Abstract
Background.
Substance use behaviors have been identified as a risk factor that places juveniles at greater risk for engaging in delinquent behaviors and continual contact with the juvenile justice system. Currently, there is lack of research that explores comorbid factors associated with substance use, such as post-traumatic stress disorder (PTSD) symptoms, that could help identify youth who are at greatest risk. The aim of the present study was to examine if PTSD symptomology moderated the relationship between substance use disorder (SUD) symptoms and externalizing behaviors and commission of a violent crime; hypothesizing that risk would be heightened among youth with elevated SUD and PTSD symptomology compared to those with elevated SUD symptoms but lower PTSD symptoms.
Method.
The study included 194 predominantly male (78.4%), non-White (74.2%) juvenile justice youth between the ages of 9–18 (M=15.36). Youth provided responses to assess PTSD symptoms, SUD symptoms, and externalizing behaviors. Commission of a violent crime was based on parole officer report.
Results.
Findings indicated that SUD symptomology was associated with greater externalizing behaviors at high levels of PTSD symptomology. At low levels of PTSD symptomology, SUD symptoms were inversely associated with externalizing behaviors. An interactive relationship was not observed for commission of violent crimes.
Discussion.
Findings suggest that the association between SUD symptoms and externalizing behaviors among juvenile offenders may be best explained by the presence of PTSD symptomology.
Scientific Significance.
Addressing PTSD rather than SUD symptoms may be a better target for reducing risk for externalizing behaviors among this population of youth.
Keywords: substance use disorder, posttraumatic stress disorder, externalizing behaviors, juvenile justice
Introduction
In a given year approximately 2.4 million youth are arrested in the United States for engagement in illegal or violent behaviors, which accounts for almost one-fifth of all arrests1–3. Numerous risk models and assessment tools have been constructed to help identify factors that place juveniles at greater risk for engaging in delinquent behaviors4–6. Often included within these models and tools is the extent to which a youth engages in problematic substance use,7–9 as involvement with drugs or alcohol has been shown to increase the likelihood of continued contact within the juvenile justice system10,11 and is also associated with the severity of the committed offense12. Moreover, youth with a substance use disorder (SUD) are at increased risk for delinquency and recidivism3,13. The link between substance use and delinquency or recidivism may be in part explained by impulsivity, which is characterized by deficits in the ability to inhibit strong responses, lack of forethought and planning, an inability to persist on difficult tasks, and sensitivity to rewards and immediate gratification14. Given that dysregulation of impulse control is a common factor in engagement in both behaviors15, and may be a mechanism that helps explains why youth who engage in substance use are at increased risk for delinquency and recidivism.
It is also true that not every youth who uses substances will engage in delinquent acts, thus more research is needed to better understand comorbid factors that may help differentiate those youth who are at the highest risk. One factor that may play a key role in the relationship between adolescent substance use and delinquent behavior is trauma exposure, more specifically the development of posttraumatic stress disorder (PTSD) symptomatology3. It has been posited by theories such as the self-medication hypothesis16,17 that individuals who experience trauma and/or symptoms of PTSD may engage in substance use as a means to manage distress from traumatic experiences and PTSD symptoms 18. As such, there is a substantial body of literature documenting the association between trauma exposure 19,20, PTSD symptoms 21,22, and PTSD diagnosis 19,23 with substance use outcomes.
Among justice-involved youth, trauma exposure, such as experiencing physical and sexual abuse, domestic and community violence, or serious illness, is highly prevalent 24,25, with the Office of Juvenile Justice and Delinquency Prevention reporting that approximately 90% of youth have been exposed to such adverse events 26. These traumatic experiences are common factors that also aid in the development of PTSD among adolescent populations27. Given the high rate of trauma exposure among justice-involved youth, it is not surprising that rates of PTSD are up to three times higher among youth within juvenile justice populations than among general adolescent populations28,29. In addition to the high prevalence of PTSD among justice-involved youth, the development of PTSD is also concerning given its association with risk for recidivism5, substance abuse and dependence30, and other psychosocial problems such as risk for aggression and juvenile delinquency31,32.
There are several theories available to help understand the association between PTSD and these outcomes. First, the cycle of violence theory33, suggests that being a victim of childhood abuse and neglect increases risk of also engaging in delinquent behaviors and perpetrating violence. It is postulated that this is in part due to deficits in emotion regulation and impulse control, which often occurs as a consequence of experiencing trauma34. Additionally, the general strain theory35 suggests that the experience of adverse life events, such as trauma, can result in elevations in negative affect, which in turn increases risk for engagement in crime and delinquency as a maladaptive coping strategy. Thus the events associated with PTSD symptoms or diagnosis may lead to negative behavioral outcomes, including violent offending, as a maladaptive means to manage distress36.
