Supplemental Digital Content is available in the text
Keywords: chronic obstructive pulmonary disease, lymphocytes, meta-analysis, neutrophils
Abstract
Objective:
Neutrophil to lymphocyte ratio (NLR) is considered as an inflammatory biomarker for clinical outcomes in patients with chronic obstructive pulmonary disease (COPD). We aimed to conduct a meta-analysis to evaluate the prognostic values of NLR for the exacerbation and mortality in patients with COPD.
Methods:
We searched the database of Cochrane Central Register of Controlled Trials, EMBASE, and PubMed, before September 2017. The eligible studies were retrieved by 2 authors independently following the criteria. The pooled odds ratios (ORs) of included studies were used to evaluate the prognostic values of NLR. Subgroup analyses were conducted to make the results more accurate.
Results:
Nine studies with 5140 patients were enrolled in this analysis. The high NLR was associated with higher risk of exacerbation (OR: 3.81, 95% confidence interval [CI]: 1.20–12.13, P = .02) and mortality (OR: 2.60, 95% CI: 1.48–4.57, P < .01). By subgroup analysis, high NLR could predict the mortality in patients >70 years (OR: 2.16, 95% CI: 1.17–3.98, P = .01) but not in patients <70 years (OR: 4.08, 95% CI: 0.91–18.24, P = .07), and had a higher predictive ability in Asian group (OR: 3.64, 95% CI: 1.87–7.08, P < .01) than Eurasia group (OR: 1.82, 95% CI: 1.43–2.32, P < .01). In addition, high NLR could predict the short-term mortality (OR: 2.70, 95% CI: 1.10–6.63, P = .03) and the long-term mortality (OR: 2.61, 95% CI: 1.20–5.65, P = .02).
Conclusions:
The NLR may be an independent predictor for incidence of exacerbation in patients with COPD. In addition, high NLR may be associated with higher mortality in patients with COPD, especially for Asian and the patients with higher mean NLR.
1. Introduction
Chronic obstructive pulmonary disease (COPD) is characterized with the presence of air flow limitation and exacerbations caused by inflammation.[1,2] COPD is the third leading cause of mortality worldwide, and approximately 3 million patients died for COPD in 2012.[3] The severity of COPD is generally assessed by lung function, especially forced expiratory volume in 1 second (FEV1). However, the severity of inflammation could not be reflected by the measurements[4] and lung function is not routinely applied in the status of exacerbation.[5–7] Previous studies demonstrated the severity of inflammation and exacerbation could be identified by various biomarkers, such as C-reactive protein,[4,8–10] IL-6,[11] erythrocyte sedimentation rate,[12] procalcitonin,[13] and platelet to lymphocyte ratio.[14] Recently, neutrophil to lymphocyte ratio (NLR) in peripheral blood is drawing more attention as an inflammatory biomarker.
NLR has been considered as a predictor for clinical outcomes in various tumors[15,16] and ischemic stroke.[17–20] The NLR is the ratio of neutrophil and lymphocyte, which represent innate and adaptive immune, respectively.[16,21] The variation of NLR reflects the change of immune system and the inflammation response. Gunay et al[22] firstly used the NLR as a quick, cheap, and easily measurable biomarker for severity of inflammation in patients with COPD. Later, many studies showed that the NLR was an independent predictor for COPD exacerbation[23,24] and mortality.[23,25,26]
However, the prognostic value of NLR for COPD remains controversial. Lee et al[24] suggested the NLR was an effective predictor for respiratory hospitalization, while another study[27] showed the NLR had no significant association with COPD exacerbation. In addition, Yao et al[25] and Rahimirad et al[28] demonstrated the higher NLR was associated with higher mortality in COPD, while Sorensen et al[29] showed the NLR was not a biomarker for mortality in the COPD patients treated by systemic glucocorticoids. Thus, we conducted a meta-analysis to evaluate the prognostic values of NLR for exacerbation and mortality in patient with COPD.
2. Materials and methods
2.1. Search strategy
This meta-analysis was conducted following the PRISMA flow diagram.[30] A literature search was conducted using the search engines on the database of Cochrane Central Register of Controlled Trials, EMBASE, and PubMed, before April 2019. The eligible articles were searched using the keywords “neutrophil lymphocyte ratio” or “NLR” and “chronic obstructive pulmonary disease” or “COPD.” References in the eligible studies were checked to find additional related articles. This is a meta-analysis and the ethical approval was not necessary.
