Background:
The extent of variation in analgesic prescribing following musculoskeletal injury among countries and cultural contexts is poorly understood. Such an understanding can inform both domestic prescribing and future policy. The aim of our survey study was to evaluate how opioid prescribing by orthopaedic residents varies by geographic context.
Methods:
Orthopaedic residents in 3 countries in which residents are the primary prescribers of postoperative analgesia in academic medical centers (Haiti, the Netherlands, and the U.S.) responded to surveys utilizing vignette-based musculoskeletal trauma case scenarios. The residents chose which medications they would prescribe for post-discharge analgesia. We standardized opioid prescriptions in the surveys by conversion to morphine milligram equivalents (MMEs). We then constructed multivariable regressions with generalized estimating equations to describe differences in opiate prescription according to country, the resident’s sex and training year, and the injury site and age in the test cases.
Results:
U.S. residents prescribed significantly more total MMEs per case (mean [95% confidence interval] = 383 [331 to 435]) compared with residents from the Netherlands (229 [160 to 297]) and from Haiti (101 [52 to 150]) both overall (p < 0.0001) and for patients treated for injuries of the femur (452 [385 to 520], 315 [216 to 414], and 103 [37 to 169] in the U.S., the Netherlands, and Haiti, respectively), tibial plateau (459 [388 to 531], 280 [196 to 365], and 114 [46 to 183]), tibial shaft (440 [380 to 500], 294 [205 to 383], and 141 [44 to 239]), wrist (239 [194 to 284], 78 [36 to 119], and 63 [30 to 95]), and ankle (331 [270 to 393], 190 [100 to 280], and 85 [42 to 128]) (p = 0.0272). U.S. residents prescribed significantly more MMEs for patients <40 years old (432 [374 to 490]) than for those >70 years old (327 [270 to 384]) (p = 0.0019).
Conclusions:
Our results demonstrate greater prescribing of postoperative opioids at discharge in the U.S. compared with 2 other countries, 1 low-income and 1 high-income. Our findings highlight the high U.S. reliance on opioid prescribing for postoperative pain control after orthopaedic trauma.
Clinical Relevance:
Our findings point toward a need for careful reassessment of current opioid prescribing habits in the U.S. and demand reflection on how we can maximize effectiveness in pain management protocols and reduce provider contributions to the ongoing opioid crisis.
Musculoskeletal injuries are responsible for a large global burden of preventable injuries, disability, and death1,2. In the U.S., opioid prescribing for such conditions is currently considered problematic and appears to be a major factor contributing to what is considered an opioid epidemic by bodies such as the Centers for Disease Control and Prevention (CDC)3-5.
Over the past 20 years, U.S. opioid prescriptions and opioid-related deaths have increased greatly5. U.S. physicians and policymakers have attempted to address the opioid crisis by curtailing the frequency and quantity of opioid prescriptions5,6. Understanding the variation that exists across countries and cultures can help inform prescribing and domestic policy. While musculoskeletal injuries occur globally, the extent of variation in analgesic prescribing among countries for similar injuries remains poorly understood7. Although there have been several international studies of opioid prescribing practices in the Dominican Republic, the Netherlands, and China, these studies have been qualitative or retrospective, or have not addressed opioid prescribing after operative management7-9. We are aware of only a single quantitative comparative study of international postoperative opioid prescribing, which compared the U.S. and the Netherlands10.
We employed surveys to explore how opioid prescribing, in terms of total quantity and duration, at discharge after orthopaedic trauma surgery varies by national context. We used a vignette-based design because it has lower social desirability bias, allows greater variable manipulation, and has greater hypothesized construct validity and reliability11. The study purpose was to improve orthopaedic trauma care by providing the groundwork for pain management practices. This study represents the first quantitative analysis comparing opioid use between high and low-income countries to contextualize U.S. prescribing practices.
Materials and Methods
This survey study was approved by the Brigham and Women’s Hospital institutional review board.
Setting
Orthopaedic residents at 9 academic residency programs across 3 countries (the U.S., the Netherlands, and Haiti) were surveyed, between April and November 2017, utilizing a set of vignettes summarizing 10 musculoskeletal trauma case scenarios. Of the 10 patients described in the vignettes, 5 were men and 5 were women, 5 were <45 years old and 5 were >70 years old, and 2 each described trauma to the ankle, femur, wrist, tibial shaft, and tibial plateau. Respondents were asked to indicate the type of drug, dose (mg), number of tablets, and duration (days) that they would prescribe as a postoperative discharge pain regimen in each of the 10 cases. The solicited responses were for prescriptions for the initial episode of care; refill requests were not evaluated.
