Abstract
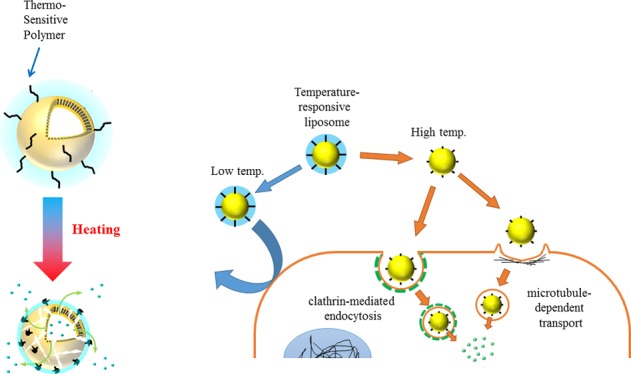
Drug delivery by nanoparticle carriers has been limited by inefficient intracellular drug delivery. Temperature-responsive poly(N-isopropylacrylamide) (PNIPAAm)-modified liposomes can release their content following heating. In this study, we synthesized the temperature-responsive polymer poly(N-isopropylacrylamide)-co-N,N′-dimethylaminopropylacrylamide (P(NIPAAm-co-DMAPAAm)) and investigated the properties of liposomes modified with P(NIPAAm-co-DMAPAAm) for intracellular drug carriers. The copolymer displayed a thermosensitive transition at a lower critical solution temperature (LCST) that is higher than body temperature. Above the LCST, the temperature-responsive liposomes started to aggregate and release. The liposomes showed a fixed aqueous layer thickness (FALT) at the surface below the LCST, and the FALT decreased with increasing temperature. Above 37 °C, cytosolic release from the temperature-responsive liposomes was higher than that from the PEGylated liposomes, indicating intracellular uptake. Here, we showed that the tunable surface properties of the temperature-responsive polymer-modified liposomes possibly enabled their dehydration by heating, which likely induced a faster cellular uptake and release. Therefore, the liposomes could be highly applicable for improving intracellular drug-delivery carriers.
1. Introduction
Drug delivery by nanoparticle carriers is an attractive strategy for cancer therapy to enhance therapeutic efficacy while reducing side effects.1 In particular, PEGylated liposomes prepared by the conjugation of poly(ethylene glycol) (PEG) to the liposome surface have been widely used to enhance the accumulation of liposomes in tumor tissues through enhanced permeability and retention effects mediated by their long circulation time.2−5 However, the hydration layer of the PEGylated liposomes creates a major drawback because of its limited cellular uptake of carriers and cellular release of drug content from liposomes.6,7 Strategies to overcome the drawback of limited drug release include stimuli-responsive liposomes that trigger drug release using external stimuli such as temperature and pH. In particular, temperature is mostly used to trigger the release of temperature-responsive liposomes.8,9
Temperature-responsive liposomes are classified into two types: traditional temperature-responsive liposomes composed of temperature-responsive lipids and liposomes modified with temperature-responsive polymers.10 The traditional temperature-responsive liposomes show the greatest permeation of the lipid membrane at its gel-to-liquid crystalline phase transition temperature. The temperature-responsive liposomes remain intact at 37 °C and exhibit a site-specific drug release from the liposomes following heating above 37 °C. An example of this type of temperature-responsive liposomes loaded with doxorubicin, ThermoDox, reached phase III trials in 2014.11 In addition, liposomes modified with temperature-responsive polymers exhibit a lower critical solution temperature (LCST) behavior. The polymers are soluble in an aqueous solution at a low temperature but are dehydrated and aggregated by heating above the LCST. Liposomes modified with temperature-responsive polymers show an enhanced release above the polymer LCST. Poly(N-isopropylacrylamide) (PNIPAAm) shows an LCST behavior at approximately 32 °C.12,13,14 The polymer LCST can be modulated by copolymerization with other monomers.15 PNIPAAm and its copolymers have been widely used for the modification of liposomes.16,17
In most cases, the temperature-responsive liposomes described so far rapidly release the entrapped drug before cellular uptake following heating, as intended. This results in drug penetration through the cell membrane by simple diffusion.10 Nanoparticles and liposomes are internalized into cells by endocytosis. PEGylated liposomes penetrate cells slowly and, therefore, exhibit a limited release of their content in the cells due to low affinity for the cell membrane because of the steric barrier of PEG.6,7 Temperature-responsive polymer-modified liposomes activated by heating are useful as intracellular carriers for hydrophilic, high-molecular-weight, and biodegradable drugs, such as peptide and gene products that cannot penetrate membranes and are expected to enhance the cellular drug uptake and subsequently release their content.
However, to the best of our knowledge, the surface properties of PNIPAAm-copolymer-modified liposomes for intracellular drug delivery have not been reported to date. To increase the intracellular uptake, PEGylated traditional temperature-responsive liposomes modified with ligands and antibodies18−20 as well as temperature-responsive polymer-modified liposomes conjugated with antibody and exposed to ultrasound have been reported.21−23 Moreover, interestingly, nanoparticles without liposomes, including our temperature-responsive poly(N-isopropylacrylamide)–poly(lactic acid) (PNIPAAm–PLA) nanoparticles,24 temperature-responsive poly(ε-caprolactone) micellar nanoparticles,25 poly(N-isopropylacrylamide)-co-N,N-dimethylaminoethyl methacrylate (PNIPAAm-co-DMAEMA) nanoparticles,26 PNIPAAm-chitosan-modified magnetite nanoparticles,27 and poly(N-isopropylacrylamide)-block-poly((3-acrylamidopropyl)trimethylammonium chloride) (PNIPAAm–PAMPTMA) polymer complex with siRNA,28 were reported to be internalized in cells following heating. In addition, recently, temperature-responsive biopolymer elastin-like polypeptide-modified liposomes have been reported to show an induced cellular uptake following dehydration of the molecules on the liposomal surface.29 As dehydration of the polymer increases its interaction with the cell membrane, PNIPAAm-copolymer-modified liposomes are expected to contribute to the enhancement of both the cellular uptake of the liposomes and the release of their content in the cells following heating.
In this study, we synthesized poly(N-isopropylacrylamide)-co-N,N′-dimethylaminopropylacrylamide (P(NIPAAm-co-DMAPAAm)) (molar ratio, 95/5; molecular weight, 5500)–1,2-dioleoyl-sn-glycero-3-phospho-ethanolamine (l-α-phosphatidylethanolamine dioleoyl; DOPE) and compared the physicochemical properties of the DOPE-conjugated, P(NIPAAm-co-DMAPAAm)-modified N-[1-(2,3-dioleoyloxy) propyl]-N,N,N-trimethyl-ammonium methylsulfate (DOTAP)/DOPE liposomes as temperature-responsive liposomes to those of hydrated PEGylated liposomes to develop intracellular drug carriers. Here, we showed that the tunable surface properties of the temperature-responsive polymer-modified liposomes enabled their heat-activated dehydration, which induced faster cellular uptake and release.
2. Results and Discussion
2.1. LCST of P(NIPAAm-co-DMAPAAm)
The NIPAAm and DMAPAAm in the P(NIPAAm-co-DMAPAAm) acted as the temperature-responsive and hydrophilic moieties, respectively. In aqueous solution, PNIPAAm exhibits an expanded coil conformation below the LCST because it is strongly hydrated; however, it changes to a globular form above the LCST because of its sudden dehydration.30 It was reported that the coil–globule transition of PNIPAAm could be detected using differential scanning calorimetry (DSC).