2.2. Study selection
After reviewing the titles and abstracts of all available articles, 2 reviewers retrieved the related articles independently with the inclusion criteria: articles reporting the COPD were diagnosed as the FEV1 lower than 70% of forced vital capacity (FVC) after bronchodilation[27,31]; articles reporting the odds ratios (ORs) and 95% confidence intervals [CIs] of NLR for the mortality or the exacerbation, which were defined as aggravation of respiratory symptoms and needed additional treatments (corticosteroids or antibiotics)[24,27]; case–control studies and cohort studies were included. Letters, case reports, reviews, or nonclinical articles were excluded.
2.3. Data extraction
The following data were extracted by 2 authors with a standard data form: year of publication, country, study design, number of patients, sex, mean age of patients, mean of FEV1/FVC, study period, mean NLR, follow-up time, ORs, and 95% CIs for mortality or exacerbation. The ORs and 95% CIs of multiple regression analysis would be first choice, if not available, the ORs and 95% CIs of univariate regression analysis would be used. The Quality In Prognosis Studies (QUIPS) tool was used to assess the risk of bias.[32,33]
2.4. Data analysis
The pooled ORs of were used to evaluate the association of NLR with mortality and exacerbation. We used the Review Manager Version 5.3 (Cochrane collaboration, Oxford, UK) to pool the results. The random effects model was used for all analyses. When there was a considerable heterogeneity with I2 >50% or P < .10, the sensitivity analysis would be used to make the results more conservative. The subgroup analysis also would be used to analyze the heterogeneity between the included studies. Using the STATA 13.0 (STATA Corporation, College Station, TX), the publication bias of included articles was evaluated by funnel plot with Begg rank correlation. There was a statistical significance if P < .05.
3. Results
3.1. Literature research
The initial research retrieved 63 articles and 2 authors screened the title and abstracts of all articles independently. One record was identified after checking the references of eligible articles. Seventeen articles were retrieved after excluding the unrelated articles and the full text of these eligible articles were inspected following the inclusion criteria.
After assessing the full text of eligible articles, 9 articles[23–28,34–36] were left and included in our analysis, and 6 records were excluded for exclusion criteria and without the available data for OR and 95% CIs. Based on the QUIPS tool, 2 studies[23,25] were rated as moderate risk and 6 studies[24,26–28,34,35] were rated as high quality. The supplemental Figure 1 showed the assessment of the risk of bias of the studies included.
3.2. Study characteristics
The characteristics of included studies were showed in the Table 1. Nine articles with 5140 patients, including 3 prospective studies and 5 retrospective studies, were included in this meta-analysis. Three studies were conducted in Eurasia and the rest of studies were conducted in Asia. The mean age of patients ranged from 61 to 72 years, and most of mean FEV1/FVC in included articles were about 50% (Figs. 1–3).
Table 1.
Characteristics of the included articles.
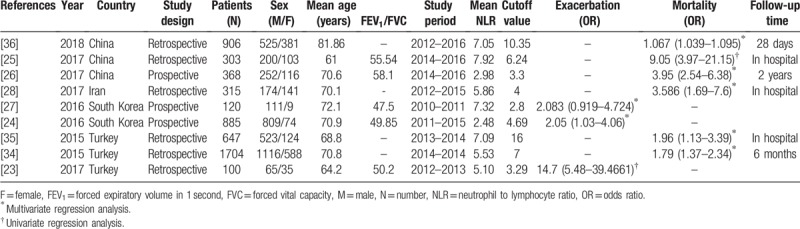
Figure 1.