Given the link between PTSD and SUD, it is plausible that among justice-involved youth those with comorbid symptoms of both disorders may be a subgroup of justice-involved youth who are at heightened risk for negative behavioral outcomes and recidivism. However, to date, the majority of studies examining PTSD and SUD among justice-involved youth have examined each in isolation37. Moreover, literature examining the co-occurrence of PTSD and SUD among justice-involved youth have only examined prevalence rates,3,38 with none to our knowledge examining the interactive effect between the disorders or symptom levels of the disorders. The current study aims to fill this gap in the literature by examining the effect of PTSD and SUD symptomology on behavioral and criminal outcomes among justice-involved youth. It is hypothesized that PTSD symptoms will moderate the relationship between SUD symptoms and the outcome variables, such that risk would be heightened among youth with elevated SUD and PTSD symptoms compared to those with elevated SUD symptoms but lower PTSD symptoms. Establishing findings on the co-occurrence of PTSD and SUD symptomology among justice-involved youth can help identify those youth who are at greatest risk for behavioral and criminal outcomes and can provide valuable information to help improve interventions for this population of at-risk youth.
Method
Procedure
Following initial involvement with the juvenile court (i.e., charged but not sentenced) in a large, Mid-western, U.S. city, youth in the present sample were referred to the university’s medical school to complete a court ordered psychological assessment. The referral for psychological testing typically conducted if the youth was being considered for residential or prison placement for their sentence. Additionally, probation officers would provide referrals if there were suspicions of mental health or substance-related problems that might impair the youth’s judgment. Following referral, a licensed clinical psychologist or supervised doctoral student reported to the Juvenile Detention Center or the youth’s current placement (residential facility or home) to complete a psychological assessment. After youth provided assent for the psychological assessment, clinicians conducted a structured clinical interview and administered an assessment battery. The current study is a secondary analysis of the collected data, as the primarily reason for data collection was for clinical evaluation for placement. All data analysis procedures were approved by the university IRB.
Participants
Participants in the present sample were drawn from 305 total justice-involved youth who completed psychological assessments. Of the 305-youth assessed, 287 were age 18 or under and had valid demographic data on file, comprising our final sample. Most participants included in these analyses were male (78.4%) and non-White (74.2%; 66.2% African American/Black, 3.8% Hispanic/Latino, and 4.2% Multiracial). The age of participants ranged from 9–18 (M =15.36).
Measures
Demographics and control variables.
Each youth self-reported their age, gender, and race/ethnicity.
Externalizing behaviors.
The Youth Self-Report (YSR)39 externalizing broad-band scale was used to assess externalizing problems. The 32-item subscale of the YSR asks youth to rate themselves on various behavioral and emotional problems and competencies related to rule-breaking behavior (e.g., stealing, truancy, swearing) and aggressive behavior (e.g., destruction of property, argumentative behavior, fighting). Response options for each item range from 0 (not true) to 2 (very often or often true), and a total scale score is computed. Scale scores were converted to t-scores with corresponding percentile rankings. T-scores < 65 on YSR scales were considered to fall in the “normal” range and increases in t-scores over 65 correspond with elevations in symptom severity. The YSR has been validated for use in samples of juvenile justice-involved youth40.
Substance use disorder (SUD) symptoms.
The symptoms (SYM) subscale from the Adolescent Substance Use Subtle Screening Inventory (SASSI-A2)41 was used to assess SUD symptoms. The SYM subscale includes 9-item that assesses problems related to substance use, including consequences and loss of control in usage to help determine if a youth is at risk for SUD 32. Response options for each item are “true” or “false”, with raw scores ranging from 0–9. Raw scores were converted to t-scores, with scores > 61 (males) and > 67 (females) indicative of a high probability of an SUD 42. The symptoms scale has shown high test-retest reliability (r = .87) and internal consistency (Cronbach’s alpha = .82), and demonstrated a 100% correct classification rate for DSM SUD diagnoses 41.
Posttraumatic stress disorder (PTSD) symptoms.
The post-traumatic stress problem scale (PTSP) 39 also from the YSR was used to examine symptoms of PTSD. This 14-item scale assesses symptoms typically associated with the experience of traumatic stress (e.g., problems concentrating, nightmares, paranoia, mood changes). Items are rated from 0 (not true) to 2 (very true or often true) and scale scores are converted into T-scores with scores of 65 or greater indicating elevations in symptoms severity. The scale has been shown to have high internal consistency among youth (α=.75–85)39,43.
Violent Crime.
Commission of a violent crime was derived from the preliminary report prepared by the youth’s probation officer. A violent crime was defined as at least one report of perpetrating physical harm towards another person (e.g., battery, assault, child molestation, etc.). This measured was dichotomized as the presence or absence of a violent crime.
