Supplemental Digital Content is available in the text
Keywords: CT-imaging, neuroimaging, non-pediatric departments, pediatric departments, pediatric minor brain injury
Abstract
To investigate the use of neuroimaging in children and adolescents with minor brain injury in pediatric and non-pediatric departments.
In this observational cohort study data were extracted from a large German statutory health insurance (AOK Plus Dresden ∼3.1 million clients) in a 7-year period (2010–2016). All patients with International Classification of Diseases (ICD) code S06.0 (concussion; minor brain injury; commotio cerebri) aged ≤ 18 years were included. Demographic and clinical data were analyzed by logistic regression analysis for associations with the use of CT and MRI (independent variables: gender, age, length of stay, pediatric vs non-pediatric department, university vs non-university hospital).
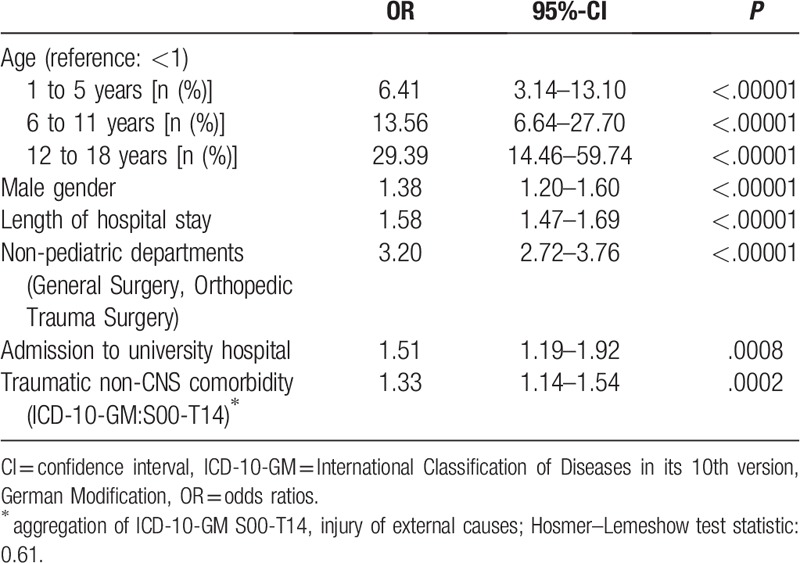
A total of 14,805 children with minor brain injuries (mean age 6.0 ± 5.6; 45.5% females) were included. Treatment was provided by different medical departments: Pediatrics (N = 8717; 59%), Pediatric Surgery (N = 3582, 24%), General Surgery (N = 2197, 15%), Orthopedic Trauma Surgery (N = 309, 2.1%). Patients admitted to pediatric departments (Pediatrics and Pediatric Surgery) underwent head CT-imaging significantly less frequently (3.8%) compared to patients treated in non-pediatric departments (18.5%; P < .001; General Surgery: 15.6%; Orthopedic Trauma Surgery: 39.2%). Logistic regression confirmed a significantly higher odds ratio (OR) for the use of cranial CT by the non-pediatric departments (OR: 3.2 [95-%-CI: 2.72–3.76]).
CT was significantly less frequently used in pediatric departments. Educational efforts and quality improvement initiatives on physicians, especially in non-pediatric departments may be an effective approach to decreasing rates of CT after minor traumatic brain injuries.
1. Introduction
For children and adolescents an incidence of 185 per 100,000 for minor traumatic brain injuries is reported.[1,2] A cranial computed tomography (CT) scan is still the imaging modality of choice to identify intracranial brain injuries and skull fractures.[3–5] Correspondingly, 5% to 70% of blunt head trauma is evaluated by CT.[4] However, the potential long-term consequences of radiation exposure in children and the increased risk of cancer mortality requires a judiciously use of this imaging modality.[6,7] Therefore, in this observational cohort study, we analyzed the use of neuroimaging in children and adolescents with minor traumatic brain injuries in pediatric and non-pediatric departments in Germany.