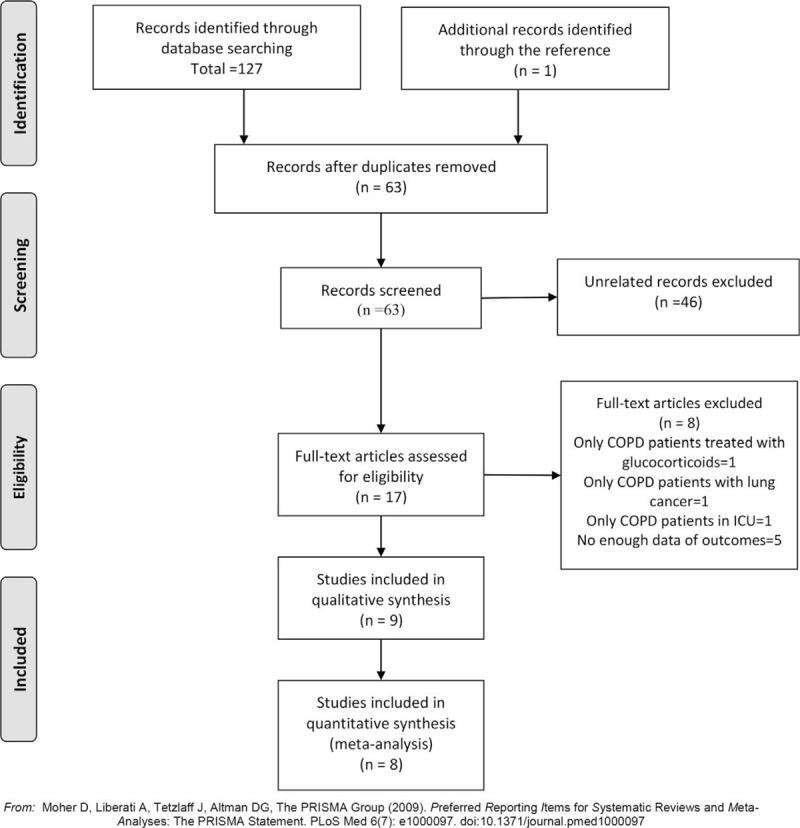
The flow diagram of procedure to search the included studies. COPD = chronic obstructive pulmonary disease.
Figure 3.
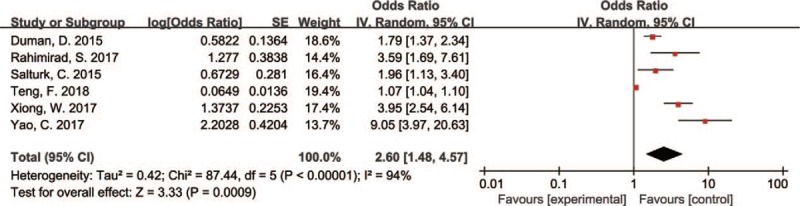
Forest plots for relationship between neutrophil to lymphocyte ratio and mortality.
Figure 2.
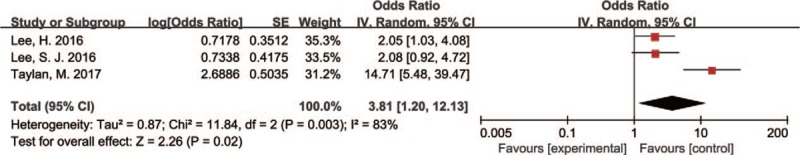
Forest plots for relationship between neutrophil to lymphocyte ratio and exacerbation.
3.2.1. Association of NLR and the exacerbation of COPD
Three articles[23,24,27] including 1105 subjects reported the relationship between NLR and exacerbation of COPD. Two[24,27] articles were prospective studies using multiple regression analysis, while the rest[23] were retrospective study using univariate regression analysis (Table 2). The pooled results suggested the high NLR had a higher risk of exacerbation (OR: 3.81, 95% CI: 1.20–12.13, P = .02). For the high heterogeneity (P = .003, I2 = 83%), we conducted the sensitivity analysis and found the heterogeneity was attributed to the study by Taylan et al.[23] After excluding this study, the heterogeneity significantly decreased (P = .98, I2 = 0%), and there was still a significant association between NLR and exacerbation with OR of 2.06 (95% CI: 1.22–3.49, P = .007).
Table 2.
Subgroup analysis results of exacerbation in chronic obstructive pulmonary disease.
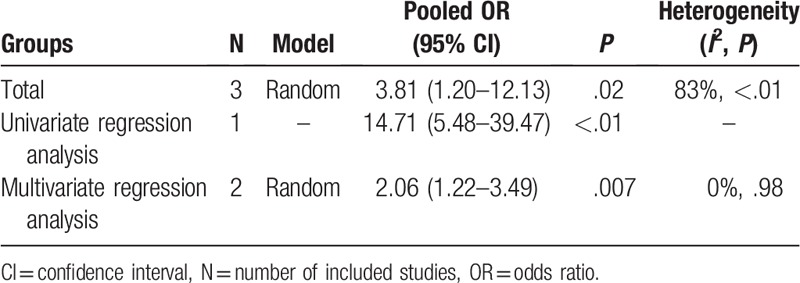
3.2.2. Subgroup analysis of NLR and exacerbation
The pooling results of 2 studies, which evaluated the association by multivariate regression analysis, suggested the higher NLR was associated with exacerbation of COPD (OR: 2.06, 95% CI: 1.22–3.49, P = .007) with no heterogeneity (P = .98, I2 = 0%).
