Abstract
Rationale:
Lunate dislocation is a rare injury to the wrist caused by high-energy trauma, and poor prognosis is often associated with missed initial diagnosis. To date, there is no consensus regarding an effective treatment plan for such cases.
Patient concerns:
Here, we describe the case of a 36-year-old man who presented with lunate dislocation following a delay in diagnosis of over 7 weeks, and further illuminate its diagnosis and treatment.
Diagnosis:
The diagnosis of chronic lunate dislocation was rendered.
Interventions:
The patient was treated using reduction via the dorsal approach brachial plexus anesthesia. After the reduction, a headless compression screw fixation was performed for first-stage scapholunate fusion, and Kirschner wire fixation of the lunate-triquetrum-hamate was used to stabilize the distal and proximal carpal rows.
Outcomes:
The patient was followed up for 1 year and showed wrist function recovered well; radiographic examination showed no lunate dislocation and successful scapholunate bony fusion. A satisfactory outcome was achieved.
Lessons:
The case study presented here provide evidence that performing an effective first-stage scapholunate fusion is recommended to achieve better therapeutic outcomes for a chronic lunate dislocation. Furthermore, this approach led to a good long-term clinical outcome in our case.
Keywords: Kirschner wire, lunate dislocation, missed diagnosis, scapholunate fusion
1. Introduction
Lunate dislocation is commonly associated with volar dislocation, and was first reported by Russell in 1945.[1] The causative mechanism of lunate dislocation is based on the fact that the volar portion of the lunate is wider and larger than the dorsal portion.[2] When the wrist joint is extremely extended, the volar joint capsule is pulled and ruptured, subjecting the lunate to volar dislocation as the distal radius and the capitate compress it.[2] To date, there is no consensus regarding the optimal treatment of lunate dislocations. Traditional treatments mainly include reduction of the lunate, repair of the surrounding ligaments and joint capsules, and Kirschner wire or screw fixation of the scaphoid-lunate-capitate[3–5] or scaphoid-lunate-triquetrum.[6,7] However, complications are frequent and often yield unsatisfactory results; scapholunate separation and carpal bone collapse often occur, and a secondary operation for the removal of the proximal carpal row is required, resulting in disability and teratogenicity.[8] Therefore, to maintain the stability of the wrist joint, prolong joint life, and reduce postoperative complications, we used a new treatment approach, first stage scapholunate fusion, and obtained satisfactory results. To our knowledge, this is the first case report to describe first-stage scapholunate fusion to treat a chronic lunate dislocation.
This manuscript follows the CAse REport guidelines,[9] and written informed consent was obtained from the patient for the publication of this manuscript and the accompanying images.
2. Case report
A 36-year-old man sustained an extreme extension injury of the left wrist due to an accident in October 2017 and was initially diagnosed with a fracture of the styloid process of the radius based on prehospitalized x-ray examination of the wrist (Fig. 1A, B). After 6 weeks of splinting, the patient continued to have wrist pain, swelling, and numbness. 3-dimensional computed tomography (3D-CT) showed free bone at the distal end of the radius with a sclerosed edge and volar displacement of the lunate (Fig. 2A–D); more detailed findings included an irregularly shaped distal radius, carpal bones, and metacarpal bones, and widened spaces between the lunate, triquetrum, pisiform, and distal radius. Magnetic resonance imaging indicated lunate dislocation, bone marrow edema, and fracture of the styloid process of the radius (Fig. 2E, F). On admission, in December 2017 physical examination findings revealed a bulge of the palmar bone, slight numbness in the radial three and a half fingers, limited motion range of the wrist, inability to restore thumb opposition function, and a positive Tinel's sign at the wrist. In-hospital x-ray examination showed a triangular appearance of the lunate on the posterior-anterior view and volar dislocation of the lunate on the lateral view; the capitolunate articular surface was turned to the palmar side and the continuity of the styloid process of the radius was disrupted (Fig. 3A, B). Therefore, the patient was diagnosed with a chronic left lunate dislocation accompanied by fracture of the styloid process of the radius and median nerve compression syndrome. He was hospitalized for definitive surgical treatment.
Figure 1.

