the systematic reviews, 5/98 appeared in three of them and none appeared in more than three (Table S5).
Quality assessment
For the umbrella review, the included systematic reviews were generally good quality. All of the CASP criteria were fulfilled (or not applicable) for seven of the nine. The other two systematic reviews failed to show quality assessment of their included studies.
For the systematic review within primary dental care, quality of the included studies was more variable, with QATSDD scores ranging from 11 to 39 out of a possible total of 40. General weaknesses across the studies concerned identification of a theoretical framework, sample size, validity of measurement tools and evidence of user involvement in study design. Detailed results of these assessments are presented in Tables S3 and S4. No papers were excluded based on these assessments as all included results that were relevant to meeting the aims of the systematic review.
Thematic analysis
A total of 30 factors associated with prescribing were identified across both the umbrella review of primary care and the systematic review of primary dental studies. Descriptors of each of these factors and how they map to the domains of the TDF are presented in Table 3. Details of which factors were identified from each review are shown in Tables S6 and S7, respectively.
Table 3.
Factors associated with prescribing of antibiotics for acute conditions in primary care setting: short name, descriptor and mapping to the TDF
| Factor short name | Descriptor | TDF domain |
|---|---|---|
| Access | Access to the right care for the right patient at the right time, including when the practice is shut (e.g. weekends), whilst the patient is on holiday, for patients who live a distance from the practice continuity of care by a single clinician, and if necessary access to specialist care through referral services and laboratory equipment and/or testing. | Environmental context & resources |
| Accountability | Clinicians held accountable (or feel like they are held accountable) for their antibiotic prescribing patterns. | Beliefs about consequences |
| Antibiotic awareness | Level of clinician knowledge about the relationship between antibiotic use and resistant infections. | Knowledge |
| Antibiotic beliefs | Level of personal responsibility towards antibiotics, including blaming others for misuse of antibiotics and/or resistant infections. Belief that antibiotics are low risk: describing use as ‘Better safe than sorry’. | Beliefs about consequences |
| Clinician characteristics | Clinician age, sex, years in practice, location of primary dental qualification, previous clinical experience. | Does not map to TDF |
| Competing demands | Availability of sufficient time to treat patient in accordance with guidelines, including ‘sit and wait’ approach to booking urgent patients and other patients waiting. | Environmental context & resources |
| Conflict | Fear of conflict with patient due to dissatisfaction and subsequent loss of the patient to the practice. | Emotion |
| Efficacy of options | Beliefs about the efficacy of different treatment options, including, ability of antibiotics versus other approach/procedure to resolve conditions and belief that a procedure may worsen symptoms. | Beliefs about consequences |
| Fear about outcome | Fear about adverse outcomes, including anxiety about making a mistake and the prospect of serious complications if patients with symptoms go without antibiotics. Described as ‘just-in-case’ or ‘belt-and-braces’. | Emotion |
| Feelings about decisions | Feeling about the appointment and decisions, including frustration at lack of consent for gold standard treatment or clinician's emotional state at the appointment start. | Emotion |
| Financial burden | Beliefs about financial burden on patients, including ability to pay for clinical consultation or fees for laboratory tests. | Beliefs about consequences |
| Fix the problem | Goal for the appointment is to fix the patient's problem: symptomatic relief and/or preventing the problem returning. | Goals |
| Guidance–practice gap | Gap between guidance and clinical practice, including clinician concerns about the application of the guidelines to specific clinical encounters and belief about whether their clinical practice (such as delayed prescribing in dentistry) adheres to relevant guidance. | Beliefs about consequences |
| Guidelines & information | Knowledge about relevant guidelines and other sources of information (such as from the internet and pharmaceutical company medical representatives), including appropriate treatment of acute conditions/prescribing. | Knowledge |