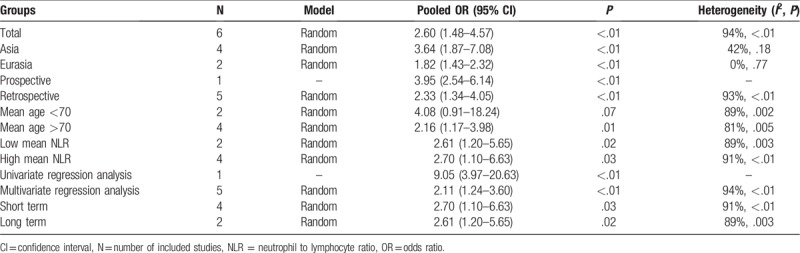
3.2.3. Association of NLR and the mortality
After pooling the results of 6 articles[25,26,28,34,35] with 4035 subjects, we found the higher NLR was associated with the higher mortality (OR: 2.60, 95% CI: 1.48–4.57, P < .01). Using the sensitivity analysis for the high heterogeneity (P < .01, I2 = 94%), we found the heterogeneity attributed to the study by Yao et al,[25] Xiong et al,[26] and Teng et al.[36] The pooling result was consistent and heterogeneity significantly decreased (P = .23, I2 = 31%) after excluding these studies (OR: 1.94, 95% CI: 1.54–2.44, P < .001).
3.2.4. Subgroup analysis of NLR and the mortality
The subgroup analysis of NLR and the mortality was performed by locations, study design, mean age of patients, mean NLR, follow-up time, and univariate/multivariate regression analysis. The higher NLR had effects on the mortality in Asian group (OR: 3.64, 95% CI: 1.87–7.08, P < .01) and Eurasia group (OR: 1.82, 95% CI: 1.43–2.32, P < .01), without significant heterogeneity (P = .18, I2 = 42% and P = .77, I2 = 0%, respectively). The pooling result showed the NLR was associated with higher mortality in retrospective group (OR: 2.33, 95% CI: 1.34–4.05, P < .01) and prospective group (OR: 3.95, 95% CI: 2.54–6.14, P < .01), which was consistent with the result in whole included studies. The pooled OR for mortality in patients with age <70 years suggested the NLR could not predict the mortality (OR: 4.08, 95% CI: 0.91–18.24, P = .07), while the higher NLR was associated with mortality in patients with age >70 years (OR: 2.16, 95% CI: 1.17–3.98, P = .01). The predictive ability in patients with low mean NLR (OR: 2.61, 95% CI: 1.20–5.65, P = .02) was lower than in high NLR group (OR: 2.70, 95% CI: 1.10–6.63, P = .03). The pooled results showed there was a significant association between higher NLR and short-term mortality (OR: 2.70, 95% CI: 1.10–6.63, P = .03) and long-term mortality (OR: 2.61, 95% CI: 1.20–5.65, P = .02). Only 1 article reported the OR of NLR for mortality by univariate regression analysis (OR: 9.05, 95% CI: 3.97–20.63, P < .01), and the pooled results of 4 studies using multivariate regression analysis also suggested the higher NLR had a negative effect on the mortality in patients with COPD (OR: 2.11, 95% CI: 1.24–3.60, P < .01).
3.3. Publication bias
By using STATA 13.0, the funnel plots and Begg test showed no evidence of publication bias (Fig. 4, P = .221).
Figure 4.