The vignettes were translated from English into French for the residents in Haiti and Dutch for those in the Netherlands and were back-translated for quality control by native language speakers. Surveys were administered electronically using the Qualtrics survey tool in the U.S. and the Netherlands (Qualtrics.com). Pen-and-paper surveys were distributed in Haiti at a national orthopaedic continuing medical education (CME) conference with representation from all 3 Haitian orthopaedic residencies.
Participants
Our study population consisted of orthopaedic resident physicians in the countries of interest. In all centers surveyed, residents were the primary prescribers of postoperative analgesics, and they decided on the medication type, dose, frequency, and duration after surgery. We included all residents who had responded to the questions about what they would prescribe for at least 1 of the vignette cases and who had completed the demographic information. We excluded responses that were incomplete or could not be interpreted.
U.S. and Dutch respondents indicated their choice of ≥1 of the following medications for each case: Tylenol (paracetamol), ibuprofen, acetaminophen with codeine #3, tramadol, oxycodone, or hydromorphone, or chose “no medication” (see Appendix 1). Because of differences in medications available in Haiti, case medications were modified in conjunction with a native Haitian physician. Acetaminophen with codeine #3 was changed to codeine, ibuprofen was changed to diclofenac, and Tylenol (paracetamol) was changed to paracetamol. Opioid prescriptions in the surveys were standardized across countries by conversion into morphine milligram equivalents (MMEs)12. MMEs prescribed per case, MMEs prescribed per day, and total duration of opioid prescription were then derived from the responses.
Statistical Analysis
We described the characteristics of the residents and vignette cases using means and percentages. We performed multivariable regressions with generalized estimating equations (GEEs) with compound symmetry working correlation to examine the relationship between opiate prescription and (1) country, (2) resident’s sex, (3) resident’s training year, (4) test case age, and (5) test case site of injury. We also examined the interaction effect between country and (1) age and (2) injury site on total opiates prescribed. We included all variables with a p value of <0.05, including the interaction effects in the multivariable GEE regression. Study sample sizes were determined by feasibility and the maximum number of responses obtainable. Given that our analysis was exploratory in nature, no adjustment for multiple comparisons was performed. Variables that were not significant in the multivariable model were removed from the final model. We used SAS statistical software (SAS Institute) for all analyses.
Results
Study Sample
Table I presents demographic characteristics of the study participants. In total, 139 residents participated in the study. Eighty-five (61%) were from the U.S., 30 (22%) were Dutch, and 24 (17%) were Haitian. Seventy-four (87%) of the U.S. residents, 15 (50%) of the Dutch respondents, and 21 (91%) of the Haitian respondents were male. Fifteen (18%) of the U.S. residents were in the first year of their residency; 19 (22%), in the second; 19 (22%), in the third; 11 (13%), in the fourth; and 21 (25%), in the fifth. Four (33%) of the Dutch respondents were in the first year of their residency; 6 (50%), in the second; 1 (8%), in the third; and 1 (8%), in the fourth. Six (30%) of the Haitian respondents were in the first year of their residency; 1 (5%), in the second; 10 (50%), in the third; and 3 (15%), in the fourth. Response rates were 67% of 85 (U.S.), 50% of 30 (Netherlands), and 79% of 24 (Haiti). In addition to the 30 Dutch residents, 7 Dutch non-residents responded to the survey but were excluded from the analyses. Given concern that limited resources may hamper prescribing patterns in a low-resource setting, at the end of the survey we asked Haitian respondents whether they felt that the pain medications and dosing prescribed were adequate for post-discharge pain control; 11 of the 15 Haitian respondents who answered this question stated that they did.
TABLE I.
Descriptive Statistics of Survey Respondents
| No. (%) | |||
| U.S. | Netherlands*† | Haiti†‡ | |
| Sex | |||
| Male | 74 (87%) | 19 (51%) 15 (50%) | 21 (91%) |
| Female | 11 (13%) | 18 (49%) 15 (50%) | 2 (9%) |
| Resident | |||
| Yes | 85 (100%) | 30 (81%) | 24 (100%) |
| No | 7 (19%) | ||
| Full response to ≥1 case | |||
| Yes | 57 (67%) | 19 (51%) 15 (50%) | 19 (79%) |
| No | 28 (33%) | 18 (49%) 15 (50%) | 5 (21%) |
| Training year | |||
| 1 | 15 (18%) | 5 (31%) 4 (33%) | 6 (30%) |
| 2 | 19 (22%) | 6 (38%) 6 (50%) | 1 (5%) |
| 3 | 19 (22%) | 1 (6%) 1 (8%) | 10 (50%) |
| 4 | 11 (13%) | 1 (6%) 1 (8%) | 3 (15%) |
| 5 | 21 (25%) | 2 (13%) | |
| 6 | 1 (6%) | ||
The values for the residents only in the Netherlands are in bold.