| Habits | Prescribing habits of clinician, including patterns of prescribing and practitioner-level variation. | Memory, attention & decision processes |
| Healthcare context | Healthcare system context in relation to prescription of antibiotics, including perceived pressure to reduce antibiotic prescribing, ability to reuse a prescription, and availability of antibiotics without a prescription. | Environmental context & resources |
| Incentives | Incentives for and against antibiotic use, including the impact of a ‘time is money’ business approach on unscheduled/urgent appointments and the financial risk of losing dissatisfied patients. | Reinforcement |
| Patient/condition characteristics | Characteristics of the patient (age, sex, ethnicity), their presenting condition (signs, symptoms and diagnosis), their medical history/comorbidities and their socioeconomic background (level of education, affluence/deprivation etc.). | Does not map to TDF |
| Patient influence | Influence of (perceptions about) patients, including: antibiotic-seeking behaviour (expectations/demand); negotiating skills; patient knowledge/attitudes towards antibiotics; fear of adverse outcomes without antibiotics; and willingness/ability to accept operative dental procedure. Also the influence of poor/irregular attenders and the impact of late-running unscheduled appointments making other patients who are waiting for their scheduled appointment angry. | Social influences |
| Patient management | Skills in patient management, diagnosis, treatment planning and consent, including eliciting concerns, interpreting the patient’s description of their symptoms, managing anxious patients, managing expectations and avoiding confrontation. Negotiation, persuasion, education and hedging. Communication skills. | Skills |
| Patient satisfaction | Belief about patient satisfaction, including impact of failing to meet patient expectations, impact of repeat visits and failure to relieve symptoms. | Beliefs about consequences |
| Peers & colleagues | Influence of peers and other colleagues in practice, including: prescribing patterns locally; professional courtesy by avoiding encroaching when treating another clinician's patient; confusion caused by different treatment patterns by different clinicians (patients uncertain what is correct); and utility of peer support when dealing with demanding situations. | Social influences |
| Planning & consent | Belief about ability to plan treatment and gain consent during urgent appointments, including ‘do nothing’ options and managing anxious/phobic patients. | Beliefs about capabilities |
| Practice characteristics | Characteristics of the practice, including public/private/insurance provision, geographic location (rural versus urban) and country. | Does not map to TDF |
| Procedure possible | Belief about whether it is possible to provide treatment due to issues beyond the dentist’s skills during urgent appointments, including the ability to achieve adequate local anaesthesia and/or to provide operative treatment (in accordance with guidelines) to dentally phobic patients without sedation. | Beliefs about capabilities |
| Professional role | Influence of professional role on managing urgent appointments, including what is the means to care for patients, and feeling ‘morally obliged’ to offer something tangible (to ‘do nothing’ is difficult). The ability to prescribe antibiotics and use own ‘rules of thumb’ are both signs of expertise and power. | Professional/social role & identity |
| Relationship | Desire to build/maintain a good clinician-patient relationship. | Goals |
| Risk perception | Beliefs about risks when managing the patient's condition, including worsening of the condition, failure of (or inability to complete) an operative procedure, and pain during or after provision of a procedure or medicolegal complaint. | Beliefs about consequences |
| Treatment skills | Skills in providing urgent procedures, including placing local anaesthetic by injection in difficult clinical situations or lancing an abscess in the presence of swelling. | Skills |
| Workload | Belief about impact on workload, including time taken to explain treatment options, gain informed consent, deliver treatment options and/or treat the patient another day on recall. | Beliefs about consequences |
Three factors did not map to the TDF: clinician characteristics, patient/condition characteristics and practice characteristics. Upon inspection it was agreed by the authors that they should be classed as non-modifiable factors. The most frequently identified non-modifiable factor, ‘patient/condition characteristics’, was found in all systematic reviews included within the umbrella review and six out of seven dental studies within the systematic review.