Data Analysis
All analyses were performed in SPSS 24.0. Hierarchical multiple linear regression and logistic regression analyses were used to predict externalizing behaviors and violent crime, respectively, from symptoms of SUD and PTSD. In each regression analysis, demographic variables were entered into Step 1 (race was coded White or non-White with non-White as the reference group). SUD symptoms were entered in Step 2, followed by PTSD symptoms in Step 3. In Step 4, the interaction of SUD and PTSD symptoms was entered into the model. To probe the magnitude and direction of the interactions, we used the PROCESS macro44, which uses the Johnson-Neyman technique to estimate the conditional effect of the independent variable on the dependent variable at different values of the moderator.
Results
Among participants, 44.7% were currently detained for a violent crime and most (93.8%) had previous criminal referrals to the juvenile court system. In regards to substance use, most participants reported substance use in the past year (87.5%), with the most commonly used substance being cannabis (83.3%%) followed by alcohol (57.1%). See Table 1 for participant characteristics on the variables of interest.
Table 1.
Summary of Demographics and Descriptive data
| M(SD) or % |
1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1. Age | 15.36 (141) |
||||||
| 2. Gender (female) | 21.6% | −.14* | |||||
| 3. Race (non-white) | 74.2% | −.10 | −.20 | ||||
| 4. SUD | 50.09 (10.05) |
.11 | .06 | − 24*** | |||
| 5. PTSD | 60.49 (10.10) |
−.09 | .00 | −.05 | .53*** | ||
| 6. External | 61.93 (12.00) |
−.14* | .10 | .01 | 55*** | 63*** | |
| 7. Violent Crime | 44.7% | −.05 | −.04 | −.02 | −.05 | −.02 | −.04 |
Note:
p < .05.
p < .01.
p < .001.
In Step 1 of the linear regression predicting externalizing behavior, demographic factors were not statistically predictive of externalizing behaviors although they did collectively explain 3.1% of the variance in the model. In Step 2, SUD symptoms was a significant predictor of externalizing behaviors (ß = .18, p =.013), accounting for an additional 3.1% of variance in externalizing behaviors. In Step 3, PTSD symptoms was a significant predictor of externalizing behaviors (ß = .21, p = .012), explaining an additional 3.1% of the variance in externalizing behaviors. However, in this step SUD symptoms were no longer significant (ß = .066, p = .445). Finally, in Step 4, the interaction of SUD symptoms and PTSD symptoms was significant (ß = 2.53, p < .001), explaining an additional 7.8% of the variance in externalizing behaviors. Significant main effects for SUD and PTSD symptoms were also found at this step (Table 2).
Table 2.
Summary of Hierarchical Regression Analysis for Variables Predicting Externalizing Behavior (N = 194 )
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β |
| Age | 85.32 | 57.25 | .00 | −.31 | 3.49 | −.01 | .75 | 3.47 | .02 | .48 | 3.33 | .01 |
| Race | −25.94 | 10.72 | −.18 | −18.59 | 10.98 | −.13 | −21.05 | 10.87 | −.14 | −19.75 | 10.42 | −.13 |
| Gender | −3.81 | 11.37 | −.02 | −4.99 | 11.23 | −.03 | −4.07 | 11.07 | −.03 | −1.84 | 10.63 | −.01 |
| SUD SYMP | 1.21 | .48 | .18* | .43 | .57 | .07 | −9.48 | 2.43 | −1.44*** | |||
| PTSD SYMP | 1.32 | .52 | .21* | −7.21 | 2.10 | −1.15** | ||||||
| SUD x PTSD | .16 | .04 | 2.53*** | |||||||||
| R | .23 | .63 | .73 | .73 | ||||||||
| R2 | .03 | .06 | .09 | .17 | ||||||||
| F F Change |
3.63 3.63 |
30.44 104.89*** |
42.16 54.5*** |
35.98 2.91* |
||||||||
Note: SUD SYMP = Substance Use Disorder Symptoms. PTSD SYMP = Posttraumatic Stress Disorder Symptoms.
p < .05.
p < .01.
p < .001.
Further probing of the interaction revealed that SUD symptoms were associated with externalizing behaviors at high levels (i.e., one standard deviation above the mean) of PTSD symptoms (b = 1.67, SE = .62, p = .007), but not mean levels of PTSD symptoms (b = .07, SE = .55, p = .895). At low levels (i.e., one standard deviation below the mean) of PTSD symptoms, SUD symptoms were inversely associated with externalizing behaviors (b = −1.53, SE = .72, p = .034) (Figure 1).
Figure 1.