The total number for training years differs from the total number of residents because of non-response.
The total number for sex differs from the total numbers of residents because of non-response.
Opioid Use Data
Bivariate Analyses
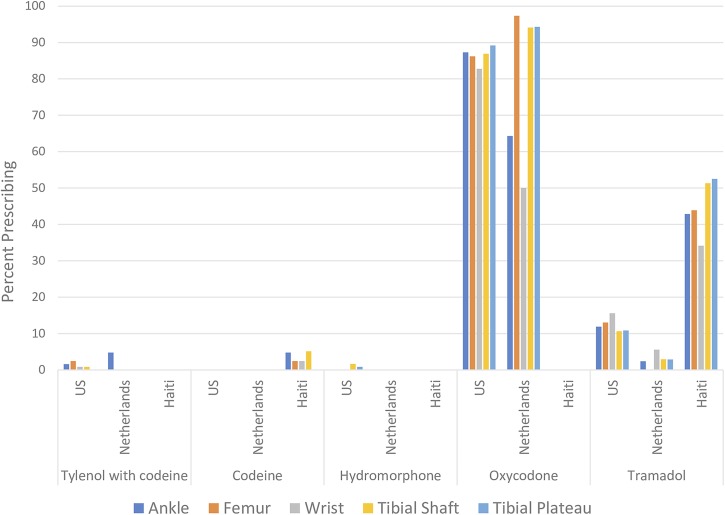
Opioid selection by the survey respondents is presented in Figure 1, stratified by injury site (ankle, femur, wrist, tibial shaft, and tibial plateau). Oxycodone was the opioid of choice in the U.S. and the Netherlands, whereas tramadol was in Haiti.
Fig. 1.
Percentages of respondents in each country prescribing each opioid.
Bivariate analyses of total MMEs prescribed per case revealed significant differences among countries (mean number of MMEs [95% confidence interval] = 383 [331 to 435] for the U.S., 229 [160 to 297] for the Netherlands, and 101 [52 to 150] for Haiti; p < 0.0001), between patient age groups (<40 years: 326 [278 to 374] and >70 years: 267 [226 to 308]; p = 0.0018), and according to injury site (tibial plateau: 358 [303 to 412], femur: 357 [304 to 411], tibial shaft: 354 [304 to 404], ankle: 257 [211 to 303], and wrist: 175 [142 to 207]; p < 0.0001) (Table II).
TABLE II.
Bivariate Analyses of Total MMEs Prescribed
| Total MMEs | |||
| Mean (Standard Deviation) | 95% Confidence Interval | P Value | |
| Country | <0.0001 | ||
| U.S. | 383 (27) | 331-435 | |
| Netherlands | 229 (35) | 160-297 | |
| Haiti | 101 (25) | 52-150 | |
| Sex | 0.8727 | ||
| Female | 291 (53) | 186-395 | |
| Male | 300 (23) | 255-345 | |
| Training year | 0.0221 | ||
| 1 | 292 (60) | 174-411 | |
| 2 | 341 (43) | 256-425 | |
| 3 | 216 (28) | 162-270 | |
| 4 | 263 (40) | 186-341 | |
| ≥5 | 466 (67) | 336-597 | |
| Age | 0.0018 | ||
| <40 yr | 326 (25) | 278-374 | |
| >70 yr | 267 (21) | 226-308 | |
| Injury site | <0.0001 | ||
| Ankle | 257 (23) | 211-303 | |
| Femur | 357 (27) | 304-411 | |
| Wrist | 175 (17) | 142-207 | |
| Tibial shaft | 354 (26) | 304-404 | |
| Tibial plateau | 358 (28) | 303-412 | |
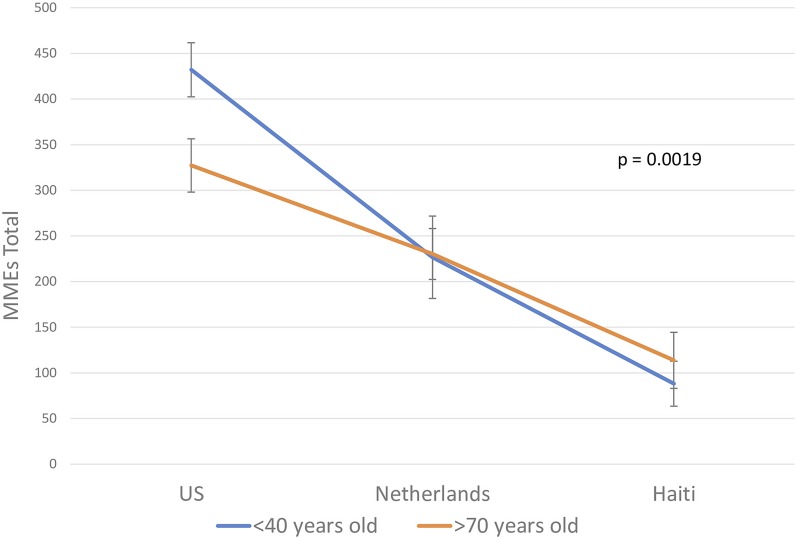