A, The initial x-ray image after injury showing lunate dislocation and fracture of the styloid process of the radius. B, Lateral view of the left wrist showing volar dislocation of the lunate (arrow) and the “spilled teacup” sign. The scapholunate angle (α) is >70°.
Figure 2.
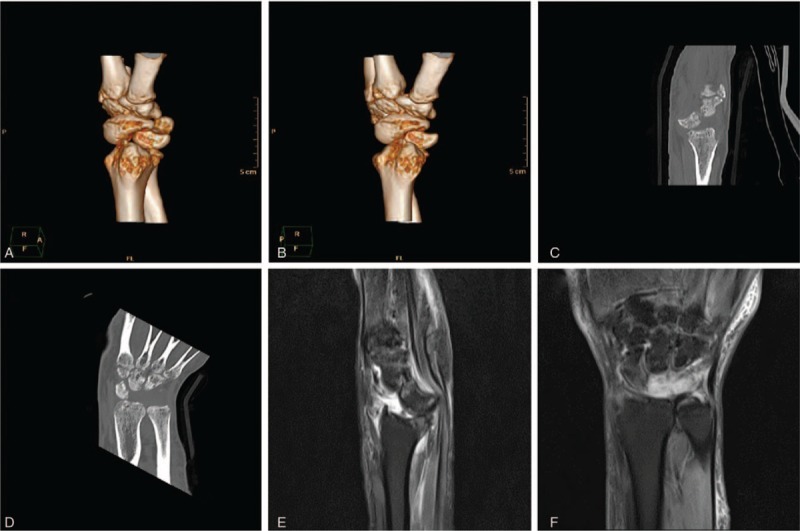
A–D, 3D-computed tomography scan showing lunate dislocation and fracture of the styloid process of the radius. E–F, Magnetic resonance image showing lunate dislocation, bone marrow edema, and fracture of the styloid process of the radius.
Figure 3.

Preoperative x-ray images. Posterior-anterior view of the left wrist showing disruption of the normally smooth arc of the radiocarpal row, as well as an abnormal scapholunate space (d) of >3 mm.
Under brachial plexus anesthesia, the patient underwent the following procedures: lunate reduction via the dorsal approach of the wrist using traction to restore the dislocation of the lunate and the capitolunate gap; correction of the rotated lunate bone to restore the normal scapholunate position, cutting the adjacent articular cartilage of the scaphoid and lunate bones until uniform bleeding was observed with the tourniquet loosened, and scapholunate fusion using a headless compression screw fixation; on the ulnar carpal side, 1 Kirschner wire was used to fix the joint of the triquetrum and lunate, and another used to fix the hamate and triquetrum through the second and third metacarpal spaces to further stabilize the proximal and distal carpal rows with a carpal height ratio of 56.75% (Fig. 4A, B). Considering that the median nerve compression symptoms had originated from the lunate dislocation which was successfully corrected, we elected not to perform a carpal nerve release.
Figure 4.

Postoperative x-ray 1 day after scapholunate fusion with a headless compression screw fixation; to stabilize the proximal and distal carpal rows, 1 Kirschner wire was used to fix the triquetrum-lunate joint, and another to fix the hamate-triquetrum joint. The carpal height ratio was 56.75%.
Immediately after surgery, the patient underwent functional fixation using a plaster cast. Six weeks after the operation, the Kirschner wires were removed and a functional exercise program initiated. The median nerve compression symptoms resolved and the carpal height ratio was 55.81% three months postoperatively (Fig. 5A, B). The patient's Mayo[10] score was 60 (fair), the disability of shoulder, arm, and hand questionnaire (DASH)[10] score was 49, and the Patient-Rated Wrist Evaluation (PRWE)[11] score was 59. Six months after surgery, radiographic images showed that the carpal height ratio was 54.35% (Fig. 6A, B). His Mayo score was 70 (fair), DASH score was 31, and PRWE score was 32. One year after surgery, radiographic images showed no dislocation of the lunate, and scapholunate bony fusion was noted. The carpal height ratio was 53.31% (Fig. 7A, B). At this time the patient's Mayo score was 90 (good), DASH score was 16, and PRWE score was 17. He exhibited satisfactory function of the wrist joint (Fig. 8).
Figure 5.

X-ray 3 months after surgery showed that the carpal height ratio was 55.81%.