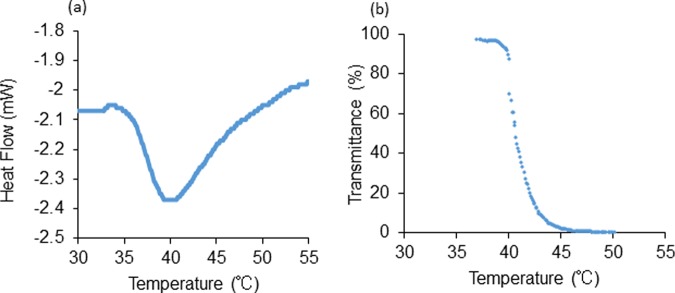
The temperature-responsive transition of the P(NIPAAm-co-DMAPAAm) suspension in water was examined using DSC and transmittance measurement. The DSC curve showed a large and sharp endotherm centered at 40.5 °C (Figure 1a), whereas the transmittance curve with 50% transmittance was observed at 40.2 °C (Figure 1b). These results indicate that the copolymer chains efficiently transitioned sharply from a hydrophilic to a hydrophobic state at approximately 40 °C. Therefore, the copolymer LCST was determined to be approximately 40 °C, which is above the normal body temperature.
Figure 1.
LCST of P(NIPAAm-co-DMAPAAm) in water determined using (a) DSC and (b) transmittance measurement.
2.2. Colloidal Stability and Carboxyfluorescein (CF) Release from Polymer-Modified Liposomes
We prepared temperature-responsive and PEGylated liposomes composed of DOTAP, DOPE, and P(NIPAAm-co-DMAPAAm) or PEG–distearoylphosphatidylethanolamine (DSPE) (molar ratio, 30/65/5) in phosphate-buffered saline (PBS). The DOTAP/DOPE (molar ratio, 3:7) liposomes prepared as the control were unstable because of the high DOPE content; thus, they could not be evaluated.31 Therefore, we prepared DOTAP/DOPE (molar ratio, 1:1) liposomes as a nonmodified liposome. It is noteworthy that the modification of the P(NIPAAm-co-DMAPAAm)–DOPE or PEG–DSPE with the unstable DOTAP/DOPE (3:7) liposomes successfully produced stable liposomes. The stability was achieved because the PEG–lipid in the liposomal membrane prevented DOPE–liposome aggregation and the subsequent phase transition.32,33 This finding suggests that the temperature-responsive liposomes had hydrophilic layers at their surface similar to those of the PEGylated liposomes. The physicochemical properties of the temperature-responsive liposomes, such as colloidal stability and release of content with increasing temperature, were examined.
The colloidal stability of the liposomes was evaluated by measuring the particle size of the suspensions (Figure 2). At room temperature, the particle sizes of the temperature-responsive, PEGylated, and nonmodified liposomes (25 °C) were 125 ± 0.3, 145 ± 0.7, and 118.2 ± 0.2 nm (mean ± standard deviation (SD)), respectively. When the temperature was increased, the particle size of the temperature-responsive liposomes did not increase until 39 °C, indicating that they were stable at physiological temperatures. However, above the LCST (40 °C), the particle size of the suspension increased markedly, indicating that the liposomes lost their colloidal stability and formed an aggregate. On the other hand, the PEGylated and nonmodified liposomes were stable throughout the tested temperature region.
Figure 2.
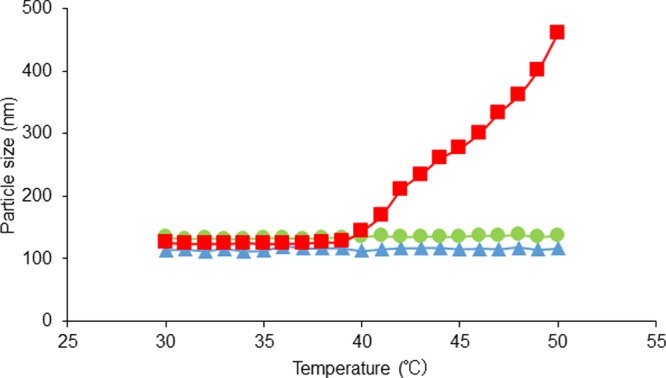
Change in the particle size of liposome suspension in PBS with increasing temperature: nonmodified (triangle), PEGylated (circle), and poly-N-Isopropylacryamide-co-N,N′-dimethylaminopropylacrylamide [P(NIPAAm-co-DMAPAAm)] modified (square) liposomes.
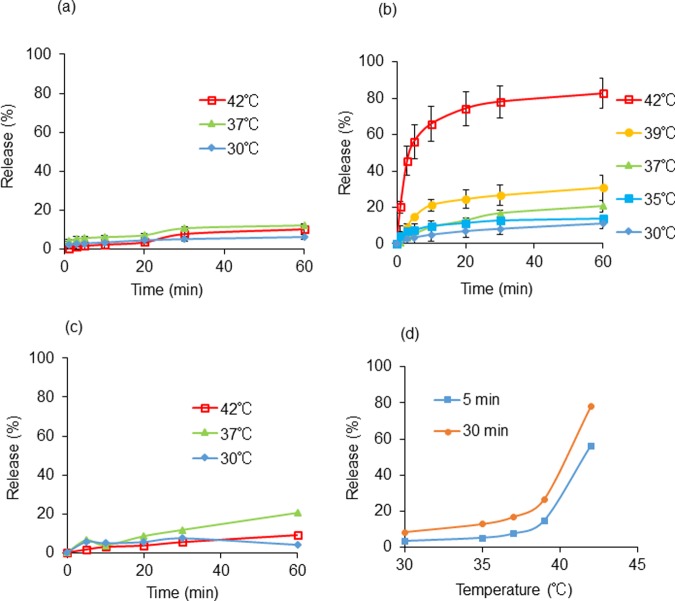
The CF released from CF-entrapped temperature-responsive liposomes was measured after incubation at different temperatures (Figure 3). The PEGylated (Figure 3a) and nonmodified (Figure 3c) liposomes retained their CF content tightly throughout their exposure to the tested temperature region. The temperature-responsive liposomes also retained the CF content tightly below 37 °C and released approximately 15% in 30 min at 37 °C (Figure 3b,d). Then, the CF release increased markedly at temperatures >39 °C, near the LCST, and at 42 °C, which was above the LCST, the liposomes released approximately 80% of the CF in 30 min (Figure 3d). The initiation temperatures of the aggregation and CF release of the temperature-responsive liposomes in PBS were slightly lower than those of the copolymer LCST measured in water.
Figure 3.
CF release (%) in suspension of (a) PEGylated liposomes, (b) P(NIPAAm-co-DMAPAAm)-modified liposomes, (c) nonmodified liposome in PBS from 0 to 60 min at each temperature, and (d) P(NIPAAm-co-DMAPAAm)-modified liposomes incubated at each temperature for 5 and 30 min (squares and circles, respectively) (mean ± SD (n = 3)).
The destabilization by aggregation and the content release of the temperature-responsive liposomes were induced by the temperature-dependent characteristic change of the copolymer. Below the LCST, similar to the PEGylate liposomes, the hydrated copolymer chains may sufficiently cover the liposome surface and, thereby, increase the stability of the unstable DOTAP/DOPE (3:7) liposomes.32 However, above the LCST, the dehydrated copolymer chains may be distributed partly at the liposomal surface and, therefore, may not cover the entire liposome, which would greatly decrease the stability of the liposomes. In this case, the copolymer LCST appeared to tune the temperature of the liposomes, causing them to aggregate and release their content.