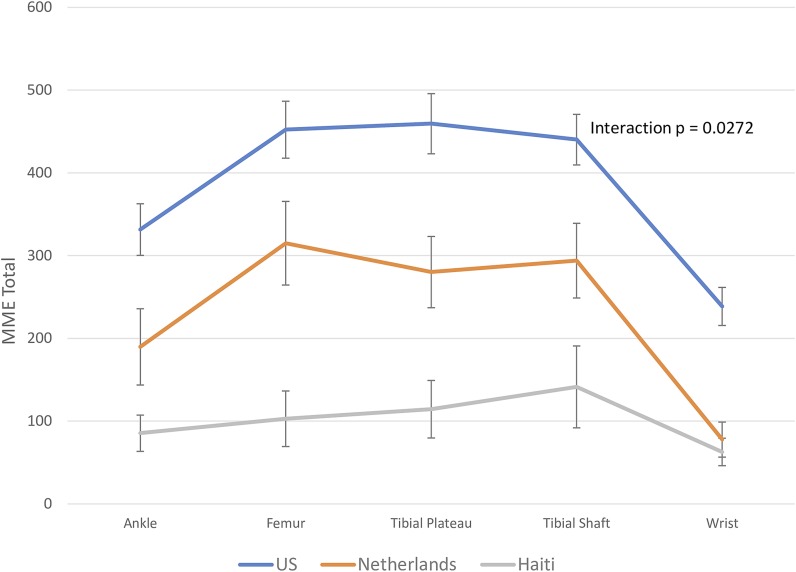
We found a significant interaction between patient age and country of prescriber for total MMEs prescribed (p = 0.0019), driven by increased opioid prescriptions by U.S. prescribers for patients <40 years of age (mean number of MMEs [95% confidence interval] U.S.: 432 [374 to 490], Netherlands: 227 [138 to 315], and Haiti: 88 [40 to 136]) compared with those >70 years of age (U.S.: 327 [270 to 384], Netherlands: 230 [176 to 285], and Haiti: 114 [54 to 174]) (Fig. 2). Similarly, the interaction between injury site and country of prescriber was also significant (p = 0.0272), with U.S. residents prescribing more MMEs overall than residents from the Netherlands or Haiti and Dutch residents prescribing more than Haitian residents for all injury sites—i.e., the femur (U.S.: 452 [385 to 520], Netherlands: 315 [216 to 414], and Haiti: 103 [37 to 169]), tibial plateau (U.S.: 459 [388 to 531], Netherlands: 280 [196 to 365], and Haiti: 114 [46 to 183]), tibial shaft (U.S.: 440 [380 to 500], Netherlands: 294 [205 to 383], and Haiti: 141 [44 to 239]), wrist (U.S.: 239 [194 to 284], Netherlands: 78 [36 to 119], and Haiti: 63 [30 to 95]), and ankle (U.S.: 331 [270 to 393], Netherlands: 190 [100 to 280], and Haiti: 85 [42 to 128]) (Fig. 3).
Fig. 2.
Mean total opioid prescription stratified by country and patient age. Our findings indicate a large difference in opioid prescribing based on patient age in the U.S., while prescription levels in Haiti and the Netherlands varied to a lesser degree on the basis of patient age. The I bars indicate the standard deviation.
Fig. 3.
Mean total opioid prescription stratified by country and injury site. Our findings indicate that residents in the U.S. are prescribing opioids at consistently higher levels than those in the Netherlands and Haiti. Residents in the Netherlands prescribed consistently higher levels of opioids than residents in Haiti except for cases of wrist injury. The I bars indicate the standard deviation.