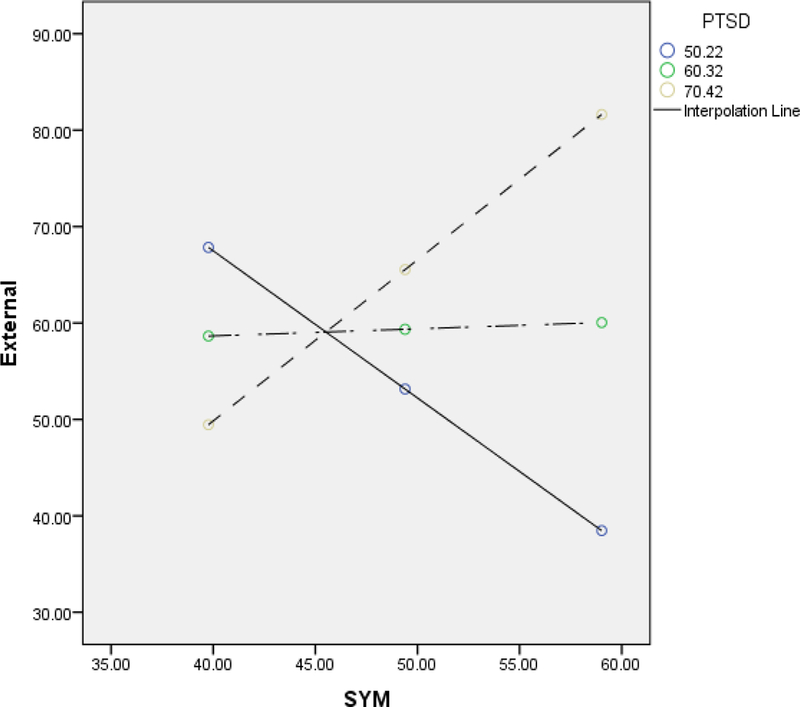
Interactive effect of PTSD and SUD symptoms on externalizing behavior.
Results of the logistic regression analysis predicting violent crime revealed that SUD symptoms was related to decreased likelihood of committing a violent crime (OR = .819, 95% CI: .68- .99, p = .035). However, no other predictors in this model were significant and no interaction effect was observed (OR = 1.00, 95% CI: 1.00 −1.01, p = .053).
Discussion
Given the limited number of studies that have examined both PTSD and SUD outcomes among juvenile justice youth37, and none to our knowledge examining their interactive effect, the purpose of this study was to examine the effect of PTSD and SUD symptomology on externalizing and criminal outcomes among a sample of justice-involved youth. Our finding that SUD symptoms was associated with greater externalizing behaviors at high levels of PTSD symptoms but was associated with decreased risk for externalizing problems among youth with lower PTSD symptoms, suggests that the relationship between SUD symptoms and externalizing behaviors may be more likely due to risk posed by PTSD symptoms. Although mediation was not assessed in the current study, PTSD and SUD symptoms may interact such that PTSD symptoms increases risk for substance use as a coping response, which in turn increases risk for SUD symptoms and externalizing behaviors 45,46. Whether the interaction between PTSD and SUD symptoms is explained by a moderating or mediation relationship, findings can inform intervention programming by highlighting the need to address PTSD symptoms among juvenile justice youth. Specifically, interventions such, as Trauma-Focused CBT47, may be effective at reducing externalizing behaviors among justice-involved youth as it specifically addresses PTSD symptoms. Additionally, based on the self-medication hypothesis16,17 and general strain theory35, the influence of PTSD symptoms on externalizing behaviors may be due to deficits in emotion-regulation. To directly address these deficits, interventions such as Trauma Affect Regulation: Guide for Education and Therapy (TARGET) 48, have been developed for incarcerated youth with PTSD symptomology, with findings providing support for its use in decreasing the number of disciplinary incidents, aggressive behaviors, and prolonged stays in detention centers among youth49,50.
Moreover, given the complexities associated with youth involved in the juvenile justice system, a comprehensive model that addresses PTSD symptoms and other mental health issues, may prove to be most efficacious for youth involved within the juvenile justice system. A suggested form of intervention planning is a collaboration between the juvenile justice and mental health systems51. These attempts to systematically strategize and identify mental health needs among juvenile justice-involved youth that would divert youth to opportunities of effective treatments within the community and report those needs to the juvenile justice system. This model51 considers dispositional alternatives (juvenile correctional placement or probation) and re-entry (returning home) as critical intervention points where examination of mental health issues and collaboration with the community can improve opportunity for treatment and use of the interventions mentioned above. The collective implementation of collaboration between the juvenile system and mental health services to provide treatment for PTSD and SUD symptoms and proper matching introduced by these comprehensive services may be the best approach to reduce the likelihood of negative behavioral outcomes among this population of youth52.
Two unexpected findings for the current study were in regard to SUD symptoms, such that youth high on SUD symptoms but low on PTSD symptoms were at lower risk for externalizing behaviors. Additionally, youth with greater SUD symptoms were also at lower risk for commission of a violent crime. These findings are counterintuitive given evidence that substance use and SUDs are risk factors for externalizing behaviors and offending among youth3,10,53. It is plausible that youth within our sample who reported higher SUD symptoms but few PTSD symptoms are qualitatively different in regards to behavioral and criminal outcomes from those youth with higher symptoms of both SUD and PTSD. The former group may be more likely to engage in impulsive behaviors and minor criminal behaviors, such as status offenses, whereas the latter may be more likely to engage in aggressive or more serious offenses, such as violent crimes. To investigate this hypothesis, we ran post-hoc analyses on percentage of status offenses based on levels of SUD and PTSD symptoms. Although our findings indicated similar levels of status offenses, which were 55% across groups, it is plausible that differences may be found based on specific types of offenses.
