Abstract
We aim to examine temporal trends of orthopedic operations and opioid-related hospital stays among seniors in the nation and states of Oregon and Washington where marijuana legalization was accepted earlier than any others.
As aging society advances in the United States (U.S.), orthopedic operations and opioid-related hospital stays among seniors increase in the nation.
A serial cross-sectional cohort study using the healthcare cost and utilization project fast stats from 2006 through 2015 measured annual rate per 100,000 populations of orthopedic operations by age groups (45–64 vs 65 and older) as well as annual rate per 100,000 populations of opioid-related hospital stays among 65 and older in the nation, Oregon and Washington states from 2008 through 2017. Orthopedic operations (knee arthroplasty, total or partial hip replacement, spinal fusion or laminectomy) and opioid-related hospital stays were measured. The compound annual growth rate (CAGR) was used to quantify temporal trends of orthopedic operations by age groups as well as opioid-related hospital stays and was tested by Rao–Scott correction of χ2 for categorical variables.
The CAGR (4.06%) of orthopedic operations among age 65 and older increased (P < .001) unlike the unchanged rate among age 45 to 64. The CAGRs of opioid-related hospital stays among age 65 and older were upward trends among seniors in general (6.79%) and in Oregon (10.32%) and Washington (15.48%) in particular (all P < .001).
Orthopedic operations and opioid-related hospital stays among seniors increased over time in the U.S. Marijuana legalization might have played a role of gateway drug to opioid among seniors.
Keywords: drug policy, marijuana, opioid, orthopedic surgeries
1. Introduction
The growing crisis of the United States (U.S.) opioid epidemic affects all of us and has become grave public health threat. The prevalence of aging-related orthopedic conditions necessarily increases along with the prolonged life expectancy. In the U.S., lower back pain and other degenerative joint diseases have been the leading causes of disability from 1990 to 2016.[1] Due to the longer life expectancy, advancement in surgical techniques, technologies (eg, implants, instrumentation), and postoperative care, the number of orthopedic operations, for example, lumbar fusion procedures among Medicare beneficiaries increased during the past decade.[2] Considering the nation's opioid epidemic, the demands for opioid prescription most likely increases among seniors who had orthopedic operations. However, the strict controlled substance policies make the opioid prescription more difficult across the states. Also, in order to reduce misuse and abuse of prescribed opioids, more than 30 states have implemented the prescription drug monitoring program (PDMP) during the past 2 decades. Yet, PDMPs have not been effective in reducing drug overdose mortality rates.[3] As such, PDMPs may not be effective to comprehensively address prescription diversions, doctor shopping, or other abusive behaviors of other than prescribed opioids. Federal rescheduling hydrocodone product, the most commonly prescribed opioid analgesic, from schedule III to schedule II in 2014 faced unexpected increase in opioid-related hospitalizations without documented opioid prescriptions that may represent an increase in illegal use among Medicare beneficiaries.[4]
No previous studies focused on the trends of orthopedics operations due to degenerative joint diseases in general among older adults. Older adults are particularly susceptible to toxicity and adverse effects from opioid use.[5] Understanding the interactions between trends of orthopedics operations and opioid-related hospital stays in older adults is critical to the development of timely and effective interventions.
Although medical marijuana laws are associated with a reduction in overdose deaths from opioid pain relievers, the effect of marijuana legalization on both prescribed and illicit opioids use needs further attention, in older adults in particular. The current brief report examined temporal trends of orthopedics operations due to degenerative joint disease and opioid-related hospital stays in the nation and states of Oregon and Washington where marijuana legalization was accepted earlier than other states and shared similar timeline of legal processes.
2. Methods
2.1. Data source
Study design was a serial retrospective cross-sectional data analysis. We obtained data from the healthcare cost and utilization project (HCUP) fast stats: most common operations during inpatient stays from 2006 through 2015 and opioid-related hospital use in the nation, and states of Oregon and Washington from 2008 through 2017 (HCUP, 2017 and 2018). Institutional review board review was not necessary because all data were secondary, completely de-identified, and publicly available.
2.2. Main measurements and variables of interest
The main measurements were annual rates per 100,000 populations to estimate the trends of orthopedic operations and opioid-related hospital stays. Orthopedic operations were limited to the hospital inpatient procedures for degenerative joint conditions: knee arthroplasty, total or hip replacement, spinal fusion or laminectomy. Orthopedic operations and opioid-related conditions were identified by using the international classification of disease, 9th revision (until 2015 3rd quarter) or 10th revision (from 2015 4th quarter), clinical modification (ICD-9 or 10-CM) and were defined by the HCUP elsewhere.[6] The annual trends of orthopedics operations were categorized by 2 age groups (age 65 and older, our interest group; age 45–64, reference group). Young age groups were not added in analysis due to too low rates of orthopedic operations.