Multivariable Analyses
We constructed multivariable models and found that injury site (p < 0.0001), country (p < 0.0001), and the interaction between patient age and country (p = 0.0015) were significantly associated with total MMEs prescribed (Table III). Training year was no longer significant in our final model and was excluded from the subsequent analyses. The resulting estimates for the mean number of total MMEs (95% confidence interval) prescribed by injury site were 112 (84 to 141) for wrist injuries, 193 (154 to 232) for ankle injuries, 291 (246 to 336) for tibial shaft injuries, 297 (251 to 342) for tibial plateau injuries, and 298 (253 to 342) for femoral injuries after accounting for other variables in the model. The mean total number of MMEs prescribed for patients >70 years old was lowest in Haiti (116 [56 to 176]), with higher values in the Netherlands (230 [175 to 285]) and U.S. (326 [270 to 383]). Similar results were found for patients <40 years of age, with a mean total number of MMEs of 88 (40 to 136) in Haiti, 234 (147 to 321) in the Netherlands, and 435 (377 to 493) in the U.S.
TABLE III.
Least Square Means for Total MME Prescription from the Multivariable Model with GEEs
| Effects | MME Estimate (95% Confidence Interval) | P Value |
| Main | ||
| Injury site | <0.0001 | |
| Ankle | 193 (154-232) | |
| Femur | 298 (253-342) | |
| Tibial plateau | 297 (251-342) | |
| Tibial shaft | 291 (246-336) | |
| Wrist | 112 (84-141) | |
| Interaction | ||
| Patient age × country | 0.0015 | |
| >70 yr old × Haiti | 116 (56-176) | |
| >70 yr old × Netherlands | 230 (175-285) | |
| >70 yr old × U.S. | 326 (270-383) | |
| <40 yr old × Haiti | 88 (40-136) | |
| <40 yr old × Netherlands | 234 (147-321) | |
| <40 yr old × U.S. | 435 (377-493) |
In addition to total MMEs, we also analyzed MMEs prescribed per day, opioid prescription duration, and likelihood of opioid prescription. Bivariate and multivariable analyses of MMEs prescribed per day and prescription duration demonstrated similar results to those performed for total MME prescription (see Appendices 2 through 6).
Discussion
Knowing how opioid prescribing varies among countries can help inform approaches to address the current U.S. opioid epidemic, but this variation remains poorly understood7. Our survey study evaluated how opioid prescription quantity and duration varied by national context in the setting of orthopaedic surgery postgraduate training.
We demonstrated a clinically meaningful difference between the U.S. and the Netherlands and Haiti in essentially all analyses performed. U.S. residents, compared with Dutch and Haitian residents, were more likely to prescribe opioids, prescribe more opioids per day, prescribe more total opioids for a given injury, and prescribe opioids for a longer duration.
The preponderance of opioids prescribed by U.S. residents suggests a heavy reliance on opioids for postoperative pain management compared with other countries. Prior work has demonstrated that filled opioid prescriptions for analgesia after low-risk surgical procedures significantly increased between 2004 and 2012, driven by an increase in prescribed MMEs/day13. Investigators examining orthopaedic pain management in the Dominican Republic revealed that patients relied on multiple analgesic modalities, ranging from nonsteroidal anti-inflammatory drugs (NSAIDs) to non-pharmacologic management14, suggesting that cultural differences may also account for different patient expectations for pharmacologic pain management. Furthermore, recent work from the Netherlands and Canada demonstrated non-inferiority of non-opioid treatment for postoperative pain control in adult and pediatric populations15,16. There has also been increasing evidence for the role of mental health factors in patient perception and self-modulation of pain17-20. Further research is required to explore how non-pharmacologic techniques of pain management as well as patient expectation management are employed in different contexts and how such differences might inform domestic opioid prescribing practices. In total, these findings suggest that, within the U.S., NSAIDs and other alternatives to opioids may hold potential in postoperative analgesia.
We also found that U.S. residents prescribed opioids for a significantly greater duration compared with those from the Netherlands or Haiti (see Appendices 2 and 6). This difference may be driven by cultural factors, past practices, and biases influencing opioid use in these countries relative to the U.S.21,22, greater opioid prescribing in the U.S., and limited access to opioids in Haiti. Reasons for the third possibility are not fully understood but may relate to higher costs of opioids in Haiti than in developed countries, possible restrictions from government regulation21, or simply subjective norms in prescriber training. At least for low-risk operations, the duration of U.S. opioid prescriptions has remained stable since 2004, with the rise in opioid use due largely to increases in mean daily doses over the past decade13. This finding suggests that rising opioid consumption in the U.S. has not been greatly influenced by prescription duration. It remains unclear to what extent new federal and state legislation limiting opioid prescription duration will impact these trends in the coming years.