Thus, additional research is needed to better understand characteristics and circumstances that may differentiate risk for behavioral and criminal outcomes among justice-involved youth with high levels of only SUD symptoms compared to high levels of both SUD and PTSD symptoms. For example, it is plausible that youth with high SUD symptoms but few PTSD symptoms may exhibit characteristics that protect them from risk for externalizing behaviors, such as resilient personality, social support, or protective family factors 54–56. Conversely, it is plausible that when a direct effect is observed between substance use and externalizing and criminal outcomes, other co-occurring factors such as violent peers 57 and gang membership58 are driving the association. These variables were not included in our dataset and thus could not be analyzed, but should be explored in future research. Examining both the direct and interactive effect of SUD symptoms with other comorbid factors is significant, as it will help expand our understanding on what characteristics among justice-involved youth who exhibit SUD symptoms place them at lower versus higher risk for externalizing behaviors and or other criminal outcomes.
It is also plausible that our lack of an effect for PTSD symptoms on violent crime may be due to measurement, as there is literature to suggest that witnessing violence or trauma is also associated with increased risk for violent crimes among youth59. Thus, examining trauma exposure specifically rather than PTSD symptoms may provide different results. Another potential cause for the non-significant effect of PTSD symptoms on violent crime may be due to a reporter effect, as commission of a violent crime was based on the youth’s probation officer’s report. Given evidence of a positive association between PTSD symptoms and commission of a violent crime based on participant’s self-report60–62, future studies are needed to examine the interactive effect between PTSD and SUD symptoms on violent crime based on youth self-report.
Limitations and Future Research
Although these findings add to the current body of literature on interactive effect of SUD and PTSD symptoms on behavioral outcomes among justice-involved youth, there are some limitations that need to be addressed. First, the current study was a secondary analysis of data that was collected primarily for clinical purposes of psychological testing prior to sentencing, thus most measures were based on the youth’s self-report, with only criminal offense based on a different reporter. This might explain the relationships found among the self-report variables and the absence of relationships found with the crime variable, which was based on the probation officer’s report. Future studies should examine whether the relationship between PTSD, SUD, externalizing behaviors and commission of violent crime differs based on reporter (e.g., parent, teacher, parole officer, self-report, etc.). Second, regarding the predictor variables, only data on PTSD and SUD symptoms were available, which limited interpretation to severity of symptom levels of each disorder rather than the presence of the disorder or more nuanced assessments, such as exposure to trauma. Third, related to measurement, assessment of PTSD symptoms was based on the YSR/CBCL PTSD subscale, which has been shown to have poor predictive and discriminate validity among youth with and without PTSD 32,63–66. However, these studies included small sample sizes among primarily children and young adolescents, and the assessment of PTSD symptoms were based on parent rather than self-report. Moreover, participants were not justice-involved youth, limiting the generalizability of these findings. Thus, additional research is needed on the psychometric properties of the YSR/CBCL PTSD subscale among juvenile justice youth. Lastly, because this study was interested in examining the interactive effect of PTSD and SUD symptomology among justice-involved youth, the findings may not be generalizable to youth not involved with the justice system or individuals involved in the justice system who are over the age of 18.
Conclusion
Our findings provide support on the risk posed by greater PTSD and SUD symptomology on externalizing behaviors, which was not observed among youth with high SUD symptomology but low PTSD symptomology. This finding suggests that interventions should focus on treatments like CBT and emotion focused interventions, that can address PSTD symptoms and related emotion dysregulation which may in turn decrease risk for externalizing behaviors. Moreover, intervention approaches that include collaboration between the juvenile justice and mental health systems, as well as proper matching to community-based treatment center may not only alleviate presenting symptoms related to PTSD and SUD, but provide the best outcomes for long-term reduction in negative behavioral outcomes and recidivism among this population of youth 52. As for risk for violent crime, future studies are needed to examine risk based on self-report of violent crime by the youth, as well as examine factors outside of PTSD and SUD symptomatology that may pose risk for justice-involved youth.
Acknowledgements:
This project was supported in part by NIH award R25 DA035163, P30 DA027827, and K01 DA043654 to Dr. Tamika Zapolski (Indianapolis, IN).