2.3. Change in the Fixed Aqueous Layer Thickness (FALT) of Temperature-Responsive Polymer-Modified Liposomes
To investigate the surface properties of the liposomes, we measured the zeta potential of polymer-modified liposomes as the surface potential at different temperatures (Table 1). All of the liposomes exhibited a positive zeta potential, resulting from the DOTAP. However, the temperature-responsive liposomes showed a lower zeta potential than the nonmodified and PEGylated liposomes. With increasing temperature, the temperature-responsive liposomes showed a markedly increased zeta potential, whereas the nonmodified and PEGylated liposomes did not show a similar behavior over the tested temperature range (Table 1).
Table 1. Zeta (ζ) Potential of Polymer-Modified and Nonmodified Liposomes in Watera.
| ζ potential (mV) | 30 °C | 37 °C | 45 °C |
|---|---|---|---|
| nonmodified liposome | 61.7 ± 0.3 | 64.4 ± 0.4 | 62.4 ± 2.9 |
| PEGylated liposome | 53.5 ± 4.7 | 54.1 ± 4.3 | 61.0 ± 2.2 |
| P(NIPAAm-co-DMAPAAm)-modified liposome | 28.2 ± 0.4 | 38.7 ± 0.3 | 47.9 ± 1.3 |
Mean ± SD, n = 3.
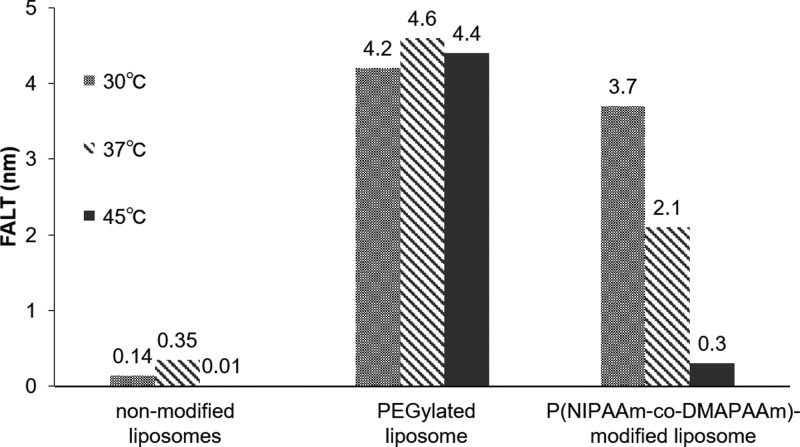
The zeta potential values decreased when the NaCl concentration was increased. The calculated FALT values are shown in Figure 4; it was low (0.17 nm) for the nonmodified liposomes, whereas it was high (approximately 4.4 nm) for the PEGylated liposomes and not temperature-dependent in this range. The FALT of the PEGylated liposomes was in agreement with the previously described value of 3.5 nm.34 The temperature-responsive liposomes showed a FALT of approximately 3.7 nm at 30 °C, which was also comparable to that of the PEGylated liposomes; however, at 45 °C, it decreased to 0.3 nm, indicating an increased dehydration of the liposomal surface. On the basis of the results indicating that the surface of the liposomes was dehydration above LCST, we propose that the temperature-responsive liposomes have the potential to enhance cellular uptake and drug release by temperature control.
Figure 4.
Changes in the FALT of PEGylated, P(NIPAAm-co-DMAPAAm)-modified, and nonmodified liposomes.
2.4. Enhanced Cellular Uptake of Temperature-Responsive Polymer-Modified Liposomes
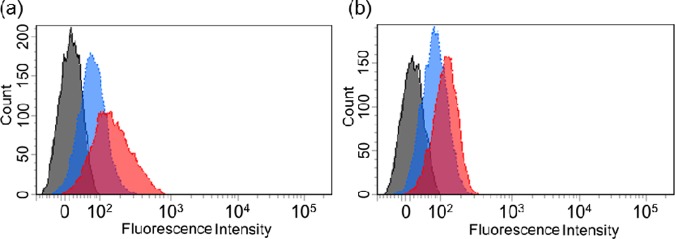
Here, we examined the cellular uptake of liposomes after incubation for 30 min using flow cytometry and fluorescence microscopy. The flow cytometry results revealed that an incubation of RAW264.7 cells with both the rhodamine-labeled liposomes increased the fluorescence intensity in a temperature-dependent manner, indicating an increased cellular association (Figure 5a,b). The cellular association of the rhodamine-labeled temperature-responsive liposomes was more highly increased in a temperature-dependent manner than that of the PEGylated liposomes. We calculated the ratio of the fluorescence intensity of rhodamine-labeled liposomes at 30 °C and compared it to that at 40 °C, which is above body temperature, for each liposome. The increased ratio of fluorescence intensity, that is, the association ratio of the temperature-responsive and PEGylated liposomes was 2.22 and 1.48, respectively (Figure 6). The temperature-responsive liposomes showed a significantly higher association ratio than the PEGylated liposomes (p < 0.02). This finding indicates that the temperature-responsive liposomes showed a faster cellular association at 40 °C than that at 30 °C compared to that of the PEGylated liposomes. It is suggested that the easy interaction of the temperature-independent hydrated PEGylated liposomes with the cell membrane was hindered even with the cationic surface charge. On the other hand, the partly dehydrated temperature-responsive liposomes may exhibit enhanced cellular uptake above the LCST.
Figure 5.
Cellular association of rhodamine-labeled (a) P(NIPAAm-co-DMAPAAm)-modified and (b) PEGylated liposomes incubated with RAW264.7 cells for 30 min at 30 °C (blue) and 40 °C (red), and the untreated cells (black).
Figure 6.

Effect of increasing the incubation temperature from 30 to 40 °C on the cellular association of rhodamine-labeled PEGylated and P(NIPAAm-co-DMAPAAm)-modified liposomes. Rhodamine fluorescence intensity ratio indicated following incubation of each liposome at 40/30 °C in Figure 5. Mean ± SD, n = 3; p < 0.02.