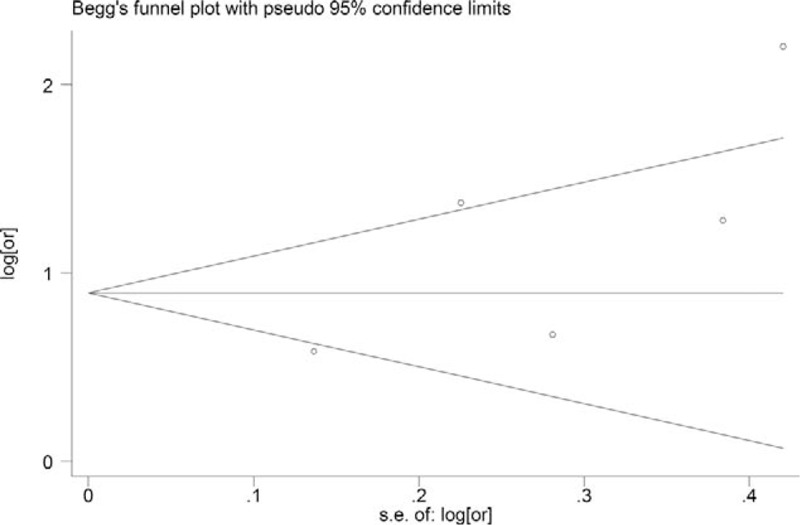
The Begg publication bias plot of the studies that reported mortality, and no publication bias was found in these studies with P = .221 for mortality.
4. Discussion
4.1. Implications
The present study aimed to identify the prognostic value of NLR for the exacerbation and mortality in patients with COPD by a meta-analysis. This study, including 9 articles of 5140 patients, suggested that the higher NLR was associated with the exacerbation of COPD. In addition, NLR was a positive prognostic marker for mortality, especially for the Asian and the patients older than 70. To our best knowledge, this is the first study to systematically evaluate the prognostic role of NLR in COPD by a meta-analysis.
The NLR was an inflammation biomarker for clinical outcomes in patients with COPD, which were caused by systemic inflammation and enhanced airway.[37] Higher NLR was reflected by increased neutrophils and decreased lymphocytes. The activated neutrophils could release the inflammatory cytokines and proteolytic enzymes (such as matrix metalloproteinase, calprotectin, and elastase), which resulted in the emphysema[24,38] and decreased FEV1.[39] Lymphocytes played an important role in immune system, and lymphopenia was associated with a high risk of infection[40,41] and mortality.[29] Thus, increase of inflammatory response (neutrophil) and reduction of immune function (lymphocytes) might explain the fact that higher NLR was associated with poor clinical outcomes in patients with COPD.
Previous studies[23,24] showed the higher NLR was negatively associated with incidence of exacerbation in COPD, while another study[27] showed no significant association by multiple regression analysis. We found the NLR was associated with the exacerbation of COPD; however, there was significant heterogeneity attributed to the study by Taylan et al.[23] After excluding the study, the result was consistent with pooling results of 3 studies. There were many factors to influence the incidence of exacerbation, such as age, smoking status, and use of inhaled corticosteroid[24]. Lee et al,[24] and Lee et al,[27] adjusted the results with body mass index, FEV1 (% predicted), and exacerbation during previous year, and also suggested the NLR was an independent predictor for the exacerbation in patients with COPD using multiple regression analysis. Thus, higher NLR increased the risk of exacerbation.
The prediction ability of NLR for mortality in patients with COPD was still on debate. Some previous studies[25,26,28,34,35] showed NLR could predict the mortality in patients with COPD, while 1 study[29] suggested the NLR was not a predictor for mortality with the use of glucocorticoid. Several studies[42,43] demonstrated the use of glucocorticoid would result in lymphopenia and neutrophilocytosis, which increased the values of NLR and influenced the prediction of NLR for mortality. However, Duman et al[34] showed that the NLR could predict the mortality independently after adjusting by use of steroid. Our pooled results showed that NLR was a predictor for mortality in patients with COPD. After subgroup analysis (Table 3), we found the heterogeneity obviously decreased in Asia group and Eurasia group, respectively, and the pooled ORs were higher in Asia group (OR: 4.48) than Eurasia group (OR: 1.82). Some studies[44,45] also reported that the higher predictive ability of NLR for various diseases was found in Asian. In addition, we found that NLR had a higher prognostic values in Asian patients. The cutoff values of NLR were different and most of studies reported a cutoff from 3 to 7. Previous studies[46,47] showed the higher cutoff would have a stronger predictive ability for clinical outcomes in tumors. The results in 1 prospective article and 4 retrospective articles also suggested NLR was a predictor for mortality, which was consistent with the results of included articles. Moreover, we found the pooled OR was higher in high mean NLR group (OR: 3.83) than low mean NLR group (OR: 2.61). This suggested the predictive ability might increase in the patients with a high mean NLR. The incidence of mortality could also be affected by other factors, such as age,[35] CRP,[26,34] and use of steroid.[34] After adjusting by other factors, the pooled results showed the NLR was an independent predictor for mortality, which was consistent with the results of 5 included articles. Thus, the NLR was an independent predictor for mortality in patients with COPD. Moreover, NLR had a higher prognostic value in Asian patients than Eurasian patients with COPD or patients with higher mean NLR.