Footnotes
Declaration of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Reference
- 1.Abram KM, Teplin LA, Charles DR, Longworth SL, McClelland GM, Dulcan MK. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry. 2004;61(4):403–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robertson AA, Dill PL, Husain J, Undesser C. Prevalence of mental illness and substance abuse disorders among incarcerated juvenile offenders in Mississippi. Child Psychiatry & Human Development. 2004;35(1):55–74. [DOI] [PubMed] [Google Scholar]
- 3.Cottle CC, Lee RJ, Heilbrun K. The Prediction of Criminal Recidivism in Juveniles. Criminal Justice and Behavior. 2001;28(3):367–394. [Google Scholar]
- 4.Keenan K, Shaw D, Delliquadri E. Evidence for the continuity of early problem behaviors: application of a development model. Journal of Abnormal Child Psychology. 1998;26(6):441–452. [DOI] [PubMed] [Google Scholar]
- 5.Ryan JP, Williams AB, Courtney ME. Adolescent Neglect, Juvenile Delinquency and the Risk of Recidivism. Journal of Youth and Adolescence. 2013;42(3):454–465. [DOI] [PubMed] [Google Scholar]
- 6.Sampson RJ, Laub JH. LIFE-COURSE DESISTERS? TRAJECTORIES OF CRIME AMONG DELINQUENT BOYS FOLLOWED TO AGE 70*. Criminology. 2003;41(3):555–592. [Google Scholar]
- 7.Marsiglia FF, Kulis S, Hecht ML, Sills S. Ethnicity and Ethnic Identity as Predictors of Drug Norms and Drug Use Among Preadolescents in the US Southwest. Substance use & misuse. 2004;39(7):1061–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shufelt JL, Cocozza JJ. Youth with mental health disorders in the juvenile justice system: Results from a multi-state prevalence study. National Center for Mental Health and Juvenile Justice; Delmar, NY; 2006. [Google Scholar]
- 9.Teplin LA, Abram KM, McClelland GM, Mericle AA, Dulcan MK, Washburn JJ. Pyschiatric disorders of youth in detention. In: Jusitce USDo, ed. Juvenille Justice Bulletin: Office of Juvenille Justice and Delinquency Prevention; 2006:1–15. [Google Scholar]
- 10.Belenko S, Sprott J. Comparative recidivism rates of drug and nondrug juvenile offenders: Results from three jurisdictions. Paper presented at: Academy of Criminal Justice Sciences annual conference, Anaheim, CA, March2002. [Google Scholar]
- 11.Chassin L Juvenile justice and substance use. The Future of Children. 2008;18(2):165–183. [DOI] [PubMed] [Google Scholar]
- 12.Lipsey M, Derzon J. Predictors of Violent or Serious Delinquency in Adolescence and Early Adulthood: A Synthesis of Longitudinal Research (From Serious and Violent Juvenile Offenders: Risk Factors and Successful Interventions, P 86–105, 1998, Loeber Rolf, Farrington David P., eds.-See NCJ-171234). In: Sage Publications, Inc; 1998. [Google Scholar]
- 13.Wierson M, Forehand R. Predicting recidivism in juvenile delinquents: the role of mental health diagnoses and the qualification of conclusions by race. Behaviour Research and Therapy. 1995;33(1):63–67. [DOI] [PubMed] [Google Scholar]
- 14.Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and individual differences. 2001;30(4):669–689. [Google Scholar]
- 15.Barnes GM, Welte JW, Hoffman JH, Dintcheff BA. Shared predictors of youthful gambling, substance use, and delinquency. Psychology of Addictive Behaviors. 2005;19(2):165. [DOI] [PubMed] [Google Scholar]
- 16.Capell H, Greeley J. Alcohol and tension reduction: An update on research and theory Psychological Theories of Drinking an Alcoholism New York: Guilford; 1987. [Google Scholar]
- 17.Khantzian EJ. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry. 2003;10(9):47–54. [Google Scholar]
- 18.Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. American Journal of Psychiatry. 2001;158(8):1184–1190. [DOI] [PubMed] [Google Scholar]
- 19.Acierno R, Kilpatrick DG, Resnick H, Saunders B, De Arellano M, Best C. Assault, PTSD, family substance use, and depression as risk factors for cigarette use in youth: findings from the National Survey of Adolescents. Journal of traumatic stress. 2000;13(3):381–396. [DOI] [PubMed] [Google Scholar]
- 20.Ford JD, Elhai JD, Connor DF, Frueh BC. Poly-Victimization and Risk of Posttraumatic, Depressive, and Substance Use Disorders and Involvement in Delinquency in a National Sample of Adolescents. Journal of Adolescent Health. 2010;46(6):545–552. [DOI] [PubMed] [Google Scholar]
- 21.Gilhooly T, Bergman AJ, Stieber J, Brown EJ. Posttraumatic Stress Disorder Symptoms, Family Environment, and Substance Abuse Symptoms in Emerging Adults. Journal of Child & Adolescent Substance Abuse. 2018;27(3):196–209. [Google Scholar]
- 22.Sanders J, Hershberger AR, Kolp HM, Um M, Aalsma M, Cyders MA. PTSD Symptoms Mediate the Relationship Between Sexual Abuse and Substance Use Risk in Juvenile Justice–Involved Youth. Child maltreatment. 2017:1077559517745154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68(1):19–30. [DOI] [PubMed] [Google Scholar]
- 24.Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology. 2002;70(6):1224–1239. [DOI] [PubMed] [Google Scholar]
- 25.Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry. 2002;59(12):1133–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.OJJPD. Statistical Briefing Book, Law Enforcement & Juvenile Crime, Juvenile Arrests. 2010; http://www.ojjdp.gov/ojstatbb/crime/qa05101.asp?qaDate=2010.