Identifying potential determinants of behaviour
The 27 factors that mapped to the TDF were classed as potentially modifiable determinants of antibiotic prescribing in primary care. Of these, 20 were identified in both reviews; 5 factors were identified only from the umbrella review across primary care and 2 factors only from the systematic review in primary dental care (Table 4). As with previously published systematic reviews about antibiotic prescribing, the factors were found to group into clinician-related, patient-related, clinical context-related and wider social–political context-related.30–32,36
Table 4.
Summary of potentially modifiable determinants of behaviour associated with the decision whether to prescribe systemic antibiotics for adult patients with acute conditions, showing a comparison between factors identified in the umbrella review across primary care and/or systematic review of primary dental care
| Both umbrella and systematic review | Umbrella review across primary care studies only | Systematic review of dental care studies only |
|---|---|---|
| Access | accountability | procedure possible |
| Competing demands | antibiotic awareness | treatment skills |
| Efficacy of options | antibiotic beliefs | |
| Fear about outcome | conflict | |
| Feelings about decisions | financial burden | |
| Fix the problem | ||
| Guidance–practice gap | ||
| Guidelines & information | ||
| Habits | ||
| Healthcare context | ||
| Incentives | ||
| Patient influence | ||
| Patient management | ||
| Patient satisfaction | ||
| Peers & colleagues | ||
| Planning & consent | ||
| Professional role | ||
| Relationship | ||
| Risk perception | ||
| Workload |
Potentially modifiable factors: across primary care
The ‘patient influence’ factor was found in all of the systematic reviews of the umbrella review (Table 2). As described in Table 1, this included but was not limited to demand for antibiotics and/or the clinician’s perception of the patient’s desire for them. Five factors were found only in the umbrella review: ‘accountability’, ‘antibiotic awareness’, ‘antibiotic beliefs’, ‘conflict’ and ‘financial burden’ (Table 4).
Potentially modifiable factors: primary dental care
Only ‘guidelines & information’ was found in all of the dental studies (Table 3). Two factors were found only in dental studies: ‘procedure possible’ and ‘treatment skills’.13,42,43 Dentists’ beliefs about whether it was possible to deliver operative dental procedures in accordance with guidelines (due to issues beyond the dentist’s skill) were identified as important (‘procedure possible’).13,43 Similarly, ‘treatment skills’ to undertake difficult elements of urgent dental procedures, such as ‘achieving adequate anaesthesia’ and ‘how to lance an abscess when swelling is present’, were included in two of the dental studies.13,42,43 Antibiotics were identified as a way of balancing the ‘competing demands’ of a busy list of patients booked for routine dental care with the addition of unscheduled patients, sometimes as ‘sit and wait’ due to lack of available appointment slots.13,14,41,43,44
Comparing potentially modifiable factors: between primary care settings including dental care
Twenty factors were found in both the umbrella review across primary care and the systematic review in primary dental care (Table 4). Of these, ‘patient influence’ was the most frequently identified factor, being found in all of the systematic reviews of the umbrella review and six of the seven dental studies of the systematic review (Table 3).
Communication with patients during urgent appointments, including managing anxious patients and negotiation towards a shared decision, were found to be important to the prescribing decision in both dental and wider healthcare settings (‘patient management’).14,32,36,38,43 Clinicians’ fear about the potential for adverse outcomes, including when the patient had reduced access to medical/dental services (such as when going away on holiday or at weekends/bank holidays) were frequently identified (‘fear about outcome’ and ‘access’).30–32,35,38–41,43 Maintaining a good patient–clinician relationship, including by avoiding conflict, was an important goal shared across primary care and primary dental care, where enduring relationships are central to the model of care provision (‘relationship’).31,35,36,38,39,43
Potentially modifiable factors: comparing countries
‘Accountability’ was the only factor not identified from any of the UK-based studies included within the umbrella review’s systematic reviews.36 It has, however, been reported as important in at least one recent UK study. When exploring the experience of prescribers in OOH primary care settings, it was found that nurse practitioners felt greater accountability for their antibiotic prescribing than general practitioners (GPs).46
Eleven factors were identified from studies involving LMICs; no factors were identified only from studies undertaken in LMICs (Table 5). Exploring the detail within the factors, however, found that access to internet-based ‘guidelines & information’ was lower in LMICs compared with high-income countries.38 Furthermore, pharmaceutical industry medical representatives were identified by several non-UK studies as being an important source of ‘guidelines & information’, especially in LMICs where local guidelines were not always available.30,32,35,38 Upon closer examination of the studies included in the reviews, the medical representatives most often influenced decisions about what to prescribe; only one of the studies referenced within the umbrella review’s systematic reviews was about whether to prescribe antibiotics.32,47
Table 5.