2. Methods
The study was approved by the local institutional review board (IRB 00001750). Data were extracted from a large German statutory health insurance fund AOK Plus – Die Gesundheitskasse für Sachsen und Thüringen (3.1 million clients) in a 7-year period (2010–2016). Previous studies have demonstrated that claims data are an appropriate source of evidence regarding pediatric health services research.[8–10] Diagnosis and procedures were made based on the German modification of International Classification of Diseases in its 10th version (ICD-10-GM) and on the International Classification of Procedures in Medicine (ICPM). Participating researchers confirmed standards of data protection according to the Good Practice Secondary Data Analysis (GPS).[11] The study protocol was established in accordance to the ethical guidelines of the 1975 Declaration of Helsinki. All patients with ICD-10-GM code S06.0 (concussion; minor brain injury; commotio cerebri) aged ≤ 18 years who had been continuous members of the AOK Plus for at least one year after their index diagnosis were included. The ICD-10-GM code S06.0 defines a minor traumatic head injury with a temporary loss of brain function. Concussion may cause a variety of physical, cognitive, and emotional symptoms (loss of consciousness, memory loss, nausea, headache, difficulty with concentration, balance, mood), which may not be recognized if subtle. According to the ICPM the study population was further divided into 4 subgroups: “Native Computed Tomography (CT)” of the head (OPS code 3–200), ”Native Magnetic Resonance Imaging (MRI)” of the head (OPS code 3–800), “CT and MRI” and “no neuroimaging”. Patient characteristics such as age, gender, type of department (pediatrics, pediatric surgery, general surgery, orthopedic trauma surgery, neurosurgery and neurology), type of hospital (university hospital/non-university hospital), neuroimaging modality (CT, MRI, CT or MRI, CT&MRI), length of hospital stay, and traumatic non-CNS comorbidity were evaluated.
Data were analyzed using descriptive statistics as well as multivariate regression methods. Chi-Squared tests were used to investigate the relationship between two categorical variables and Wilcoxon Rank–Sum–Test for continuous variables. Reported coefficients from the logistic regression models are Odds Ratios. Demographic and clinical data were processed by logistic regression analysis of the use of neuroimaging defined as CT or MRI (independent variables: age, gender, length of hospital stay, pediatric vs non-pediatric department, university vs non-university hospital). Furthermore, we checked for multicollinearity by tolerance and variance inflation factor and fit of the model by Hosmer and Lemeshow goodness-of-fit test. Statistical analysis was performed using SAS version 9.4 and SAS Enterprise Guide 6.1.
3. Results
A total of 14,805 children with minor traumatic brain injuries (mean age 6.0 ± 5.6; 45.5% females) were included. Treatment was provided by different medical departments: Pediatrics (N = 8717; 58.8%), Pediatric Surgery (N = 3582; 24.2%), General Surgery (N = 2197; 14.8%), Orthopedic Trauma Surgery (N = 309; 2.1%), Neurosurgery (N = 11; <1%) and Neurology (N = 4; <1%). The mean length of stay of all patients was 1.95 ± 1.02 days; 1907 (12.9%) individuals were treated at a university hospital. Due to very low patient numbers, children admitted to Neurosurgery or Neurology were excluded from further analysis for reasons of data protection and lack of statistical power.
Patients admitted to pediatric departments (Pediatrics and Pediatric Surgery) underwent neuroimaging (CT or MRI) significantly less frequently (5.6%) compared to patients treated in non-pediatric departments (20.4%; P < .001) (Table 1). The rate of cranial CT was 3.8% in pediatric departments (Pediatrics: 3.8%, Pediatric Surgery: 3.6%) versus 18.5% in non-pediatric departments (General Surgery: 15.6%; Orthopedic Trauma Surgery: 39.2%; Table 1). Logistic regression confirmed a significantly higher odds ratio (OR) for the use of neuroimaging (CT or MRI) by the non-pediatric departments (OR: 2.3 [95%-CI: 2.01–2.71]; Table 2). The estimated odds ratio for use of cranial CT only was even higher (OR: 3.2 [95%-CI: 2.72–3.76]; Table 3). The likelihood that a pediatric patient with minor traumatic brain injury underwent evaluation by a CT scan increased 3.2-fold if the child was treated in non-pediatric departments. Other factors associated with the use of neuroimaging included age, male gender, length of hospital stay, admission to a university hospital (vs a non-university hospital), traumatic non-CNS comorbidity (Tables 2 and 3). Analysis of different age groups showed that the chance for the use of cranial CT increased 14-fold for patients aged 6 to 11 years and 29-fold in children older than 11 years (Table 3).