Differences in opioid prescriptions between U.S. and Dutch prescribers may be due in part to several causes, such as a cultural norm of low opioid prescribing8,23. Differences in reimbursement models may also limit opioid prescribing, as the Dutch capitated system limits “doctor shopping,” perhaps allowing Dutch physicians to be stricter with opioid prescriptions23. Another hypothesis relates to differences in advertising, as opioid advertising is heavily curtailed in the Netherlands24, whereas aggressive pharmaceutical advertising in the U.S. has been posited as a potential contributor to the opioid epidemic25. Differences in analgesia training for residents may also contribute, although prior work indicates little training is provided to residents in either country26-28. Another potential contributing factor may be differences between Dutch and U.S. pain protocols, although this hypothesis remains subject to debate as no prior systematic comparison has been identified in the literature and Dutch protocols have been found to vary widely29.
Recent work demonstrated that U.S. patients received opioids for musculoskeletal trauma at a higher rate than Dutch patients while they were inpatients and at the time of discharge22. The latter finding suggests that a potential way to improve the practice of U.S. postoperative pain management may be by reducing opioid prescriptions at hospital discharge and considering using more non-opioid modalities postoperatively to manage pain.
When the patients were stratified by age, it was found that only residents from the U.S. prescribed significantly more MMEs/day and MMEs in total for younger patients (<40 years) than for older patients (>70) (Fig. 2 and Appendix 4 [Figs. 1 and 2]). The duration of opioid prescription did not differ significantly between the 2 age groups. It may be that lower doses are prescribed to elderly patients out of concern about adverse events in that population, such as increased risk for chronic opioid use or delirium postoperatively30. However, U.S. prescribers may inadvertently be placing younger patients at greater risk for long-term use. Higher opioid doses have previously been associated with a dose-dependent increase in the risk of various postoperative complications31 and have been shown to increase the risk of overdose death for all opioid users, including those taking opioids for acute or postoperative pain32. It remains unclear whether patient perception of pain objectively differs by age or if it justifies increased prescribing for younger patients.
Limitations
This study has several limitations. First, while we sought to characterize real prescription trends in pain management, our surveys only approximate actual prescription data. As we did not include patient-reported pain scores in our survey vignettes, we cannot conclude if trends described in this study are accurately reflected in clinical practice. However, we believe that, because we provided standardized cases to all survey participants, the differences observed in our comparisons among countries remain valid. Second, our comparison between the U.S. and a low-income country (Haiti) poses data interpretation challenges, given problems with resource availability in Haiti and differences in clinical training33. However, as the comparisons between the U.S. and Netherlands indicate, the large differences in opioid prescribing are not simply a reflection of low versus high-resource settings or opioid availability. Interestingly, the majority (73%) of the 15 responding Haitian orthopaedic residents indicated that they believed that their prescriptions were sufficient, suggesting that differences between Haiti and the U.S. cannot be attributed to resource limitations in Haiti alone. Third, our survey response rates ranged from 50% to 79% among the countries surveyed, raising the possibility of non-response bias. Fourth, we surveyed only a subset of residents in each country, with a preponderance of responses from the U.S. This discrepancy occurred because there are far fewer orthopaedic residents in Haiti or the Netherlands as compared with the U.S., limiting our obtainable sample size. While differences in sample sizes might accentuate differential compositions of each country’s orthopaedic residents and thereby potentially contribute to bias, multivariable analyses did not show any resident demographic except nationality to significantly contribute to differential opioid prescriptions (Table III). Finally, our study focused only on prescribing by residents and not by attending physicians, as the former provide the majority of pain management prescriptions in academic medical centers34. We believe that focusing on resident prescribing accurately captures opioid prescribing patterns as occurs in clinical practice, and this is supported by the literature27.
Conclusions
In summary, this study provides insight into cross-cultural opioid prescribing patterns for analgesia after orthopaedic trauma surgery. We found that U.S. resident physicians prescribe opioids more frequently, more opioids per day, and more total MMEs for a given injury and prescribe them for longer durations than Dutch or Haitian residents. These findings strongly suggest a potential overreliance on opioids for postoperative analgesia in the U.S. Such findings point toward a need for careful reassessment of current opioid prescribing habits in the U.S. and demand reflection on how we can maximize effectiveness in pain management protocols and reduce provider contributions to the ongoing opioid crisis.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F308).