Summary of potentially modifiable determinants of behaviour associated with the decision whether to prescribe systemic antibiotics for adult patients with acute conditions, showing a comparison between those identified in studies of high-income countries and LMICs
| High-income countries only | High-income countries and LMICs | LMICs only |
|---|---|---|
| Accountability | access | |
| Antibiotic awareness | antibiotic beliefs | |
| Efficacy of options | competing demands | |
| Feeling about decisions | conflict | |
| Guidance–practice gap | fear about outcome | |
| Guidelines & information | financial burden | |
| Incentives | fix the problem | |
| Patient management | habits | |
| Patient satisfaction | healthcare context | |
| Peers & colleagues | patient influence | |
| Planning & consent | treatment skills | |
| Professional role | ||
| Relationship | ||
| Risk perception | ||
| Procedure possible | ||
| Workload |
The ability to use a prescription more than once was identified from studies involving LMICs.32,38,48 Further differences between UK-based and other studies were found within the ‘healthcare context’ factor, including the availability of antibiotics without a prescription.35,42
Discussion
A comprehensive list of potentially modifiable and non-modifiable factors associated with the decision whether to prescribe systemic antibiotics for adults with acute conditions in primary care has been collated. Mapping of the potentially modifiable factors to the TDF has provided a resource for those wishing to develop new antibiotic stewardship interventions informed by behavioural theory. By identifying variation within non-modifiable factors between clinical contexts, it provides addition information to enable targeting of specific interventions at specific groups. By comparing and contrasting the potentially modifiable factors between settings, the results should inform the design of future antibiotic stewardship interventions. It should also enable the identification of elements of existing antibiotic stewardship interventions which could be amenable for translation into new settings.
With antibiotic resistance recognized as an important element of global sustainable development, a strength of this study is its inclusion of international studies, including studies from LMICs.21,49 Most of the sparse dental literature base (five out of seven studies) originated in the UK (Table 2). This pattern was also identified in a systematic review of dental antibiotic stewardship interventions, where all five of the intervention tests in general dental practices were UK based.18 Researchers planning to implement existing dental antibiotic stewardship interventions in other countries (or to develop new ones) should first seek to understand which factors are relevant to the prescribers’ decisions in their specific context.
Owing to the heterogeneous nature of the included studies, attribution of causality between the factors found to be associated with antibiotic prescribing and actual prescribing rates was not possible. Similarly, it was not possible to say whether factors identified from the umbrella review across primary care but not identified in the systematic review of dental studies were relevant in dental settings; it could only be concluded that these factors were not found in the published dental studies within this review. Although the 30 factors identified have been presented as distinct, many are interlinked, such as the relationships between ‘patient satisfaction’, ‘conflict’ and ‘incentives’. There was a risk of the factors being either too generic to be useful or too specific (and hence too numerous) to be manageable. To address this, synthesis was guided iteratively through reference to the TDF.
Social scientists are part of the contexts they study and it is not possible to step outside in order to study the topic entirely objectively.50 The authors were acutely aware, therefore, of their unique knowledge, attitudes and expectations in relation to antibiotic use. Recognizing this, the authors attempted to remain exact, sincere and impartial when handling the data.51 Results were checked for sense and understanding with non-clinical colleagues, including the study’s PPI advisers. Nevertheless, the authors acknowledge that the conclusions were inherently related to their specific interpretations and that other equally valid conclusions could be drawn from the same data.