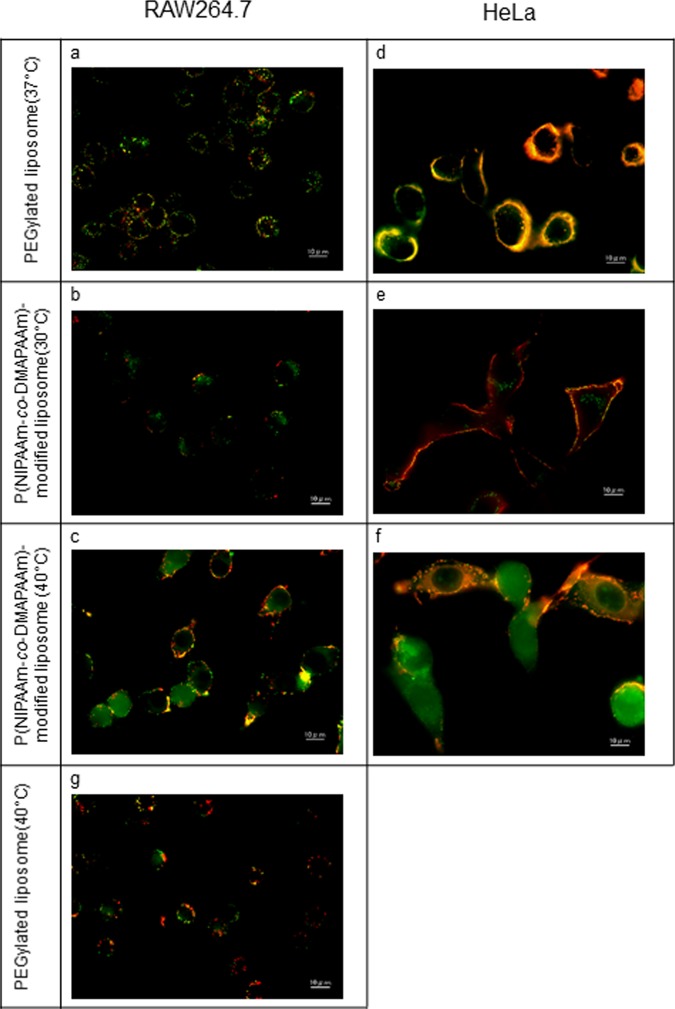
Using fluorescence microscopy, we further confirmed the cellular uptake of the CF-entrapped liposomes labeled with rhodamine in the RAW264.7 and HeLa cell lines incubated for 30 min. The initial incubation of free CF or the mixture of free CF and the control (empty temperature-responsive liposomes) with the RAW264.7 cells did not induce a green fluorescence by the CF in the cells. This indicates that the CF alone could not penetrate the cells at 30 and 40 °C following incubation for 30 min (data not shown).
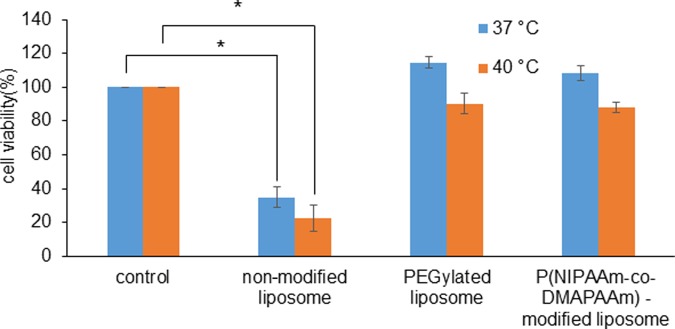
The PEGylated liposomes incubated with the RAW264.7 cells at 37 °C (Figure 7a) and 40 °C (Figure 7g) displayed a punctate fluorescence induced by the CF (green) and rhodamine (red) and their colocalization (yellow) on the cell surface, which was greater with the HeLa cells than that with the RAW264.7 cells (Figure 7d). This indicated an association of the liposomes with the cell surface. Interestingly, the temperature-responsive liposomes incubated with both the cells at 30 °C exhibited a low level of punctate fluorescence of CF in the cells and a strong localization of rhodamine on the cell surface (Figure 7b,e). This observation suggests that the liposomes were localized in the endosomes. At 40 °C, the CF fluorescence spread dramatically in the cytosol (Figure 7c,f), indicating that the CF was released from the internalized temperature-responsive liposomes following the increase in temperature. We attributed this increase in fluorescence to the leakage of CF from the liposomes and their dilution in the cell interior as described previously.20 In addition, it was surprising to note that the majority of the liposome-entrapped CF was associated with the cell surface, confirming that the elevated temperatures used for these experiments were not detrimental to the cells based on a cell viability assay (Figure 8). The nonmodified liposomes showed a significantly decreased cell viability, whereas the PEGylated and temperature-responsive liposomes did not show a similar behavior at 37 or 40 °C (Figure 8)
Figure 7.
Fluorescence micrographs of CF-entrapped liposomes labeled with rhodamine in (a–c, g) RAW264.7 cells and (d–f) HeLa cells. PEGylated liposomes incubated at (a, d) 37 °C and (g) 40 °C and P(NIPAAm-co-DMAPAAm)-modified liposomes incubated at (b, e) 30 °C and (c, f) 40 °C for 30 min. CF is shown in green, and rhodamine is shown in red. The scale bar is 10 μm.
Figure 8.
Comparison of viabilities of cells incubated with nonmodified, PEGylated, and P(NIPAAm-co-DMAPAAm) liposomes at 37 and 40 °C. Mean ± SD, n = 3; p < 0.01 vs control.
Microscopy findings of the RAW264.7 cells corresponded well with flow cytometry findings, as mentioned above. The observation of CF release from the temperature-responsive liposomes in the cells indicates that the cellular uptake rate was enhanced by the dehydration of the liposomal surface induced by the transition of P(NIPAAm-co-DMAPAAm) with increasing temperature. It is noteworthy that even the PEGylated liposomes taken up into the cells did not release CF following heating. Furthermore, the higher association of both the liposomes with the HeLa cells than with the RAW264.7 cells may be due to the strong interaction between the cationic liposomes and the negatively charged cell membrane.
The cellular uptake of the PNIPAAm-copolymer- and PNIPAAm-chitosan-modified magnetite nanoparticles27 as well as the PNIPAAm–PAMPTMA polymer complex with siRNA28 was reported following heating. However, the dehydration-induced cellular uptake of the PNIPAAm-copolymer-modified liposomes has not been clearly reported. The difference between the cellular uptakes of nanoparticles and liposomes may be attributed to the temperature-induced change in particle size. The self-assembled PNIPAAm-copolymer micellar and solid nanoparticles covered with the copolymer are hardly or slowly aggregated by the heat-induced dehydration of copolymer and, therefore, retain their small particle size, resulting in cellular uptake.24 Moreover, PNIPAAm-copolymer-modified liposomes exhibited a relatively fast heat-induced aggregation to induce a rapid drug release and a large particle size, resulting in a lower cellular uptake than that of the nanoparticles. In this study, our temperature-responsive liposomes started to aggregate and release CF at the copolymer LCST and exhibited a low rate of heat-induced aggregation. Furthermore, this effect maintained their small particle size and reduced the CF release before their penetration into the cells, contributing to the higher cellular uptake and release. The hydrated layer of the PNIPAAm copolymer on the unstable DOPE-rich cationic liposomes conferred a colloidal stability and a low cytotoxicity on the liposomes, which were comparable to those of PEG. The heat-induced dehydration of the liposomes increased their aggregation, destabilization, and release of content. In the intracellular delivery mediated by dehydration of the temperature-responsive liposomes, a delicate balance between the aggregation of liposomes and the release of content might be achieved. Therefore, considering these factors in designing PNIPAAm copolymers could increase the intracellular delivery of the modified liposomes.
2.5. Cellular Uptake Mechanism
Next, we investigated the cellular uptake mechanism of the temperature-responsive liposomes. The cellular uptake study was performed at 4 °C or in the presence of various endocytic inhibitors. The HeLa cells were incubated for 1 h at 37 °C with or without the inhibitors and then treated with the temperature-responsive liposomes at 4 or 40 °C, above body temperature, for 30 min. We used cells that were incubated with the liposomes in the absence of inhibitors as the control. The endocytic inhibitors and concentrations were determined on the basis of previous studies.35 The inhibitor concentrations that showed a cell viability ≥80% was selected for this study. Cytochalasin D, nocodazole, sucrose, and filipin III are the inhibitors of actin-based transport, microtubular transport, clathrin-mediated endocytosis, and caveolin-mediated endocytosis pathways, respectively. The cell internalization of the liposomes was mainly an energy-dependent process because approximately 65% of the cellular uptake was significantly blocked at 4 °C (Figure 9). The decrease in the measured liposome rhodamine fluorescence compared to that of the control indicated the involvement of specific endocytotic mechanism mediated by the inhibitors (Figure 9). A statistically significant inhibition of the uptake of the liposomes was observed for sucrose (28.5%), which is a clathrin-mediated endocytosis pathway inhibitor (p < 0.05), and nocodazole (35.6%), which causes microtubule disruption (p < 0.01). The inhibition of cellular uptake by nocodazole suggests that the microtubules participate in the uptake of liposomes that are known to participate in microtubule-dependent transport.36
Figure 9.