2.3. Statistical analysis
The compound annual growth rate (CAGR) was used to quantify temporal trends of annual rate of orthopedic operations and opioid-related hospital stays per 100,000 populations. Statistical significance was tested by the Rao–Scott correction of χ2 tests for categorical variables. In the CAGR, year A is x, and year B is y; thus, CAGR = (y/x){1/(B/A)}−1. All reported P values were 2-tailed, P values <.05 were considered statistically significant.
3. Results
The CAGR (4.06%) of orthopedic operations among 65 and older increased (3269 per 100,000 in 2006; 4675 per 100,000 in 2015, P < .001) unlike the unchanged rate among age 45 to 64 (CAGR = 1.17%, P = .239) as presented in Figure 1A. Figure 1B presents trends of annual rate of opioid-related hospital stay per 100,000. The CAGR of opioid-related hospital stay was 6.79% in the nation (192 per 100,000 in 2008; 304 per 100,000 in 2015, P < .001); 10.32% in Oregon (368 per 100,000 in 2008; 790 per 100,000 in 2016, P < .001); 15.48% in Washington (213 per 100,000 in 2008; 778 per 100,000 in 2017, P < .001). We also found out the geographic variation in the trends of opioid-related hospital use among 65 years or older. The absolute gap between annual rates of opioid-related hospital stays in the States of Oregon/Washington and that of national average has been wider over time. These gaps were less than 2 times in 2008. However, these gaps were more than twice in 2015.
Figure 1.
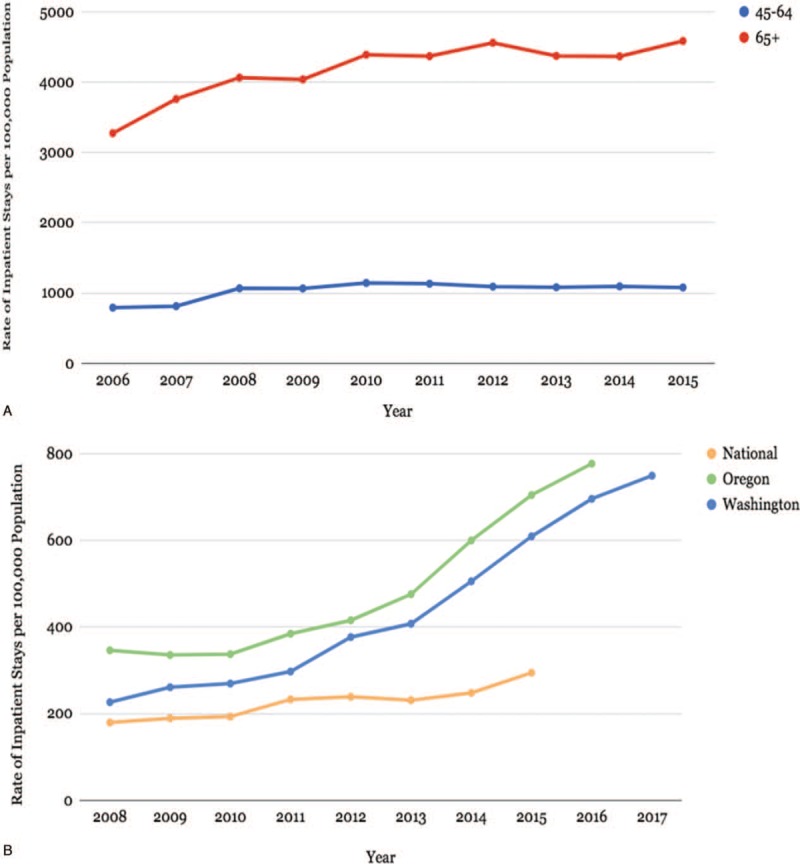
(A) Annual rate of orthopedic operations by age groups: 2006-15. (B) Annual rate of opioid-related hospital stays among age 65+: National, Oregon, and Washington states.