Table 3.
Subgroup analysis results of mortality in chronic obstructive pulmonary disease.
Platelet lymphocyte ratio (PLR) in peripheral blood was also a novel inflammation biomarker. Kumar et al[48] suggested that PLR higher than 235 had a significant association with mortality. Yao et al[25] compared the prognostic values of NLR and PLR in 303 patients with COPD, and showed that NLR had a better predictive ability for mortality than PLR, with area under the curve of 0.803 and 0.639, respectively. However, only 1 study compared the NLR with the PLR, and the prognostic values of NLR and PLR in COPD may need more studies to evaluate.
The analysis of exacerbation presented significant heterogeneity and we found the heterogeneity was attributed to the study by Taylan et al.[23] This study only provided the OR of univariate regression analysis without considering other confounding factors, which might affect the results. After subgroup analysis of mortality, we found the different races resulted in the heterogeneity. After grouping by countries, there was no significant heterogeneity in Asia group and Eurasia group (Table 3).
4.2. Limitations
There were several limitations in this study. First, there were only 9 articles included this meta-analysis, and the limited number of articles for each outcome might affect the results. Second, there was significant heterogeneity in the included articles. Although we did sensitivity analysis and subgroup analysis to make the outcomes conservative, the prognostic values of NLR in COPD need more high-quality clinical evidence. In addition, this meta-analysis lacked of the data from the United States and other countries of Europe. The studies referring in the relationship between NLR and COPD in these countries could make the result more reliable in future.
4.3. Conclusion
Higher NLR may be independent predictor for the higher incidence of exacerbation and mortality in patients with COPD. In addition, NLR may have a various predictive ability for mortality in different races, and a higher predictive ability for mortality in Asian and COPD patients with higher mean NLR. Nevertheless, due to the heterogeneity, more studies were needed to verify these results.
Acknowledgments
The authors thank the reviewers for their constructive comments.
Author contributions
Conceptualization: Yongzhong Cheng, Zengpanpan Ye, Chao You.
Data curation: Zengpanpan Ye.
Formal analysis: Zengpanpan Ye, Xiaolin Ai.
Funding acquisition: Chao You.
Methodology: Xiaolin Ai, Zenglin Liao.
Software: Xiaolin Ai, Zenglin Liao.
Writing – original draft: Zengpanpan Ye, Xiaolin Ai.
Writing – review & editing: Yongzhong Cheng, Zenglin Liao, Chao You.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, COPD = chronic obstructive pulmonary disease, F = female, FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity, M = male, N = number, NLR = neutrophil to lymphocyte ratio, OR = odds ratio, PLR = platelet lymphocyte ratio, QUIPS = Quality In Prognosis Studies.