Table 1.
Patient characteristics.
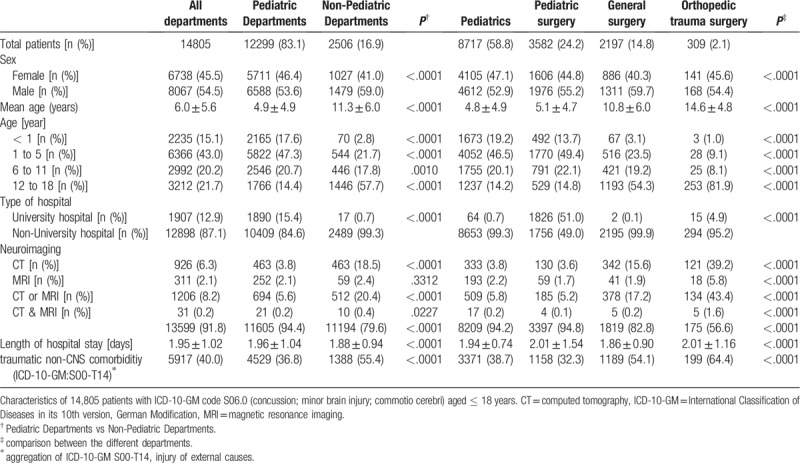
Table 2.
Estimated odds ratios for use of neuroimaging vs no use of neuroimaging.
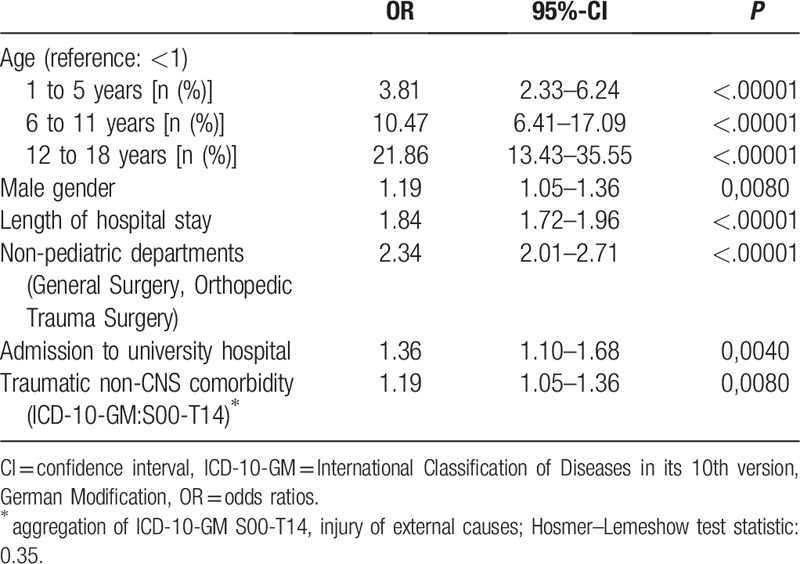
Table 3.
Estimated odds ratios for use of CT vs no CT.
In contrast, the examination of the data concerning MRI as imaging modality showed no significant difference between pediatric (2.1%) and non-pediatric departments (2.4%; P = .33) (Table 1, Supplement 1). The logistic regression revealed a lesser likelihood for the use of MRI in pediatric departments. However, these results seem not be reliable because the Hosmer and Lemeshow goodness-of-fit test was significant (P = .02) indicating an inadequate model specification (data not shown).
4. Discussion
In this observational cohort study, we set out to evaluate the usage of neuroimaging in children and adolescents with minor traumatic brain injury (concussion) in pediatric and non-pediatric departments. We used the database of a large German statutory health insurance fund AOK Plus – Die Gesundheitskasse für Sachsen und Thüringen (3.1 million clients) in a 7-year period (2010–2016). Therefore, we were able to analyze a representative number of patients.