4. Discussion
Upward trends of orthopedic operations and opioid-related hospital stays among older adults were observed in the nation in general as well as states of Oregon and Washington states where marijuana legalization was accepted earlier than other states and shared similar timeline of legal processes. In response to the increased volume of orthopedic operations, a substantial growth in opioid prescriptions among 65 years old and older Medicare beneficiaries have been observed in the previous nationally representing data.[4] Opioid-related hospital use concerns overdose as well as underutilization (pain crisis or opioid withdrawal) even though we cannot discern these 2 opposite directions of opioid-related hospital use.[5] The sharp increase in opioid-related hospital stays overall during the transition to ICD-10-CM may be partly explained by coding instability due to more missing cases from old ICD-9-CM system.[6]
Oregon and Washington states share the similarity of drug policies such as the same year of PDMP in 2011 and medical marijuana legalization in 1998, and its dispensary in 2009.[7] The residents of Oregon and Washington have quickly accepted, within 3 to 5 years of medical marijuana dispensary, the recreational marijuana due to the familiarity with medical marijuana dispensary, socially/locally accepted marijuana use at home and affordable price.[7] Marijuana might have played a role of gateway drug to opioid.[8] Medical marijuana laws appear to have advanced an unhealthy social contagion of substance use in general, contributing to a collective trend toward the passage of recreational marijuana legalization laws, according to the 3 nationally representing U.S. adult surveys.[9] This speculation was empirically assessed by Shen et al. using the national emergency department (ED) visit dataset, Nationwide Emergency Department Sample.[10] Rates of marijuana-associated ED visits showed significant increases in the West region as compared with other regions between 2006 and 2014.[10] These findings indicate a potential linkage between effect of recreational marijuana legalization and changing trends in marijuana use. It has taken over 11 years from the legalization to the local dispensaries, older adults eagerly waited for the medical marijuana to become available.[8] Such experience arguably resulted in older adults’ greater responsiveness to the availability of the opioids. Middle-age group (45–54 years) most likely will have similar degenerative joint diseases in near future and may follow the similar trends to the current older adults. In fact, the recent study using a nationwide private insurance claim database, there was no association between the number of initial opioid prescription and likelihood of opioid refill after surgery.[11] In other words, variation in probability of refill opioids after surgery was not attributed by surgery itself, but, was more attributed by psychosocial factors such as mental health and substance use disorders.[11] Especially, among retirement-age adults, the poor, as well as Medicaid enrollees, were disproportionate users of opioid (both prescribed and illicit) out of perceived necessity rather than out of choice based on the Health and Retirement Study, nationally representing survey analysis.[12]
Upward trends of the opioid-related hospital use among seniors in general and in Oregon and Washington in particular, call for immediate actions. First, research should precisely differentiate purposes of opioid-associated hospital use in a nationally representative sample. Second, more interdisciplinary and patient-centered care should be taken to manage older adults with degenerative joint diseases. For example, possible interventions include:
-
(1)
promoting collaborations between healthcare providers (surgeon, pain specialist, and primary care provider) and maintaining single prescriber-pharmacy to optimize pain management,
-
(2)
improving care coordination to streamline mobility, transportation, and durable medical equipment support among older adults with degenerative joint diseases, and
-
(3)
avoiding stigmatizing the opioid-use disorders to maintain the social well-being of individuals and their family in communities.
We acknowledge several limitations. First, usually, low sensitivity and high specificity in weighted estimates occurred when identifying persons who use illicit drug from administrative claim data.[13] Second, the coding accuracy of opioid-related conditions as well as transition stability from the ICD-9 to ICD-10 systems remains relatively low.[6,14] Lastly, the states of Oregon and Washington may not represent west or southwest region where most of these states adopted marijuana legalization. Despite these potential limitations, we believe this is the first study to report several new insights to the current. To the best of our knowledge, there was no previous study that examined the trends of orthopedic operations and opioid-related hospital stays among seniors in the nation and states of Oregon and Washington where marijuana was legalized.
Author contributions
Conceptualization: Pearl Kim, Takashi Yamashita, Jinwook Hwang, Se Won Lee, Hee-Taik Kang, Yong-Jae Lee.
Data curation: Jay J Shen, Georgia Dounis, Dong-Hun Han, Ji Eun Kim, David Byun.
Formal analysis: Seong-Min Park.
Investigation: Pearl Kim, Seong-Min Park, Se Won Lee, Hee-Taik Kang, Dong-Hun Han, Ji Eun Kim, David Byun.
Methodology: Seong-Min Park, Jinwook Hwang, Yong-Jae Lee, Dong-Hun Han.
Project administration: Sung-Youn Chun, Hee-Taik Kang, Ji Eun Kim, Tsigab Bahta, Ji Won Yoo.