This work is supported by Science and technology supportive project of Sichuan Province. Project: Intracerebral haemorrhage prevention and diagnostic treatment skills (No. 2015SZ0051, gainer: C.Y.); Outstanding subject development 135 project: An international, multicenter, large sample randomized controlled trial of supratentorial deep intracerebral hematoma surgery and conservative treatment in adults (No. ZY2016102, gainer: C.Y.).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Asia Pacific COPD Roundtable Group. Global Initiative for Chronic Obstructive Lung Disease strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: an Asia-Pacific perspective. Respirology 2005;10:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 Report. GOLD executive summary. Am J Respir Crit Care Med 2017;195:557–82. [DOI] [PubMed] [Google Scholar]
- [3].Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Rep 2012;61:1–51. [PubMed] [Google Scholar]
- [4].Thomsen M, Ingebrigtsen TS, Marott JL, et al. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA 2013;309:2353–61. [DOI] [PubMed] [Google Scholar]
- [5].Jones PW, Agusti AG. Outcomes and markers in the assessment of chronic obstructive pulmonary disease. Eur Respir J 2006;27:822–32. [DOI] [PubMed] [Google Scholar]
- [6].Nishimura K, Izumi T, Tsukino M, et al. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 2002;121:1434–40. [DOI] [PubMed] [Google Scholar]
- [7].Cazzola M, MacNee W, Martinez FJ, et al. Outcomes for COPD pharmacological trials: from lung function to biomarkers. Eur Respir J 2008;31:416–69. [DOI] [PubMed] [Google Scholar]
- [8].Dahl M, Vestbo J, Zacho J, et al. C reactive protein and chronic obstructive pulmonary disease: a Mendelian randomisation approach. Thorax 2011;66:197–204. [DOI] [PubMed] [Google Scholar]
- [9].Silva DR, Gazzana MB, Knorst MM. C-reactive protein levels in stable COPD patients: a case-control study. Int J Chron Obstruct Pulmon Dis 2015;10:1719–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Clark TW, Medina MJ, Batham S, et al. C-reactive protein level and microbial aetiology in patients hospitalised with acute exacerbation of COPD. Eur Respir J 2015;45:76–86. [DOI] [PubMed] [Google Scholar]
- [11].Hurst JR, Perera WR, Wilkinson TM, et al. Systemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2006;173:71–8. [DOI] [PubMed] [Google Scholar]
- [12].Barouchos N, Papazafiropoulou A, Iacovidou N, et al. Comparison of tumor markers and inflammatory biomarkers in chronic obstructive pulmonary disease (COPD) exacerbations. Scand J Clin Lab Invest 2015;75:126–32. [DOI] [PubMed] [Google Scholar]
- [13].Pazarli AC, Koseoglu HI, Doruk S, et al. Procalcitonin: is it a predictor of noninvasive positive pressure ventilation necessity in acute chronic obstructive pulmonary disease exacerbation? J Res Med Sci 2012;17:1047–51. [PMC free article] [PubMed] [Google Scholar]
- [14].Karadeniz G, Aktogu S, Erer OF, et al. Predictive value of platelet-to-lymphocyte ratio in exacerbation of chronic obstructive pulmonary disease. Biomark Med 2016;10:701–10. [DOI] [PubMed] [Google Scholar]
- [15].Yin Y, Wang J, Wang X, et al. Prognostic value of the neutrophil to lymphocyte ratio in lung cancer: a meta-analysis. Clinics (Sao Paulo) 2015;70:524–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Li MX, Liu XM, Zhang XF, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review and meta-analysis. Int J Cancer 2014;134:2403–13. [DOI] [PubMed] [Google Scholar]
- [17].Tao C, Hu X, Wang J, et al. Admission neutrophil count and neutrophil to lymphocyte ratio predict 90-day outcome in intracerebral hemorrhage. Biomark Med 2017;11:33–42. [DOI] [PubMed] [Google Scholar]
- [18].Bhat T, Teli S, Rijal J, et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther 2013;11:55–9. [DOI] [PubMed] [Google Scholar]
- [19].Tokgoz S, Keskin S, Kayrak M, et al. Is neutrophil/lymphocyte ratio predict to short-term mortality in acute cerebral infarct independently from infarct volume? J Stroke Cerebrovasc Dis 2014;23:2163–8. [DOI] [PubMed] [Google Scholar]
- [20].Brooks SD, Spears C, Cummings C, et al. Admission neutrophil-lymphocyte ratio predicts 90 day outcome after endovascular stroke therapy. J Neurointerv Surg 2014;6:578–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gasteiger G, Rudensky AY. Interactions between innate and adaptive lymphocytes. Nat Rev Immunol 2014;14:631–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Gunay E, Sarinc Ulasli S, Akar O, et al. Neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease: a retrospective study. Inflammation 2014;37:374–80. [DOI] [PubMed] [Google Scholar]
- [23].Taylan M, Demir M, Kaya H, et al. Alterations of the neutrophil-lymphocyte ratio during the period of stable and acute exacerbation of chronic obstructive pulmonary disease patients. Clin Respir J 2017;11:311–7. [DOI] [PubMed] [Google Scholar]