A cranial CT scan is still the imaging modality of choice to identify traumatic brain injuries and skull fractures in children and adults.[3–5] However, there is controversy regarding the use of neuroimaging for pediatric head injuries. Only 10% of CT scans show findings related to traumatic brain injury and less than 1% of children with minor head trauma and a CT scan require neurosurgical intervention.[12]
Considering the potential long-term consequences of radiation exposure during childhood the use of a cranial CT scan in the diagnostic workup of children with minor head injuries is of special concern. In our study there was a great variation in the rate of neuroimaging among different medical disciplines ranging from 5.2% to 43.4% (Table 1). This practice variation in the use of CT is well in line with data from earlier studies.[3–5,13,14] In a large prospective cohort study with more than 42,000 children, Kuppermann et al reported that 35.3% of pediatric patients with minor head injury obtained a CT scan. They identified a large group of children in whom CT could have been avoided. Moreover, they developed and validated an age-specific algorithm to predict relevant intracranial injury for guiding physicians to efficiently use cranial CT scans.[15] However, evidence-based decision instruments are not consistently applied by physicians in their daily practice.[16–19] It remains unknown how these guidelines influence practice patterns and whether they can reduce CT scans in children and adolescents with minor head injury.[3] Correspondingly, Lenstra et al demonstrated a significant increase in CT-assessments for mild traumatic head trauma despite the implementation of a guideline for CT-assessment based on certain risk factors.[20] Treatment in a pediatric department (Pediatrics and Pediatric Surgery) was associated with a significantly lower frequency of CT compared to patients treated in non-pediatric departments (Table 1). This finding is similar to other studies.[3–5,12,21,22] We hypothesize that physicians with Pediatric or Pediatric Surgical training have clinical skills and experience that enable them to manage children with minor head injuries without neuroimaging. Additionally, they may have a sharpened awareness of the potential long-term consequences of radiation exposure in children, which is associated with an increased risk of cancer mortality.[6,7] Moreover, pediatric departments usually collaborate with pediatric radiologists who ensure that radiation is limited to a minimum. Although there is no upper dose limit at the individual level, in individual cases as much radiation can be used as necessary for diagnostics. However, there are diagnostic reference levels (DRLs) which serve as orientation and should not be exceeded in the majority of cases. At the European level, DRLs have been defined and published in the “European Guidelines on Diagnostic Reference Levels for Paediatric Imaging.”[23] Even if these DRLs are complied with, there is a relevant additional radiation exposure. Therefore, the replacement of CT examinations by radiation free MRI examinations should be the focus of radiation protection.
Our analysis of data concerning MRI as alternative imaging modality showed a lesser likelihood for the use of MRI in pediatric departments compared to non-pediatric departments. However, due to statistical reasons we could not further analyze or verify this finding.
Other factors associated with the use of neuroimaging included age, male gender, length of hospital stay, admission to a university hospital (vs a non-university hospital), and traumatic non-CNS comorbidity.
Associations between head imaging and patient age in children up to 18 years of age have been demonstrated before.[5] It is unclear why neuroimaging is obtained more frequent with increasing age, especially in teenagers. Mannix et al speculated that the mechanisms of injury in this age group might be more concerning.[3] Moreover, the possibility to perform neuroimaging in teenagers without sedation may contribute to this finding.
It has been shown repeatedly that boys sustain more frequent and more severe injuries than girls.[24,25] Explanations for these gender differences take account of parental socialization, cognitive appraisals of injury risk and individual differences in child behavior patterns.[24] These factors in combination with more concerning mechanisms of injury may lead to a lower threshold for CT assessment in the diagnostic evaluation of blunt head trauma in boys.
In our study, concomitant traumatic non-CNS injuries were associated with the use of neuroimaging. One explanation for this finding may be that patients who present with additional traumatic non-CNS injuries are more likely to be triaged as more severely injured resulting in a higher use rate of CT and MRI in general, which may include neuroimaging. This might also be a possible explanation for the association with lengthened hospital stay which may be prolonged due to traumatic non-CNS injuries.
Logistic regression confirmed that admission to a university hospital (vs a non-university hospital) was associated with the use of cranial CT imaging. Marin et al demonstrated that designated trauma centers are more likely to perform cranial CT imaging for pediatric head trauma.[16] They assumed that this reflects the consistent and protocolized approach of these centers to the care of injured patients. University hospitals (in Germany) are designated trauma centers with highly standardized and protocolized procedures in the ED. With respect to Marin et al this might be one cause for the association between hospital type (university hospital vs a non-university hospital) and CT rate.