- 27.Dixon A, Howie P, Starling J. Trauma Exposure, Posttraumatic Stress, and Psychiatric Comorbidity in Female Juvenile Offenders. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(8):798–806. [DOI] [PubMed] [Google Scholar]
- 28.Ruchkin VV, Schwab-Stone M, Koposov R, Vermeiren R, Steiner H. Violence exposure, posttraumatic stress, and personality in juvenile delinquents. J Am Acad Child Adolesc Psychiatry. 2002;41(3):322–329. [DOI] [PubMed] [Google Scholar]
- 29.Wood S, Sage JR, Shuman T, Anagnostaras SG. Psychostimulants and Cognition: A Continuum of Behavioral and Cognitive Activation. Pharmacological Reviews. 2014;66(1):193–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosenberg HJ, Vance JE, Rosenberg SD, Wolford GL, Ashley SW, Howard ML. Trauma exposure, psychiatric disorders, and resiliency in juvenile-justice-involved youth. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(4):430–437. [Google Scholar]
- 31.Stimmel MA, Cruise KR, Ford JD, Weiss RA. Trauma exposure, posttraumatic stress disorder symptomatology, and aggression in male juvenile offenders. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(2):184–191. [Google Scholar]
- 32.Rosner R, Arnold J, Groh E-M, Hagl M. Predicting PTSD from the Child Behavior Checklist: Data from a field study with children and adolescents in foster care. Children and Youth Services Review. 2012;34(9):1689–1694. [Google Scholar]
- 33.Widom CS, Maxfield MG. A prospective examination of risk for violence among abused and neglected children. Annals of the New York Academy of Sciences. 1996;794(1):224–237. [DOI] [PubMed] [Google Scholar]
- 34.Van der Kolk BA. The complexity of adaptation to trauma: Self-regulation, stimulus discrimination, and characterological development. 1996. [Google Scholar]
- 35.Agnew R Building on the foundation of general strain theory: Specifying the types of strain most likely to lead to crime and delinquency. Journal of research in crime and delinquency. 2001;38(4):319–361. [Google Scholar]
- 36.Maschi T, Bradley CA, Morgen K . Unraveling the Link Between Trauma and Delinquency: The Mediating Role of Negative Affect and Delinquent Peer Exposure. Youth Violence and Juvenile Justice. 2008;6(2):136–157. [Google Scholar]
- 37.Wasserman GA, McReynolds LS, Ko SJ, Katz LM, Carpenter JR. Gender Differences in Psychiatric Disorders at Juvenile Probation Intake. American Journal of Public Health. 2005;95(1):131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abrantes AM, Hoffmann NG, Anton R. Prevalence of Co-Occurring Disorders Among Juveniles Committed to Detention Centers. International Journal of Offender Therapy and Comparative Criminology. 2005;49(2):179–193. [DOI] [PubMed] [Google Scholar]
- 39.Achenbach TM, & Rescorla LA Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2007. [Google Scholar]
- 40.Vreugdenhil C, van den Brink W, Ferdinand R, Wouters L, Doreleijers T. The ability of YSR scales to predict DSM/DISC-C psychiatric disorders among incarcerated male adolescents. European Child & Adolescent Psychiatry. 2006;15(2):88–96. [DOI] [PubMed] [Google Scholar]
- 41.Miller GA, Renn WR, & Lazowski LE The adolescent SASSI-A-2: A quick reference for administration and scoring. Springville, IN: SASSI Institute; 2001. [Google Scholar]
- 42.Miller GA, & Lazowski LE SASSI-A-2 manual. Springville, IN: SASSI Institute; 2001. [Google Scholar]
- 43.You DS, Youngstrom EA, Feeny NC, Youngstrom JK, Findling RL. Comparing the Diagnostic Accuracy of Five Instruments for Detecting Posttraumatic Stress Disorder in Youth. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53 . 2017;46(4):511–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 45.Bonn‐Miller MO, Vujanovic AA, Feldner MT, Bernstein A, Zvolensky MJ. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event‐exposed marijuana users. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2007;20(4):577–586. [DOI] [PubMed] [Google Scholar]
- 46.Colins O, Vermeiren R, Vreugdenhil C, Schuyten G, Broekaert E, Krabbendam A. Are psychotic experiences among detained juvenile offenders explained by trauma and substance use? Drug and Alcohol Dependence. 2009;100(1–2):39–46. [DOI] [PubMed] [Google Scholar]
- 47.Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. Guilford Publications; 2016. [Google Scholar]