- [24].Lee H, Um SJ, Kim YS, et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One 2016;11:e0156511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Yao C, Liu X, Tang Z. Prognostic role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis 2017;12:2285–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Xiong W, Xu M, Zhao Y, et al. Can we predict the prognosis of COPD with a routine blood test? Int J Chron Obstruct Pulmon Dis 2017;12:615–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Lee SJ, Lee HR, Lee TW, et al. Usefulness of neutrophil to lymphocyte ratio in patients with chronic obstructive pulmonary disease: a prospective observational study. Korean J Intern Med 2016;31:891–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Rahimirad S, Ghaffary MR, Rahimirad MH, et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease. Tuberk Toraks 2017;65:25–31. [PubMed] [Google Scholar]
- [29].Sorensen AK, Holmgaard DB, Mygind LH, et al. Neutrophil-to-lymphocyte ratio, calprotectin and YKL-40 in patients with chronic obstructive pulmonary disease: correlations and 5-year mortality: a cohort study. J Inflamm 2015;12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Stovold E, Beecher D, Foxlee R, et al. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst Rev 2014;3:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Fabbri LM, Hurd SS, Committee GS. Global strategy for the diagnosis, management and prevention of COPD: 2003 update. Eur Respir J 2003;22:1–2. [DOI] [PubMed] [Google Scholar]
- [32].Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med 2013;158:280–6. [DOI] [PubMed] [Google Scholar]
- [33].Kim JG, Shin H, Kim W, et al. The value of decreased thyroid hormone for predicting mortality in adult septic patients: a systematic review and meta-analysis. Sci Rep 2018;8:14137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Duman D, Aksoy E, Agca MC, et al. The utility of inflammatory markers to predict readmissions and mortality in COPD cases with or without eosinophilia. Int J Chron Obstruct Pulmon Dis 2015;10:2469–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Salturk C, Karakurt Z, Adiguzel N, et al. Does eosinophilic COPD exacerbation have a better patient outcome than non-eosinophilic in the intensive care unit? Int J Chron Obstruct Pulmon Dis 2015;10:1837–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Teng F, Ye H, Xue T. Predictive value of neutrophil to lymphocyte ratio in patients with acute exacerbation of chronic obstructive pulmonary disease. PLoS One 2018;13:e0204377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Gan WQ, Man SF, Senthilselvan A, et al. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 2004;59:574–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kim V, Rogers TJ, Criner GJ. New concepts in the pathobiology of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2008;5:478–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Gray RD, Imrie M, Boyd AC, et al. Sputum and serum calprotectin are useful biomarkers during CF exacerbation. J Cyst Fibros 2010;9:193–8. [DOI] [PubMed] [Google Scholar]
- [40].Dirnagl U, Klehmet J, Braun JS, et al. Stroke-induced immunodepression: experimental evidence and clinical relevance. Stroke 2007;382 Suppl:770–3. [DOI] [PubMed] [Google Scholar]
- [41].Drewry AM, Samra N, Skrupky LP, et al. Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock 2014;42:383–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Yu DT, Clements PJ, Paulus HE, et al. Human lymphocyte subpopulations. Effect of corticosteroids. J Clin Invest 1974;53:565–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Mishler JM, Emerson PM. Development of neutrophilia by serially increasing doses of dexamethasone. Br J Haematol 1977;36:249–57. [DOI] [PubMed] [Google Scholar]
- [44].Chen N, Liu S, Huang L, et al. Prognostic significance of neutrophil-to-lymphocyte ratio in patients with malignant pleural mesothelioma: a meta-analysis. Oncotarget 2017;8:57460–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Mei Z, Shi L, Wang B, et al. Prognostic role of pretreatment blood neutrophil-to-lymphocyte ratio in advanced cancer survivors: a systematic review and meta-analysis of 66 cohort studies. Cancer Treat Rev 2017;58:1–3. [DOI] [PubMed] [Google Scholar]
- [46].Yu Y, Qian L, Cui J. Value of neutrophil-to-lymphocyte ratio for predicting lung cancer prognosis: a meta-analysis of 7219 patients. Mol Clin Oncol 2017;7:498–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Zhao QT, Yuan Z, Zhang H, et al. Prognostic role of platelet to lymphocyte ratio in non-small cell lung cancers: a meta-analysis including 3720 patients. Int J Cancer 2016;139:164–70. [DOI] [PubMed] [Google Scholar]
- [48].Kumar P, Law S, Sriram KB. Evaluation of platelet lymphocyte ratio and 90-day mortality in patients with acute exacerbation of chronic obstructive pulmonary disease. J Thorac Dis 2017;9:1509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