Figure 6.

X-ray 6 months after surgery showed that the carpal height ratio was 54.35%.
Figure 7.

X-ray 1 year after surgery showed no dislocation of the lunate; successful scapholunate bony fusion was noted, and the carpal height ratio was 53.31%.
Figure 8.
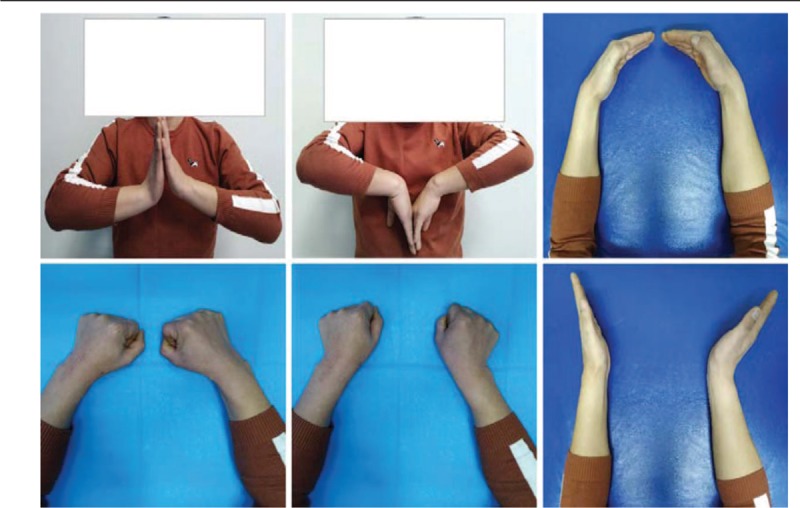
The patient showed satisfactory function of the wrist joint 1 year after surgery.
3. Discussion
Lunate dislocation is a relatively rare occurrence, accounting for <10% of all wrist injuries.[12] It often occurs after a high-energy wrist injury due to a traffic accident or a fall.[2] Acute lunate dislocation is likely to misdiagnosed at the first visit, leading to delayed treatment and poor prognosis.[13] As reported by Herzberg, about 25% of lunate dislocations and perilunate dislocations were missed at the initial visit, and only 61% were treated within the first week after injury.[12] Missed diagnosis results in median nerve compression, triggering carpal tunnel syndrome, and can induce ischemic necrosis of the lunate bone, long-term wrist instability after reduction, scapholunate separation, and carpal bone collapse, causing disability and teratogenicity.[14,15] The carpal bones are small in size, irregular in shape, complex in structure, and overlap on radiographic images. Insufficient understanding of lunate dislocations by clinicians is considered to be the most important cause of missed diagnosis.[16] In addition, lunate dislocations are often associated with fractures of the styloid process of the ulna and the radius, and other carpal bones, particularly the scaphoid. The complex nature of the situation often results in the clinician being engaged in treating other fractures, which may lead to a missed diagnosis of the lunate dislocation.[17,18]
Lunate dislocation should be suspected at the initial visit in patients with a history of extreme extension of the wrist joint. Patients with lunate dislocation often show certain characteristic findings on physical examination: the wrist joint is enlarged in the anteroposterior diameter, rounded, and swollen; the patient has difficulty performing finger flexion and dorsal extension of the wrist; there is tenderness at the transverse wrist crease; the dislocated lunate bone can be palpated; the third metacarpal bone is obviously collapsed while clenching a fist; and percussion of the metacarpal bone produces pain. When the median nerve is involved, the radial three and a half fingers have abnormal sensation, and thumb opposition function is poor.[19,20] Radiographic findings on the anteroposterior view indicate that the lunate bone has changed from a quadrangular to triangular appearance or orange-petal shape, with the tip facing the distal side and the bottom facing the proximal side; the lunate is also displaced to the ulnar side. Collectively, these findings are called the “piece of pie” sign.[21] The distal and proximal Gilula arcs of the proximal carpal rows are disrupted as well.[21,22] The lateral radiographic views indicate an abnormal axial relationship of the radius, lunate, and capitate; the lunate is rotated away from the original position and is no longer connected with the capitate, thus rotated toward the volar side, which is visually similar to the “spilled teacup” sign.[13] A CT or 3D-CT scan can be performed if necessary.[23]
There is no uniform protocol for managing lunate dislocation cases and specific treatment usually depends on the time and type of injury. Lunate dislocations are classified into 3 types according to the degree and location of the injury.