- 48.Ford JD, Chapman JF, Hawke J, Albert D. Trauma among youth in the juvenile justice system: Critical issues and new directions. National Center for Mental Health and Juvenile Justice. 2007:1–8. [Google Scholar]
- 49.Ford JD, Hawke J. Trauma affect regulation psychoeducation group and milieu intervention outcomes in juvenile detention facilities. Journal of Aggression, Maltreatment & Trauma. 2012;21(4):365–384. [Google Scholar]
- 50.Marrow MT, Knudsen KJ, Olafson E, Bucher SE. The value of implementing TARGET within a trauma-informed juvenile justice setting. Journal of Child & Adolescent Trauma. 2012;5(3):257–270. [Google Scholar]
- 51.Skowyra KR, Cocozza JJ. Blueprint for change: A comprehensive model for the identification and treatment of youth with mental health needs in contact with the juvenile justice system. Policy Research Associates, Inc. 2007. [Google Scholar]
- 52.Montgomery IM, Torbet P, Malloy D, Adamcik L, Toner M, Andrews J. What works: Promising interventions in juvenile justice: Program report. Pittsburgh: National Center for Juvenile Justice, Office of Juvenile Justice and Delinquency Prevention (OJJDP), US Department of Justice; 1994. [Google Scholar]
- 53.Chassin L, Mansion AD, Nichter B, Pandika D. Substance use and substance use disorders as risk factors for juvenile offending. 2016. [Google Scholar]
- 54.Hart JL, O’Toole SK, Price-Sharps JL, Shaffer TW. The risk and protective factors of violent juvenile offending: An examination of gender differences. Youth Violence and Juvenile Justice. 2007;5(4):367–384. [Google Scholar]
- 55.Lodewijks HP, de Ruiter C, Doreleijers TA. The impact of protective factors in desistance from violent reoffending: A study in three samples of adolescent offenders. Journal of interpersonal violence. 2010;25(3):568–587. [DOI] [PubMed] [Google Scholar]
- 56.Wasserman GA, Keenan K, Tremblay RE, et al. Risk and Protective Factors of Child Delinquency. OJJDP Child Delinquency Bulletin Series. 2003. [Google Scholar]
- 57.Zimmerman GM, Messner SF. Neighborhood context and the gender gap in adolescent violent crime. American Sociological Review. 2010;75(6):958–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baglivio MT, Jackowski K, Greenwald MA, Howell JC. Serious, violent, and chronic juvenile offenders: A statewide analysis of prevalence and prediction of subsequent recidivism using risk and protective factors. Criminology & Public Policy. 2014;13(1):83–116. [Google Scholar]
- 59.Shaffer JN, Ruback RB. Violent Victimization as a Risk Factor for Violent Offending among Juveniles. Juvenile Justice Bulletin. 2002. [Google Scholar]
- 60.Allwood MA, Bell DJ. A preliminary examination of emotional and cognitive mediators in the relations between violence exposure and violent behaviors in youth. Journal of Community Psychology. 2008;36(8):989–1007. [Google Scholar]
- 61.Howard R, Karatzias T, Power K, Mahoney A. Posttraumatic stress disorder (PTSD) symptoms mediate the relationship between substance misuse and violent offending among female prisoners. Social psychiatry and psychiatric epidemiology. 2017;52(1):21–25. [DOI] [PubMed] [Google Scholar]
- 62.Mueller-Bamouh V, Ruf-Leuschner M, Dohrmann K, Schauer M, Elbert T. Are experiences of family and of organized violence predictors of aggression and violent behavior? A study with unaccompanied refugee minors. European journal of psychotraumatology. 2016;7(1):27856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Denton R, Frogley C, Jackson S, John M, Querstret D. The assessment of developmental trauma in children and adolescents: A systematic review. Clinical child psychology and psychiatry. 2017;22(2):260–287. [DOI] [PubMed] [Google Scholar]
- 64.Loeb J, Stettler EM, Gavila T, Stein A, Chinitz S. The child behavior checklist PTSD scale: Screening for PTSD in young children with high exposure to trauma. Journal of Traumatic Stress. 2011;24(4):430–434. [DOI] [PubMed] [Google Scholar]
- 65.Saigh PA, Yasik AE, Oberfield RA, Halamandaris PV, McHugh M. An analysis of the internalizing and externalizing behaviors of traumatized urban youth with and without PTSD. Journal of Abnormal psychology. 2002;111(3):462. [DOI] [PubMed] [Google Scholar]
- 66.Ruggiero KJ, McLeer SV. PTSD scale of the child behavior checklist: Concurrent and discriminant validity with non‐clinic‐referred sexually abused children. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2000;13(2):287–299. [DOI] [PubMed] [Google Scholar]