Footnotes
Investigation performed at Harvard Medical School and the Harvard Combined Orthopaedic Residency Program, Boston, Massachusetts
Disclosure: This work was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases: P30 AR072577, K24 AR057827. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F307).
References
- 1.Agarwal-Harding KJ, von Keudell A, Zirkle LG, Meara JG, Dyer GS. Understanding and addressing the global need for orthopaedic trauma care. J Bone Joint Surg Am. 2016. November 2;98(21):1844-53. [DOI] [PubMed] [Google Scholar]
- 2.Mock C, Cherian MN. The global burden of musculoskeletal injuries: challenges and solutions. Clin Orthop Relat Res. 2008. October;466(10):2306-16. Epub 2008 Aug 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helmerhorst GT, Teunis T, Janssen SJ, Ring D. An epidemic of the use, misuse and overdose of opioids and deaths due to overdose, in the United States and Canada: is Europe next? Bone Joint J. 2017. July;99-B(7):856-64. [DOI] [PubMed] [Google Scholar]
- 4.Manchikanti L, Helm S, 2nd, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States. Pain Physician. 2012. July;15(3)(Suppl):ES9-38. [PubMed] [Google Scholar]
- 5.Morris BJ, Mir HR. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015. May;23(5):267-71. [DOI] [PubMed] [Google Scholar]
- 6.The National Academies of Sciences, Engineering, and Medicine Health and Medicine Division. Pain management and the opioid epidemic: balancing societal and individual benefits and risks of prescription opioid use. http://nationalacademies.org/hmd/reports/2017/pain-management-and-the-opioid-epidemic.aspx. 2017. July 13. Accessed 2018 Feb 22. [PubMed]
- 7.Devine CA, Yu A, Kasdin RG, Bogart LM, Davis AM, Alcántara Abreu L, Ghazinouri R, Thornhill TS, Katz JN. Postoperative pain management among Dominican and American health-care providers: a qualitative analysis. J Bone Joint Surg Am. 2016. June 15;98(12):e50. [DOI] [PubMed] [Google Scholar]
- 8.Lindenhovius AL, Helmerhorst GT, Schnellen AC, Vrahas M, Ring D, Kloen P. Differences in prescription of narcotic pain medication after operative treatment of hip and ankle fractures in the United States and the Netherlands. J Trauma. 2009. July;67(1):160-4. [DOI] [PubMed] [Google Scholar]
- 9.Zhu H, Gao Y, Zhang C, Zheng X. A prospective evaluation of patient-reported opioid utilization after nonoperative treatment of fractures and dislocations. J Bone Joint Surg Am. 2018. July 18;100(14):1177-83. [DOI] [PubMed] [Google Scholar]
- 10.Helmerhorst GT, Lindenhovius AL, Vrahas M, Ring D, Kloen P. Satisfaction with pain relief after operative treatment of an ankle fracture. Injury. 2012. November;43(11):1958-61. Epub 2012 Aug 16. [DOI] [PubMed] [Google Scholar]
- 11.Steiner PM, Atzmüller C, Su D. Designing valid and reliable vignette experiments for survey research: a case study on the fair gender income gap. J Methods Meas Soc Sci. 2016;7(2):52-94. [Google Scholar]
- 12.Centers for Medicare and Medicaid Services. Opioid morphine equivalent conversion factors. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-March-2015.pdf. 2014. May Accessed 2018 Feb 24.