Resources: Jay J Shen, Seong-Min Park, Sung-Youn Chun, Sun Jung Kim, Jinwook Hwang, Se Won Lee, Georgia Dounis, Yong-Jae Lee, Dong-Hun Han, Hyeyoung Yeom, Tsigab Bahta, Ji Won Yoo.
Software: Sung-Youn Chun, Sun Jung Kim, Georgia Dounis.
Supervision: Takashi Yamashita, Sung-Youn Chun, Sun Jung Kim, Jinwook Hwang, Ji Won Yoo.
Validation: Takashi Yamashita, Sun Jung Kim, Jinwook Hwang, Yong-Jae Lee, Ji Eun Kim, Ji Won Yoo.
Visualization: Sun Jung Kim, Jinwook Hwang, Se Won Lee, Yong-Jae Lee, Ji Eun Kim, Hyeyoung Yeom, David Byun, Tsigab Bahta.
Writing – original draft: Takashi Yamashita, Jay J Shen, Hyeyoung Yeom, Ji Won Yoo.
Writing – review and editing: Takashi Yamashita, Jinwook Hwang, Se Won Lee, Georgia Dounis, Hee-Taik Kang, Yong-Jae Lee, Dong-Hun Han, Ji Eun Kim, Hyeyoung Yeom, David Byun, Tsigab Bahta, Ji Won Yoo.
Takashi Yamashita orcid: 0000-0003-2325-126X.
Footnotes
Abbreviations: CAGR = compound annual growth rate, ED = emergency department, HCUP = healthcare cost and utilization project, ICD-9, ICD-10-CM = international classification of disease, 9th revision, 10th revision, clinical modification, PDMP = prescription drug monitoring program, U.S. = United States.
PK and TY equally contributed as lead authors.
The manuscript has been seen and approved by all authors.
The authors have no conflicts of interest to disclose.
References
- [1].The US Burden of Disease Collaborators. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA 2018;319:1444–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Buser Z, Ortega B, D’Oro A, et al. Spine degenerative conditions and their treatments: national trends in the United States of America. Global Spine J 2018;8:57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Nam YH, Shea DG, Shi Y, et al. State prescription drug monitoring programs and fatal drug overdoses. Am J Manag Care 2017;23:297–303. [PubMed] [Google Scholar]
- [4].Kuo YF, Raji MA, Liaw V, et al. Opioid prescriptions in older medicare beneficiaries after the 2014 federal rescheduling of hydrocodone products. J Am Geriatr Soc 2018;66:945–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rubin R. Analysis reveals large increase in hospitalizations in recent years among older patients prescribed opioids. JAMA 2014;312:1621–3. [DOI] [PubMed] [Google Scholar]
- [6].Moore BJ, Barrett ML. Case study: exploring how opioid-related diagnosis codes translate from ICD-9-CM to ICD-10-CM. Posted April 24th 2017. Agency for Healthcare Research and Quality. Available at: https://www.hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp Accessed June 25, 2018. [Google Scholar]
- [7].Pacula RL, Smart R. Medical marijuana and marijuana legalization. Annu Rev Clin Psychol 2017;13:397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hall W, Lynskey M. Why it is probably too soon to assess the public health effects of legalization of recreational cannabis use in the USA. Lancet Psychiatry 2016;3:900–6. [DOI] [PubMed] [Google Scholar]
- [9].Hashin DS, Sarvet AL, Cerda M, et al. US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws 1991-1992 to 2012-2013. JAMA Psychiatry 2017;74:579–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Shen JJ, Shan G, Kim PC, et al. Trends and related factors of cannabis-associated emergency department visits in the United States: 2006–2014. J Addict Med 2018;Epub ahead print. [DOI] [PubMed] [Google Scholar]
- [11].Sekhri S, Arona NS, Cottrell H, et al. Probability of opioid prescription refilling after surgery. Ann Surg 2018;268:271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Grol-Prokopczk H. Use and opinions of prescription opioids among older American adults: socioepidemographic predictors. J Gerontol B Psychol Sci Soc Sci 2018;Epub ahead print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kim HM, Smith EG, Stano CM, et al. Validation of key behaviorally based mental health diagnoses in administrative data: suicide attempt, alcohol use, illicit drug use and tobacco use. BMC Health Serv Res 2012;12:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Green CA, Perrin NA, Janoff SL, et al. Assessing the accuracy of opioid overdose and poisoning codes in diagnostic information from electronic health records, claims data, and death records. Pharmacopeidemiol Drug Saf 2017;26:509–17. [DOI] [PubMed] [Google Scholar]