We are aware of several limitations of our study. Patient data included demographics, diagnosis and procedure codes. The accuracy of coding may have been affected by hospital coding practices. Therefore, it may be possible that the results were influenced by misclassification of the imaging outcomes. In addition, claims data are primarily collected for accounting purposes. This results in missing information for some variables, e.g., the severity of the disease. Accordingly, there was no information of the initial or subsequent state of consciousness (Glasgow Coma Scale) and the decision to use neuroimaging could not be entirely reconstructed. Finally, local standards, technical and personnel resources and the setting in which the primary evaluation took place may have been important confounders influencing the variability of neuroimaging rates.
5. Conclusion
In this study we demonstrated substantial variation in the use of neuroimaging for managing children and adolescents with minor traumatic head trauma in Germany. CT was significantly less frequently used in pediatric departments. Educational efforts and quality improvement initiatives on physicians, especially in non-pediatric departments may be an effective approach to decrease the rate of CT scans ordered to evaluate minor pediatric head trauma.
Author contributions
Conceptualization: Mike Klora, Jan Zeidler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Data curation: Mike Klora, Jan Zeidler, Stefan Bassler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Formal analysis: Mike Klora, Jan Zeidler, Stefan Bassler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Funding acquisition: Peter Zimmermann.
Investigation: Mike Klora, Jan Zeidler, Stefan Bassler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Methodology: Mike Klora, Jan Zeidler, Stefan Bassler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Project administration: Peter Zimmermann.
Resources: Mike Klora, Jan Zeidler, Stefan Bassler.
Software: Mike Klora, Jan Zeidler, Stefan Bassler.
Supervision: Jan Zeidler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Validation: Mike Klora, Jan Zeidler, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Visualization: Mike Klora, Jan Zeidler, Peter Zimmermann.
Writing – original draft: Mike Klora, Peter Zimmermann.
Writing – review & editing: Jan Zeidler, Stefan Bassler, Franz Wolfgang Hirsch, Jan-Hendrik Gosemann, Martin Lacher, Peter Zimmermann.
Supplementary Material
Footnotes
Abbreviations: AOK = Allgemeine Ortskrankenkasse, CNS = central nervous system, CT = computed tomography, GPS = Good Practice Secondary Data Analysis, ICD = International Classification of Diseases, ICD-10-GM = International Classification of Diseases in its 10th version, German Modification, ICPM = International Classification of Procedures in Medicine, IRB = institutional review board, MRI = Magnetic Resonance Imaging, OPS = Operationen- und Prozedurenschlüssel (ICPM, German Modification), OR = odds ratio, SAS = statistical analysis system.
ORCID ID: 0000-0001-6571-5283.
We acknowledge support from the German Research Foundation (DFG) and Leipzig University within the program of Open Access Publishing.
We give explicit assurance that each of the listed authors meets each of the authorship requirements as stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals (www.icmje.org).
The study was approved by the local institutional review board (IRB 00001750). This article does not contain any studies with human participants or animals performed by any of the authors.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Rickels E, von Wild K, Wenzlaff P. Treatment of traumatic brain injury in Germany. Unfallchirurg 2011;114:417–23. [DOI] [PubMed] [Google Scholar]
- [2].Wendling-Keim DS, König A, Dietz HG, et al. Ambulatory or inpatient management of mild TBI in children: a post-concussion analysis. Pediatr Surg Int 2017;33:249–61. [DOI] [PubMed] [Google Scholar]
- [3].Mannix R, Meehan WP, Monuteaux MC, et al. Computed tomography for minor head injury: variation and trends in major United States pediatric emergency departments. J Pediatr 2012;160:136–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Stanley RM, Hoyle JD, Jr, Dayan PS, et al. Emergency department practice variation in computed tomography use for children with minor blunt head trauma. J Pediatr 2014;165:1201–6. [DOI] [PubMed] [Google Scholar]