- 13.Wunsch H, Wijeysundera DN, Passarella MA, Neuman MD. Opioids prescribed after low-risk surgical procedures in the United States, 2004-2012. JAMA. 2016. April 19;315(15):1654-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu A, Devine CA, Kasdin RG, Orizondo M, Perdomo W, Davis AM, Bogart LM, Katz JN. Pain management among Dominican patients with advanced osteoarthritis: a qualitative study. BMC Musculoskelet Disord. 2016. May 17;17:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helmerhorst GTT, Zwiers R, Ring D, Kloen P. Pain relief after operative treatment of an extremity fracture: a noninferiority randomized controlled trial. J Bone Joint Surg Am. 2017. November 15;99(22):1908-15. [DOI] [PubMed] [Google Scholar]
- 16.Poonai N, Datoo N, Ali S, Cashin M, Drendel AL, Zhu R, Lepore N, Greff M, Rieder M, Bartley D. Oral morphine versus ibuprofen administered at home for postoperative orthopedic pain in children: a randomized controlled trial. CMAJ. 2017. October 10;189(40):E1252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014. February 11;348:g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finger A, Teunis T, Hageman MG, Ziady ER, Ring D, Heng M. Association between opioid intake and disability after surgical management of ankle fractures. J Am Acad Orthop Surg. 2017. July;25(7):519-26. [DOI] [PubMed] [Google Scholar]
- 19.Rosenbloom BN, McCartney CJL, Canzian S, Kreder HJ, Katz J. Predictors of prescription opioid use 4 months after traumatic musculoskeletal injury and corrective surgery: a prospective study. J Pain. 2017. August;18(8):956-63. Epub 2017 Mar 25. [DOI] [PubMed] [Google Scholar]
- 20.Bot AGJ, Bekkers S, Arnstein PM, Smith RM, Ring D. Opioid use after fracture surgery correlates with pain intensity and satisfaction with pain relief. Clin Orthop Relat Res. 2014. August;472(8):2542-9. Epub 2014 Apr 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chahal HS, St Fort N, Bero L. Availability, prices and affordability of essential medicines in Haiti. J Glob Health. 2013. December;3(2):020405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helmerhorst G. Pain relief after musculoskeletal trauma. Br J Sports Med. 2019. March;53(5):318 Epub 2018 Sep 7. [DOI] [PubMed] [Google Scholar]
- 23.Wagemaakers FN, Hollingworth SA, Kreijkamp-Kaspers S, Tee EHL, Leendertse AJ, van Driel ML. Opioid analgesic use in Australia and the Netherlands: a cross-country comparison. Int J Clin Pharm. 2017. August;39(4):874-80. Epub 2017 Jun 12. [DOI] [PubMed] [Google Scholar]
- 24.Hoorneman W, de Vrey R, Essink B, Chistyakova A. Distribution and marketing of drugs in the Netherlands: overview. http://global.practicallaw.com/5-618-5575. 2015. Accessed 2019 Mar 5.
- 25.Sullivan MD, Howe CQ. Opioid therapy for chronic pain in the United States: promises and perils. Pain. 2013. December;154(Suppl 1):S94-100. Epub 2013 Sep 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Boekel RL, Steegers MAH, Verbeek-van Noord I, van der Sande R, Vissers KCP. Acute pain services and postsurgical pain management in the Netherlands: a survey. Pain Pract. 2015. June;15(5):447-54. Epub 2014 Mar 24. [DOI] [PubMed] [Google Scholar]
- 27.Chiu AS, Ahle SL, Freedman-Weiss MR, Yoo PS, Pei KY. The impact of a curriculum on postoperative opioid prescribing for novice surgical trainees. Am J Surg. 2019. February;217(2):228-32. Epub 2018 Aug 25. [DOI] [PubMed] [Google Scholar]
- 28.Gaspar MP, Pflug EM, Adams AJ, Jacoby SM, Shin EK, Osterman AL, Kane PM. Self-reported postoperative opioid-prescribing practices following commonly performed orthopaedic hand and wrist surgical procedures: a nationwide survey comparing attending surgeons and trainees. J Bone Joint Surg Am. 2018. October 3;100(19):e127. [DOI] [PubMed] [Google Scholar]
- 29.Ossendorp R, Forouzanfar T, Ashton-James CE, Bloemers F. Protocols for treating the postoperative pain of fractures in Dutch hospitals. J Pain Res. 2013;6:635-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016. September 1;176(9):1286-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cozowicz C, Olson A, Poeran J, Mörwald EE, Zubizarreta N, Girardi FP, Hughes AP, Mazumdar M, Memtsoudis SG. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain. 2017. December;158(12):2422-30. [DOI] [PubMed] [Google Scholar]
- 32.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011. April 6;305(13):1315-21. [DOI] [PubMed] [Google Scholar]
- 33.Nau BJ, Woolley PM, Vertilus R. Orthopaedics in Haiti. J Bone Joint Surg Am. 2018. January 17;100(2):e9. [DOI] [PubMed] [Google Scholar]
- 34.Chiu AS, Healy JM, DeWane MP, Longo WE, Yoo PS. Trainees as agents of change in the opioid epidemic: optimizing the opioid prescription practices of surgical residents. J Surg Educ. 2018. Jan-Feb;75(1):65-71. Epub 2017 Jul 10. [DOI] [PubMed] [Google Scholar]