The broad range of methodologies employed within the included studies [systematic reviews, meta-ethnographies and primary research (both quantitative and qualitative)] complicated the quality assessment as well as extraction, interpretation and presentation of the results. All of the included dental studies relied on self-reporting by clinicians about real or simulated clinical cases through interviews and/or questionnaires. Studies that rely on self-reported perceptions are inherently at risk of bias in the way people account for their and others’ behaviour and people are usually not aware of what influences their unconscious/instinctive behaviour.52 This was a recognized limitation of the included studies and could account in part for the two most frequently found factors across the two reviews: ‘patient/condition characteristics’ and ‘patient influence’. A study of clinical autonomy in relation to prescribing in general practice found that to balance the requirements of the patients and the healthcare system, doctors may state ‘clinical need’ when it suits them to do so, otherwise they blame ‘patient demand’.53 Studies of GP consultations and with patients have found a mismatch between GP reports of patient expectations/demand for antibiotics and patient reports.54–56 Similar studies are required, therefore, to explore which factors influence actual prescribing decisions in general dental practice.
The results of these studies should assist the theory-informed design of new interventions (and the fine-tuning of existing interventions) aimed at helping clinicians to optimize their prescribing of antibiotics during urgent appointments. They will draw on the experience of existing multifactorial interventions developed for GPs that have been shown to be effective at reducing antibiotic prescribing. One intervention for managing adults with acute cough, GRACE INTRO, used enhanced communication skills and a point-of-care test for the C-reactive protein biomarker of bacterial infection (CRP POCT). The intervention positively influenced three factors identified in this review, as tested in the process evaluation of the trial: (i) increased clinician confidence to reduce antibiotic prescribing (‘guidance–practice gap’); (ii) increased perceived importance of decreasing prescribing (‘antibiotic awareness’); and (iii) reduced perceived risk of decreasing prescriptions (‘risk perception’).50,51
Conclusions
This study provides a robust identification of the breadth of factors associated with the decision whether to prescribe systematic antibiotics for adults presenting with acute conditions in a range of primary care contexts around the world. Further studies are needed to provide more detailed understanding of which factors are relevant determinants of behaviour during actual clinical encounters to inform the theory-informed design of context-specific antibiotic stewardship interventions.
Supplementary Material
Acknowledgements
This research was carried out as part of a PhD by the first author. With thanks to the PhD supervisors and PPI advisors, as well as to Judy Wright and Natalie King for their guidance as information specialists.
Funding
This work was supported by a University of Leeds Anniversary Research Scholarship as part of W. T.’s PhD research. W. T.’s on-going research is supported by the National Institute for Health Research (NIHR Doctoral Research Fellowship, Mrs Wendy Thompson, DRF-2016–09-148). In addition, W. T., S. H. P., G. V. A. D. and J. A. T. S. are supported by the NIHR infrastructure at Leeds. S. T.-C. is supported by NIHR through the Health Protection Research Unit (NIHR HPRU) in Healthcare Associated Infections and Antimicrobial Resistance at the University of Oxford in partnership with Public Health England (PHE)(HPRU-2012–10041).
Transparency declarations
W. T. received funds from Health Education England for speaking at continuing professional development events aimed at optimizing antimicrobial prescribing by primary care dentists and GPs in relation to acute dental conditions. W. T. had contracts with Bradford District Care NHS Trust, Cumbria Partnership NHS Trust and Integrated Dental Holdings Ltd to provide primary care dentistry on behalf of the NHS. S. H. P. oversees clinical trials/research funded by NIHR, industry (Solvay, GSK, Proctor & Gamble) and charities (Multiple Sclerosis Society and British Society for Oral & Dental Research). All other authors: none to declare.