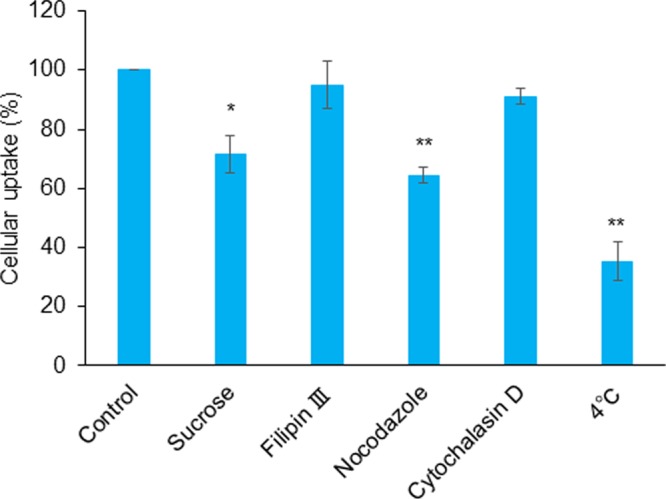
HeLa cells were pretreated with sucrose, filipin III, nocodazole, and cytochalasin D at 37 °C for 1 h or incubated at 4 °C for 1 h. Control was not pretreated. Then, the cellular association of rhodamine-labeled liposomes and P(NIPAAm-co-DMAPAAm) liposomes was examined in the pretreated HeLa cells following incubation at 40 or 4 °C for 30 min. Mean ± SD (n = 3); *p < 0.05 vs control and **p < 0.01 vs control.
Together, these data show that the uptake of the temperature-responsive liposomes into the HeLa cells was mediated by microtubule-dependent transport and clathrin-mediated endocytosis rather than caveolin-mediated endocytosis. Particle size has been reported to determine the route of cellular entry. However, the size dependence for uptake by caveola- or clathrin-coated vesicles was found to vary with the nature of the particles, the cell types studied, or both.37 In this study, temperature-responsive liposomes were enlarged by aggregation, and their surfaces were dehydrated by heating. Microtubules may mostly be involved in the uptake of larger particles. Therefore, these surface-tunable polymer-modified liposomes could have a great potential as intracellular drug-delivery carriers for products such as genes. We previously examined temperature-responsive liposomes as carriers of siRNA and plasmid DNA and observed their effective intracellular delivery, which will soon be reported in a separate article. However, further studies are needed to elucidate the cellular uptake and intracellular trafficking mechanisms involved in these processes and the contributions of the polymer characteristics of the liposomes.
3. Conclusions
To improve the cellular uptake and release of the liposome content, we synthesized P(NIPAAm-co-DMAPAAm)–DOPE and investigated its physicochemical properties by using it to modify DOTAP/DOPE liposomes as temperature-responsive liposomes. Below the LCST of the copolymer, the temperature-responsive liposomes had similar hydrated layer thickness to that of the PEGylated liposomes. Furthermore, the temperature-responsive liposomes were stable and did not release their liposomal content under the aforementioned condition. Above the LCST of the copolymer, the temperature-responsive liposomes showed an increased cellular uptake and released the liposomal content into the cytosol more than the PEGylated liposomes did, although they exhibited aggregation and release of liposomal content in response to heating. To the best of our knowledge, this is the first study to report that the dehydration of temperature-responsive polymer-modified liposomes induced faster cellular uptake and release than the nonmodified liposomes. The temperature-triggered tunable surface properties of the temperature-responsive P(NIPAAm-co-DMAPAAm)-modified liposomes could be highly applicable to intracellular drug-delivery carriers.
4. Materials and Methods
4.1. Chemicals
The NIPAAm provided by KJ Chemicals Co. (Tokyo, Japan) was purified by recrystallization from n-hexane and dried at room 25 °C in vacuo. The N,N′-dimethylaminopropylacrylamide (DMAPAAm) was purchased from KJ Chemicals Co. (Tokyo, Japan), and 2,2′-azobisisobutyronitrile (AIBN), 3-mercaptopropionic acid (MPA), sucrose, cytochalasin D, nocodazole, and DOPE were purchased from Wako Pure Chemical Industries, Ltd. (Osaka, Japan). N-Hydroxysuccinimide (NHS) and N,N′-dicyclohexylcarbodiimide (DCC) were purchased from Kanto Chemical Co. (Tokyo, Japan). 5(6)-CF and chlorpromazine were purchased from Sigma-Aldrich Corp. (St. Louis, MO). Filipin III was purchased from Cayman Chemical (Ann Arbor, MI). Dulbecco’s modified Eagle’s medium was purchased from Thermo Fisher Scientific (Waltham, CA), and the fetal bovine serum (FBS) was purchased from Biosera (Sussex, U.K.). The rhodamine B 1,2-dihexadecanoyl-sn-glycero-3-phosphoethanolamine triethylammonium salt (rhodamine–DHPE) was purchased from Life Technologies Co. (Carlsbad, CA), and DOTAP and N-[methoxy (PEG) 2000]–distearoylphosphatidylethanolamine (PEG–DSPE) were purchased from Avanti Polar Lipids Inc. (Alabaster, AL). All other reagents and solvents were of analytical grade.
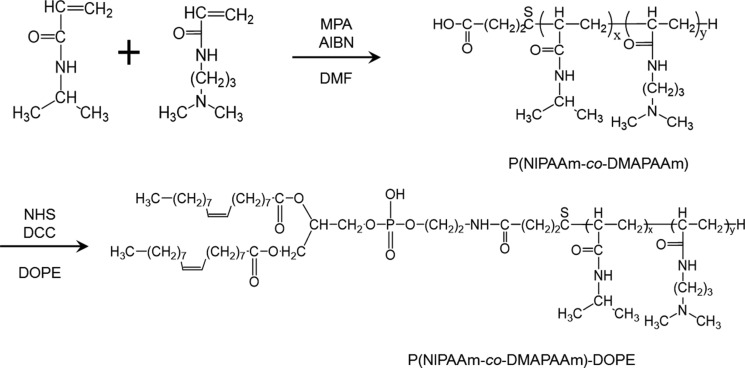
4.2. Synthesis of P(NIPAAm-co-DMAPAAm) Copolymer Conjugate with DOPE
The synthesis of the semitelechelic NIPAAm copolymer (molecular weight 5500) was carried out by radical polymerization, as previously reported.14,15,38 The synthesis route of P(NIPAAm-co-DMAPAAm) and the P(NIPAAm-co-DMAPAAm) conjugate with DOPE, [P(NIPAAm-co-DMAPAAm)–DOPE], is shown in Figure 10. NIPAAm and DMAPAAm at a fixed molar ratio of 95/5 (total 88 mmol), MPA (2.4 mmol), and AIBN (0.35 mmol) were dissolved in freshly distilled dimethylformamide (20 mL). Then, the solution was heated at 70 °C for 5 h in an atmosphere of nitrogen gas (N2). The copolymer was recovered by precipitation with diethyl ether, dissolved in acetone, precipitated again with diethyl ether, and then vacuum-dried. The copolymer, NHS, and DCC (0.2, 0.5, and 0.5 mmol, respectively) were dissolved in freshly distilled dichloromethane (10 mL). Then, the solution was reacted at 25 °C for 24 h; the obtained polymer was recovered by suction filtration and then precipitated with diethyl ether. The polymer and DOPE (0.2 mmol each) were dissolved in dioxane, the solution was reacted at 25 °C for 24 h, and then the polymer was vacuum-dried (Figure S1).