[2] Type 1 involves the rupture of the posterior radiolunate ligament or an avulsion fracture of the posterior horn of the lunate leading to volar dislocation, with the convex surface facing backward and the concave surface facing forward. Type 2 involves the rupture of the posterior radiolunate ligament triggering a 270o rotation of the lunate, with the convex surface facing forward and the concave surface facing backward. Type 3 is a lunate dislocation wherein a large external force fractures the anterior and posterior radiolunate ligaments, and the lunate is displaced toward the distal radius at the volar side, with the convex surface facing backward and the concave surface facing forward. Because of the rupture of the anterior and posterior ligaments, patients with type 3 lunate dislocation have no blood supply in that area and can develop avascular necrosis of the lunate. In such cases, first-stage lunate resection or resection of the proximal carpal row is usually performed.[23,24] For type 1 and type 2 lunate dislocations, the choice of surgical approach is complex. Conventional surgical approaches include the dorsal, volar, and combined approaches.[25] However, Wu et al[26] found that the incidence of avascular necrosis associated with the volar approach to the lunate bone was 4 times that with the dorsal approach; moreover, in the treatment of a chronic lunate dislocation, the probability of avascular necrosis of the lunate bone is higher. In patients with median nerve compression, lunate reduction is achieved through a dorsal incision to restore the normal volume of the carpal tunnel, and median nerve symptoms can subsequently resolve without nerve release.[20,26] In the present case, we used a single dorsal approach to protect the volar ligament structure, avoid aggravating the damage to the blood supply of the lunate, and avert the adverse effects of scar contracture on the median nerve and wrist function.[27]
The focus of treatment for lunate dislocation is long-term preservation of the appropriate postreduction scapholunate position, because 60% of the stress to the distal carpal row is transmitted through the scaphoid-capitate joint.[28] Earlier, to ensure this, the main treatment approach was to repair the perilunate ligament and joint capsule, followed by temporary Kirschner wire fixation of the scaphoid-lunate-capitate[3–5] or scaphoid-lunate-triquetrum.[6,7] However, a simple first-stage scapholunate fixation was ineffective, as patients were prone to develop scapholunate separation and progressive carpal collapse during long-term follow-up. This is mainly because the scaphoid and lunate bones are the axes of carpal movement and the main loading-bearing column of the carpal bones. After temporary fixation of the Kirschner wire, the ligaments have poor long-term healing ability, and have insufficient strength to maintain the stability of the wrist.[7] Larson and Stern used cortical screws to permanently fasten the scapholunate joint; however, long-term follow-up results revealed that the screws could loosen due to stress. The bone density around the screw had decreased, and both scapholunate separation and carpal bone collapse occurred, resulting in persistent wrist pain and dysfunction.[8] In such cases, a second resection procedure of the proximal carpal row may be required.[29] Therefore, the use of compression screw fixation for first-stage scapholunate fusion should be considered to avoid the scapholunate separation and carpal bone collapse. The scapholunate fusion procedure was first developed in 1945.[1] Russell used it to treat recurrent scaphoid subluxation with a simple Kirschner wire fixation previously and achieved good outcomes of range of motion of the wrist. This method was then gradually adopted to treat chronic scapholunate separation.[30,31] This technique is preferred particularly when the scapholunate ligament loses its ability to recover efficiently and the scapholunate position cannot be stabilized by a simple scar repair.[30–32] Clinical studies[33,34] and cadaveric studies[35] have shown that scapholunate fusion can effectively treat scapholunate separation and improve function leading to generally satisfactory clinical results.[1,36–38] Our result in this case mirrors that experience. However, previous reports suggest that the nonunion rate is high, mainly because the contact area between the scaphoid and lunate is too small to produce stability for a solid bony union. The considerable magnitude of forces across the scapholunate joint, improper selection of internal fixation, and improper technique during surgery are also related.[35,39,40] In our case, we cut the adjacent articular cartilage of the scaphoid and lunate until there was uniform bleeding and used a headless compression screw for fixation, which may have been the main factor that contributed to the bony union in this patient. However, even if bony union cannot be achieved, studies have shown that fibrous union can provide adequate stabilization.[31,33,38]