Author contributions
W. T. undertook all aspects of this study and production of this paper for publication. All other authors contributed to design of the reviews and the process of finalizing the set of potentially modifiable and non-modifiable behaviours, as well as more specifically: S. T.-C. provided independent assessment of the factors and their mapping to the TDF, contributed to analysis and drafting of the manuscript; S. H. P. provided a sense check for the resulting themes and drafting of the manuscript; R. R. C. M. assisted with the iterative process of developing factors and mapping them to the TDF, contributed to analysis and drafting of the manuscript; G. V. A. D. provided independent assessment for elements relating to the systematic review of primary dental care studies and drafting of the manuscript; V. R. A. participated in the quality assessment of included studies for the systematic review of dental studies and critically reviewed the manuscript from a clinical and methodological perspective; J. A. T. S. provided independent assessments for all elements relating to the umbrella review across primary care, contributed to analysis and drafting of the manuscript.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health and Social Care.
References
- 1.UK Parliament. Health & Social Care Committee 11th Report: Antimicrobial Resistance 2018. https://publications.parliament.uk/pa/cm201719/cmselect/cmhealth/962/962.pdf.
- 2. Davies S, Gibbens N.. UK Five Year Antimicrobial Resistance Strategy 2013 to 2018. London: Department of Health, 2013. [Google Scholar]
- 3. Cleveland J, Kohn W.. Antimicrobial resistance and dental care: a CDC perspective. Dent Abstr 1998; 43: 108–10. [Google Scholar]
- 4. Roberts RM, Bartoces M, Thompson SE. et al. Antibiotic prescribing by general dentists in the United States, 2013. J Am Dent Assoc 2017; 148: 172–8.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Marra F, George D, Chong M. et al. Antibiotic prescribing by dentists has increased: why? J Am Dent Assoc 2016; 147: 320–7. [DOI] [PubMed] [Google Scholar]
- 6. Sivaraman SS, Hassan M, Pearson JM.. A national survey of pediatric dentists on antibiotic use in children. Pediatr Dent 2013; 35: 546–9. [PubMed] [Google Scholar]
- 7.Public Health England. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report. 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/759975/ESPAUR_2018_report.pdf.
- 8.NHS Digital. NHS Dental Statistics for England - 2015-16 https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/nhs-dental-statistics-for-england-2015-16.
- 9.NHS England. Quick Guide: Best Use of Unscheduled Dental Care Services https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/11/quick-guid-unscheduled-dental-care.pdf.
- 10.Faculty of General Dental Practitioners (FGDP). Antimicrobial Prescribing for General Dental Practitioners. 2012. https://www.fgdp.org.uk/guidance-standards/antimicrobial-prescribing-gdps.
- 11.Scottish Dental Clinical Effectiveness Programme S. Drug Prescribing for Dentistry 2016. www.sdcep.org.uk/published-guidance/drug-prescribing/. [DOI] [PubMed]
- 12.Joint Formulary Committee T. British National Formulary. London: BMJ Group and Pharmaceutical Press, 2018. [Google Scholar]
- 13. Cope AL, Francis NA, Wood F. et al. Antibiotic prescribing in UK general dental practice: a cross-sectional study. Community Dent Oral Epidemiol 2016; 44: 145–53. [DOI] [PubMed] [Google Scholar]
- 14. Tulip DE, Palmer NO.. A retrospective investigation of the clinical management of patients attending an out of hours dental clinic in Merseyside under the new NHS dental contract. Br Dent J 2008; 205: 659–64. [DOI] [PubMed] [Google Scholar]
- 15.Public Health England. Improving People’s Health: Applying Behavioural and Social Sciences to Improve Population Health and Wellbeing in England 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/744672/Improving_Peoples_Health_Behavioural_Strategy.pdf.