Figure 10.
Synthesis of P(NIPAAm-co-DMAPAAm) copolymer and its conjugation to 1,2-dioleoyl-sn-glycero-3-phospho-ethanolamine (DOPE).
4.3. Determination of LCST of P(NIPAAm-co-DMAPAAm) Copolymer
The copolymer LCST in water was evaluated using DSC and transmittance measurement. The transmittance of the copolymer aqueous solution (5 mg/mL) at 500 nm was monitored using a spectrophotometer (V-630; JASCO Corp., Tokyo, Japan) with a water-jacketed cell holder coupled with a circulating bath. The temperature was increased at a rate of 0.1 °C/min. The LCST was considered as the temperature at the peak of the DSC curve and the 50% point in the resulting transmittance versus temperature curve. The transition of the copolymer aqueous solution (100 mg/mL) was monitored using the DSC-60Plus (Shimadzu Corp., Kyoto, Japan). The aluminum pan was sealed using a tablet press machine, and the heating scan was carried out from 20 to 60 °C at a scanning rate of 1 °C/min under dry N2.
4.4. Preparation of Polymer-Modified Liposomes
The liposomes were prepared with DOTAP, DOPE, and P(NIPAAm-co-DMAPAAm)–DOPE or PEG–DSPE (Figure S2), each combined at a fixed molar ratio of 30/65/5, when necessary, mixed with rhodamine–DHPE (0.01 mol %) in chloroform solution, and the solution in the flask was subsequently evaporated. The nonmodified liposomes were prepared with DOTAP and DOPE (molar ratio, 1:1). The thin lipid and the polymer membrane were dispersed in 1 mL of 2 mM CF in PBS (pH 7.4) or PBS alone to prepare the CF-entrapped or empty liposomes, respectively, and sonicated in a bath sonicator. The liposomes were extruded through a polycarbonate membrane with a pore diameter of 100 nm. The free lipid, polymer, and CF were removed using gel permeation chromatography on a SephadexG-25M column using PBS. The liposomes were kept at 4 °C until analysis.
4.5. Measurements of Particle Size, Zeta Potential, and FALT of Polymer-Modified Liposomes
The particle size and zeta potentials of the liposomes were measured using dynamic light scattering with a Zetasizer Nano-ZS (Malvern Instruments Ltd., Worcestershire, U.K.) and the electrophoretic light scattering ELSZK-2 KOP apparatus (Otsuka Electronics Co., Ltd., Osaka, Japan), respectively. The liposome suspension was dispersed in PBS, and the particle size was measured as the colloidal stability at 25 °C. The temperature-induced changes in particle size and zeta potential were measured from 30 to 50 °C.
To calculate the FALT of each polymer-modified liposome, the liposome suspension was dispersed in 9% sucrose solution. We calculated the FALT using Gouy–Chapman theory.39,40 According to this theory, the zeta potential, ψ (L), calculated as the electrostatic potential at the position of the slipping plane, L (nm), was expressed as
| 1 |
where A is a constant; κ is the Debye–Hückel parameter, which is equal to √C/0.3 for univalent salts; and C is the molality of electrolytes. When zeta potentials are measured from the changing concentration of sodium chloride (NaCl) and plotted against κ, the slope, L, gives the position of the slipping plane or FALT in nanometers. On the basis of this theory, the FALT of each liposome was estimated from 30 to 45 °C.
4.6. Determination of CF Release from Polymer-Modified Liposomes
The CF-entrapped liposome suspension was added to PBS in a quartz cell (final CF concentration was 1 μM) at a given temperature, and the fluorescence intensity of the solution was monitored using a spectrometer. The excitation and emission wavelengths were 492 and 518 nm, respectively. As the liposomes released the CF rapidly at temperatures >40 °C, it was difficult to estimate the initial intensity of the CF-entrapped liposome suspension. We considered the fluorescence intensity at 20 °C as the standard release for the CF release measurement, as previously described.9 Furthermore, the percentage release of CF was defined as
| 2 |
where F, F′0, and F″0 are the intermediary, initial, and final fluorescence intensities, respectively, and F″ is the final fluorescence intensity at each temperature. F″ and F″0 were obtained as the fluorescence intensities of the liposome suspension after the rupturing of liposomes was induced by the addition of Triton X-100. The change in CF release from the liposomes was measured from 30 to 45 °C.
4.7. Cell Culture
RAW264.7 macrophage and human epithelioid cervix carcinoma HeLa cells (RIKEN BRC Cell Bank, Ibaraki, Japan) were cultured as subconfluent monolayers in a 75 cm2 culture flask with a vent cap using minimum essential medium supplemented with 10% FBS, 50 units/mL penicillin, and 50 μg/mL streptomycin at 37 °C in a humidified incubator exposed to 5% CO2. Subconfluent RAW264.7 cells were dissociated using a cell scraper (30 cm, TPP, Switzerland) and cultured in a flask for 2–3 days. The subconfluent HeLa cells were dissociated using 0.05% w/v trypsin, 0.53 mmol/L ethylenediaminetetraacetic acid (EDTA)·4Na solution (Wako Pure Chemical Industries, Ltd., Osaka, Japan) and cultured in a flask for 3–4 days.
4.8. Determination of Cellular Uptake of Polymer-Modified Liposomes Using Flow Cytometry
To detect the cellular association of the liposomes, the RAW264.7 cells were seeded in a 60 mm dish at a density of 5.0 × 105 cells per dish in 5 mL of the medium. After an overnight incubation, the cells were further incubated for 30 min with rhodamine-labeled PEGylated liposomes and rhodamine-labeled temperature-responsive liposomes at 30 or 40 °C in a humidified atmosphere of 5% CO2. Then, the RAW264.7 cells were washed twice with PBS, harvested with trypsin/EDTA, resuspended in PBS, and the cell-associated fluorescence was subsequently detected using a flow cytometer (BD LSRII, BD Biosciences, San Jose, CA).
4.9. Evaluation of Cellular Uptake of Polymer-Modified Liposomes Using Fluorescence Microscopy
HeLa and RAW264.7 cells (1 × 105 and 2 × 105 cells/dish, respectively) were grown in 2 mL of medium with 10% FBS. After an overnight incubation, 50 μL of rhodamine-labeled liposomes entrapped with CF was added and incubated at 30, 37, or 40 °C for 30 min. Then, the cells were rinsed thrice with PBS, fixed with 4% paraformaldehyde at 4 °C for 20 min, rinsed thrice with PBS, and observed using a fluorescence microscope (BZ-9000; Keyence Corp., Osaka, Japan).