- [5].Blackwell CD, Gorelick M, Holmes JF, et al. Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Ann Emerg Med 2007;49:320–4. [DOI] [PubMed] [Google Scholar]
- [6].Brenner DJ. Estimating cancer risks from pediatric CT: going from the qualitative to the quantitative. Pediatr Radiol 2002;32:228–33. [DOI] [PubMed] [Google Scholar]
- [7].Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176:289–96. [DOI] [PubMed] [Google Scholar]
- [8].Gosemann JH, Lange A, Zeidler J, et al. Appendectomy in the pediatric population - a German nationwide cohort analysis. Langenbecks Arch Surg 2016;401:651–9. [DOI] [PubMed] [Google Scholar]
- [9].Dingemann C, Dietrich J, Zeidler J, et al. Early complications after esophageal atresia repair: analysis of a German health insurance database covering a population of 8 million. Dis Esophagus 2016;29:780–6. [DOI] [PubMed] [Google Scholar]
- [10].Dingemann C, Dietrich J, Zeidler J, et al. Surgical management of congenital abdominal wall defects in Germany: a population-based study and comparison with literature reports. Eur J Pediatr Surg 2017;27:516–25. [DOI] [PubMed] [Google Scholar]
- [11].AGENS, DGSMP, DGEpi, GMDS. GPS - good practice in secondary data analysis: revision after fundamental reworking;2008. _http://dgepi.de/fileadmin/pdf/leitlinien/gps-version2-final_ENG.pdf_.[accessed 5 June 2015]. [Google Scholar]
- [12].Mannix R, Bourgeois FT, Schutzman SA, et al. Neuroimaging for pediatric head trauma: do patient and hospital characteristics influence who gets imaged? Acad Emerg Med 2010;17:694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Maguire JL, Boutis K, Uleryk EM, et al. Should a headinjured child receive a head CT scan? A systematic review of clinical prediction rules. Pediatrics 2009;124:145–54. [DOI] [PubMed] [Google Scholar]
- [14].Klassen TP, Reed MH, Stiell IG, et al. Variation in utilization of computed tomography scanning for the investigation of minor head trauma in children: a Canadian experience. Acad Emerg Med 2000;7:739–44. [DOI] [PubMed] [Google Scholar]
- [15].Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically important brain injuries after head trauma: a prospective cohort study. Lancet 2009;374:1160–70. [DOI] [PubMed] [Google Scholar]
- [16].Marin JR, Weaver MD, Barnato AE, et al. Variation in emergency department head computed tomography use for paediatric head trauma. Acad Emerg Med 2014;21:987–95. [DOI] [PubMed] [Google Scholar]
- [17].Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999;282:1458–65. [DOI] [PubMed] [Google Scholar]
- [18].Sood R, Sood A, Ghosh AK. Non-evidence-based variables affecting physicians’ test-ordering tendencies: a systematic review. Neth J Med 2007;65:167–77. [PubMed] [Google Scholar]
- [19].Bautista AB, Burgos A, Nickel BJ, et al. Do clinicians use the American College of Radiology appropriateness criteria in the management of their patients? AJR 2009;192:1581–5. [DOI] [PubMed] [Google Scholar]
- [20].Lenstra JJ, Pikstra ARA, Fock JM, et al. Influence of guidelines on management of paediatric mild traumatic brain injury: CT-assessment and admission policy. Eur J Paediatr Neurol 2017;21:816–22. [DOI] [PubMed] [Google Scholar]
- [21].Stiell IG, Wells GA, Vandemheen K, et al. Variation in ED use of computed tomography for patients with minor head injury. Ann Emerg Med 1997;30:14–22. [DOI] [PubMed] [Google Scholar]
- [22].Commission on Clinical Policies and Research, American Academy of Pediatrics. Committee on Quality Improvement, American Academy of Pediatrics. The management of minor closed head injury in children. Pediatrics 1999;104:1407–15. [PubMed] [Google Scholar]
- [23].Granata C, Sorantin E, Seuri R, Owens CM. European Society of Paediatric Radiology Computed Tomography and Dose Task Force: European guidelines on diagnostic reference levels for paediatric imaging. Pediatr Radiol 2019;495:702–5. doi: 10.1007/s00247-019-04346-z. Epub 2019 Feb 19. [DOI] [PubMed] [Google Scholar]
- [24].Karazsia BT1, Guilfoyle SM, Wildman BG. The mediating role of hyperactivity and inattention on sex differences in paediatric injury risk. Child Care Health Dev 2012;38:358–65. [DOI] [PubMed] [Google Scholar]
- [25].Rivara FP. Epidemiology of childhood injuries: review of current research and presentation of conceptual framework. Arch Pediatr Adoles Med 1998;136:399–405. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