- 16. Charani E, Edwards R, Sevdalis N. et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis 2011; 53: 651–62. [DOI] [PubMed] [Google Scholar]
- 17.Public Health England. Antibiotic Prescribing and Behaviour Change in Healthcare Settings: Literature Review and Behavioural Analysis. Public Health England, 2015. https://www.gov.uk/government/publications/antibiotic-prescribing-and-behaviour-change-in-healthcare-settings. [Google Scholar]
- 18. Löffler C, Böhmer F.. The effect of interventions aiming to optimise the prescription of antibiotics in dental care—a systematic review. PLoS One 2017; 12: e0188061.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lorencatto F, Charani E, Sevdalis N. et al. Driving sustainable change in antimicrobial prescribing practice: how can social and behavioural sciences help? J Antimicrob Chemother 2018; 73: 2613–24. [DOI] [PubMed] [Google Scholar]
- 20. Zellweger RM, Carrique-Mas J, Limmathurotsakul D. et al. A current perspective on antimicrobial resistance in Southeast Asia. J Antimicrob Chemother 2017; 72: 2963–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Bank. Drug-Resistant Infections: A Threat to Our Economic Futurehttp://documents.worldbank.org/curated/en/323311493396993758/pdf/114679-REVISED-v2-Drug-Resistant-Infections-Final-Report.pdf.
- 22. Pearson M, Doble A, Glogowski R. et al. Antibiotic Prescribing and Resistance: Views from LMIC Prescribing and Dispensing Professionals. Report to WHO AMR Secretariat. London: London School of Hygiene and Tropical Medicine, 2018. [Google Scholar]
- 23. Ivanovska V, Hek K, Mantel Teeuwisse AK. et al. Antibiotic prescribing for children in primary care and adherence to treatment guidelines. J Antimicrob Chemother 2016; 71: 1707–14. [DOI] [PubMed] [Google Scholar]
- 24.NHS England. Primary Care Services https://www.england.nhs.uk/primary-care/.
- 25. Moher D, Liberati A, Tetzlaff J. et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2009; 8: 336–41. [DOI] [PubMed] [Google Scholar]
- 26. Aromataris E, Fernandez R, Godfrey C. et al. The Joanna Briggs Institute Reviewers’ Manual 2014: Methodology for JBI Umbrella Reviews. Adelaide: Joanna Briggs Institute, 2014. [Google Scholar]
- 27.Critical Appraisal Skills Programme C. CASP Checklist: 10 Questions to Help You Make Sense of a Systematic Review https://casp-uk.net/wp-content/uploads/2018/01/CASP-Systematic-Review-Checklist_2018.pdf.
- 28. Sirriyeh R, Lawton R, Gardner P. et al. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract 2012; 18: 746–52. [DOI] [PubMed] [Google Scholar]
- 29. Thomas J, Harden A.. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lopez-Vazquez P, Vazquez-Lago JM, Figueiras A.. Misprescription of antibiotics in primary care: a critical systematic review of its determinants. J Eval Clin Pract 2012; 18: 473–84. [DOI] [PubMed] [Google Scholar]
- 31. McKay R, Mah A, Law MR. et al. Systematic review of factors associated with antibiotic prescribing for respiratory tract infections. Antimicrob Agents Chemother 2016; 60: 4106–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rodrigues AT, Roque F, Falcao A. et al. Understanding physician antibiotic prescribing behaviour: a systematic review of qualitative studies. Int J Antimicrob Agents 2013; 41: 203–12. [DOI] [PubMed] [Google Scholar]
- 33. Atkins L, Francis J, Islam R. et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Sci 2017; 12: 77.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WorldBank. World Bank Country and Lending Groups https://datahelpdesk.worldbank.org/knowledgebase/articles/906519#High_income%20Accessed%202%20August%202017.