4.10. Cellular Uptake after Treatment with Inhibitors of Endocytosis
HeLa cells (5.0 × 104 cells/well) were prepared by plating them on a six-well culture plate 24 h before each experiment. For the pretreatment, we incubated the cells at 4 °C or with medium containing dissolved cytochalasin D (5 μg/mL), nocodazole (3 μg/mL), sucrose (69 mg/mL), and filipin III (2 μg/mL) at 37 °C for 1 h. Subsequently, 30 μL of rhodamine-labeled liposomes was added to the above medium and further incubated at 40 °C for 30 min with 10% FBS. After incubation, the cells were washed twice with PBS, harvested with trypsin/EDTA, resuspended in PBS, and the cell-associated fluorescence of rhodamine was subsequently detected using a flow cytometer equipped with a PE filter argon-ion laser.
4.11. Cell Viability Assay
HeLa cells (5.0 × 103 cells/well) were prepared by plating on a 96-well culture plate. Each liposome was diluted in 100 μL of medium supplemented with 10% FBS, and the mixture was applied to the cells. After 24 h incubation at 37 or 40 °C, 10 μL of water-soluble tetrazolium-8 (Dojindo, Kumamoto, Japan) was applied to each well and incubated at 37 °C for 1 h. The absorbance at 450 nm was measured using a microplate reader (TECAN infinite M-1000; Tecan Japan Co., Kanagawa, Japan).
4.12. Statistical Analysis
Student’s nonpaired t-test was used to compare the normally distributed values between the groups. Statistical significance was set at p < 0.02.
Acknowledgments
This study was supported by a Grant-in-Aid for Exploratory Research (grant no. 25670081) from the Japan Society for the Promotion of Science (JSPS), Japan.
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acsomega.6b00342.
P(NIPAAm-co-DMAPAAm)–DOPE characterization by 1H NMR, gel permeation chromatography analysis method, and chemical structures of DOTAP, DOPE, and PEG–DSPE (PDF)
The authors declare no competing financial interest.
Supplementary Material
References
- Wicki A.; Witzigmann D.; Balasubramanian V.; Huwyler J. Nanomedicine in cancer therapy: challenges, opportunities, and clinical applications. J. Controlled Release 2015, 200, 138–157. 10.1016/j.jconrel.2014.12.030. [DOI] [PubMed] [Google Scholar]
- Vllasaliu D.; Fowler R.; Stolnik S. PEGylated nanomedicines: recent progress and remaining concerns. Expert Opin. Drug Delivery 2014, 11, 139–154. 10.1517/17425247.2014.866651. [DOI] [PubMed] [Google Scholar]
- Matsumura Y.; Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986, 46, 6387–6392. [PubMed] [Google Scholar]
- Klibanov A. L.; Maruyama K.; Torchilin V. P.; Huang L. Amphipathic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Lett. 1990, 268, 235–237. 10.1016/0014-5793(90)81016-H. [DOI] [PubMed] [Google Scholar]
- Blume G.; Cevc G. Liposomes for the sustained drug release in vivo. Biochim. Biophys. Acta 1990, 1029, 91–97. 10.1016/0005-2736(90)90440-Y. [DOI] [PubMed] [Google Scholar]
- Leus N. G.; Talman E. G.; Ramana P.; Kowalski P. S.; Woudenberg-Vrenken T. E.; Ruiters M. H.; Molema G.; Kamps J. A. Effective siRNA delivery to inflamed primary vascular endothelial cells by anti-E-selectin and anti-VCAM-1 PEGylated SAINT-based lipoplexes. Int. J. Pharm. 2014, 459, 40–50. 10.1016/j.ijpharm.2013.11.008. [DOI] [PubMed] [Google Scholar]
- Remaut K.; Lucas B.; Braeckmans K.; Demeester J.; De Smedt S. C. Pegylation of liposomes favours the endosomal degradation of the delivered phosphodiester oligonucleotides. J. Controlled Release 2007, 117, 256–266. 10.1016/j.jconrel.2006.10.029. [DOI] [PubMed] [Google Scholar]
- Kumashiro Y.; Huh K. M.; Ooya T.; Yui N. Modulatory factors on temperature-synchronized degradation of dextran grafted with thermoresponsive polymers and their hydrogels. Biomacromolecules 2001, 2, 874–879. 10.1021/bm015527y. [DOI] [PubMed] [Google Scholar]
- Kono K.; Ozawa T.; Yoshida T.; Ozaki F.; Ishizaka Y.; Maruyama K.; Kojima C.; Harada A.; Aoshima S. Highly temperature-sensitive liposomes based on a thermosensitive block copolymer for tumor-specific chemotherapy. Biomaterials 2010, 31, 7096–7105. 10.1016/j.biomaterials.2010.05.045. [DOI] [PubMed] [Google Scholar]
- Yatvin M. B.; Weinstein J. N.; Dennis W. H.; Blumenthal R. Design of liposomes for enhanced local release of drugs by hyperthermia. Science 1978, 202, 1290–1293. 10.1126/science.364652. [DOI] [PubMed] [Google Scholar]
- Poon R. T.; Borys N. Lyso-thermosensitive liposomal doxorubicin: a novel approach to enhance efficacy of thermal ablation of liver cancer. Expert Opin. Pharmacother. 2009, 10, 333–343. 10.1517/14656560802677874. [DOI] [PubMed] [Google Scholar]
- Duan Q.; Miura Y.; Narumi A.; Shen X.; Sato S.; Satoh T.; Kakuchi T. Synthesis and thermoresponsive property of end-functionalized poly(N-isopropylacrylamide) with pyrenyl group. J. Polym. Sci., Part A: Polym. Chem. 2006, 44, 1117–1124. 10.1002/pola.21208. [DOI] [Google Scholar]
- Gil E. S.; Hudson S. M. Stimuli-reponsive polymers and their bioconjugates. Prog. Polym. Sci. 2004, 29, 1173–1222. 10.1016/j.progpolymsci.2004.08.003. [DOI] [Google Scholar]
- Yamada A.; Hiruta Y.; Wang J.; Ayano E.; Kanazawa H. Design of Environmentally Responsive Fluorescent Polymer Probes for Cellular Imaging. Biomacromolecules 2015, 16, 2356–2362. 10.1021/acs.biomac.5b00591. [DOI] [PubMed] [Google Scholar]
- Hiruta Y.; Nagumo Y.; Suzuki Y.; Funatsu T.; Ishikawa Y.; Kanazawa H. The effects of anionic electrolytes and human serum albumin on the LCST of poly(N-isopropylacrylamide)-based temperature-responsive copolymers. Colloids Surf., B 2015, 132, 299–304. 10.1016/j.colsurfb.2015.05.032. [DOI] [PubMed] [Google Scholar]
- van Elk M.; Deckers R.; Oerlemans C.; Shi Y.; Storm G.; Vermonden T.; Hennink W. E. Triggered release of doxorubicin from temperature-sensitive poly(N-(2-hydroxypropyl)-methacrylamide mono/dilactate) grafted liposomes. Biomacromolecules 2014, 15, 1002–1009. 10.1021/bm401904u. [DOI] [PubMed] [Google Scholar]
- Hayashi H.; Kono K.; Takagishi T. Temperature-dependent associating property of liposomes modified with a thermosensitive polymer. Bioconjugate Chem. 1998, 9, 382–389. 10.1021/bc9701454. [DOI] [PubMed] [Google Scholar]