In this case, a patient with type 1 chronic lunate dislocation[1] presented with a scapholunate space (d) of >3 mm and a scapholunate angle (α) >70°. We considered that the scapholunate ligament was avulsed from the scaphoid and/or lunate[41–44] and since the ligament was initially injured 7 weeks prior to presentation, it would have been impossible to suture or repair the ligament directly to maintain scapholunate stability.[45,46] In addition, the other perilunate ligaments had also been ruptured and lost the ability to recover effectively, making it difficult to ensure carpal bone stability; therefore, we believed that early-stage intercarpal fixation of the proximal and distal carpal rows was necessary. Previously, capitate-lunate fixation was often used to stabilize the proximal and distal carpal rows, but the operation is complex and technically difficult, and may compromise blood supply to the lunate. In the present case, the hamate-triquetrum fixation at the ulnar side was performed for proximal and distal row stabilization, and to achieve satisfactory intercarpal arrangement and avoid repeated puncture of the lunate due to the difficulty of capitate-lunate fixation. It also may have contributed to successfully achieving a scapholunate bony union. At the 1-year follow-up, there was no significant effect of the procedure upon range of motion of the wrist; function of the wrist joint was nearly normal. No dislocation or fracture occurred following scapholunate fusion, the wrist height ratio remained in the normal range (54% ± 3%),[47] and the carpal structures were stabilized. The patient's overall recovery was satisfactory. The wrist height ratio was slightly reduced, although still within normal range. This slight reduction may be attributable to the fact that although the scapholunate joint was stabilized well early on, the capitolunate ligament was not repaired, and the axial stress of the wrist joint that was transmitted to the proximal end induced a shift or rotation of the capitate due to compression between the third metacarpal bone and the fused scapholunate. However, there is no clear imaging data from the recent follow-up visit to support this hypothesis, and further long-term follow-up will be needed. Therefore, we believe that reduction using first-stage scapholunate fusion and scaphoid-lunate-capitate fusion may be a targeted treatment for a chronic lunate dislocation, which can help to avoid capitolunate separation in the long term and stabilize the proximal and distal carpal rows by capitolunate fusion.[8,31]
4. Conclusion
In summary, lunate dislocations that have not been accurately diagnosed and treated in the acute phase can be treated with careful reduction. However, long-term scapholunate separation and carpal bone collapse are unavoidable when performing temporary fixation with Kirschner wire or permanent fixation with screw. Therefore, performing an effective first-stage intercarpal fusion is recommended to achieve better therapeutic outcomes.
Author contributions
Data curation: Chao Huang, Di You, Wenlai Guo, Yuchen Hu.
Project administration: Rui Li.
Resources: Chao Huang, Wenlai Guo, Wenrui Qu, Yuchen Hu.
Writing – original draft: Chao Huang, Di You.
Writing – review and editing: Wenrui Qu, Rui Li, Zhe Zhu.
Footnotes
Abbreviations: 3D-CT = 3-dimensional computed tomography, DASH = disability of shoulder, arm and hand questionnaire, PRWE = Patient-Rated Wrist Evaluation.