- 35. Germeni E, Frost J, Garside R. et al. Antibiotic prescribing for acute respiratory tract infections in primary care: an updated and expanded meta-ethnography. Br J Gen Pract 2018; 68: e633–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Keller SC, Tamma PD, Cosgrove SE. et al. Ambulatory antibiotic stewardship through a human factors engineering approach: a systematic review. J Am Board Fam Med 2018; 31: 417–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ness V, Price L, Currie K. et al. Influences on independent nurse prescribers' antimicrobial prescribing behaviour: a systematic review. J Clin Nurs 2016; 25: 1206–17. [DOI] [PubMed] [Google Scholar]
- 38. Rezal RSM, Hassali MA, Alrasheedy AA. et al. Physicians' knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Exp Rev Anti-Infect Ther 2015; 13: 665–80. [DOI] [PubMed] [Google Scholar]
- 39. Tonkin-Crine S, Yardley L, Little P.. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother 2011; 66: 2215–23. [DOI] [PubMed] [Google Scholar]
- 40. Touboul-Lundgren P, Jensen S, Drai J. et al. Identification of cultural determinants of antibiotic use cited in primary care in Europe: a mixed research synthesis study of integrated design “Culture is all around us”. BMC Public Health 2015; 15: 908.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dailey YM. Are antibiotics being used appropriately for emergency dental treatment? Br Dent J 2001; 191: 391–3. [DOI] [PubMed] [Google Scholar]
- 42. Kaptan RF, Haznedaroglu F, Basturk FB. et al. Treatment approaches and antibiotic use for emergency dental treatment in Turkey. Ther Clin Risk Manag 2013; 9: 443–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Newlands R, Duncan EM, Prior M. et al. Barriers and facilitators of evidence-based management of patients with bacterial infections among general dental practitioners: a theory-informed interview study. Implement Sci 2016; 11: 11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Palmer NAO, Pealing R, Ireland RS. et al. A study of therapeutic antibiotic prescribing in National Health Service general dental practice in England. Br Dent J 2000; 188: 554–8. [DOI] [PubMed] [Google Scholar]
- 45. Vessal G, Khabiri A, Mirkhani H. et al. Study of antibiotic prescribing among dental practitioners in Shiraz, Islamic Republic of Iran. East Mediterr Health J 2011; 17: 763–9. [PubMed] [Google Scholar]
- 46. Williams S, Halls A, Tonkin-Crine S. et al. General practitioner and nurse prescriber experiences of prescribing antibiotics for respiratory tract infections in UK primary care out-of-hours services (the UNITE study). J Antimicrob Chemother 2017; 73: 795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Caamaño F, Figueiras A, Gestal-Otero JJ.. Influence of commercial information on prescription quantity in primary care. Eur J Public Health 2002; 12: 187–91. [DOI] [PubMed] [Google Scholar]
- 48. Kotwani A, Wattal C, Katewa S. et al. Factors influencing primary care physicians to prescribe antibiotics in Delhi India. Fam Pract 2010; 27: 684–90. [DOI] [PubMed] [Google Scholar]
- 49.United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. Resolution Adopted by the General Assembly. Geneva: United Nations, 2015. [Google Scholar]
- 50. Ritchie J, Lewis J, Nicholls CM. et al. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage, 2013. [Google Scholar]
- 51. Ambedkar B. Who Were the Shudras? Bombay: Thacker & Co Ltd, 1946. [Google Scholar]
- 52. Conner M, Norman P.. Predicting Health Behaviour. Maidenhead: McGraw-Hill Education (UK; ), 2005. [Google Scholar]
- 53. Britten N. Prescribing and the defence of clinical autonomy. Sociol Health Illn 2001; 23: 478–96. [Google Scholar]
- 54. Stivers T, Mangione-Smith R, Elliott MN. et al. Why do physicians think parents expect antibiotics? What parents report vs what physicians believe. J Fam Pract 2003; 52: 140–7. [PubMed] [Google Scholar]
- 55. Gaarslev C, Yee M, Chan G. et al. A mixed methods study to understand patient expectations for antibiotics for an upper respiratory tract infection. Antimicrob Res Infect Control 2016; 5: 39.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cole A. GPs feel pressurised to prescribe unnecessary antibiotics, survey finds. BMJ 2014; 349: g5238.. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.