- Kim M. S.; Lee D. W.; Park K.; Park S. J.; Choi E. J.; Park E. S.; Kim H. R. Temperature-triggered tumor-specific delivery of anticancer agents by cRGD-conjugated thermosensitive liposomes. Colloids Surf., B 2014, 116, 17–25. 10.1016/j.colsurfb.2013.12.045. [DOI] [PubMed] [Google Scholar]
- Sullivan S. M.; Huang L. Enhanced delivery to target cells by heat-sensitive immunoliposomes. Proc. Natl. Acad. Sci. U.S.A. 1986, 83, 6117–6121. 10.1073/pnas.83.16.6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.; Lyakhov I.; Loomis K.; Needle D.; Baxa U.; Yavlovich A.; Capala J.; Blumenthal R.; Puri A. Hyperthermia-triggered intracellular delivery of anticancer agent to HER2+ cells by HER2-specific affibody (ZHER2-GS-Cys)-conjugated thermosensitive liposomes (HER2+ affisomes). J. Controlled Release 2011, 153, 187–194. 10.1016/j.jconrel.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simard P.; Leroux J. C. pH-sensitive immunoliposomes specific to the CD33 cell surface antigen of leukemic cells. Int. J. Pharm. 2009, 381, 86–96. 10.1016/j.ijpharm.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kono K.; Takashima M.; Yuba E.; Harada A.; Hiramatsu Y.; Kitagawa H.; Otani T.; Maruyama K.; Aoshima S. Multifunctional liposomes having target specificity, temperature-triggered release, and near-infrared fluorescence imaging for tumor-specific chemotherapy. J. Controlled Release 2015, 216, 69–77. 10.1016/j.jconrel.2015.08.005. [DOI] [PubMed] [Google Scholar]
- Ta T.; Bartolak-Suki E.; Park E. J.; Karrobi K.; McDannold N. J.; Porter T. M. Localized delivery of doxorubicin in vivo from polymer-modified thermosensitive liposomes with MR-guided focused ultrasound-mediated heating. J. Controlled Release 2014, 194, 71–81. 10.1016/j.jconrel.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayano E.; Karaki M.; Ishihara T.; Kanazawa H.; Okano T. Poly (N-isopropylacrylamide)-PLA and PLA blend nanoparticles for temperature-controllable drug release and intracellular uptake. Colloids Surf., B 2012, 99, 67–73. 10.1016/j.colsurfb.2011.10.003. [DOI] [PubMed] [Google Scholar]
- Cheng Y.; Hao J.; Lee L. A.; Biewer M. C.; Wang Q.; Stefan M. C. Thermally controlled release of anticancer drug from self-assembled gamma-substituted amphiphilic poly(epsilon-caprolactone) micellar nanoparticles. Biomacromolecules 2012, 13, 2163–2173. 10.1021/bm300823y. [DOI] [PubMed] [Google Scholar]
- Peng C. L.; Tsai H. M.; Yang S. J.; Luo T. Y.; Lin C. F.; Lin W. J.; Shieh M. J. Development of thermosensitive poly(n-isopropylacrylamide-co-((2-dimethylamino) ethyl methacrylate))-based nanoparticles for controlled drug release. Nanotechnology 2011, 22, 265608 10.1088/0957-4484/22/26/265608. [DOI] [PubMed] [Google Scholar]
- Sundaresan V.; Menon J. U.; Rahimi M.; Nguyen K. T.; Wadajkar A. S. Dual-responsive polymer-coated iron oxide nanoparticles for drug delivery and imaging applications. Int. J. Pharm. 2014, 466, 1–7. 10.1016/j.ijpharm.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoso A. M.; Calejo M. T.; Morais C. M.; Cardoso A. L.; Cruz R.; Zhu K.; Pedroso de Lima M. C.; Jurado A. S.; Nystrom B. Application of thermoresponsive PNIPAAM-b-PAMPTMA diblock copolymers in siRNA delivery. Mol. Pharmaceutics 2014, 11, 819–827. 10.1021/mp400510a. [DOI] [PubMed] [Google Scholar]
- Na K.; Lee S. A.; Jung S. H.; Hyun J.; Shin B. C. Elastin-like polypeptide modified liposomes for enhancing cellular uptake into tumor cells. Colloids Surf., B 2012, 91, 130–136. 10.1016/j.colsurfb.2011.10.051. [DOI] [PubMed] [Google Scholar]
- Schild H. G.; Tirrell D. A. Microcalorimetric Detection of Lower Critical Solution Temperatures in Aqueous Polymer-Solutions. J. Phys. Chem. 1990, 94, 4352–4356. 10.1021/j100373a088. [DOI] [Google Scholar]
- Ishida T.; Kirchmeier M. J.; Moase E. H.; Zalipsky S.; Allen T. M. Targeted delivery and triggered release of liposomal doxorubicin enhances cytotoxicity against human B lymphoma cells. Biochim. Biophys. Acta 2001, 1515, 144–158. 10.1016/S0005-2736(01)00409-6. [DOI] [PubMed] [Google Scholar]
- Johnsson M.; Edwards K. Phase behavior and aggregate structure in mixtures of dioleoylphosphatidylethanolamine and poly(ethylene glycol)-lipids. Biophys. J. 2001, 80, 313–323. 10.1016/S0006-3495(01)76016-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirpotin D.; Hong K.; Mullah N.; Papahadjopoulos D.; Zalipsky S. Liposomes with detachable polymer coating: destabilization and fusion of dioleoylphosphatidylethanolamine vesicles triggered by cleavage of surface-grafted poly(ethylene glycol). FEBS Lett. 1996, 388, 115–118. 10.1016/0014-5793(96)00521-2. [DOI] [PubMed] [Google Scholar]
- Kreider R. B.; Miller G. W.; Schenck D.; Cortes C. W.; Miriel V.; Somma C. T.; Rowland P.; Turner C.; Hill D. Effects of phosphate loading on metabolic and myocardial responses to maximal and endurance exercise. Int. J. Sport Nutr. 1992, 2, 20–47. 10.1123/ijsn.2.1.20. [DOI] [PubMed] [Google Scholar]
- Kapoor M.; Burgess D. J. Cellular uptake mechanisms of novel anionic siRNA lipoplexes. Pharm. Res. 2013, 30, 1161–1175. 10.1007/s11095-012-0952-9. [DOI] [PubMed] [Google Scholar]
- Perez A. P.; Cosaka M. L.; Romero E. L.; Morilla M. J. Uptake and intracellular traffic of siRNA dendriplexes in glioblastoma cells and macrophages. Int. J. Nanomed. 2011, 6, 2715–2728. 10.2147/IJN.S25235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rejman J.; Oberle V.; Zuhorn I. S.; Hoekstra D. Size-dependent internalization of particles via the pathways of clathrin- and caveolae-mediated endocytosis. Biochem. J. 2004, 377, 159–169. 10.1042/bj20031253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanazawa H.; Sunamoto T.; Matsushima Y.; Kikuchi A.; Okano T. Temperature-responsive chromatographic separation of amino acid phenylthiohydantions using aqueous media as the mobile phase. Anal. Chem. 2000, 72, 5961–5966. 10.1021/ac0004658. [DOI] [PubMed] [Google Scholar]
- Verwey E. J. Theory of the stability of lyophobic colloids. J. Phys. Colloid Chem. 1947, 51, 631–636. 10.1021/j150453a001. [DOI] [PubMed] [Google Scholar]
- Marra J.; Israelachvili J. Direct measurements of forces between phosphatidylcholine and phosphatidylethanolamine bilayers in aqueous electrolyte solutions. Biochemistry 1985, 24, 4608–4618. 10.1021/bi00338a020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.