Consent for publication: Written informed consent for publication of the patient's clinical details and images was obtained.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Russell TB. Inter-carpal dislocations and fracture-dislocations. J Bone Joint Surg Br 1949;31B:524–31. [PubMed] [Google Scholar]
- [2].Grabow RJ. Carpal dislocations. Hand Clin 2006;22:485–500. [DOI] [PubMed] [Google Scholar]
- [3].Zaidenberg EE, Roitman P, Gallucci GL, et al. Foreign-body reaction and osteolysis in dorsal lunate dislocation repair with bioabsorbable suture anchor. Hand (N Y) 2016;11:368–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fonseca KD, Rueger JM. Diagnostik und Therapie von perilunären Luxationen und Luxationsfrakturen. J Der Unfallchirurg 2012;115:576–81. [DOI] [PubMed] [Google Scholar]
- [5].Virani SR, Wajekar S, Mohan H, et al. A unique case of bilateral trans-scaphoid perilunate dislocation with dislocation of lunate into the forearm. J Clin Orthop Trauma 2016;7suppl 1:110–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Mahmut K, Mustafa K, Kutay Engin O, et al. Early and delayed treatment of dorsal transscaphoid perilunate fracture-dislocations 2008;22:535–40. [DOI] [PubMed] [Google Scholar]
- [7].Budoff JE. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am 2008;33:1424–32. [DOI] [PubMed] [Google Scholar]
- [8].Larson TB, Stern PJ. Reduction and association of the scaphoid and lunate procedure: short-term clinical and radiographic outcomes. J Hand Surg Am 2014;39:2168–74. [DOI] [PubMed] [Google Scholar]
- [9].Rison RA, Kidd MR, Koch CA. The CARE (CAse REport) guidelines and the standardization of case reports 2013;7:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Green DP, O’Brien ET. Open reduction of carpal dislocations: Indications and operative techniques 1978;3:250–65. [DOI] [PubMed] [Google Scholar]
- [11].Changulani M, Okonkwo U, Keswani T, et al. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop 2008;32:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Herzberg G. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am 1993;18:768–79. [DOI] [PubMed] [Google Scholar]
- [13].Perron AD, Brady WJ, Keats TE, et al. Orthopedic pitfalls in the ED: lunate and perilunate injuries. Am J Emerg Med 2001;19:157–62. [DOI] [PubMed] [Google Scholar]
- [14].Ott F, Mattiassich G, Kaulfersch C, et al. Initially unrecognised lunate dislocation as a cause of carpal tunnel syndrome. BMJ Case Rep 2013;pii: bcr2013009062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Oka Y, Tokunaga D, Fujiwara H, et al. Carpal tunnel syndrome caused by volar dislocation of the lunate in a patient with rheumatoid arthritis. Mod Rheumatol 2006;16:404–9. [DOI] [PubMed] [Google Scholar]
- [16].Çolak I, Bekler HI, Bulut G, et al. Lack of experience is a significant factor in the missed diagnosis of perilunate fracture dislocation or isolated dislocation. Acta Orthop Traumatol Turc 2018;52:32–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mudgal C, Hastings H. Scapho-lunate diastasis in fractures of the distal radius: Pathomechanics and treatment options. J Hand Surg Br 1993;18:725–9. [DOI] [PubMed] [Google Scholar]
- [18].Reichel LM, Bell BR, Michnick SM, et al. Radial styloid fractures. J Hand Surg Am 2012;37:1726–41. [DOI] [PubMed] [Google Scholar]
- [19].Chen WS. Median-nerve neuropathy associated with chronic anterior dislocation of the lunate. J Bone Joint Surg Am 1995;77:1853–7. [DOI] [PubMed] [Google Scholar]
- [20].Bhatia M, Sharma A, Ravikumar R, et al. Lunate dislocation causing median nerve entrapment. Med J Armed Forces India 2016;73:88–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Scalcione LR, Gimber LH, Ho AM, et al. Spectrum of carpal dislocations and fracture-dislocations: imaging and management. AJR Am J Roentgenol 2014;203:541–50. [DOI] [PubMed] [Google Scholar]
- [22].Sochart DH, Birdsall PD, Paul AS. Perilunate fracture-dislocation: a continually missed injury. J Accid Emerg Med 1996;13:213–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Draaijers LJ, Mick K, Mario M. Palmar dislocation of the lunate bone with complete disruption of all ligaments. A report on two cases. Acta Orthop Belg 2003;69:452–4. [PubMed] [Google Scholar]
- [24].Inoue G, Imaeda T. Management of trans-scaphoid perilunate dislocations. Arch Orthop Trauma Surg 1997;116:338–40. [DOI] [PubMed] [Google Scholar]
- [25].Capo JT, Shamian B, Nourbakhsh A, et al. Treatment of dorsal perilunate dislocations and fracture–dislocations using a standardized protocol. Hand (N Y) 2012;7:380–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wu X, Cai ZD, Lou LM, et al. Treatments for acute and old distal radius fracture with lunate dislocation. Eur J Orthop Surg Traumatol 2013;23:191–6. [DOI] [PubMed] [Google Scholar]
- [27].Green DP, O’Brien ET. Classification and management of carpal dislocations. Clin Orthop Relat Res 1980;149:55–72. [PubMed] [Google Scholar]
- [28].Viegas SF, Patterson R, Peterson P, et al. The effects of various load paths and different loads on the load transfer characteristics of the wrist. J Hand Surg Am 1989;14:458–65. [DOI] [PubMed] [Google Scholar]
- [29].Andersson JK. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev 2017;2:382–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Peterson HA, Lipscomb PR. Intercarpal arthrodesis. Arch Surg 1967;95:127–34. [DOI] [PubMed] [Google Scholar]
- [31].Hom S, Ruby LK. Attempted scapholunate arthrodesis for chronic scapholunate dissociation. J Hand Surg Am 1991;16:334–9. [DOI] [PubMed] [Google Scholar]
- [32].Stewart DT, Froelich JM, Shin AY. Intercarpal arthrodeses. J Hand Surg Am 2014;39:373–7. [DOI] [PubMed] [Google Scholar]
- [33].Pettersson K, Wagnsjö PJSJoP, Surgery R. Arthrodesis for chronic static scapholunate dissociation: a prospective study in 12 patients. Scand J Plast Reconstr Surg Hand Surg 2004;38:166–71. [DOI] [PubMed] [Google Scholar]
- [34].Zubairy AI, Jones WA. Scapholunate fusion in chronic symptomatic scapholunate instability. J Hand Surg Br 2003;28:311–4. [DOI] [PubMed] [Google Scholar]
- [35].Han KD, Kim JM, DeFazio MV, et al. Changes in wrist motion after simulated scapholunate arthrodesis: a cadaveric study. J Hand Surg Am 2016;41:e285–93. [DOI] [PubMed] [Google Scholar]
- [36].Hastings DE, Silver RL. Intercarpal arthrodesis in the management of chronic carpal instability after trauma. J Hand Surg Am 1984;9:834–40. [DOI] [PubMed] [Google Scholar]
- [37].Alnot JY, Cheveigne CD, Bleton R. Instabilité scapho-lunaire chronique post-traumatique traitée par arthrodèse scapho-lunaire. J Annales De Chirurgie De La Main Et Du Membre Supérieur 1992;11:107–18. [DOI] [PubMed] [Google Scholar]
- [38].Howard FM, Fahey T, Wojcik E, et al. Rotatory subluxation of the navicular. Clin Orthop Relat Res 1974;104:134–9. [DOI] [PubMed] [Google Scholar]
- [39].Linscheid RL, Dobyns JH. Treatment of scapholunate dissociation. Rotatory subluxation of the scaphoid. Hand Clin 1992;8:645–52. [PubMed] [Google Scholar]
- [40].Siegel JM, Ruby LK. A critical look at intercarpal arthrodesis: review of the literature. J Hand Surg Am 1996;21:717–23. [DOI] [PubMed] [Google Scholar]
- [41].Pappou IP, Basel J, Deal DN. Scapholunate ligament injuries: a review of current concepts. Hand (N Y) 2013;8:146–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Sulkers GS, Schep NW, Maas M, et al. The diagnostic accuracy of wrist cineradiography in diagnosing scapholunate dissociation. J Hand Surg Eur Vol 2014;39:263–71. [DOI] [PubMed] [Google Scholar]
- [43].Tucker A, Marley W, Ruiz A. Radiological signs of a true lunate dislocation. BMJ 2013;pii: bcr2013009446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Harvey C, Moran SL. Wrist essentials: the diagnosis and management of scapholunate ligament injuries. Plast Reconstr Surg 2014;134:312e–22e. [DOI] [PubMed] [Google Scholar]
- [45].Beredjiklian PK, Dugas J, Gerwin M. Primary repair of the scapholunate ligament. Tech Hand Up Extrem Surg 1998;2:269–73. [DOI] [PubMed] [Google Scholar]
- [46].Bickert B, Sauerbier M, Germann G. Scapholunate ligament repair using the Mitek TM bone anchor: technique and preliminary results. J Hand Surg 2000;25:188–92. [DOI] [PubMed] [Google Scholar]
- [47].Green DP, Hotchkiss RN, Pederson WC, Green's Operative Hand Surgery. 4th ed. Sidcup, Kent, UK: Churchill Livingstone; 1998. [Google Scholar]


